Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Gross description | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1Cite this page: Ma L. Clear cell borderline tumor. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/ovaryclearcellborderlinetumor.html. Accessed January 21st, 2025.
Definition / general
- Adenofibromatous tumor with clear cells demonstrating low grade cytologic atypia and some degree of glandular crowding but without stromal invasion
Essential features
- Abundant adenofibromatous stroma with small glands / cysts with low grade nuclear atypia but without stromal invasion
- No solid, papillary or cribriform growth
- Pure clear cell borderline tumors are rare; more frequently associated with clear cell carcinoma
- If pure clear cell adenofibroma or borderline tumor is present, additional sampling is recommended to exclude clear cell carcinoma
Terminology
- No longer recommended historical terms:
- Atypical proliferative clear cell tumor
- Clear cell tumor of low malignant potential
ICD coding
- ICD-10: D39.10 - neoplasm of uncertain behavior of unspecified ovary
Epidemiology
- Pure clear cell borderline tumors are very rare
- < 1% of all ovarian borderline tumors
- ~21% of ovarian clear cell carcinomas contain a clear cell adenofibromatous component (Am J Surg Pathol 2007;31:999)
- Most patients are postmenopausal (age range of 36 - 82 years old) (Ann Surg Oncol 2022;29:1165)
Sites
- Ovary, almost all unilateral
Pathophysiology
- May be a component of the adenofibromatous pathway of the pathogenesis of ovarian clear cell carcinoma (see Diagrams / tables) (J Cancer 2011;2:94)
- Also see Molecular / cytogenetics description
Etiology
- Associated with endometriosis (~15%) (J Cancer 2011;2:94)
Diagrams / tables
Clinical features
- Incidental imaging finding
- Abdominal / pelvic pain
Diagnosis
- Surgical excision
- Definite diagnosis requires extensive sampling
Prognostic factors
- Good prognosis
- No clinical evidence of aggressive behavior (Cancer 1984;53:1156, J Cancer 2011;2:94)
- Rare recurrences have been reported (Int J Gynaecol Obstet 1996;54:37)
Case reports
- 50 year old woman with 6.5 cm cystic mass in right ovary (Int J Surg Pathol 2018;26:578)
- 53 year old postmenopausal woman with a 12 cm solid ovarian mass (Oman Med J 2012;27:e031)
- 53 year old woman with benign, borderline and clear cell carcinoma of the ovary arising in endometriosis (J Pathol Transl Med 2016;50:155)
- 58 year old woman with 8 cm solid ovarian mass (Case Rep Pathol 2017;2017:3860107)
Treatment
- Surgical resection
- Tumors are typically stage I (Int J Gynecol Cancer 2012;22:993)
Gross description
- Predominantly solid, white-tan mass
- May have small or large cysts, imparting a honeycomb cut surface
Frozen section description
- Small glands or cysts in background of fibromatous stroma
- Lining epithelium comprising 1 - 2 layers of cuboidal, flat or hobnail cells
- Absence of the admixture of growth patterns characteristic of clear cell carcinoma (tubulocystic, papillary and solid)
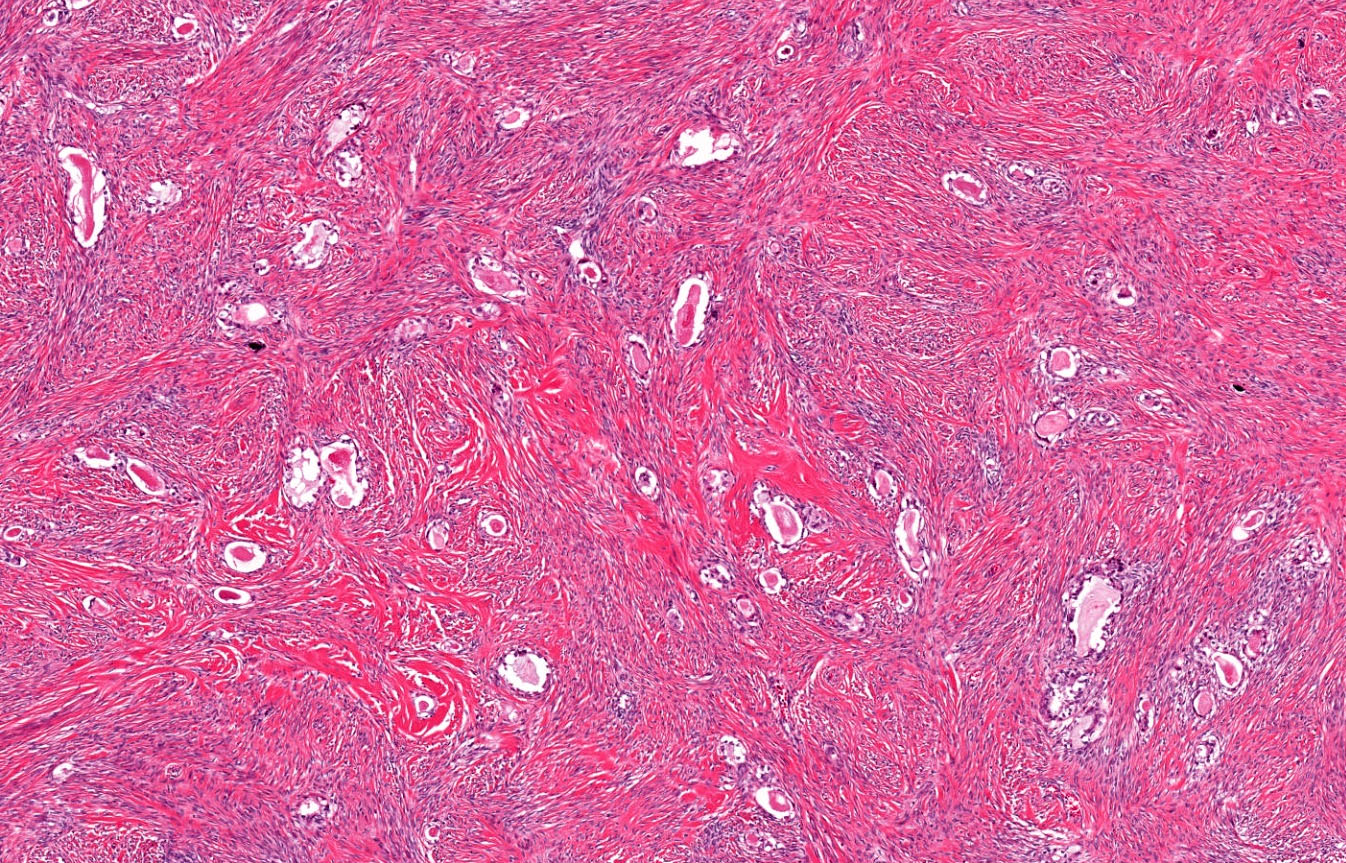
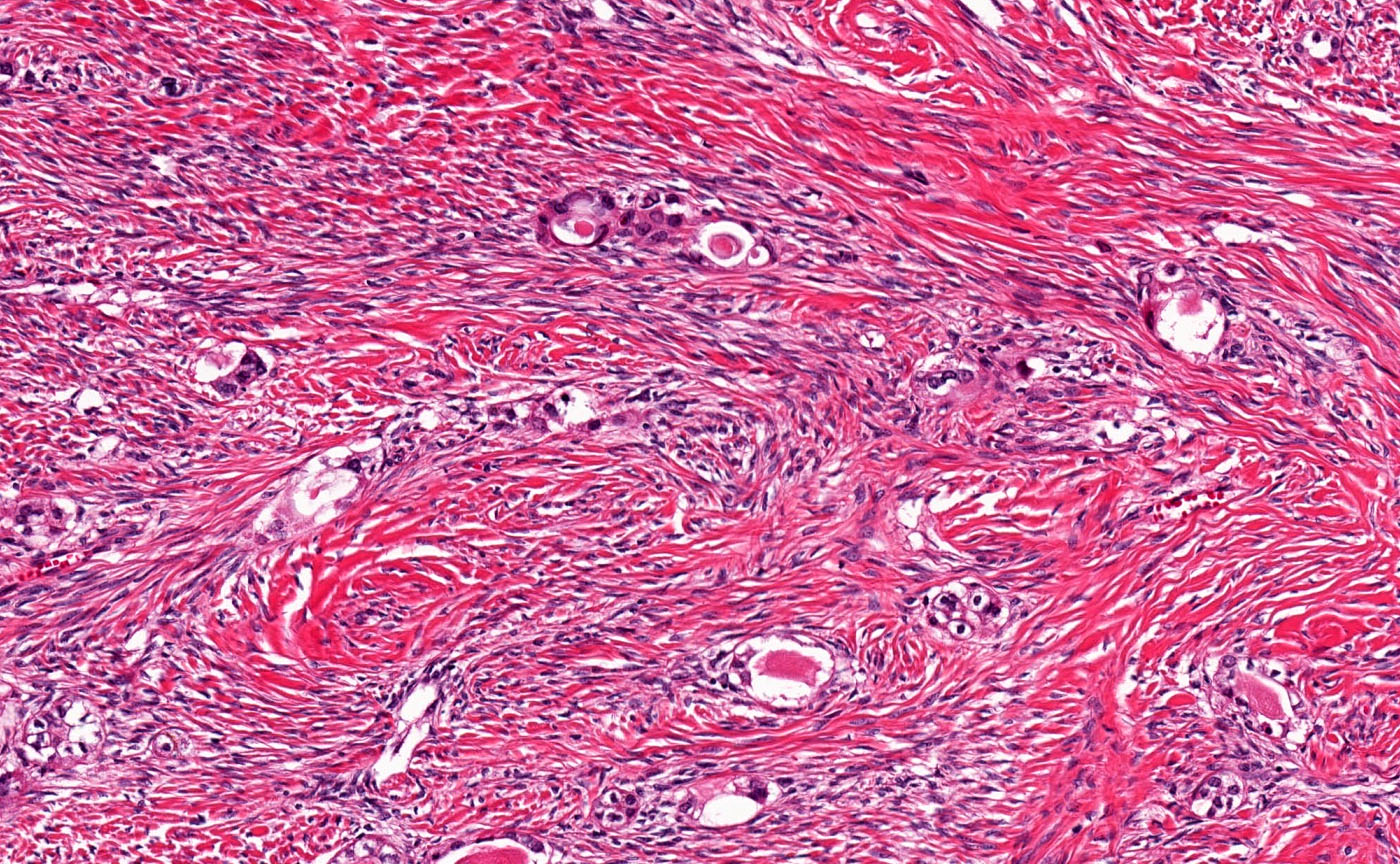
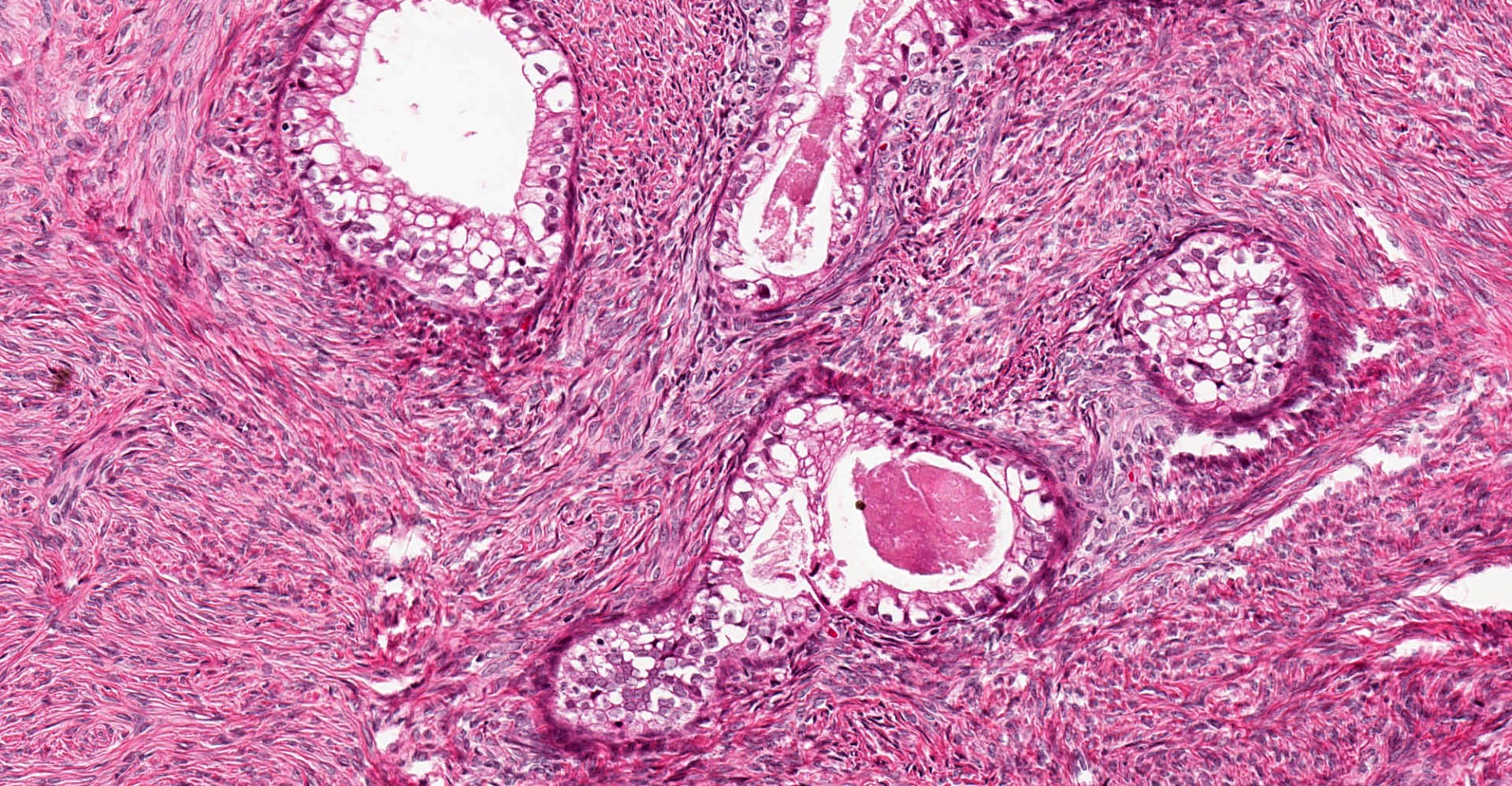
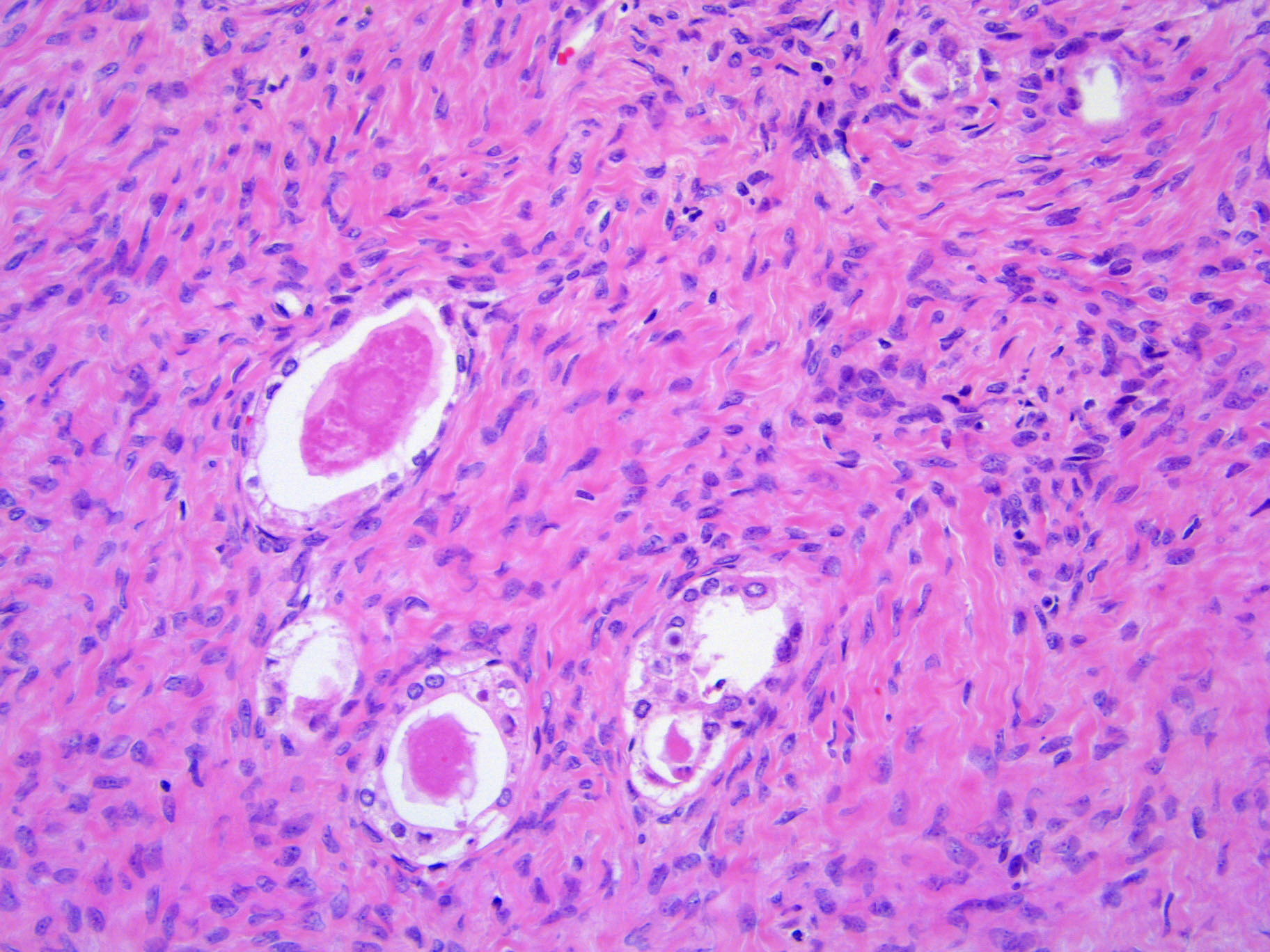
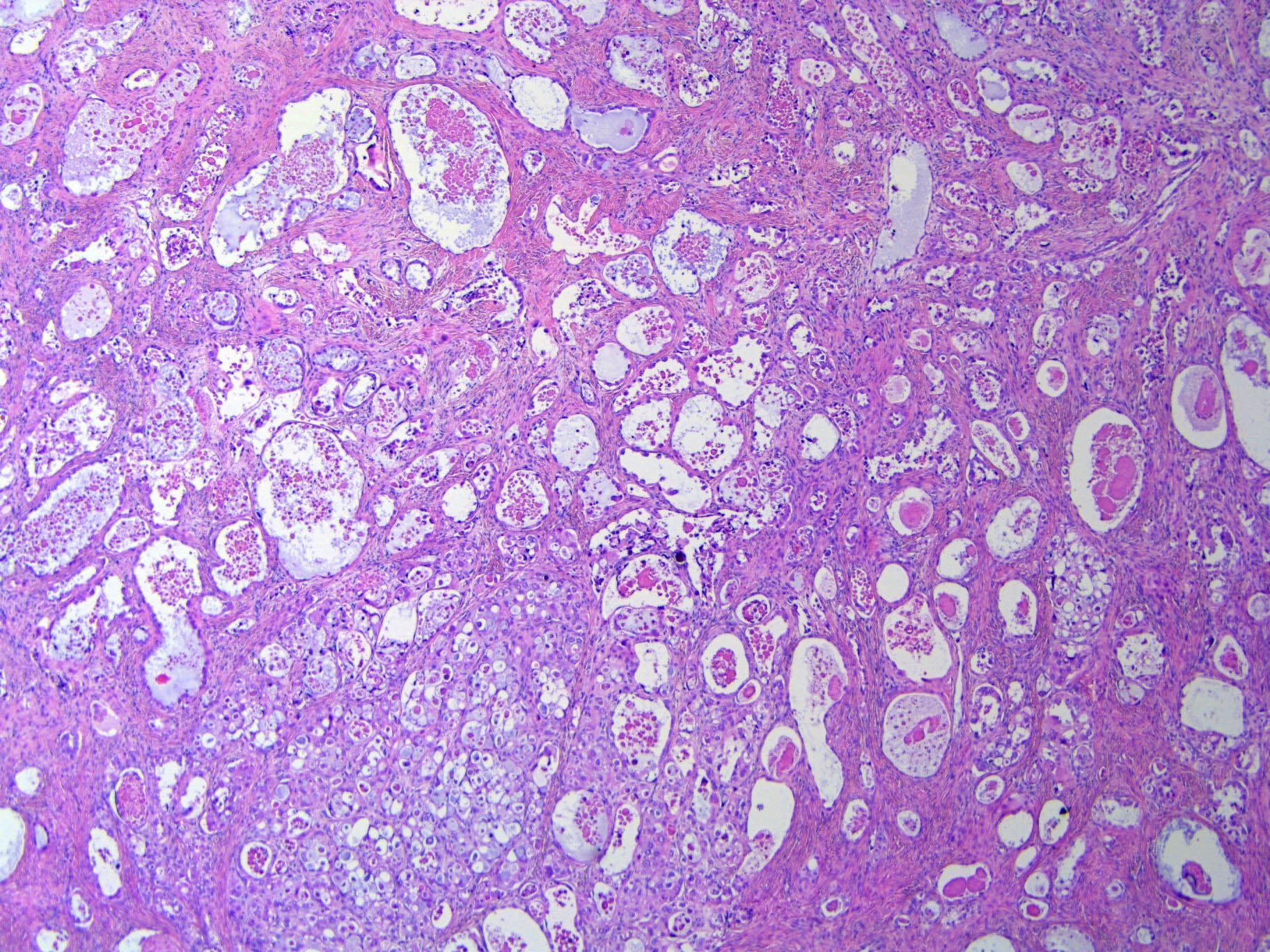
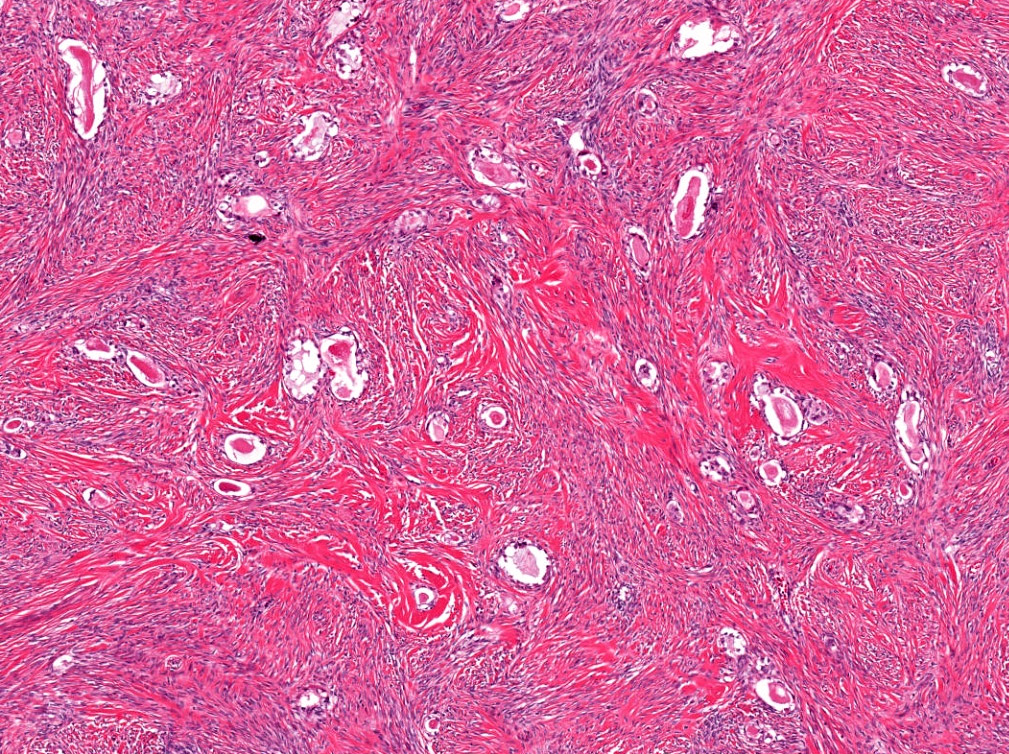
Microscopic (histologic) description
- Abundant fibromatous stroma
- Small glands or cysts lined by 1 - 2 layers of cuboidal, flat or hobnail cells with clear cytoplasm and low grade nuclear atypia (Cancer 1985;56:2922)
- Atypia: nuclear enlargement, hyperchromasia, small nucleoli
- Presence of atypia may be subjective
- No stromal invasion; lacks architectural complexity
- No confluent, solid, papillary and cribriform architecture
- May show intraluminal eosinophilic secretions
- May show simple cystic outpouchings
- Typically a component of clear cell carcinoma
- Initial sections that demonstrate exclusive clear cell borderline tumor or pure adenofibromatous component warrant additional sampling to exclude clear cell carcinoma
Microscopic (histologic) images
Positive stains
Molecular / cytogenetics description
- Loss of ARID1A is seen in both clear cell carcinoma and its adjacent adenofibromatous component (Mod Pathol 2012;25:615)
- Loss of heterozygosity (LOH) of 5q, 10q and 22q is seen in benign, borderline and malignant clear cell tumors (J Pathol 2008;216:103)
- However, LOH of 1p and 13q is only seen in clear cell carcinoma, suggesting association with malignant transformation
Sample pathology report
- Right ovary and fallopian tube, salpingo-oophorectomy:
- Clear cell borderline tumor, 6 cm
Differential diagnosis
- Clear cell adenofibroma:
- Extremely rare
- No cytologic atypia (Cancer 1984;53:1156)
- No glandular crowding
- Clear cell carcinoma:
- Variety of architectural patterns
- Tubulocystic, papillary, solid
- More often cystic with mural nodule
- Presence of hyalinized stroma
- Variety of architectural patterns
- Endometrioid adenofibroma:
- Clear cell struma ovarii:
- May be associated with a component of mature cystic teratoma
- Areas of classic thyroid tissue typically present, including macrofollicles filled with colloid
- TTF1, thyroglobulin positive
- Napsin A, HNF1β negative
- Yolk sac tumor, polyvesicular vitelline pattern:
- Younger patients; elevated serum AFP levels
- May have prominent cystic component (Am J Surg Pathol 2013;37:393)
- May be associated with other yolk sac tumor patterns
- SALL4, AFP, glypican 3 positive
- Napsin A, PAX8, CK7, EMA negative
Additional references
Board review style question #1
A 52 year old patient undergoes a left salpingo-oophorectomy for a 6 cm ovarian mass. The mass is well sampled and a representative section is shown. Immunohistochemical stains demonstrate that the tumor is positive for PAX8, CK7 and Napsin A, while it is negative for ER, PR, TTF1 and AFP. What is the best diagnosis?
- Clear cell borderline tumor
- Endometrioid adenofibroma
- Struma ovarii
- Yolk sac tumor
Board review style answer #1
A. Clear cell borderline tumor. The image shows an adenofibromatous neoplasm with an immunoprofile consistent with clear cell borderline tumor. Endometrioid adenofibromas are typically ER and PR positive. Yolk sac tumors are typically AFP positive and mostly negative for PAX8 and CK7. While struma ovarii is positive for PAX8 and CK7, it is also positive for TTF1 and negative for Napsin A.
Comment Here
Reference: Clear cell borderline tumor
Comment Here
Reference: Clear cell borderline tumor