Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Pathophysiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Frozen section description | Frozen section images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Lechner A, Parra-Herran C. Colorectal adenocarcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/ovarytumorcolorectaladeno.html. Accessed April 3rd, 2025.
Definition / general
- Secondary ovarian involvement by colorectal cancer (CRC) is, by definition, evidence of advanced tumor stage (pM1)
- There is significant overlap of clinical, radiologic and pathologic features between primary and metastatic ovarian adenocarcinoma
- In the workup of mucinous or endometrioid-like ovarian neoplasms, a secondary malignancy should always be excluded, either pathologically or clinically
Essential features
- Mimic of primary ovarian endometrioid or mucinous adenocarcinoma
- Most common metastatic tumor to ovary; usually arising from rectosigmoid colon (Int J Colorectal Dis 2020;35:1035)
- Usual gross morphologic features of ovarian metastasis (bilateral, < 10 cm, surface involvement) may not be seen
- Variably sized glands, nuclear atypia that is more pronounced than in ovarian primary, dirty necrosis, multinodular / infiltrative growth
- SATB2+, CK20+, CDX2+, CK7-, PAX8-
Terminology
- Metastases to the ovary (OM) are also known as secondary tumors of ovary (STO)
- Although commonly used to refer to all metastatic carcinoma involving the ovary, Krukenberg tumor (KT) strictly refers to adenocarcinoma with signet ring cell differentiation, most of which (76%) arise from the stomach (Am J Surg Pathol 2006;30:277)
ICD coding
Epidemiology
- Rate of OM among all ovarian malignancies varies from 15 - 30% (Int J Gynecol Cancer 2006;16:132, Virchows Arch 2015;467:79, Anal Quant Cytopathol Histpathol 2013;35:241)
- Between 10 - 33% of OM are from CRC, which is the most common primary tumor type (World J Gastrointest Surg 2010;2:109, Virchows Arch 2015;467:79, Anal Quant Cytopathol Histpathol 2013;35:241)
- Median age is 51 - 60 years; 24% are 40 years or younger (World J Gastrointest Surg 2010;2:109, Virchows Arch 2015;467:79, Anal Quant Cytopathol Histpathol 2013;35:241)
- 3.4 - 4.2% of women with CRC present with or will develop OM (Int J Colorectal Dis 2020;35:1035, Int J Colorectal Dis 2021;36:2567)
- Slightly more frequent in premenopausal / perimenopausal (≤ 55 years) women (Int J Colorectal Dis 2021;36:2567)
Pathophysiology
- Spread to the ovaries can be hematogenous, lymphatic, transperitoneal or by direct extension (Clin Exp Metastasis 2017;34:295)
- Hematogenous spread may be more important for colorectal primary than other sites of origin (Obstet Gynecol Int 2011;2011:612817)
Diagrams / tables
- See Figure 5 for algorithm to determine origin using currently available markers: Int J Gynecol Pathol 2016;35:191
Table 1. Most common immunohistochemical expression
patterns seen in primary ovarian mucinous neoplasms and
secondary epithelial tumors from gastrointestinal origin
| Lower GI | Upper GI | Ovarian | |
| CK7 | Negative | Positive | Positive |
| SATB2 | Positive | Negative | Negative |
| PAX8 | Negative | Negative | Positive* |
| CK20 | Positive | Pos / neg | Pos / neg |
| CDX2 | Positive | Pos / neg | Pos / neg |
| MUC2 | Positive | Pos / neg | Pos / neg |
| ER | Negative | Negative | Pos / neg |
| Beta catenin | Pos / neg | Negative | Negative |
| MUC1 | Pos / neg | Positive | Positive |
- GI = gastrointestinal; pos = positive; neg = negative
- In this table, positive markers are those with expression in > 75% and negative markers those with expression in < 25% of tumors in the indicated category
- Expression ranging from 25 to 75% is coded as pos / neg
- *PAX8 expression was 75% in all primary ovarian neoplasms but lower in the subgroup of primary ovarian carcinomas (65%)
- Table contents adapted from Int J Gynecol Pathol 2016;35:191
Clinical features
- Most patients manifest changes in bowel habits, rectal bleeding and bloating; constitutional symptoms are less frequent
- Symptoms related to a pelvic mass include abdominal pain, discomfort or bowel obstruction
- Abnormal vaginal bleeding or even virilization may result from metastasis induced luteinization of the ovarian stroma (Am J Surg Pathol 2006;30:277)
- Mean size of the metastatic lesion usually exceeds the size of the primary tumor
- Right sided CRC with OM is more likely to present with peritoneal carcinomatosis than those with left sided primary (Curr Oncol 2021;28:2914)
- Most cases are stage pT3 (full thickness wall involvement) or pT4 (perforation of visceral peritoneum or direct invasion of adjacent structures); nodal involvement occurs in 87% (Int J Clin Oncol 2020;25:1822)
- Left sided CRC is more common among OM (Curr Oncol 2021;28:2914)
- Rectosigmoid is most common site (Int J Colorectal Dis 2020;35:1035, Virchows Arch 2015;467:79)
Diagnosis
- Imaging is not reliable in distinguishing STO from primary malignancy; definitive diagnosis requires pathologic evaluation
Laboratory
- Elevated CA125 levels (> 100 U/mL) are more characteristic of primary ovarian malignancy but may be seen in OM (J Gastrointest Oncol 2021;12:226)
- In the setting of known CRC, elevated CA125 may suggest OM
- CA125:CEA ratio < 25 is common and accurately excludes ovarian primary; CA19-9 may be elevated but is more specific for pancreaticobiliary origin (Indian J Surg Oncol 2021;12:152)
Radiology description
- On imaging, the ovarian mass often has cystic and solid components (Int J Clin Oncol 2020;25:1663)
- Palisading layered structures (mille-feuille sign) were specific for colorectal origin in one study (Eur J Radiol 2020;124:108823)
- Necrosis is common (Transl Cancer Res 2021;10:3248)
- Smooth mass margin (contour) on CT is seen in most lesions (92%), compared to primary ovarian tumors (45%) (Abdom Radiol (NY) 2019;44:1493, J Comput Assist Tomogr 2005;29:69)
Prognostic factors
- Median survival of 25.5 months when ovary is sole site of metastasis (Int J Colorectal Dis 2020;35:1035)
- Poor prognostic factors (Int J Colorectal Dis 2020;35:1035, Int J Clin Oncol 2020;25:1822):
- Additional sites of metastasis
- Residual disease after cytoreductive surgery
- Poorly differentiated or undifferentiated tumor or signet ring cell differentiation
- Age ≥ 70
Case reports
- 29 year old woman with cystic ovarian lesion found 1 month after low anterior resection for pT4bN1b CRC (J Gastrointest Oncol 2021;12:3141)
- 44 year old woman with menorrhagia and a mixed cystic and solid adnexal mass (Radiol Case Rep 2021;16:2799)
- 74 year old woman with pelvic mass, elevated CA125 and CA19-9 (Medicine (Baltimore) 2019;98:e17782)
Treatment
- Given the high frequency of ovarian involvement by CRC and the high proportion of cases that are unsuspected before oophorectomy, preoperative investigation in a patient with an ovarian mass should include consideration for colonoscopy (Int J Gynecol Pathol 2008;27:182)
- Prophylactic oophorectomy is not universally recommended in the setting of known CRC but has been considered in certain contexts (e.g., postmenopausal, synchronous cystic ovarian lesions, ovarian tethering to site of primary tumor, pelvic ascites accumulation) (Updates Surg 2021;73:391)
- Cytoreductive surgery with adjuvant chemotherapy (particularly hyperthermic intraperitoneal chemotherapy [HIPEC]) shows improved survival over primary resection or palliative treatment alone (Int J Colorectal Dis 2020;35:1035, J Gastrointest Oncol 2021;12:226)
Gross description
- Bilateral in 45 - 59% of cases; left sided colorectal primary is most likely to present with unilateral OM (Curr Oncol 2021;28:2914, Int J Clin Oncol 2020;25:1663, Eur J Radiol 2020;124:108823)
- Mass is frequently complex (solid and cystic) or purely solid with multinodular growth (Int J Clin Oncol 2020;25:1822, J Gastrointest Oncol 2021;12:226)
- Purely cystic unilocular lesions are rare
- Surface involvement varies (Curr Oncol 2021;28:2914):
- Right sided primary (58%)
- Left sided primary (25%)
- Although OM are generally smaller (< 10 cm) than ovarian primaries, OM from CRC can be large ranging from 5 - 20 cm (Int J Clin Oncol 2020;25:1822)
- A simple size and laterality algorithm accurately distinguishes OM from primary ovarian malignancy in several metastatic tumor types; however, metastatic CRC appears to routinely violate this model (Am J Surg Pathol 2008;32:128)
Frozen section description
- OM can frequently be mistaken for primary ovarian malignancy on frozen section, particularly in the setting of an occult primary (Int J Gynecol Pathol 2005;24:356)
- Useful features to suggest OM include:
- Bilateral
- Small (< 10 cm)
- Surface involvement
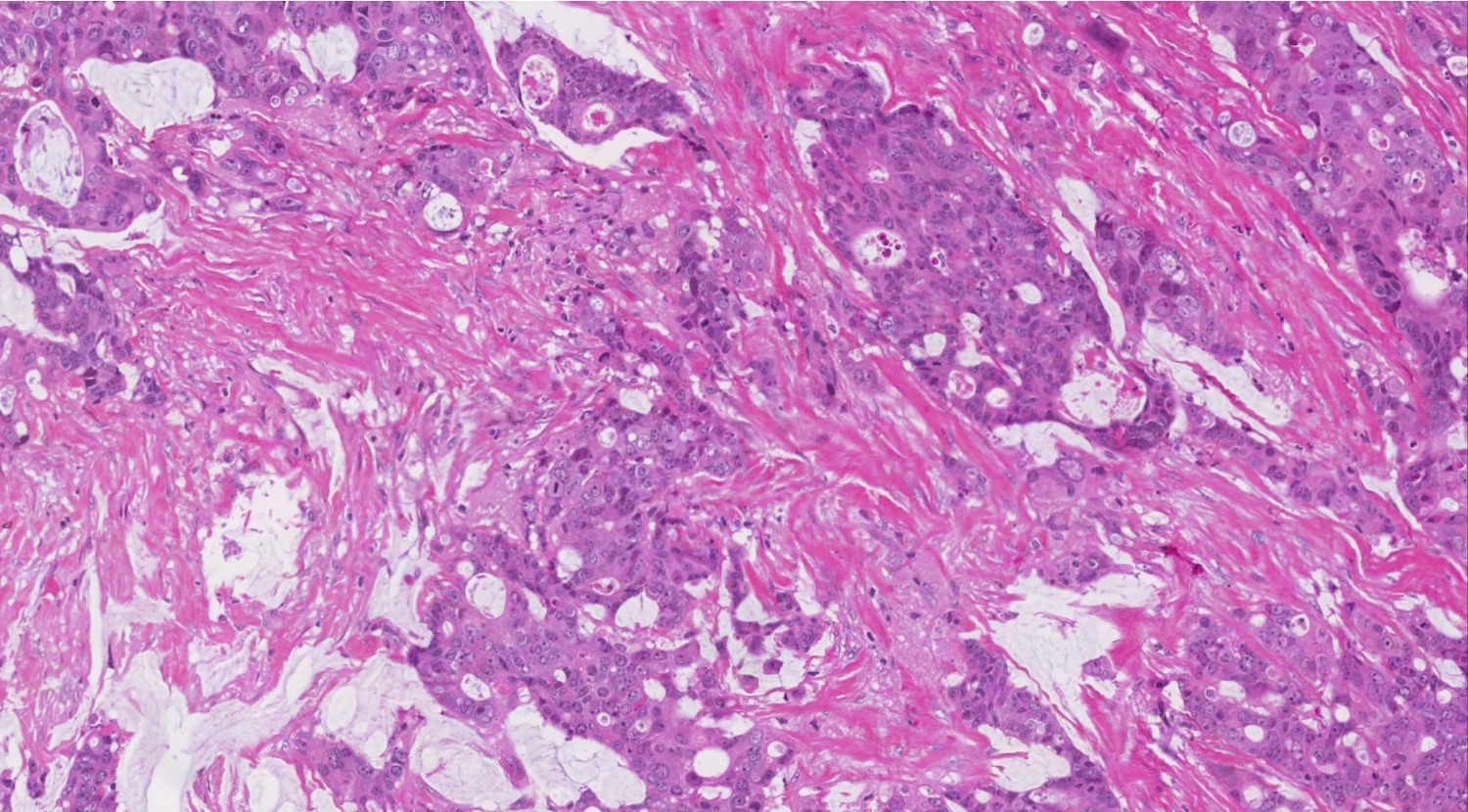
- Multinodular growth pattern with desmoplasia
- Intervening benign ovarian stroma
- Features suggestive of CRC origin (Am J Surg Pathol 2006;30:177):
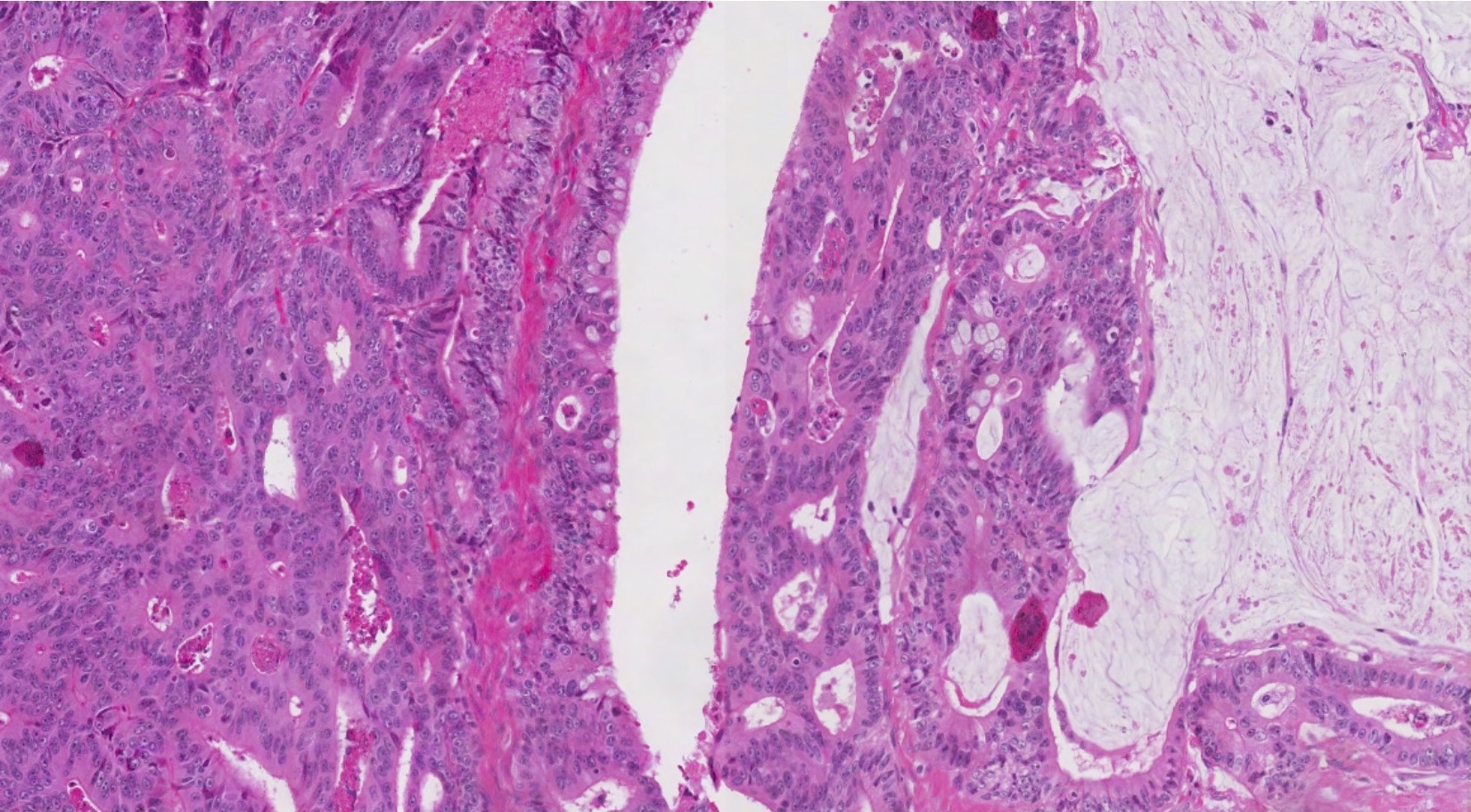
- Variably sized glands often with cystic dilation
- Garland pattern
- Intraluminal dirty necrosis
- Diagnostic accuracy of frozen section for CRC with OM specifically, is not well known
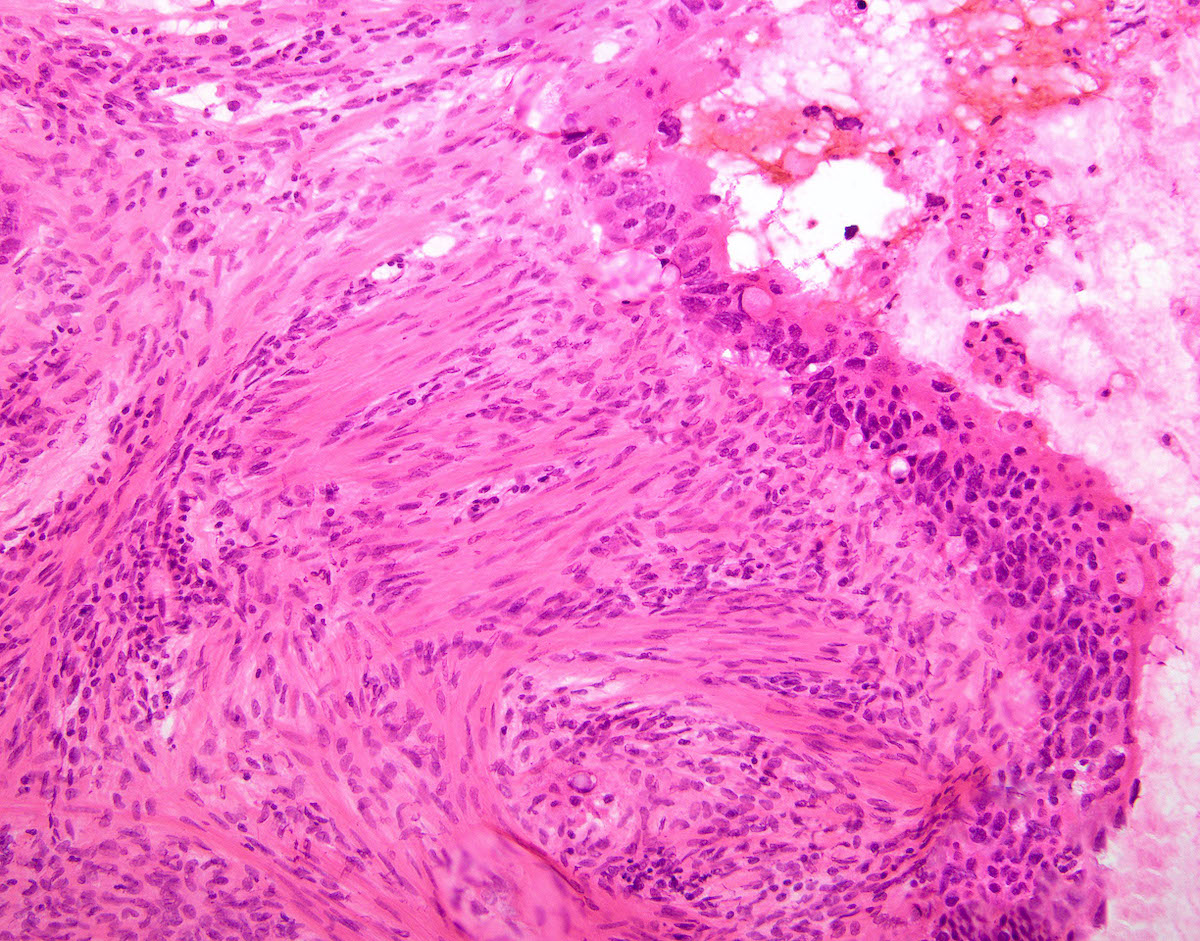
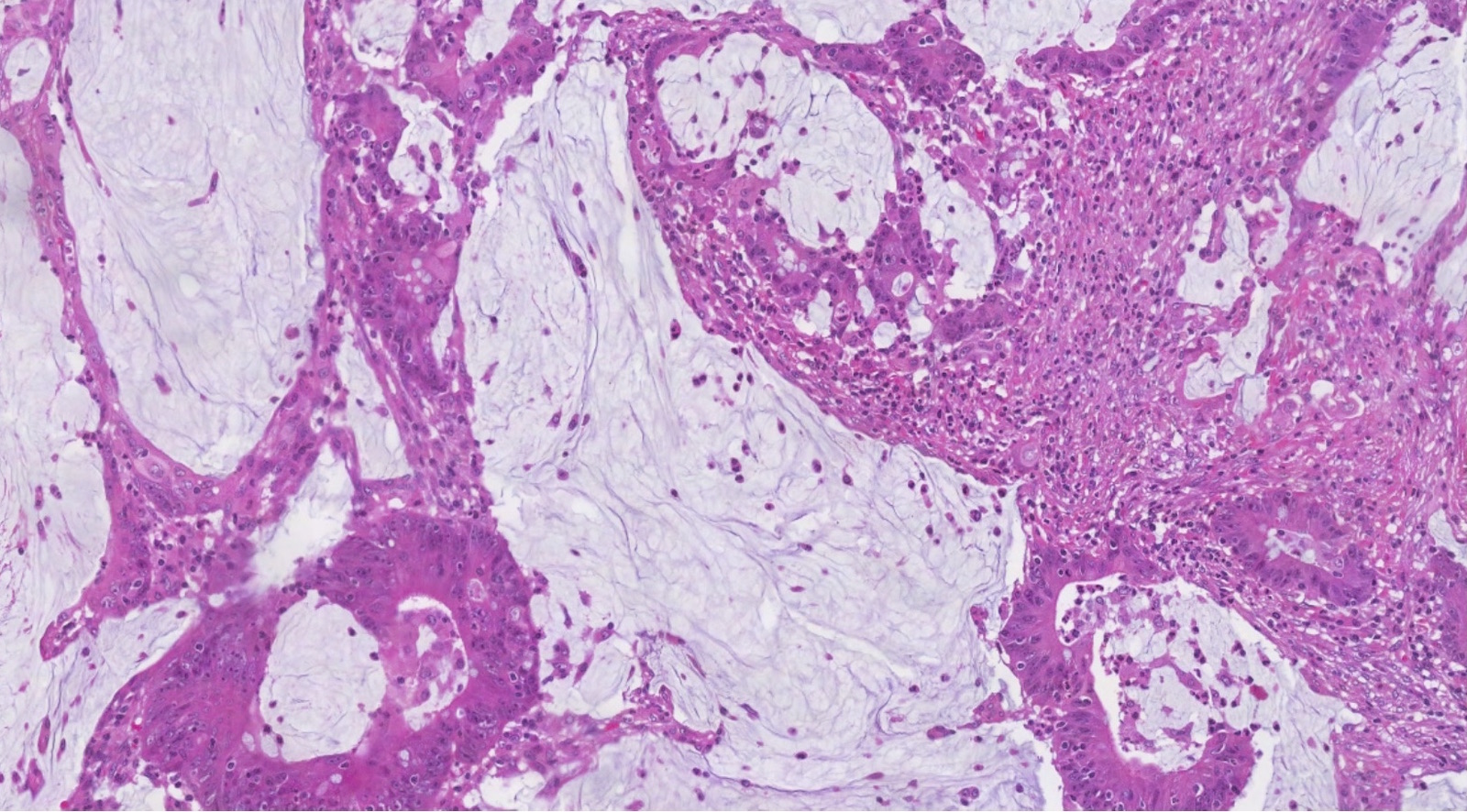
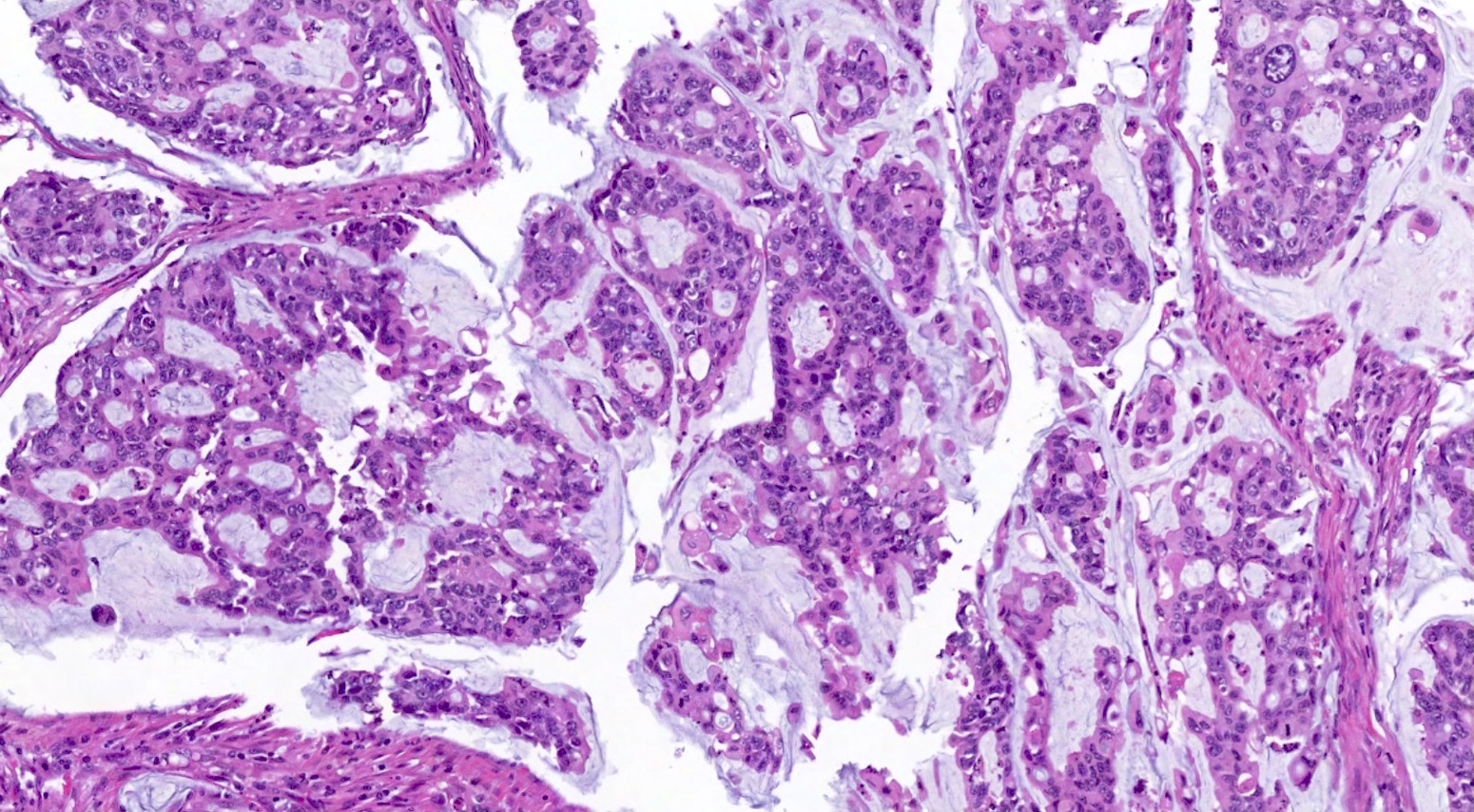
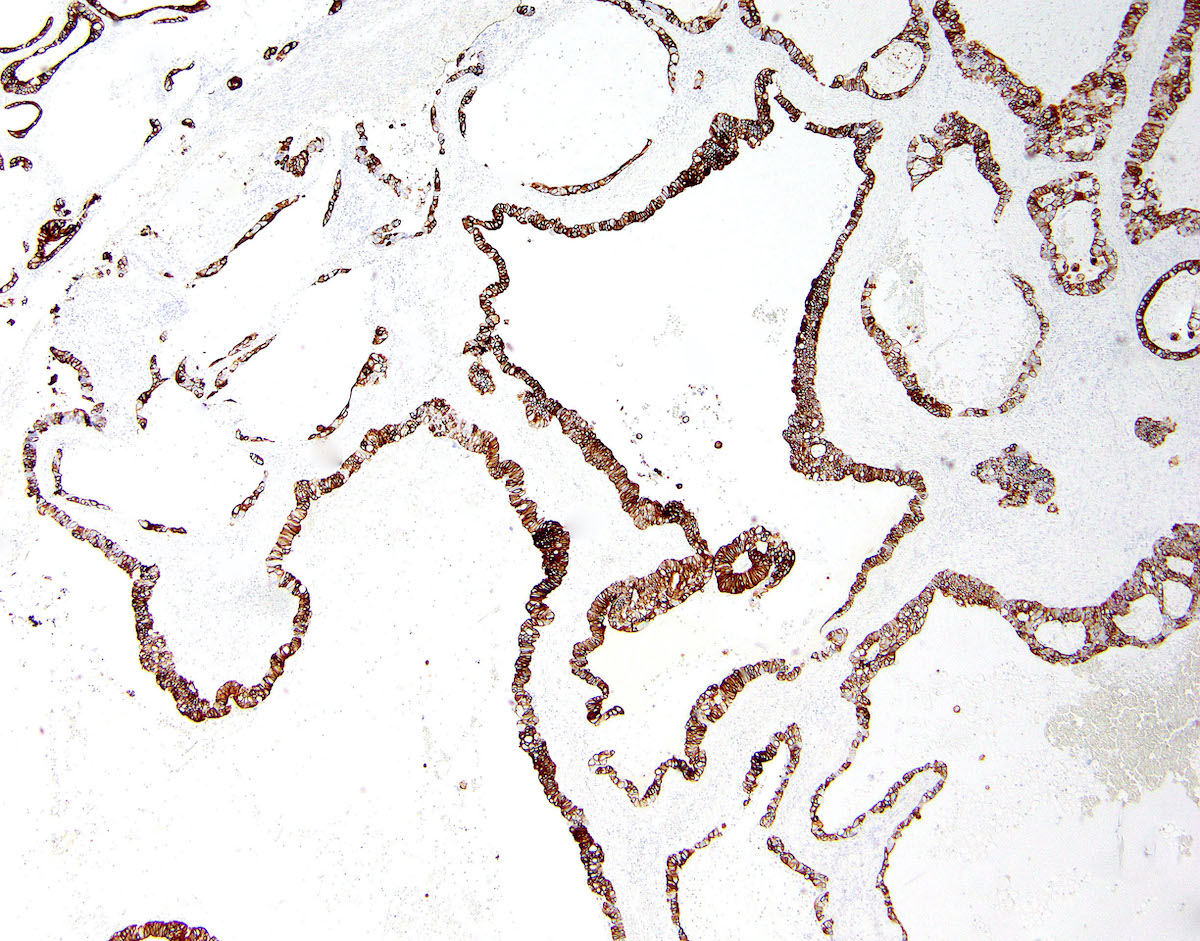
Microscopic (histologic) description
- Metastatic colorectal adenocarcinoma to the ovary usually has a mucinous or a conventional glandular appearance
- Mucinous carcinomas have intestinal (goblet cell) differentiation
- Mucin extravasation and signet ring cell morphology can be seen
- Krukenberg tumor is a term that should be reserved for adenocarcinoma involving the ovary with a signet ring cell component > 10% of the tumor volume, regardless of its site of origin (Adv Anat Pathol 2006;13:205)
- Conventional tumor cytomorphology with mucin depletion mimics the architecture and cytoplasmic appearance of a primary ovarian endometrioid tumor
- Nuclear pleomorphism and hyperchromasia tend to be prominent and exceed what is expected for a primary ovarian tumor
- Central glandular necrosis (dirty necrosis) is also more typical of colorectal tumors, although it is not entirely specific
- Desmoplastic stromal response
- Mucinous metastases frequently mimic the appearance of an ovarian mucinous neoplasm and may have areas mimicking a borderline or even benign primary mucinous tumor
- Several clinical and pathologic features have been described as indicative of secondary (metastatic) origin, including (Am J Surg Pathol 2003;27:281, Diagn Pathol 2021;16:20):
- Bilaterality
- Size < 10 cm
- Surface involvement
- Infiltrative pattern of growth with intervening benign ovarian stroma
- Presence of signet ring cells
- Extensive lymphovascular space invasion
- Mucin extravasation
- If any of the above features is present, the possibility of a metastasis should be considered and prompt ancillary testing and clinical investigation should be performed
Microscopic (histologic) images
Contributed by Carlos Parra-Herran, M.D. and Adam Lechner
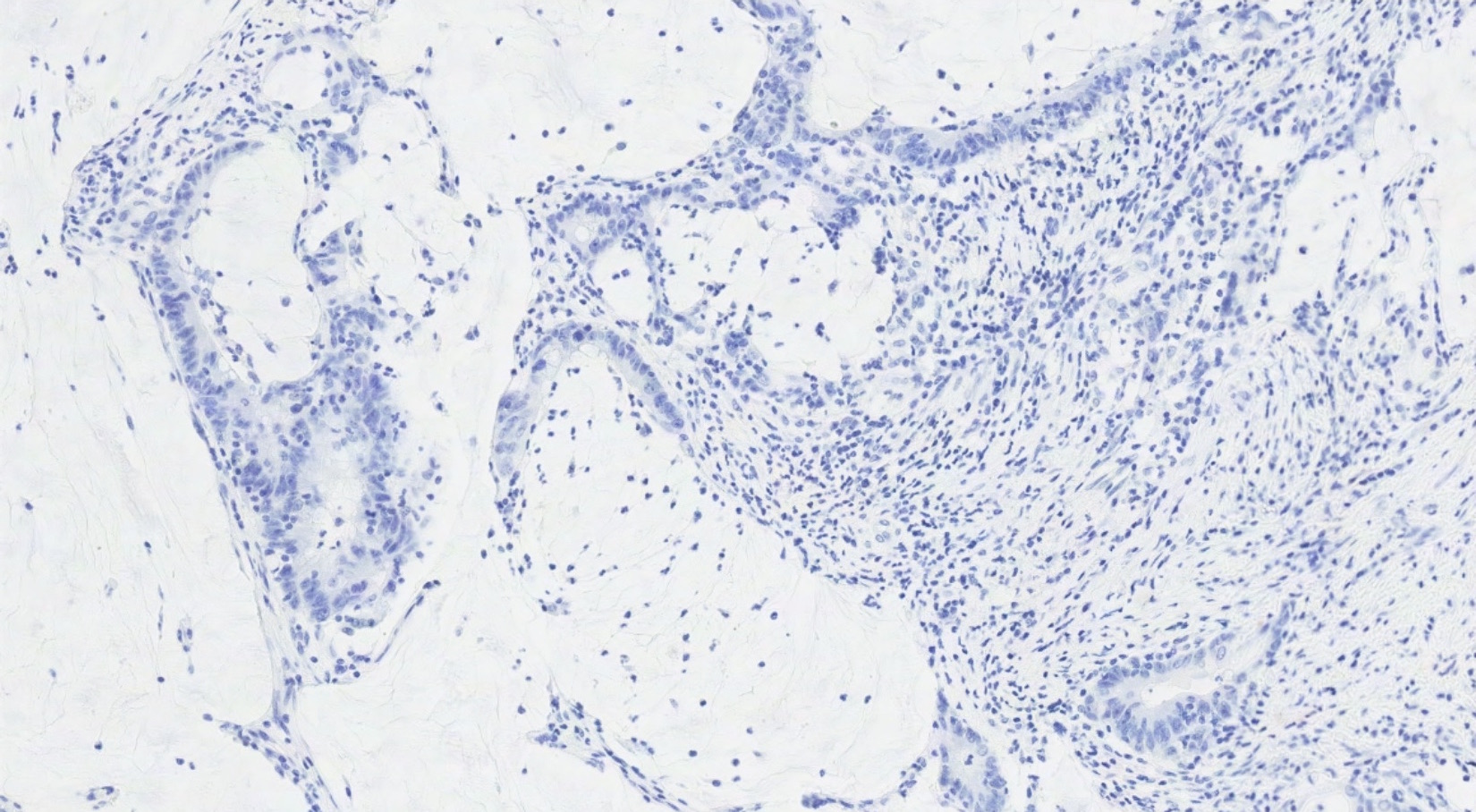
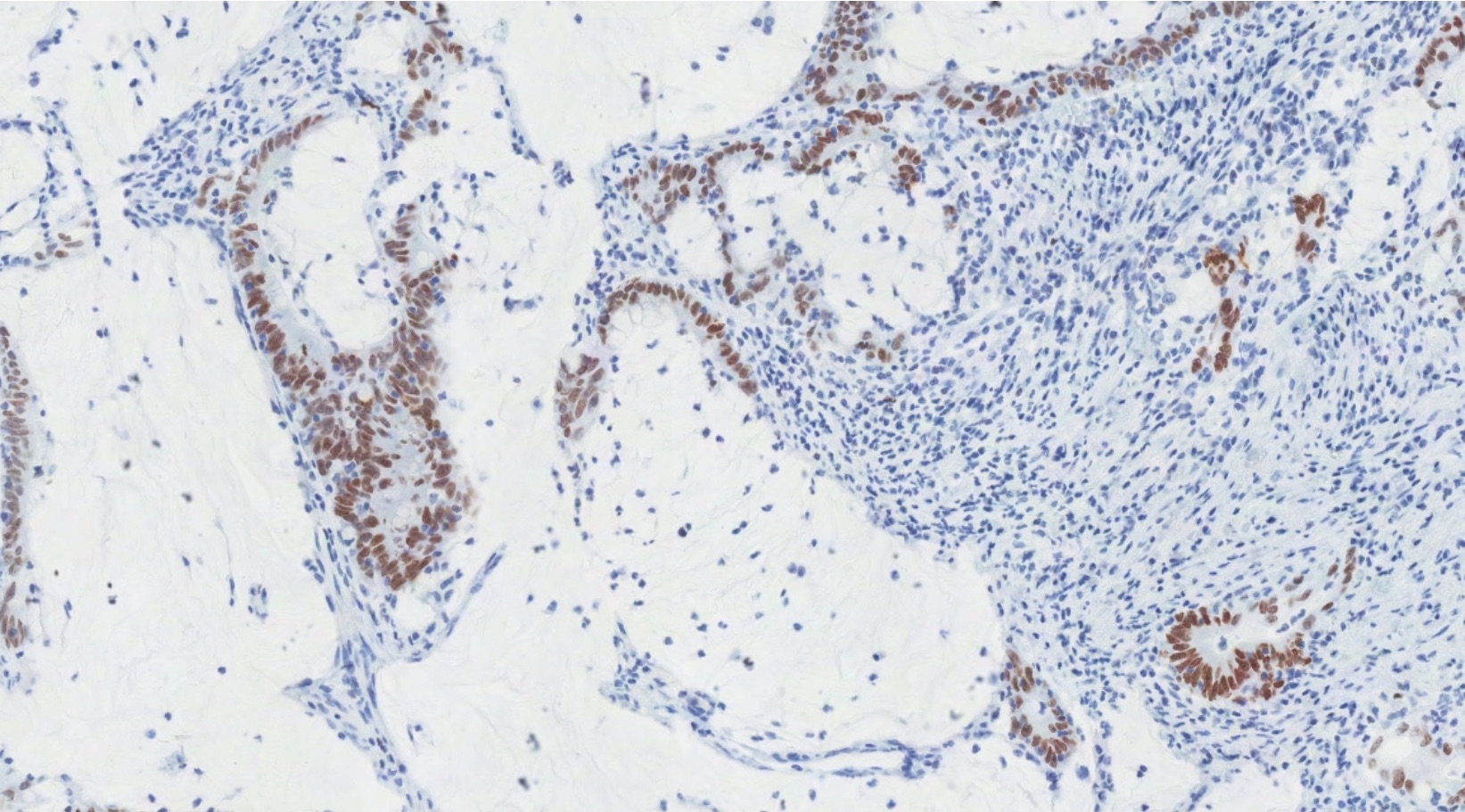
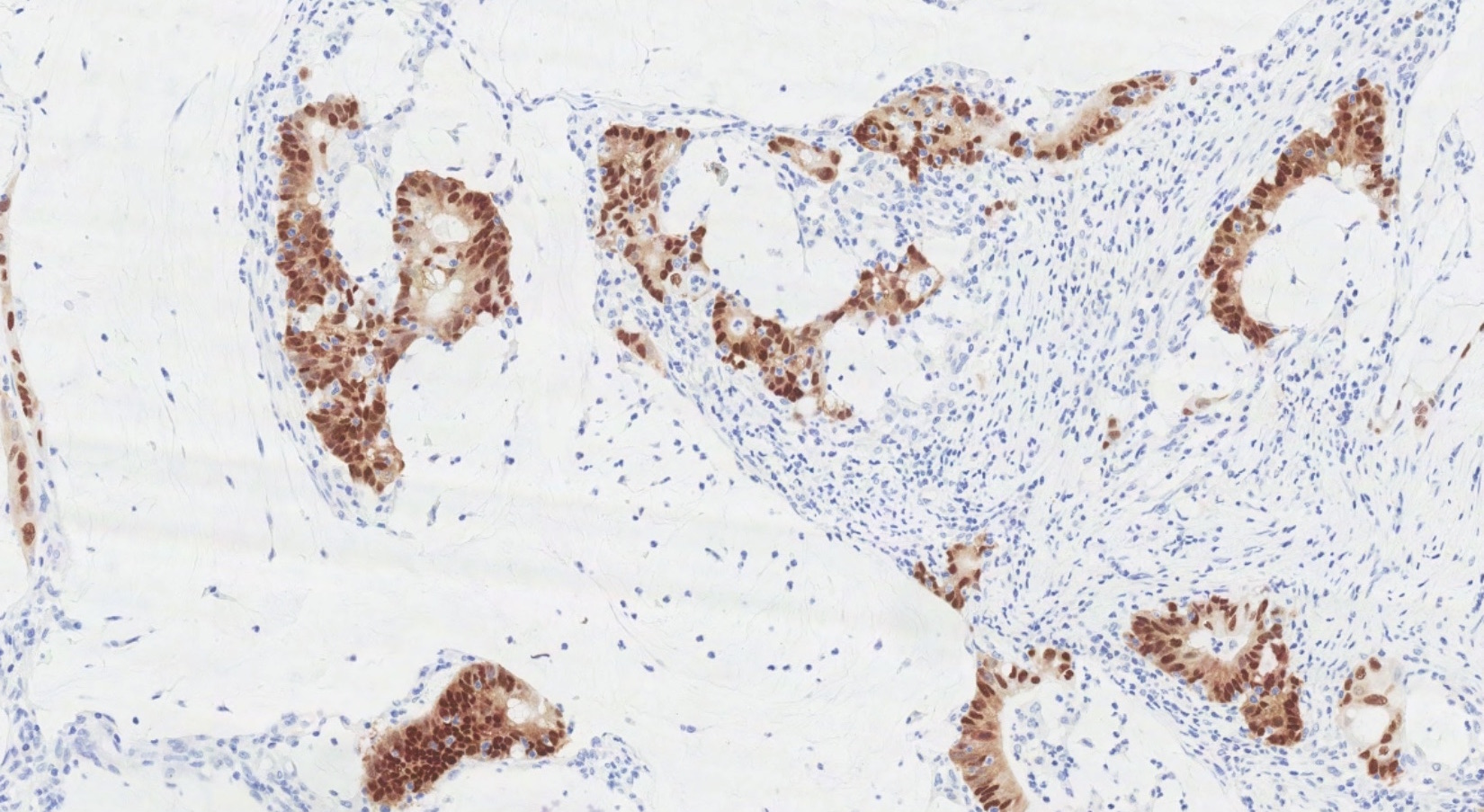
Positive stains
- Immunohistochemistry is useful to distinguish primary ovarian tumors and GI metastases but must be interpreted with caution, since there is significant overlap in expression (Int J Gynecol Pathol 2016;35:191)
- CK20, CDX2 and MUC2 are sensitive markers of colorectal origin
- They lack specificity since they are frequently positive in primary ovarian tumors
- SATB2 is a more specific marker of colorectal origin (Int J Gynecol Pathol 2016;35:191, BMC Res Notes 2019;12:770)
- Combination of CK7 and SATB2 using 3 tiered interpretation (absent / focal / diffuse) yields diagnostic accuracy of > 95% (Mod Pathol 2019;32:1834)
- Rates of expression in colorectal tumors are (Am J Surg Pathol 2016;40:419, Am J Surg Pathol 2018;42:160, Int J Gynecol Pathol 2016;35:191, Ann Diagn Pathol 2015;19:249):
- SATB2: 75 - 79% (versus 5% of primary ovarian mucinous tumors and 0% of primary ovarian endometrioid tumors)
- CK20: 68 - 85% (versus 45% of primary ovarian tumors)
- CDX2: 64 - 100% (versus 50% of primary ovarian tumors)
- MUC2: 97% (versus 40% of primary ovarian tumors)
- Beta catenin: 51% (versus 5% of primary ovarian tumors)
- CK7: 21% (versus 95% of primary ovarian tumors)
Negative stains
- PAX8: 0% (versus 30 - 65% of primary ovarian mucinous tumors and 80% of primary ovarian endometrioid tumors)
- ER: 0% (versus 30% of primary ovarian tumors)
- See Diagrams / tables
Molecular / cytogenetics description
- EGFR and HER2 overexpression is more common in OM than other metastatic sites of CRC (BMC Clin Pathol 2019;19:3)
- PIK3CA mutations are significantly less common in CRC with OM (Cancer Biol Ther 2015;16:1726)
- Lower RRM1 protein expression is also seen and may indicate sensitivity to gemcitabine (Cancer Biol Ther 2015;16:1726)
- Reference: Cancer 2017;123:1134
Sample pathology report
- Ovary, oopherectomy:
- Metastatic adenocarcinoma, moderately differentiated (see comment)
- Comment: Immunostaining demonstrates SATB2+, CDX2+, CK20+, CK7- and PAX8- in lesional cells. The cytomorphology and immunohistochemical profile is most consistent with metastatic adenocarcinoma of colorectal primary.
Differential diagnosis
- Metastases from upper GI tract:
- Metastases from cervix:
- p16 positive (strong, diffuse)
- Primary ovarian neoplasm (benign, borderline or malignant):
- Most often mucinous or endometrioid types; less likely high grade serous and clear cell types
- No suspicious features described above (bilaterality, surface involvement, signet ring cell morphology, etc.)
- PAX8+, CK7+, CK20-, CDX2-, SATB2-
- For endometrioid tumors: squamous differentiation, adenofibromatous background, involvement by endometriosis, ER+
- For mucinous tumors: association with teratoma or Brenner tumor, CK7+, PAX8+ (50 - 65% of cases)
- For serous tumors: complex papillary architecture, severe pleomorphism, ER+, WT1+
Board review style question #1
A 51 year old woman presents with a 6 month history of menorrhagia and abdominal discomfort. Pelvic imaging identifies bilateral complex cystic adnexal masses of 7 and 9 centimeters. Whole body PET / CT identifies an additional hypermetabolic lesion in the cecum and in the liver. A representative section taken from a bilateral salpingo-oopherectomy specimen is shown above. Which of the following immunohistochemical results provides the strongest support for the diagnosis?
- CDX2+
- CK7+
- MUC2+
- SATB2+
Board review style answer #1
D. SATB2+. Bilateral, small (< 10 cm) ovarian masses are concerning for a metastatic process. The presence of a lesion in the cecum with an additional metastatic focus in the liver raises the possibility of colorectal origin. Histology shows punched out, angulated glands with intraluminal dirty necrosis consistent with metastatic colorectal adenocarcinoma. The immunoprofile of this tumor is CK7- / CK20+, CDX2+, SATB2+, MUC2+, PAX8-. Although MUC2, CDX2 and SATB2 are both positive in CRC, primary ovarian malignancies (particularly mucinous neoplasms) are often positive for CDX2 and MUC2 as well (usually with patchy distribution).
Comment Here
Reference: Colorectal adenocarcinoma
Comment Here
Reference: Colorectal adenocarcinoma
Board review style question #2
A 60 year old woman is diagnosed with colorectal adenocarcinoma with isolated metastases to the left ovary. She undergoes cytoreductive surgery, including low anterior resection and oophorectomy. Which of the following statements is correct?
- Adjuvant chemotherapy is contraindicated
- The presence of signet ring cell differentiation would indicate better overall survival
- This patient's colorectal cancer likely originated in the cecum
- This patient has a relatively better prognosis compared to those with additional metastases beyond the ovary
Board review style answer #2
D. This patient has a relatively better prognosis compared to those with additional metastases beyond the ovary. Isolated ovarian metastasis in colorectal adenocarcinoma shows improved survival over additional metastases to extraovarian sites. Unilateral ovarian metastasis in CRC most commonly originates from a left sided primary. HIPEC adjuvant therapy at the time of cytoreductive surgery improves survival. Signet ring cell differentiation is a uniformly negative prognostic factor.
Comment Here
Reference: Colorectal adenocarcinoma
Comment Here
Reference: Colorectal adenocarcinoma