Table of Contents
Definition / general | Essential features | Embryology | Physiology | Diagrams / tables | Clinical features | Laboratory | Gross description | Gross images | Frozen section description | Frozen section images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Negative stains | Videos | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Atwi D, Ghofrani M, Hassell LA. Anatomy & histology. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/ovarynontumornormalhistology.html. Accessed November 27th, 2024.
Definition / general
- Paired female reproductive glands located on each side of the uterus, adjacent to the lateral pelvic wall, posterior to the broad ligament and anterior to the rectum
- Originate from the genital ridge formed by the thickening of the coelomic epithelium with oogonia later migrating from the yolk sac endoderm (Am J Surg Pathol 1987;11:277)
Essential features
- Paired ovoid organs located on each side of the uterus
- Responsible for the development of the dominant follicle and the production of hormones
- Multiple histologic components can be seen in the normal ovaries and can mimic pathologic findings
Embryology
- Ovary is composed of 4 main components, each with different embryologic origins, all of which eventually come together in the developed ovary: surface epithelium, stroma, germ cells and sex cords
- Embryonic coelomic cavity is initially lined by primitive mesothelium (modified coelomic epithelium), which arises from the underlying mesoderm
- At ~5 weeks gestation, the gonadal ridge develops as a coelomic thickening and mesenchymal growth high in the abdominal cavity near where the kidneys develop
- Coelomic epithelium forms the ovarian surface epithelium
- Subcoelomic mesoderm forms the ovarian stroma
- Primordial germ cells migrate from the yolk sac endoderm to the developing ovary
- Invaginations of coelomic epithelium in the superficial ovarian cortex form the sex cords (pregranulosa cells)
- During weeks 12 - 20, the vascular network develops from the hilus towards the cortex and pregranulosa cells encircle germ cells to form primordial follicles, which in turn are encircled by stroma derived theca cells
- Germ cells differentiate into oogonia, which differentiate into primary oocytes and arrest in this stage until puberty
- Each ovary descends into the pelvis along the gubernaculum (attached inferiorly to the inguinal region); the gubernaculum becomes part of the uterine wall at entry of the fallopian tube and persists in adults as ovarian and round ligaments
- Invaginations of the coelomic epithelium at the site of the gonadal ridge also give rise to two types of genital ducts: the mesonephric (Wolffian) ducts and the paramesonephric (Müllerian) ducts
- Müllerian ducts eventually give rise to the fallopian tubes and fuse to form the uterus
- Wolffian (mesonephric) duct remnants may be seen in the vicinity of the Müllerian system later in life
- Gonadal development is influenced by both male and female promoting signals (Mol Endocrinol 2008;22:1)
- References: Wikipedia: Gonadal Ridge [Accessed 26 December 2023], Embryology: Human Embryology [Accessed 26 December 2023]
Physiology
- Function first described by Reinier de Graaf (Arch Pathol Lab Med 2000;124:1115)
- Ovaries play an essential role in the fertility and cycling of reproductive activity in women, mainly by controlling the development of the dominant follicle and producing hormones (estrogen and progesterone) (Endotext: Morphology and Physiology of the Ovary [Accessed 9 September 2021])
- Folliculogenesis starts by recruiting primordial follicles into growing follicles that eventually proceed either to ovulation or death
- Folliculogenesis is divided into preantral (growth and differentiation of follicles) and antral phase (increase in the follicle size)
- Folliculogenesis will result in the production of a single dominant follicle (Graafian follicle), which will eventually ovulate
- ~400,000 primordial follicles containing primary oocytes are present at birth in ovarian stroma (100,000 at gestational age of 15 weeks; 680,000 at 8 months) (Fertil Steril 2007;88:675)
- Follicular decay appears to advance with increasing age; prominent cystic follicles are present at birth and at puberty (Hum Reprod 2008;23:699)
- Germ cells travel from yolk sac endoderm to ovary where they develop into oogonia and oocytes, arresting at prophase of mitosis
- Ovulation: induces cyclic rupture and regenerative repair of the ovarian surface epithelium
- Following ovulation, the dominant follicle becomes the corpus luteum responsible for the production of progesterone during the luteal phase of each menstrual cycle or becomes the corpus luteum of pregnancy to sustain gestation
- Hormones produced by the dominant follicle are essential for the preparation of the uterus for implantation of the embryo (Endotext: Morphology and Physiology of the Ovary [Accessed 9 September 2021])
- Hilus cells produce steroids (predominantly androstenedione); resemble Leydig cells of testis; may produce masculinizing tumors (hilus cell tumors)
Diagrams / tables
Clinical features
- Characteristic streak gonads in patients with Turner syndrome, also known as congenital ovarian hypoplasia, due to monosomy X (45,XO); these are not functional and will subsequently manifest with symptoms of ovarian failure (J Minim Invasive Gynecol 2015;22:S15)
- Primary ovarian insufficiency: a condition diagnosed in women less than 40 years of age and characterized by depletion or dysfunction of the ovarian follicles with subsequent impaired ovarian function (N Engl J Med 2009;360:606)
Laboratory
- Tests that evaluate the ovarian function usually done in the context of primary or secondary amenorrhea or infertility problems (Am Fam Physician 2013;87:781)
- These tests include but are not limited to
- Measurement of follicle stimulating hormone (FSH) and luteinizing hormone (LH) levels
- Estrogen production: serum 17 beta estradiol level
- Serum progesterone level
Gross description
- Attachment:
- Along its anterior (hilar) margin to posterior aspect of broad ligament by mesovarium (double fold of peritoneum)
- At its medial pole to ipsilateral uterine cornu by utero-ovarian ligament
- At superior aspect of lateral pole to lateral pelvic side wall by infundibulopelvic (suspensory) ligament
- Laterality in a hysterectomy and bilateral salpingo-oophorectomy specimen established based on the
- Utero-ovarian ligament, which connects each ovary to the ipsilateral uterine cornu and is situated posterolateral and inferior to the attachment of the fallopian tubes
- Posterior peritoneal reflection, which extends over a longer segment of the uterus compared to the anterior surface, which has a longer roughened area
- Appearance of the ovary depends widely on the age / menopausal state:
- Prepubertal ovaries:
- Newborn ovaries are elongated and approximately 1.3 cm in greatest dimension
- Ovaries enlarge during infancy and childhood and reach adult size and shape by the time of puberty
- Neonatal ovaries often have cysts, which resolve spontaneously (J Pediatr Endocrinol Metab 2007;20:397)
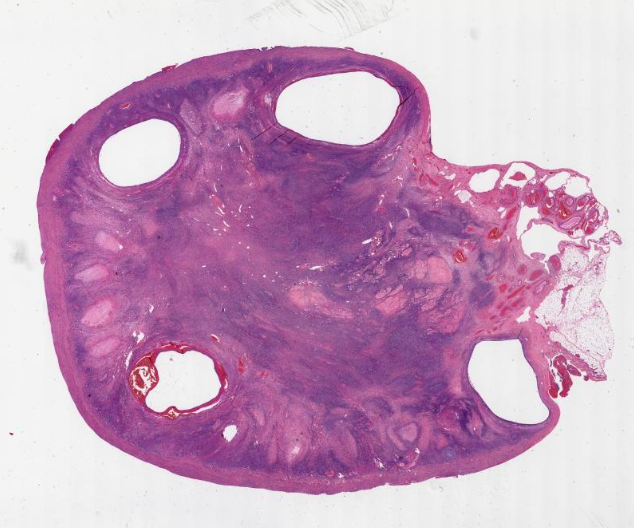
- Premenopausal ovaries:
- 3 - 5 cm long and weigh 5 - 8 g; size and weight depend on the amount of follicular derivatives (cysts and corpora albicantia / lutea)
- Pink-white exterior is initially smooth but gradually becomes more convoluted
- Cystic follicles and corpora lutea may be visible from outside
- Cut section may exhibit 3 zones: cortex, medulla and hilus, with follicular derivatives usually in the cortex and medulla
- Postmenopausal ovaries:
- Firm consistency with solid, pale cut surface
- Occasional cysts measuring several millimeters in diameter (inclusion cysts) may be discernible within the cortex
- Small white scars (corpora albicantia) are typically present within the medulla
- Thick walled blood vessels may be appreciable within the medulla and the hilus
- Prepubertal ovaries:
- Blood supply and drainage:
- Arterial supply: approximately 10 arterial branches from anastomotic arcade of ovarian artery (branch of aorta) and ovarian branch of uterine artery penetrate hilus into medulla and cortex
- Venous drainage: left ovarian vein drains to left renal vein, right ovarian vein drains to inferior vena cava
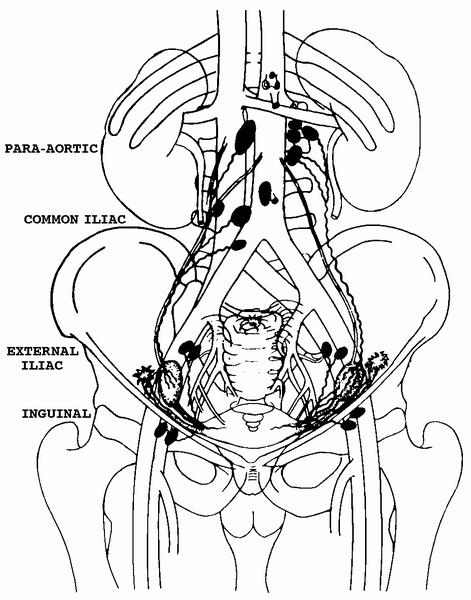
- Lymphatic drainage: originates predominantly from theca layer of follicles, exiting through the hilus, to the mesovarium, along the infundibulopelvic ligament, into upper paraaortic lymph nodes; may bypass to internal iliac, external iliac, common iliac, sacral, obturator, pelvic, retroperitoneal or inguinal nodes
Gross images
Frozen section description
- Enlarged corpus luteum cyst can trigger an intraoperative consultation; the cyst lining is yellow and has a convoluted appearance
- Luteoma of pregnancy can be discovered incidentally during cesarean section or preoperatively on imaging study mimicking an ovarian mass (J Magn Reson Imaging 2009;29:713)
Microscopic (histologic) description
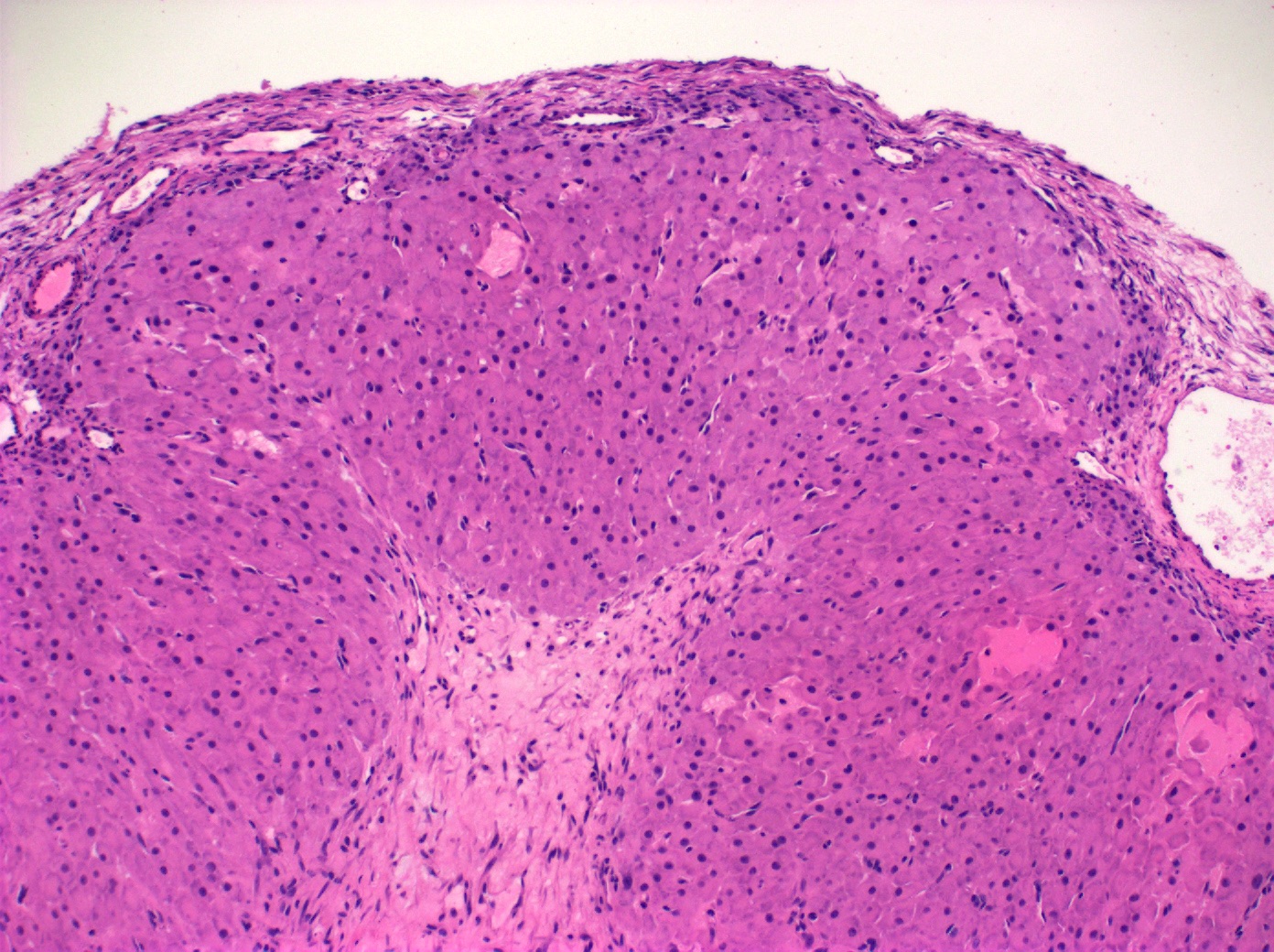
- Ovarian parenchyma can largely be divided into 3 compartments:
- Albuginea: a protective hypocellular compartment, composed of a fibrotic layer measuring approximately 0.3 mm and occupying the most superficial part of the ovary (Obstet Gynecol 1971;37:832, Ann Diagn Pathol 2020;46:151475)
- Cortex: a 0.3 mm hypercellular layer composed of spindle cells arranged parallel to the surface and housing the majority of the follicles in a premenopausal woman (Ann Diagn Pathol 2020;46:151475)
- Medulla: a hypocellular area beneath the cellular cortex and housing abundant blood vessels; nodular or diffuse proliferation of spindle cells can commonly be seen in the medulla (Ann Diagn Pathol 2020;46:151475)
- Stroma:
- Comprises bulk of ovarian tissue
- Resembles fibroblasts in whorls / storiform pattern surrounded by dense reticulin network
- Contains luteinized stromal cells, decidual cells, smooth muscle, fat, neuroendocrine cells and endometrial stroma-like cells
- Ovarian parenchyma can alternatively be defined as the ovarian follicles, given that the follicles are the constituents that perform the function of the ovary with all the other constituents being labeled as ovarian stroma (Reproduction 2020;160:R25)
- Number of primordial follicles and oocytes in premenopausal women can be markedly different between the 2 ovaries (Ann Diagn Pathol 2020;46:151475)
- Within the same ovary, the primordial follicles and oocytes exhibit an uneven distribution in the cortex with clustering in few areas (Ann Diagn Pathol 2020;46:151475)
- In addition to their more common location in the cortex, the primordial follicles can be seen in the medulla within areas of nodular proliferations, especially in women with abundant follicular cysts (Ann Diagn Pathol 2020;46:151475)
- Follicle is designated cystic when it measures 2 mm or more but less than 9 mm; these are very common and can be lateralized to 1 ovary in some individuals (Endocrinol Metab Clin North Am 1998;27:877)
- Stages of follicular development:
- Primordial follicle:
- Diplotene oocyte surrounded by a layer of flattened granulosa cells (Hum Mol Genet 2010;19:397)
- Neo-oogenesis may occur in adults (Endocrine 2005;26:301)
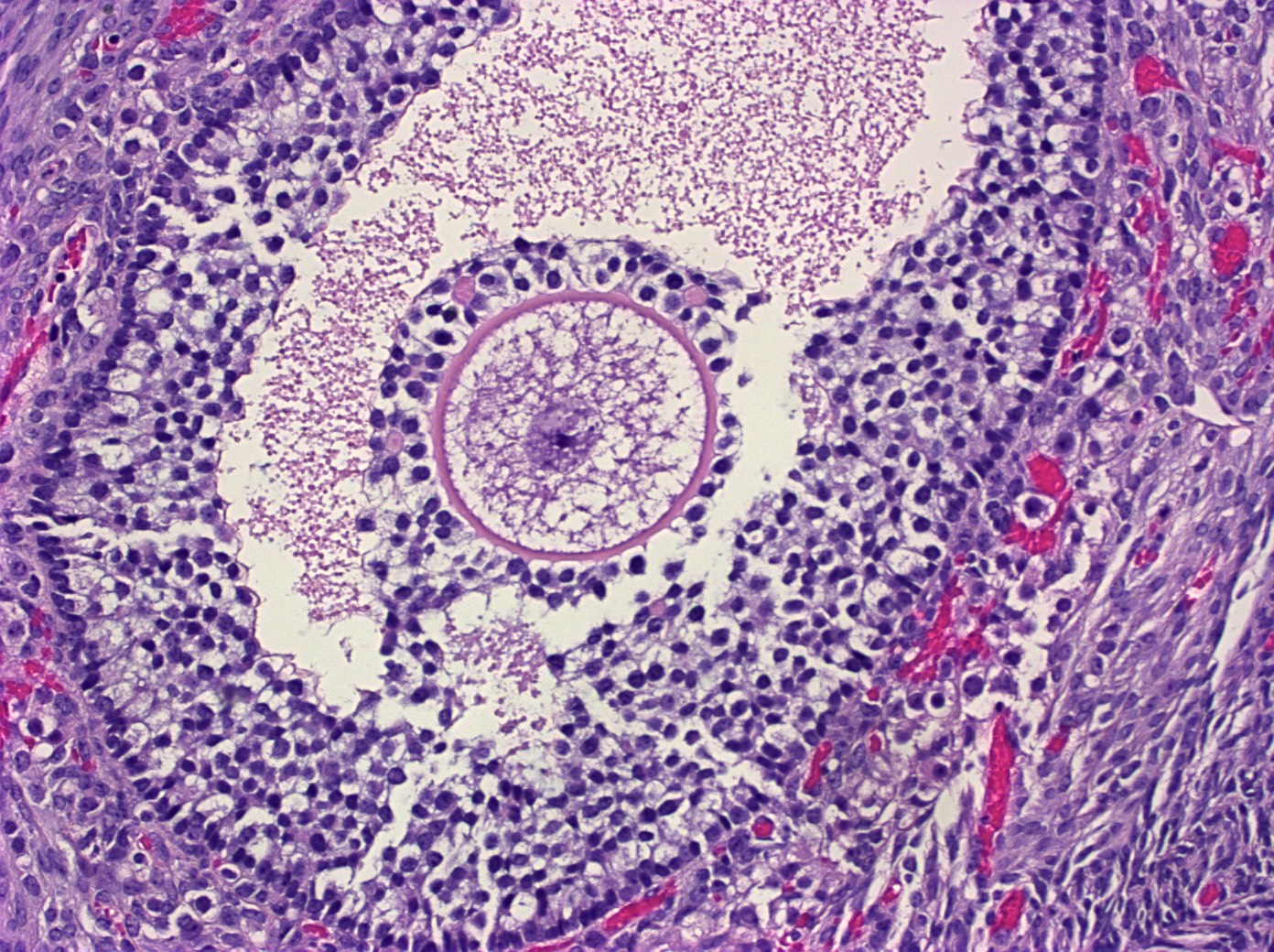
- Maturing follicle:
- Oocyte with surrounding granulosa cell layer
- Lacks reticulum
- Contains Call-Exner bodies (rosette-like formations with central filamentous / eosinophilic material consisting of excess basal lamina) and theca cells (within follicle are luteinized and produce sex hormones, external to follicle are very cellular)
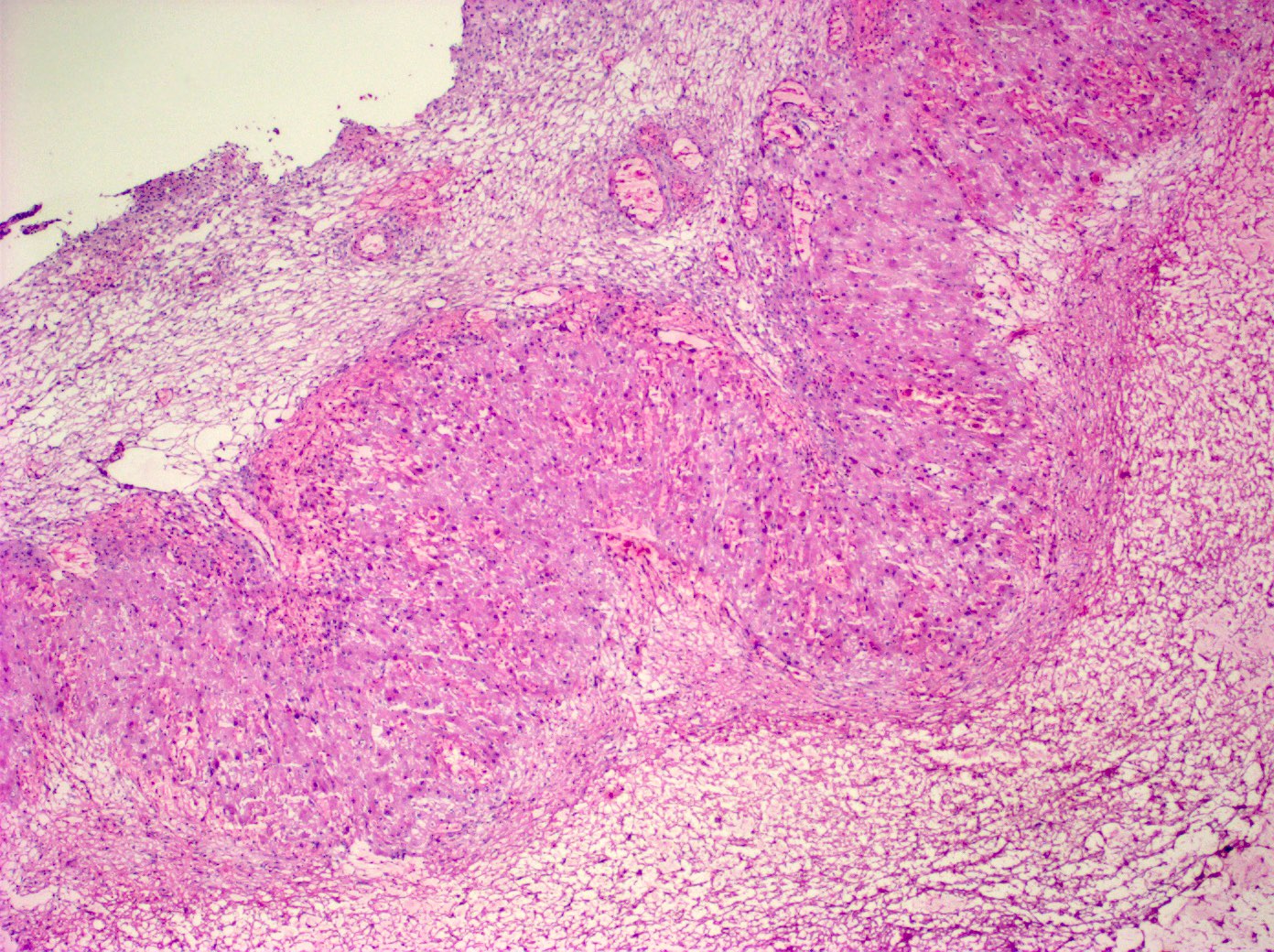
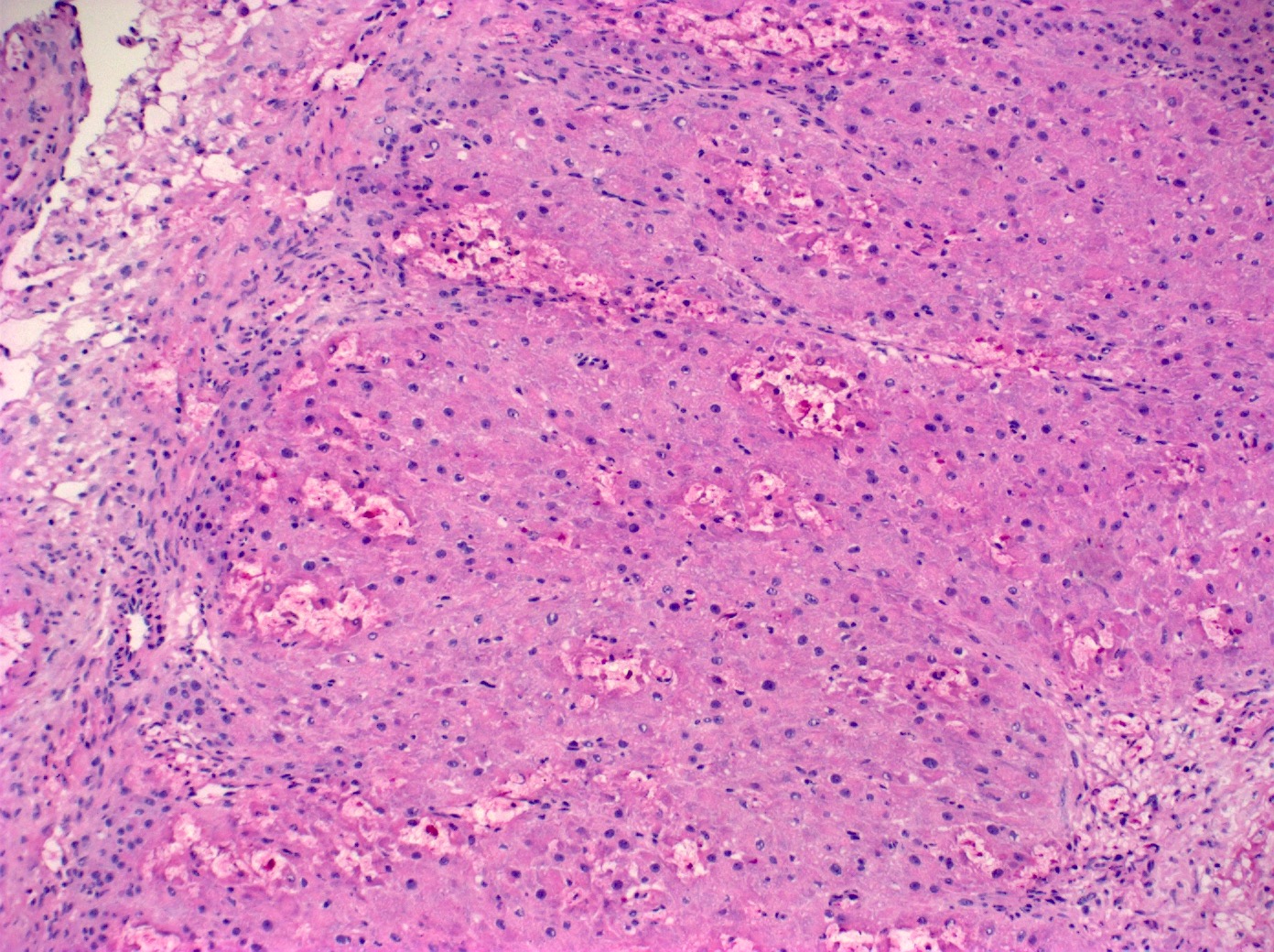
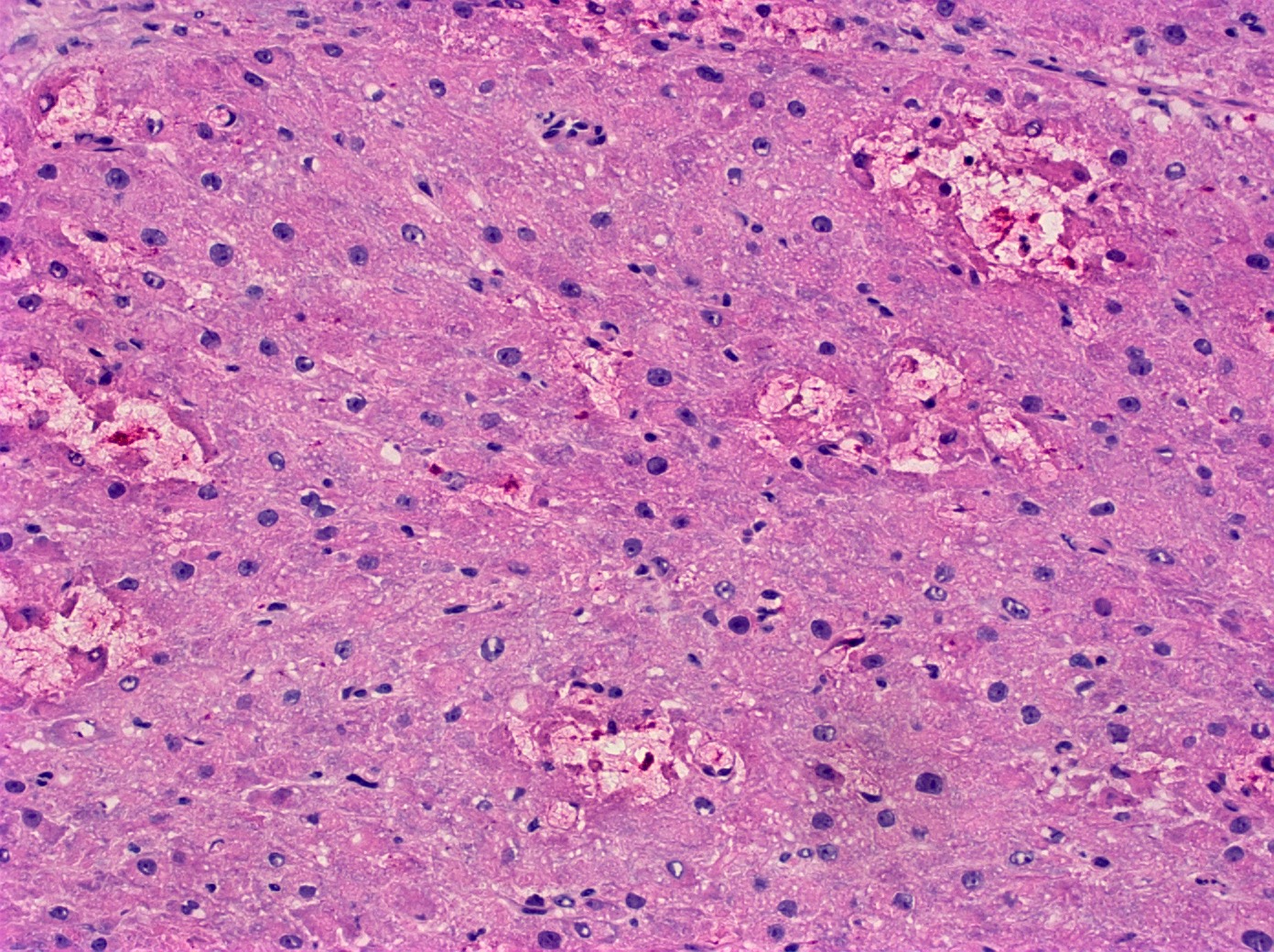
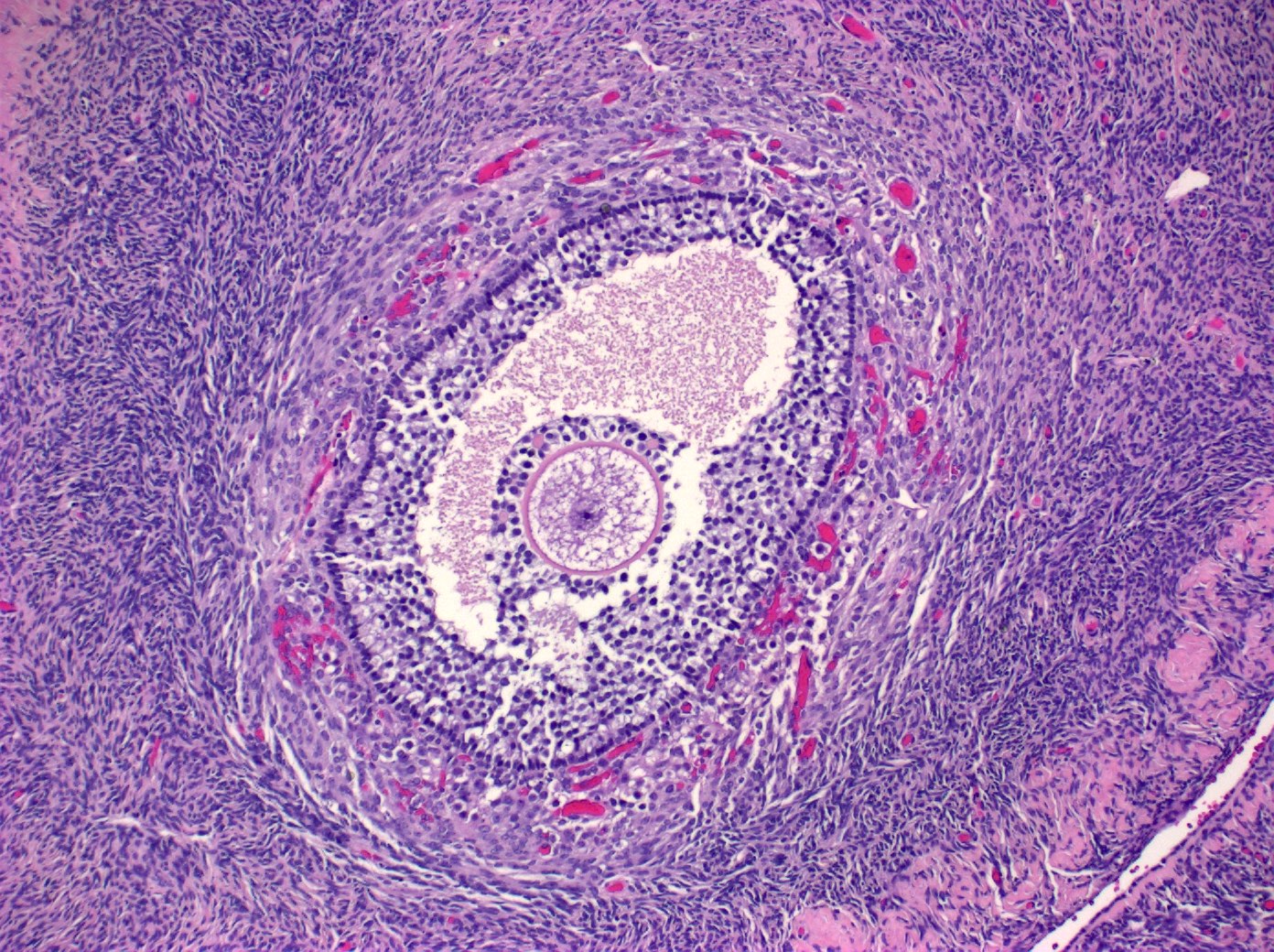
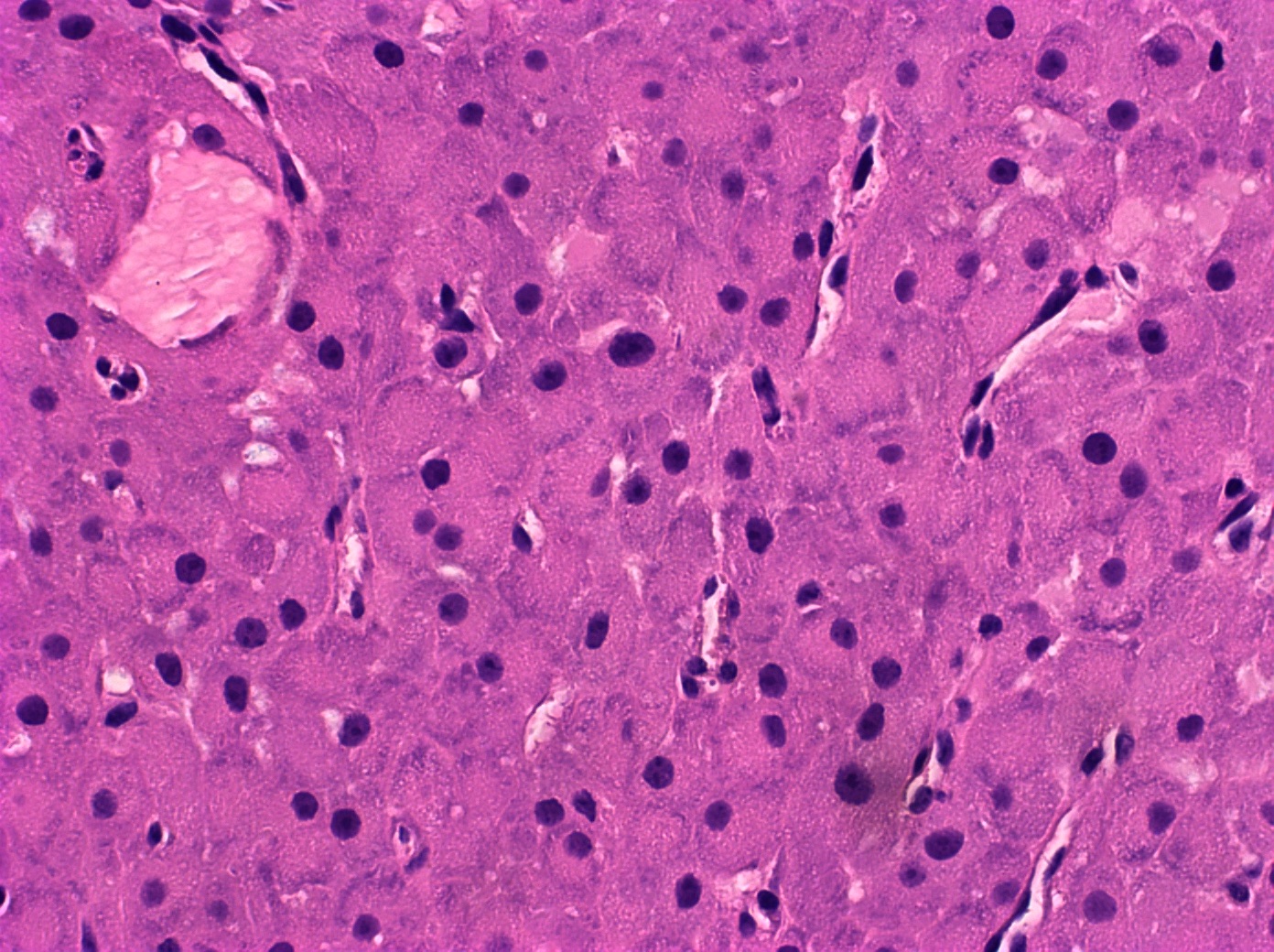
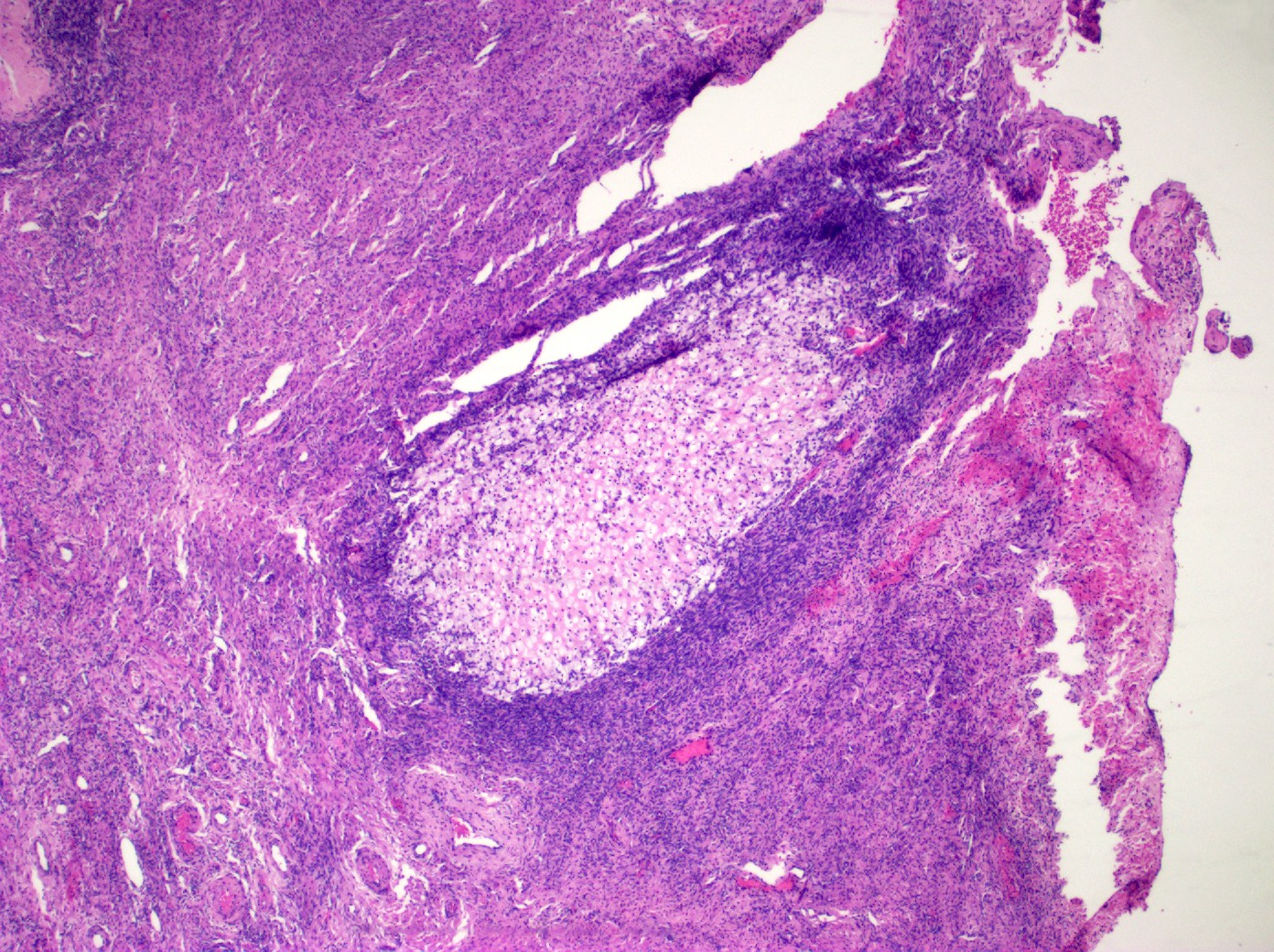
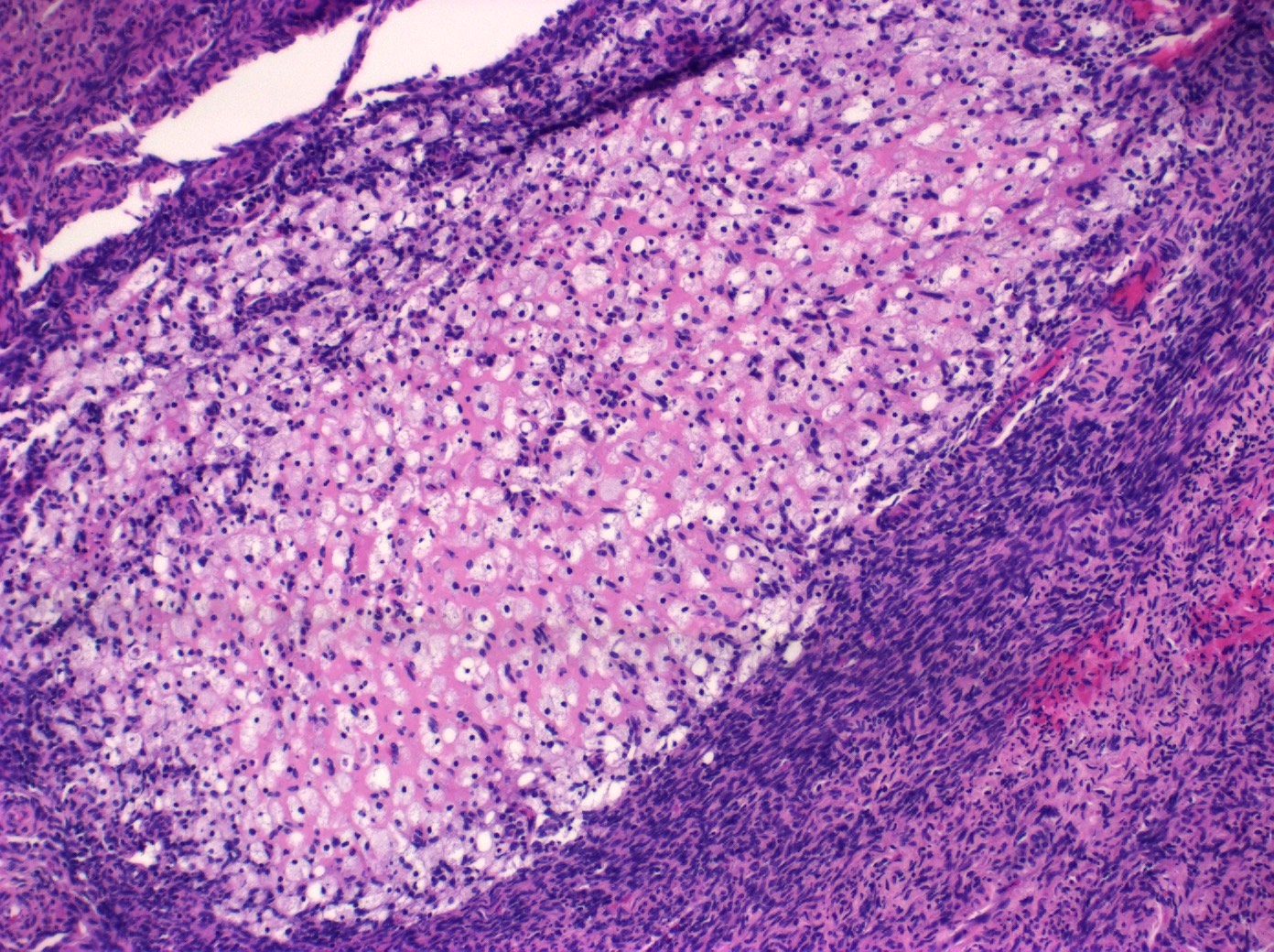
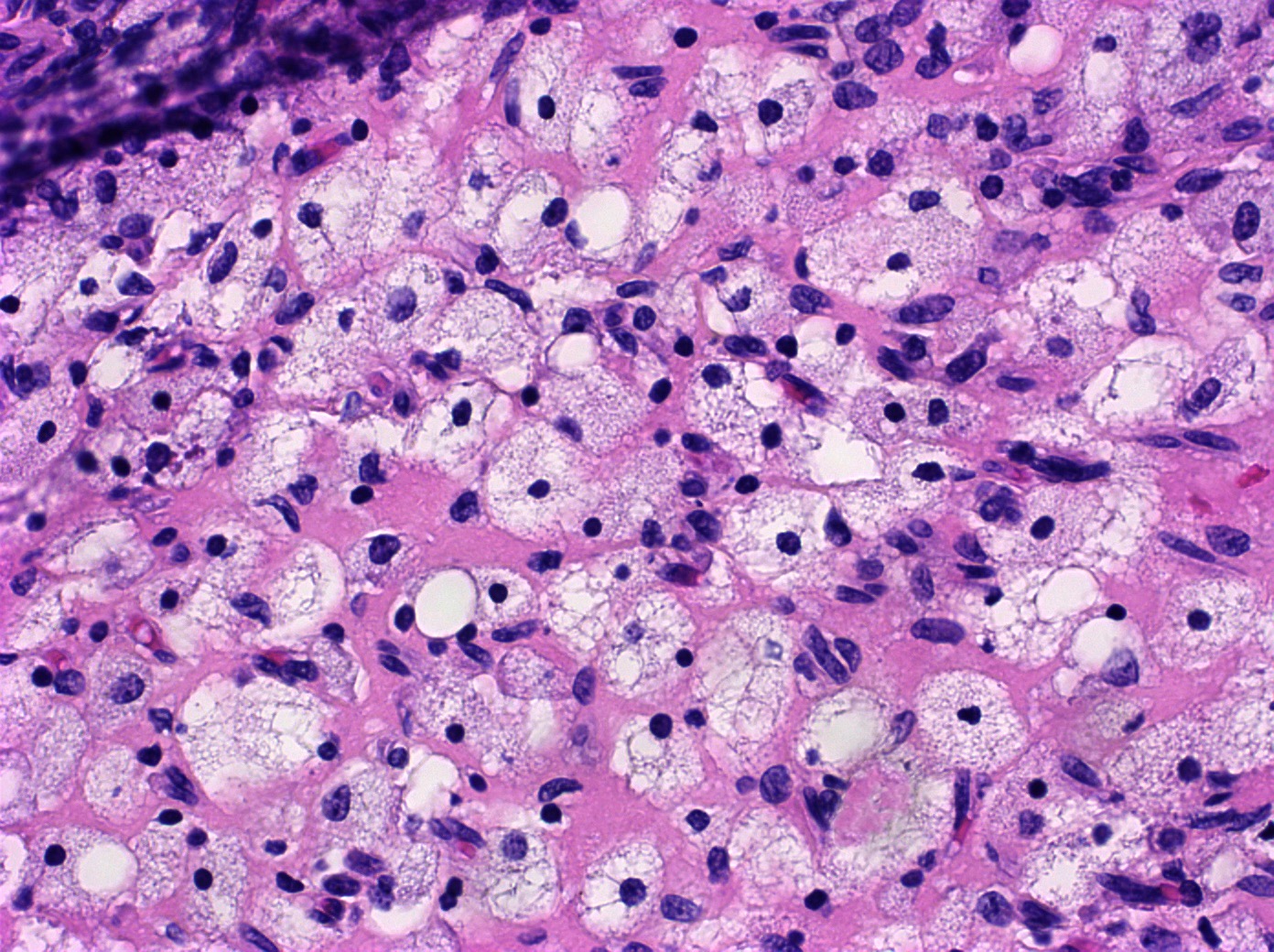
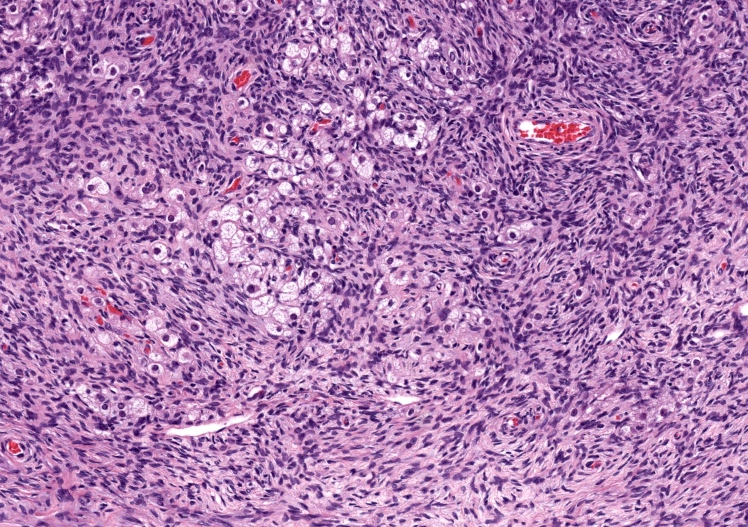
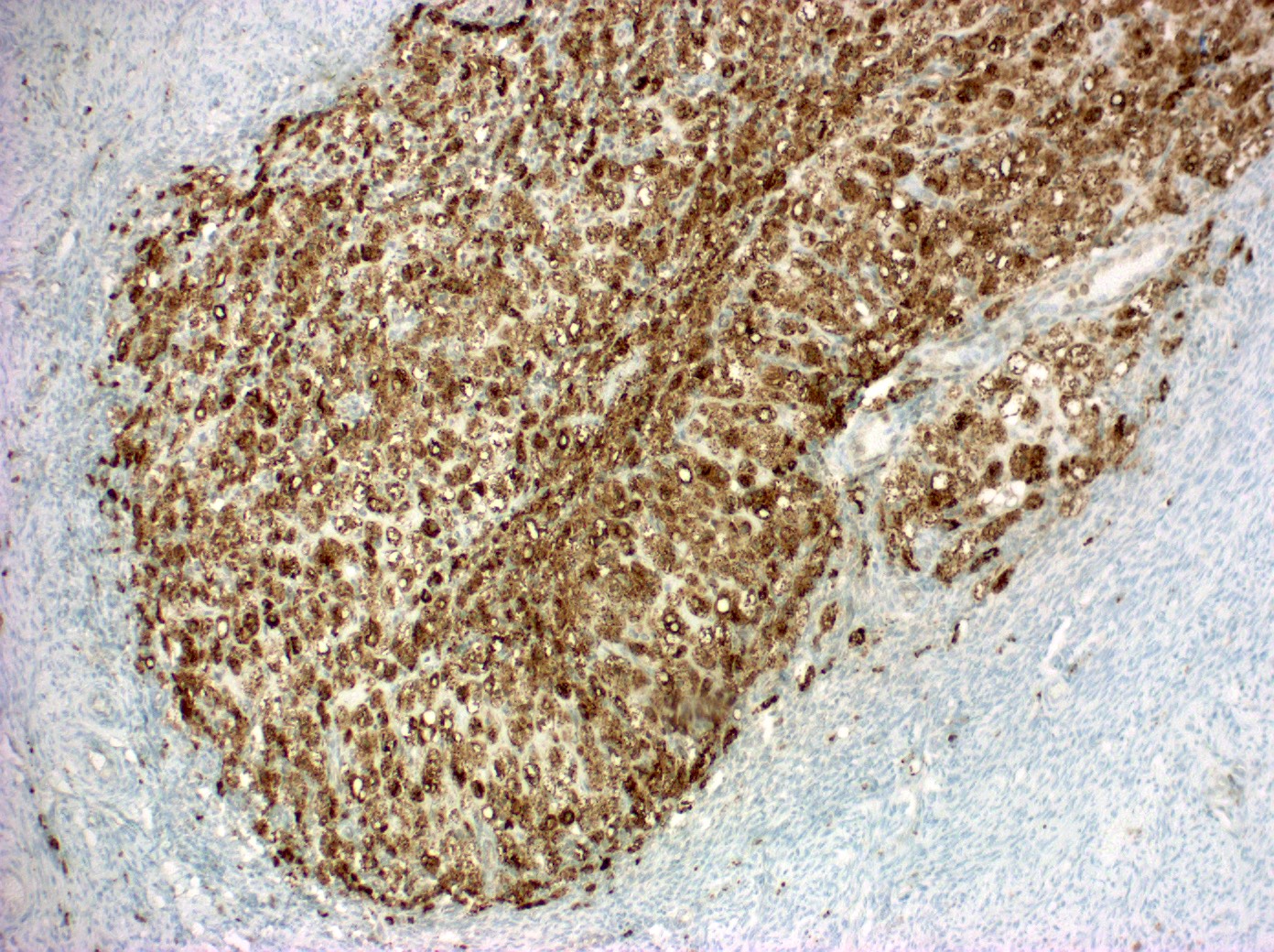
- Corpus luteum:
- 2 cm, round to serpiginous, yellow, lobulated structure with cystic center
- Has luteinized granulosa and theca cells
- In pregnancy, is larger, bright yellow with prominent central cavity, hyaline droplets and calcification
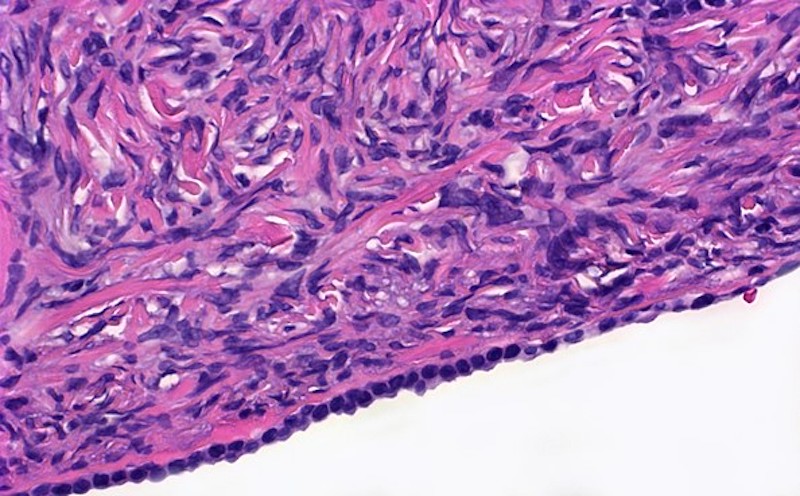
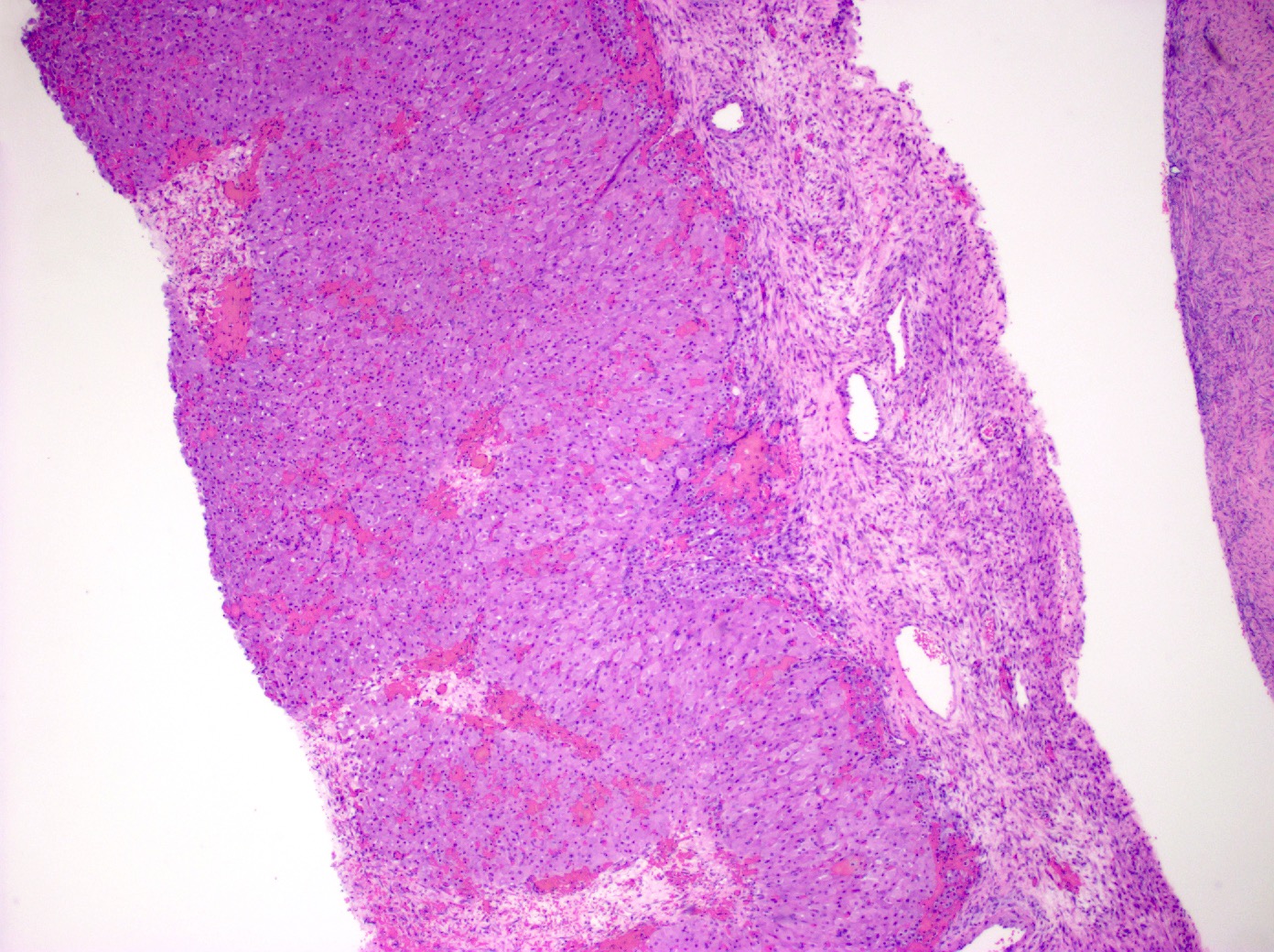
- Corpus albicans: remnant of corpus luteum, hyalinized, paucicellular fibrotic scar with serpiginous contours
- Primordial follicle:
- Other normal components:
- Surface epithelium:
- Ovarian surface epithelium (OSE) is a modified mesothelium, also called coelomic or germinal epithelium (Reprod Biol Endocrinol 2006;4:42)
- Single layer of flat to cuboidal mesothelial type cells, which appear to actively participate in the ovulatory rupture and repair process (J Histochem Cytochem 2020;68:113)
- Closely related to Müllerian duct lining epithelium
- Mesothelial inclusion cyst:
- Superficial cysts that are lined by mesothelial cells and represent invagination of the surface mesothelial epithelium
- Usually seen in ovaries with clefts (Ann Diagn Pathol 2020;46:151475)
- Endosalpingiosis:
- Group of glands and cysts with a tubal epithelial lining
- Usually seen in ovaries without clefts and commonly associated with calcification
- Rim of fibrotic tissue can surround them (Ann Diagn Pathol 2020;46:151475)
- In contrast to inclusion cysts, their presence can be associated with the recurrence of low grade serous neoplasms (Int J Gynecol Pathol 1998;17:1)
- Hilus (hilar) cells:
- Located in ovarian medulla, rarely within ovarian stroma; located away from the hilum, round to polygonal, epithelial appearing, presumed vestigial remnant of gonad from its ambisexual phase
- Closely associated with large hilar veins and lymphatics and may protrude within their lumina; also associated with nerves
- May contain Reinke crystalloids, lipid, lipochrome pigment
- Resemble steroid cells by electron microscopy with microtubular smooth endoplasmic reticulum, mitochondria with tubular cristae
- Hilar cells are seen in the fetal ovary but not in infancy and childhood; they reappear at puberty
- Hilar cell hyperplasia: associated with hCG administration, pregnancy and choriocarcinoma
- Rete ovarii:
- Counterpart of rete testis
- Seen as clefts, tubules, cysts, papillae lined by cuboidal or columnar epithelium
- Located usually in the hilum of the ovary, surrounded by spindle cell stroma
- Walthard cell nests:
- Usually microscopic cystic / solid structures with urothelial type epithelium and variable mucin seen in mesovarium, mesosalpinx and ovarian hilus
- Ovarian stem cells:
- Ovary can house stem cells for variable cell types with both somatic and germline stem cells being mentioned
- Somatic stem cells include granulosa cells, surface epithelial cells, thecal cells and stromal cells (Reproduction 2019;157:545)
- Cortical granuloma:
- Common incidental finding in the ovaries of late reproductive and postmenopausal women, composed of an aggregate of epithelioid histiocytes surrounded by a rim of lymphocytes
- They are of uncertain origin but could represent previous areas of endometriosis, luteinized stromal cells or ectopic decidua (Int J Gynecol Pathol 2016;35:544)
- Surface epithelium:
- Can show significant difference in the composition between the right and left side (Int J Gynecol Pathol 1998;17:1)
Microscopic (histologic) images
Virtual slides
Positive stains
Negative stains
Videos
Corpus luteum
Corpus albicans
Board review style question #1
The image above represents a section of a well circumscribed, yellow, cystic nodule seen on gross examination of the ovary. The cells are positive for inhibin and calretinin. Which statement is correct?
- Its presence is permanent and does not depend on the phase of the menstrual cycle or the age of the patient
- Surgical removal of the ovary is indicated to prevent metastasis
- The image represents a physiologic constituent of the ovary
- The image represents a sex cord stromal tumor
Board review style answer #1
C. The image represents a mature corpus luteum, which is a physiologic structure present in the luteal phase of menstruation. The constituent cells are polygonal with abundant, pale, eosinophilic cytoplasm representing the luteinized granulosa cells. The round nucleus contains 1 or 2 large nucleoli. These cells usually stain similar to steroid hormone producing cells and are typically positive for inhibin and calretinin.
Comment Here
Reference: Ovary - Anatomy & histology
Comment Here
Reference: Ovary - Anatomy & histology
Board review style question #2
Which of the following microscopic findings in an ovary are indicators of a pathologic condition?
- Benign tubular structures located within the ovarian cortex; constituent cells are positive for mesothelial markers
- Benign polygonal cells with clear cytoplasm, round nucleus and positive staining for inhibin and calretinin
- Epithelial cell proliferation composed of papillary structures lined by cuboidal cells and exhibiting hierarchical branching and tufting of the lining cells
- Urothelial-like nests of cells known as Walthard nests
Board review style answer #2
C. The description is that of a serous neoplasm. Complex architecture including hierarchical branching and tufting of lining epithelial cells should not be seen in normal ovary or in the context of endosalpingiosis.
Comment Here
Reference: Ovary - Anatomy & histology
Comment Here
Reference: Ovary - Anatomy & histology