Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Smith MH. Proliferative verrucous leukoplakia (PVL). PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/oralcavityverrucoushyperplasia.html. Accessed April 2nd, 2025.
Definition / general
- An oral potentially malignant disorder that shows slow growing, persistent and often multifocal proliferations of white, verruciform lesions of the oral cavity, particularly the gingiva
Essential features
- Diagnosis requires clinical - pathologic correlation
- Shows high rates (~50%) of recurrence and progression to squamous cell carcinoma (Head Neck Pathol 2021;15:572, Cancers (Basel) 2021;13:4085)
- Older women are most affected
Terminology
- Leukoplakia: white patch of the mucous membrane that is not clinically diagnostic
- Verrucous hyperplasia: a term used by Shear and Pindborg in 1980 for lesions having a histopathologic pattern similar to the bulky hyperkeratotic epithelial proliferation seen in proliferative verrucous leukoplakia and appearing histopathologically and clinically similar to verrucous carcinoma (Cancer 1980;46:1855)
ICD coding
- ICD-10: K13.21 - leukoplakia of oral mucosa
Epidemiology
- Middle aged to older women are most affected (Cancers (Basel) 2021;13:4085)
Sites
- Any oral site
- Gingiva / alveolar ridge mucosa is the most common site for hyperkeratotic PVL lesions and for malignant transformation of PVL lesions (Cancers (Basel) 2021;13:4085)
Pathophysiology
- Little is known about the molecular pathways and biologic factors associated with PVL (Head Neck Pathol 2021;15:572)
Etiology
- Etiology is unknown
- Tobacco and alcohol do not appear to be significant etiologic factors, as seen in other oral precursor lesions (Cancers (Basel) 2021;13:4085)
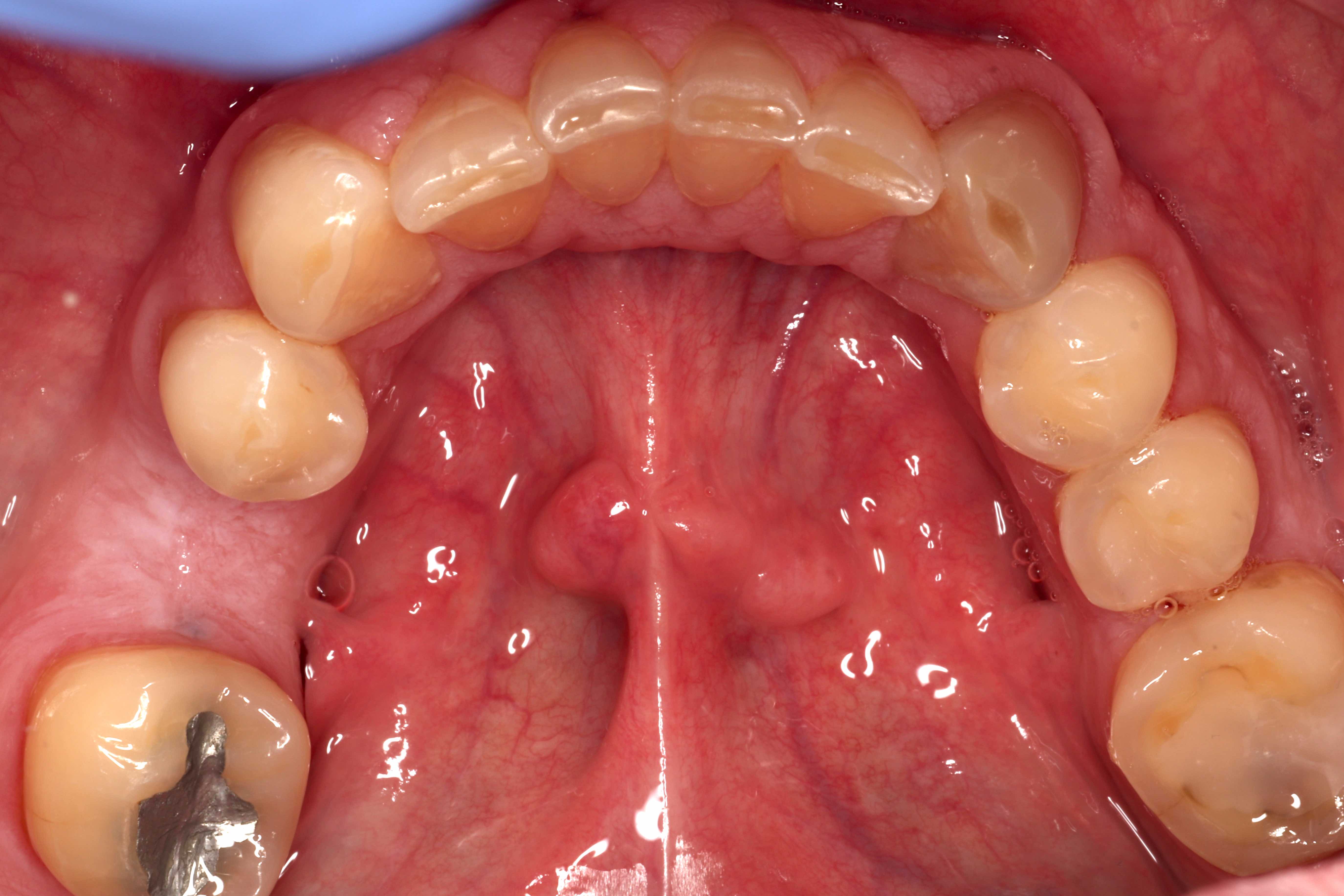
Clinical features
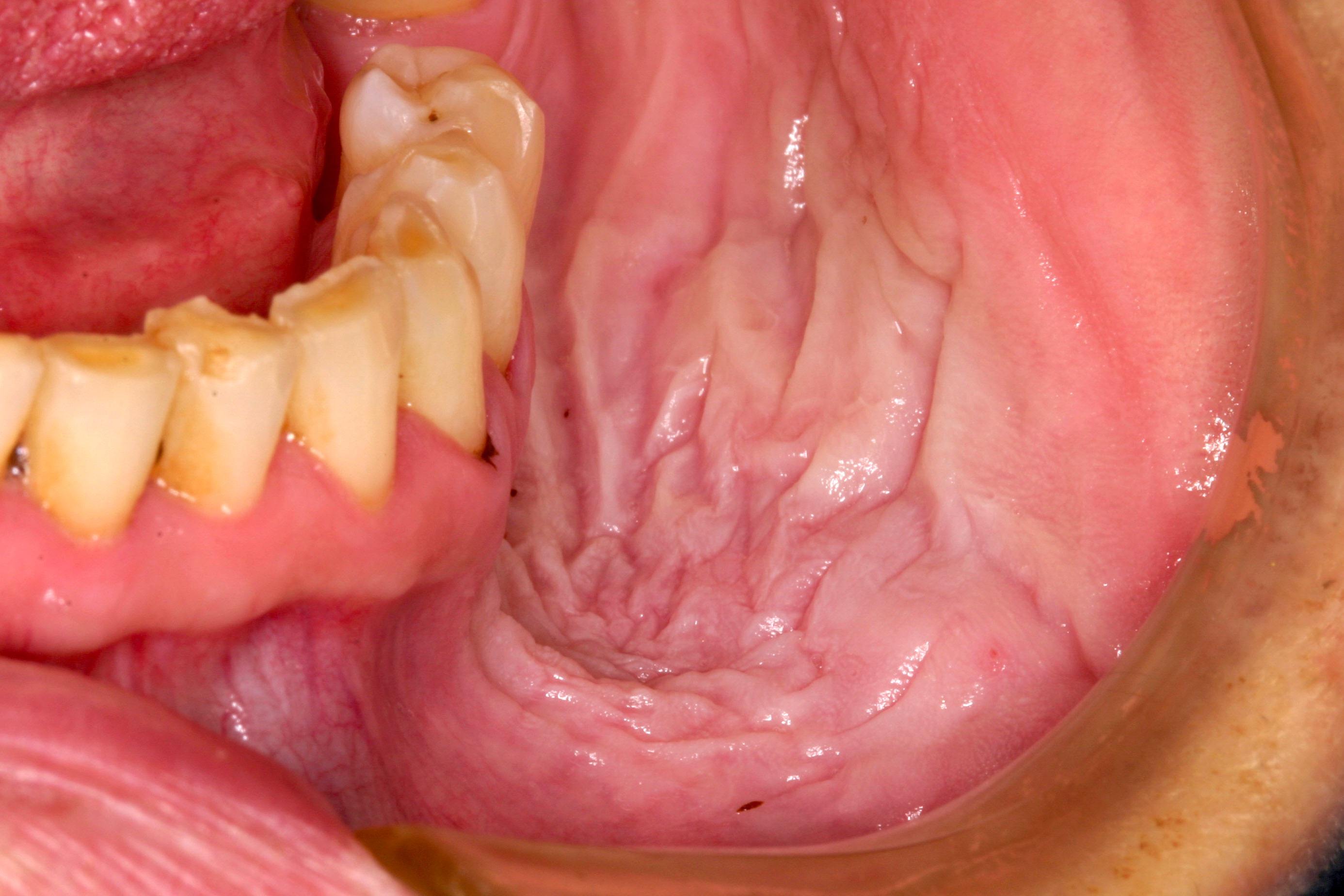
- Clinical criteria proposed by Villa et al. in 2018 (Oral Dis 2018;24:749):
- White, hyperkeratotic lesions that are smooth, fissured, verrucous or erythematous with or without ulcers
- Multifocal, noncontinuous lesions or a single, large lesion > 4 cm involving 1 site or a single, large lesion > 3 cm involving continuous sites
- Lesions that progress, expand in size or develop multifocality over time
- White / keratotic lesions of the gingiva that often demonstrate a ring around the collar appearance, where the lesion appears to follow the marginal gingiva around the tooth (Head Neck Pathol 2021;15:572)
Diagnosis
- Diagnosis is made upon clinical examination; however, biopsy is required to determine transformation of hyperkeratotic lesions into cytologic dysplasia or carcinoma
- Biopsy from uninflamed and nonulcerated sites is recommended (Head Neck Pathol 2021;15:572)
Prognostic factors
- Women have a 3 times higher risk of developing oral squamous cell carcinoma in PVL compared to men with PVL (Cancers (Basel) 2021;13:4085)
Case reports
- 38 year old man with carcinomatous transformation in a setting of PVL (J Indian Soc Periodontol 2017;21:499)
- 60 year old man presented with multifocal white patches (Contemp Clin Dent 2013;4:258)
- 84 year old woman treated with high dose rate brachytherapy (Cureus 2021;13:e15696)
Treatment
- There is no current treatment for PVL; however, management includes the following:
- Close clinical follow up (every 3 - 6 months) (Oral Dis 2018;24:749)
- Lesions should be photographed at each clinical visit and photographs should be submitted to the pathologist along with any biopsy specimens (Oral Dis 2018;24:749)
- Biopsies are taken periodically, particularly when lesions have changed character (e.g., increased significantly in size, become nodular, exophytic, indurated or more verrucoid) or when destruction of adjacent structures or tooth mobility is noticed
- Early detection and patient education is critical to management
- Early success with laser assisted photodynamic therapy has been reported (Photodiagnosis Photodyn Ther 2022;39:103002)
- Although no standard of care exists for treatment, cases of PVL with cytologic dysplasia or those diagnosed as bulky hyperkeratotic epithelial proliferation (with or without suspicion for invasion) are generally excised with conservative, assured margins when clinically feasible
Clinical images
Contributed by Molly Housley Smith, D.M.D., Michael Piepgrass, D.M.D.,
John McGehee, D.M.D., Michael Menis, D.D.S. and Trent Clifton, D.M.D., M.D.
Gross description
- White lesions demonstrate well demarcated borders, contrasting with adjacent tan, unaffected mucosa
- Pebbled, papillary, verrucoid or sometimes smooth surface texture
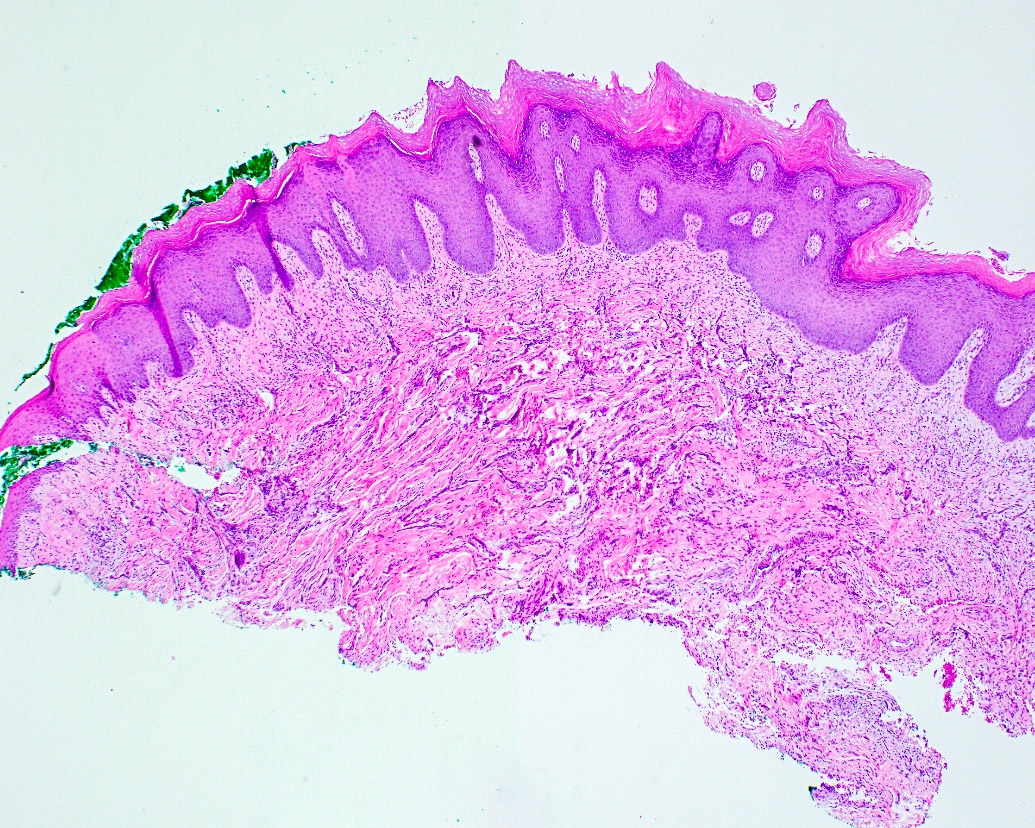
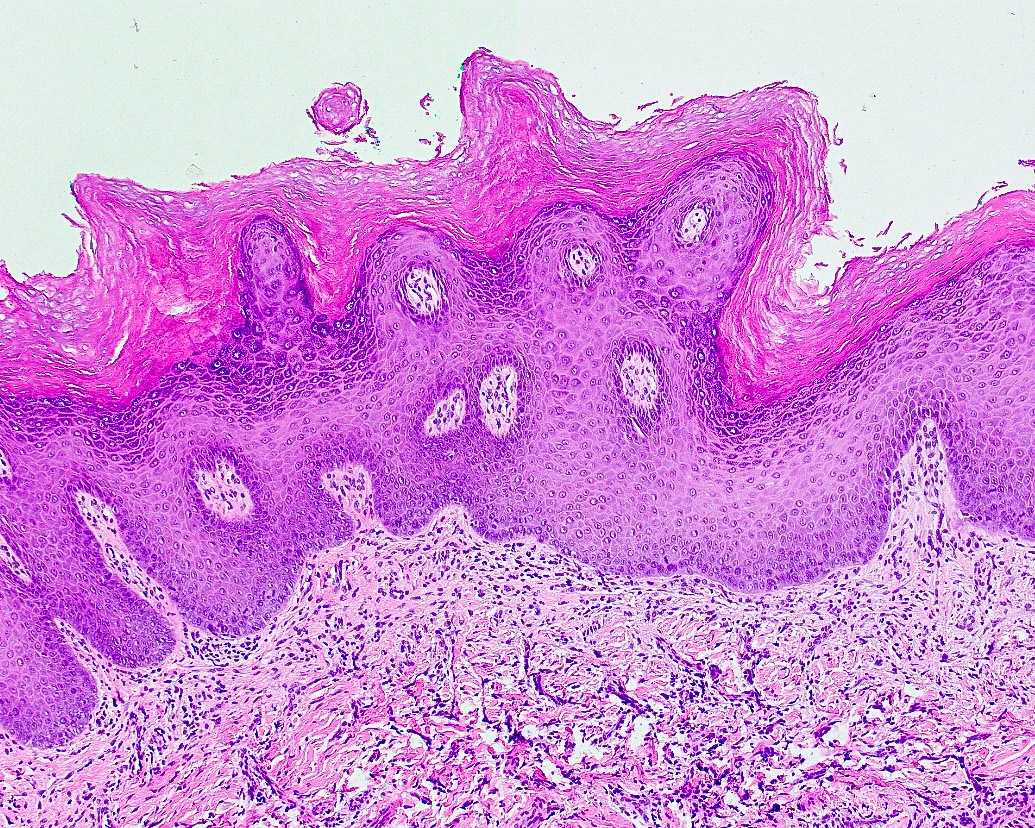
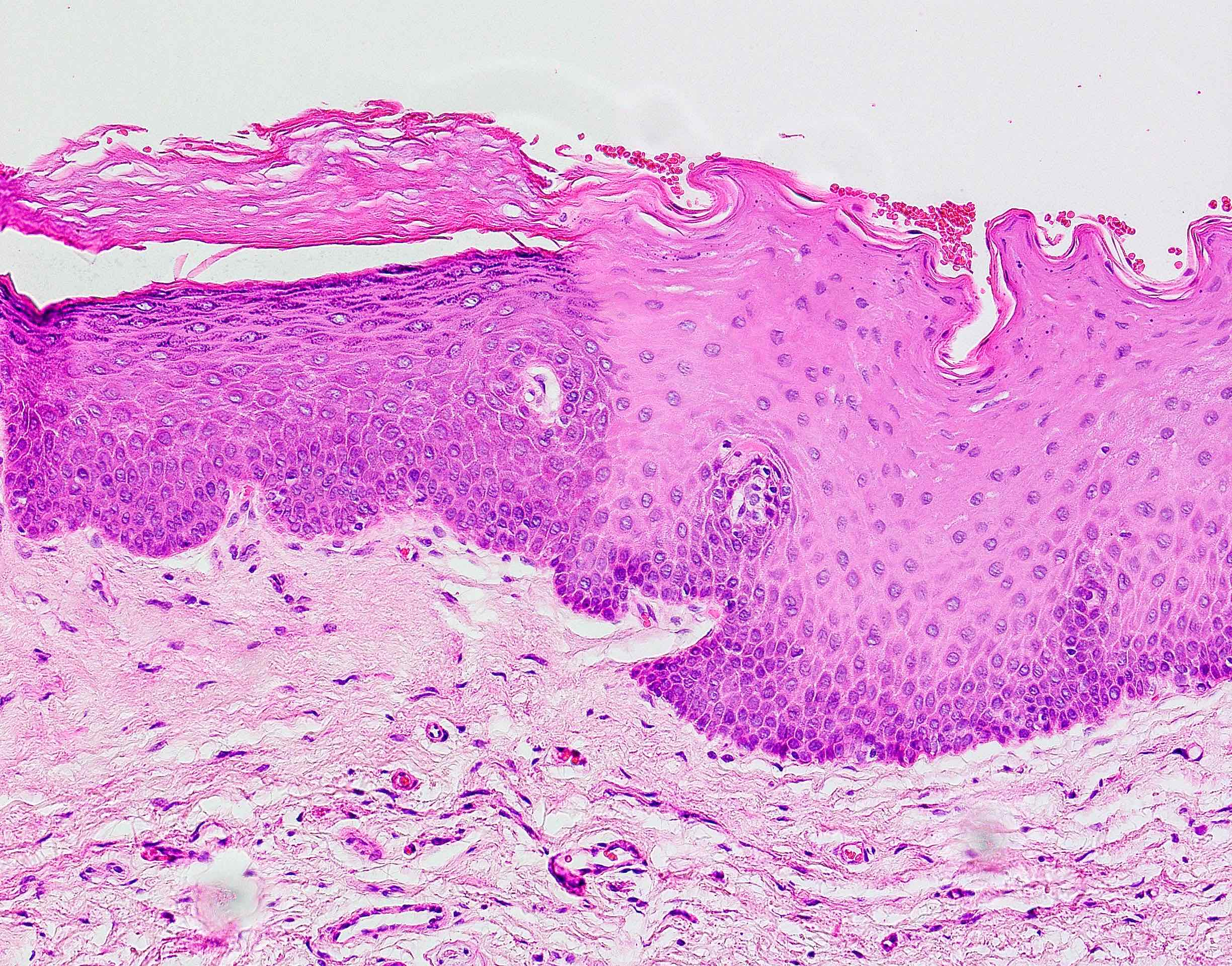
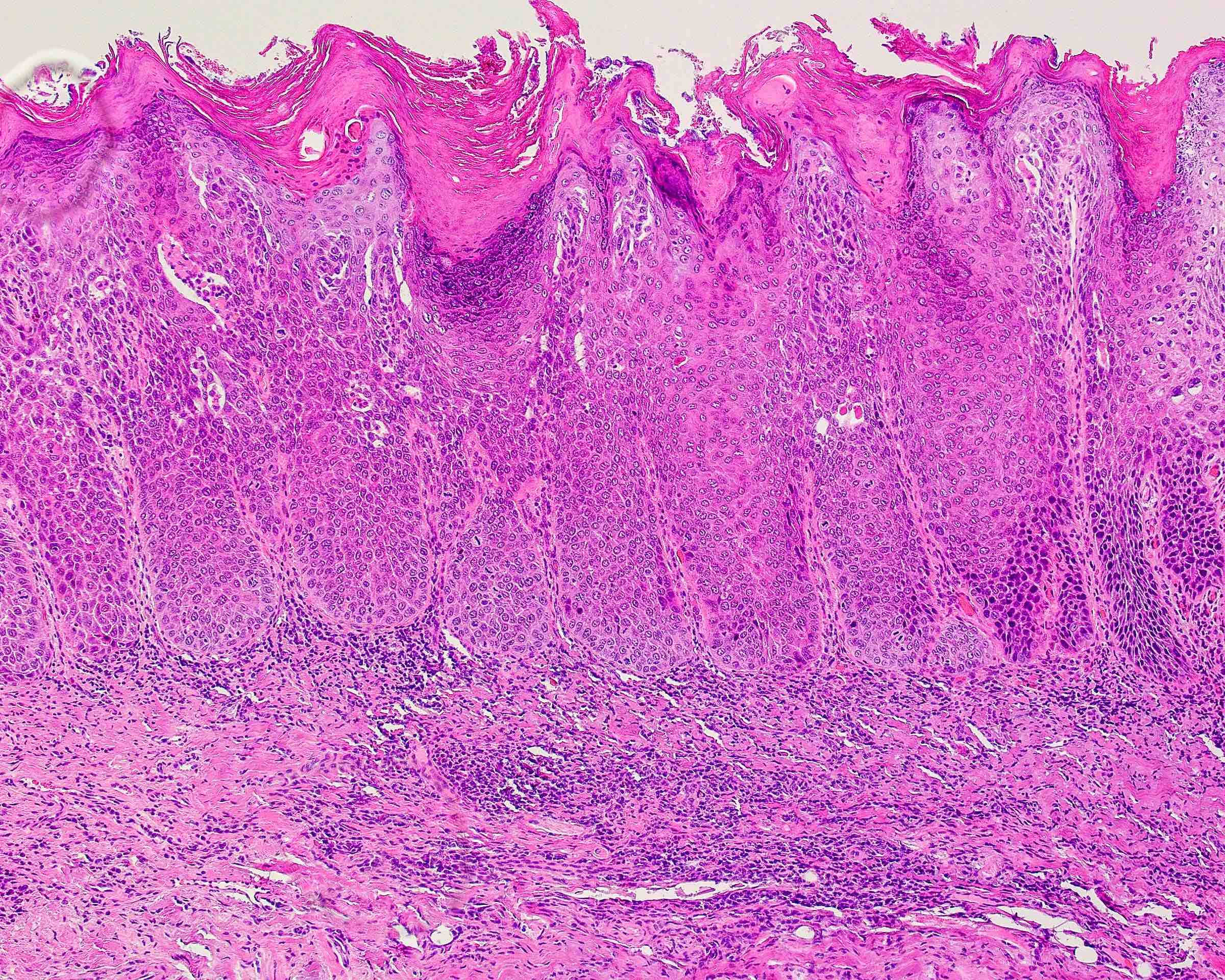
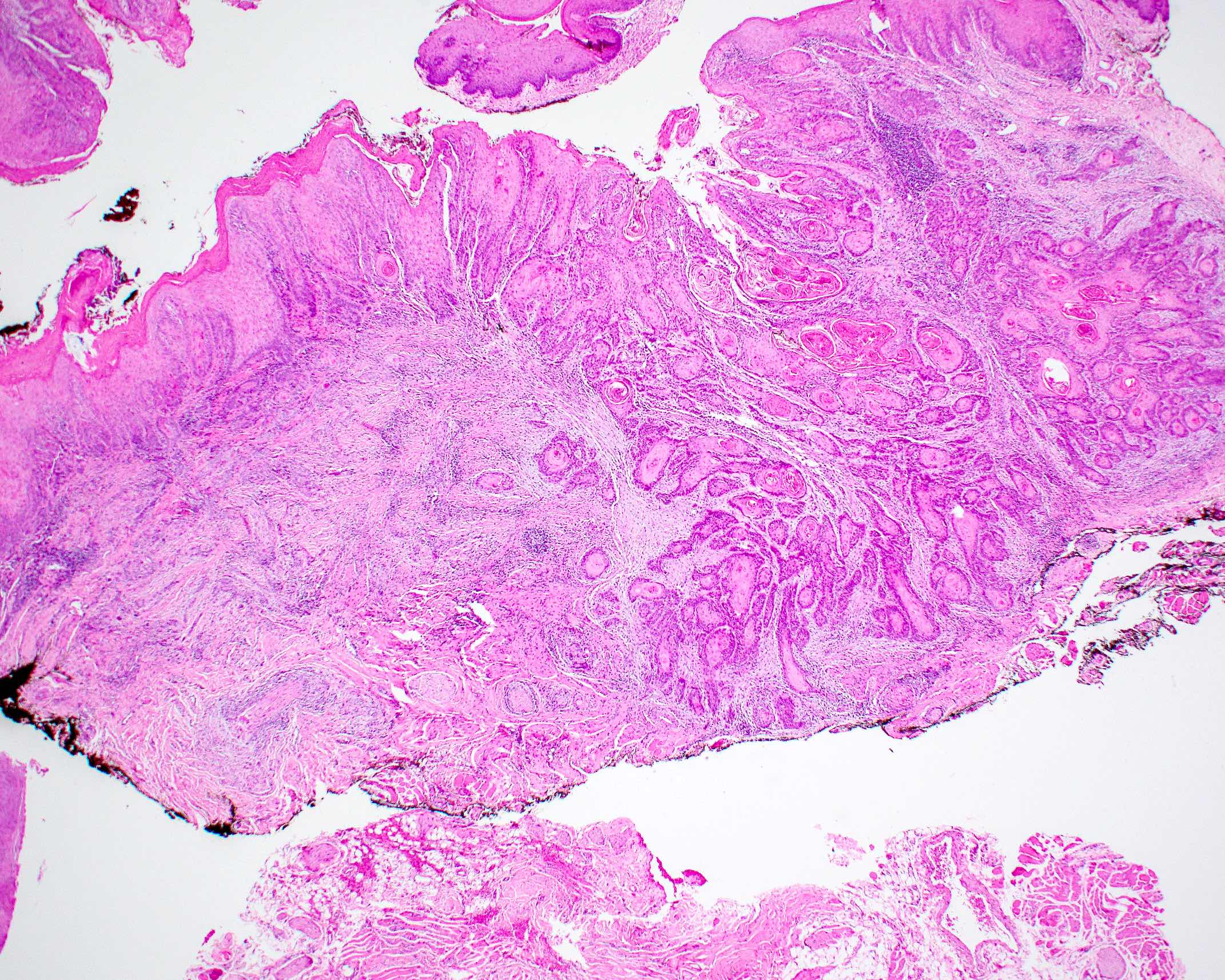
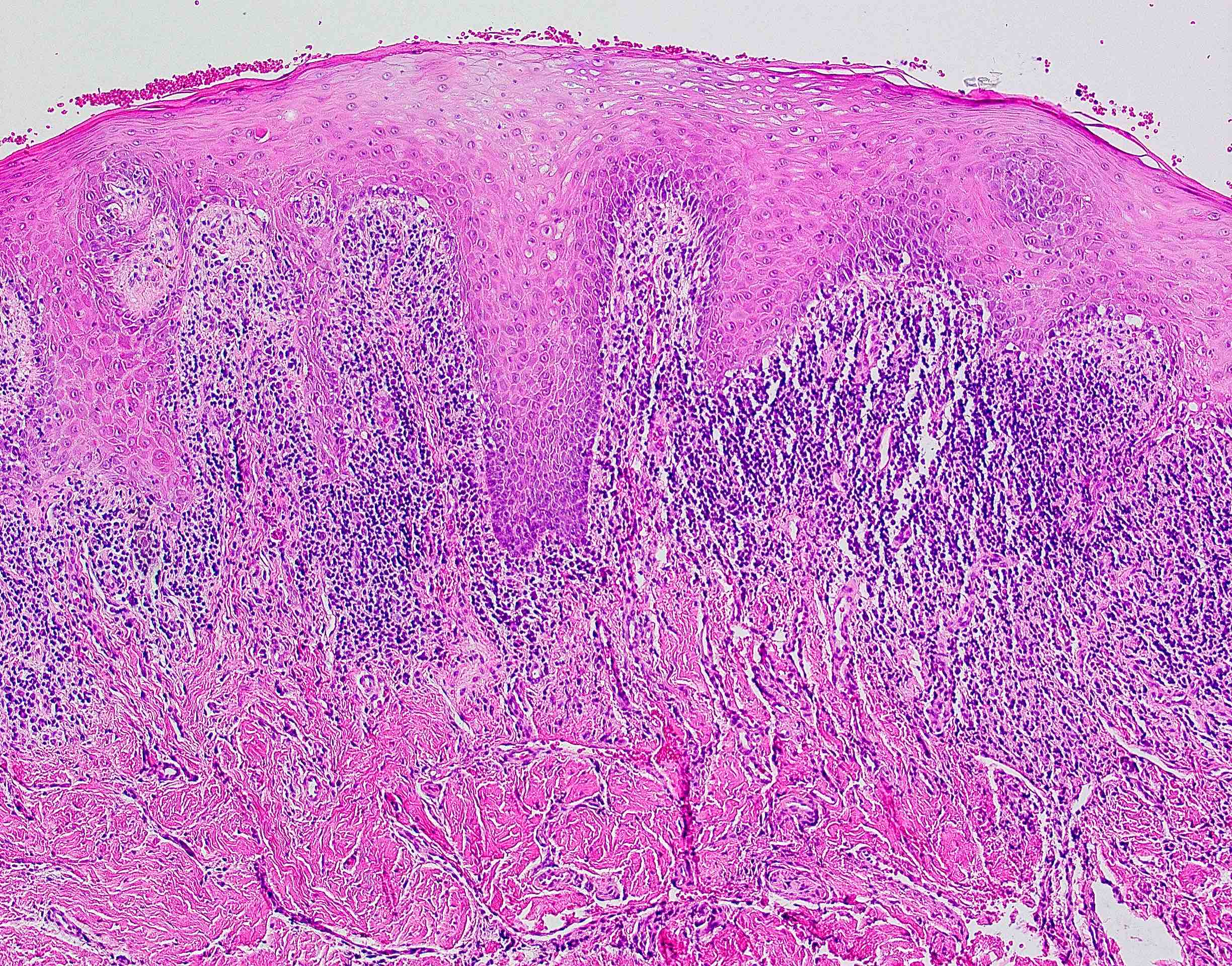
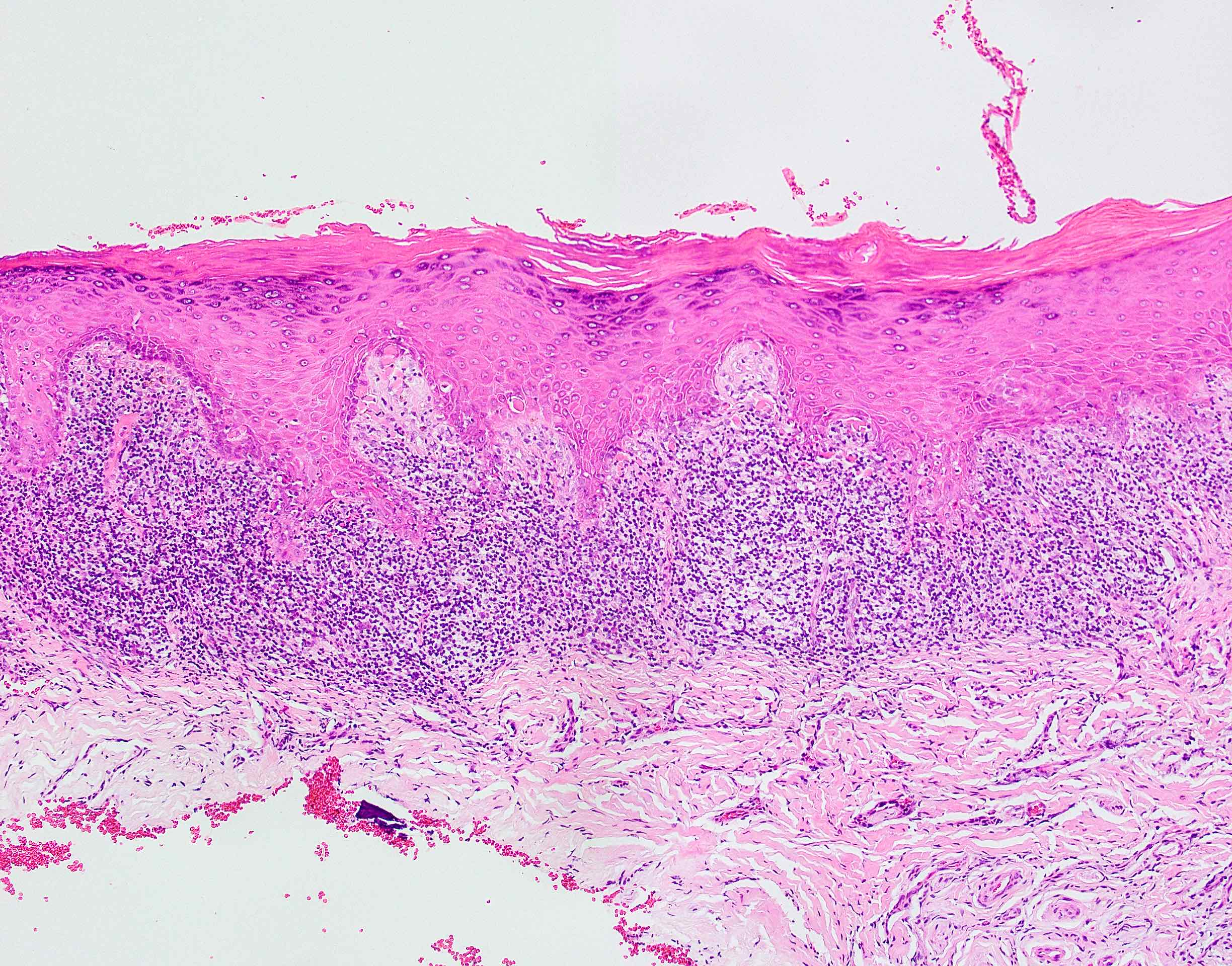
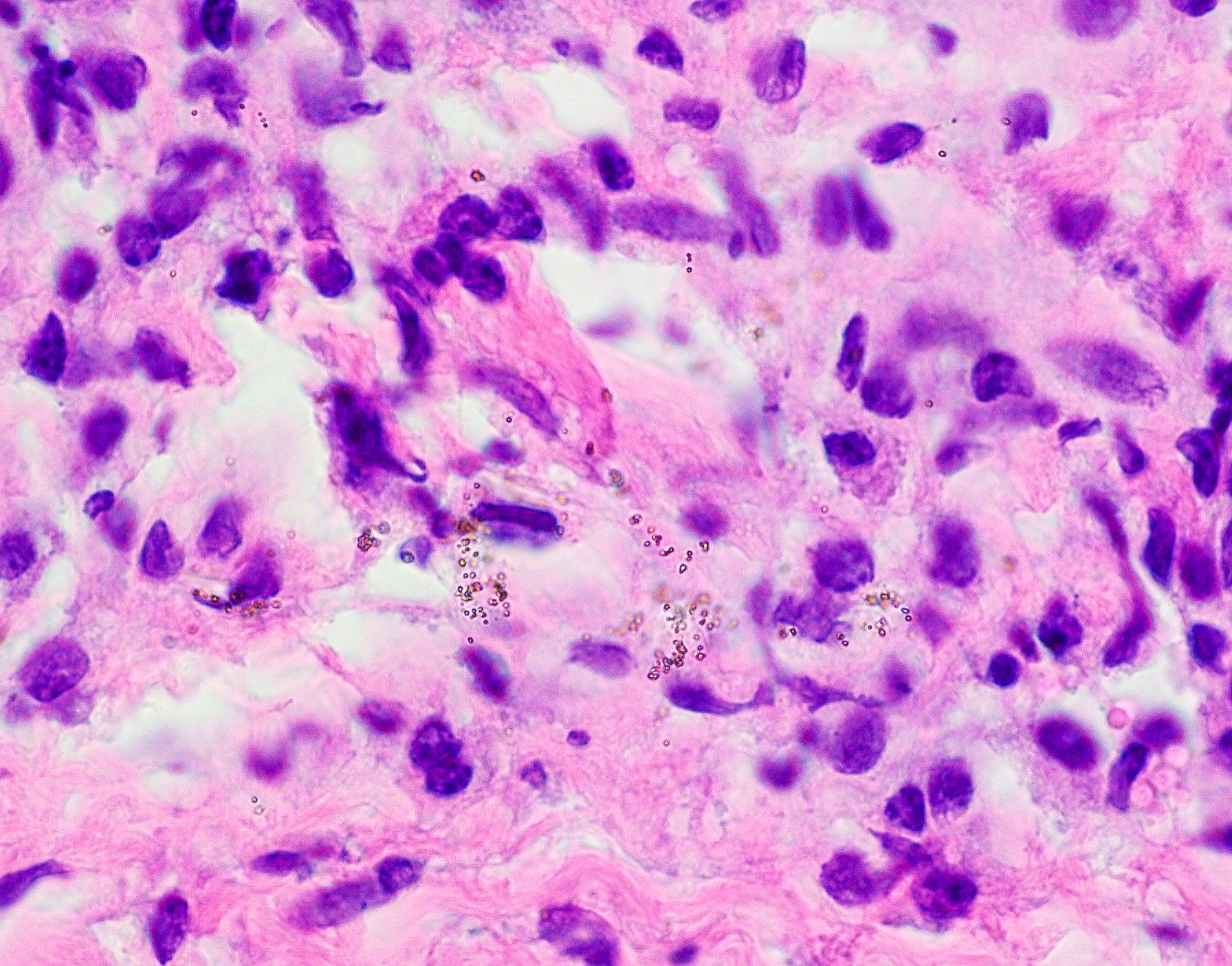
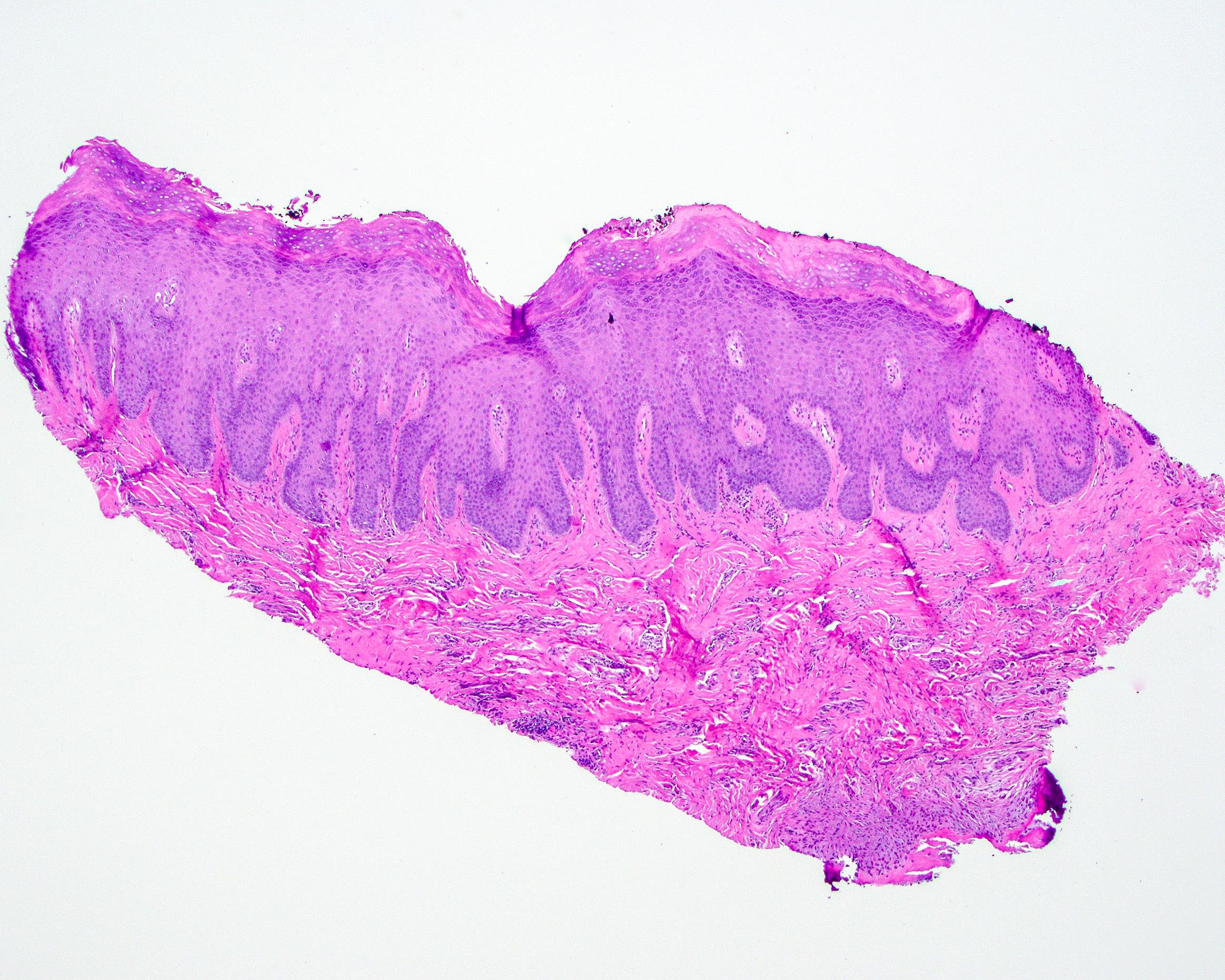
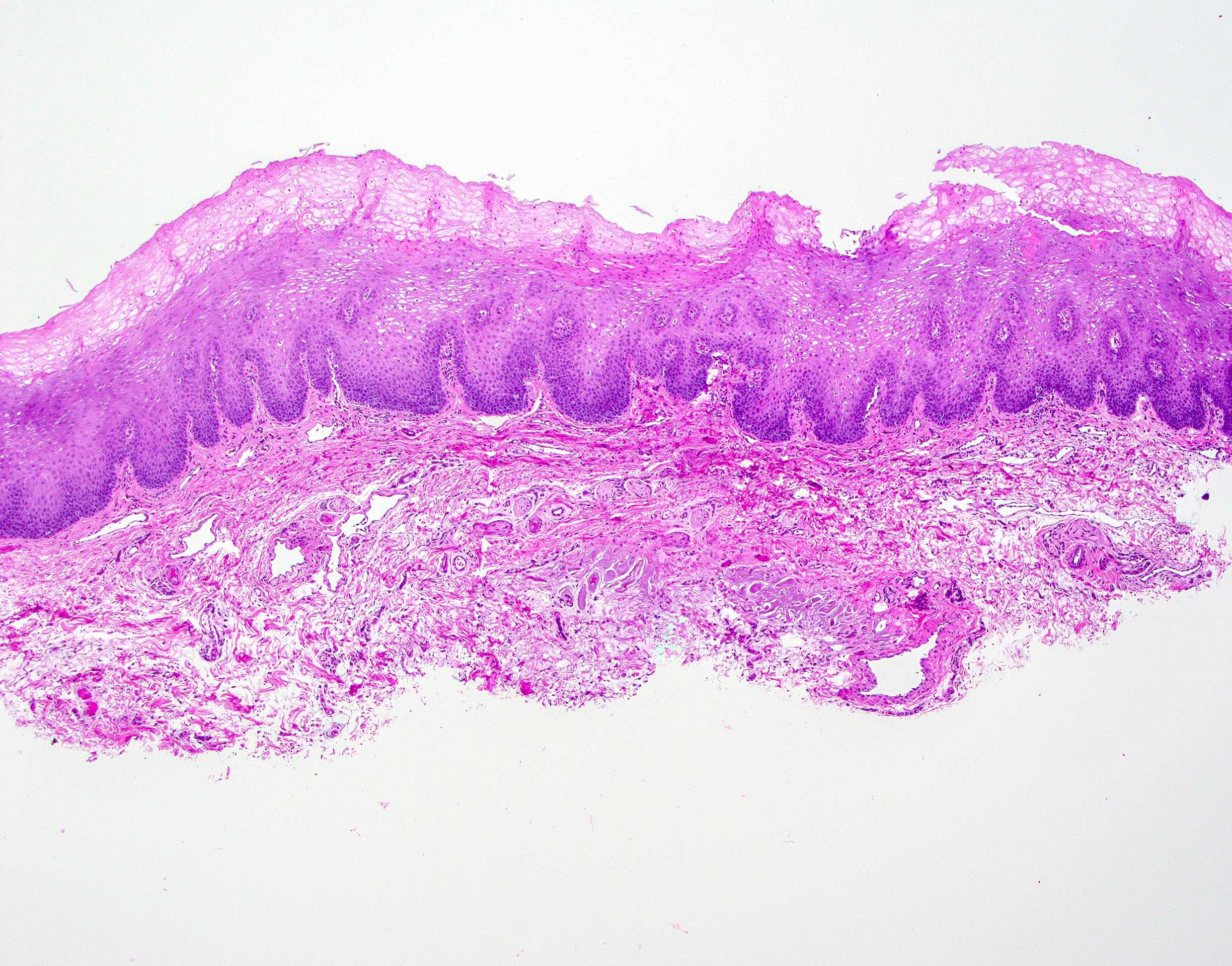
Microscopic (histologic) description
- Microscopic features may be subtle; clinical correlation or photographs are vital to diagnosis
- The following histopathologic categories of proliferative verrucous leukoplakia are taken directly from the Consensus Guideline by Thompson et al., 2021 (Head Neck Pathol 2021;15:572, see table)
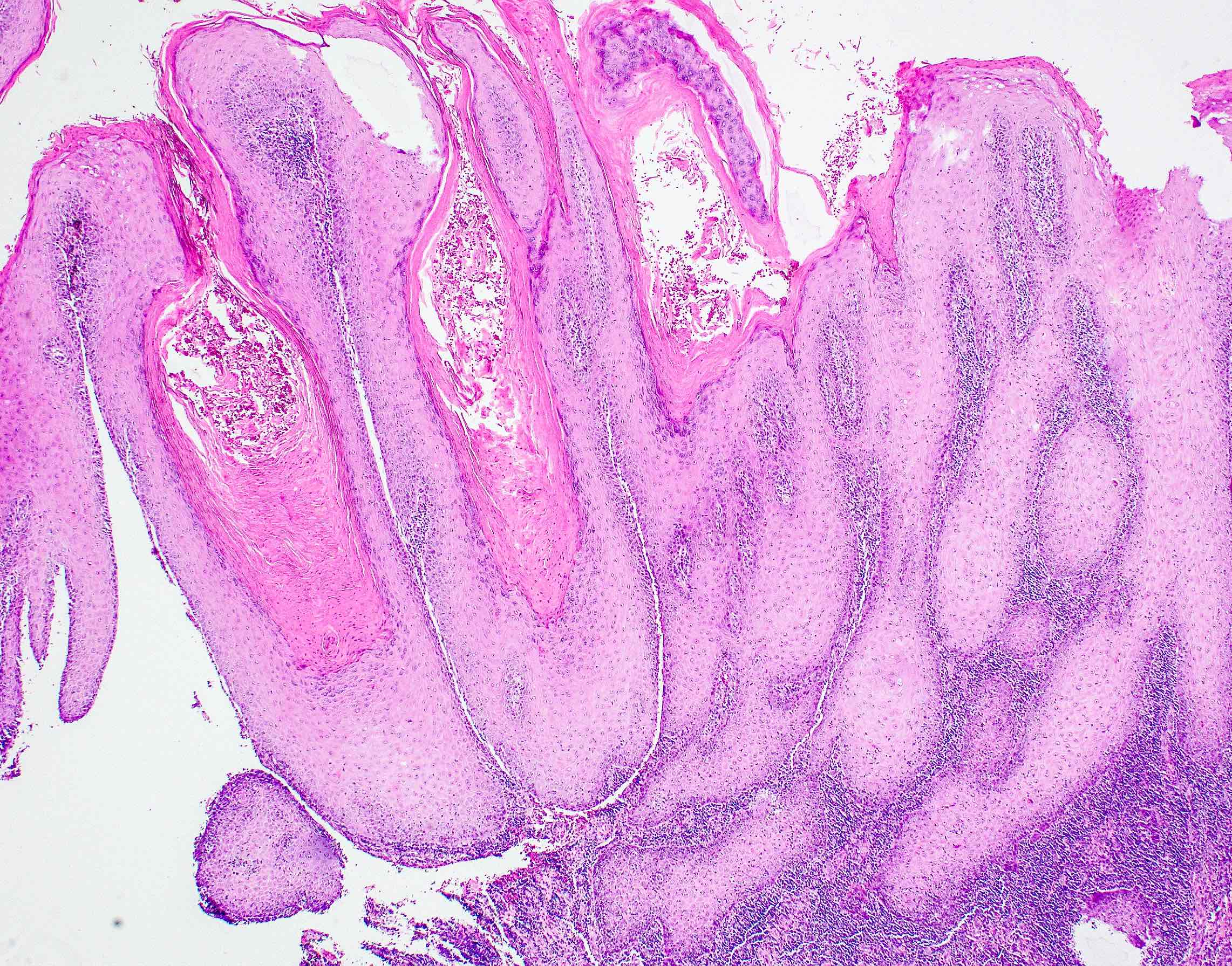
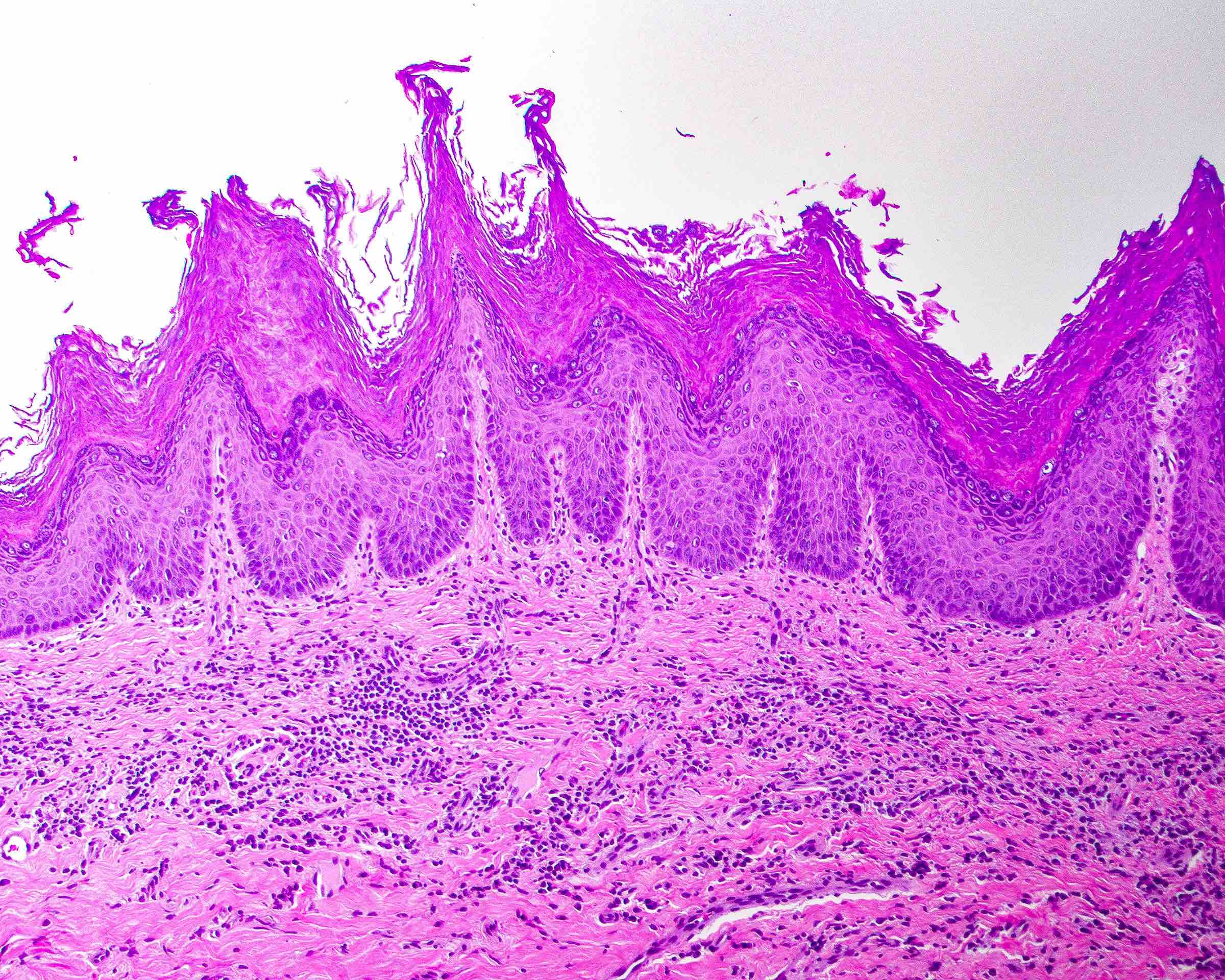
- Corrugated ortho(para)hyperkeratotic lesion, not reactive
- Disproportionate orthokeratosis
- Orthokeratosis that is > half of adjacent epithelial thickness
- Troughs and crests of keratosis or epithelium, i.e., corrugation
- Wave-like undulation commonly seen in sentinel lesions
- Prominent crests or spikes in clinically worrisome lesions (formerly Christmas tree keratosis)
- Minor subgroup in this category shows flat, dense, markedly thickened orthokeratin with atrophic underlying spinous layer (proliferative leukoplakia)
- Usually prominent granular layer
- Skip segments of ortho and parahyperkeratosis
- Absent to scant acute surface inflammation
- Loss of rete pegs or atrophic epithelium for site
- Sharp demarcation / abrupt transitions
- Architectural distortion is greater than cytologic atypia
- Disproportionate orthokeratosis
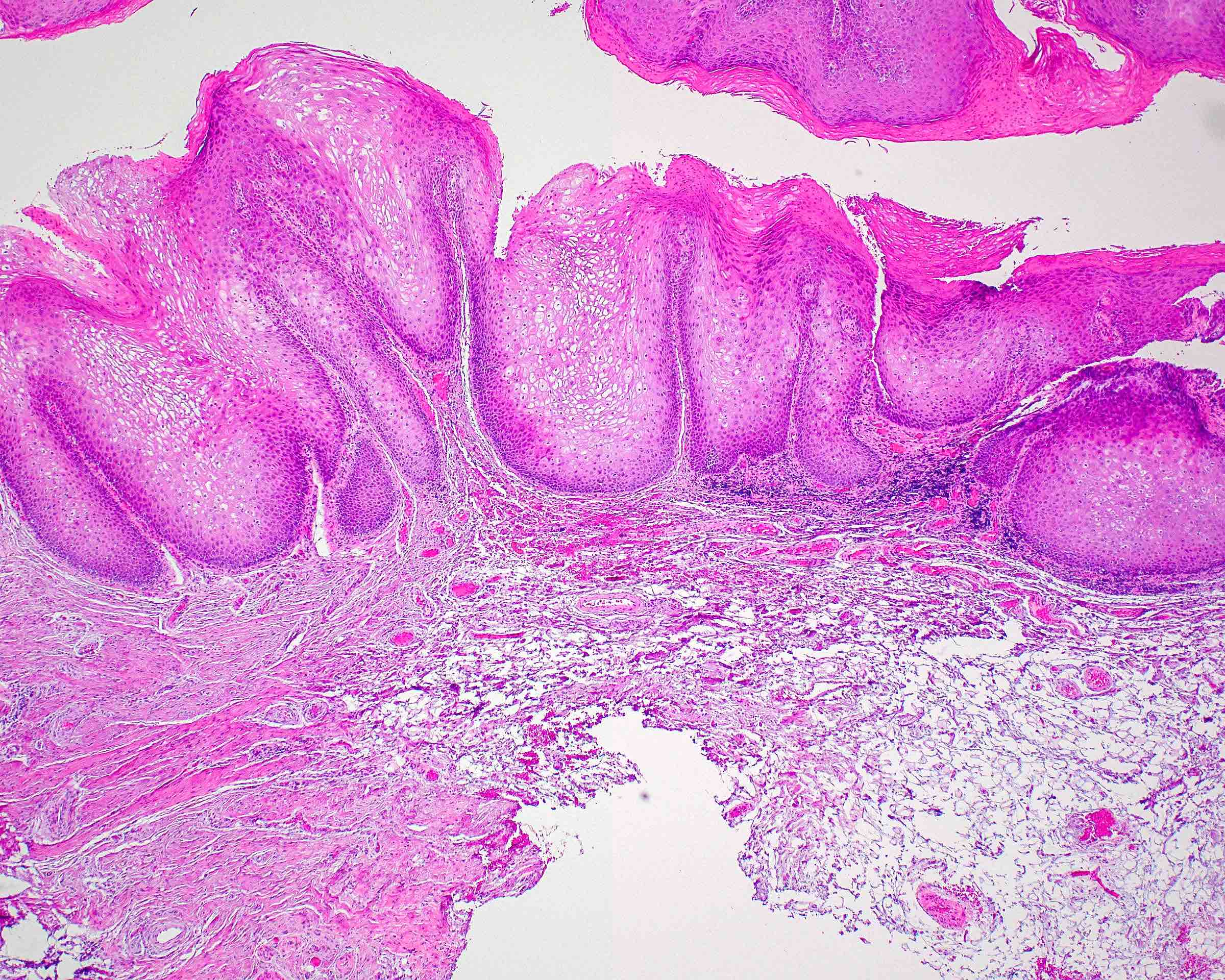
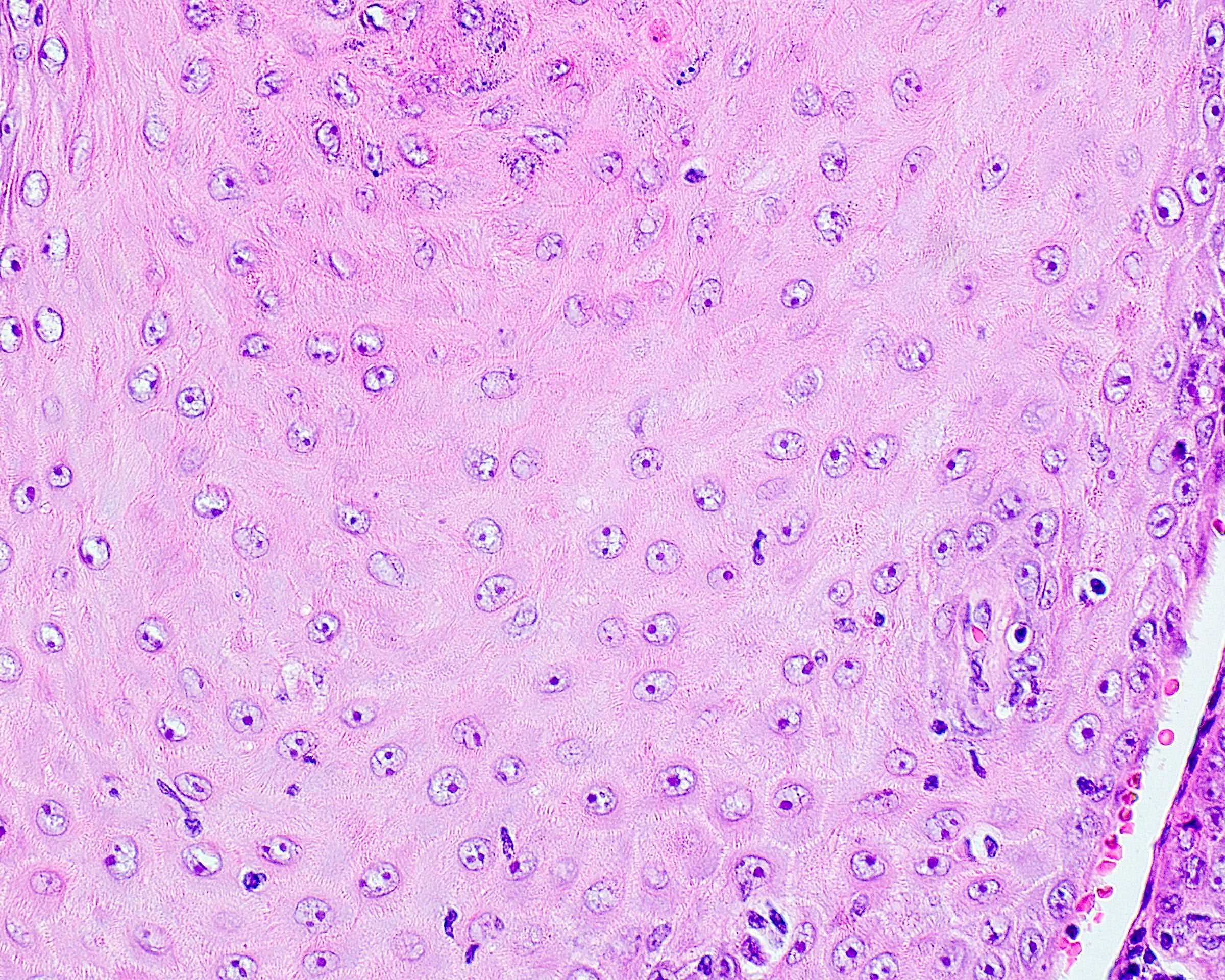
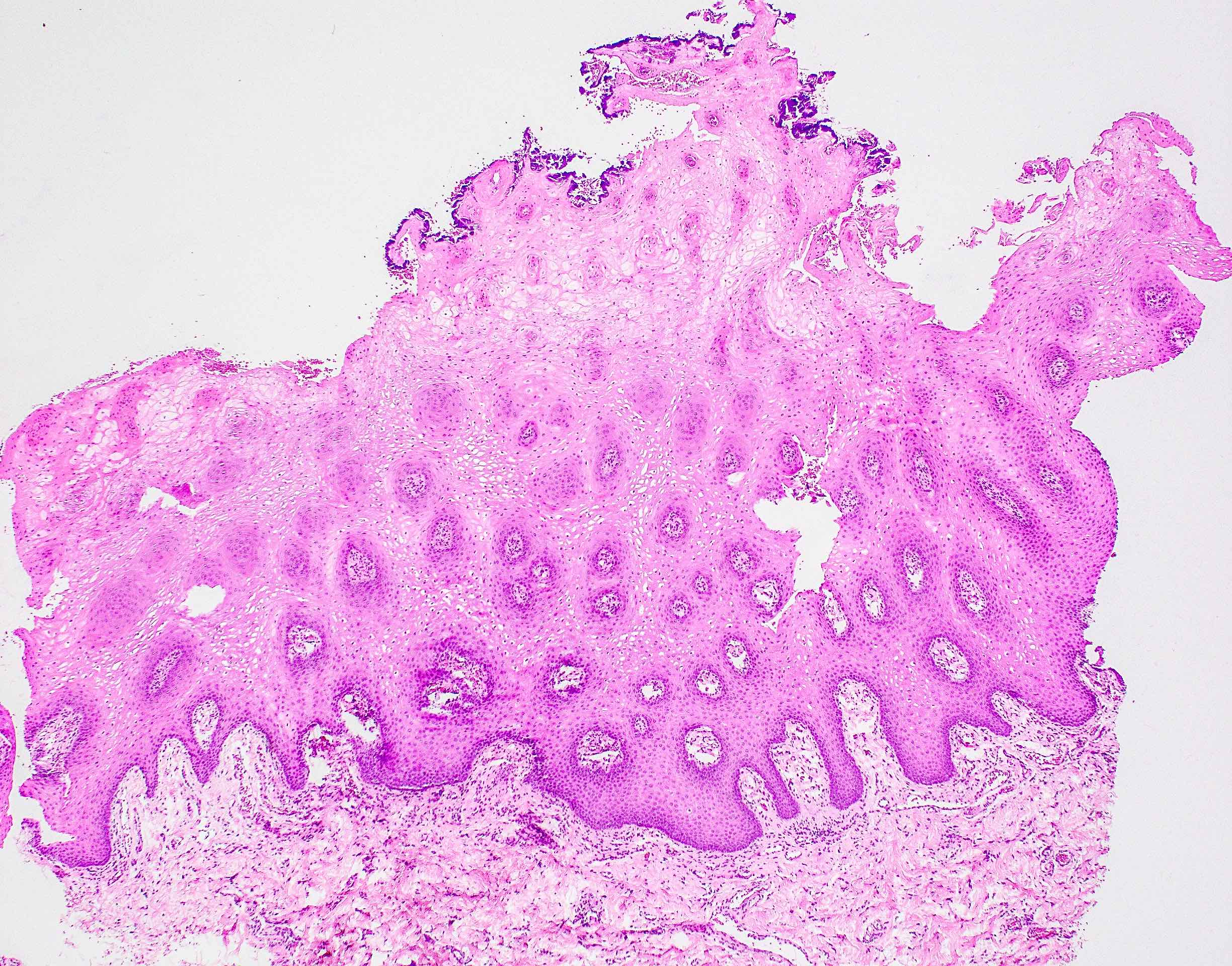
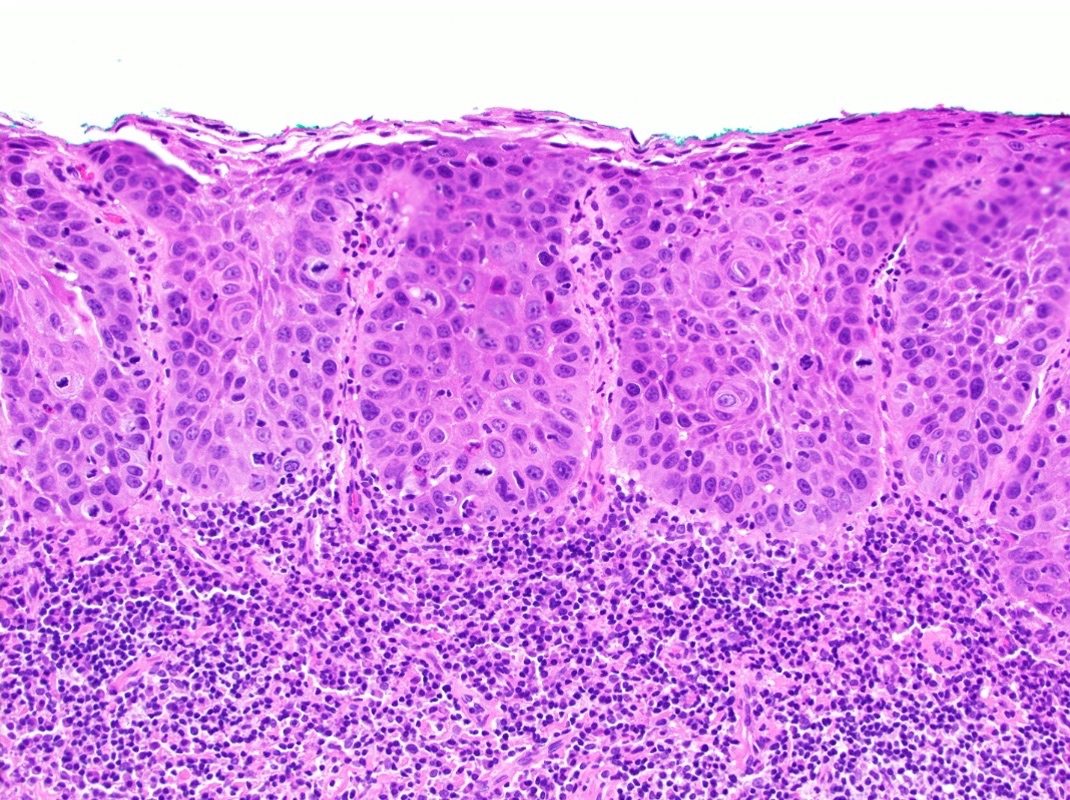
- Bulky hyperkeratotic epithelial proliferation, not reactive
- Amplified bulkiness of the epithelial proliferation that accounts for the lesion's thickness rather than keratosis (usually orthokeratosis)
- Bulbous rete pegs that sometimes coalesce to appear confluent, with architectural abnormalities overshadowing cytologic findings
- Separation artifact between epithelium and stroma
- Lichenoid inflammation at advancing epithelial front is sometimes present
- Consider risky sites in order: gingiva > soft palate > floor of mouth > buccal > tongue
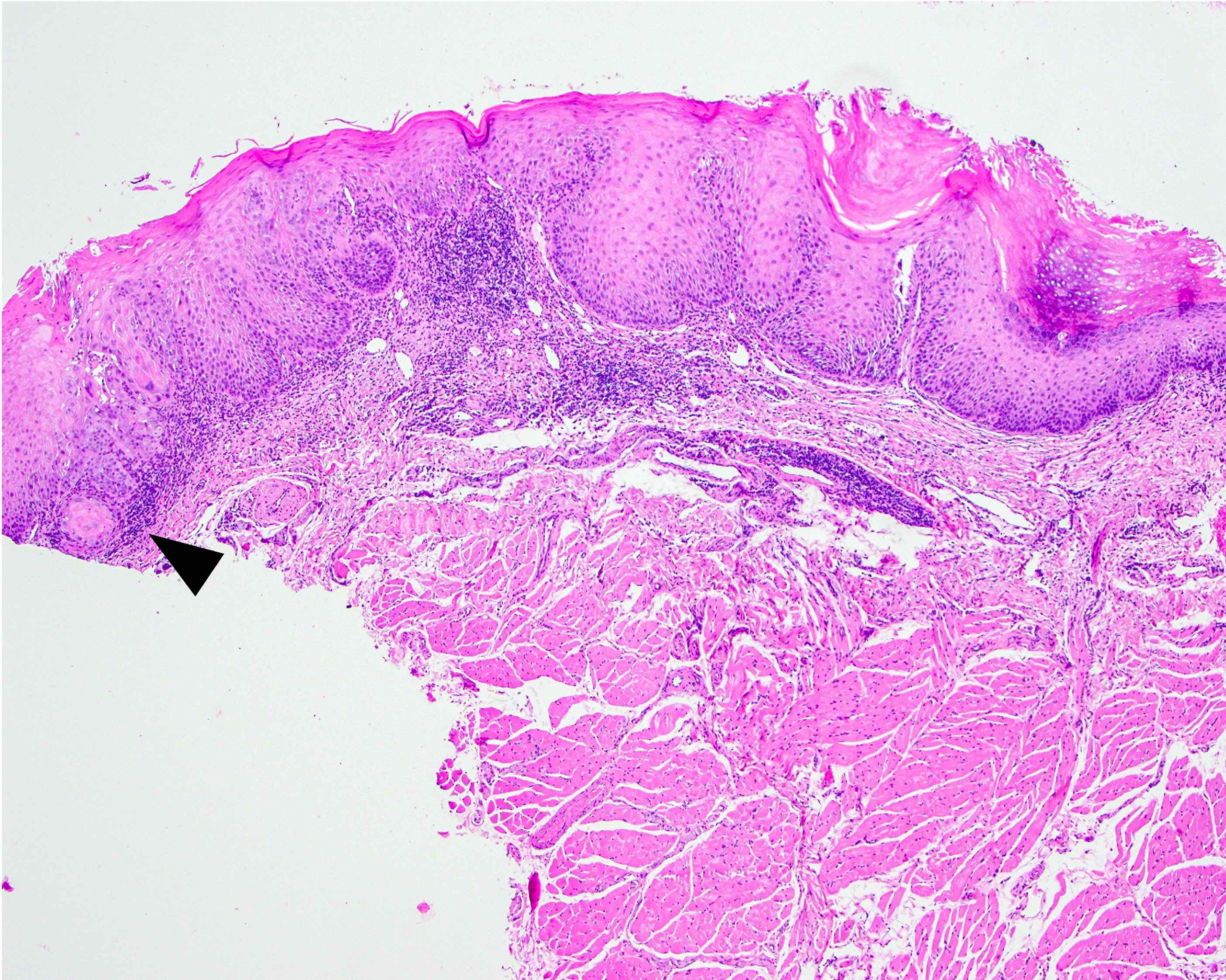
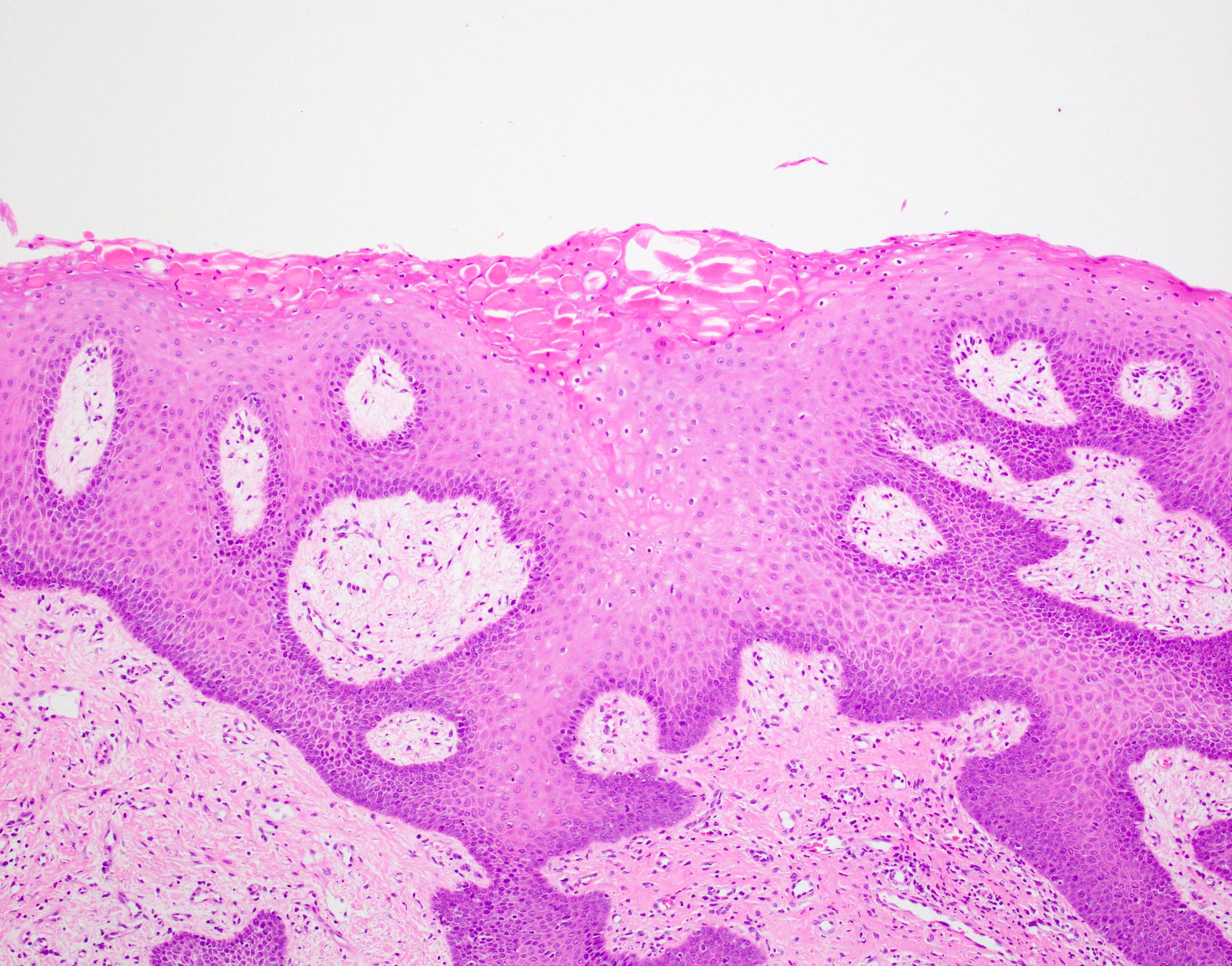
- Suspicious for or squamous cell carcinoma
- Voluminous squamous epithelial proliferation with acanthotic endophytic appearing columns with complex folding and invaginations that is > 3 - 4 times the adjacent uninvolved epithelial thickness
- Thick, clubby, bulbous, blunt, downwardly directed rete peg projections:
- May or may not extend below level of adjacent epithelium and often lacking classical invasion or extension below adjacent epithelium
- Basement membrane is often intact
- Intraepithelial microabscesses, sometimes with keratin pearls
- Increased intraepithelial eosinophils
- Muscle abutment / displacement
- Parakeratotic crypting
- Occasional church spire hyperkeratosis in some
- Focal dysplasia may be present but is usually limited
- Corrugated ortho(para)hyperkeratotic lesion, not reactive
Microscopic (histologic) images
Contributed by Molly Housley Smith, D.M.D.
Sample pathology report
- Gingiva, biopsy:
- Corrugated hyperorthokeratosis and chronic mucositis (see comment)
- Comment: When combined with the clinical description and photographs, the histomorphology is compatible with proliferative verrucous leukoplakia.
Differential diagnosis
- Lichen planus / lichenoid reaction:
- Histopathologic features
- Degeneration of the epithelium at the stromal - epithelial junction with blurring of the basal cells with the superficial lamina propria
- Band of lymphocytes within the superficial lamina propria (although lichenoid reactions often have plasma cells, histiocytes or eosinophils as well)
- Sawtooth rete ridges or atrophy
- Degenerated keratinocytes, termed Civatte, colloid or hyaline bodies
- Parakeratosis or minimal to absent orthokeratosis
- Ulceration or subepithelial separation may be present
- Cytologic dysplasia is absent
- Because lichen planus may show overlapping histopathologic features with PVL, diagnosis requires clinical - pathologic correlation (Head Neck Pathol 2021;15:572)
- Lichen planus and medication related lichenoid reactions should migrate or change patterns; although contact related reactions (e.g., due to an adjacent amalgam restoration) may remain in one place, the lesion should not progress and should ameliorate upon elimination of the adjacent irritant
- May be painful, particularly when eating acidic foods
- May show lace-like striations, papules, plaques, ulcerations / erosions or erythema
- Should respond to steroid therapy (although medication related lichenoid reactions may be recalcitrant)
- Histopathologic features
- Foreign body gingivitis with hyperkeratotic lesions:
- Recently, white, progressing, verrucous clinical lesions (mimicking PVL) were found to be strongly associated with granules of embedded foreign material (Oral Surg Oral Med Oral Pathol Oral Radiol 2019;128:250)
- Silica is the most common element found in the embedded foreign material (Oral Surg Oral Med Oral Pathol Oral Radiol 2019;128:250)
- It is uncertain whether this embedded foreign material plays a role in the pathogenesis of PVL or if it represents a separate disease process
- Alveolar ridge keratosis:
- White plaque without erythema or ulceration, present on the edentulous alveolar ridge or the retromolar pad
- Clinically exhibits fading margins rather than well demarcated margins seen in PVL (Head Neck Pathol 2021;15:572)
- White lesions that extend off the alveolar ridge are more concerning
- Histopathologically demonstrates a corrugated layer of orthokeratin but has elongated rete ridges and the inflammatory component is insignificant
- Fibrous stroma is often densely fibrotic
- Traumatic hyperkeratosis (morsicatio):
- Lesions that arise from chronic biting, nibbling or rubbing of the area
- Often arise on the buccal mucosa or lateral tongue along the line of occlusion
- Patients may or may not be aware of the biting habit
- Clinically, lesions are white and often demonstrate a shaggy or shredded surface texture; the lesions blend in with the surrounding mucosa
- Microscopic examination shows thickened parakeratin, often with bacterial surface colonies, areas of plasma / serum pooling, edema within the keratinocytes and thickening of the spinous cell layer; scattered inflammatory cells are seen within the underlying connective tissue
- Tobacco pouch keratosis:
- Mucosal alterations due to habitual use of chewing tobacco or snuff
- Clinically, the mucosa is thickened and fissured with a white-gray sheen
- Histopathologic examination reveals thickening of the spinous cell layer, basilar hyperplasia and a thickened layer of edematous ortho or parakeratin which forms epithelial peaks or chevrons; a dense band of eosinophilic hyalinization may be seen in the superficial lamina propria with use of wet snuff
- Epithelial dysplasia / unifocal leukoplakia, not attributable to PVL:
- M > F
- Associated with tobacco and alcohol use (Cancers (Basel) 2021;13:4085)
- Histopathologically shows bulbous or teardrop shaped rete ridges with variable degree of pleomorphism, hyperchromasia, hypercellularity, increased and abnormal mitotic figures, increased nuclear size and individual cell keratinization
Board review style question #1
A 73 year old woman presents with multiple, asymptomatic white patches of the attached gingiva that have progressed over a few months. The lesions do not change pattern and do not migrate. Histopathologic examination reveals epithelium with a thickened, corrugated layer of orthokeratin devoid of overt cytologic dysplasia. What condition does this patient have?
- Alveolar ridge keratosis
- Proliferative verrucous leukoplakia
- Squamous cell carcinoma
- Tobacco pouch keratosis
Board review style answer #1
Board review style question #2
Which of the following is true of the condition proliferative verrucous leukoplakia?
- Chewing tobacco is a common etiologic factor
- Males are most frequently affected
- Microscopic examination of the associated white lesions shows frank cytologic dysplasia during early stages
- Patients demonstrate a ~50% risk of developing oral squamous cell carcinoma
Board review style answer #2
D. Patients demonstrate a ~50% risk of developing oral squamous cell carcinoma
Comment Here
Reference: Proliferative verrucous leukoplakia
Comment Here
Reference: Proliferative verrucous leukoplakia