Table of Contents
Definition / general | Essential features | Terminology | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Molecular / cytogenetics description | Molecular / cytogenetics images | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Maleki Z. HPV associated. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/oralcavityHPVrelatedoropharyngeal.html. Accessed January 11th, 2025.
Definition / general
- An increasing subset of oropharyngeal carcinomas caused by high risk human papillomaviruses (HPV) (El-Naggar: WHO Classification of Head and Neck Tumours, 4th Edition, 2017)
Essential features
- Oropharyngeal squamous cell carcinoma caused by high risk HPV
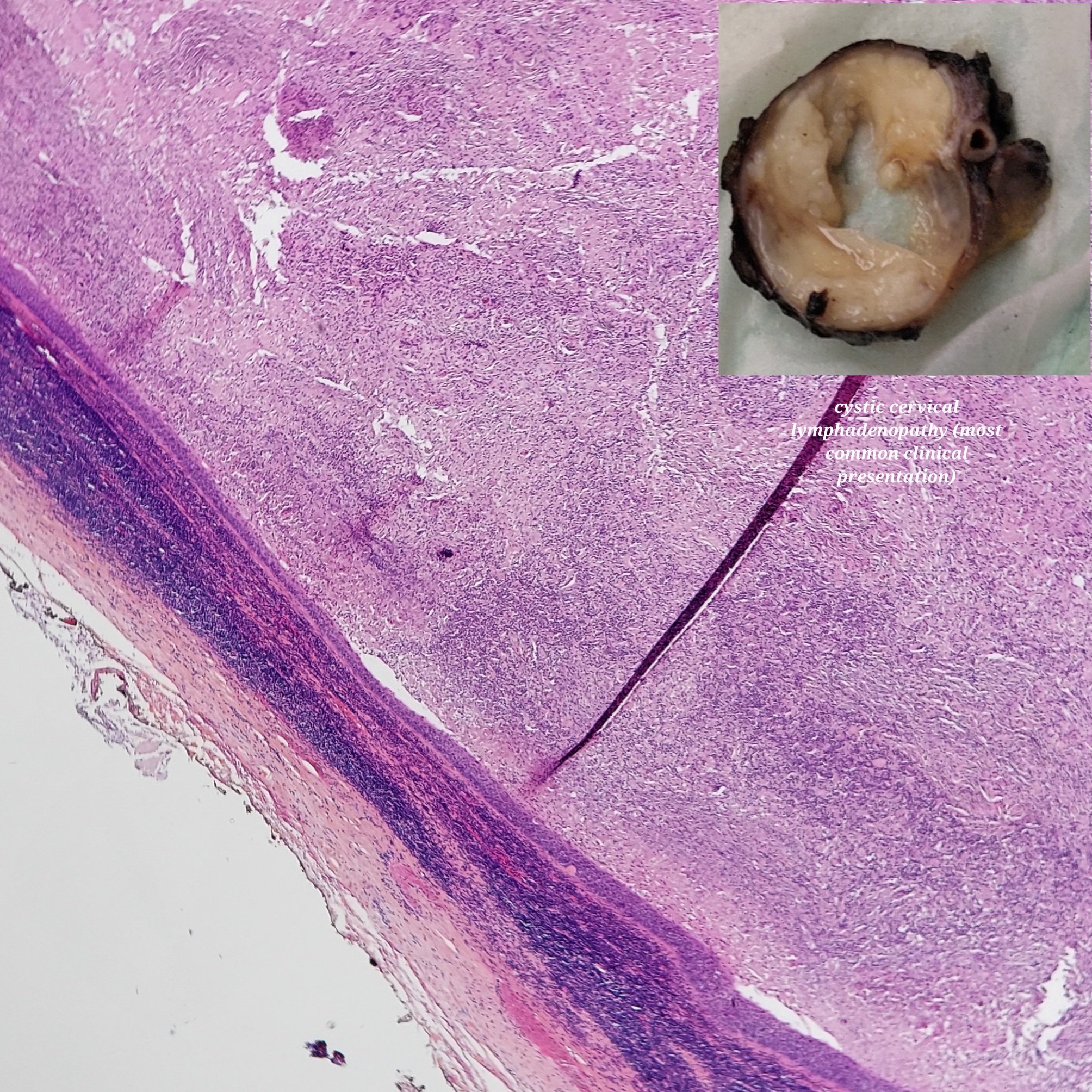
- Mostly present as a cystic or solid neck mass, enlarged cervical lymph node, or rarely enlarged tonsil
- Variable squamous differentiation characterized by orangeophilic keratinized squamous cells in Papanicolaou stain
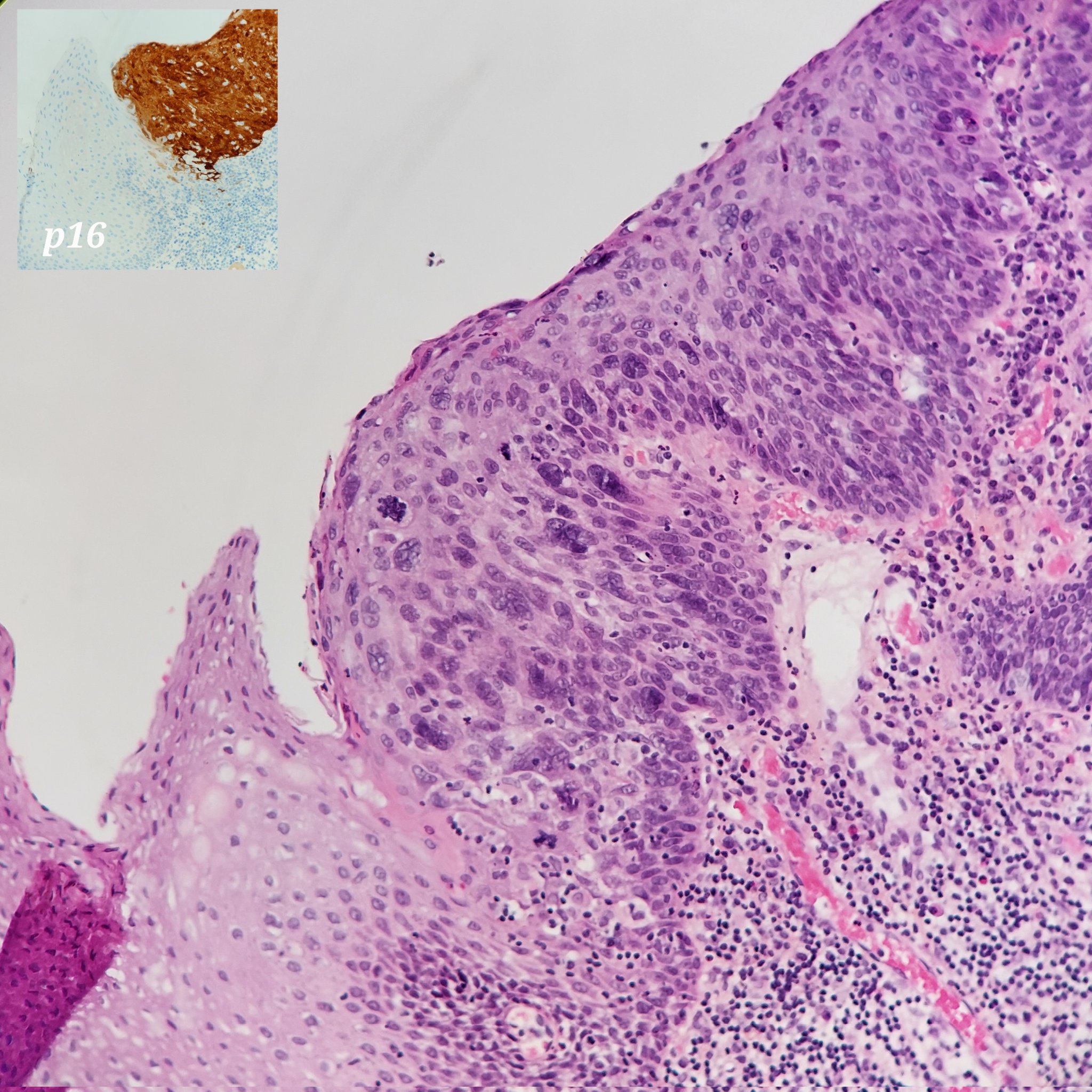
- p16 immunostain, a surrogate marker for high risk HPV, is considered positive when expressed in ≥ 70% of tumor cells with both nuclear and cytoplasmic staining; occasionally p16 is focal / patchy positive or negative
- High risk HPV can be detected by different methods such as RNA in situ hybridization
- High risk HPV testing can be performed on both primary or metastatic tumor
- No tumor grading
- Overall favorable prognosis despite early local lymph node metastasis (Cancer Epidemiol Biomarkers Prev 2019;28:1660)
- Rare cases associated with distant metastasis and poor prognosis
- HPV+ squamous cell carcinoma is associated with better prognosis than HPV- squamous cell carcinoma
Terminology
- Also known as HPV+ squamous cell carcinoma of oropharyngeal origin (El-Naggar: WHO Classification of Head and Neck Tumours, 4th Edition, 2017)
Epidemiology
- Affects both males and females, more common in white males, mostly younger than 65
- Incidence is growing rapidly (J Clin Oncol 2011;29:4294)
- U.S. incidence of oropharyngeal HPV+ squamous cell carcinoma is higher than the incidence of HPV- cases, 4.62 versus 1.82 per 100,000 (Cancer Epidemiol Biomarkers Prev 2019;28:1660)
- Patients are younger, predominantly Caucasians and higher socioeconomic status compered to HPV- squamous cell carcinoma
Sites
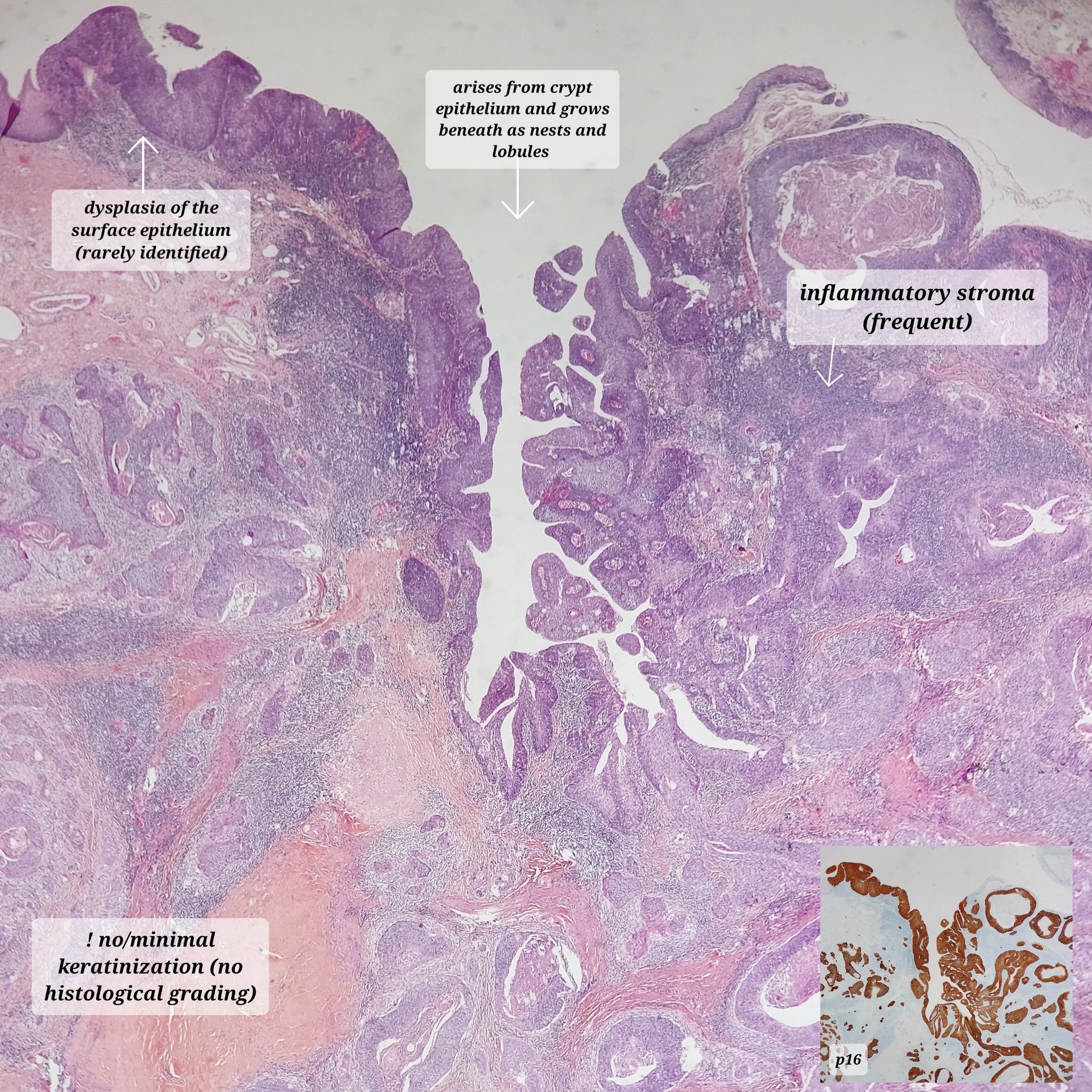
- Most common in oropharynx (tonsils, base of tongue and adenoids) and posterior pharyngeal wall
- Arise from the tonsillar crypts
Pathophysiology
- Etiologic agent is high risk HPV
- Arises from the tonsillar crypts
- Initial step is infection of the epithelial basal layer by HPV through microabrasions or trauma
- HPV double stranded DNA genome encodes oncoproteins such as Early genes E1, E2, E6 and E7 after integration into the host cell nucleus (J Dent Res 2015;94:1532)
- E1 and E2 genes activate viral replication
- E6 binds to p53 and inactivates tumor suppressor protein p53 and E7 binds to pRB and inactivates tumor suppressor protein pRB
- E6 and E7 expression promotes cellular proliferation and increases chance of malignancy (J Am Soc Cytopathol 2016;5:203)
Etiology
- Caused by high risk HPV, mostly commonly associated with HPV16 and HPV18 strains
- Also includes high risk HPV strains 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 68, 82, as well as others (Cancer Epidemiol Biomarkers Prev 1996;5:567)
- Oral sexual contact is a major risk factor, but not alcohol or tobacco (smoking or chewing)
Clinical features
- Initial presentation in most cases is a neck mass or cervical lymphadenopathy
- Occasionally presents with a unilateral enlarged tonsil
- May have distant metastases to the lungs, mediastinal lymph nodes, brain, liver, bone, skin, duodenum (J Am Soc Cytopathol 2016;5:203)
Diagnosis
- Tissue findings in which morphology, along with nuclear and cytoplasmic expression of p16 in ≥ 70% of tumor cells or detection of high risk HPV in tumor cells, is required for the diagnosis
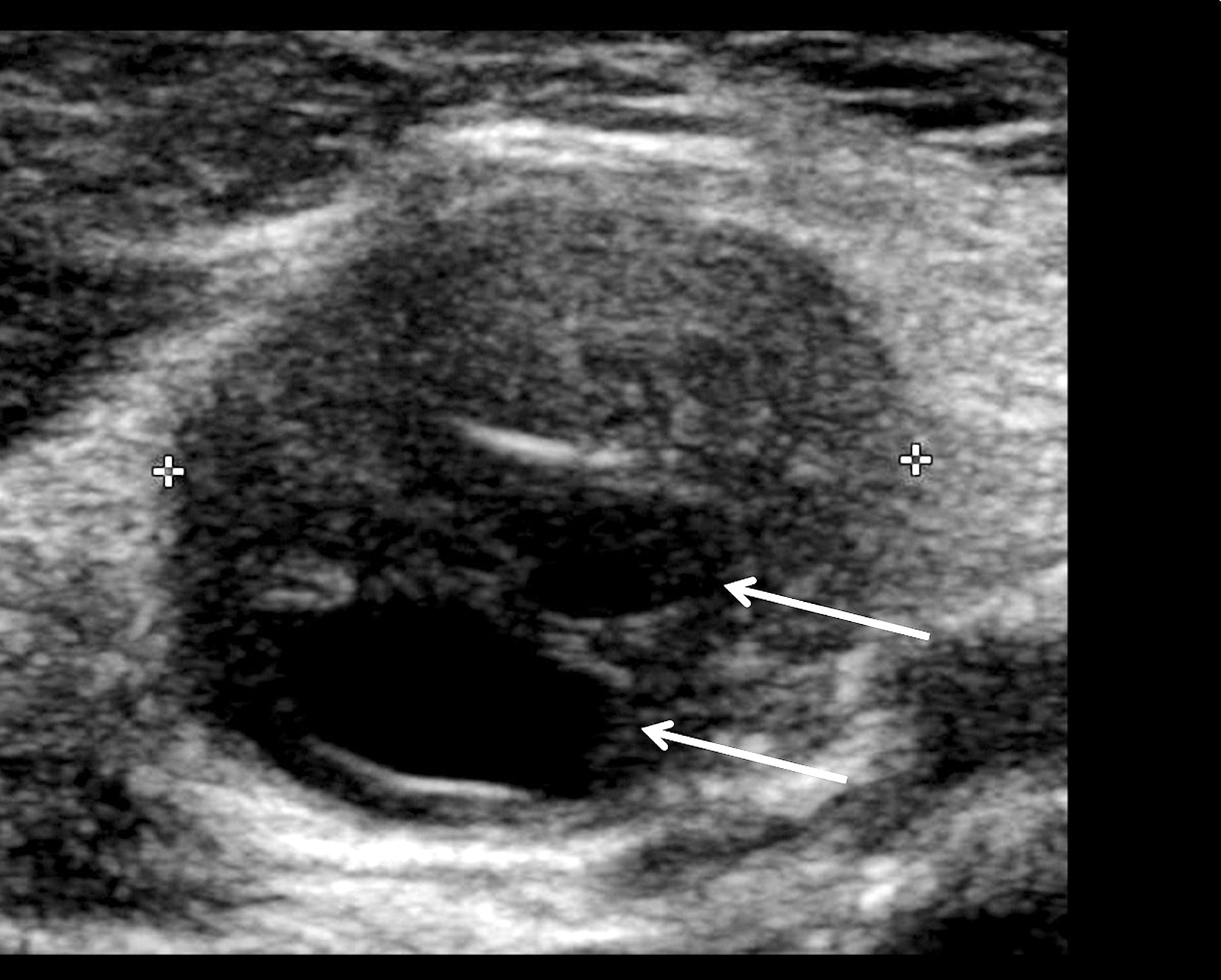
Radiology description
- Imaging findings, including ultrasound, such as enlargement, loss of the central fatty hilum, irregular cortical thickening, increased vascularity and loss of elongated shape are suspicious characteristics for metastatic HPV related squamous cell carcinoma; however, they are nonspecific
- Central necrosis appears as a cystic area within the node, demonstrating an anechoic, or completely black, echo texture enhanced through transmission (AJR Am J Roentgenol 2005;184:1691)
Prognostic factors
- Distant metastasis, although rare, is associated with poor prognosis
Case reports
- 18 year old woman with larynx tumor (Head Neck 2019;41:E59)
- 52 year old man with metastasis to the pleura (J Oral Maxillofac Surg 2018;76:2577)
- 61 year old man with solitary dural metastasis (Head Neck 2014;36:E103)
Treatment
- Resection of primary tumor with or without ipsilateral or bilateral neck dissection
- Radiation therapy or systemic therapy in cases with extranodal extension, positive margins or other high risk associated features such as pT3 or pT4 primary, one positive node > 3 cm or multiple positive nodes, nodal metastasis in levels IV or V, perineural invasion, vascular invasion and lymphatic invasion (National Comprehensive Cancer Network, J Am Soc Cytopathol 2016;5:203)
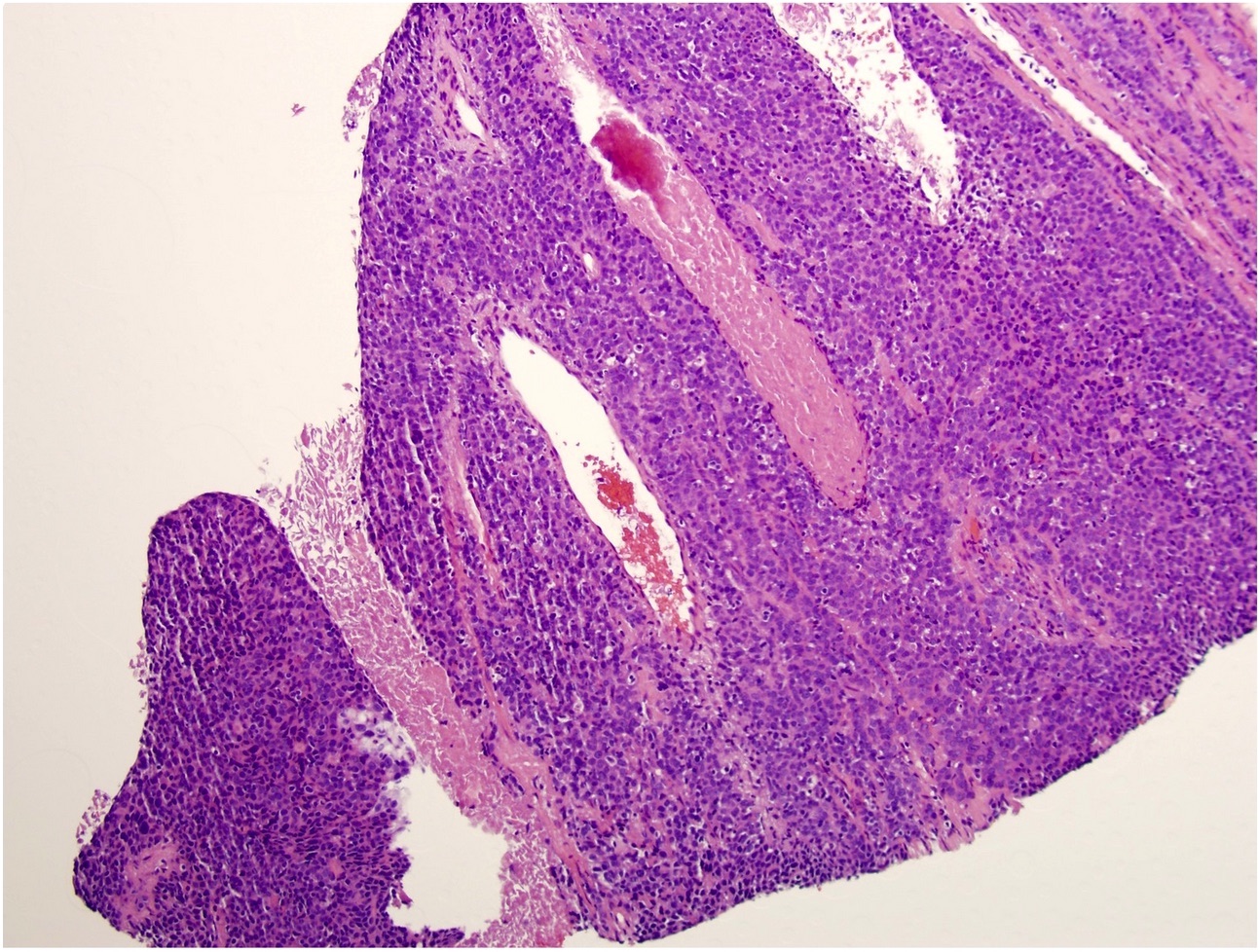
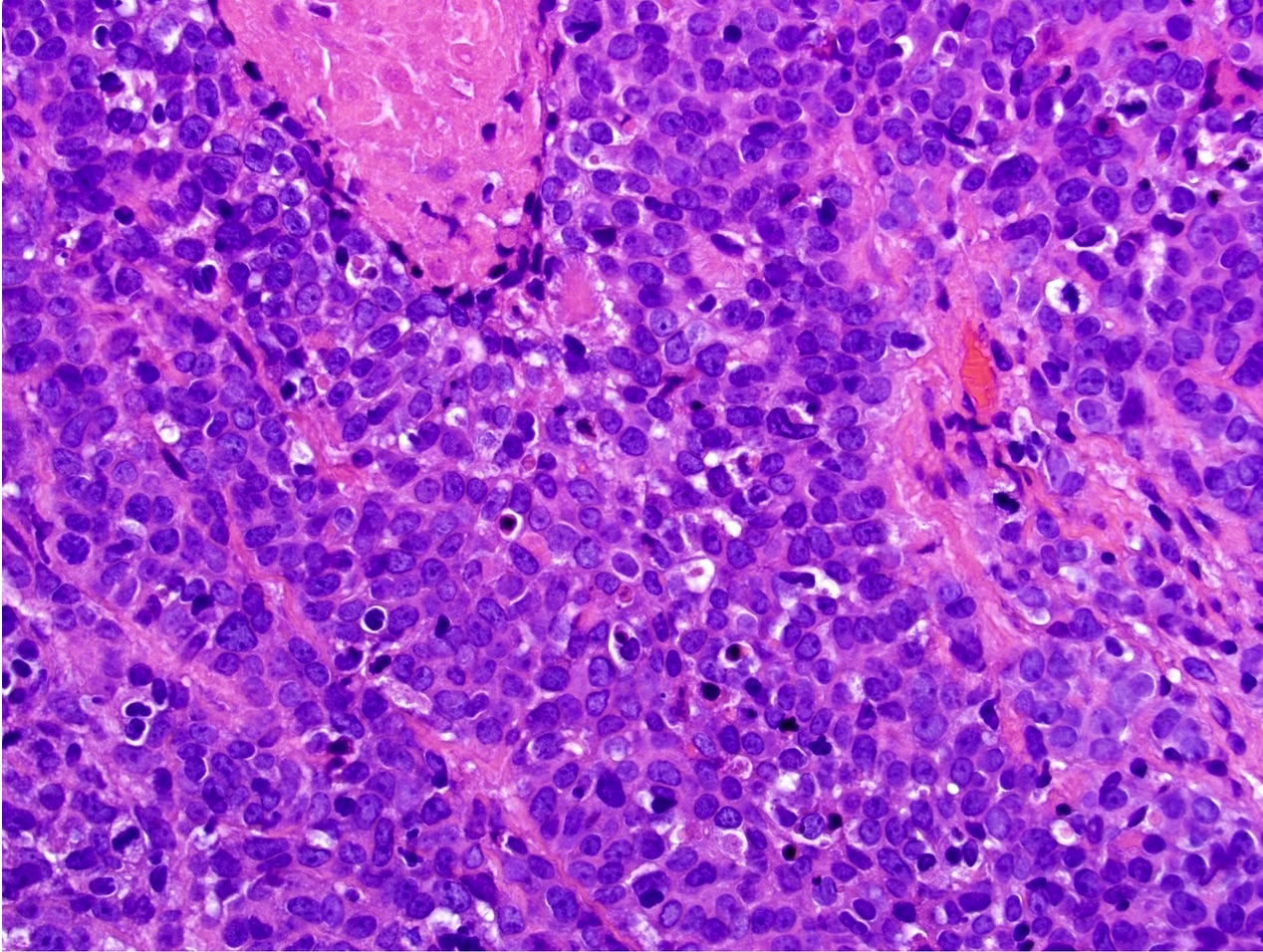
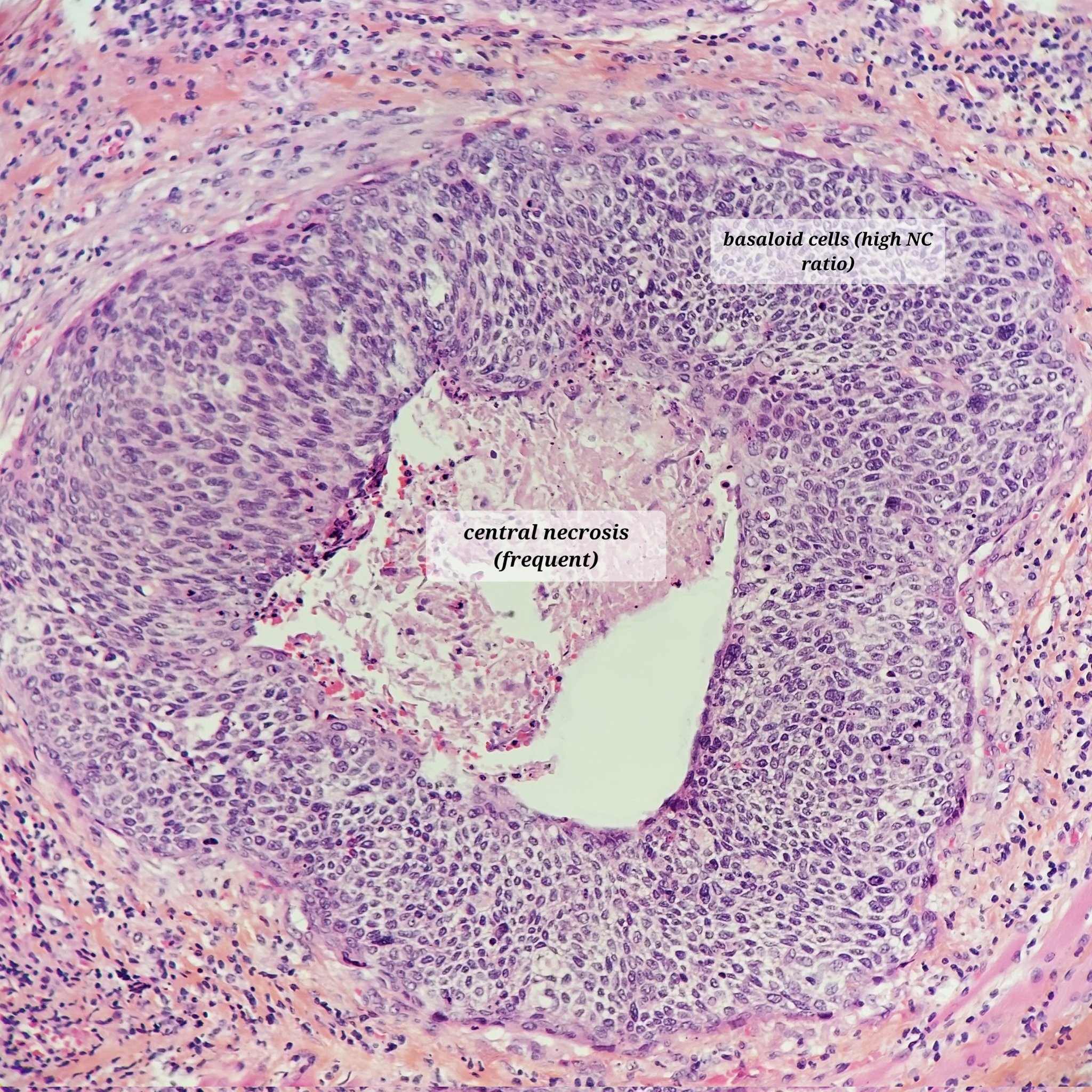
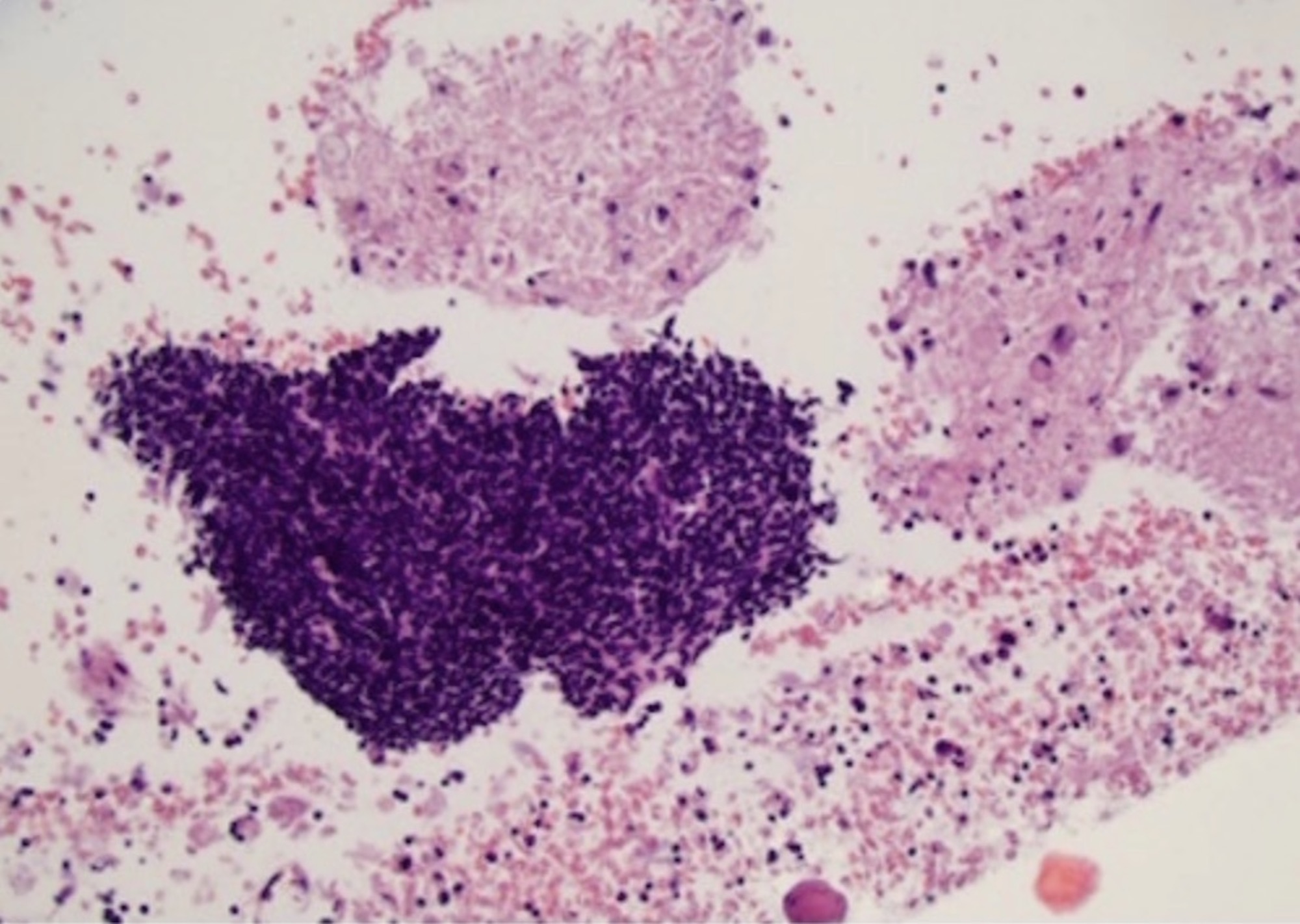
Microscopic (histologic) description
- Variable squamous differentiation including:
- Basaloid features with no squamous differentiation, most common pattern
- Focal keratinization
- Abundant keratinization
- Other morphology types:
- Nonkeratinizing squamous cell carcinoma with maturation
- Hybrid variant
- Keratinizing SCC
- Cystic / microcystic, ciliated
- Papillary SCC
- Adenosquamous SCC
- Spindle cell carcinoma (sarcomatoid)
- Undifferentiated SCC (Am J Surg Pathol 2015;39:1591)
- No tumor grade or differentiation status should be reported (CAP: Human Papillomavirus Testing in Head and Neck Carcinomas [Accessed 24 September 2019])
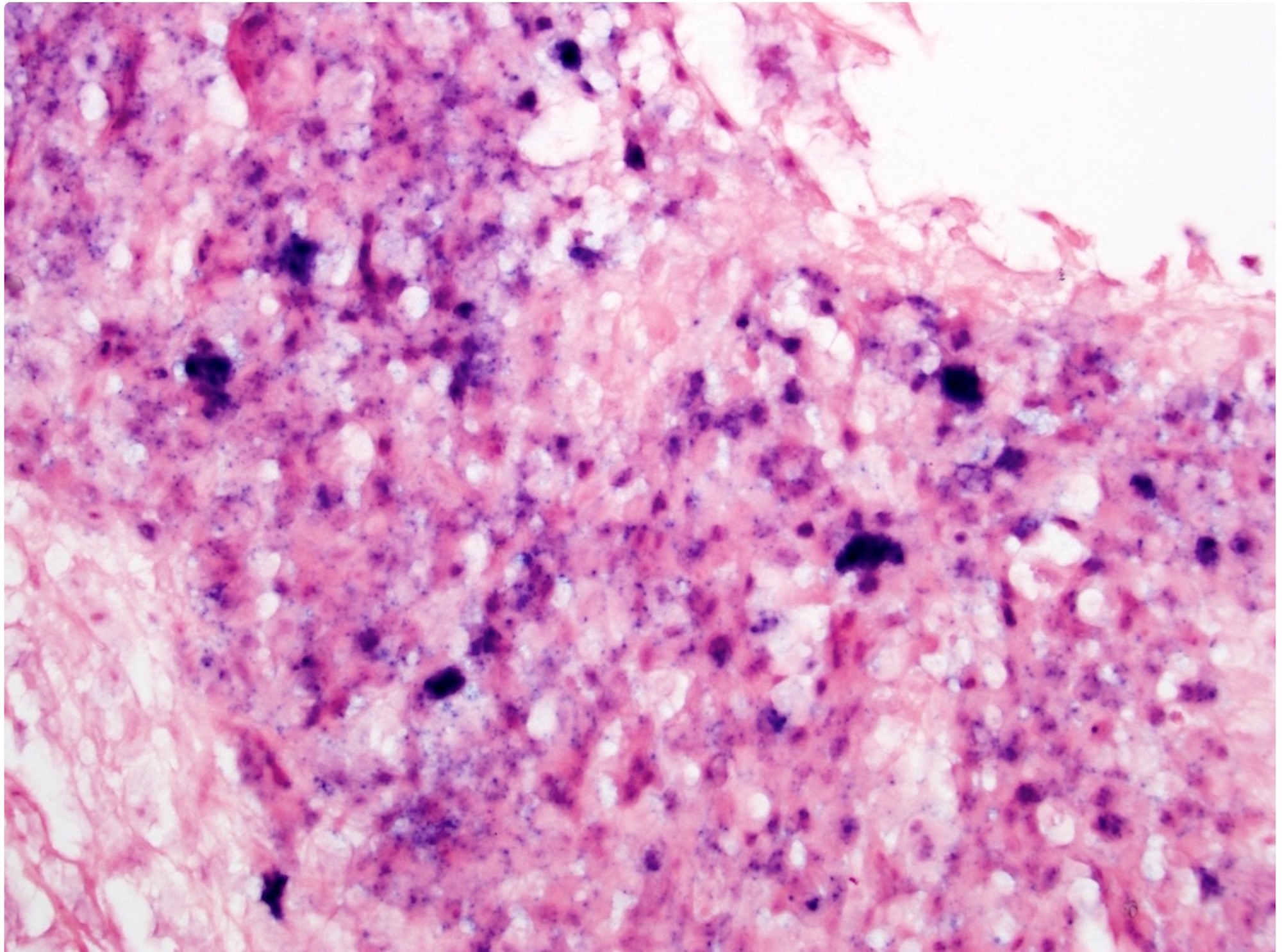
Microscopic (histologic) images
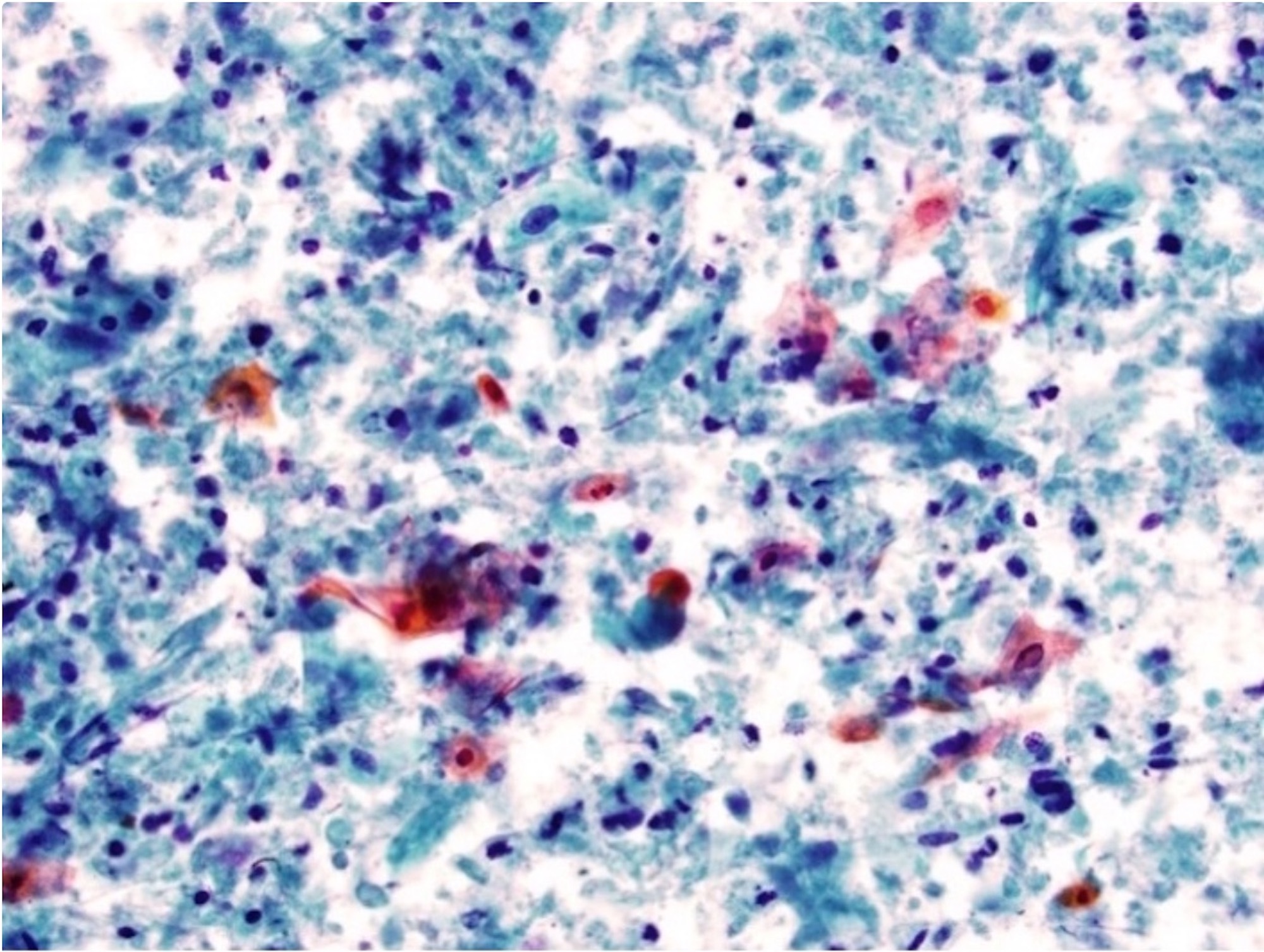
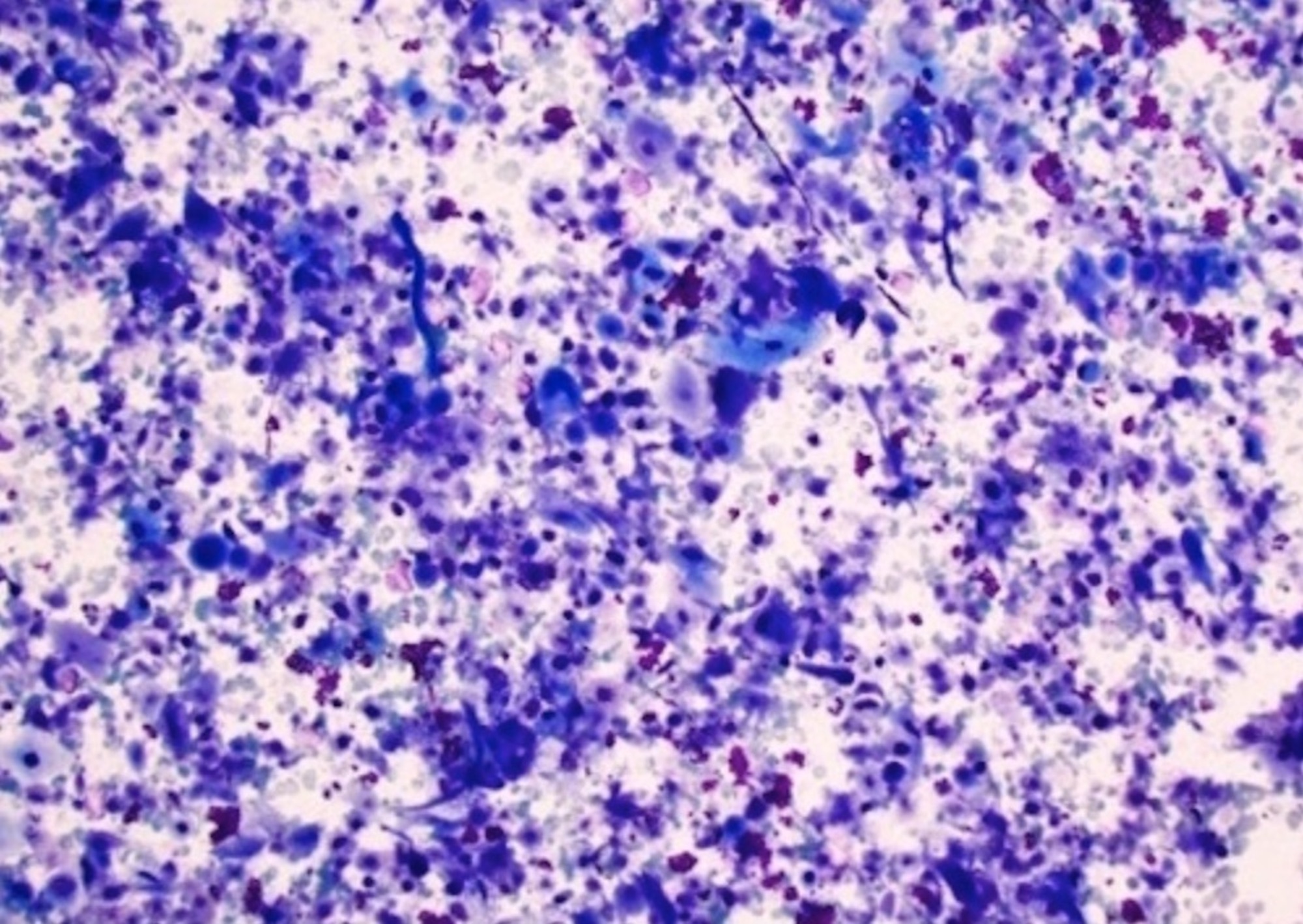
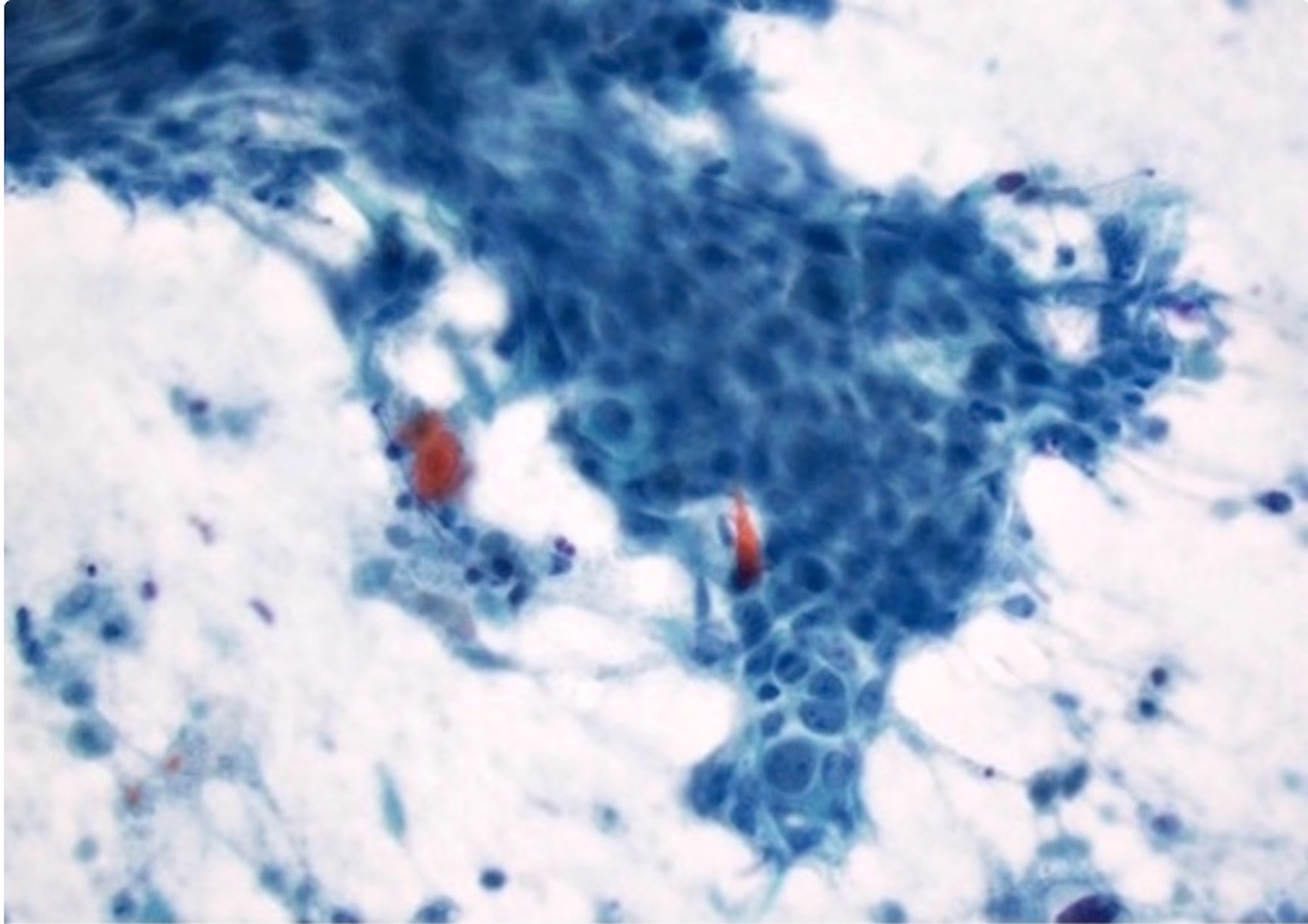
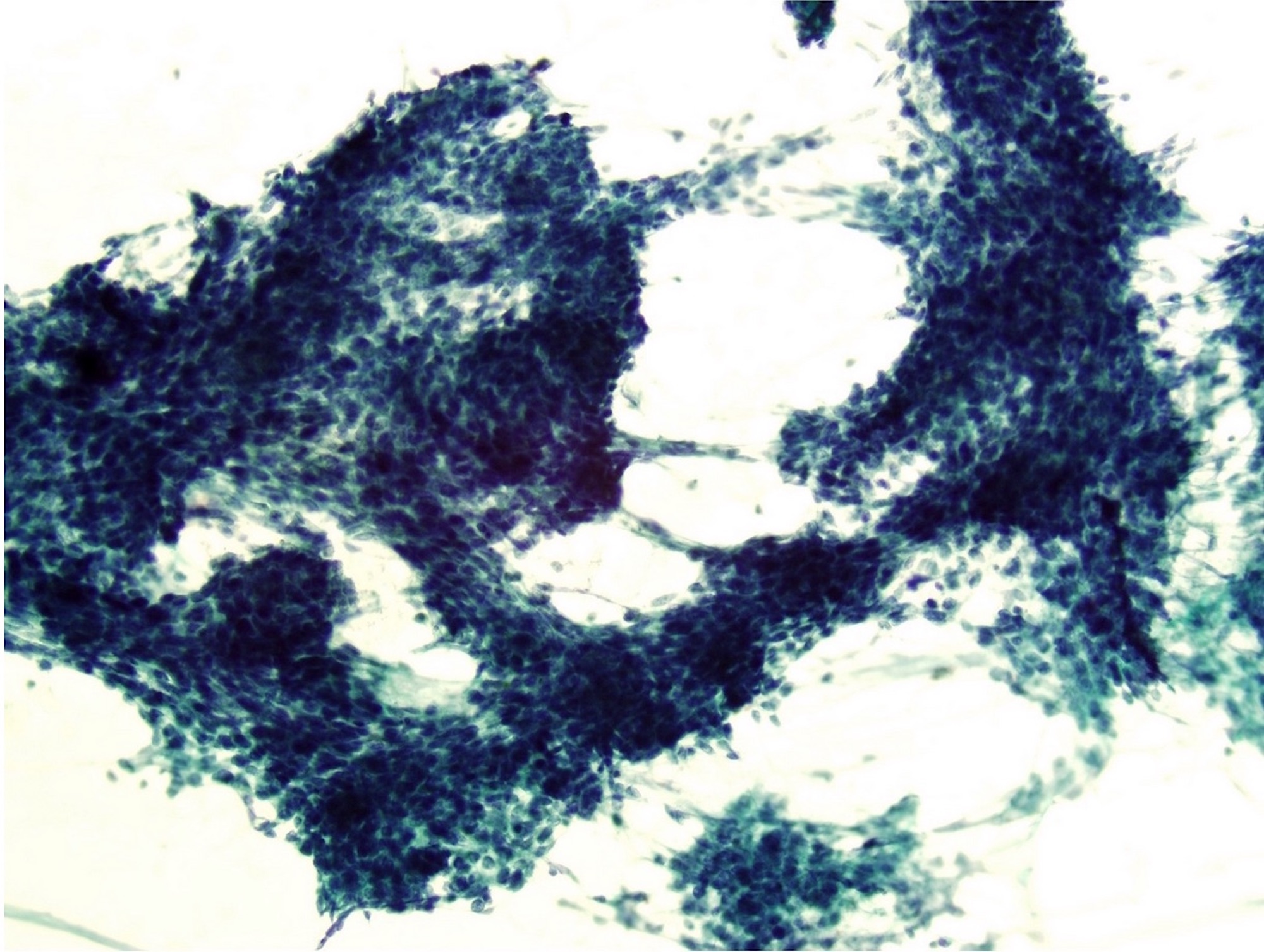
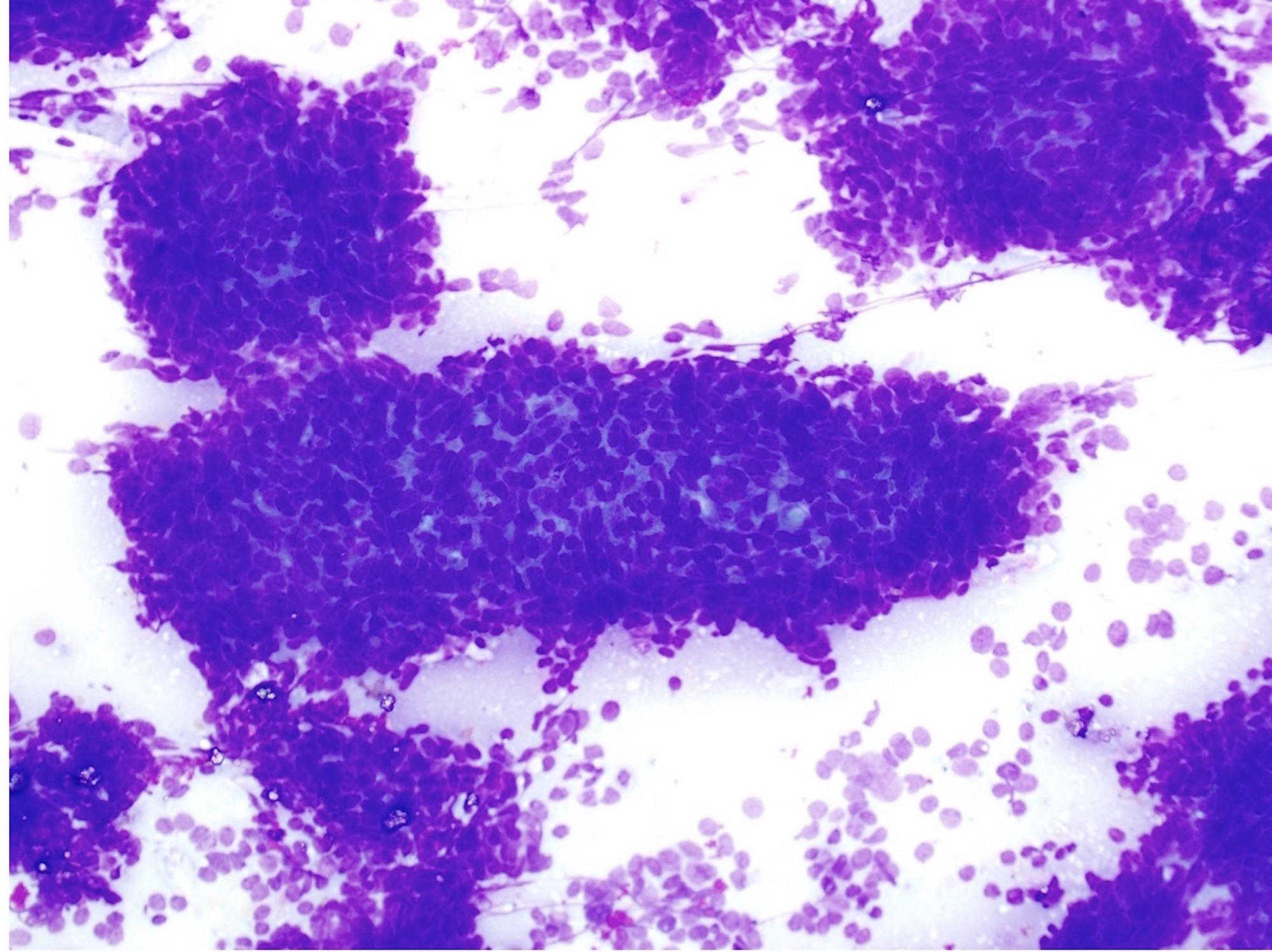
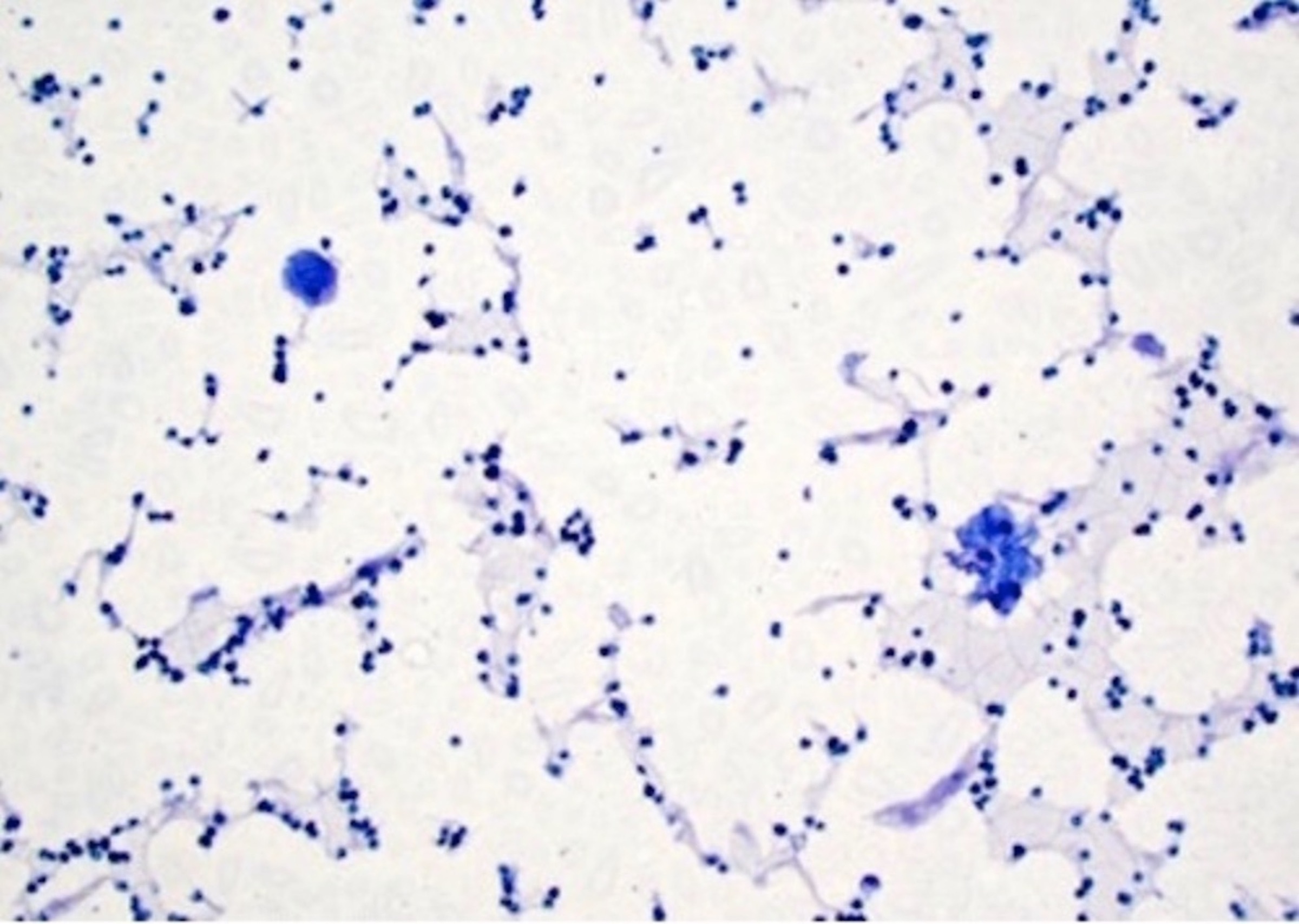
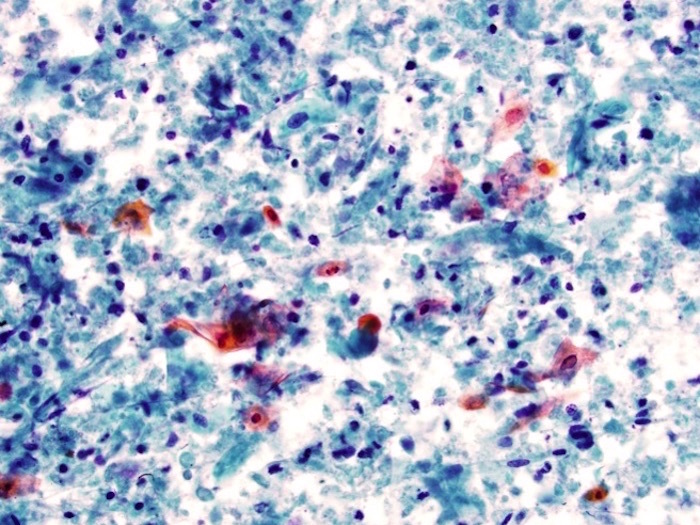
Cytology description
- Non / minimally keratinized squamous cell carcinoma, fragments of basaloid cells with high N/C ratio and hyperchromatic nuclei
- Fragments of cohesive malignant squamous cells with dense cytoplasm
- Variable squamous differentiation, tadpole, snake cells and squamous cells with orangeophilic cytoplasm in Papanicolaou stain and blue in Romanowsky stain, respectively
- Individual keratinized cells with marked pleomorphism
- Necrosis, cystic degeneration and macrophages, common
Cytology images
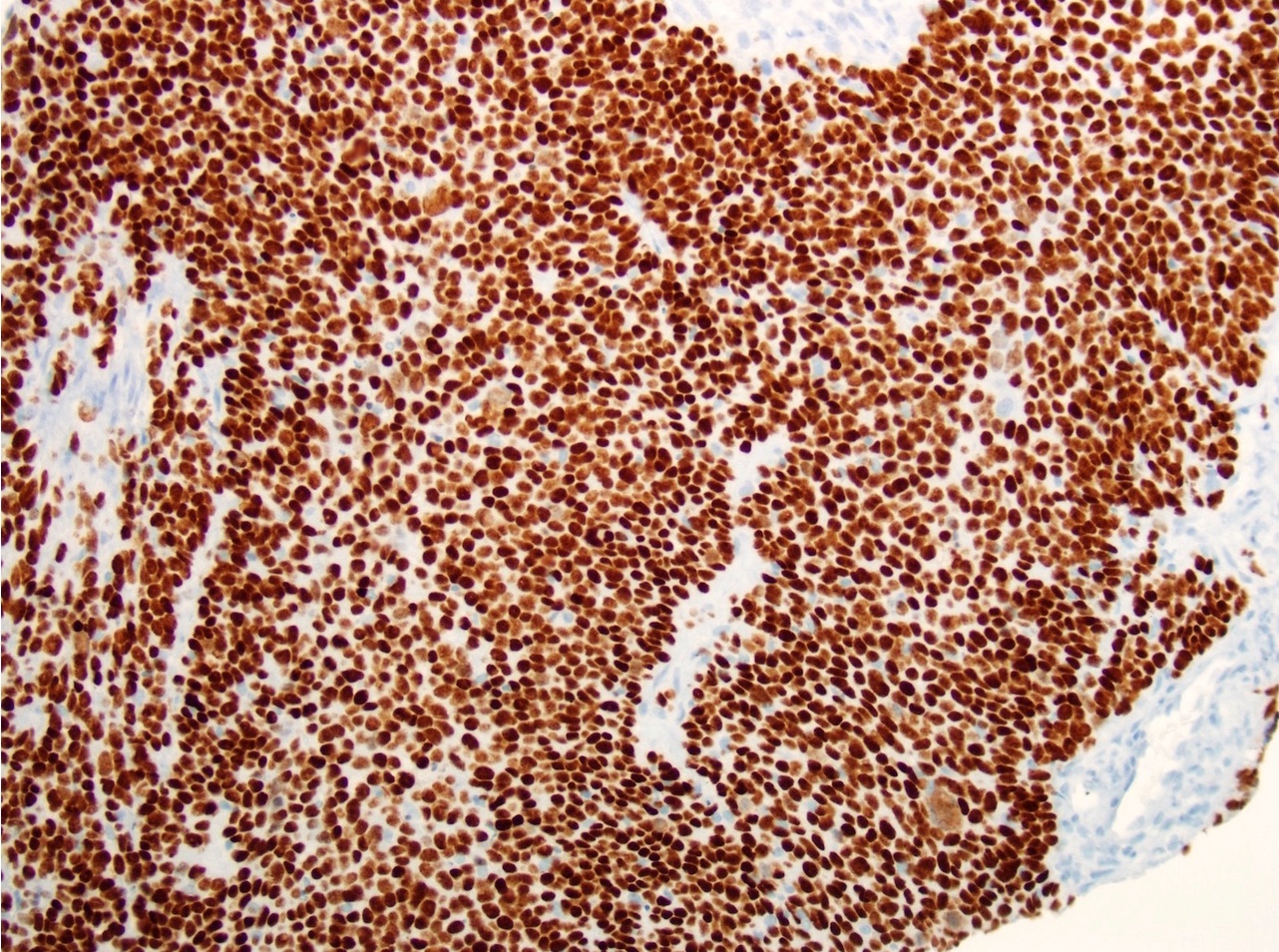
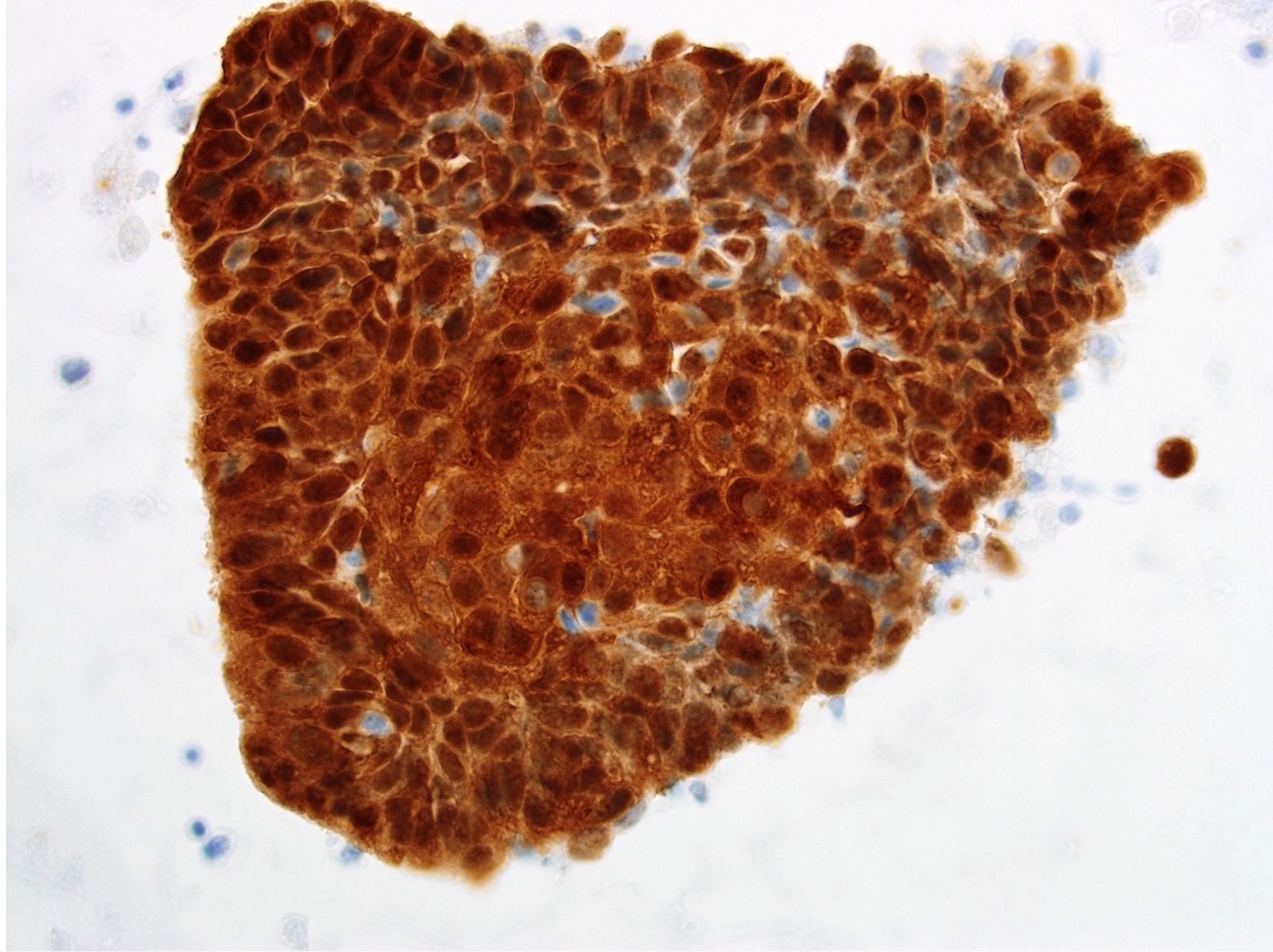
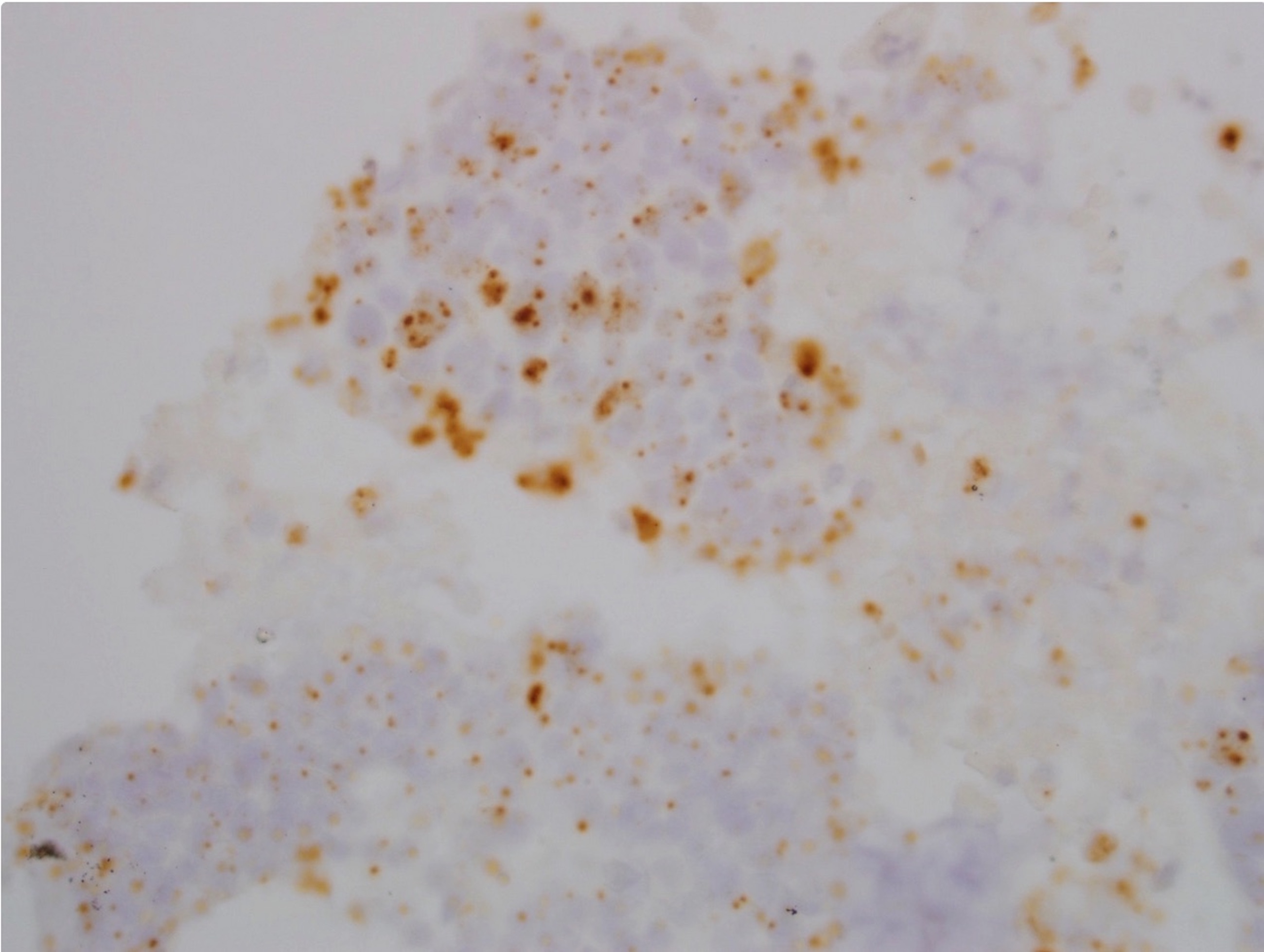
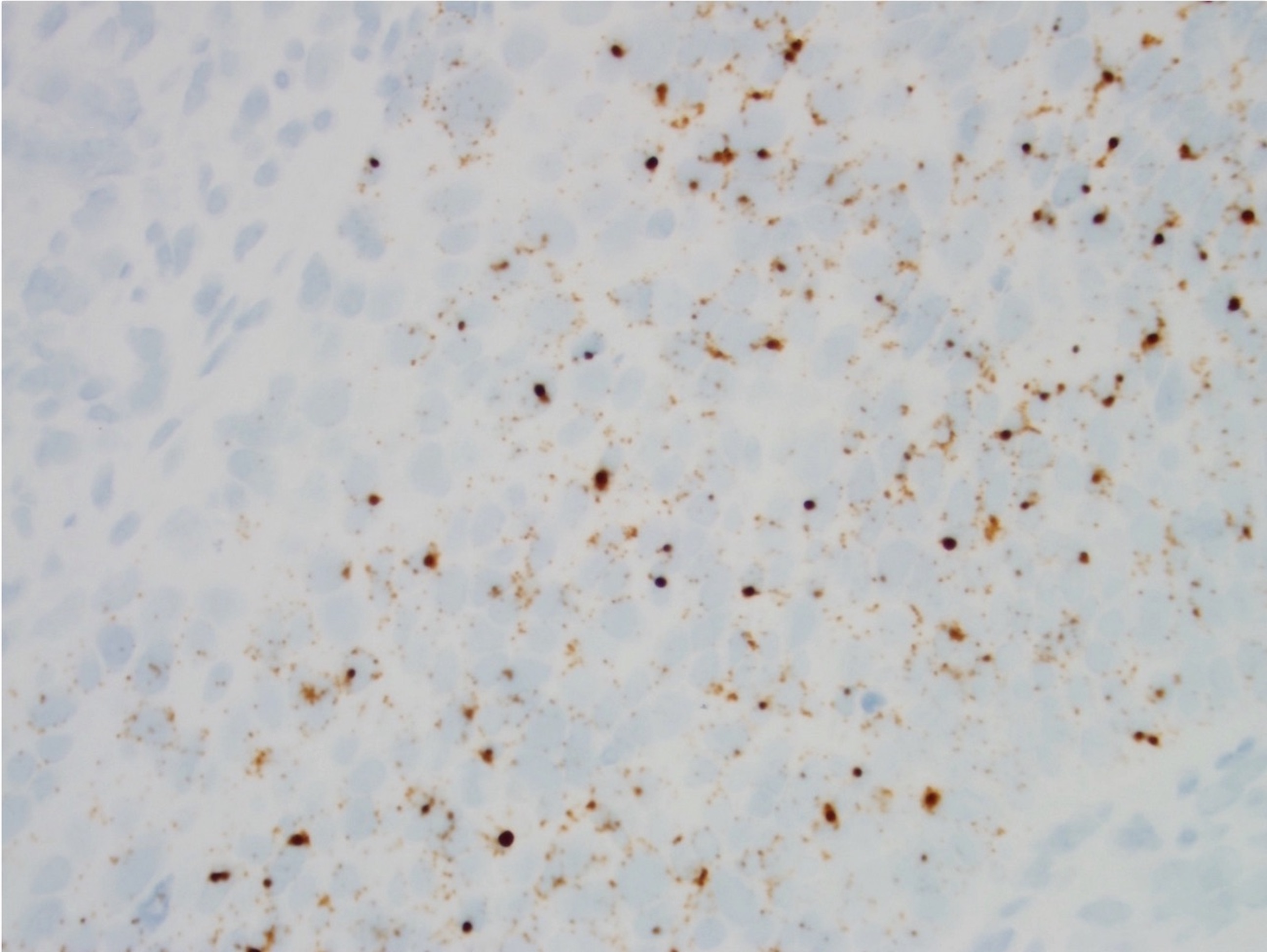
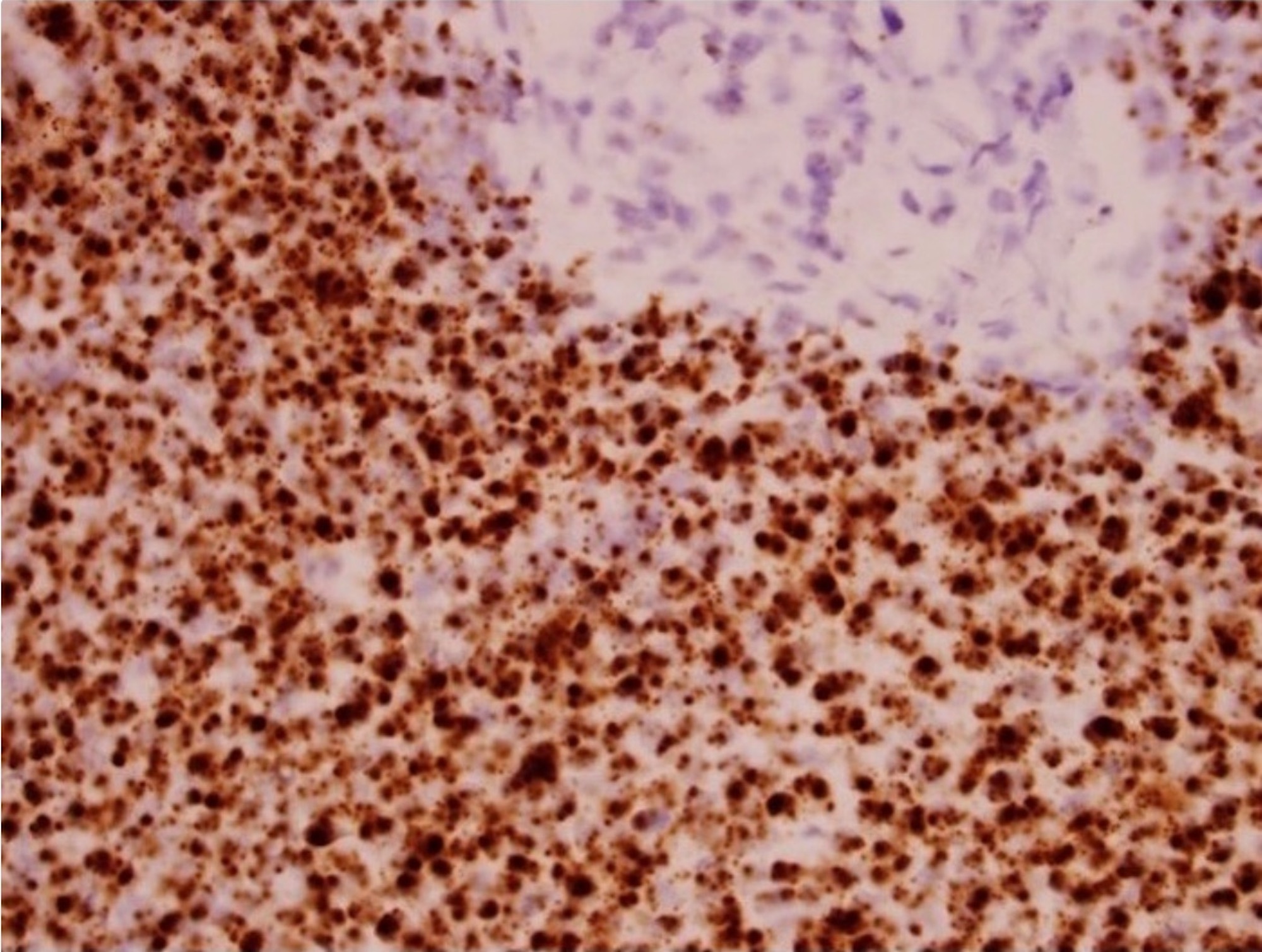
Positive stains
- p16 in ≥ 70% of tumor cells with both nuclear and cytoplasmic staining (Arch Pathol Lab Med 2018;142:559), a surrogate marker
- p40, p63, CK5/6
Molecular / cytogenetics description
- Positive for high risk HPV by hybrid captured II assay, DNA in situ hybridization, RNA in situ hybridization, PCR (J Am Soc Cytopathol 2016;5:203)
- EBER-
Molecular / cytogenetics images
Sample pathology report
- Lymph node, right level II, ultrasound guided fine needle aspiration:
- Metastatic HPV related squamous cell carcinoma (see comment)
- Comment: An immunostain for p16 is positive in 80% of the tumor cells. In situ hybridization for high risk HPV RNA is positive.
Differential diagnosis
- HPV- squamous cell carcinoma of oropharynx
- History of heavy alcohol consumption or chewing / smoking tobacco
- Shows higher degree of squamous differentiation in most cases
- p16-, high risk HPV-
- Metastatic squamous cell carcinoma of skin
- Older patients
- Shows higher degree of squamous differentiation in most cases
- p16-, high risk HPV-
- Lymphoepithelial cyst
- Overall less cellularity
- Unilateral and single cyst
- p16 focally positive, HPV-
- Nasopharyngeal carcinoma
- Presents as keratinizing squamous cell carcinoma or nonkeratinizing squamous cell carcinoma including basaloid squamous cell carcinoma and undifferentiated subtype (El-Naggar: WHO Classification of Head and Neck Tumours, 4th Edition, 2017)
- Syncytial growth pattern, vesicular nuclei with prominent central nucleoli and reactive lymphocytes in stroma
- Usually positive for Epstein-Barr virus (EBV) / Epstein-Barr encoded RNA (EBER)
- p16-, high risk HPV-
- Metastatic squamous cell carcinoma of lung
- Prior relevant clinical history
- Variable squamous differentiation
- p16-, HPV-
- Metastatic HPV related anogenital squamous cell carcinoma including uterine cervix
- Prior relevant clinical history
- Cytomorphologic overlap
- Also p16+ and high risk HPV+
- Adenoid cystic carcinoma, solid type
- Metastatic small cell carcinoma of the lung
- Chest imaging useful to differentiate these two entities
- Same morphology with small cell variant of oropharyngeal carcinoma
- CD56+, chromogranin+, synaptophysin+
- High risk HPV-
- Metastatic large cell neuroendocrine carcinoma
- Sheets and three dimensional fragments of cohesive cells with large pleomorphic nuclei and vesicular chromatin
- Mitoses, molding and necrosis common
- Neuroendocrine markers (chromogranin, synaptophysin, CD56)+, HPV-, p40-
Additional references
Board review style question #1
Board review style answer #1
E. 70% nuclear and cytoplasmic
Comment Here
Reference: HPV related oropharyngeal squamous cell carcinoma
Comment Here
Reference: HPV related oropharyngeal squamous cell carcinoma
Board review style question #2
- Which one of the following statements is true about HPV related oropharyngeal carcinoma?
- Extranodal extension has no impact on treatment
- Distant metastasis is very common
- High risk HPV testing can be performed on primary or metastatic tumor
- The prognosis is poor in most cases
- Tumor differentiation must be reported for all cases
Board review style answer #2
C. High risk HPV testing can be performed on primary or metastatic tumor
Comment Here
Reference: HPV related oropharyngeal squamous cell carcinoma
Comment Here
Reference: HPV related oropharyngeal squamous cell carcinoma
Back to top