Table of Contents
Definition / general | Prognostic factors | Case reports | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Differential diagnosis | Board review style question #1 | Board review style answer #1Cite this page: Pernick N. Oral mucosal melanoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/oralcavitymelanoma.html. Accessed April 1st, 2025.
Definition / general
- Rare; annual incidence of 1.2 cases per 10 million; more common in Japanese, black Africans, Native Americans and Hispanics
- Median age 61 years, 78% men
- Differs from cutaneous melanoma due to lack of association with sun damage, family history or atypical nevi and difference in prognostic factors
- Nodal and distant metastases are common
- References: Am J Surg Pathol 2001;25:782, Am J Surg Pathol 2002;26:883
Prognostic factors
- Extremely poor prognosis, with median survival 2 - 3 years; some lower grade tumors without vascular invasion had median survival of 8 years
- Poor prognostic factors: vascular invasion, polymorphous tumor cell population and necrosis
- No prognostic value: tumor thickness, ulceration and level of invasion
Case reports
- 17 year old girl with tender lesion of hard palate (Arch Pathol Lab Med 2002;126:1110)
- 47 year old man with tumor after low dose radiation therapy for lichen planus (Arch Pathol Lab Med 1985;109:290)
- 71 year old man with multiple firm left submandibular swellings for two months (Case #419)
Gross description
- Mucosa covering maxillary bone (62%), labial mucosa (13%) and lower gingiva (8%)
- Usually flat, erythematous or pigmented, less commonly presents as a mass
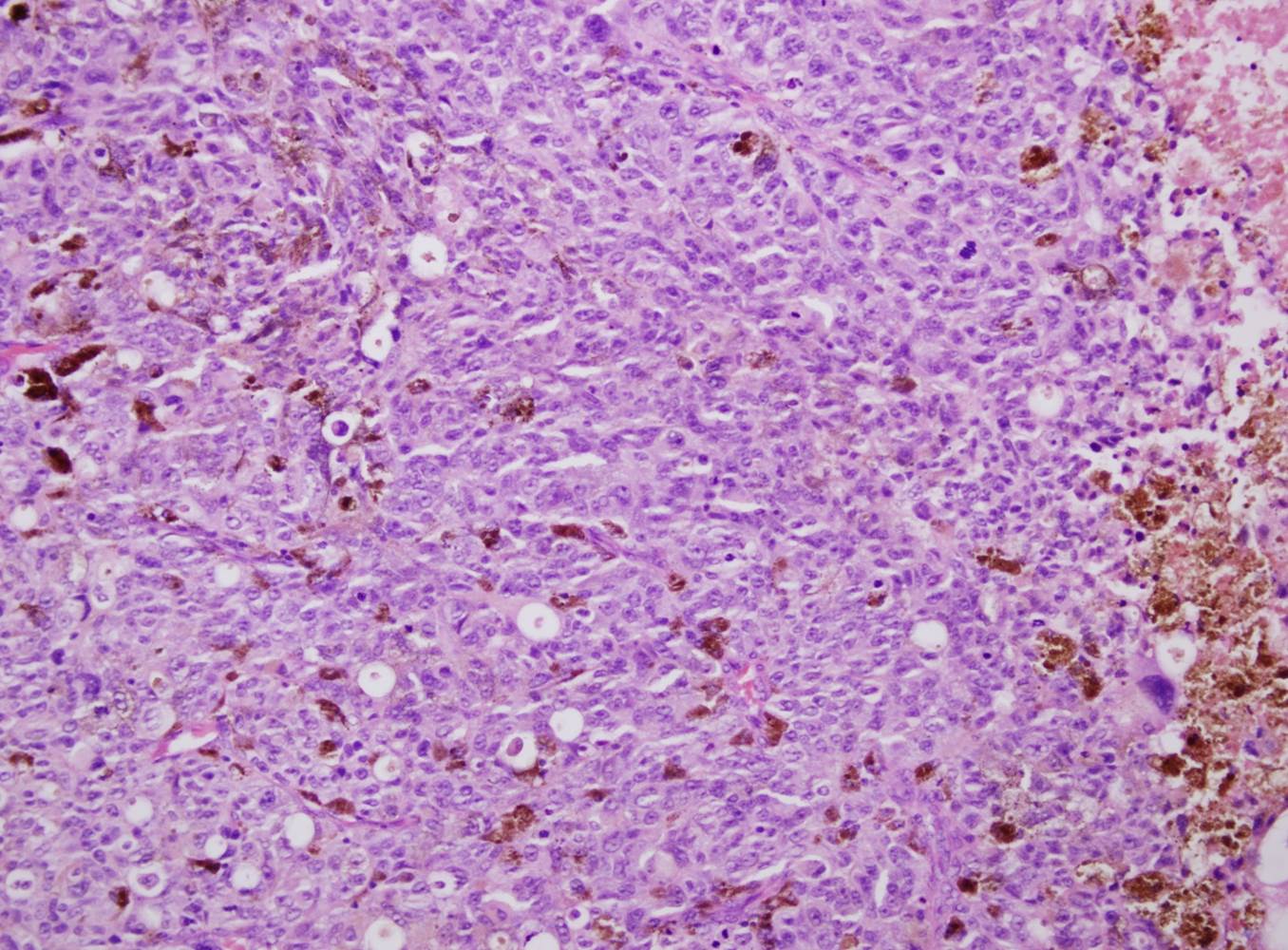
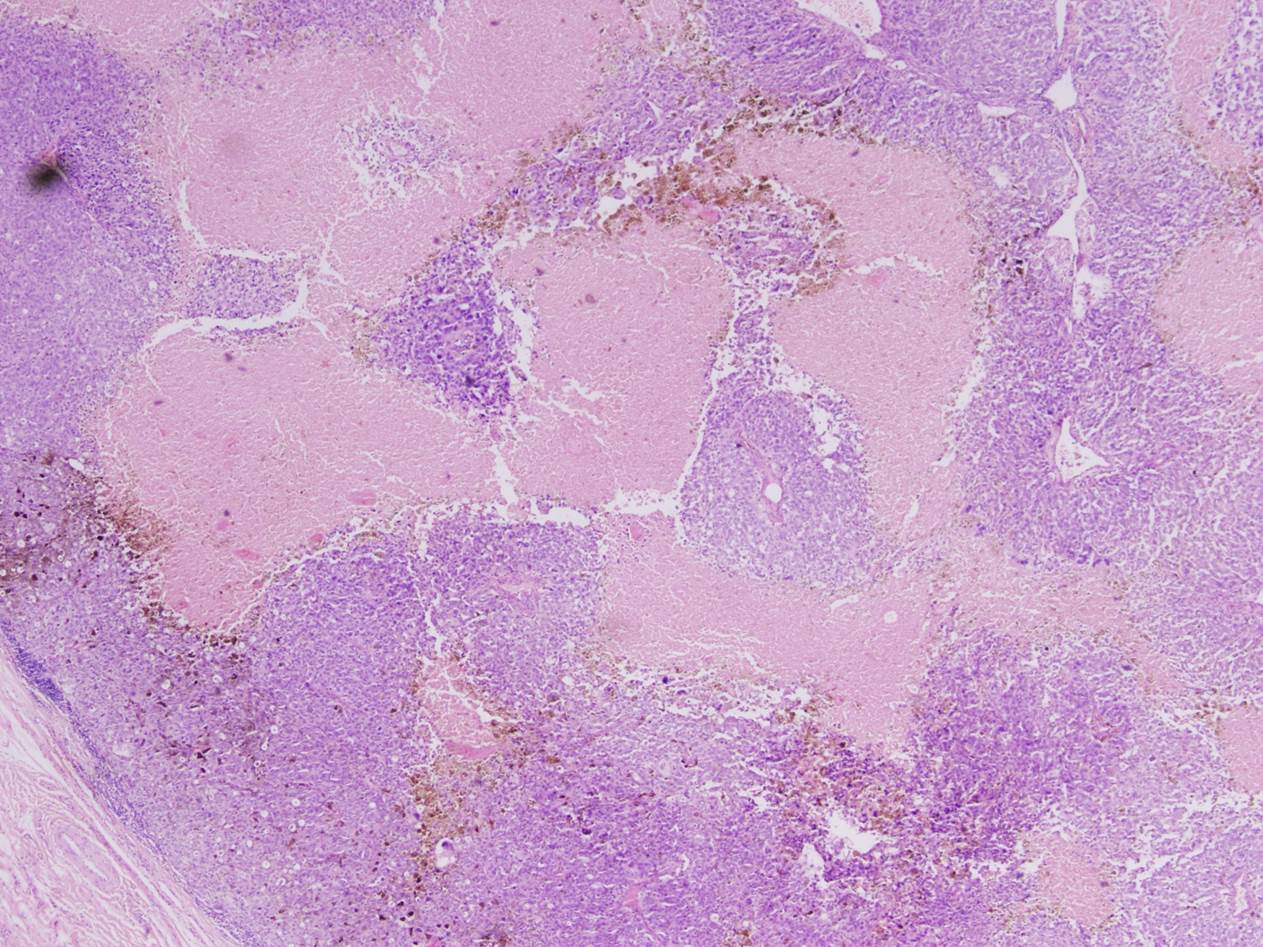
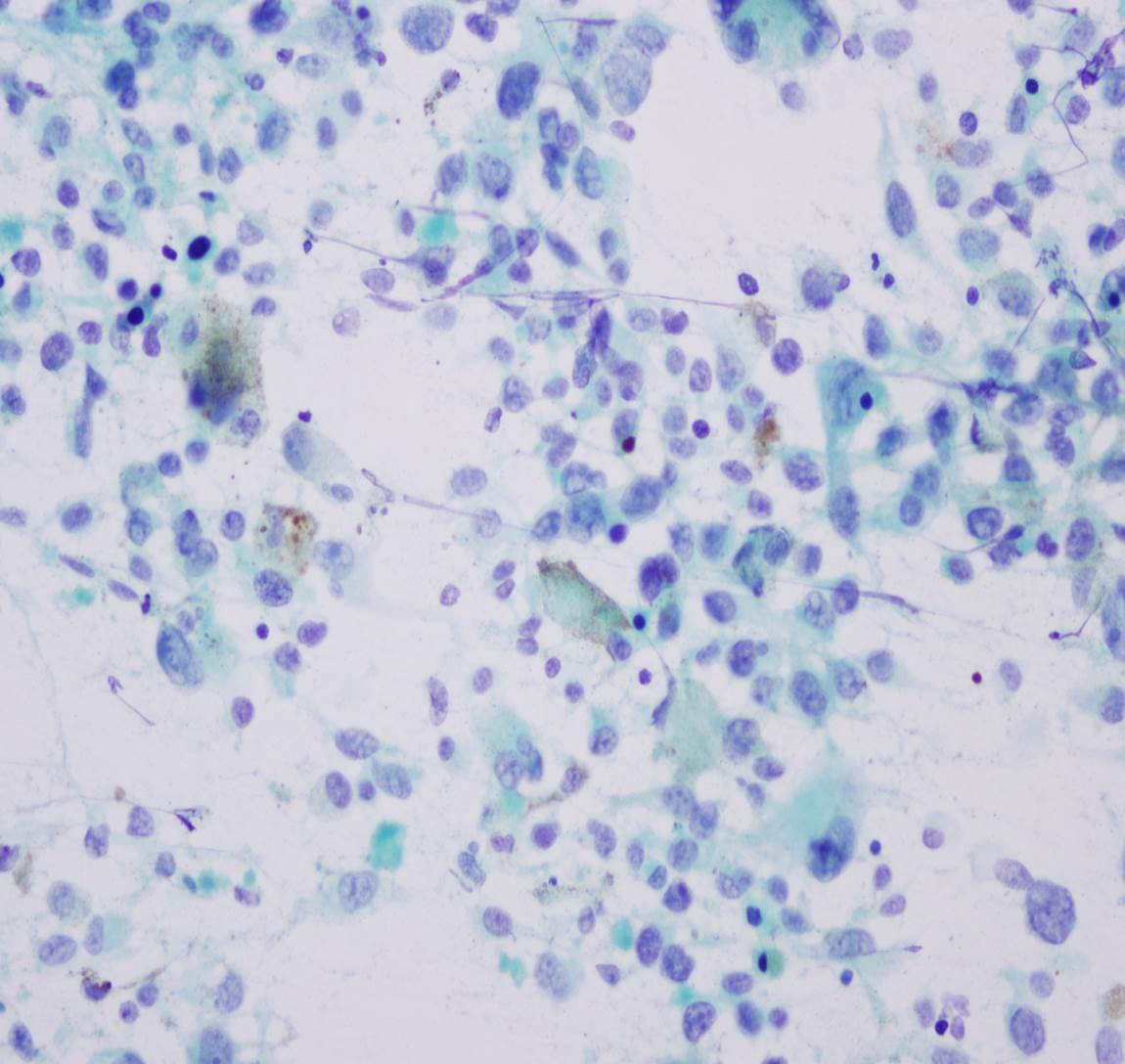
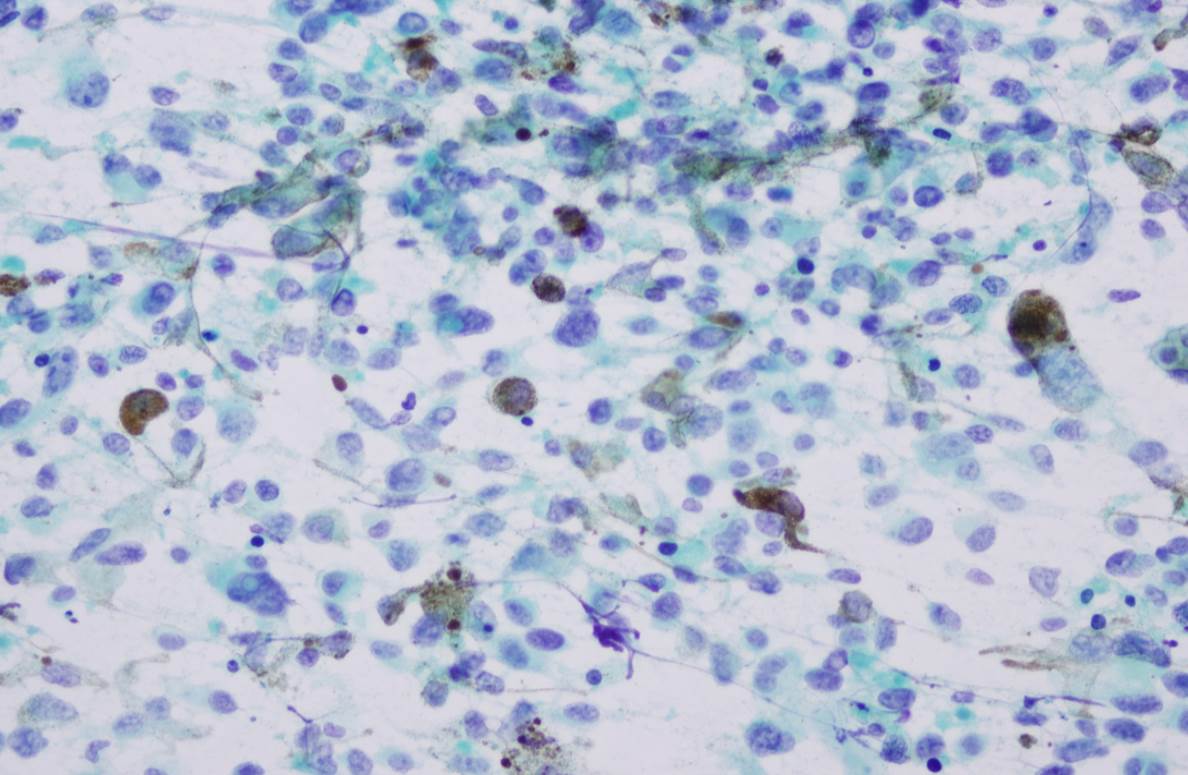
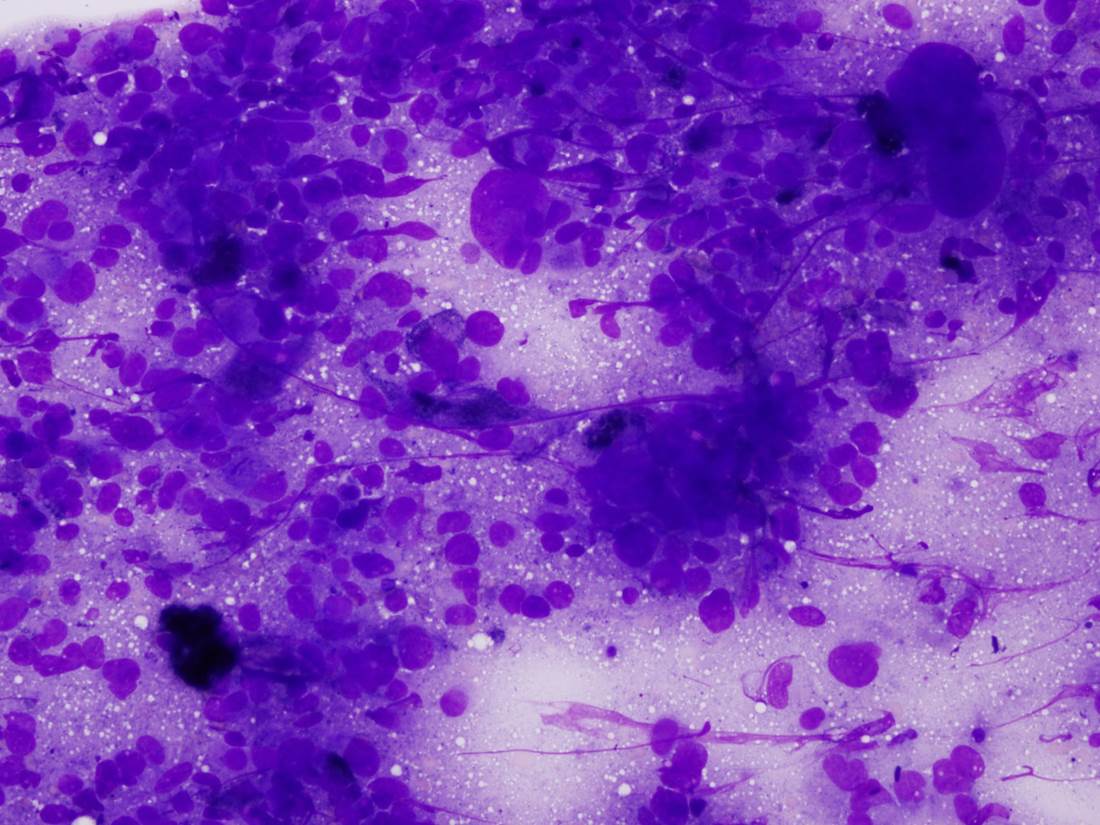
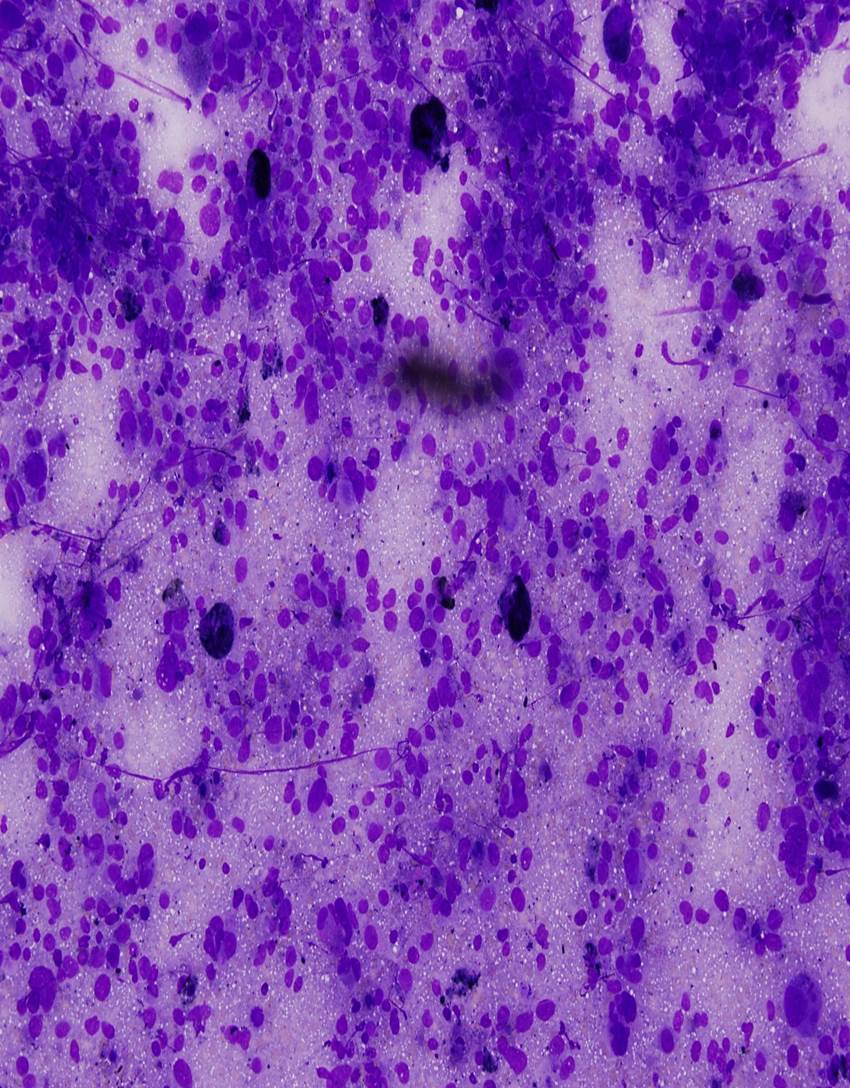
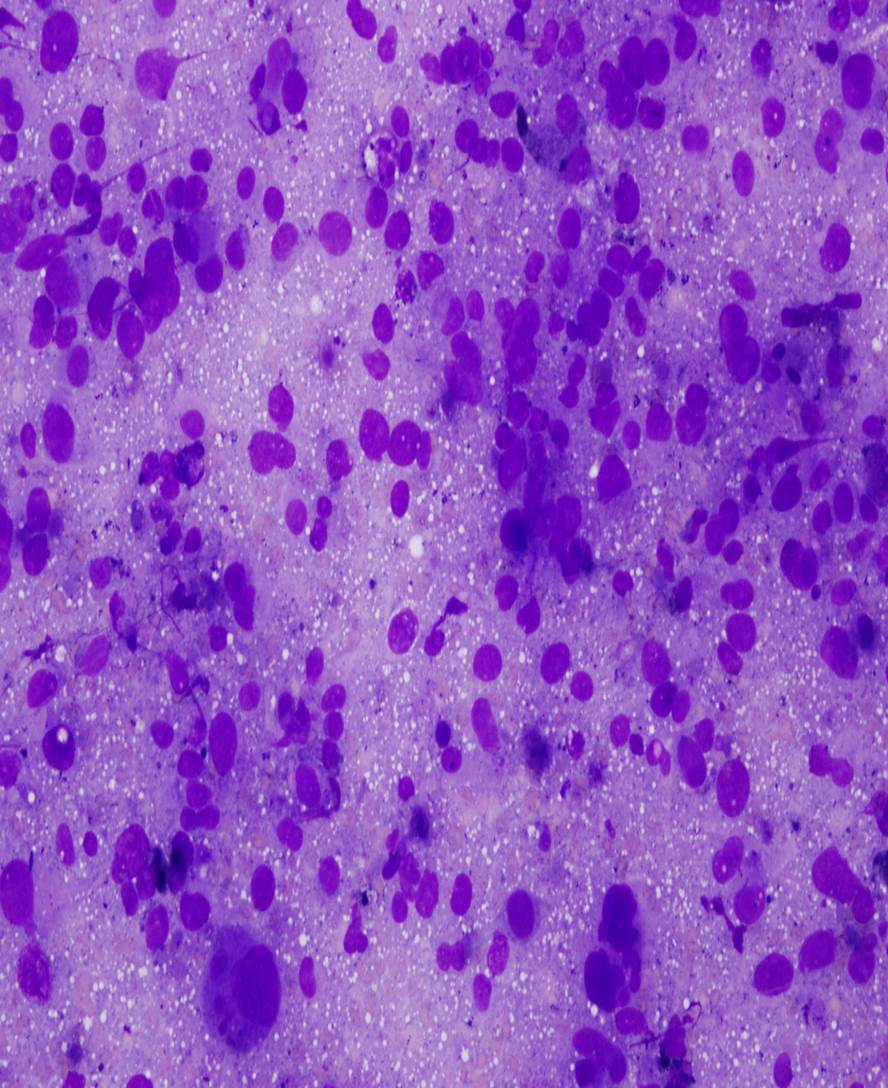
Microscopic (histologic) description
- Mean 3 mm thick; pigmented or frequently amelanotic; morphology includes epithelioid, fusiform and polymorphous cells
- Some tumor giant cells in almost all cases; 90% have associated melanoma in situ; usually mitotic figures
- Frequent ulceration, necrosis, vascular invasion and perineural invasion; may have desmoplastic features, particularly if lower lip
Microscopic (histologic) images
Positive stains
- S100 (97%), tyrosinase / T311 (94%), MelanA / Mart1 / A103 (85%), microphthalmia associated transcription factor / MITF (D5, 74%) and HMB45 (71%)
- Desmoplastic melanoma: S100, tyrosinase
Negative stains
Differential diagnosis
- Amelanotic melanomas:
- Large cell lymphoma, poorly differentiated carcinoma
Board review style question #1
What do primary mucosal melanoma and cutaneous melanoma have in common?
- Both commonly have BRAF mutations
- Both use the same staging criteria
- Sun exposure is a risk factor for both
- They have a similar prognosis
- They have the same immunohistochemical profile
Board review style answer #1
E. They have the same immunohistochemical profiles. Primary mucosal melanomas share histologic and immunohistochemical features with cutaneous melanomas but differ in terms of risk factors, aggressiveness, molecular profiles and staging criteria.
Comment Here
Reference: Melanoma
Comment Here
Reference: Melanoma