Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Rajendran S, Niblock A. Plasma cell gingivitis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/oralcavityplasmacellgingivitis.html. Accessed April 2nd, 2025.
Definition / general
- Plasma cell gingivitis (PCG) is a rare, idiopathic, nonneoplastic plasma cell proliferative disorder of the gingiva
Essential features
- Plasma cell gingivitis is a distinctive pattern of gingival inflammation of unknown etiology
- The inflammatory infiltrate is dense and composed predominantly of nonneoplastic plasma cells
- The most common clinical presentation is diffuse erythema and edema of the gingiva
- While this condition is widely considered to be idiopathic, hypersensitivity reactions to various types of antigens including flavoring agents, spices, mouthwash, tobacco, alcohol, chewing gum, candy and medications have been previously proposed in the literature (J Periodontol 1971;42:709, CDS Rev 1995;88:22, Br Dent J 1990;168:115, Oral Surg Oral Med Oral Pathol 1992;73:690, SADJ 2008;63:394)
- Therapeutic strategies are based mainly on symptom control and removal of the offending substance
- Surgical intervention has proven successful in severe cases (BMJ Case Rep 2015;2015:bcr2014207013, Int J Surg Case Rep 2022;93:106998)
Terminology
- Atypical gingivostomatitis
- Idiopathic gingivitis / gingivostomatitis
- Allergic gingivitis / gingivostomatitis
- Plasma cell gingivitis / gingivostomatitis
Epidemiology
- Based on limited data in the literature, the average age of onset is 45 years and there is a higher prevalence in males (J Clin Med 2021;10:830)
Sites
- This condition typically affects the gingiva but additional sites may be involved, including lips, tongue and larynx
Pathophysiology
- There is a diffuse and dense infiltrate of polyclonal plasma cells in the superficial lamina propria
- Plasma cells show no cytological atypia
- No nodular architecture is seen
- The overlying squamous epithelium is hyperplastic but there is no disruption of normal architecture
- Plasma cells show no affinity for vasculature
- References: J Clin Med 2021;10:830, J Indian Soc Periodontol 2022;26:434
Etiology
- Unclear
- This condition may arise in the context of a hypersensitivity reaction to environmental antigens
- Previously reported antigens include flavoring agents, spices, mouthwash, tobacco, alcohol, chewing gum, candy and medications
- Upon follow up of cases in the literature, there is no increased rate of myeloma, monoclonal gammopathy of undetermined significance (MGUS) or amyloid
- Due to the rarity of the condition and relatively small number of cases in the literature, it is not possible to classify the full extent of this condition and confirm if this is a purely localized phenomenon or if infiltration exists elsewhere
- References: J Clin Med 2021;10:830, J Indian Soc Periodontol 2022;26:434
Clinical features
- Most commonly presents as diffuse swelling and redness of the gingiva
- Tenderness and bleeding have been frequently reported
- Ulceration is rare and several case reports have described alveolar bone loss (BMJ Case Rep 2015;2015:bcr2014207013, J Oral Maxillofac Pathol 2021;25:S54, J Indian Soc Periodontol 2013;17:527)
Diagnosis
- Diagnosis is made by clinicopathological correlation
- Clinical history of antigen exposure
- Characteristic clinical features of erythema and swelling of the gingiva
- Biopsy of the gingiva shows a diffuse but benign infiltrate of plasma cells in the lamina propria
- References: J Clin Med 2021;10:830, J Indian Soc Periodontol 2022;26:434
Prognostic factors
- Type of offending stimulus
- The exact etiology of plasma cell gingivitis is uncertain but certain antigens such as flavoring agents, spices and chewing gum have been previously reported to be associated with severe symptoms
- Extent of stimulus exposure
- Condition may resolve following removal of offending stimulus
- Cases that have been followed up in the literature show no increased incidence of myeloma, MGUS or amyloid
- References: J Clin Med 2021;10:830, J Indian Soc Periodontol 2022;26:434
Case reports
- 17 year old girl with severe alveolar bone loss related to herbal toothpaste (J Indian Soc Periodontol 2013;17:527)
- 18 year old man with cheilitis that was managed by gingivectomy (Case Rep Dent 2019;2019:2939126)
- 64 year old man treated with photobiomodulation with no evidence of recurrence after 5 years (Case Rep Dent 2022;2022:2992656)
Treatment
- Treatment is based mainly on symptom control and removal of the offending agent
- Patients are advised to keep a complete dietary history and avoid potential allergens
- Allergy testing and elimination diet may prove helpful
- Other strategies including topical and systemic immunosuppressive therapies, antibiotics, radiation and tissue destruction by liquid nitrogen, carbon dioxide laser and electrocoagulation have had variable results in the literature
- Surgical treatments including gingivectomy may be effective in severe cases
- References: J Clin Med 2021;10:830, J Indian Soc Periodontol 2022;26:434
Clinical images
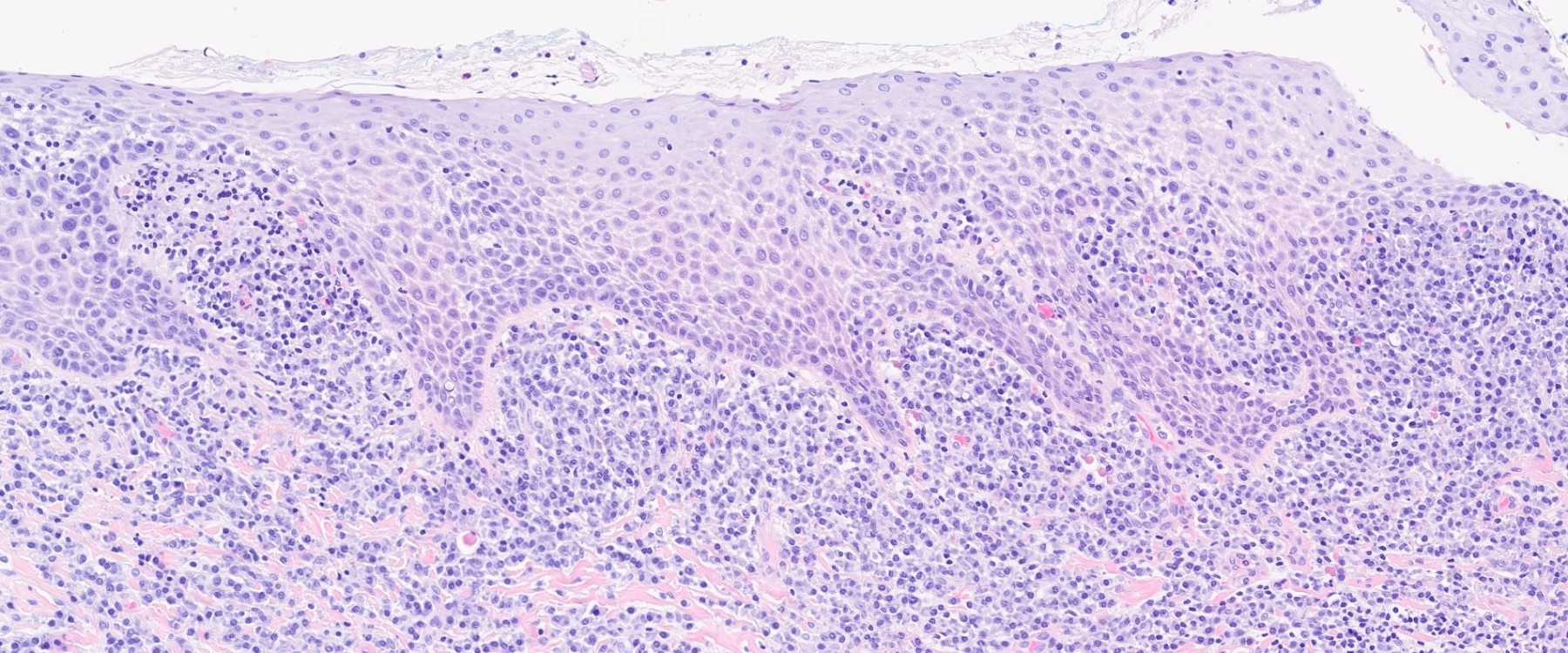
Microscopic (histologic) description
- Diagnostic criteria: nonneoplastic proliferation of predominantly plasma cells
- Histology shows hyperplastic and spongiotic squamous epithelium
- Ulceration may rarely be seen
- Juxtaepithelial tissues contain a dense inflammatory infiltrate rich in mature plasma cells
- Granulomatous inflammation, blister formation and vasculitis are absent
- References: J Clin Med 2021;10:830, J Indian Soc Periodontol 2022;26:434
Microscopic (histologic) images
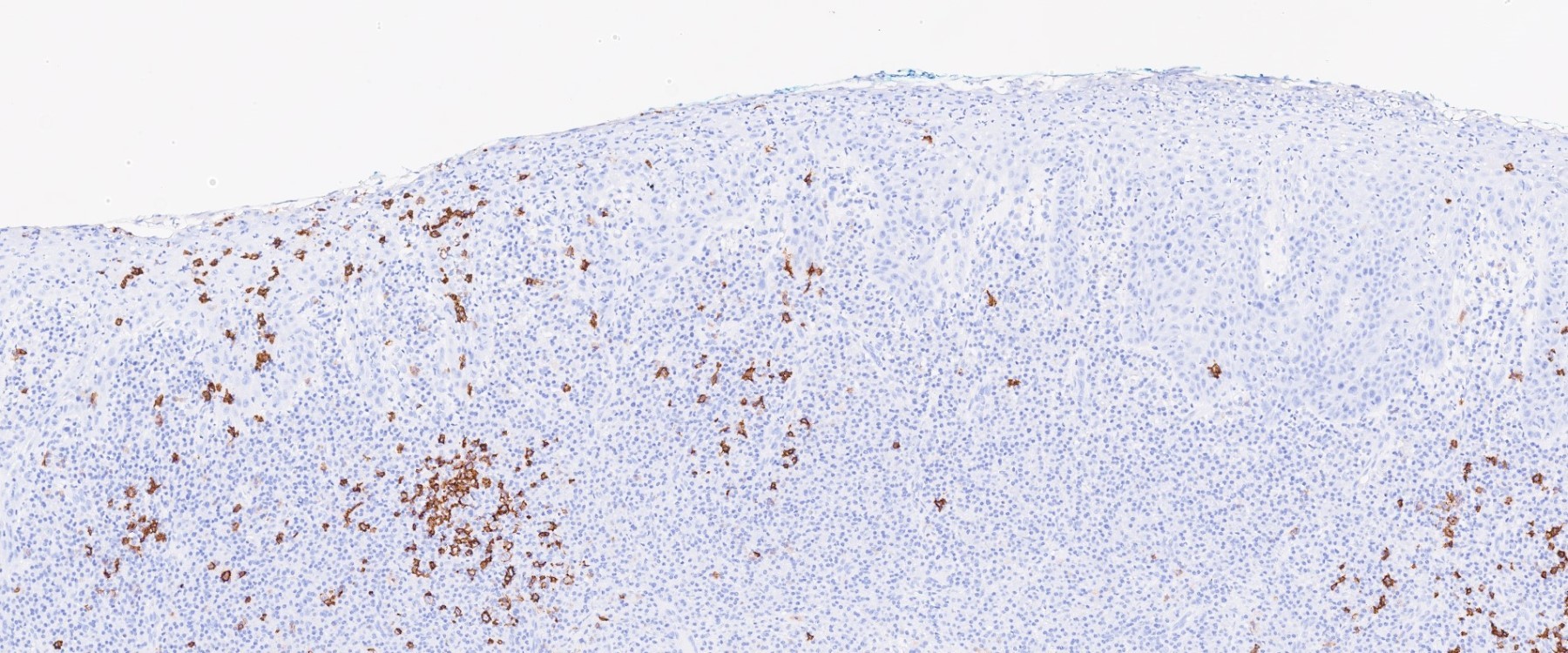
Negative stains
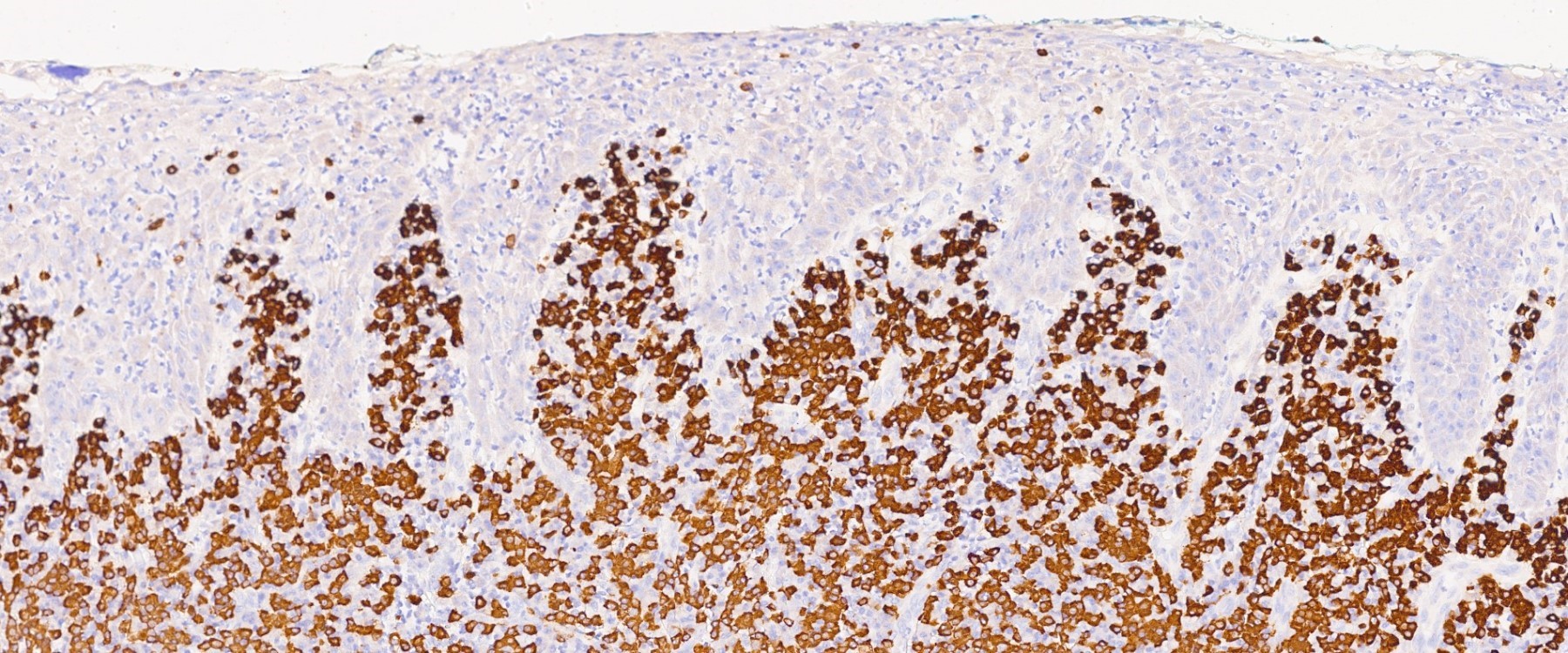
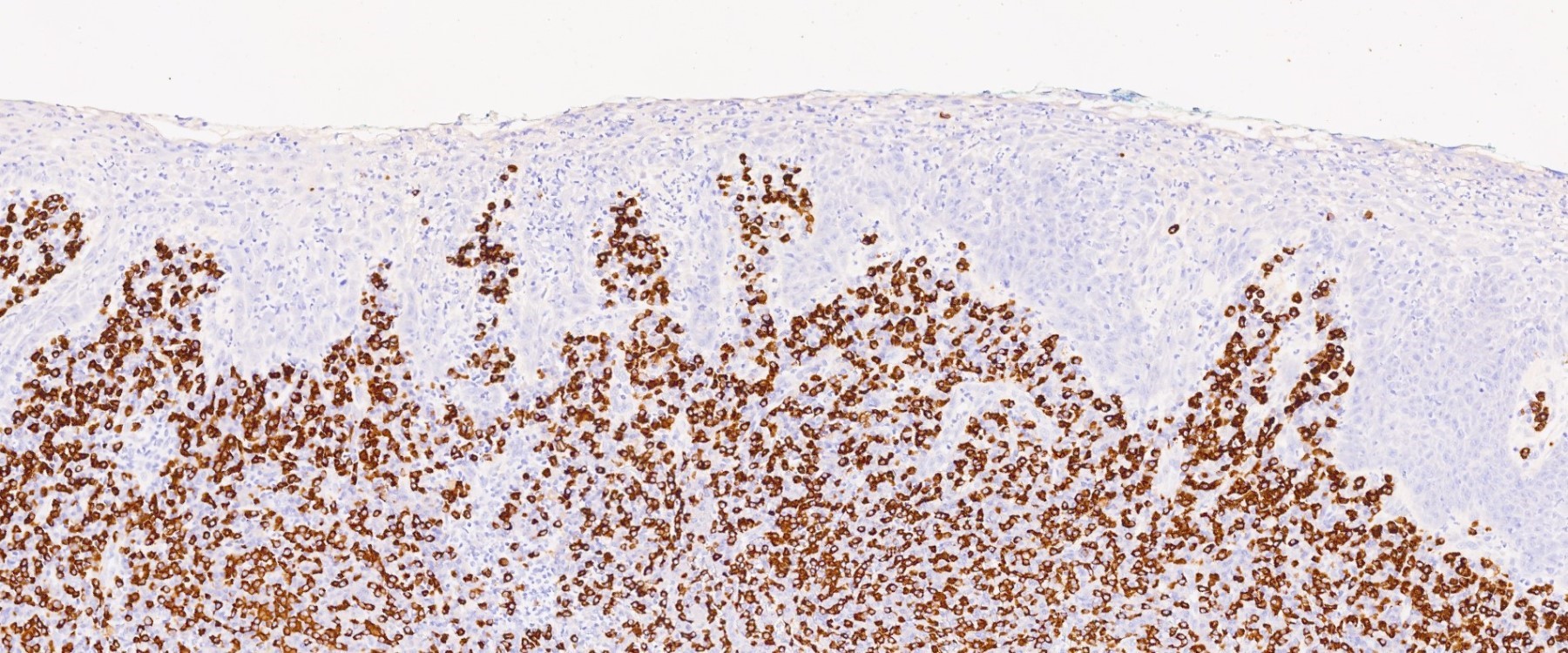
Sample pathology report
- Gingiva, biopsy:
- Plasma cell gingivitis (see comment)
- Hyperplastic and spongiotic squamous epithelium
- Dense and diffuse proliferation of mature plasma cells in the superficial lamina propria, in close juxtaposition with the squamous epithelium.
- Kappa and lambda immunohistochemistry or ISH shows a polyclonal plasma cell population.
- Plasma cells are negative for CD56.
- Relevant negative findings: No granulomas, spirochete infection, vasculitis or blister formation.
- Comment: The differentials include an allergic or hypersensitivity phenomenon (plasma cell gingivitis), response to medication or other agents (lichenoid reaction) and a nonspecific reaction to injury. Of these, plasma cell gingivitis is the most likely. Does the clinical impression support this interpretation?
Differential diagnosis
- Multiple myeloma:
- Clonal plasma cell population and 70% of cases are positive for CD56
- Solitary plasmacytoma:
- Clonal plasma cell population
- Chronic hyperplastic gingivitis:
- Absence of diffuse plasma cell infiltrate
- Granulomatous gingivitis:
- Absence of diffuse plasma cell infiltrate
- Granulomas are present
- Spirochete infection:
- Diffuse plasma cell infiltrate
- Spirochete infection will be positive with Treponema pallidum immunohistochemistry
Additional references
Board review style question #1
Board review style answer #1
C. CD20-, CD138+, CD56-. Plasma cell gingivitis is gingival inflammation composed predominantly of a population of nonneoplastic plasma cells. These cells show polyclonal pattern of staining with kappa and lambda. CD138 would be positive in both nonneoplastic and neoplastic plasma cell populations. Answer B is incorrect because CD20 and CD68 are negative in plasma cells. CD20 is a B cell marker that is retained on mature B cells until plasma cell differentiation, so it is not expressed by mature plasma cells. CD68 highlights histiocytes which would be positive in granulomatous gingivitis. Answer A is incorrect because CD56 is positive in 70% of neoplastic plasma cells and negative in nonneoplastic plasma cells. Answer D is incorrect because, in a normal or reactive plasma cell population, the ratio of kappa to lambda light chains is ~2:1. Immunoglobulins from a neoplastic (clonal) plasma cell population contain either kappa or lambda light chains. Light chain restriction or monoclonality can therefore be used to distinguish between reactive / nonneoplastic and neoplastic plasma cell proliferations.
Comment Here
Reference: Plasma cell gingivitis
Comment Here
Reference: Plasma cell gingivitis
Board review style question #2
Which antibodies could be used to highlight the plasma cells in plasma cell gingivitis?
- CD20 and CD3
- CD56
- Cyclin D1
- MUM1 / IRF4 and CD138
Board review style answer #2
D. MUM1 / IRF4 and CD138 are positive in both neoplastic and nonneoplastic plasma cell populations. Answers B and C are incorrect because CD56 and cyclin D1 are expressed in neoplastic plasma cells. Overexpression of cyclin D1 by either t(11;14) (most common) or gene amplification is a well recognized oncogenic event in both mantle cell lymphoma and myeloma (Indian J Med Paediatr Oncol 2013;34:283). CD56 is positive in 70% of neoplastic plasma cells and is usually negative in nonneoplastic plasma cells (Histopathology 2004;44:375). Answer A is incorrect because CD20 and CD3 are usually negative in plasma cells. CD20 is a B cell marker that is retained on mature B cells until plasma cell differentiation, so it is not expressed by mature plasma cells. CD3 is a T cell marker and is typically not expressed by B cells and plasma cells or their neoplastic counterparts.
Comment Here
Reference: Plasma cell gingivitis
Comment Here
Reference: Plasma cell gingivitis