Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Kadam Maruthi V, Buza N. Mixed carcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/ovarymixedcarcinoma.html. Accessed December 25th, 2024.
Definition / general
- Mixed carcinoma of the ovary is a carcinoma comprising 2 or more different histological types, including high grade serous carcinoma (HGSC), endometrioid carcinoma (EC), clear cell carcinoma (CCC), mucinous carcinoma (MC) and low grade serous carcinoma (LGSC)
- Most common combination is mixed endometrioid and clear cell carcinoma
Essential features
- Presence of 2 or more histological types with the components showing distinct morphological differences
- Any percentage of a second histologic type is adequate to label the tumor as a mixed carcinoma according to the WHO classification of female genital tumors (5th edition)
- Immunophenotype of each component mirrors that of the corresponding pure carcinoma
- Majority of mixed carcinomas of the ovary show a common clonal origin (Am J Surg Pathol 2015;39:1548)
- Divergence of 2 histological types (especially mixed clear cell and endometrioid carcinoma) from a common precursor such as endometriosis is common
Terminology
- Mixed cell adenocarcinoma
ICD coding
- ICD-O
- ICD-11
- 2C73.Y & XH2AM6 - other specific malignant neoplasms of the ovary & mixed cell adenocarcinoma
Epidemiology
- Mixed ovarian carcinomas are rare, accounting for ~1% of all ovarian carcinomas (Am J Surg Pathol 2015;39:1548)
- Endometriosis related neoplasms develop in ~1% of patients with endometriosis
- Majority of endometriosis associated tumors are malignant, with endometrioid and clear cell carcinomas being the most common
Sites
- Ovary
Pathophysiology
- Different histological components in most mixed tumors are clonally related and share the same molecular alterations (Am J Surg Pathol 2015;39:1548)
- Endometriosis provides a milieu for neoplastic transformation; the clonal relationship between endometriosis and associated cancers is well established (Cancers (Basel) 2018;10:261)
- Endometrioid and clear cell ovarian cancer with endometriosis have common shared mutations in ARID1A, PIK3CA, CTNNB1, PTEN and KRAS
Etiology
- Endometriosis plays an important role in the development of ovarian mixed carcinoma with endometrioid and clear cell components
Clinical features
- Patients usually present with a pelvic mass or symptoms related to endometriosis or ascites
- Usually occurs in peri and postmenopausal women, although data are limited in the literature
Diagnosis
- In general, imaging studies and serum markers have relatively low specificity and sensitivity for ovarian malignancies
- Definitive diagnosis requires microscopic examination of biopsy or resection specimens
Laboratory
- Serum level measurements of CA125 may be helpful at the time of initial diagnostic work up and for surveillance of disease recurrence
- Rare association with paraneoplastic syndromes with clear cell carcinoma component
Radiology description
- Transvaginal ultrasound is the screening imaging modality of choice and may show a solid or a partially solid and cystic mass with intraluminal papillary projections with increased blood flow (Cancers (Basel) 2022;14:2885)
- Magnetic resonance imaging (MRI) may be used for further work up of inconclusive or indeterminate masses
Prognostic factors
- Prognosis is dependent on the histological components of the tumor and tumor stage
- In one study, there was no significant difference in the median survival between pure ovarian clear cell adenocarcinoma, high grade serous ovarian carcinoma and mixed ovarian carcinomas (clear cell plus serous, clear cell plus endometrioid or serous plus clear cell, plus endometrioid) (Arch Gynecol Obstet 2015;292:923)
- Another study reported no prognostic difference between pure clear cell ovarian carcinoma and mixed ovarian carcinoma with a clear cell component (Int J Gynecol Cancer 2014;24:1590)
- However, further subgroup analysis revealed that patients with mixed clear cell and endometrioid histology had a better prognosis compared to those with mixed clear cell and serous carcinoma
- Endometriosis associated carcinomas are often confined to ovary at presentation and generally have a favorable prognosis (Pathology 2018;50:190)
Case reports
- 48 year old woman with mixed mesonephric-like adenocarcinoma, clear cell carcinoma and endometrioid carcinoma arising from an endometriotic cyst (Int J Surg Pathol 2024;32:1140)
- 49 year old woman with a case of mixed endometrioid and clear cell carcinoma arising from port site endometriosis (J Obstet Gynaecol Res 2019;45:1613)
- 60 year old woman with mixed serous and clear cell adenocarcinoma of the ovary presented with symptomatic hypercalcemia (Perm J 2020;24:19.125)
Treatment
- Complete staging surgery and cytoreductive surgery followed by adjuvant chemotherapy as a standard approach
Gross description
- Macroscopic appearance depends on histological components of the tumor
- Generally, a solid or partially solid and cystic mass with heterogeneous cut surface, hemorrhage and necrosis may be grossly apparent
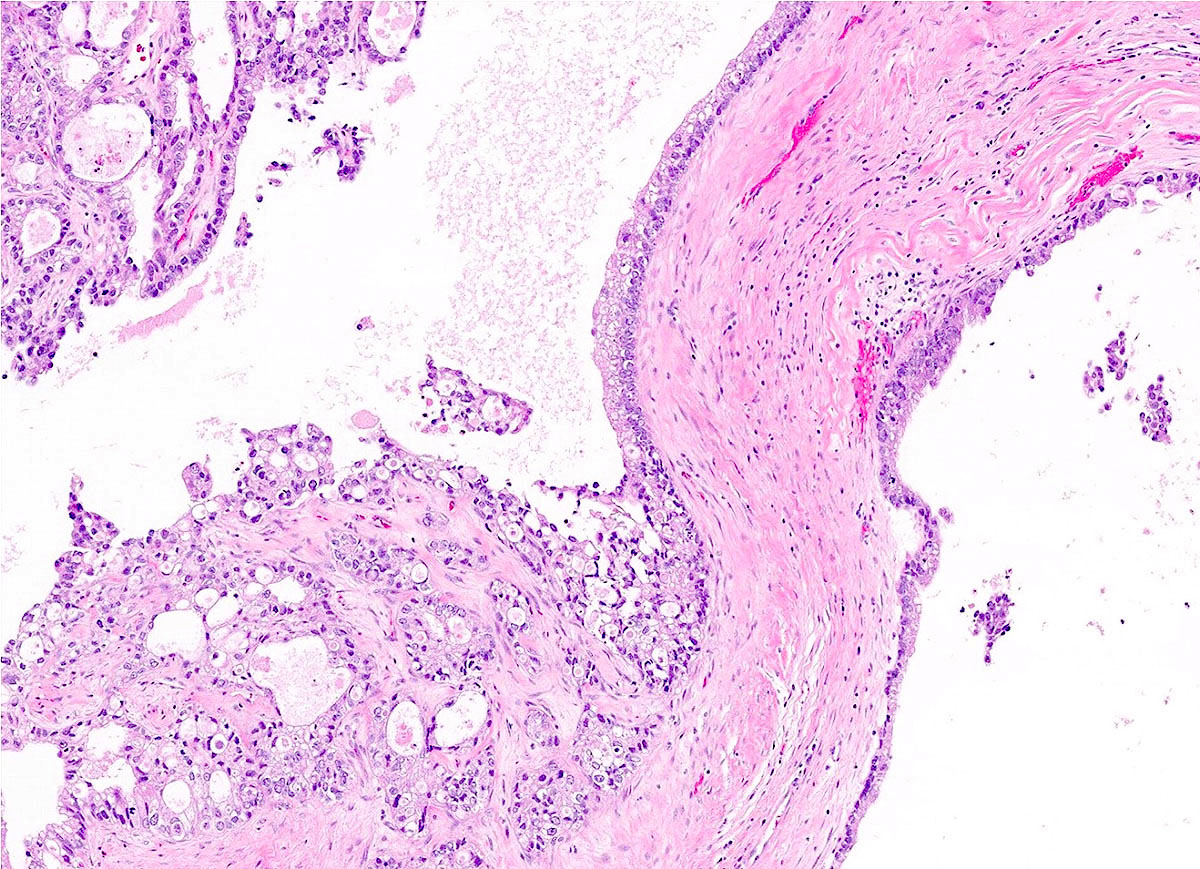
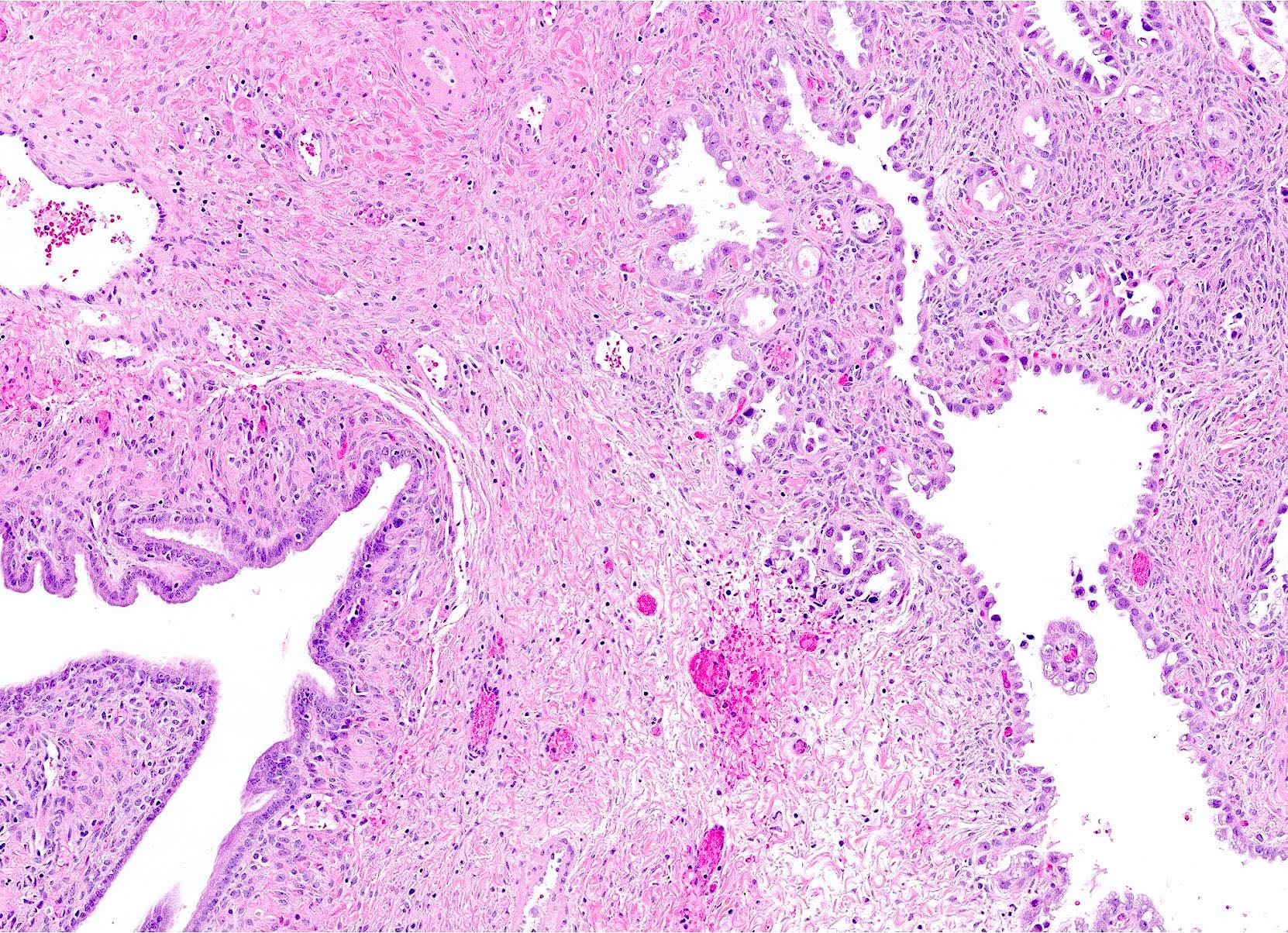
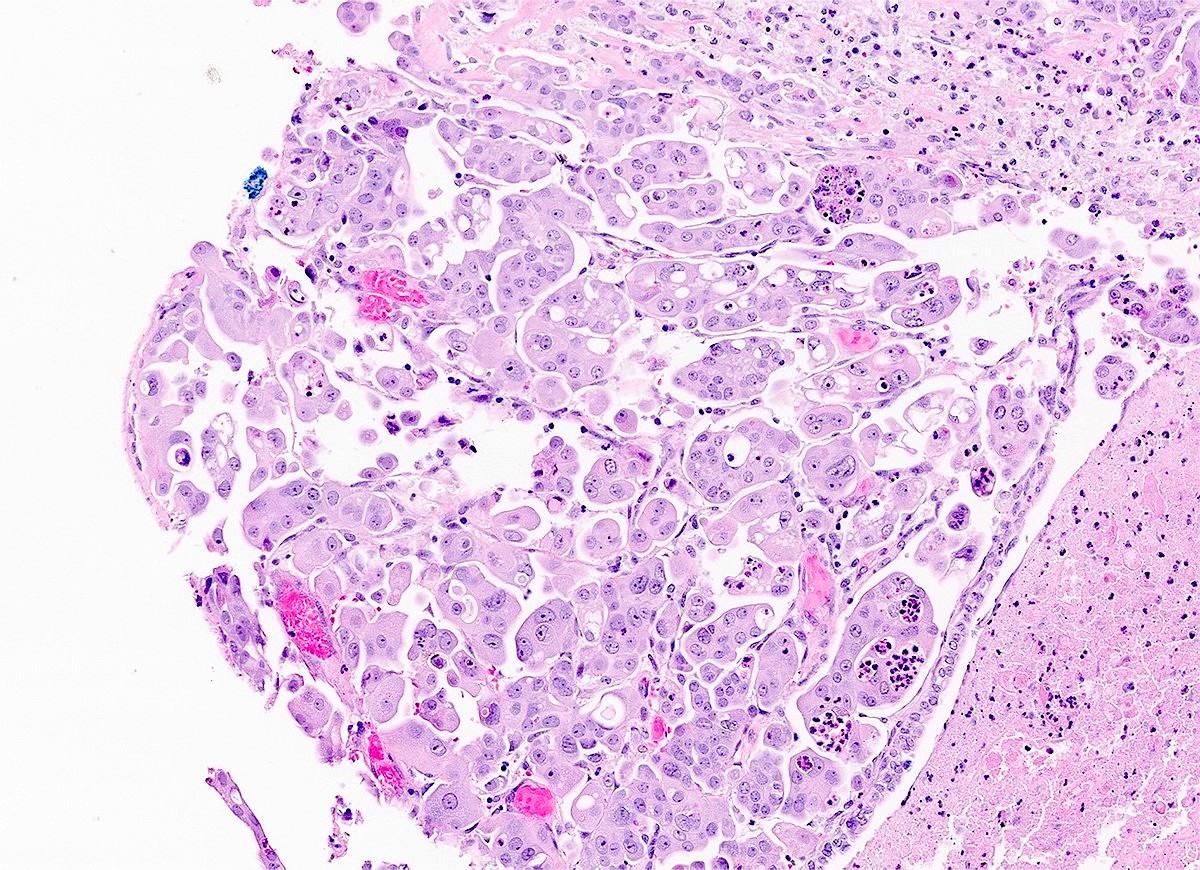
Microscopic (histologic) description
- At least 2 ovarian carcinoma histological types must be clearly recognizable on morphology (see detailed morphologic descriptions in the corresponding ovarian carcinoma topics)
- Most common combination is mixed endometrioid and clear cell carcinoma
- Any percentage of a second histologic type is sufficient to label the tumor as mixed
- Types present and their percentages should be included in the report
- Immunohistochemistry can be performed to support the presence of different histological components (Am J Surg Pathol 2015;39:1548)
Microscopic (histologic) images
Positive stains
- Immunophenotype of each component reflects that of the corresponding pure carcinoma
- Endometrioid carcinoma (EC) component: PAX8, ER, PR, p53 (wild type pattern)
- HNF-1B is also positive, although usually less intense than in the clear cell carcinoma component
- Clear cell carcinoma (CCC) component: PAX8, napsin A and HNF-1B
- Napsin A (positive in CCC component) and PR (positive in EC component) helps distinguish between the 2 tumor components (Int J Gynecol Pathol 2016;35:430)
Negative stains
Molecular / cytogenetics description
- Majority of the mixed carcinomas of the ovary show a common clonal origin (Am J Surg Pathol 2015;39:1548)
- Mixed ovarian carcinomas with EC and CCC components are often MMR deficient and a subset of cases are associated with Lynch syndrome (Am J Surg Pathol 2014;38:1173)
Sample pathology report
- Uterus, fallopian tubes and ovaries, total hysterectomy and bilateral salpingo-oophorectomy:
- Mixed carcinoma of the right ovary (clear cell carcinoma component 60% and endometrioid carcinoma component 40%) (see comment)
- Background ovarian tissue with endometriosis
- Right ovarian surface not involved by carcinoma
- Left ovary, bilateral fallopian tubes, cervix, endometrium, myometrium and serosa are not involved by carcinoma
- Comment: On immunohistochemistry, the clear cell carcinoma component is positive for PAX8, napsin A and HNF-1B and is negative for ER, PR and WT1. The endometrioid carcinoma component is positive for PAX8, ER and PR and is negative for napsin A and WT1. Both components show loss of MLH1 and PMS2 expression and retained MSH2 and MSH6 immunostaining.
Differential diagnosis
- Pure histologic types of ovarian carcinoma with ambiguous histomorphology and heterogenous morphology:
- Endometrioid carcinomas:
- Can focally display clear cell changes that mimic the solid or papillary patterns of clear cell carcinoma
- High grade serous carcinoma:
- May display a predominantly glandular morphology that mimics endometrioid carcinoma
- BRCA1 mutation associated high grade serous carcinomas have a strong association with a pseudoendometrioid morphology and may be misinterpreted as a mixed endometrioid and high grade serous carcinoma (Mod Pathol 2012;25:625)
- Endometrioid carcinoma with MMR deficiency or POLE exonuclease domain mutation:
- If there is identical MMR deficiency or POLE exonuclease mutation present in different tumor areas, the case should be diagnosed as an endometrioid carcinoma, rather than a mixed carcinoma
- Endometrioid carcinomas:
- Endometrioid carcinoma with extensive mucinous differentiation:
Additional references
Board review style question #1
Board review style answer #1
A. Endometriosis. Divergence of 2 histological types (especially mixed clear cell and endometrioid carcinoma) from a common precursor such as endometriosis is common.
Answer C is incorrect because serous borderline tumor may be associated with low grade serous carcinoma but it is not a precursor lesion of mixed ovarian carcinoma.
Answers B and D are incorrect because mucinous cystadenoma and serous cystadenoma are not precursor lesions of mixed ovarian carcinoma.
Comment Here
Reference: Mixed carcinoma
Comment Here
Reference: Mixed carcinoma
Board review style question #2
Which one of the following statements is true for mixed ovarian carcinomas?
- The most common histologic components are clear cell carcinoma and endometrioid carcinoma
- The most common histologic components are high grade serous carcinoma and endometrioid carcinoma
- They are often associated with germline BRCA1 / 2 mutations
- They are very common, comprising ~30% of all ovarian carcinomas
Board review style answer #2
A. The most common histologic components are clear cell carcinoma and endometrioid carcinoma. Divergence of 2 histological types (especially mixed clear cell and endometrioid carcinoma) from a common precursor such as endometriosis is common.
Answer D is incorrect because mixed ovarian carcinomas are very rare (< 1% of all ovarian carcinomas) (Am J Surg Pathol 2015;39:1548).
Answer B is incorrect because the most common histologic components are clear cell and endometrioid carcinoma.
Answer C is incorrect because mixed ovarian carcinomas are only very rarely associated with BRCA1 / 2 mutations, since those are typically found in high grade serous carcinomas.
Comment Here
Reference: Mixed carcinoma
Comment Here
Reference: Mixed carcinoma