Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Smith MH. Verrucous carcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/oralcavityverrucous.html. Accessed April 1st, 2025.
Definition / general
- Locally invasive, nonmetastasizing, highly differentiated, exophytic variant of squamous cell carcinoma
Essential features
- 2 - 12% of all oral carcinomas (Int J Oncol 2016;49:59)
- M > F; sixth to seventh decades of life
- May occur at any oral or pharyngeal site, although the oral cavity (tongue, buccal mucosa, alveolar mucosa) is the most common site
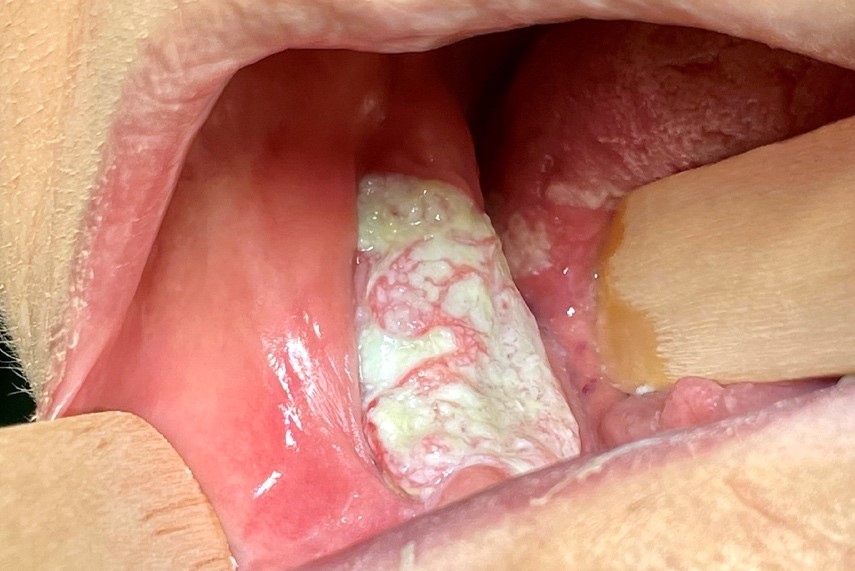
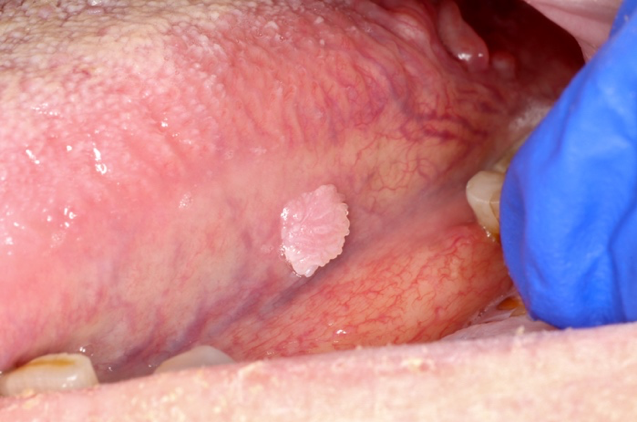
- Characterized by slow growing, verrucoid / cauliflower-like exophytic growth
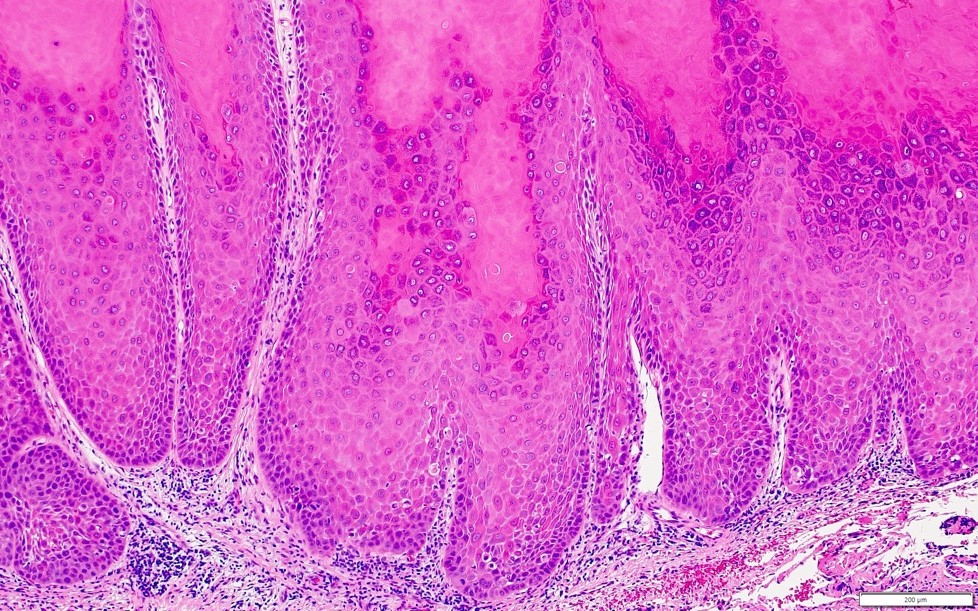
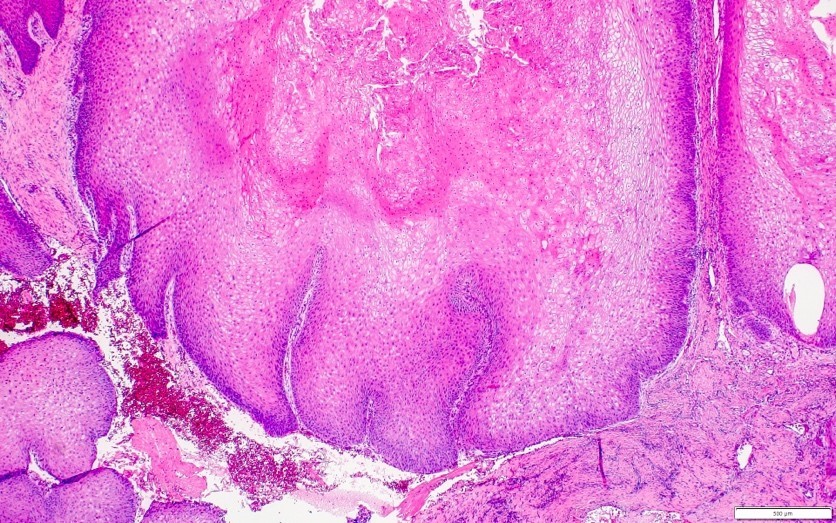
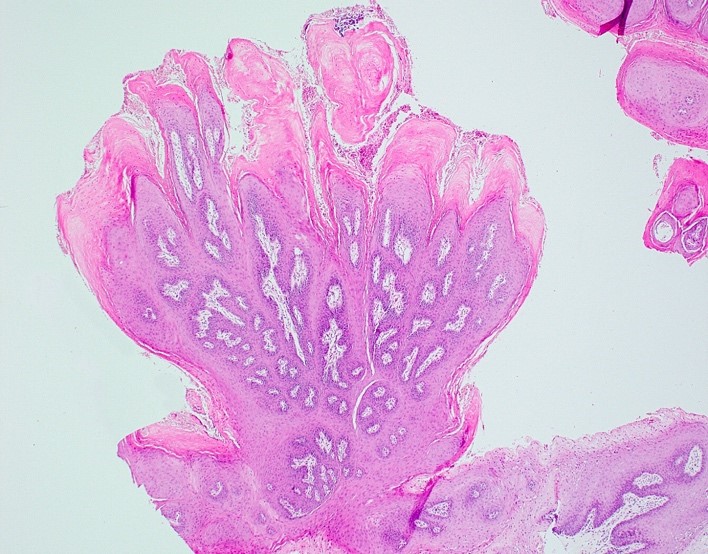
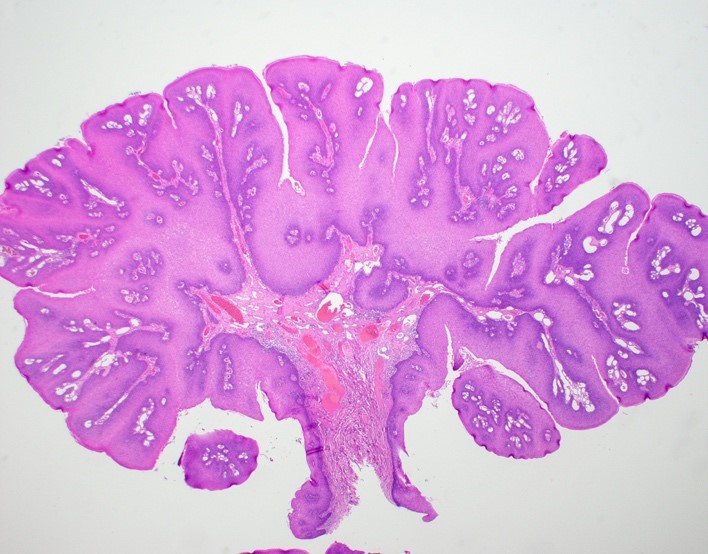
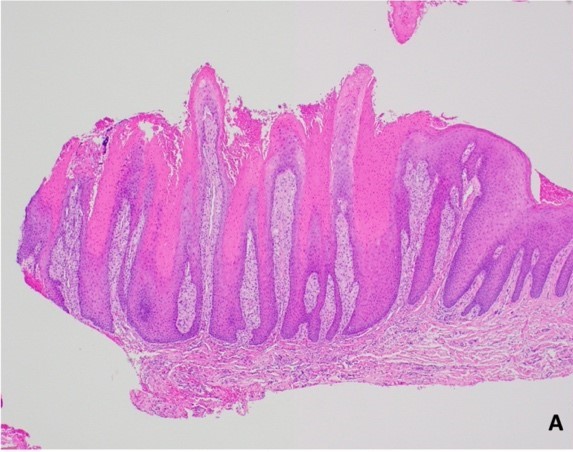
- Elongated and bulbous rete ridges exhibiting a pushing margin below the level of intact, uninvolved surface epithelium; church spire peaks of keratin, keratin clefting and bland cytology
Terminology
- Use of historic term Ackerman tumor not recommended by 5th edition of the World Health Organization
ICD coding
- ICD-10: C00 - C14 - malignant neoplasm of lip, oral cavity and pharynx
Epidemiology
- 2 - 12% of all oral carcinomas (Int J Oncol 2016;49:59)
- M > F
- Sixth to seventh decades of life; mean age at diagnosis: 69.5 years (1973 - 2012) (Laryngoscope 2018;128:393)
Sites
- Oral tongue, alveolar ridge and buccal mucosa are the most common sites (Laryngoscope 2018;128:393, Int J Oncol 2016;49:59)
Pathophysiology
- Multistep process involving genetic alterations / predisposition and environmental influences (Int J Oncol 2016;49:59)
- Several biomarkers have been studied / identified; however, DAMTS12, COL4A1, COL4A2, INHBA, MMP1, SEROINE1, TGFBI and HLF are all genes that are expressed differently in oral verrucous carcinoma when compared to traditional oral squamous cell carcinoma, suggesting future therapeutic potential (Int J Clin Exp Med 2014;7:1845, Int J Oncol 2016;49:59)
Etiology
- Proliferative verrucous leukoplakia (PVL) is a known risk factor (Cancers (Basel) 2021;13:4085)
- 29.5% prevalence of developing verrucous carcinoma in patients with proliferative verrucous leukoplakia (Cancers (Basel) 2021;13:4085)
- Associations (synergistic or independent) with tobacco use, areca nut chewing, chronic inflammation, alcohol consumption, antioxidant deficient diet and oral microbiota (Int J Oncol 2016;49:59)
- Controversial association with HPV in older literature; no conclusive association has been proven (Int J Oncol 2016;49:59, Arch Otolaryngol Head Neck Surg 1993;119:1299, Pathobiology 2008;75:257, Tumour Biol 2011;32:409, Radiat Res 1970;41:375)
- No transcriptionally active high risk HPV has been identified (Hum Pathol 2013;44:2385)
Clinical features
- Exophytic, papillary or verrucoid mass
- Slow growth
- Locoregional metastasis and or bone involvement suggests transformation (or component) of conventional invasive squamous cell carcinoma (Int J Oncol 2016;49:59)
Diagnosis
- Along with supportive histopathology, diagnosis may incorporate one or more elements such as patient history, symptoms, clinical examination and imaging
Prognostic factors
- Nodal disease is found in 1.6% of cases and likely can be attributed to transformation into traditional invasive squamous cell carcinoma (Laryngoscope 2018;128:393)
- 2, 5 and 10 year survival rates are 83%, 64% and 42%, respectively (Laryngoscope 2018;128:393)
- Recurrence rate is high if incompletely excised
Case reports
- 14 year old boy with xeroderma pigmentosum presented with verrucous carcinoma on the tip of the tongue (Cureus 2022;14:e31706)
- 30 year old gutka chewer and 60 year old patient with an areca nut and tobacco chewing habit both presented with white verrucoid lesions of the oral cavity (Contemp Clin Dent 2016;7:391)
- 56 year old man with verrucous carcinoma treated successfully with topical 5-aminolevulinic acid mediated photodynamic therapy (J Oral Pathol Med 2005;34:253)
- 67 year old woman presented with a slowly growing, white verrucoid lesion on the maxillary alveolar ridge (Case Rep Oncol Med 2012;2012:190272)
Treatment
- Surgical removal with adequate margins is preferred treatment (Contemp Clin Dent 2012;3:60, Int J Oncol 2016;49:59)
- Chemotherapy and radiation have questionable effectiveness due to poor response and anaplastic transformation (Int J Oncol 2016;49:59, Laryngoscope 2017;127:1334)
Clinical images
Gross description
- White / tan
- Exophytic, papillary, fungating, cauliflower-like growth (J Maxillofac Oral Surg 2011;10:148)
- May bluntly invade adjacent soft tissue
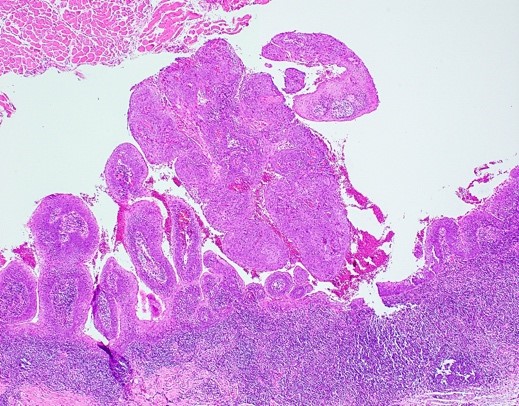
Microscopic (histologic) description
- Poor interobserver agreement among pathologists (Head Neck Pathol 2020;14:156)
- Lack of consistency with terminology for verrucoid lesions creates confusion for clinicians (Head Neck Pathol 2020;14:156)
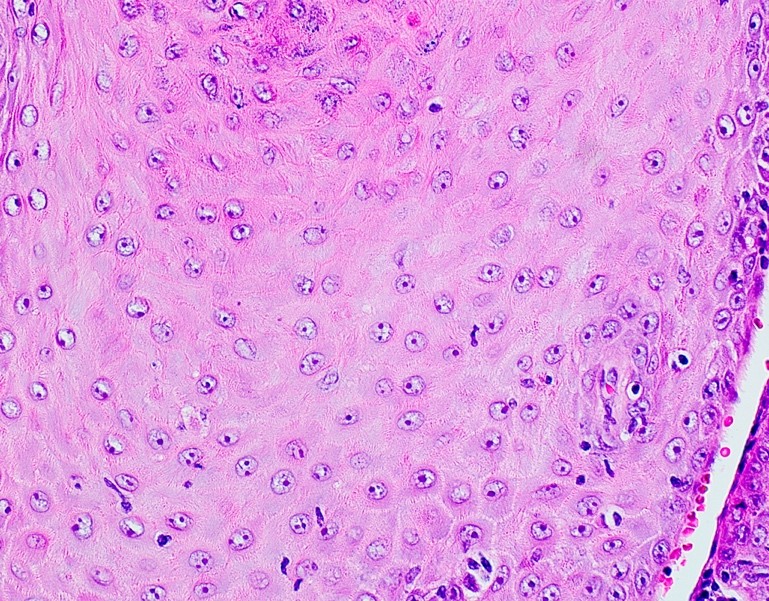
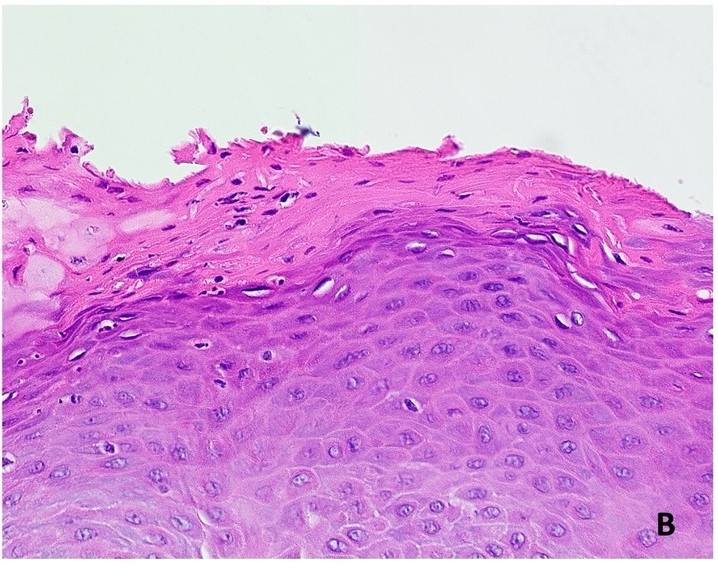
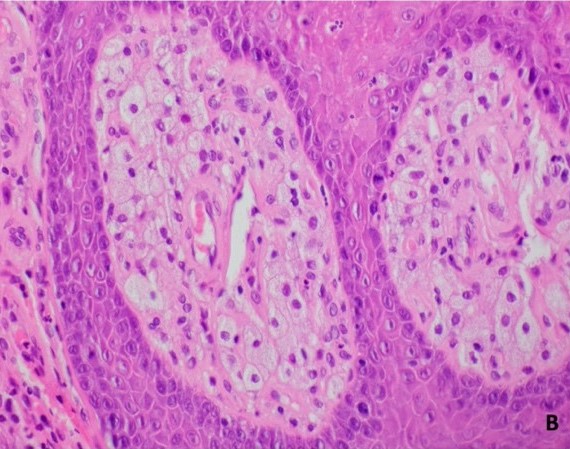
- Well differentiated / cytologically bland, hyperplastic squamous epithelium
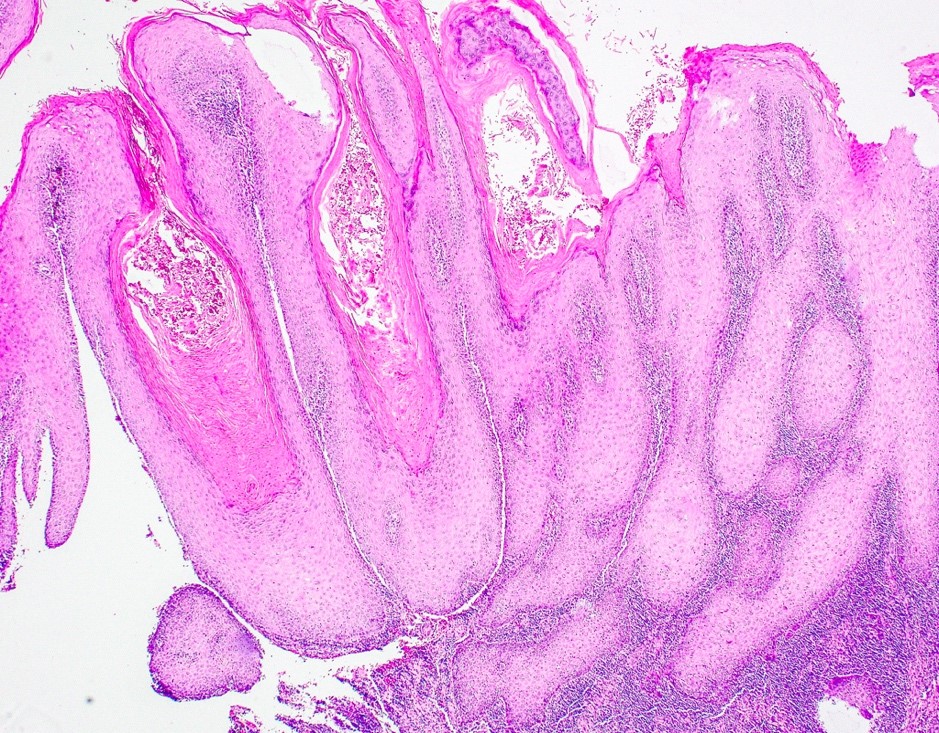
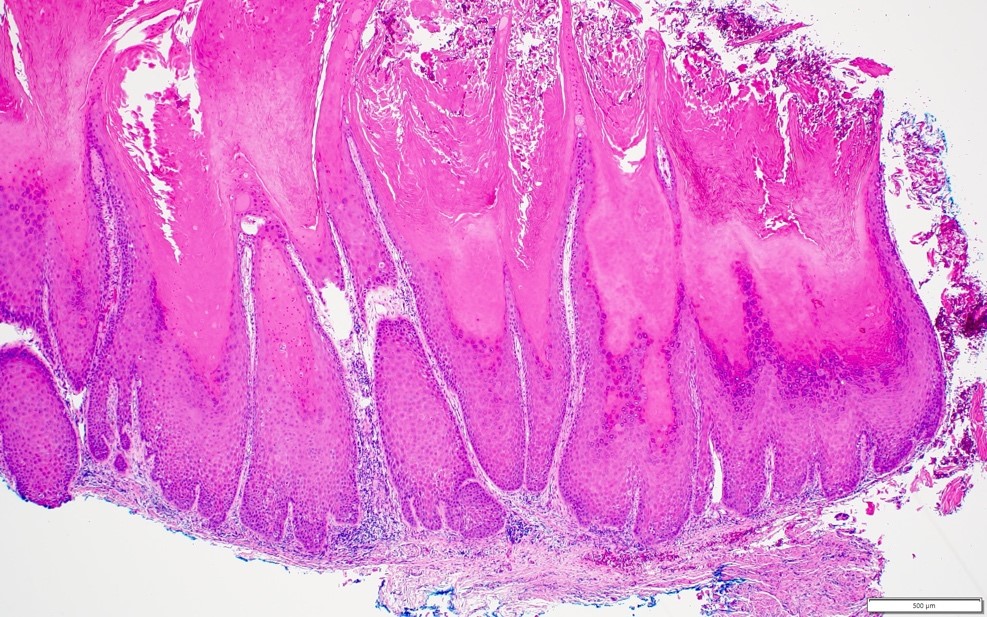
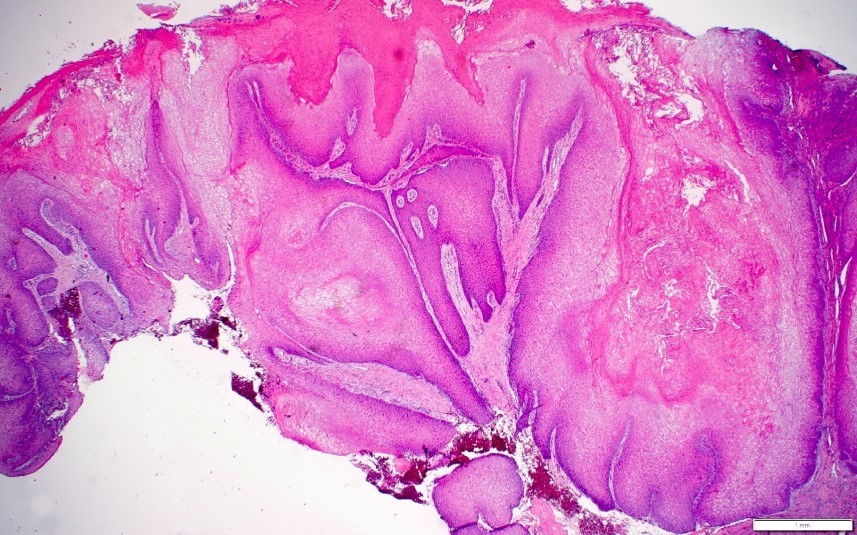
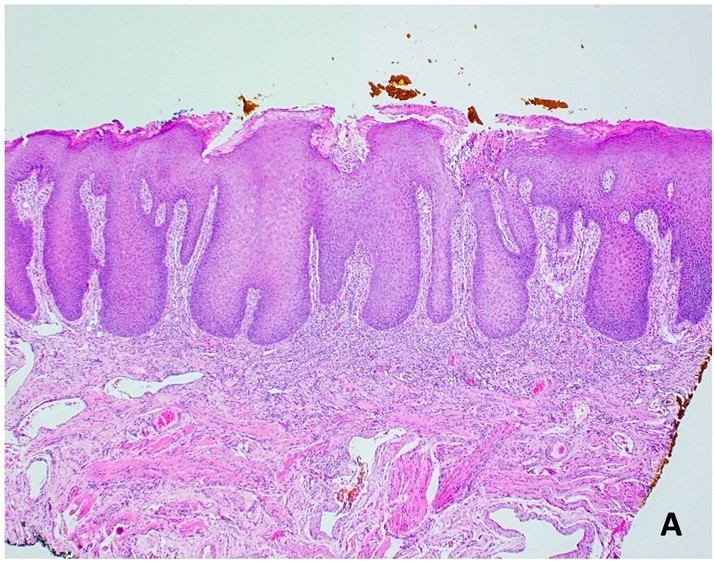
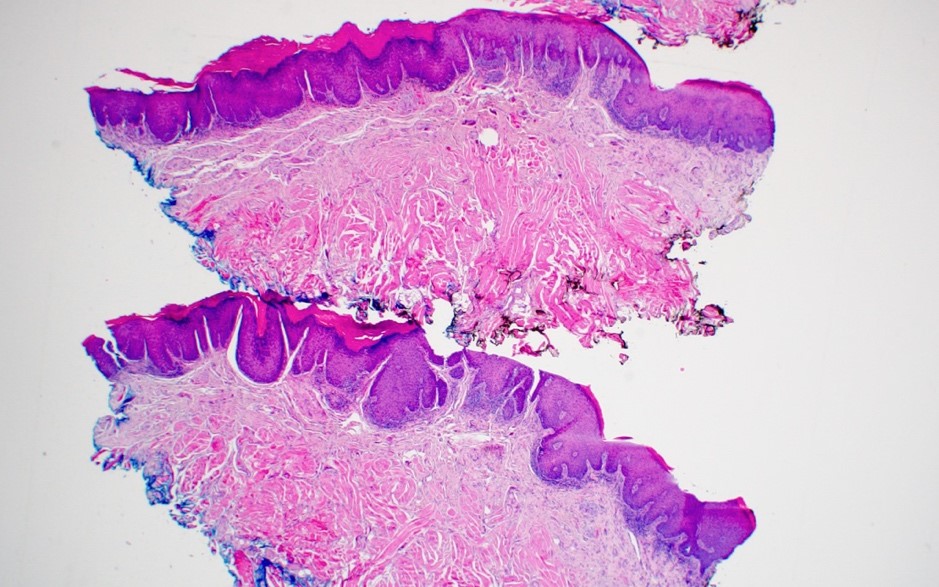
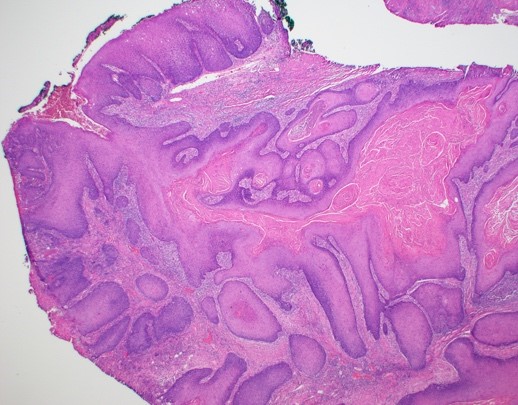
- Broad, bulbous, plunging rete ridges that demonstrate pushing encroachment on muscle or other deep submucosal structures, below the level of intact normal epithelium (Head Neck Pathol 2021;15:572)
- Church spire-like or papillary hyperkeratosis with deep keratin clefting
- Intact basement membrane (Contemp Clin Dent 2016;7:391)
- Minimal cytologic atypia
- Inward cupping of the rete pegs is not apparent
Microscopic (histologic) images
Videos
Verrucous carcinoma
Cutaneous verrucous carcinoma
Sample pathology report
- Right buccal mucosa, biopsy:
- Verrucous carcinoma (see comment)
- Comment: Microscopic examination reveals atypical superficial stratified squamous epithelium overlying fibrous connective tissue. The epithelium exhibits a significantly thickened layer of orthokeratin that forms prominent church spire-like peaks. The rete ridges are bulbous and elongated, forming a broad, pushing margin that abuts skeletal muscle. Prominent keratin clefting / plugging is apparent. The underlying connective tissue contains a dense mixed inflammatory cell infiltrate immediately subjacent to the epithelial proliferation.
Differential diagnosis
- Oral squamous papilloma:
- May be difficult to differentiate from verrucous carcinoma on small, incisional or fragmented biopsies
- Caution is advised when making a diagnosis of papilloma on incisional or fragmented biopsies or when the lesion is not well circumscribed or symmetrical
- Limited growth potential, often small
- Papillary, finger-like projections with fibrovascular connective tissue cores
- Often pedunculated but may be sessile
- Well defined margins
- Lacks endophytic growth pattern
- Lacks prominent hypergranulosis
- Variable keratinization (Head Neck Pathol 2019;13:80)
- May be difficult to differentiate from verrucous carcinoma on small, incisional or fragmented biopsies
- Condyloma acuminatum:
- Labial mucosa, soft palate, lingual frenum
- Often demonstrates a fleshy, broad based clinical appearance but should demonstrate circumscription and symmetry
- Bulbous rete pegs and blunted papillary projections
- Exophytic; lacks broad, pushing, endophytic growth pattern
- Pseudoepitheliomatous hyperplasia:
- Associated with chronic candidiasis and granular cell tumor
- Extreme caution is recommended in diagnosing pseudoepitheliomatous hyperplasia, as secondary candidal colonization may be seen on atypical epithelial processes (e.g., verrucous carcinoma)
- Excision or rebiopsy of lesional tissue remaining after antifungal therapy may be recommended
- Lacks prominent exophytic growth pattern and endophytic pushing margin into bone or skeletal muscle
- Verruciform xanthoma:
- May demonstrate similar clinical characteristics, although may have yellow hue
- Demonstrates foamy xanthoma cells within papillary projections
- Proliferative verrucous leukoplakia / verrucous leukoplakia:
- Characterized by multifocal white plaques with well defined margins
- High transformation rate into verrucous carcinoma or squamous cell carcinoma
- Very similar histology to the bulky hyperkeratotic epithelial proliferation category of proliferative verrucous leukoplakia proposed by Thompson et al. in 2021 (Head Neck Pathol 2021;15:572)
- Verruciform, church spire-like keratin peaks, prominent endophytic growth with bulbous, hyperplastic rete ridges and keratin plugging
- Lacks the pushing architectural pattern
- Squamous cell carcinoma:
- Squamous cell carcinoma (SCCa) may arise within verrucous carcinoma
- Overt evidence of connective tissue invasion lacking intact basement membrane; SCCa shows infiltrative nests of epithelium and may invade into or around nerves, blood vessels or salivary glands
- SCCa may also infiltrate into skeletal muscle bundles, as opposed to verrucous carcinoma, which only pushes into the skeletal muscle
- Carcinoma cuniculatum and papillary squamous cell carcinoma in particular may be confused with verrucous carcinoma
- Carcinoma cuniculatum demonstrates deep burrowing of the epithelium with keratin filled crypts (J Clin Diagn Res 2017;11:ZD37)
- Papillary SCCa likely is confusing based on its name
- Papillary SCCa demonstrates a papillary or filiform architecture (like verrucous carcinoma) but lacks prominent surface keratinization and cytologically exhibits malignant epithelium
Additional references
Board review style question #1
Board review style answer #1
D. Verrucous carcinoma. The microscopic image shows a broad, verrucoid / papillary epithelial proliferation with prominent church spire hyperkeratosis on top of hyperplastic, pushing rete ridges. These findings are consistent with verrucous carcinoma. Answers A, B and C are incorrect because condyloma acuminatum, squamous papilloma and verruca vulgaris all may demonstrate exophytic papillary projections; however, all 3 of these entities should demonstrate some degree of circumscription (perhaps inward cupping rate ridges) and symmetry. Most importantly, these 3 entities should lack pushing, infiltrative rete ridges.
Comment Here
Reference: Verrucous carcinoma
Comment Here
Reference: Verrucous carcinoma
Board review style question #2
A patient presents with a white and red exophytic granular growth on the alveolar ridge. Microscopic examination shows church spire-like keratin peaks, keratin plugging and bulbous shaped, hyperplastic rete ridges that push downward and abut underlying bone. What is the diagnosis?
- Condyloma acuminatum
- Squamous papilloma
- Verruca vulgaris
- Verrucous carcinoma
Board review style answer #2
D. Verrucous carcinoma. Church spire-like keratin peaks, keratin plugging and bulbous shaped, hyperplastic rete ridges that push downward and abut underlying bone are all features of verrucous carcinoma. Answers A, B and C are incorrect because condyloma acuminatum, squamous papilloma and verruca vulgaris all may demonstrate exophytic papillary projections; however, all 3 of these entities should demonstrate some degree of circumscription (perhaps inward cupping rate ridges) and symmetry. Most importantly, these 3 entities should lack pushing, infiltrative rete ridges. Additionally, the clinical image shows a large, broad based lesion lacking symmetry. Clinically, condyloma acuminatum, squamous papilloma and verruca vulgaris show circumscription and symmetry.
Comment Here
Reference: Verrucous carcinoma
Comment Here
Reference: Verrucous carcinoma