Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology / etiology | Clinical features | Radiology description | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology images | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Obeidin F, Alexiev B. Granular cell tumor. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/softtissuegranularcell.html. Accessed April 1st, 2025.
Definition / general
- Soft tissue tumor with neuroectodermal differentiation composed of large cells with eosinophilic, granular cytoplasm
Essential features
- Very rare, predominantly benign soft tissue tumor involving a wide variety of sites
- Shows neural differentiation
- Histology: large cells with eosinophilic, granular cytoplasm; may show pseudoepitheliomatous hyperplasia
- Immunohistochemistry: S100+, SOX10+, CD68+
Terminology
- Synonyms: granular cell schwannoma, granular cell nerve sheath tumor, granular cell myoblastoma, Abrikossoff tumor
- Very rare nonneural variants have been described, typically in the skin, called primitive / dermal nonneural granular cell tumor
- Granular cell change reported in several tumors separate from classic granular cell tumor (ameloblastoma, dermatofibroma, leiomyoma, leiomyosarcoma, angiosarcoma, melanoma, pleomorphic sarcoma)
- Congenital granular cell tumor (congenital epulis) describes a different tumor of uncertain histogenesis affecting primarily the alveolar ridge in neonates (J Oral Maxillofac Pathol 2013;17:440)
ICD coding
Epidemiology
- Wide age range, though most common in 30 - 50 year olds; rare in children < 5 years or adults > 80 years
- Slight female predominance (F:M = 5:4)
- Predilection for African Americans (J Surg Oncol 1980;13:301, Adv Anat Pathol 1999;6:186)
Sites
- Wide variety of sites
- Peripheral soft tissues (38%)
- Trunk (36%)
- Head and neck (20%)
- Predilection for the tongue
- Internal (16%)
- Esophagus most common
- 5 - 15% have multiple lesions
Pathophysiology / etiology
- Rare familial associations have been reported
- Multiple reports of granular cell tumors in children with Noonan syndrome (Pediatr Dermatol 2010;27:209, Eur J Pediatr Surg 2013;23:257, Pediatr Dermatol 2008;25:341)
- Multiple granular cell tumors in one patient with LEOPARD syndrome (Clin Genet 2009;75:185)
- However, sporadic granular cell tumors do not harbor Noonan syndrome or LEOPARD syndrome gene mutations such as PTPN11 or PTEN (J Clin Pathol 2018;71:93)
Clinical features
- Majority are benign (only 0.5 - 2% are malignant)
- Most are asymptomatic, typically 1 - 2 cm in greatest dimension
- Slow, indolent growth
Radiology description
- Mostly nonspecific
- MRI:
- Isointense or brighter than muscle on T1
- High peripheral signal and centrally isointense to muscle on T2
- May be affected by the amount of stromal component in the tumor
- Malignant variants show characteristics seen in other aggressive neoplasms (Skeletal Radiol 2005;34:625)
Prognostic factors
- Majority are benign with excellent outcome after surgical resection
- Some propensity for local recurrence if incompletely excised (J Surg Oncol 1980;13:301)
- Malignant granular cell tumors behave similarly to malignant peripheral nerve sheath tumors and have a 50% rate of metastasis
- Adverse prognostic factors include local recurrence, metastasis, larger tumor size, older patient age, histologic classification as malignant, presence of necrosis, increased mitotic activity, spindling of tumor cells, vesicular nuclei with large nucleoli and Ki67 ≥ 10% (Am J Surg Pathol 1998;22:779)
- Another study showed size > 5 cm and distant metastases were the factors most negatively affecting survival (J Surg Oncol 2018;118:891)
Case reports
- 5 year old girl presenting with exotropia of her right eye, found to have an intraocular mass (BMC Ophthalmol 2019;19:97)
- 28 year old woman with dysphagia found to have an esophageal mass on endoscopy (Cureus 2018;10:e2679)
- 46 year old woman with smoking history presents with a lung mass (Diagn Cytopathol 2019;47:345)
- 63 year old man with painless rectal bleeding found to have a polyp on colonoscopy (Cureus 2019;11:e4074)
- 70 year old woman with a slowly growing mass in the anal region (J Gastrointest Surg 2019 Feb 28 [Epub ahead of print])
- 74 year old woman with a right breast mass suspicious for carcinoma (SAGE Open Med Case Rep 2019;7:2050313X19841154)
Treatment
- Benign lesions treated with surgical excision have excellent prognosis
- Malignant tumors require wider surgical resection
- Lymph node dissection not recommended unless metastasis is biopsy proven
- Benefit of adjuvant radiotherapy / chemotherapy is debatable but may be helpful in controlling progression in advanced disease (J Surg Oncol 2018;118:891)
- Pazopanib showed activity in a single case report (Case Rep Med 2014;2014:794648)
Clinical images
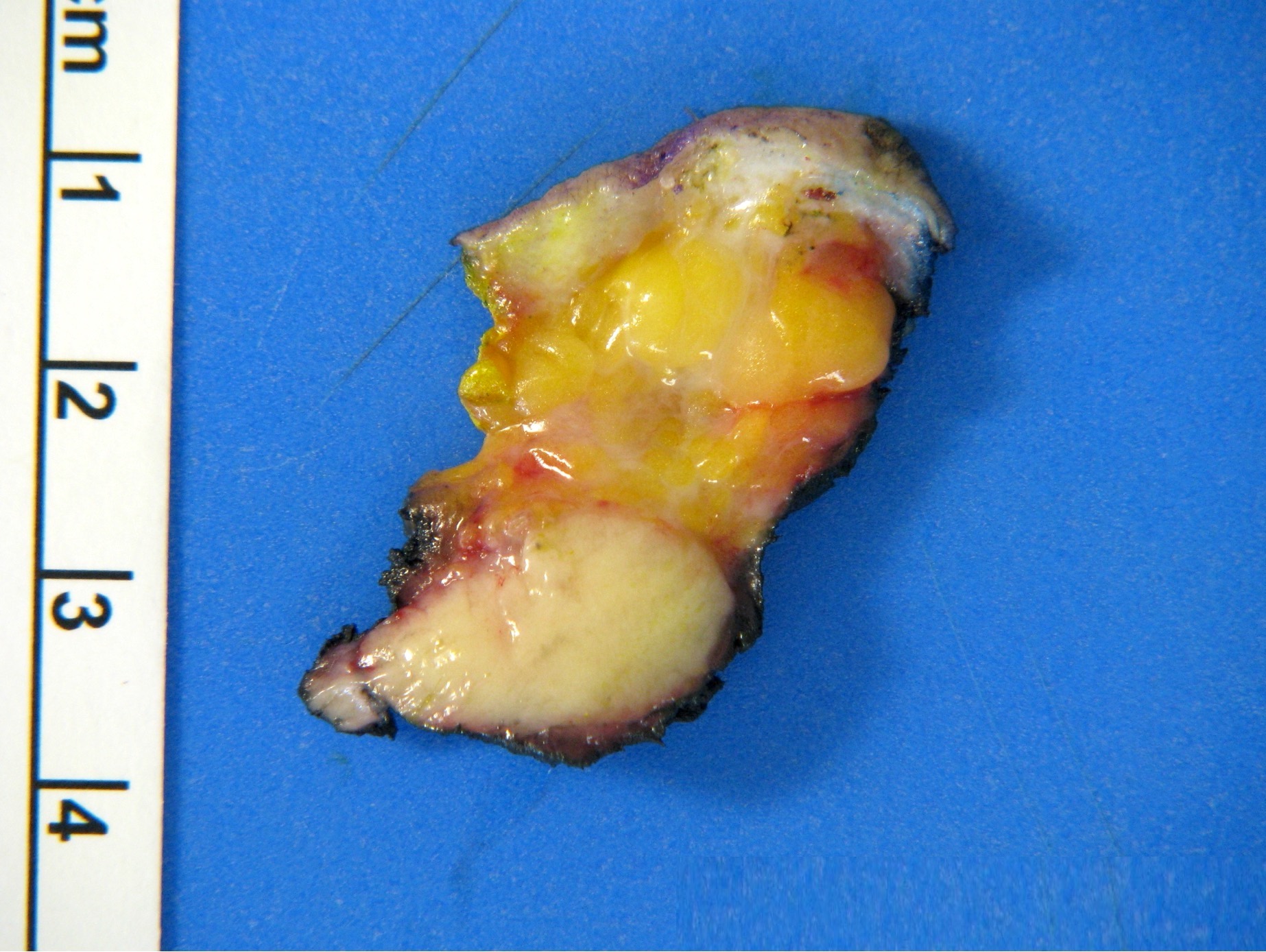
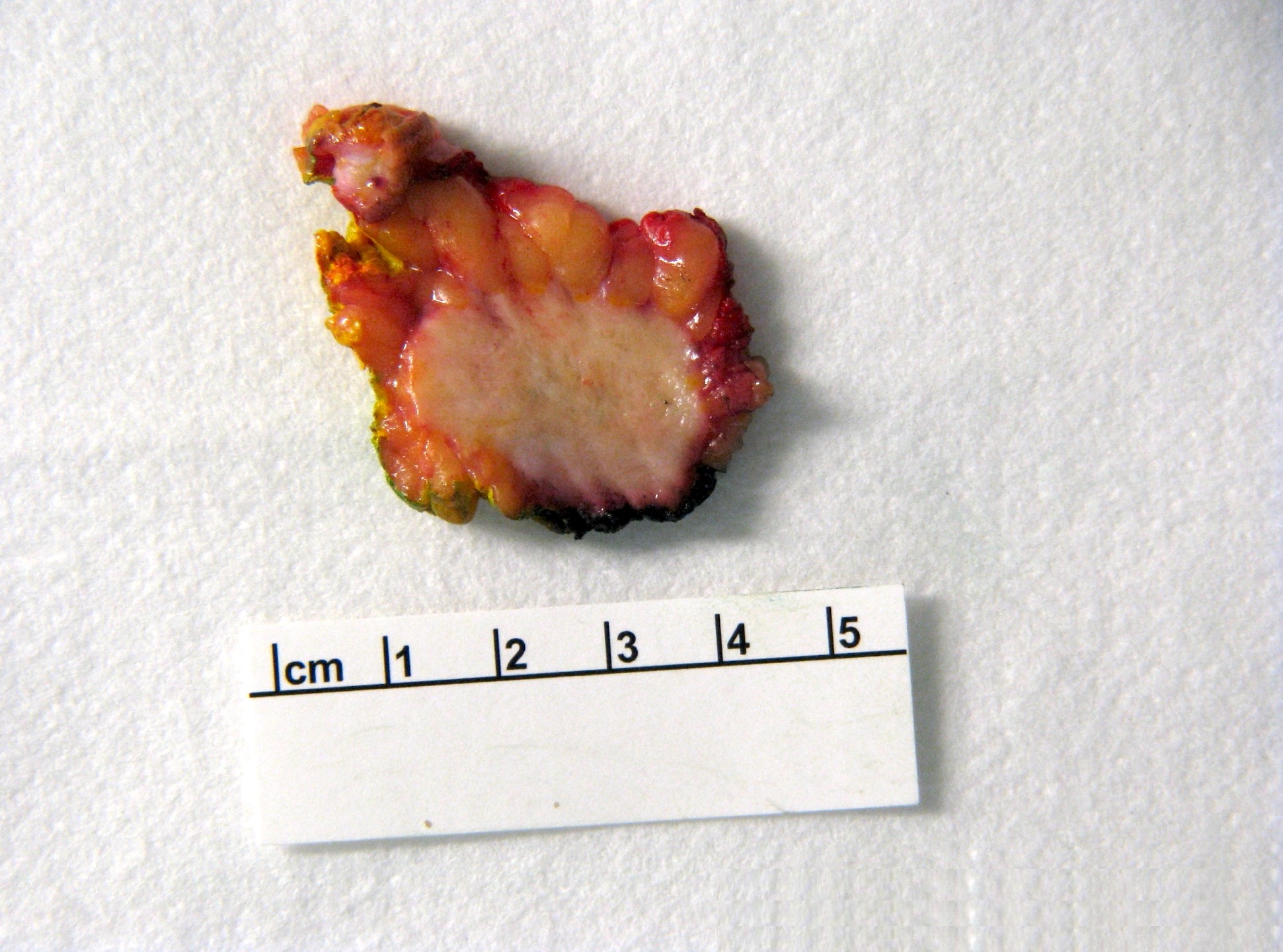
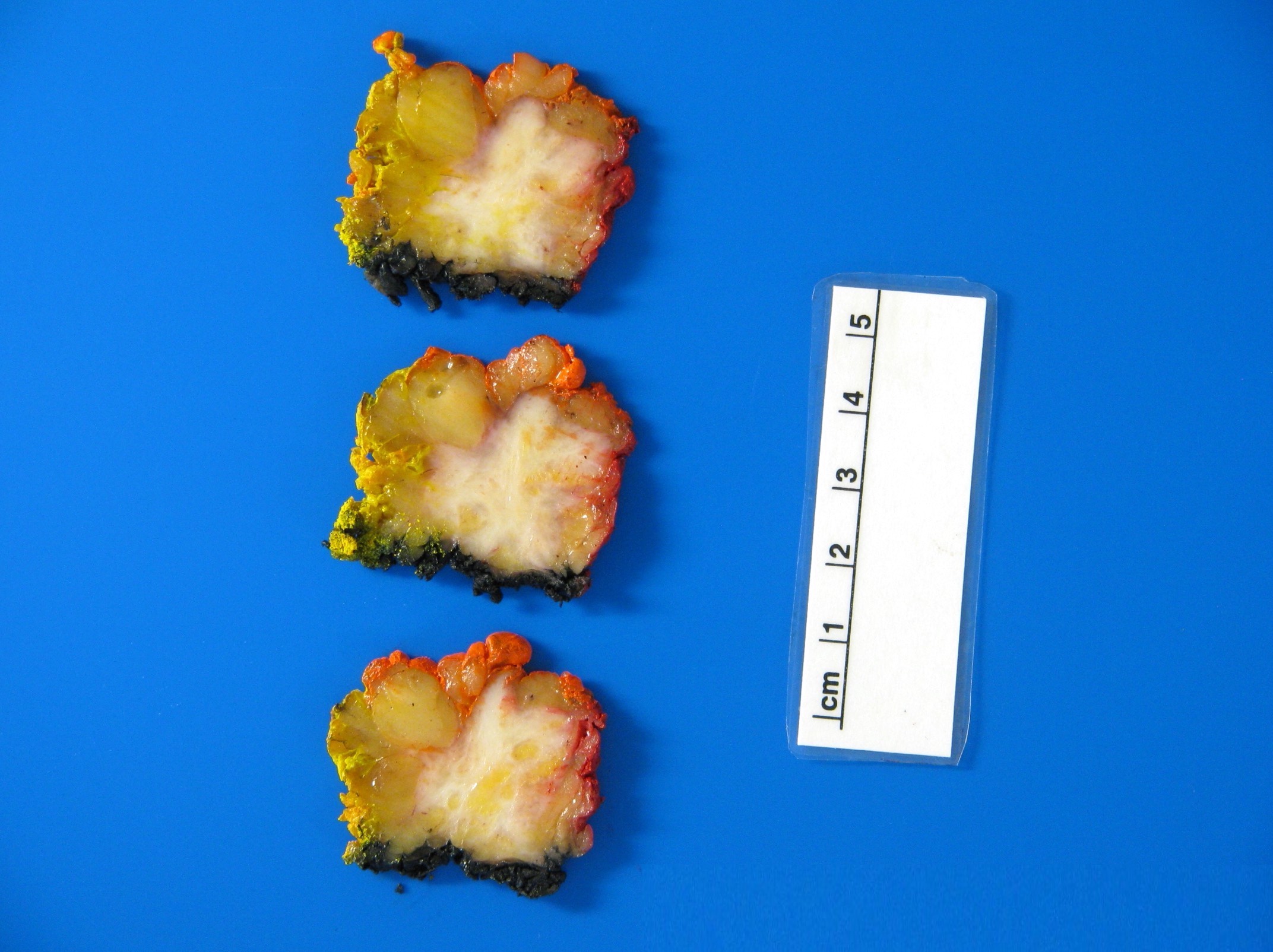
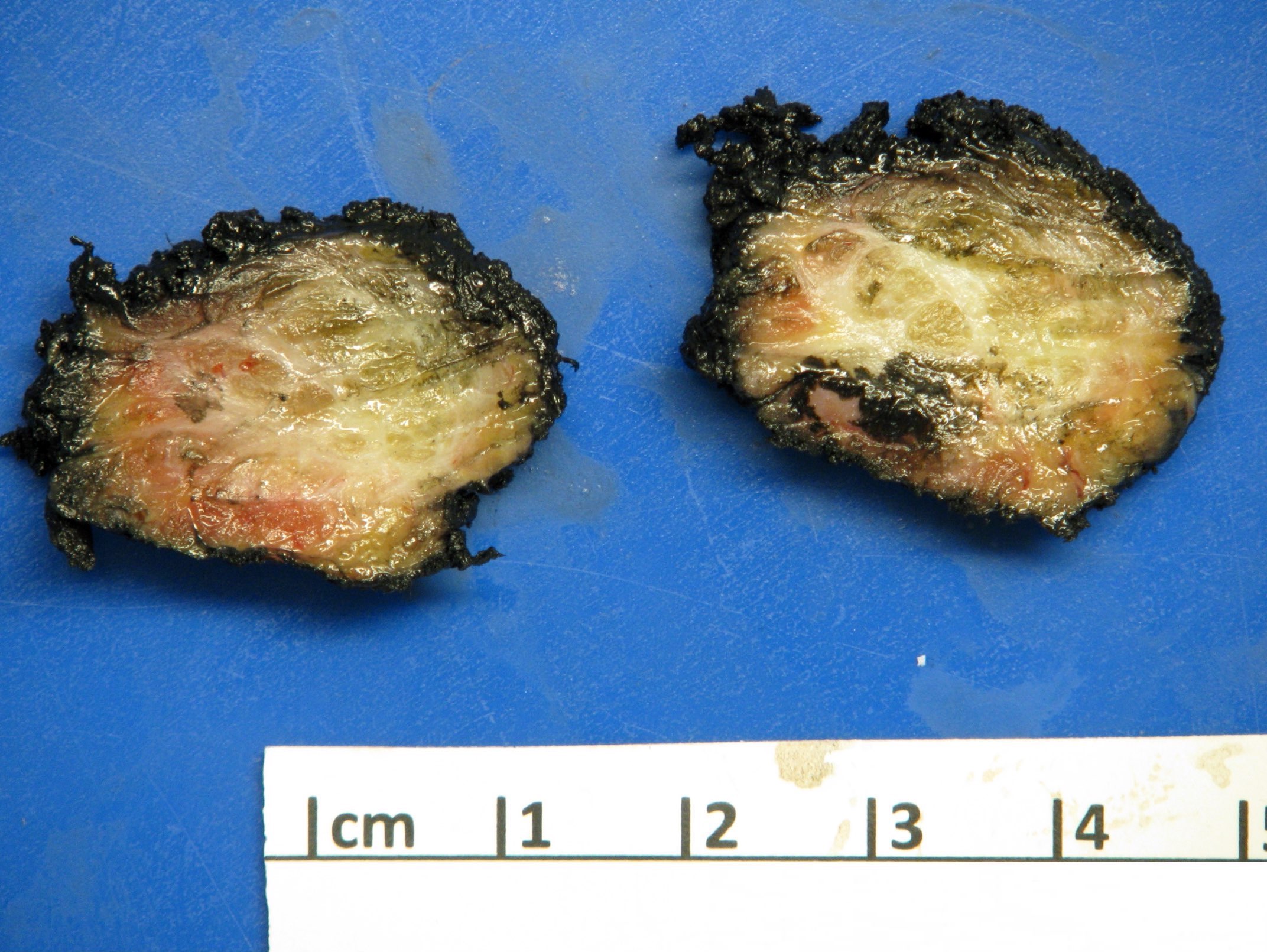
Gross description
- Uninodular firm mass
- In the skin, overlying epidermal hyperplasia can be seen
- Cut surface is yellow with finely granular texture
Gross images
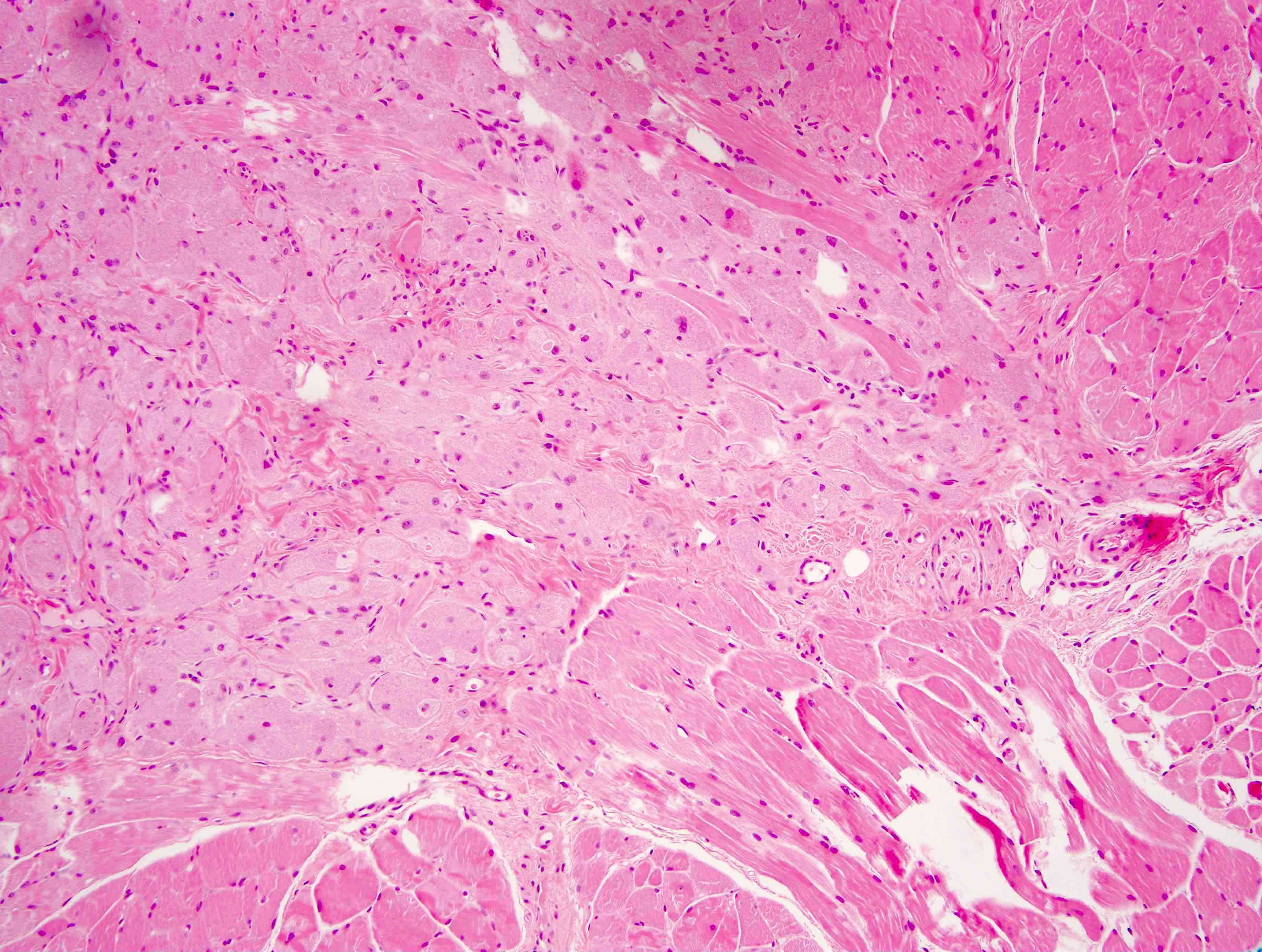
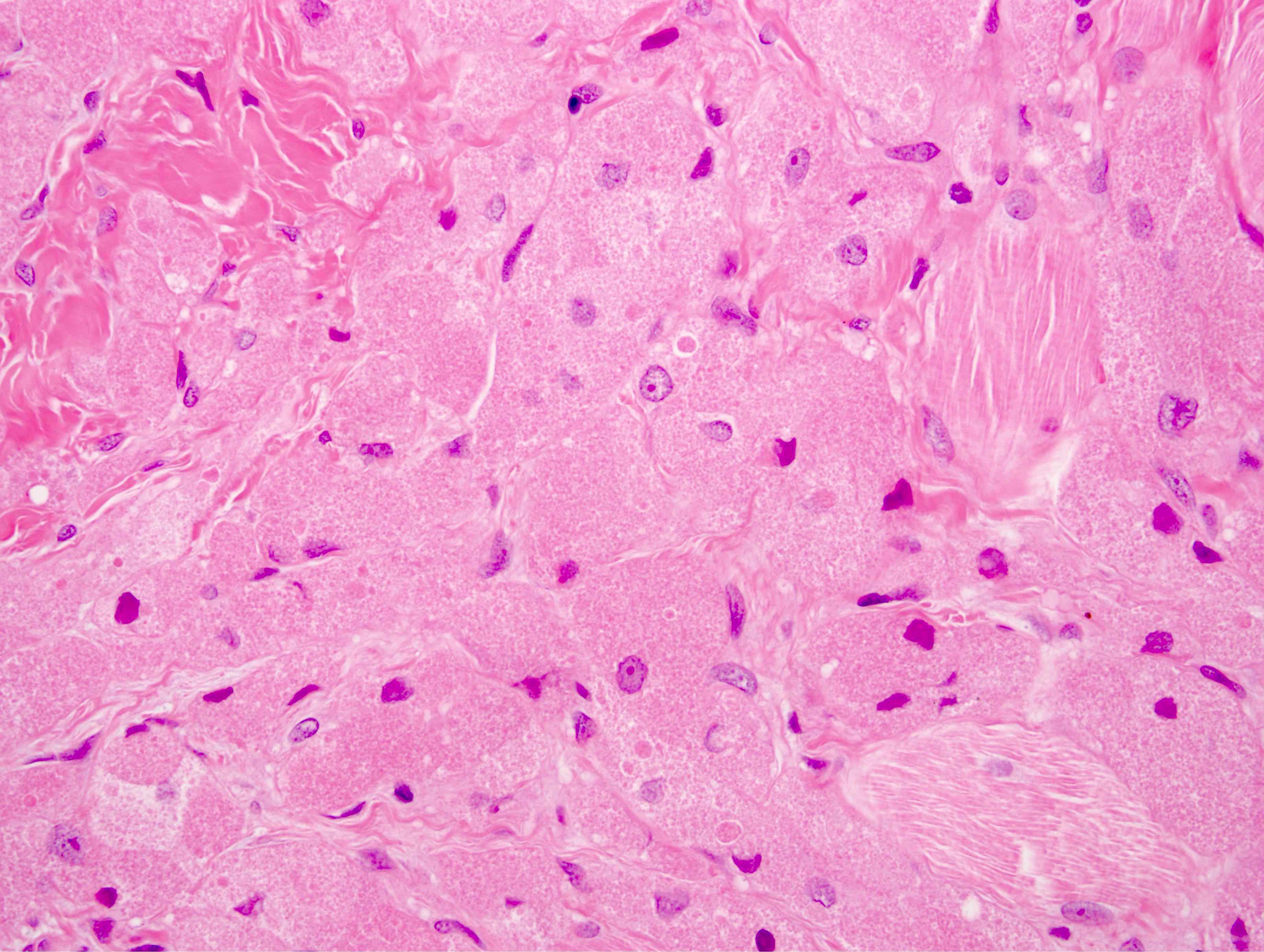
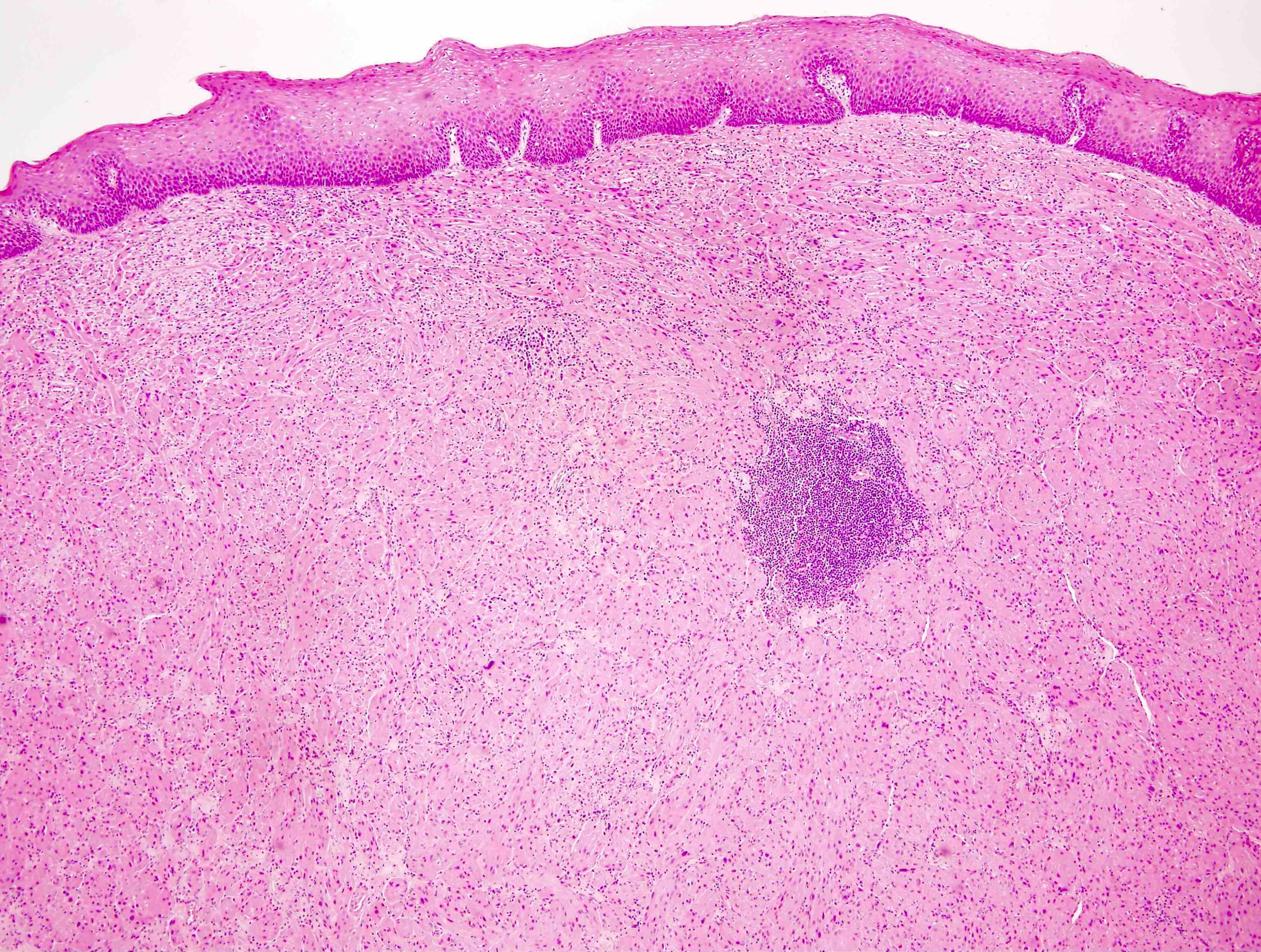
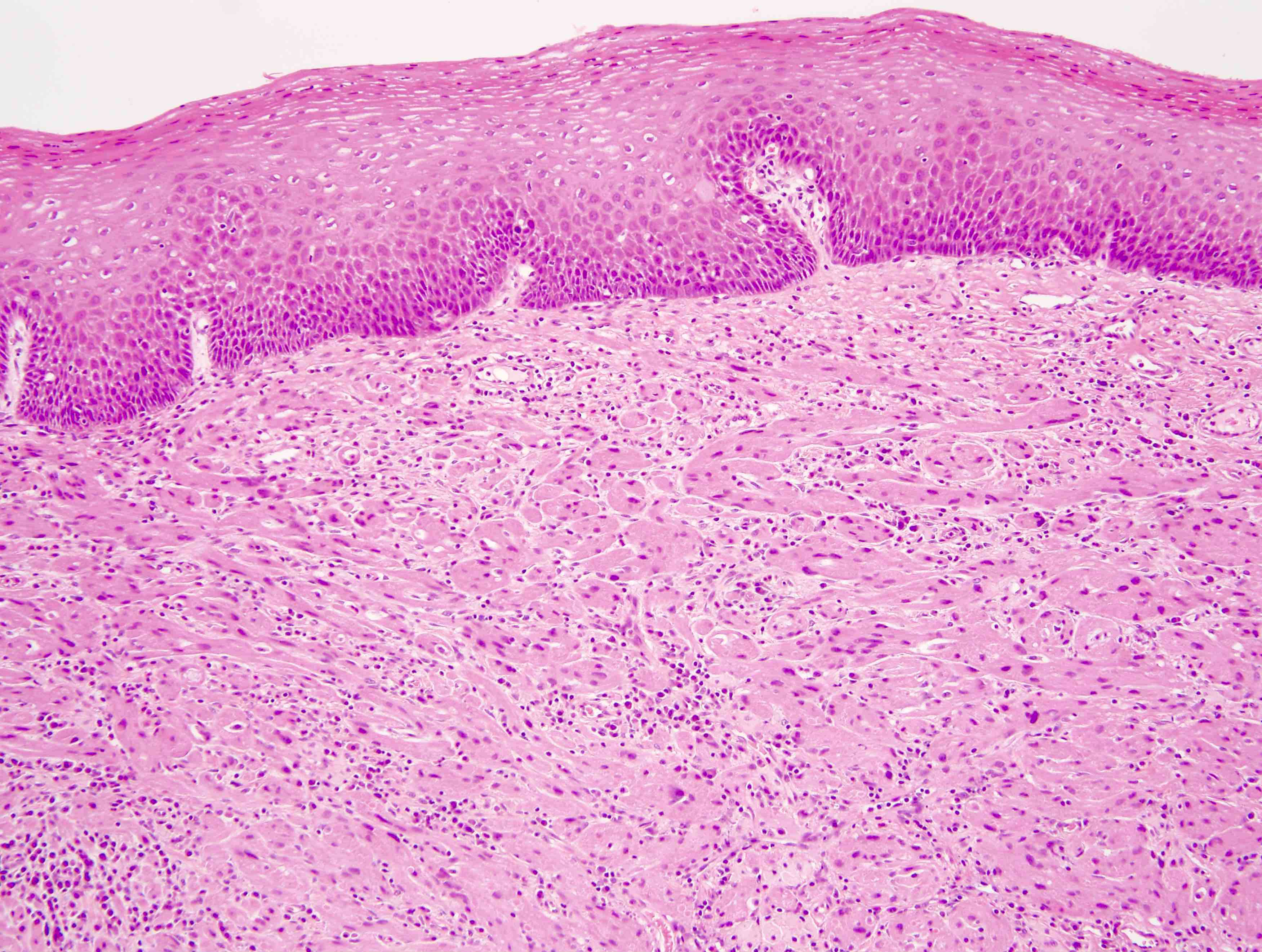
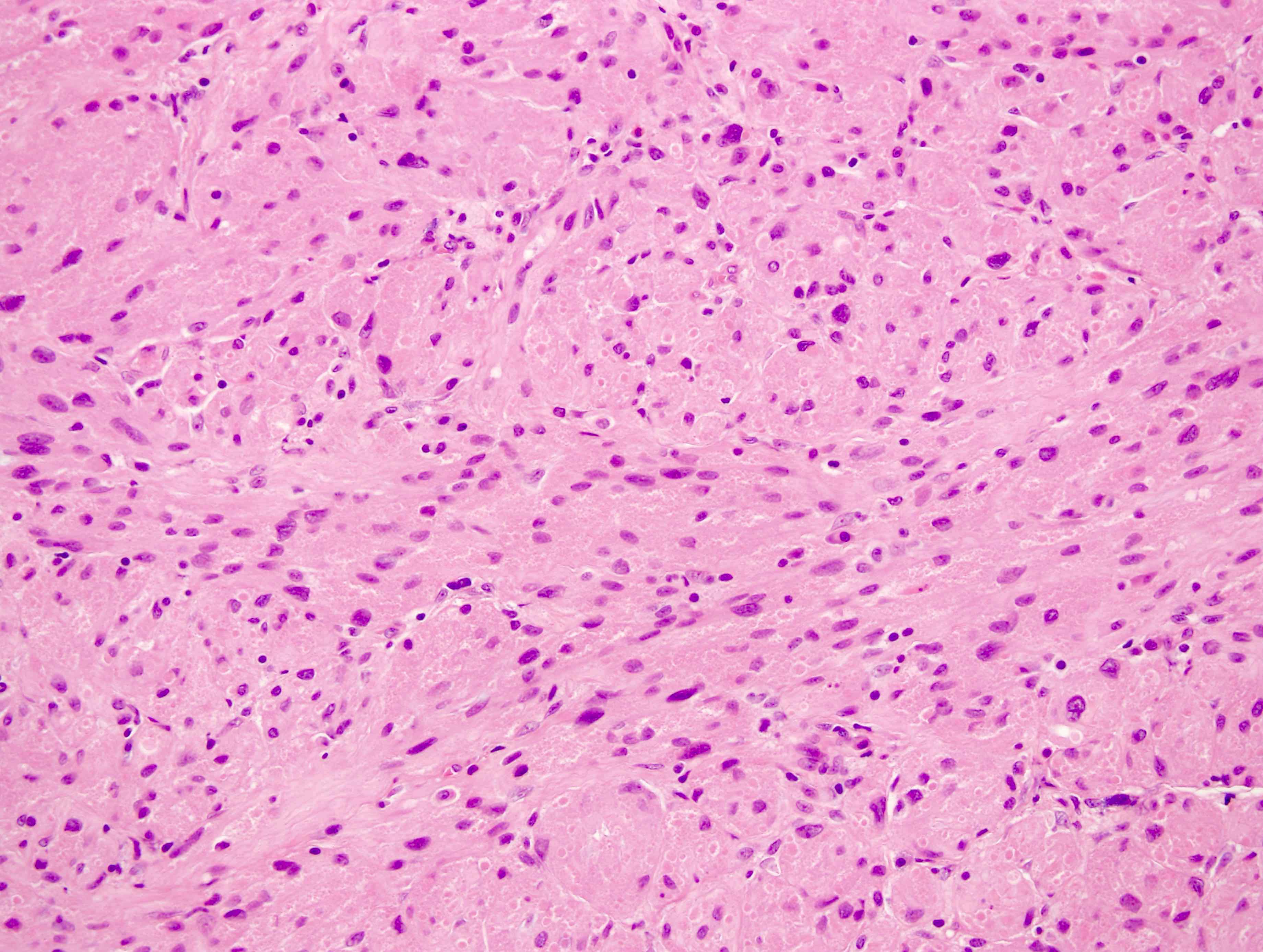
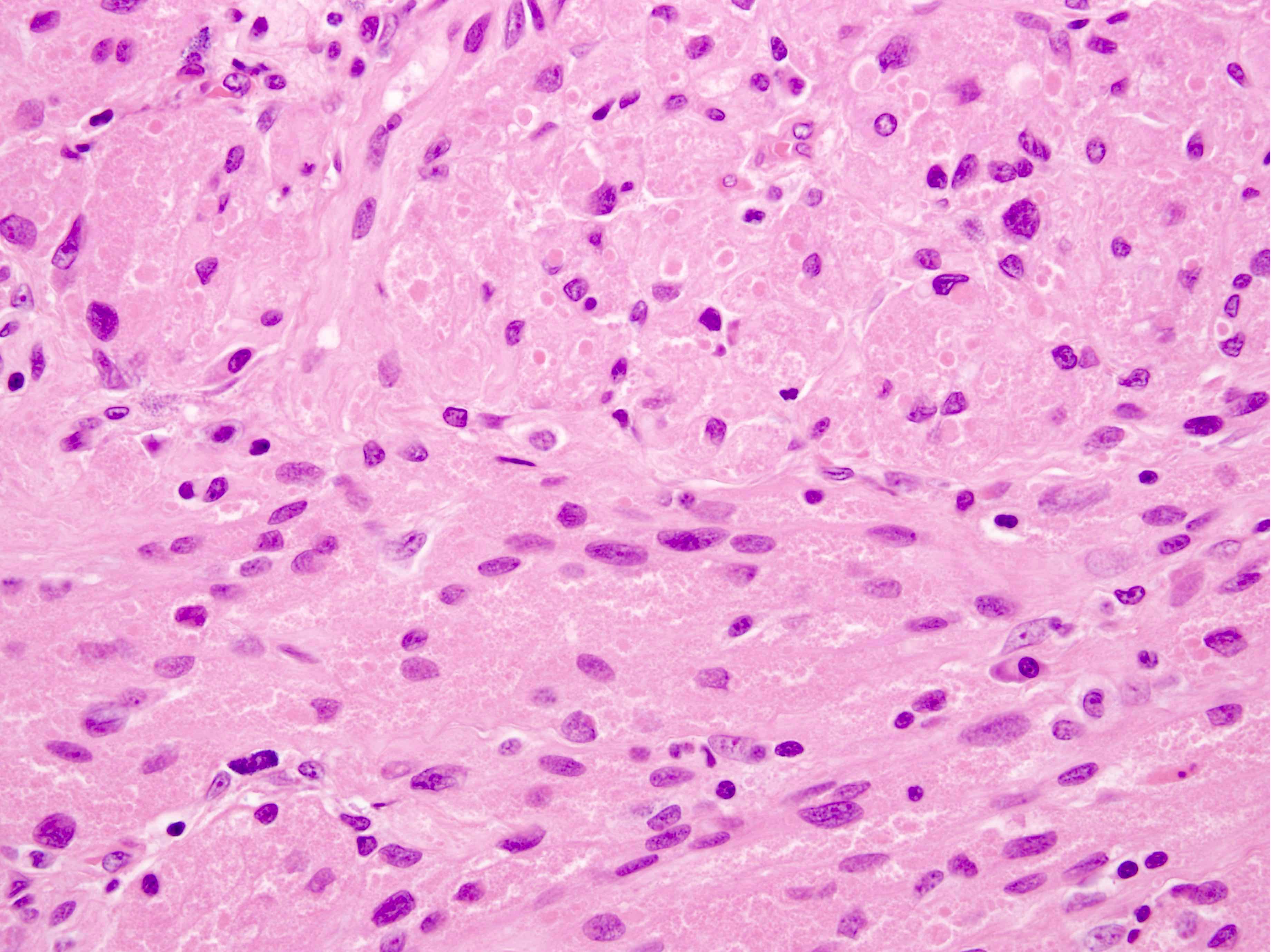
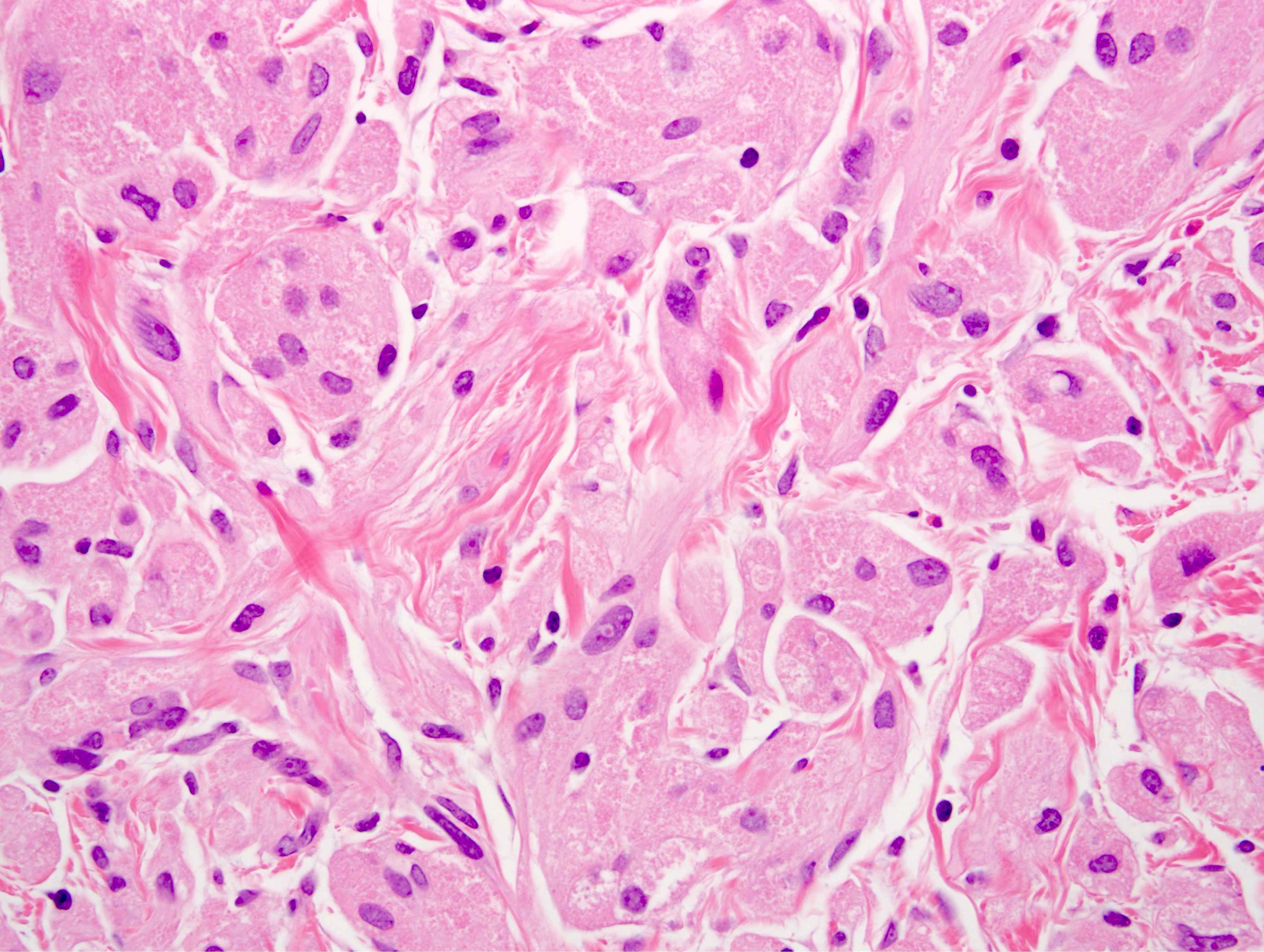
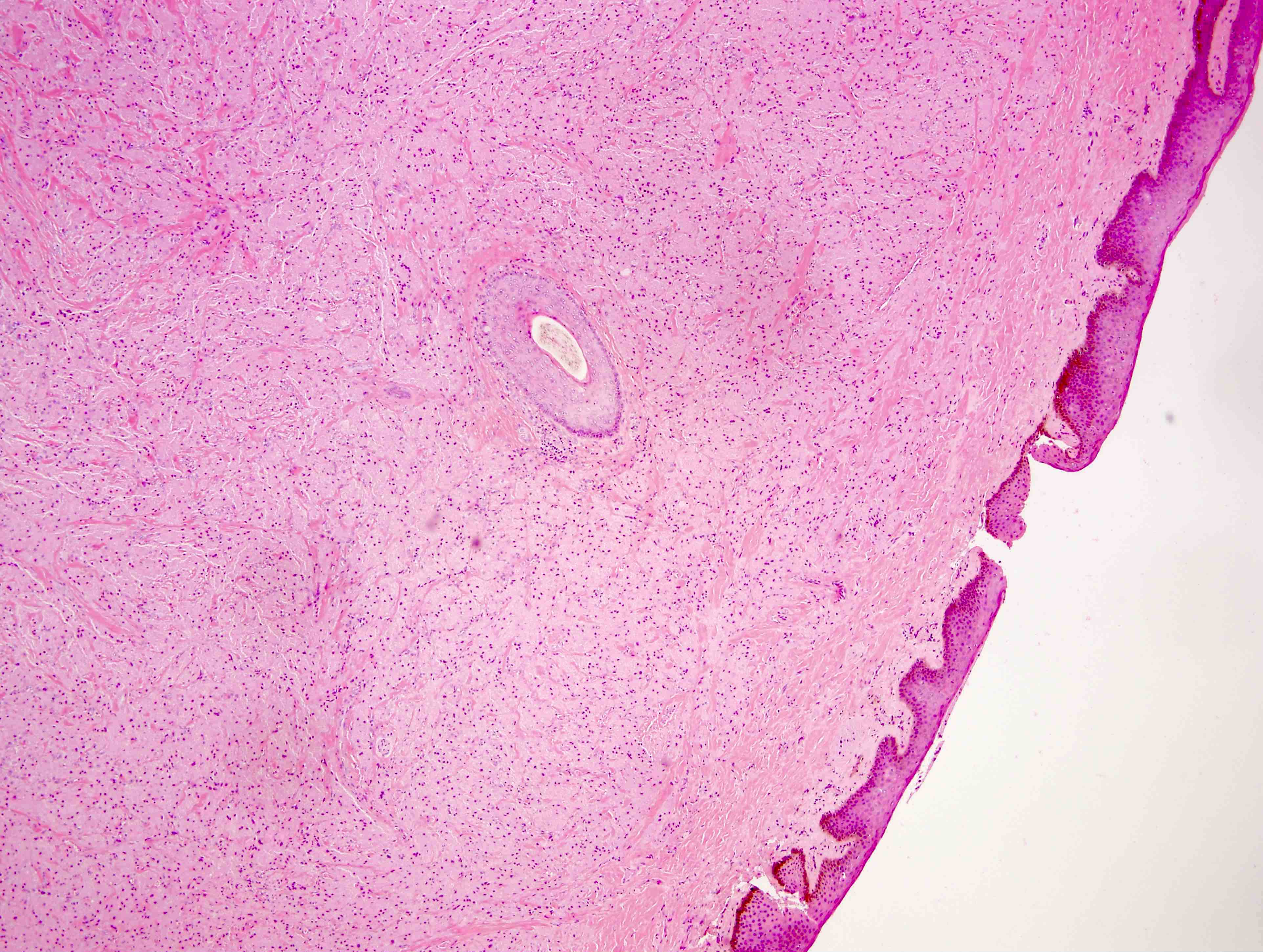
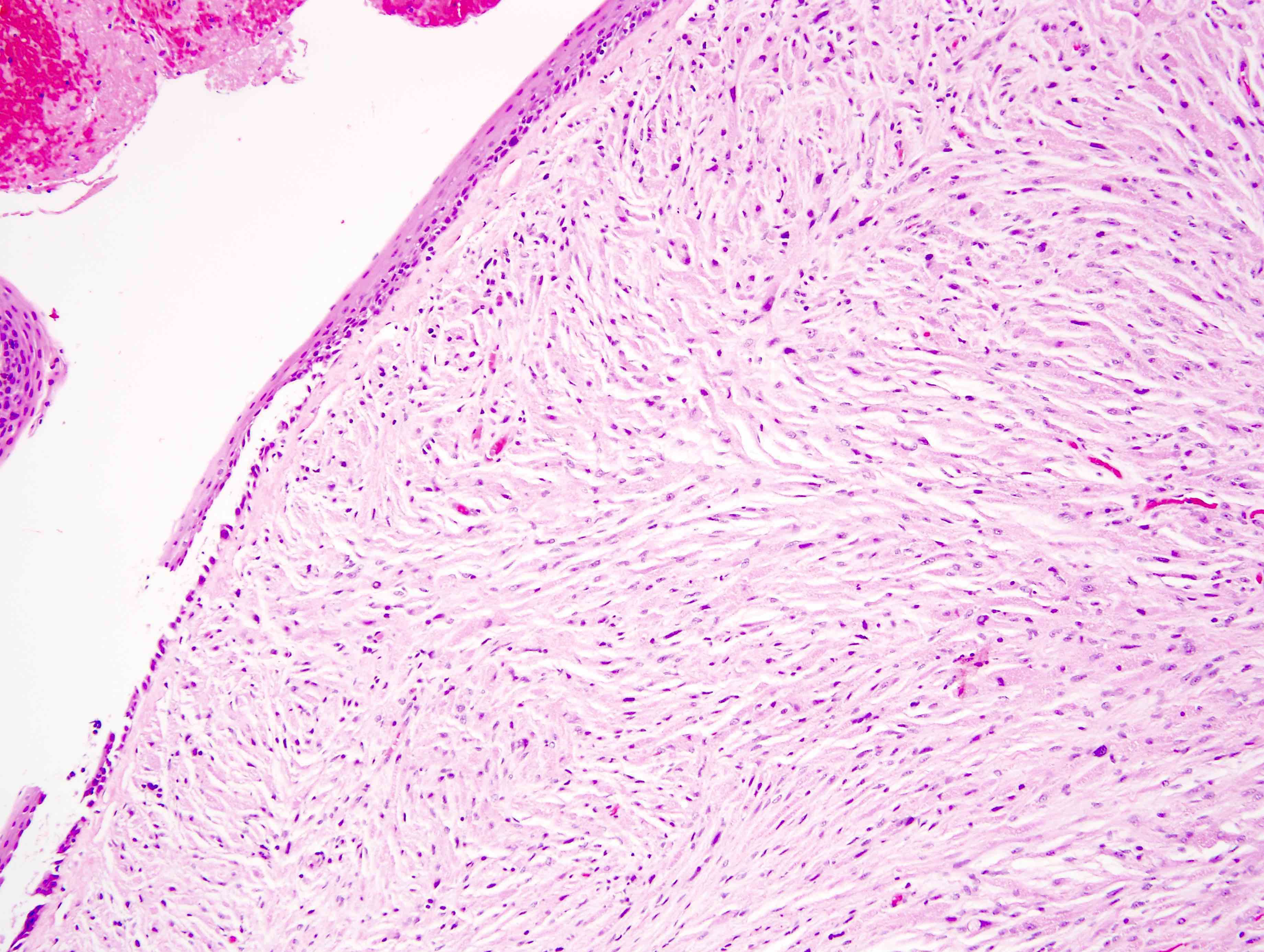
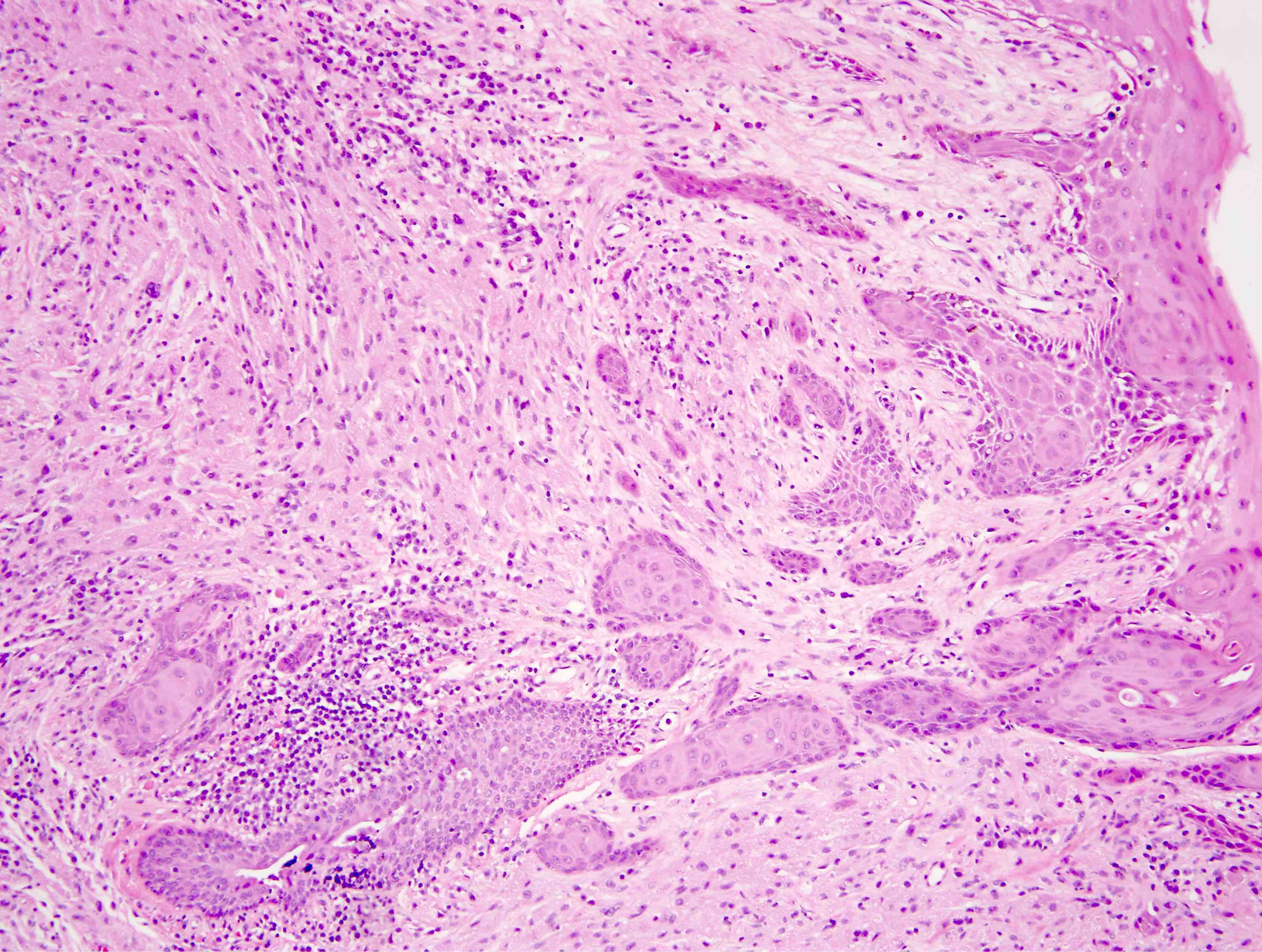
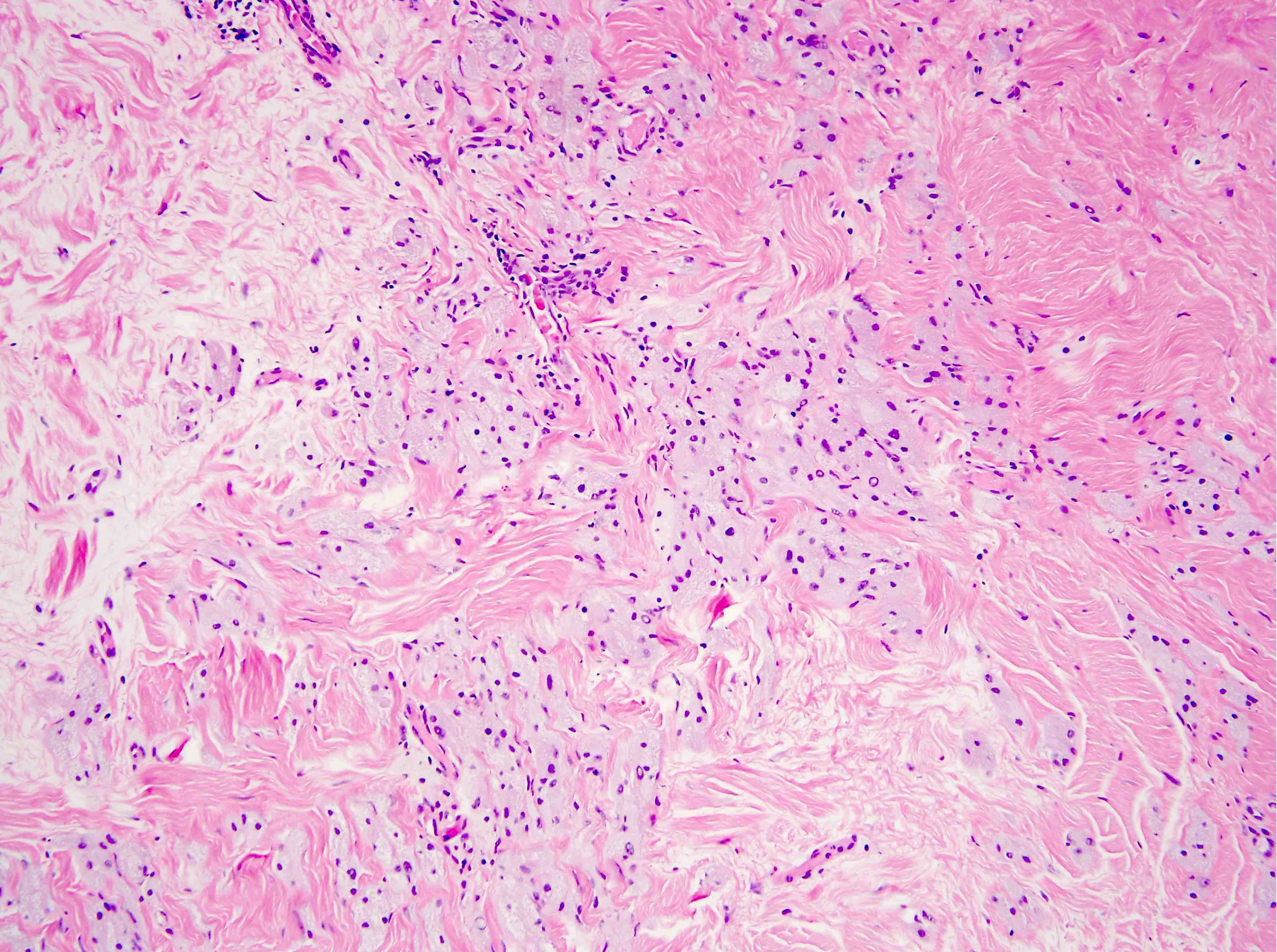
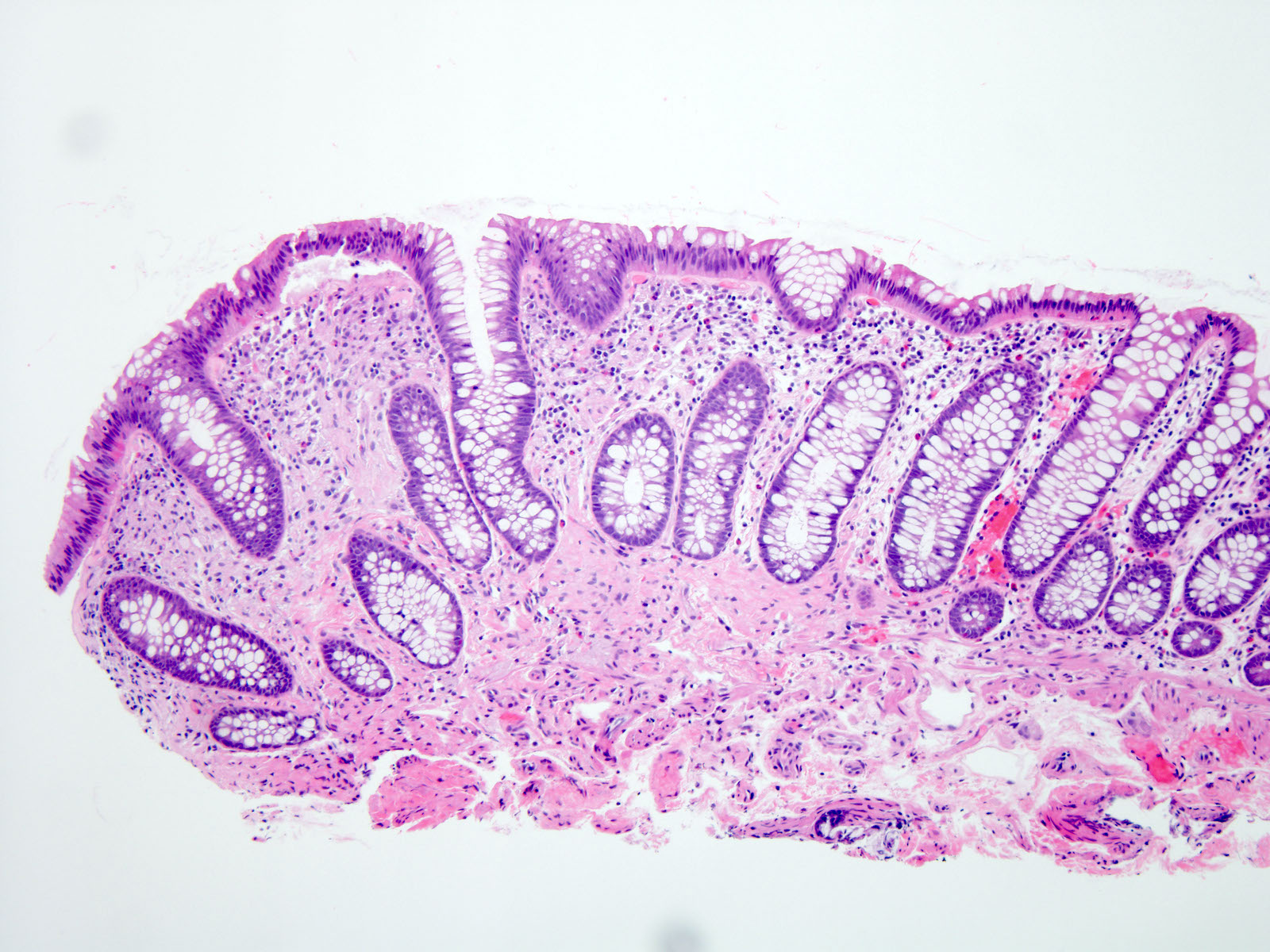
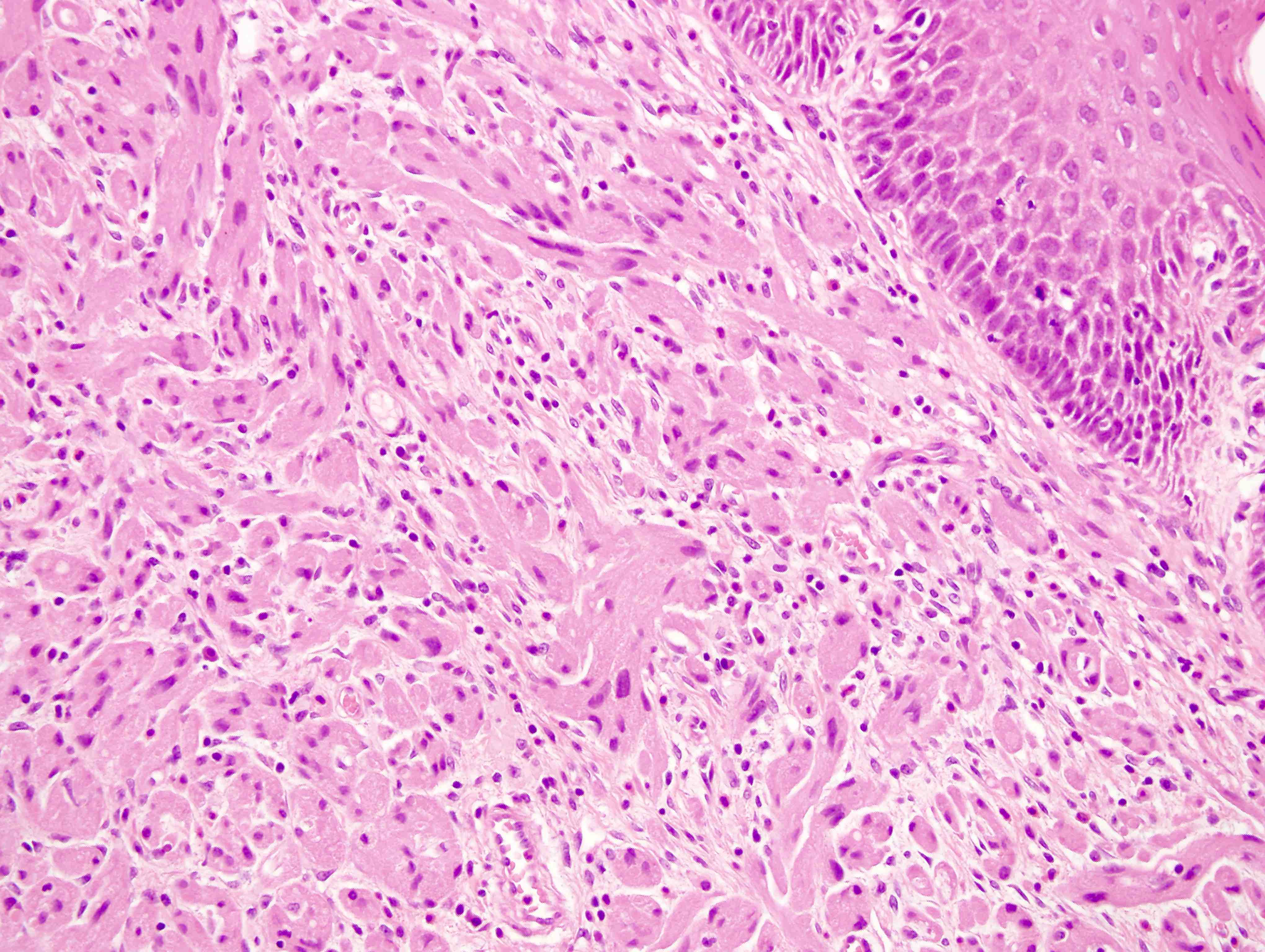
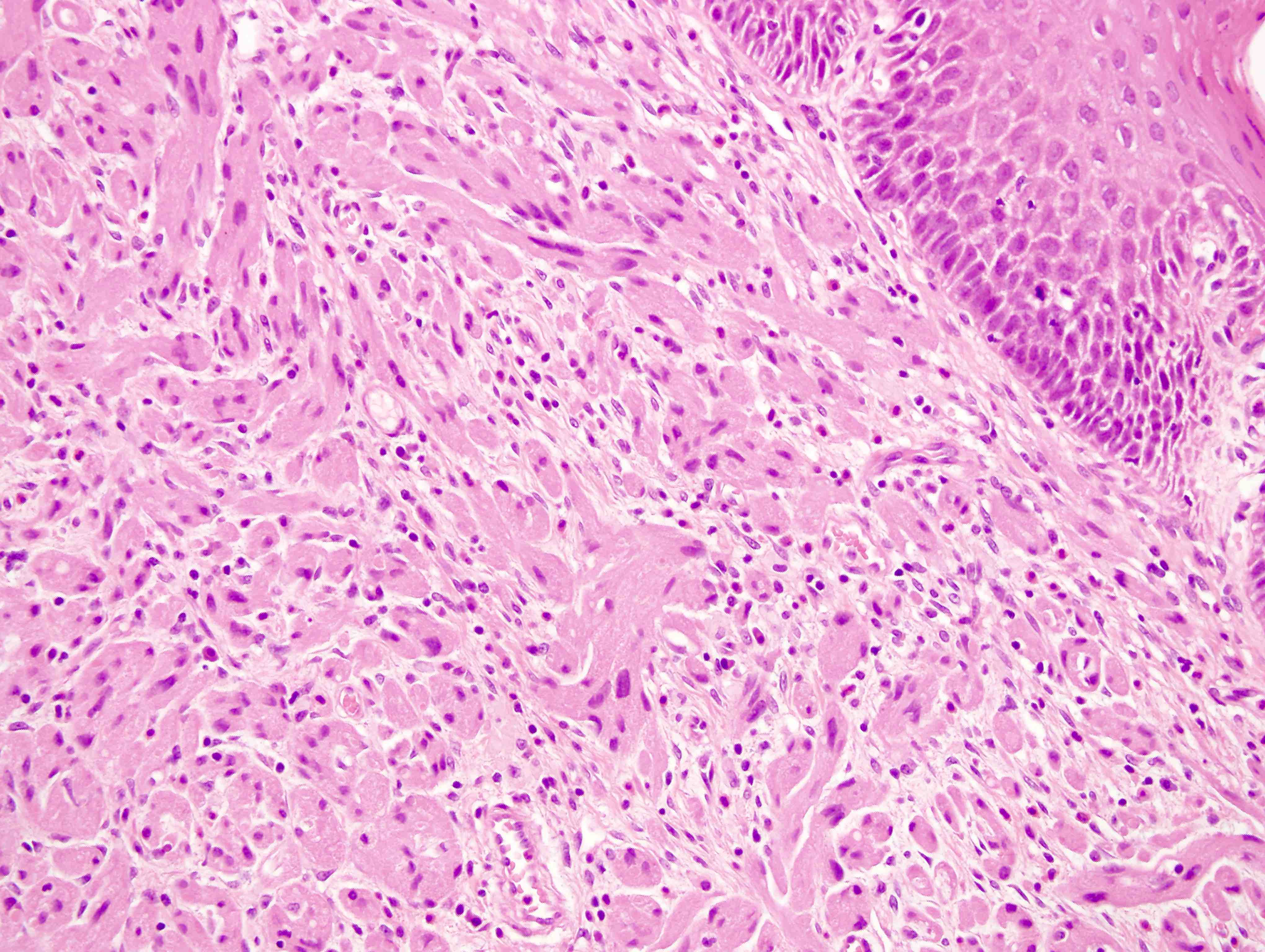
Microscopic (histologic) description
- Architecture:
- Poorly defined mass composed of sheets of cells or nests / ribbons separated by thin collagenous bands
- Cytological features:
- Cells are round and polygonal to slightly spindled; cell borders can be distinct or show a syncytial pattern
- Nuclei: range from small and dense to large and vesicular; mild to moderate nuclear atypia can be seen
- Abundant eosinophilic cytoplasm with coarse granules (representing phagolysosome aggregates)
- Overlying squamous epithelium may show pseudoepitheliomatous hyperplasia
- Malignant criteria still debated
- Fanburg-Smith criteria:
- Necrosis, tumor cell spindling, vesicular nuclei with large nucleoli, > 2 mitoses/10 high power fields, high nuclear to cytoplasmic ratio and pleomorphism
- 0: benign; 1 - 2: atypical; ≥ 3: malignant (Am J Surg Pathol 1998;22:779)
- Nasser-Ahmed-Kowalski criteria:
- Necrosis and > 2 mitoses/10 high power fields
- 0: benign; ≥ 1: granular cell tumor of uncertain malignant potential
- Metastasis was the only criteria to diagnose malignant granular cell tumor (Pathol Res Pract 2011;207:164)
- Fanburg-Smith criteria:
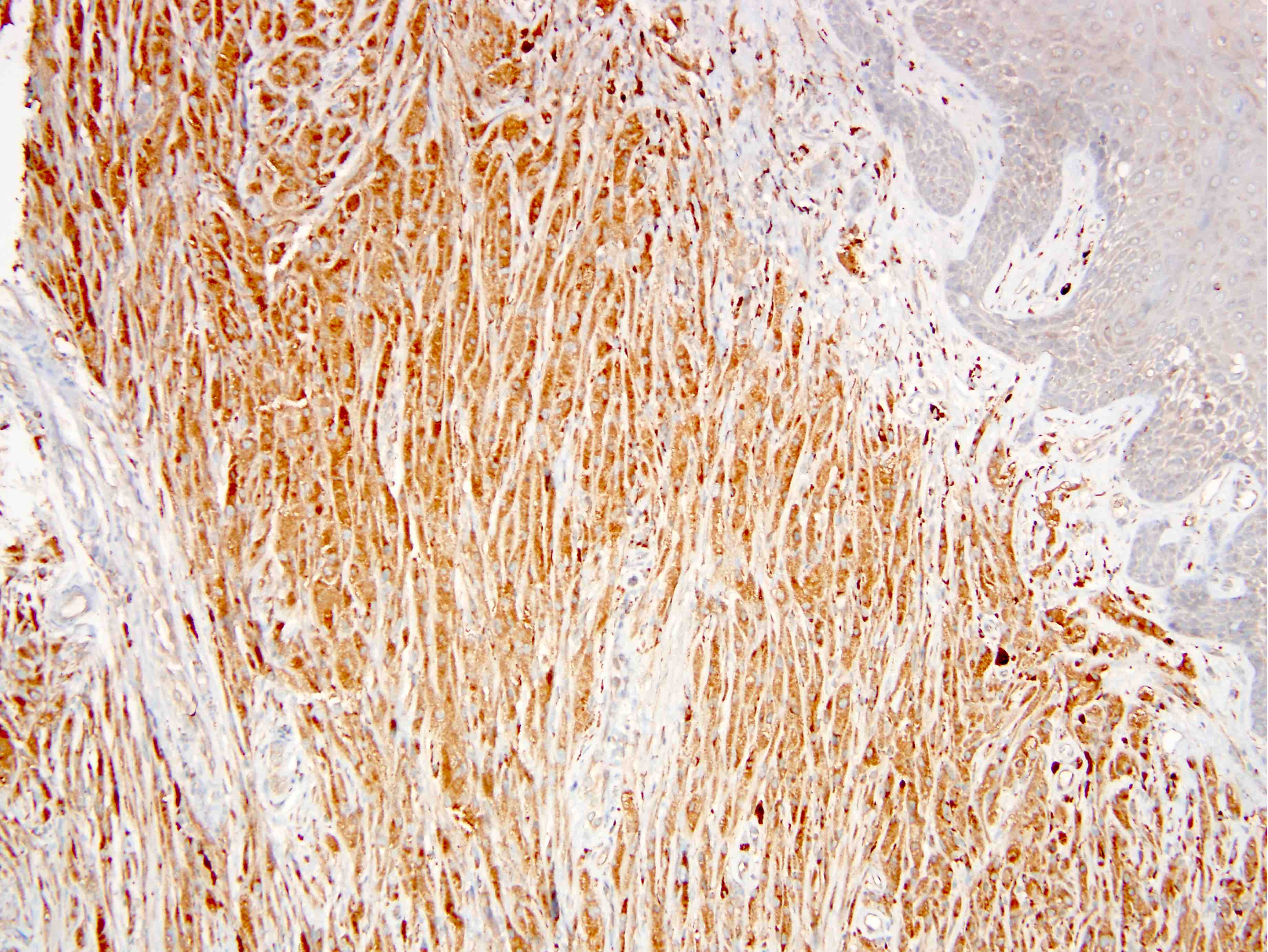
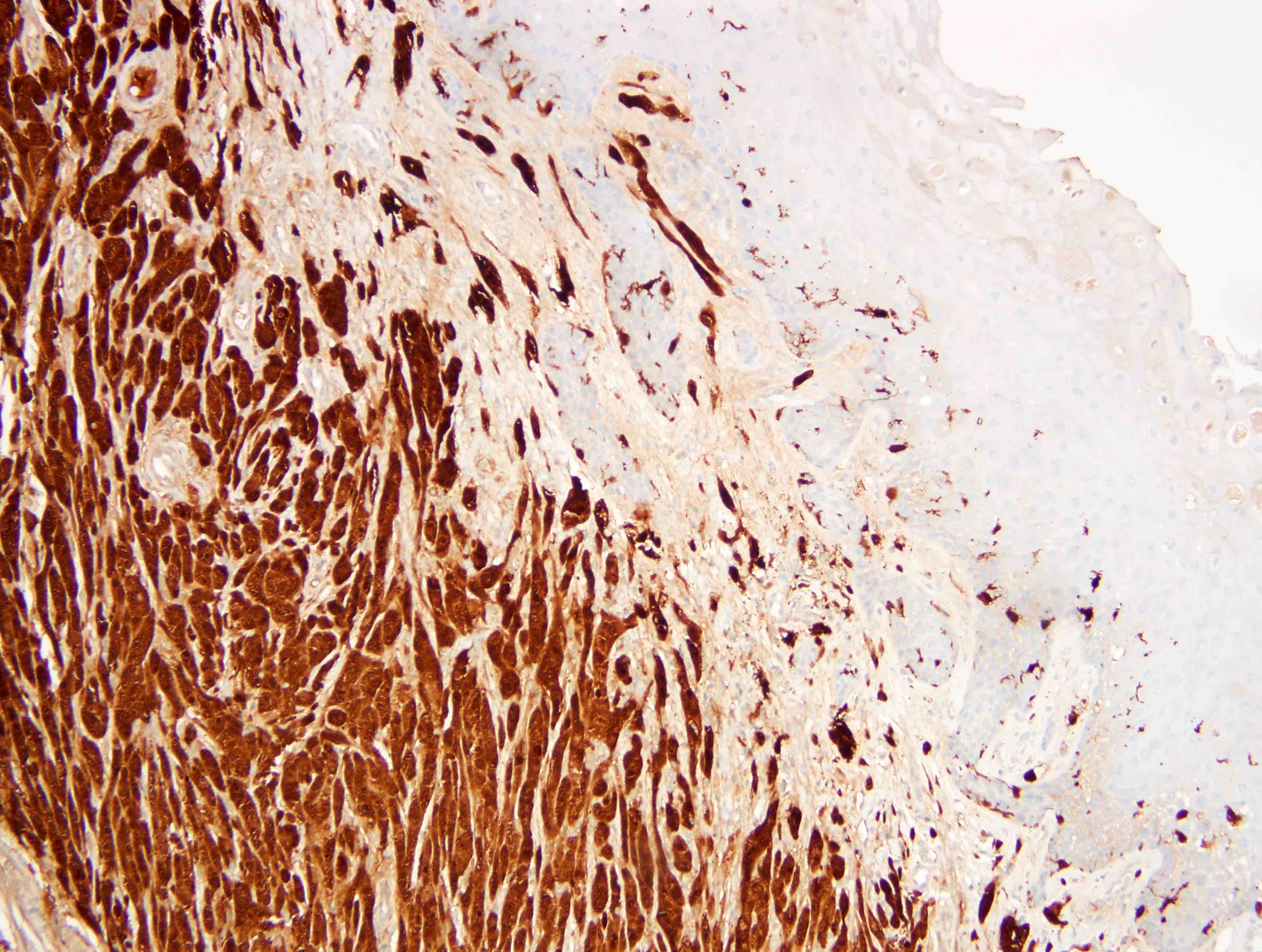
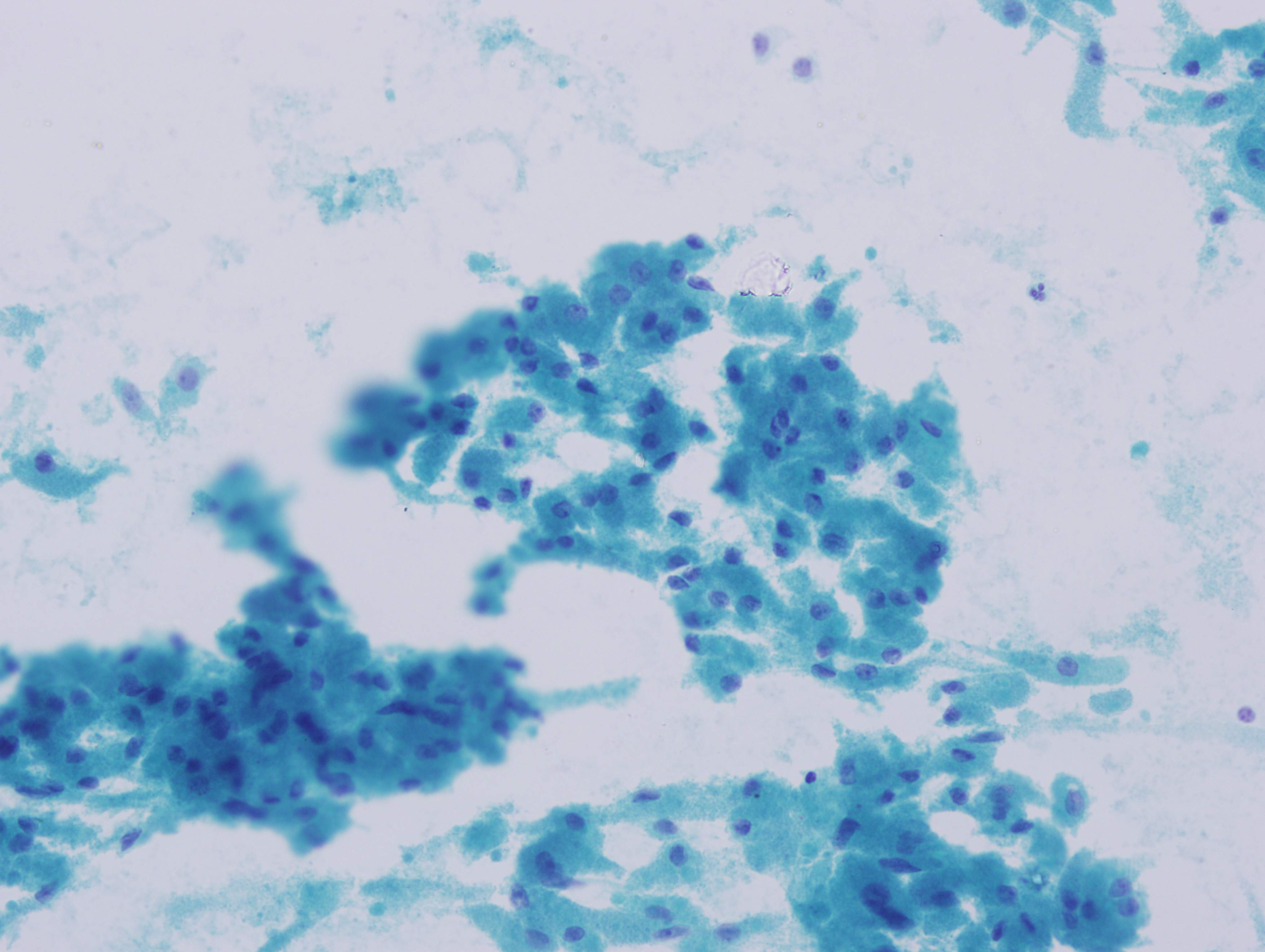
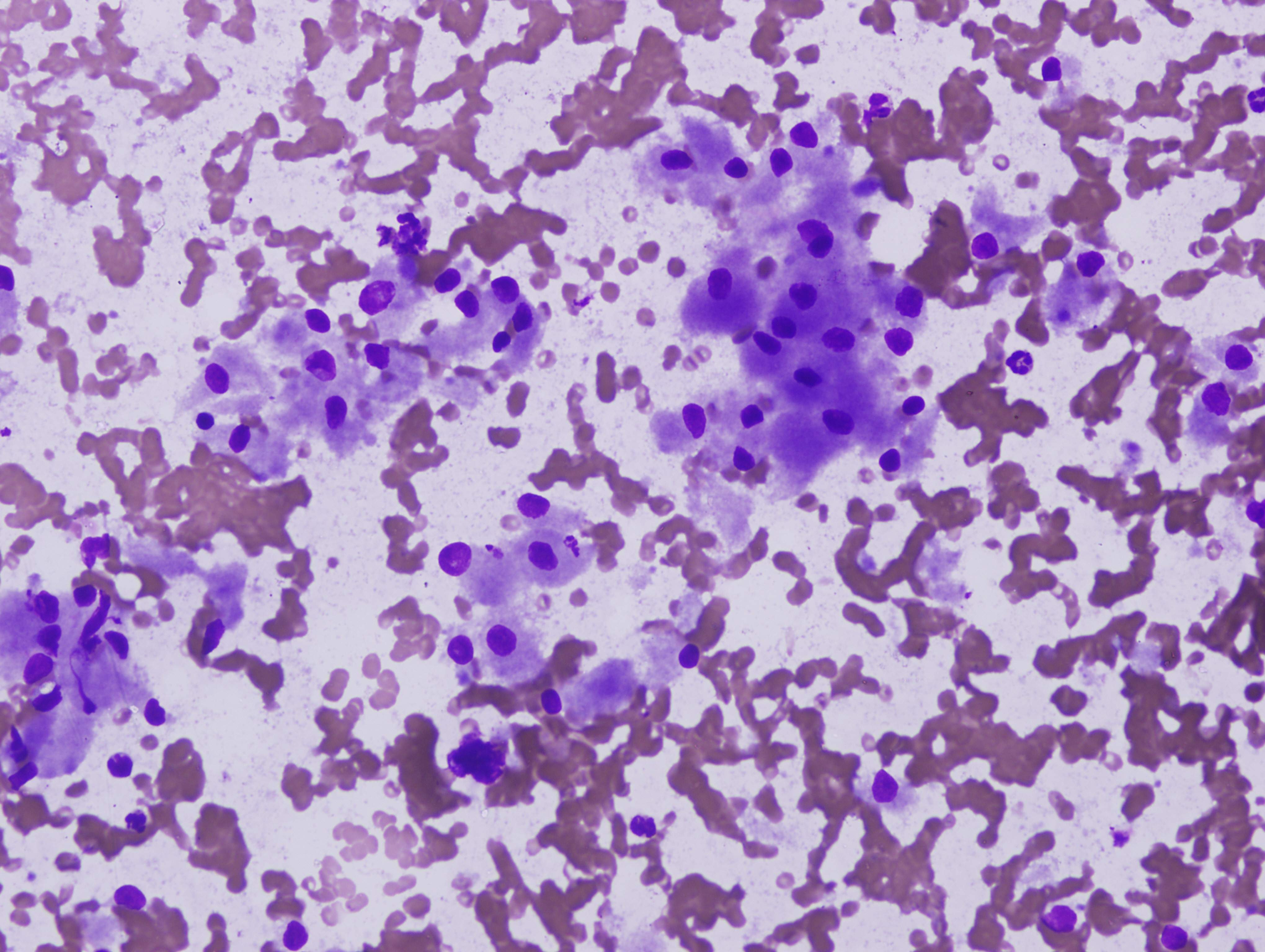
Microscopic (histologic) images
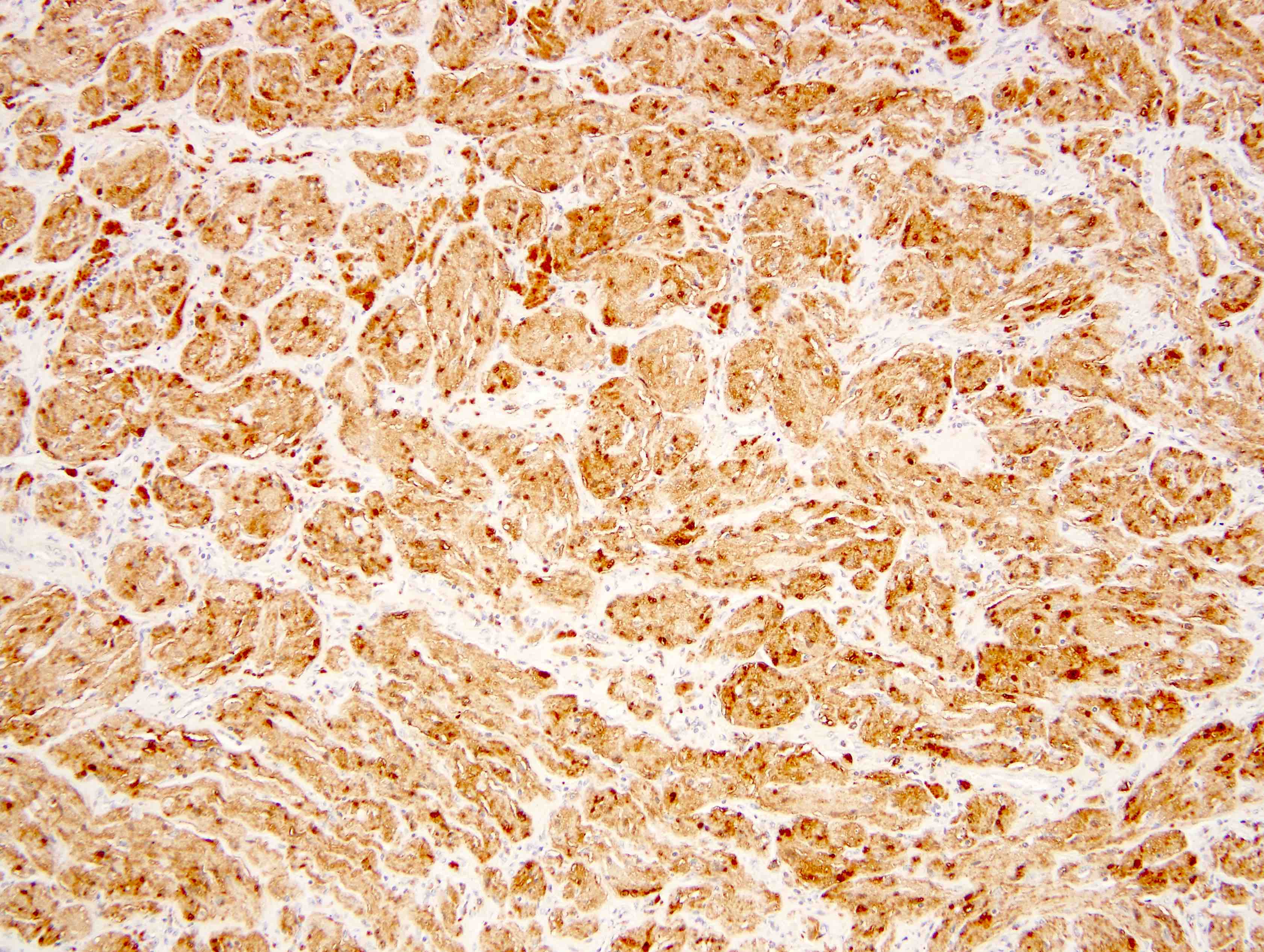
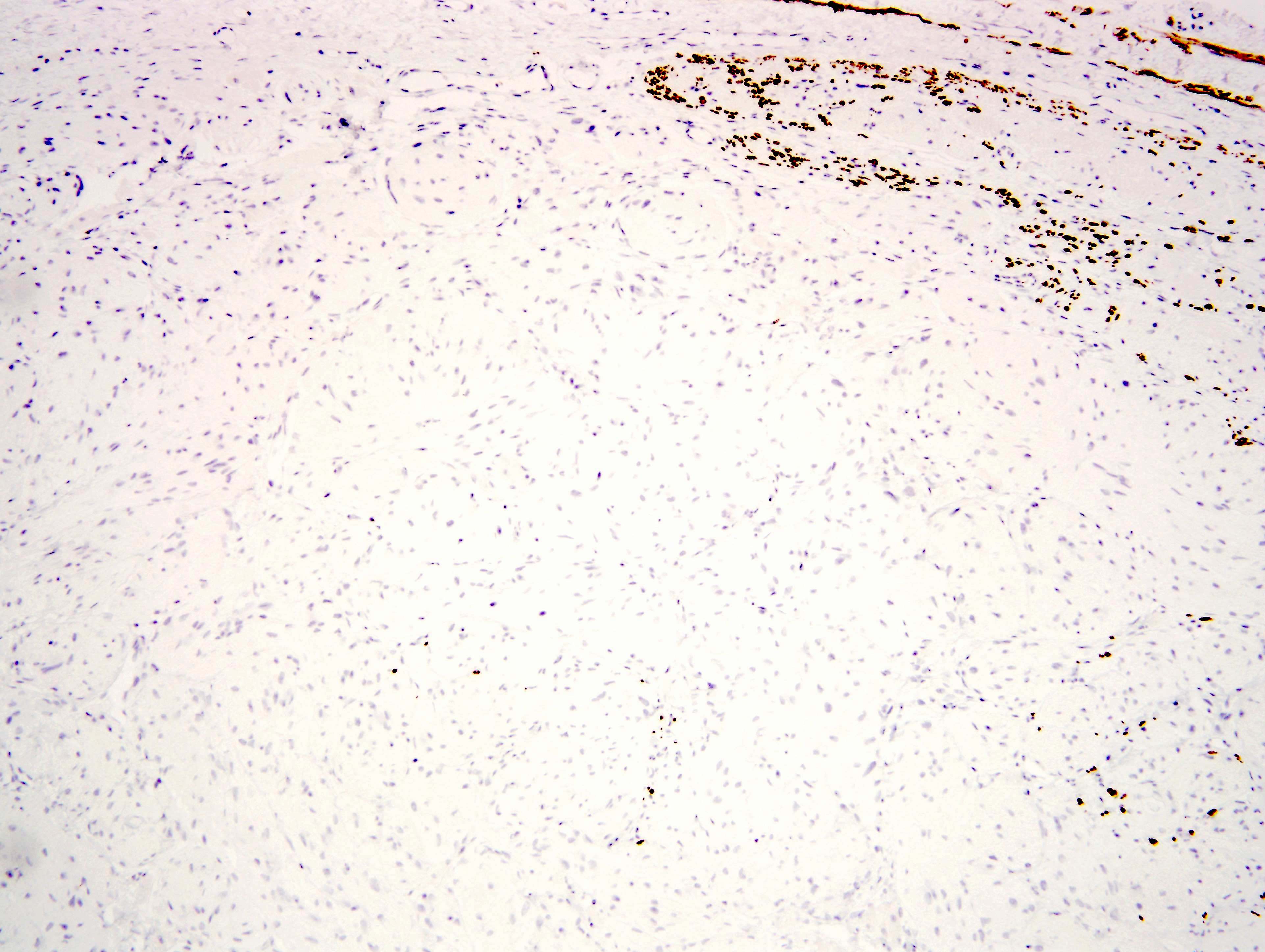
Contributed by Farres Obeidin, M.D. and Christopher Hartley, M.D.
Positive stains
- S100, SOX10, CD68 (100%)
- PGP9.5, inhibin A (100%) (Arch Pathol Lab Med 2004;128:771)
- Neuron specific enolase, CD56, EMA (100%) (Arch Dermatol Res 2015;307:151)
- Calretinin (93%, ranged from focal weak to diffuse strong staining) (Am J Clin Pathol 2003;119:259)
- PASD, nestin (100%), TFE3 (91%) (Hum Pathol 2014;45:1039)
Negative stains
Electron microscopy description
- Cells in small clusters separated by basement membrane material
- Nuclei have irregular, invaginated contour with dense granulation
- Cytoplasm is complex and filled with irregular osmophilic granules
- Occasional unmyelinated axons can be seen among the clusters of granular cells (J Surg Oncol 1980;13:301)
Molecular / cytogenetics description
- Loss of function mutations in ATP6AP1 and ATP6AP2 (Nat Commun 2018;9:3533)
- Single case report of a malignant granular cell tumor showed BRD7 and GFRA2 mutations (Cold Spring Harb Mol Case Stud 2015;1:a000380)
Sample pathology report
- Tongue, mass, resection:
- Granular cell tumor, 1.3 cm (see comment)
- Surgical margins, negative for tumor
- Comment: Microscopic sections show an ill defined proliferation of bland round to ovoid cells with prominent eosinophilic, granular cytoplasm. The overlying epithelium shows pseudoepitheliomatous hyperplasia. S100 and CD68 stains are positive, supporting the diagnosis.
Differential diagnosis
- Reactive histiocytic lesions:
- Mycobacterial pseudotumor / histoid leprosy: presence of acid fast bacilli, often in immunocompromised patients; S100-
- Malakoplakia: histiocytic proliferation with small calcospherocytes (Michaelis-Gutmann bodies); S100-
- Rosai-Dorfman disease: syncytial proliferation with lymphoid background and emperipolesis; S100 and CD68+
- Reaction to silica or polyvinylpyrrolidone (PVP): evidence of exogenous silica or PVP
- Granular cell reaction: cells surround nodules of granular, amorphous debris and are filled with an acid fast and autofluorescent ceroid lipofuscin substance
- Crystal storing histiocytosis: cells filled with refractile crystalline material (immunoglobulin, Charcot-Leyden or clofazimine crystals); S100-
- Cellular spindled histiocytic pseudotumor complicating fat necrosis: arises in the setting of fat necrosis around the breast; S100-
- Alveolar soft part sarcoma:
- Rhabdomyoma:
- Hibernoma:
- Congenital granular cell tumor (congenital epulis):
- Tumors that can rarely have granular cell morphology:
Board review style question #1
A 45 year old man presents with a 1.2 cm mass on the right subcutaneous forearm. The mass is diffusely positive for S100 and CD68. Which of the following is true about this lesion?
- Cells are filled with PAS+, diastase resistant granules
- It's likely reactive in nature and will regress without treatment
- Lesion is associated with multifocal lymphadenopathy
- Overlying epithelium is usually ulcerated and thinned
Board review style answer #1
A. Cells are filled with PAS+, diastase resistant granules. This is a granular cell tumor. The granules are composed of phagolysosomes and are PASD+. They are not reactive and typically need surgery for treatment. Granular cell tumors are not associated with lymphadenopathy and the overlying epithelium is typically hyperplastic, giving a pseudoepitheliomatous appearance.
Comment Here
Reference: Granular cell tumor
Comment Here
Reference: Granular cell tumor
Board review style question #2
Which of the following immunostaining profiles would you expect to see in a granular cell tumor?
- Desmin+, myogenin+, MyoD1+
- S100+, CD1a+, fascin+
- S100+, CD68+, TFE3+
- S100+, SOX10+, HMB45+, MelanA+
Board review style answer #2
C. S100+, CD68+, TFE3+. Granular cell tumors stain with S100, CD68 and TFE3. HMB45 and MelanA positivity favors a melanoma. Desmin and more specific myogenic markers are seen in adult type rhabdomyoma. CD1a and fascin are characteristic for Langerhans cell histiocytosis.
Comment Here
Reference: Granular cell tumor
Comment Here
Reference: Granular cell tumor