Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Negative stains | Electron microscopy description | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Menshikova E, Hanley K. Carcinoid tumor. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/ovarytumorcarcinoid.html. Accessed April 1st, 2025.
Definition / general
- Primary ovarian carcinoid tumors are well differentiated neuroendocrine tumors resembling those arising in the gastrointestinal tract
- In some cases, teratomatous components are identified (component of mature cystic teratoma)
- 4 types: insular, trabecular, strumal and mucinous
Essential features
- Unilateral
- May be associated with carcinoid syndrome
- Rare
Terminology
- Classified as monodermal teratomas
ICD coding
- ICD-O: 9091/1 - strumal carcinoid
- ICD-10
- ICD-11: 2F76 & XH2XW3 - neoplasms of uncertain behavior of female genital organs & strumal carcinoid
Epidemiology
- Primary ovarian carcinoid is rare and accounts for
- < 0.1% of all ovarian neoplasms (Medicine (Baltimore) 2020;99:e21109)
- < 2% of all carcinoid tumors (Cancer 2003;97:934)
- Patient age at time of presentation ranges from 17 to 83 years with a median of 55 (Gynecol Oncol 1996;61:259)
- Mucinous: observed in a younger group of patients compared to other ovarian carcinoids
- Insular type is the most common (~50%); mucinous is the least common
Sites
- Ovary (Curr Opin Obstet Gynecol 1997;9:44)
- Primary ovarian carcinoids are unilateral
- Metastatic nearly always bilateral
- Most arise in mature cystic teratoma or in association with mucinous tumor
- Pure form is less frequent; may be associated with struma ovarii
Pathophysiology
- Pathogenesis remains unclear
Etiology
- Arises from neuroendocrine cells within gastrointestinal type epithelium of mature cystic teratoma or rarely other tumors
- A case of carcinoid arising from the teratomatous bronchial mucosa in an ovarian mature cystic teratoma has been reported (Int J Gynecol Pathol 2018;37:123)
Clinical features
- Asymptomatic, incidental finding
- Abdominal mass
- Ascites
- Carcinoid syndrome
- ~33% of patients are > 50 years old
- Presence of carcinoid syndrome correlates with size of the tumor; typically seen in tumors > 7 cm, rarely seen in tumors < 4 cm
- Most common in insular type
- Does not require the presence of liver metastasis since venous drainage bypasses portal venous circulation (Tex Heart Inst J 2019;46:21)
- Carcinoid heart disease may be the initial manifestation
- Occurs in < 10% of cases of primary ovarian carcinoid
- Generally involves right chambers and valves
- Endocrine effects thought to occur due to stromal luteinization (Diagnostics (Basel) 2022;12:2706)
- Virilization
- Hirsutism
- Endometrial hyperplasia
- Cushing syndrome
- Constipation due to inhibitory effect on gastrointestinal motility of peptide YY secreted in strumal carcinoid (Obstet Gynecol Sci 2017;60:602)
- Hyperthyroidism in strumal carcinoid
Diagnosis
- Preoperative diagnosis of primary ovarian carcinoid is challenging; typically, the mass is properly classified postoperatively
- May be detected as a mass on physical examination
- Imaging: ovarian mass lacks typical imaging characteristics
- Somatostatin receptor scintigraphy: useful in detection of neuroendocrine tumors that show intensive octreotide intake (Am J Case Rep 2022;23:e937403)
- Cytologic features: polygonal uniform cells, round monotonous nuclei, salt and pepper chromatin, ample to eosinophilic cytoplasm, often containing red to brown argentaffin granules; low mitotic activity
- Mucinous carcinoids cytologically show cells exhibiting neuroendocrine and mucinous differentiation; signet ring cells may be seen in the stroma
- WHO essential and desirable diagnostic criteria
- Essential
- Insular architecture (if insular carcinoid)
- Trabecular or corded architecture (if trabecular carcinoid)
- Thyroid follicles intimately admixed or juxtaposed with carcinoid (if strumal carcinoid)
- Acini or glands with goblet cells free floating in mucin (if mucinous carcinoid)
- Salt and pepper chromatin pattern of the nuclei, with or without cytoplasmic granules
- Desirable: positivity for neuroendocrine markers
- Essential
Laboratory
- Tumor markers may be elevated (Acta Obstet Gynecol Scand 2023;102:935)
- Elevation of CA125 and CA19-9 may mimic ovarian carcinoma
- Neuron specific enolase (NSE)
- Carcinoembryonic antigen (CEA)
- Tumor markers used in carcinoid syndrome to monitor disease activity, response to therapy and early detection of metastasis (Endocrinol Metab Clin North Am 2017;46:669)
- 5-hydroxyindole acetic acid (5-HIAA)
- Chromogranin A
Radiology description
- Ultrasound
- Hypoechoic solid or cystic with solid component adnexal mass (Medicine (Baltimore) 2020;99:e21109)
- Computed tomography (CT)
- Unilateral, lobulated adnexal mass with scattered necrotic areas indistinguishable from other solid ovarian neoplasms
- Solid enhancing nodule in the wall of a mature cystic teratoma or a mucinous neoplasm
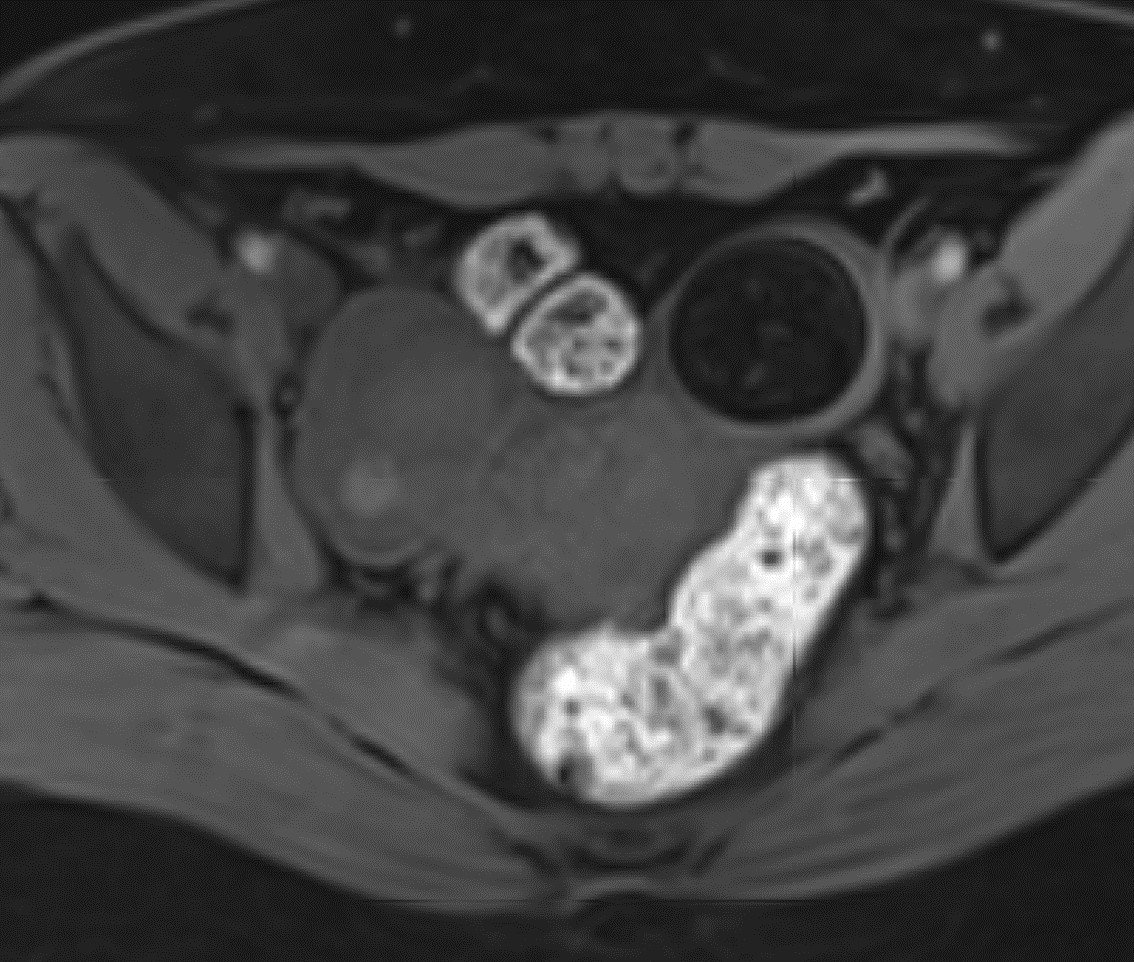
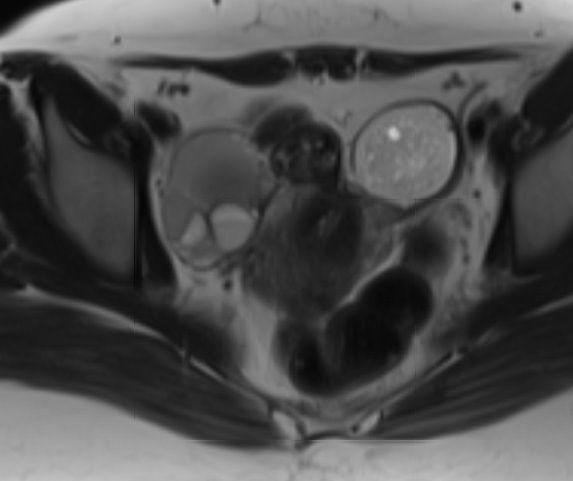
- Magnetic resonance imaging (MRI)
- On T2 weighted MR images, hypointense solid adnexal mass or low intensity focus within a multilocular cystic mass
Radiology images
Prognostic factors
- 5 year survival rate of ovarian carcinoid is 84% and 94% in patients with and without mature cystic teratoma, respectively
- Insular carcinoid
- Favorable prognosis
- Slow growing
- Only occasionally has metastasis
- Trabecular carcinoid
- Favorable prognosis
- Not associated with metastasis
- Strumal carcinoid
- Favorable prognosis
- 15 year recurrence rate is 4.4% (BMC Cancer 2022;22:1090)
- Mucinous
- Behaves more aggressively than other types of primary ovarian carcinoid
- Tends to spread mainly via lymphatics and can metastasize
- No metastases, better prognosis
- Low Ki67 proliferative index; mean index of 2.5% with a maximum of 5% (Acta Obstet Gynecol Scand 2023;102:935)
- Carcinoid heart syndrome has been reported to be associated with overall poor outcome
Case reports
- 18 year old woman with mucinous adenocarcinoma and carcinoid tumor arising within an ovarian mature cystic teratoma (Oman Med J 2023;38:e538)
- 40 year old woman with insular carcinoid with hyperandrogenism and carcinoid heart syndrome (Am J Case Rep 2022;23:e937403)
- 40 year old woman with trabecular carcinoid tumor arising from a mature cystic teratoma (Ci Ji Yi Xue Za Zhi 2019;3:192)
- 51 year old postmenopausal woman with primary ovarian carcinoid exhibiting mixed growth pattern (Medicine (Baltimore) 2023;102:e34391)
- 56 year old woman with ovarian strumal carcinoid (Fukushima J Med Sci 2023;69:51)
Treatment
- Treatment strategies vary (Acta Obstet Gynecol Scand 2023;102:935)
- Surgical
- Conservative
- Cystectomy
- Unilateral salpingo-oophorectomy, especially in reproductive age women
- Radical surgery
- Bilateral salpingo-oophorectomy
- Hysterectomy and bilateral salpingo-oophorectomy
- In mucinous carcinoid, regional lymph node dissection may be required
- Cytoreductive surgery
- Conservative
- Adjuvant treatment restricted to patients with residual or metastatic diseases
- Somatostatin analogs: may be used in metastatic or recurrent primary ovarian carcinoids; treatment of symptoms of excess hormone secretion and for tumor growth control
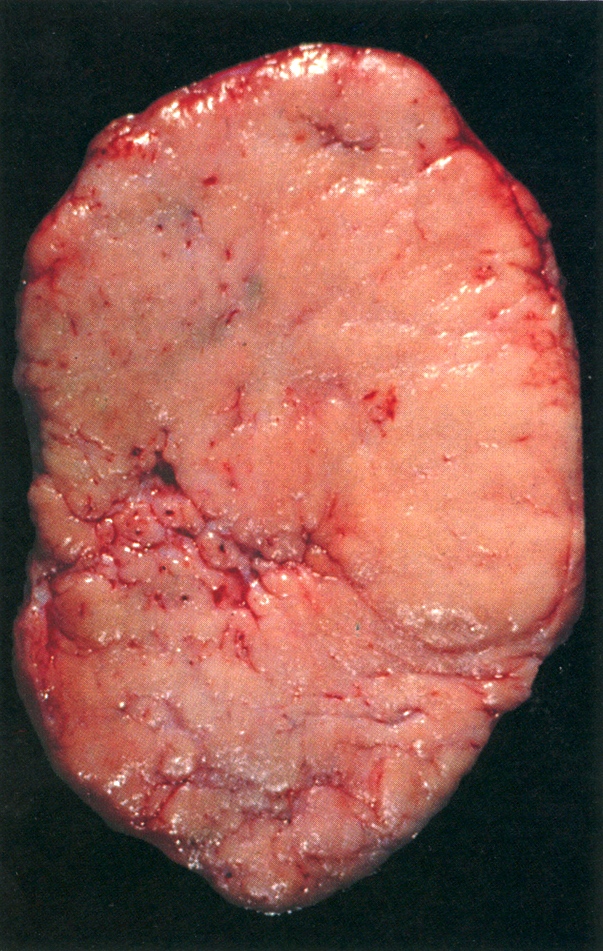
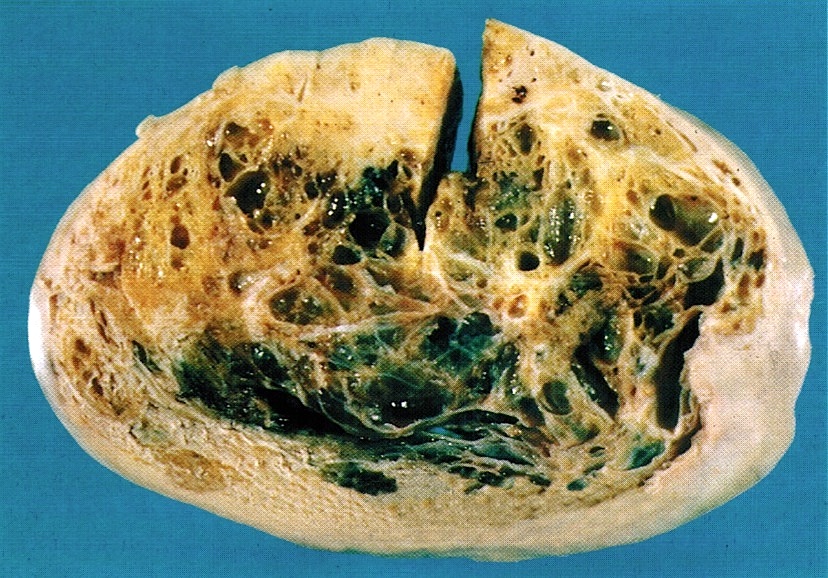
Gross description
- Usually present as firm, solid and homogeneous gray to yellow masses in association with mature teratoma or mucinous tumor (Curr Opin Obstet Gynecol 1997;9:44)
- If pure (Curr Opin Obstet Gynecol 1997;9:44)
- Strumal carcinoid: solid yellow-brown nodule with fleshy areas
- Mucinous carcinoid: gray-yellow, firm, usually solid but may contain cystic areas even when seen in a pure form; most tumors > 8 cm
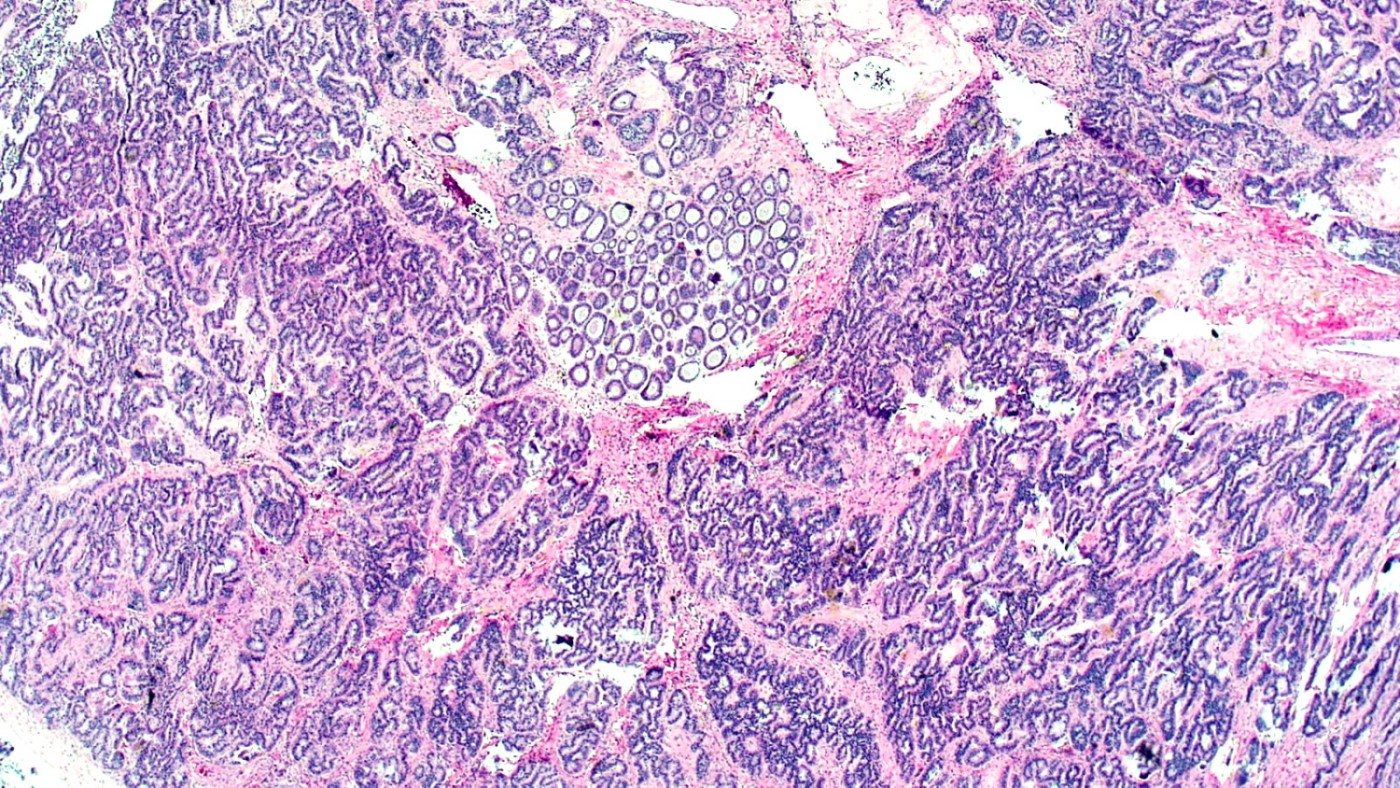
Microscopic (histologic) description
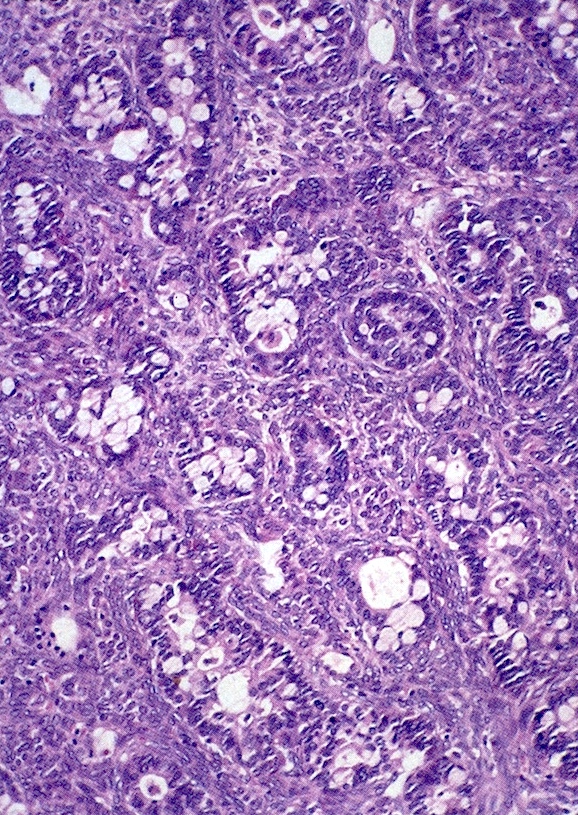
- 4 types (J Int Med Res 2021;49:3000605211034666)
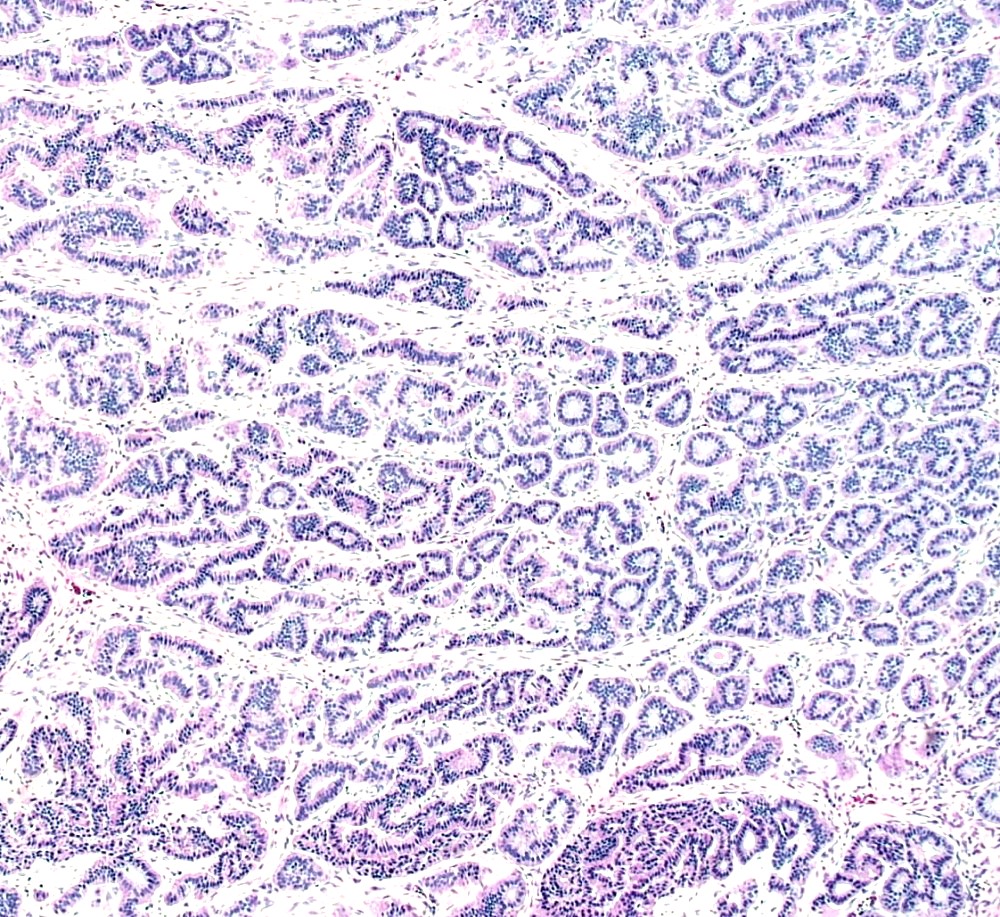
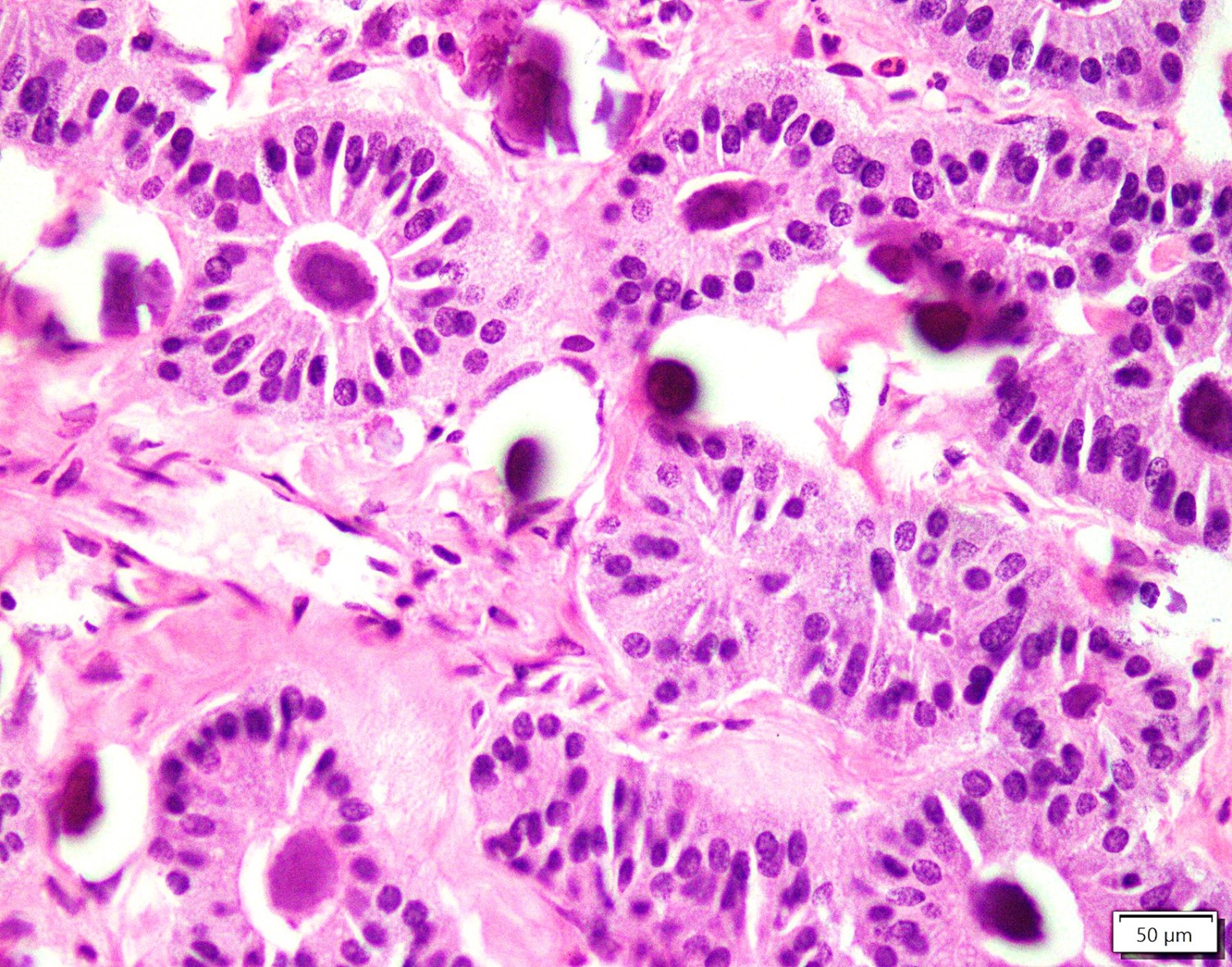
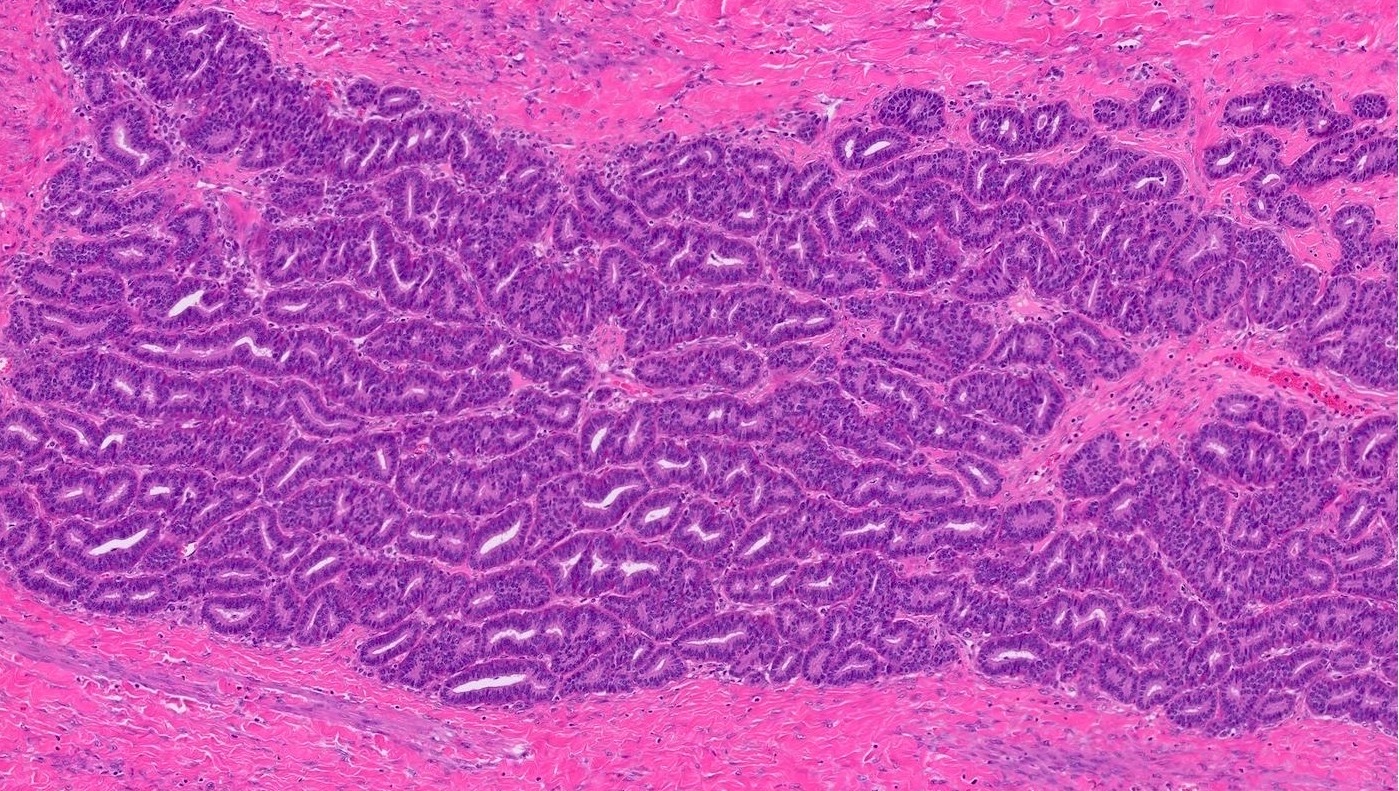
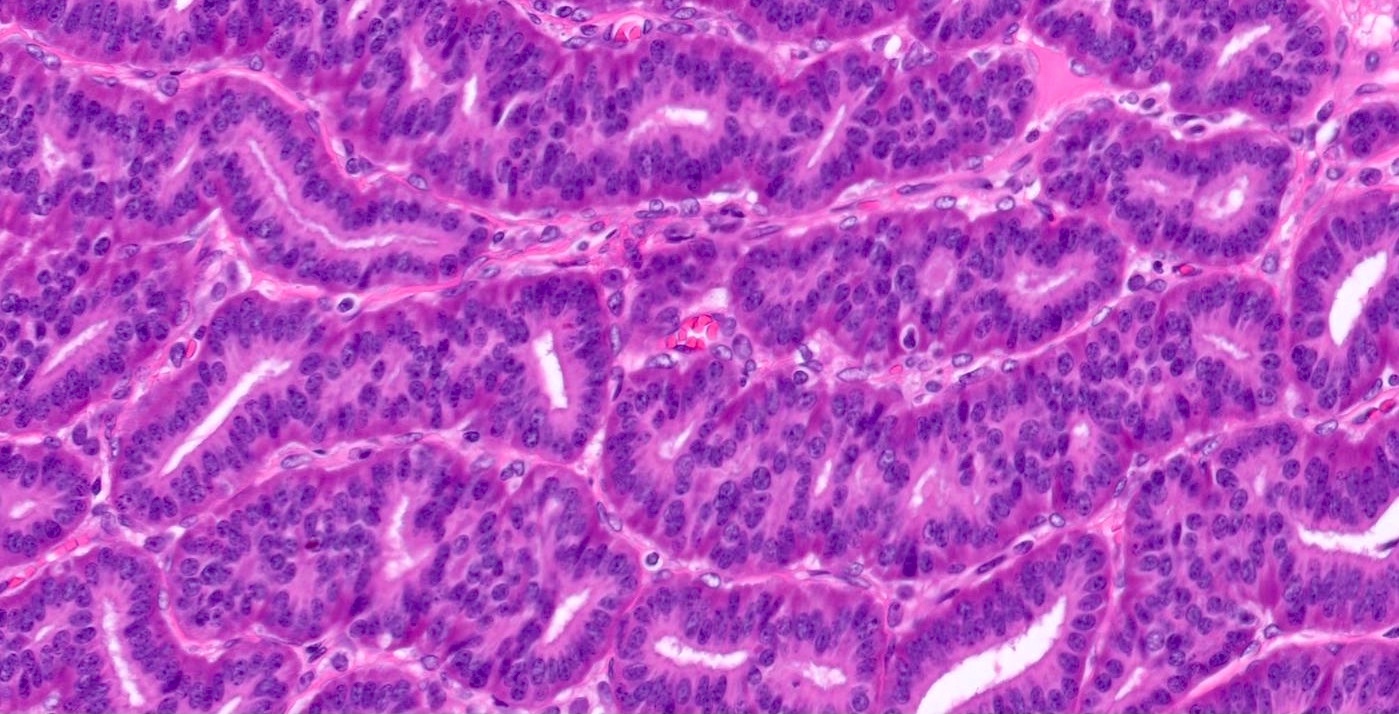
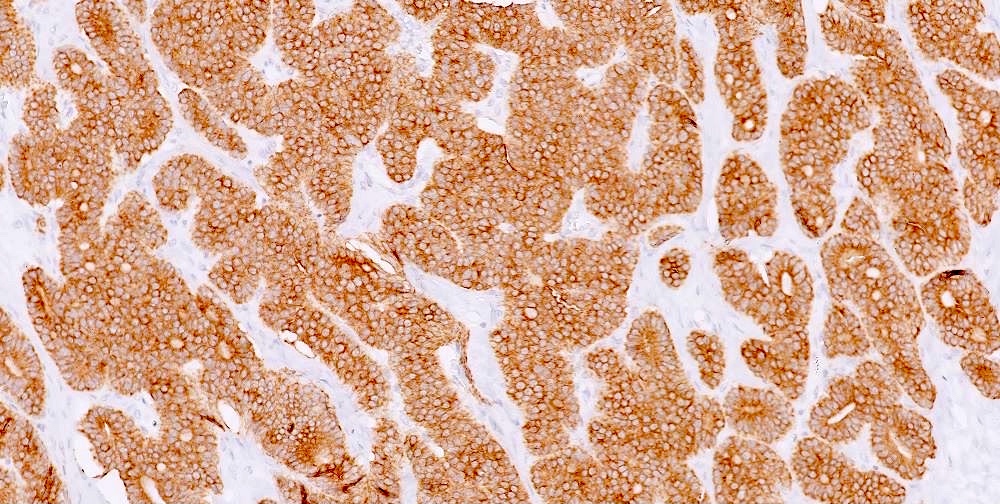
- Insular carcinoid
- Most common type of ovarian carcinoid
- Growth pattern usually shows large islands, variable sized nests, small acini or glands within the fibrous stroma
- Simple tubular glands, cribriform nests may also be seen
- Retraction artifact around tumor cells is common
- Composed of uniform polygonal epithelial cells with abundant cytoplasm and round, centrally located nuclei; cytoplasm contains red-brown granules, located basally
- Secretions in lumina, psammoma bodies
- Stroma is dense and hyalinized
- Low mitotic activity
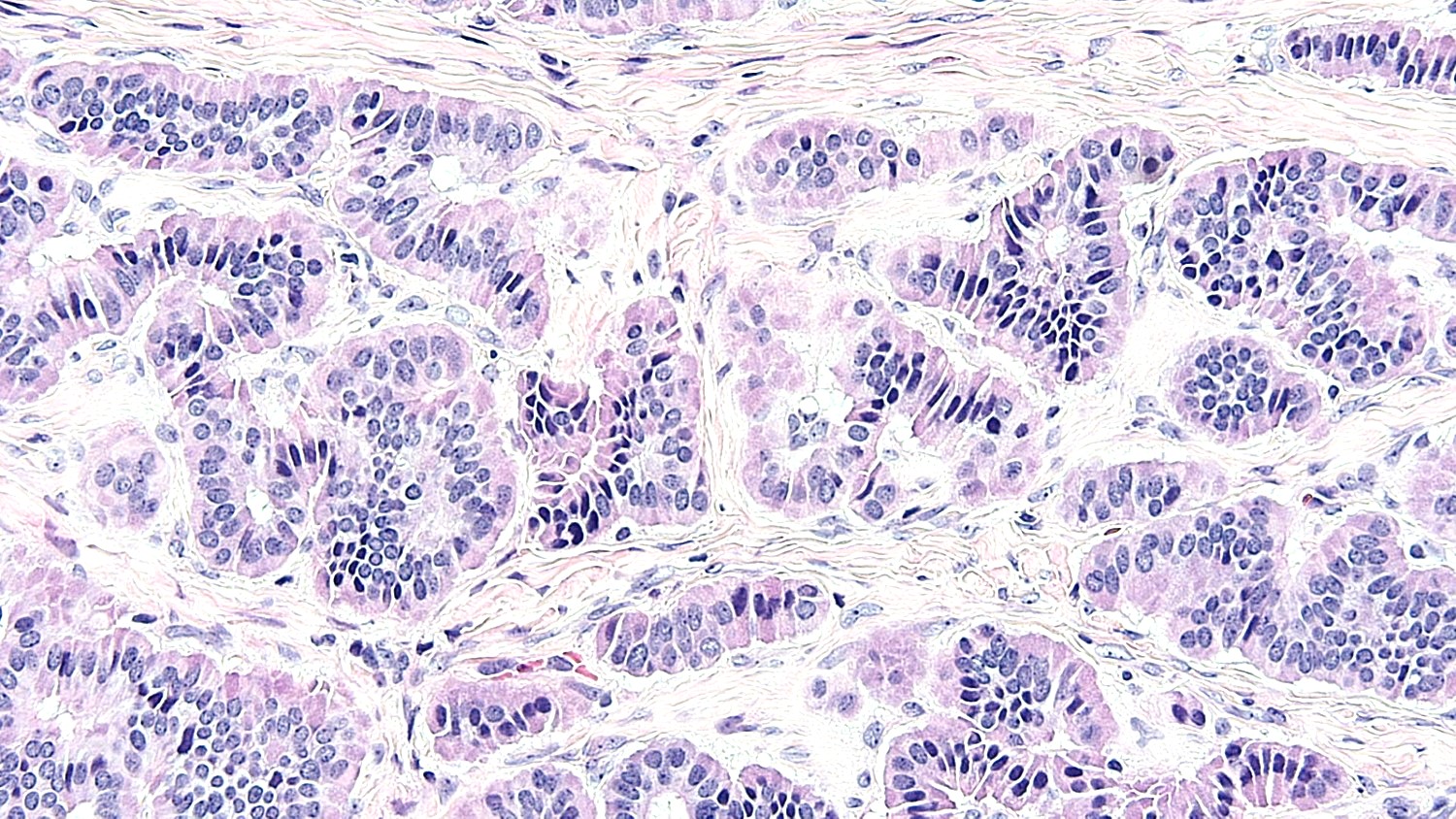
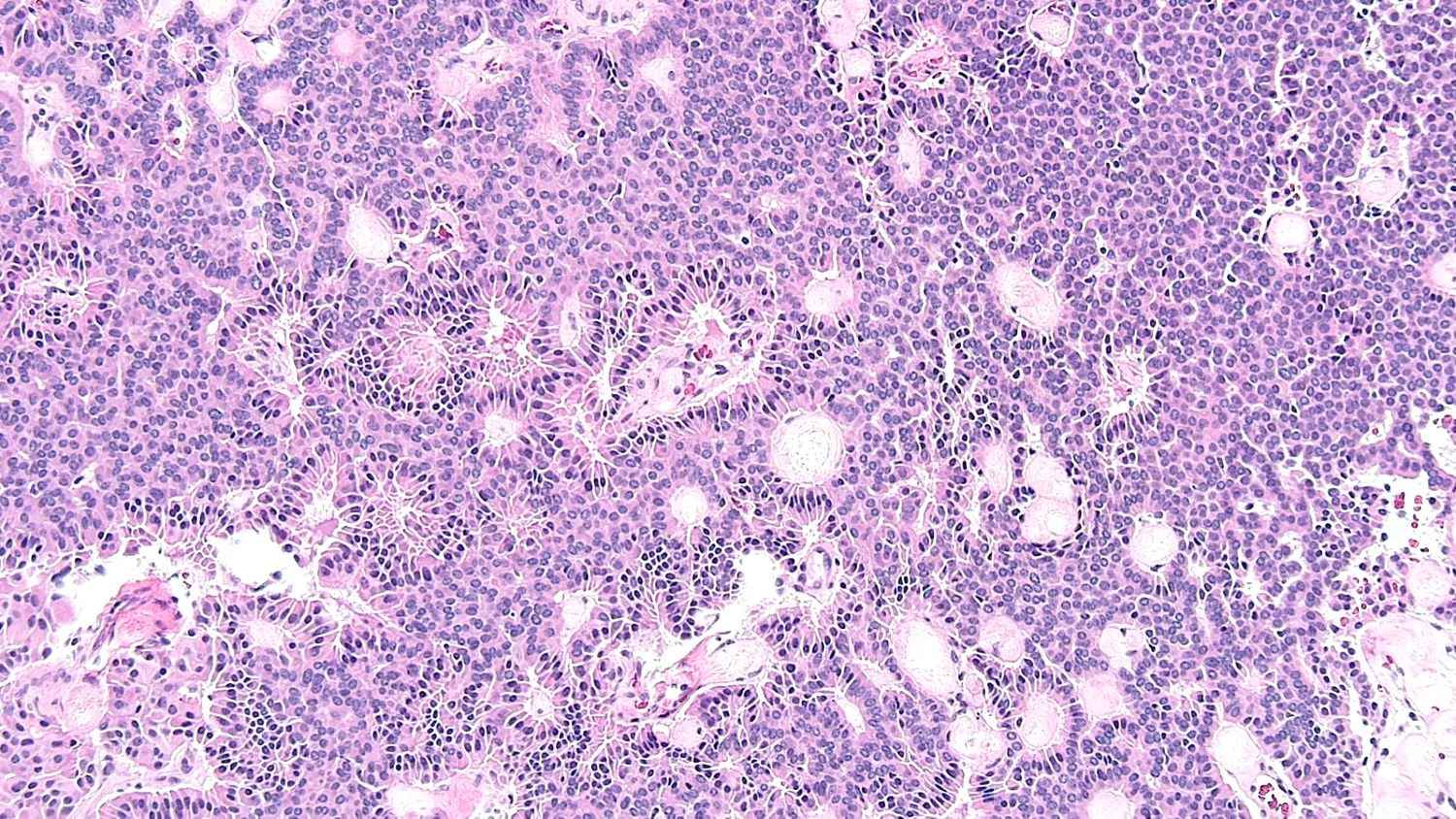
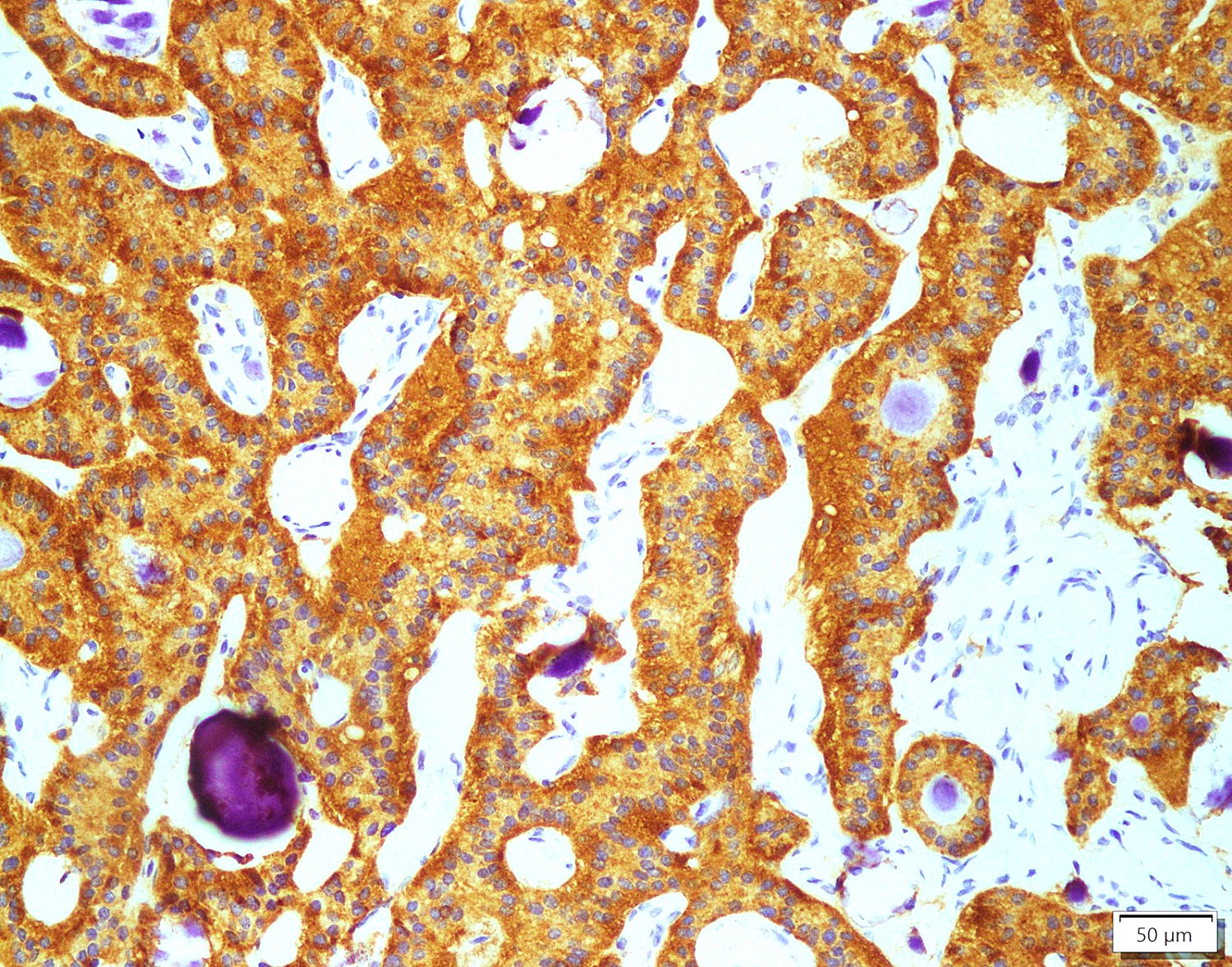
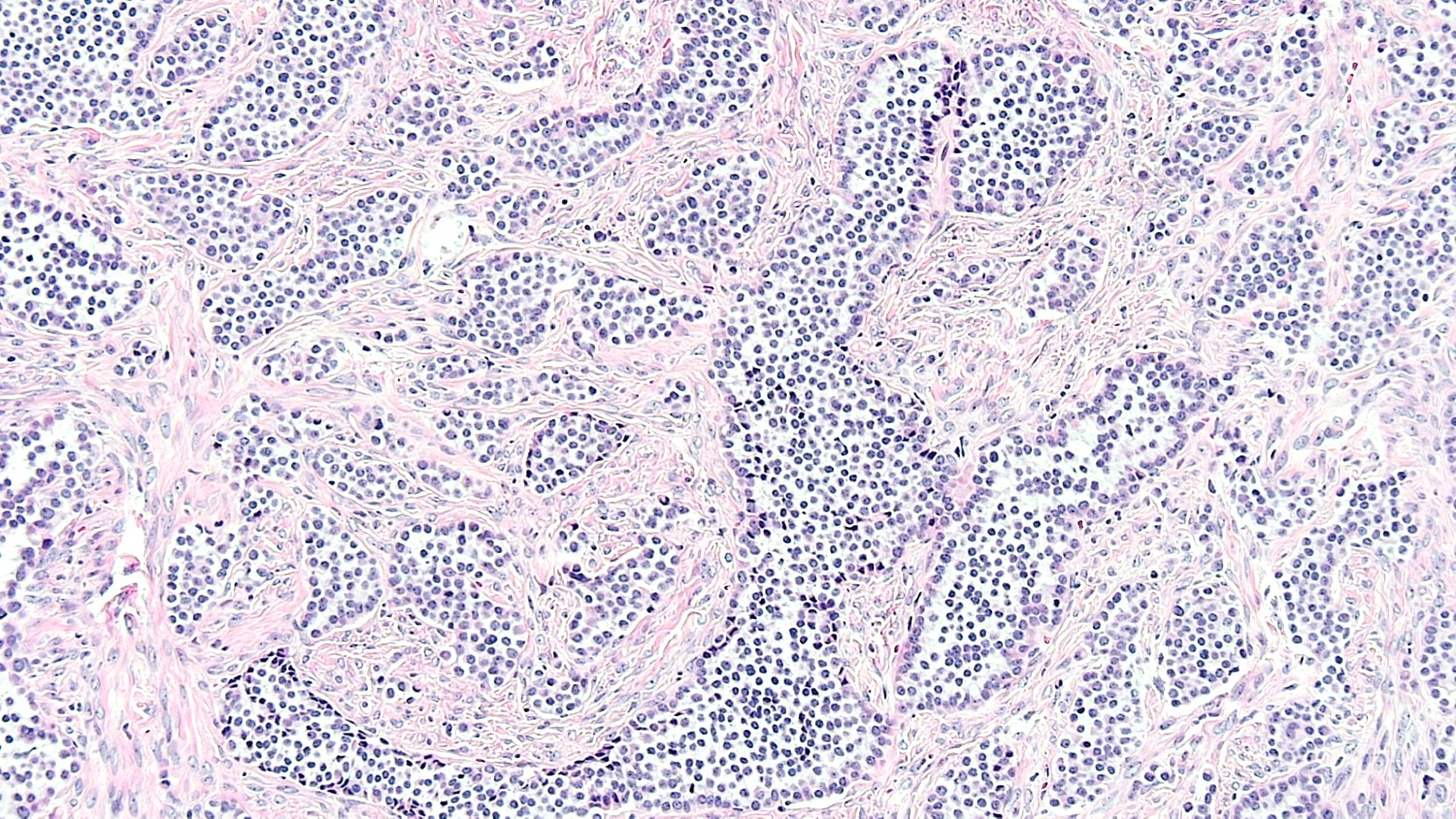
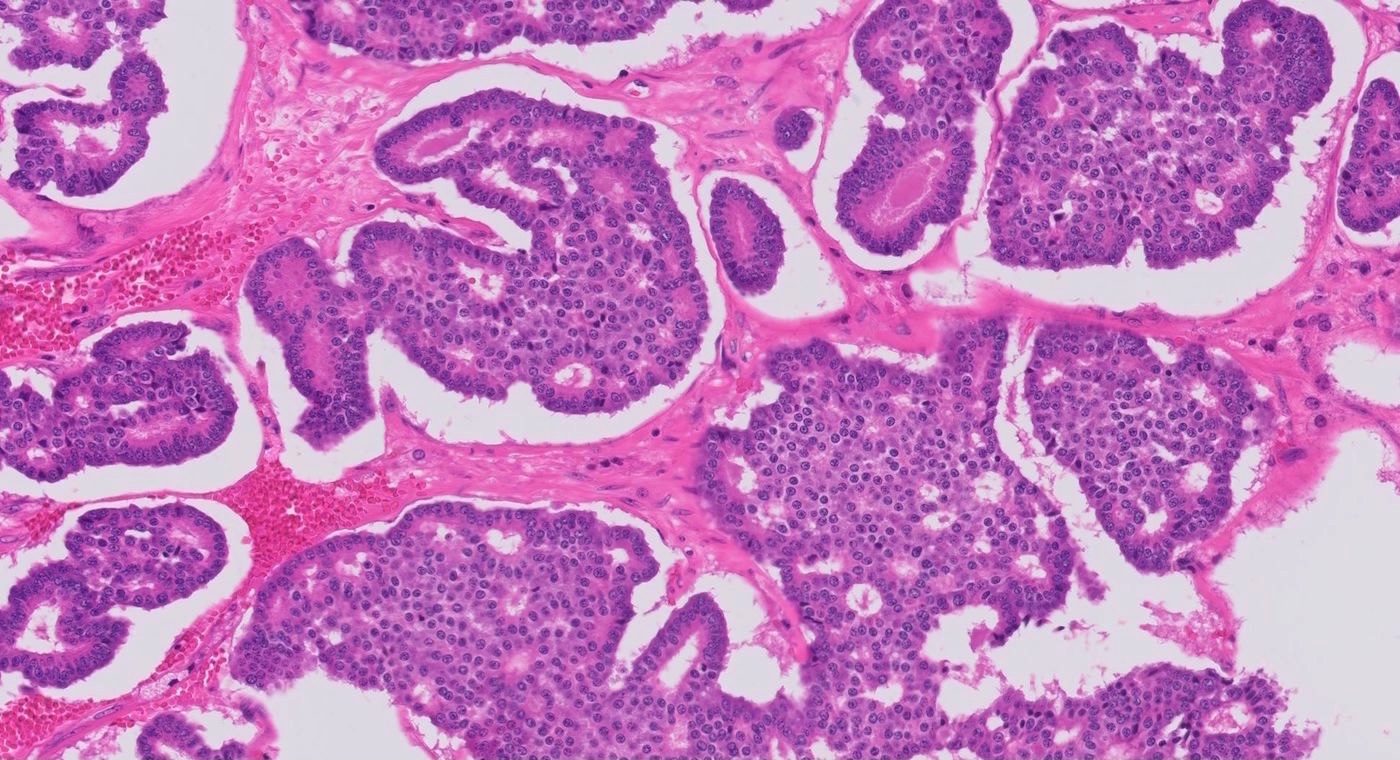
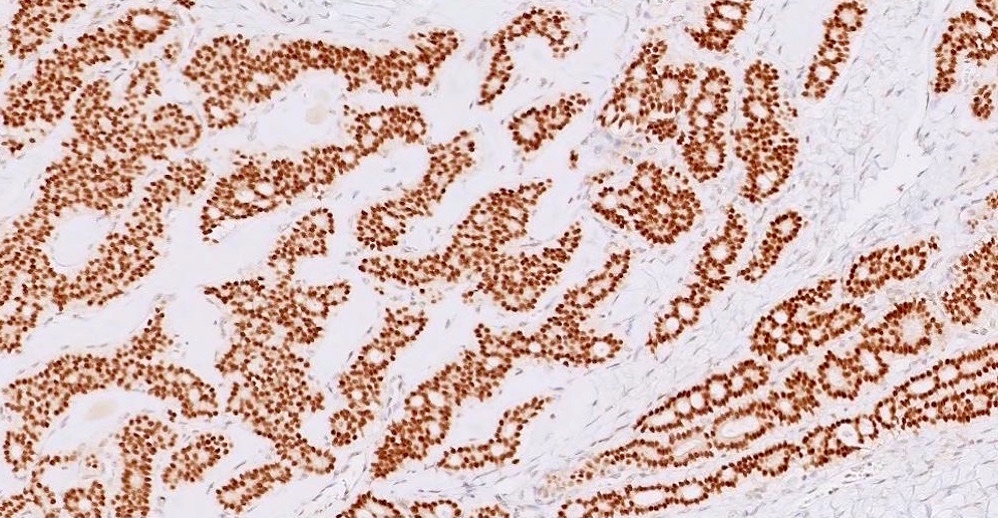
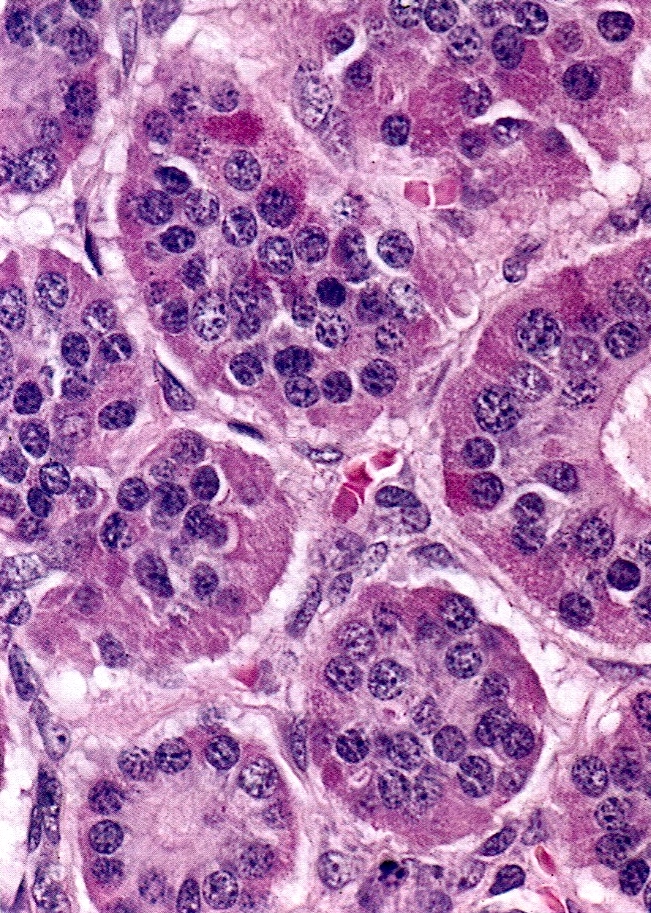
- Trabecular carcinoid
- Associated with mature cystic teratoma, rare in pure form
- 1 or 2 cell layers arranged in long, wavy, branching cords, parallel ribbons or trabeculae
- Occasionally, acinar pattern may be seen admixed with trabecular pattern
- Tumor cells are uniform, round to oval, with amphophilic, slightly granular cytoplasm at the base and prominent, centrally located, ovoid or elongated nuclei with finely stippled chromatin; red-brown granules may be seen at the cell base
- Stroma is represented by dense fibrous connective tissue, which may be hyalinized or luteinized
- Low mitotic activity, only occasional mitoses
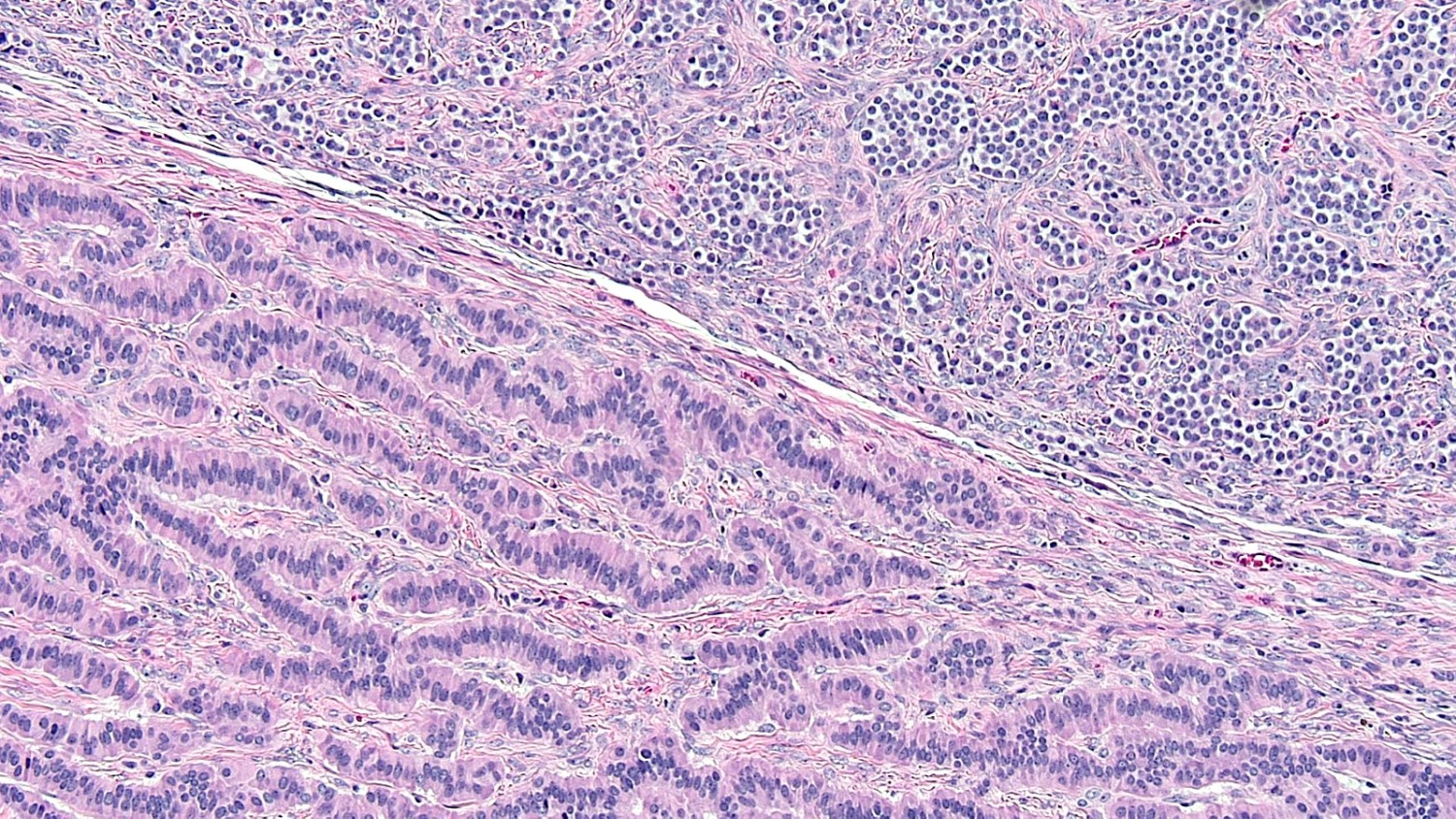
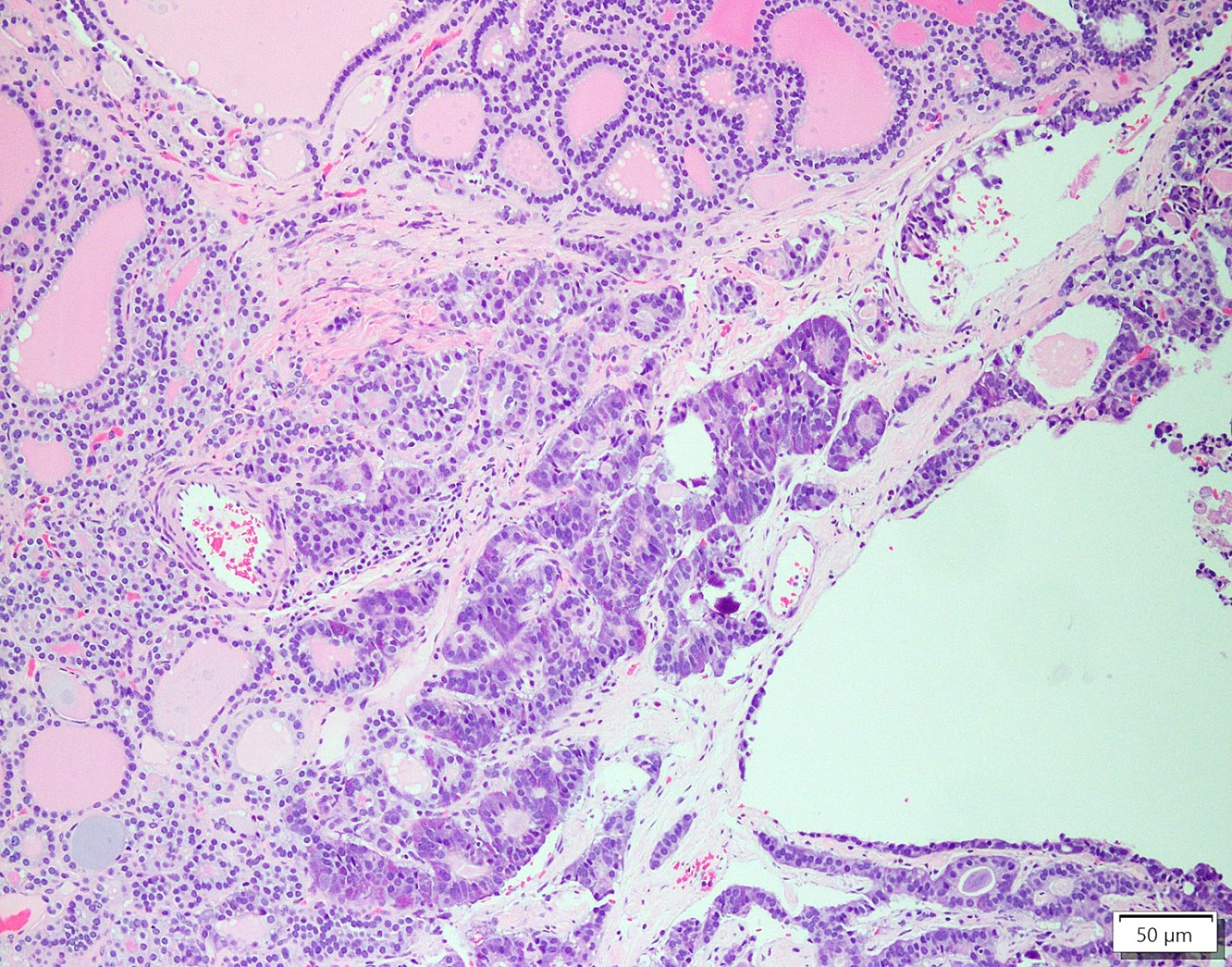
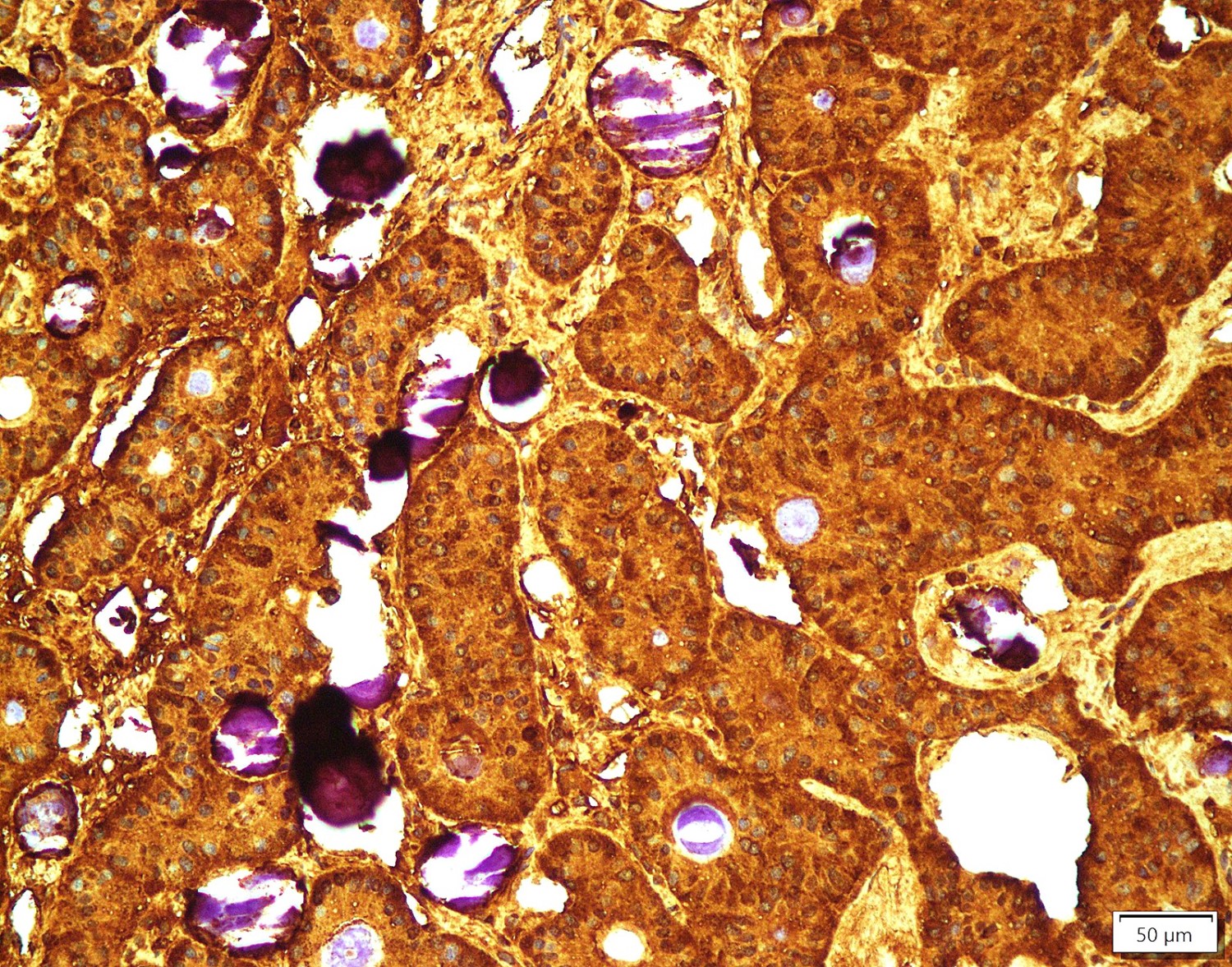
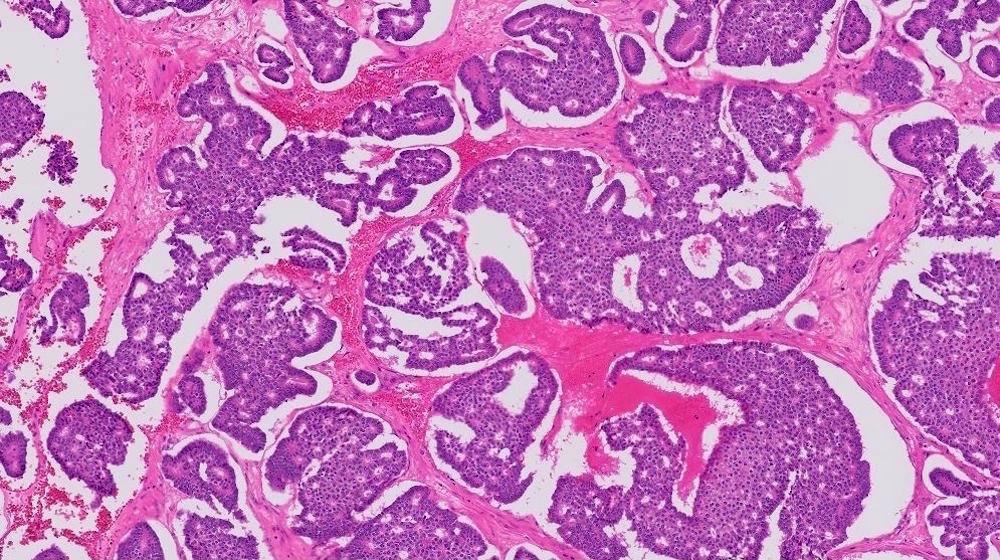
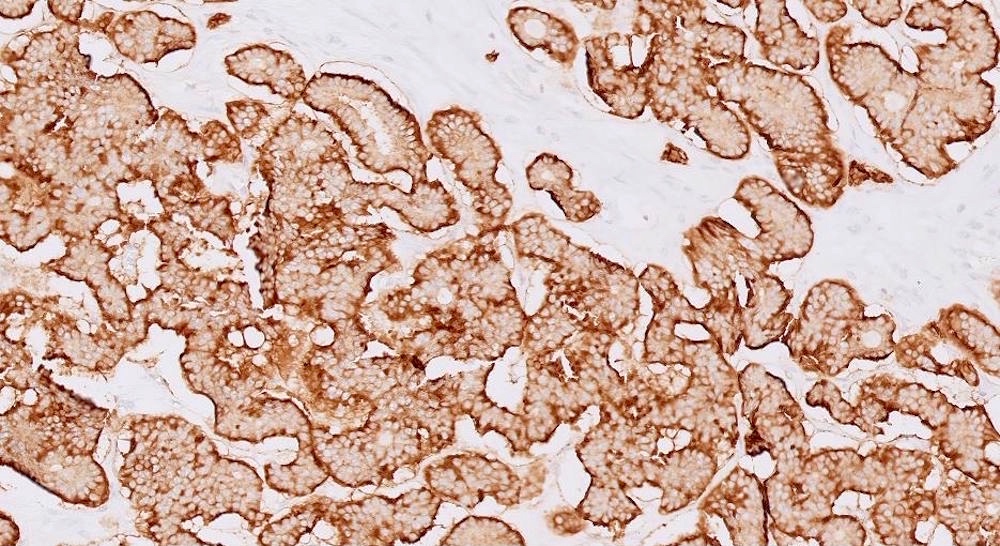
- Strumal carcinoid
- Commonly associated with mature cystic teratoma; often is seen in pure form (40%); rarely can be associated with mucinous tumor (J Cancer Res Clin Oncol 1984;107:125, J Int Med Res 2021;49:3000605211034666, Front Endocrinol (Lausanne) 2022;13:871210)
- Composed of thyroid tissue intimately admixed or juxtaposed with a neuroendocrine neoplasm (struma ovarii and carcinoid)
- Either of the components may be predominant
- Trabecular pattern >> both trabecular and insular patterns > insular only
- Thyroid component resembles normal thyroid tissue; rarely, papillary or follicular carcinoma may be present
- Stroma may show luteinization
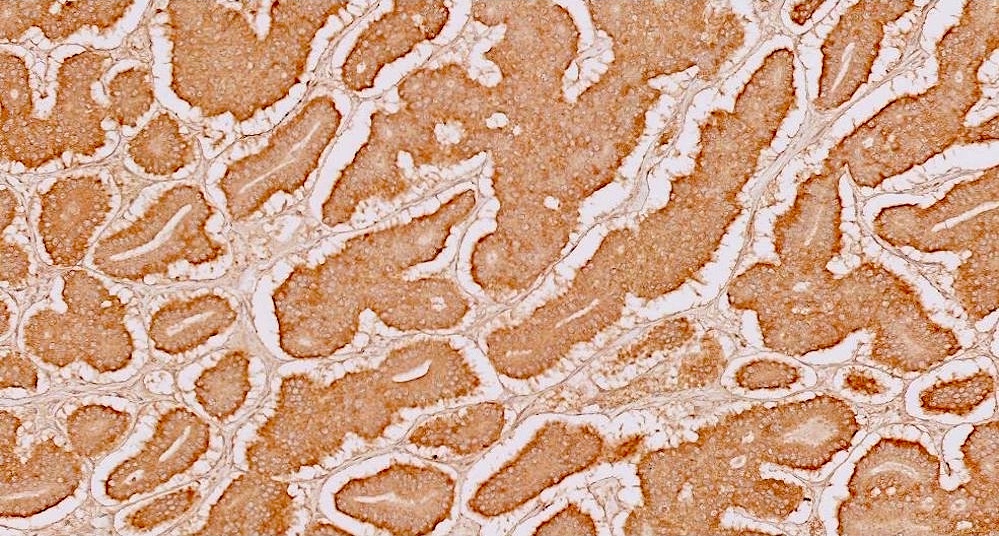
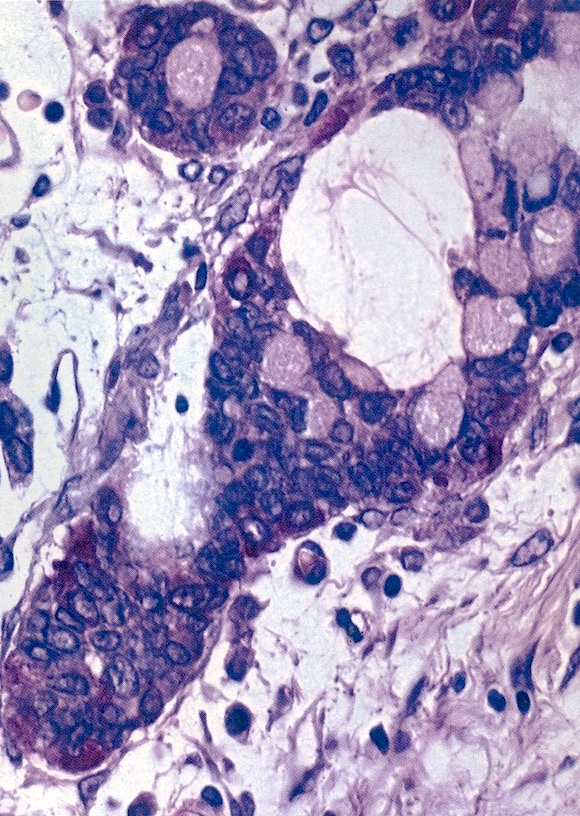
- Mucinous carcinoid
- These morphologically resemble low grade goblet cell adenocarcinoma of the appendix (previously termed goblet cell carcinoid)
- Pure form >> in association with mature cystic teratoma
- Composed of numerous small glands or acini with very small lumina floating in pools of mucin (pseudomyoxoma ovarii); some of the glands or acini may be cystically dilated containing mucin
- Lined by uniform cuboid or columnar and goblet cells and containing small round or oval nuclei and cytoplasmic neuroendocrine granules
- In some areas, the tumor cells tend to invade the surrounding connective tissue, often assuming signet ring appearance
- Tumor may form large solid aggregates, show a less uniform appearance and have more atypical features with large hyperchromatic nuclei and brisk mitotic activity
- Insular carcinoid
- Can also be mixed and present as a combination of 2 or more types of carcinoids
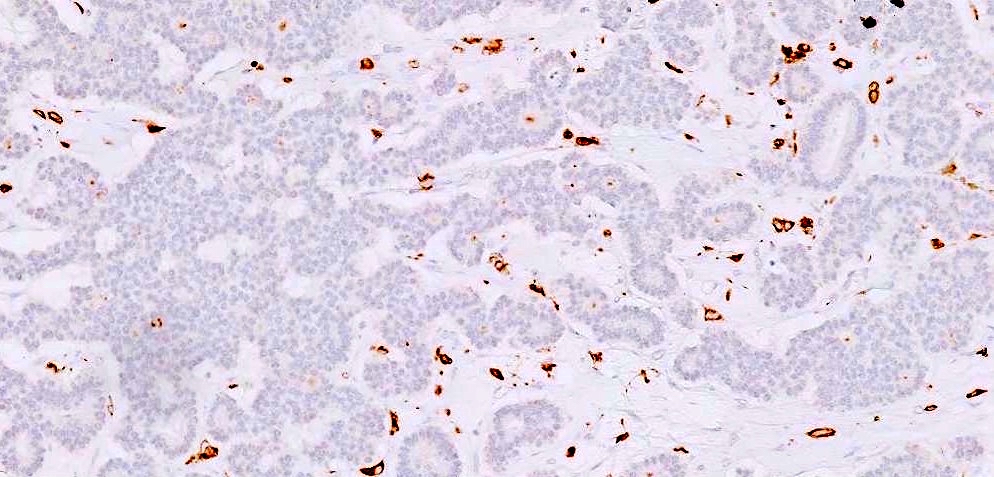
Microscopic (histologic) images
Contributed by Krisztina Hanley, M.D., Rulong Shen, M.D. and AFIP
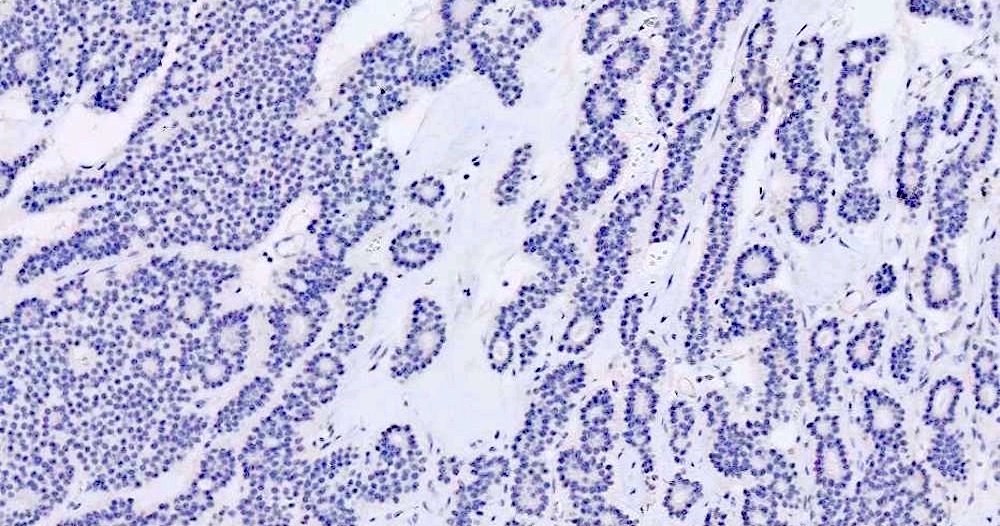
Positive stains
- Insular: chromogranin, synaptophysin, CD56
- Trabecular: synaptophysin, CD56, serotonin
- Strumal: chromogranin, synaptophysin, NSE, galectin3 in carcinoid component; TTF1 in thyroid component (Medicine (Baltimore) 2019;98:e18009)
- Mucinous: pankeratin, synaptophysin, chromogranin, CDX2, CK20
- Reference: Cancers (Basel) 2022;14:1835
Negative stains
- TTF1, PAX8, thyroglobulin only stain the struma component
Electron microscopy description
- Numerous neurosecretory granules
Videos
Germ cell neoplasms of the ovary - ovarian carcinoid tumor
by Dr. Wafaey Badawy
Sample pathology report
- Right ovary, oophorectomy:
- Ovarian carcinoid tumor, arising from struma ovarii (see comment)
- Comment: Sections show extensive involvement of the ovary by a well differentiated neuroendocrine tumor, showing acinar, trabecular, tubular, corded and some rare areas of solid growth patterns, confined to the ovary without surface involvement. Background shows benign thyroid tissue. Immunohistochemical stains including chromogranin and synaptophysin support neuroendocrine differentiation. Given the presence of benign thyroid tissue, this neoplasm is classified as a strumal carcinoid. The use of proliferative markers such as Ki67 has not been established in the grading of these tumors and in this case, it is < 1%
- Left ovarian cyst, resection:
- Ovarian carcinoid tumor (4.5 mm), trabecular type, arising in a mature cystic teratoma (dermoid cyst) (see comment)
- Comment: Extensive sampling of this mature teratoma shows a 4.5 mm trabecular carcinoid tumor. Immunohistochemical stains confirm neuroendocrine differentiation as the tumor cells are positive for synaptophysin, chromogranin, CD56, MCK (AE1 / AE3) and Ki67 is ~2%. This small focus of carcinoid tumor shows CDX2 positivity indicating midgut origin, similar to the gastrointestinal counterpart.
Differential diagnosis
- Carcinoid metastasis:
- Bilateral, no associated teratoma or struma ovarii
- Often multinodular growth
- Microscopically indistinguishable from primary
- Most commonly from midgut primary
- Brenner tumor:
- May be confused with insular carcinoid
- Transitional epithelial cells, grooved nuclei, lack of cytoplasmic granules
- Krukenberg tumor:
- Bilateral, marked cellular and nuclear pleomorphism
- Mitotically active, abundant mucin
- Signet ring cells are common
- Lymphovascular invasion is common
- Sertoli cell tumor (SCT) with trabecular architecture:
- SCT is positive for inhibin and calretinin, negative for synaptophysin
- Trabecular carcinoid is positive for synaptophysin, negative for inhibin and calretinin
Additional references
Board review style question #1
Which of the following is true for primary ovarian carcinoid?
- Most cases of primary ovarian carcinoid are associated with mature cystic teratoma
- Mucinous ovarian carcinoid behaves less aggressively than other types
- Primary ovarian carcinoids are poorly differentiated neuroendocrine tumors
- To cause carcinoid syndrome, the presence of liver metastasis is required
Board review style answer #1
A. Most cases of primary ovarian carcinoid are associated with mature cystic teratoma. Despite mucinous ovarian carcinoids more frequently occurring in pure form, 3 of 4 types, including the most common insular type, mostly arise in mature cystic teratoma.
Answer B is incorrect because mucinous ovarian carcinoid is more aggressive than other types of primary ovarian carcinoid.
Answer C is incorrect because per definition, primary ovarian carcinoid tumors are well differentiated neuroendocrine tumors.
Answer D is incorrect because ovarian veins drain directly into systemic circulation: the right ovarian vein drains directly into the inferior vena cava, while the left ovarian vein joins the left renal vein. Therefore, hormones produced by a carcinoid tumor do not undergo hepatic metabolism.
Comment Here
Reference: Carcinoid tumor
Comment Here
Reference: Carcinoid tumor
Board review style question #2
Which of the following indicates poor prognosis of patients with primary ovarian carcinoid?
- Carcinoid heart syndrome
- Insular type
- Low Ki67 proliferative index
- Trabecular type
- Tumor confined to the ovary
Board review style answer #2
A. Carcinoid heart syndrome can be a presenting symptom even in the absence of liver metastases. The 3 year survival has been reported to be 31%.
Answer B is incorrect because insular type is slow growing and only occasionally metastasizes. The prognosis is favorable.
Answer C is incorrect because a high Ki67 proliferative index, not low, is associated with worse outcomes.
Answer D is incorrect because trabecular type is not associated with metastasis and has favorable prognosis.
Answer E is incorrect because the absence of tumor spread is a good prognostic factor.
Comment Here
Reference: Carcinoid tumor
Comment Here
Reference: Carcinoid tumor