Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2 | Board review style question #3 | Board review style answer #3Cite this page: Goldfaden JS, Bilodeau EA. Frictional keratosis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/oralcavityfrictionalkeratosis.html. Accessed April 1st, 2025.
Definition / general
- Frictional keratosis is a group of extremely common, benign, reactive processes that are a result of friction or trauma to the keratinized and nonkeratinized oral mucosa
- These reactive lesions include: linea alba, benign alveolar ridge keratosis, morsicatio buccarum / labiorum (cheek / lip chewing, respectively) and morsicatio linguarum (tongue chewing)
Essential features
- Sources of trauma to the oral mucosa that induce keratosis include normal masticatory function of the dentition, parafunctional habits, food impaction, an ill fitting dental prosthesis in chronic motion, mucosal contact with a hypererupted or sharp tooth, contact with orthodontic appliances and abrasion from tooth brushing (Head Neck Pathol 2020;14:915, Head Neck Pathol 2021;15:572)
- Shaggy hyperkeratosis of the epithelium with occasional surface bacterial colonization and little to no underlying inflammation
- Frictional keratosis is a completely benign process that resolves within 2 weeks of eliminating the source of trauma (Dent J (Basel) 2019;7:15)
- In instances of persistent lesions, a biopsy is prudent to rule out a hereditary or dysplastic process; additionally, a biopsy may be considered for high risk sites or patients with significant risk factors (e.g., smoking)
Terminology
- Linea alba (white line in Latin) is used to describe a horizontal, white, linear shaped lesion typically seen on the bilateral buccal mucosa at the plane of occlusion (JAAD Case Repo 2019;5:694)
- The phrase benign alveolar ridge keratosis, often abbreviated as BARK, was introduced by Natarajan and Woo in 2008 (J Am Acad Dermatol 2008;58:151)
- Their intent was to emphasize the benign nature of keratotic lesions of the keratinized gingiva of the maxillary or mandibular alveolar ridge that is likely traumatic / frictional in origin (J Am Acad Dermatol 2008;58:151)
- The Latin phrase morsicatio buccarum (verbatim translates to biting of the mouth) first appeared in the literature in 1962 by Kocsard, et al. to describe superficial erosions of the bilateral buccal and labial mucosa in an otherwise healthy 17.5 year old medical student (Br J Dermatol 1962;74:454)
- This phenomenon is more commonly termed cheek biting
- If the labial mucosa is involved, this may be referred to as morsicatio labiorum (labiorum meaning of the lips in Latin) (Dent J (Basel) 2019;7:15)
- The term morsicatio linguarum (linguarum is plural for the Latin word lingua, which means the tongue or language) is applied to describe these erosions that affect the lateral tongue (Gen Dent 2015;63:78)
- Likewise, this finding is more commonly called tongue chewing
- The term morsicatio mucosae oris (MMO), from Latin, translates to biting of the mucosa of the mouth and emphasizes the contrast between chronic frictional keratoses and true leukoplakias (J Oral Maxillofac Surg 2009;67:140)
ICD coding
- ICD-10
Epidemiology
- Linea alba is an extremely common form of benign, reactive keratosis that has no specific age or gender predilection (Head Neck Pathol 2021;15:572)
- Benign alveolar ridge keratosis affects a broad age range from 15 to 86 years (median age of 56 years) with a male predilection (67.1% of cases) (Head Neck Pathol 2020;14:915)
- Morsicatio buccarum / labiorum and morsicatio linguarum exhibit a female predilection (F:M = 3:1) and are more common in patients over the age of 35 (Dent J (Basel) 2019;7:15)
Sites
- Linea alba may be found on either one or both buccal mucosae (Head Neck Pathol 2021;15:572)
- The most common site of benign alveolar ridge keratosis is the mandibular retromolar pad, followed by the gingiva / alveolar ridge mucosa in edentulous areas (i.e., sites of previous tooth extractions) (J Am Acad Dermatol 2008;58:151, Head Neck Pathol 2020;14:915)
- 91% of cases involve the mandibular mucosa (J Am Acad Dermatol 2008;58:151)
- Lesions of morsicatio buccarum are typically bilateral and involve the middle aspect of the anterior buccal mucosa and may extend beyond the plane of occlusion (Dent J (Basel) 2019;7:15)
- Likewise, the lesions of morsicatio labiorum and morsicatio linguarum are often bilateral but can be unilateral in some instances (Dent J (Basel) 2019;7:15)
Pathophysiology
- Linea alba is a form of reactive keratosis that is the result of friction from repeated interlocking of the dentition during normal function throughout the day; these lesions are not indicative of a parafunctional habit (Head Neck Pathol 2021;15:572)
- Benign alveolar ridge keratosis is a reactive proliferation of keratosis caused by trauma or friction to the mandibular retromolar pad, an edentulous area of the alveolar ridge mucosa or the gingiva (Head Neck Pathol 2020;14:915)
- Defined by its Latin name, morsicatio is the result of chronic, self induced chewing, biting / nibbling or sucking of the buccal / labial mucosa and the lateral surfaces of the tongue (Dent J (Basel) 2019;7:15)
Etiology
- The sources of trauma / irritation that induce benign alveolar ridge keratosis include food impaction, chronic motion of an ill fitting denture or mucosal contact with an opposing, hypererupted or sharp tooth (Head Neck Pathol 2020;14:915)
- Morsicatio is a parafunctional habit that is more prevalent in those with excessive stress and mental illness (Dent J (Basel) 2019;7:15)
- In addition to parafunctional habits, morsicatio can also be the result of abrasion from tooth brushing, orthodontic appliances and dentures (Head Neck Pathol 2021;15:572)
Clinical features
- Linea alba appears as a uniform, asymptomatic, raised white line of the buccal mucosa along the plane of occlusion
- Benign alveolar ridge keratosis appears as an asymptomatic, nonwipeable white plaque or papule on the crestal keratinized gingiva of the retromolar pad or an edentulous alveolar ridge, often with poorly demarcated borders that blend into the adjacent, uninvolved tissue
- Morsicatio buccarum / labiorum appears as shaggy / thick gray-white plaques of the bilateral buccal / labial mucosa, respectively; similarly, morsicatio linguarum appears as a poorly defined, shaggy white plaque of the lateral tongue that is often bilateral (Dent J (Basel) 2019;7:15)
- Some lesions may slightly sting (Ann Dermatol Venereol 2019;146:594)
Diagnosis
- Linea alba is often an incidental finding and is regarded as a variation of normal oral anatomy
- The lesions of benign alveolar ridge keratosis are often an incidental finding on clinical examination; however, multiple lesions may raise clinical suspicion of proliferative verrucous leukoplakia (Head Neck Pathol 2021;15:572)
- Like the lesions of benign alveolar ridge keratosis, morsicatio is often an incidental finding, though morsicatio buccarum may clinically mimic hereditary conditions such as white sponge nevus, dyskeratosis congenita or hereditary benign intraepithelial dyskeratosis (Dent J (Basel) 2019;7:15)
- The ability to scrape off the shredded keratin of morsicatio may imitate a superficial burn, pseudomembranous candidiasis or materia alba; however, this clinical feature rules out other white lesions that bear resemblance to morsicatio including lichen planus, lichenoid reactions (both contact and drug induced), graft versus host disease and even lupus erythematosus (Dent J (Basel) 2019;7:15)
- Morsicatio linguarum may be clinically concerning for a leukoplakia with dysplasia of the lateral tongue (Dent J (Basel) 2019;7:15)
Prognostic factors
- Linea alba, benign alveolar ridge keratosis, morsicatio buccarum / labiorum and morsicatio linguarum are all benign processes with excellent prognoses
Case reports
- 15 year old girl with a nervous habit of biting her buccal mucosa when studying for exams (Spec Care Dentist 2005;25:214)
- 46 year old woman with a 2 year history of asymptomatic, whitish plaques of the maxillary and mandibular labial mucosa (Clin Case Rep 2023;11:e6946)
- 55 year old man with a 3 year history of sporadic desquamation of the bilateral buccal mucosa (Skinmed 2012;10:114)
- 60 and 61 year old unrelated patients with asymptomatic, nonwipeable, slightly raised, white lines of their buccal mucosae along the plane of occlusion (JAAD Case Rep 2019;5:694)
Treatment
- No treatment is indicated for linea alba
- A biopsy may be performed on morsicatio buccarum to rule out hereditary conditions if suspected (e.g., white sponge nevus, hereditary benign intraepithelial dyskeratosis)
- If the affected mucosa extends beyond the plane of occlusion, hereditary conditions are more likely
- Prior to performing a biopsy, an attempt should be made to identify a source of irritation; with removal of the irritant, resolution of the keratotic lesion should be observed within 2 weeks
- Persistent lesions warrant biopsy (Dent J (Basel) 2019;7:15)
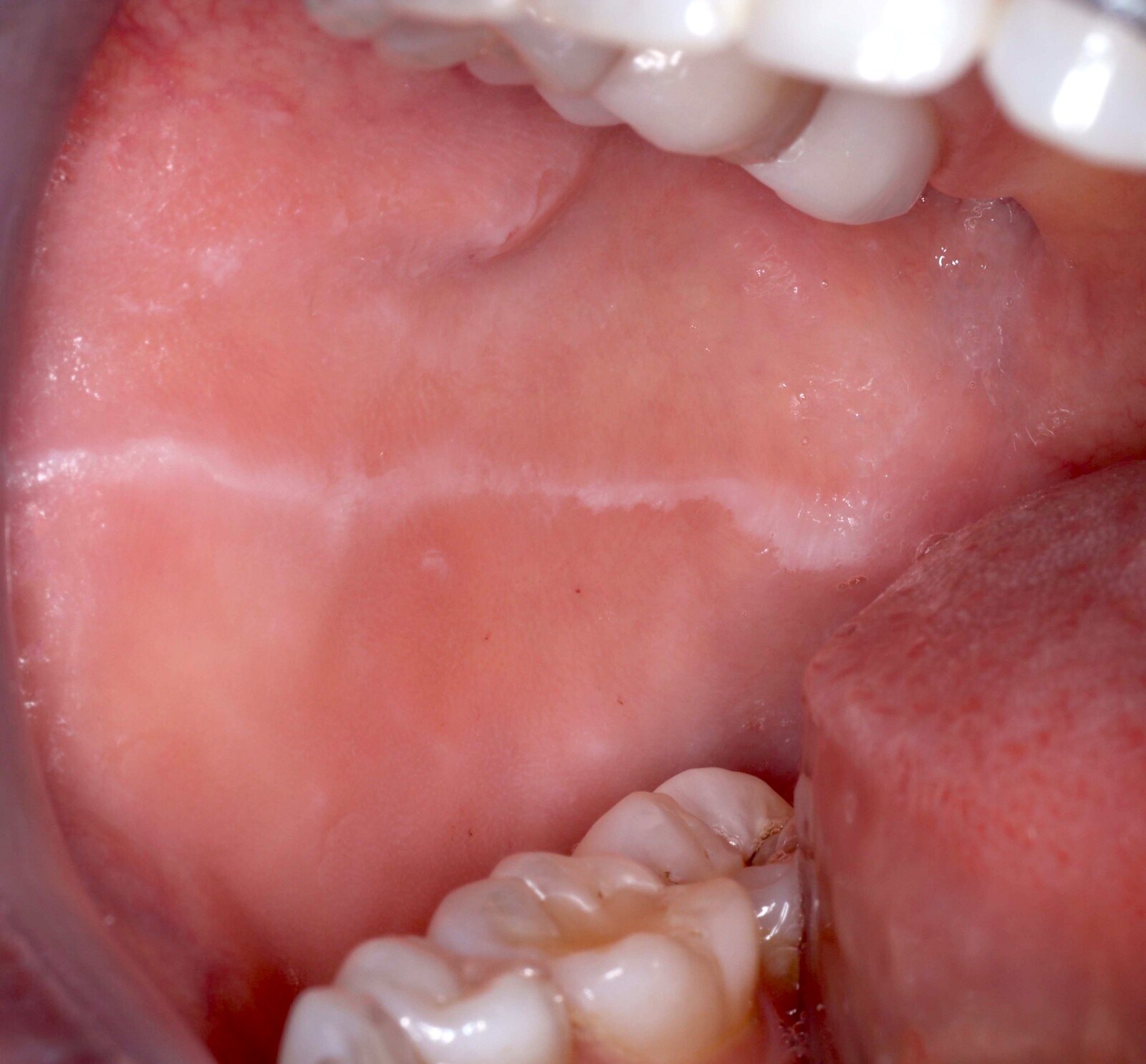
Clinical images
Microscopic (histologic) description
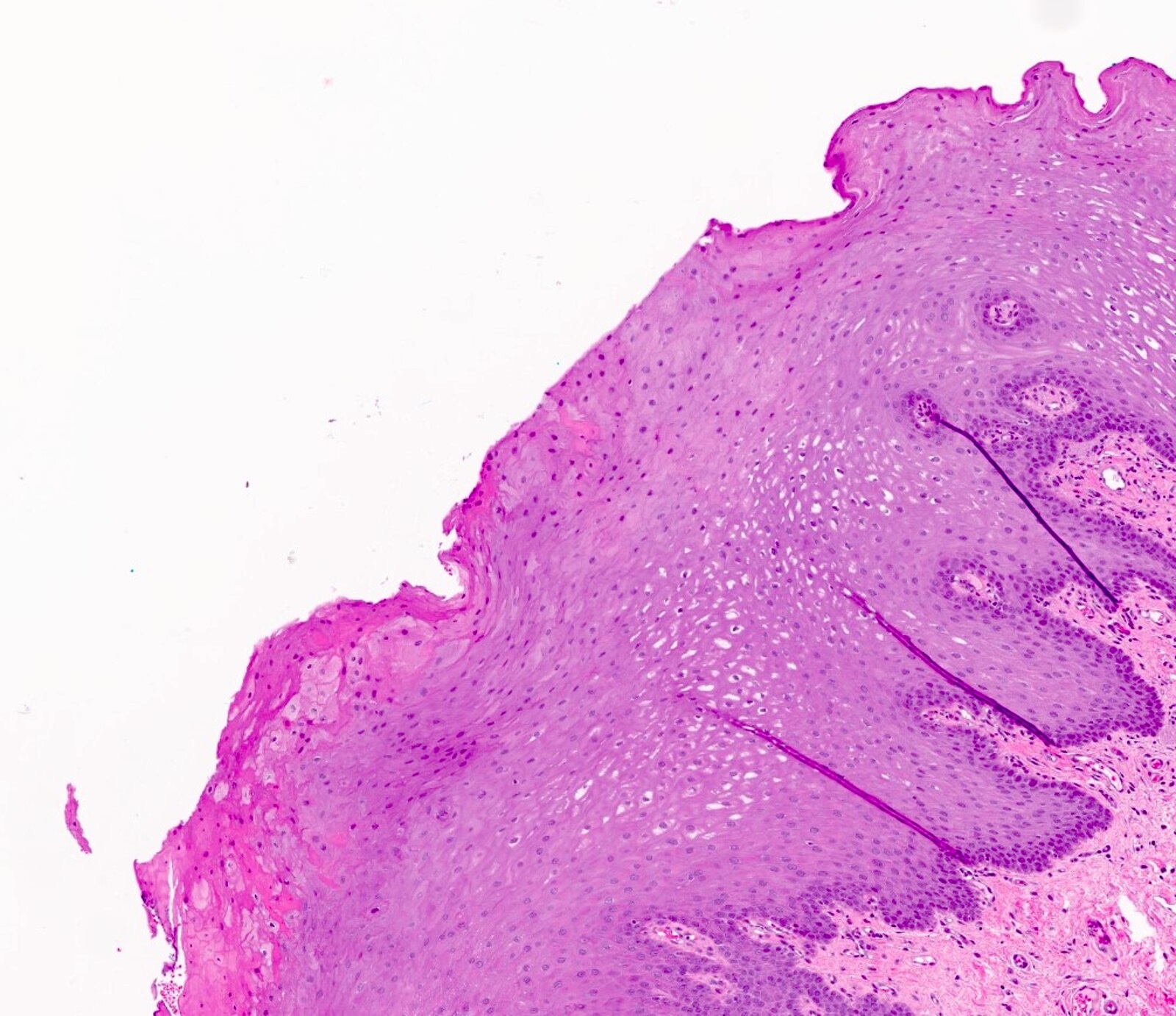
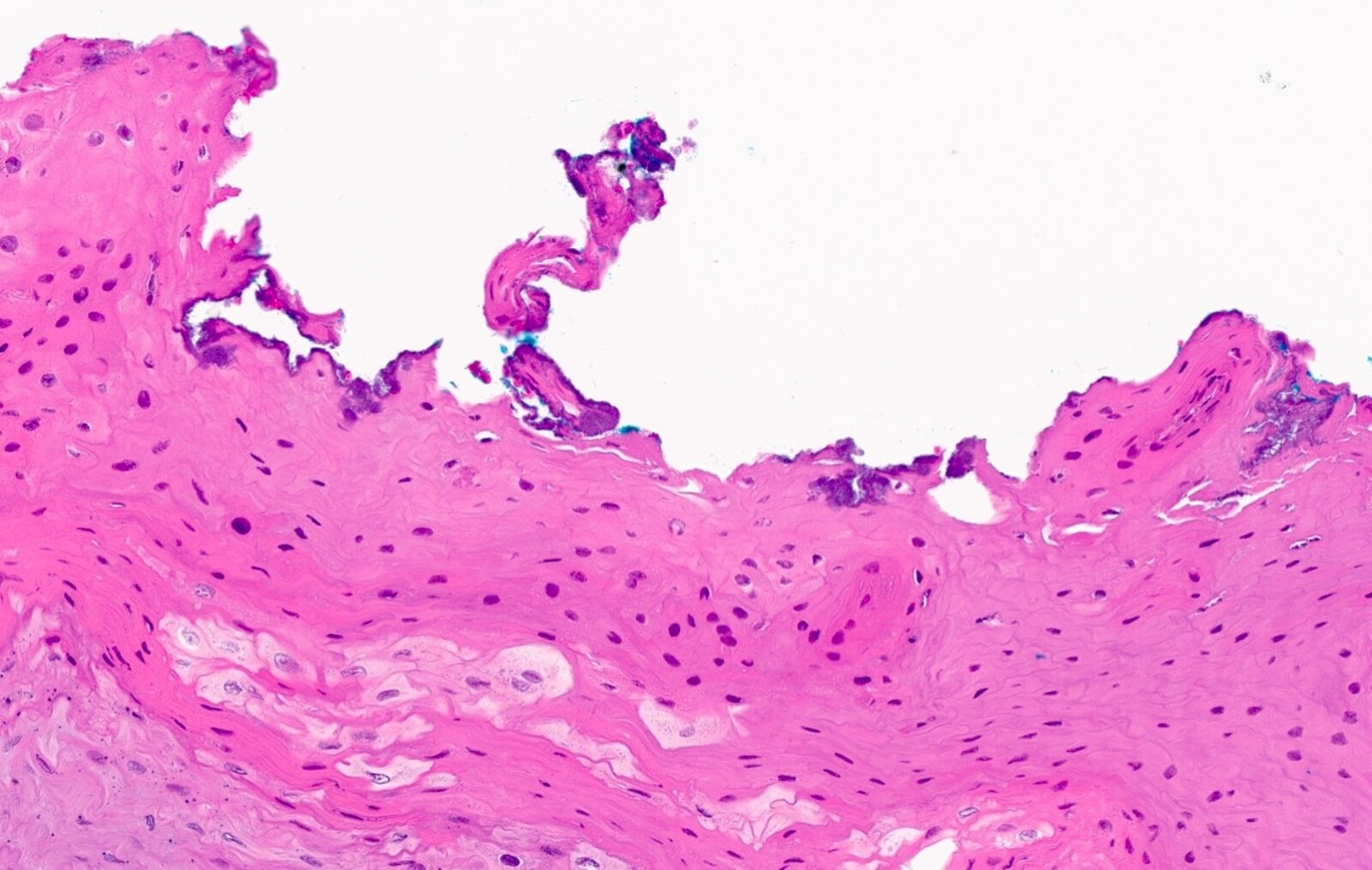
- Linea alba
- Parakeratosis overlying otherwise unremarkable stratified squamous epithelium
- Intracellular edema of keratinocytes and mild chronic inflammation of the stroma may be seen in some cases
- Parakeratosis overlying otherwise unremarkable stratified squamous epithelium
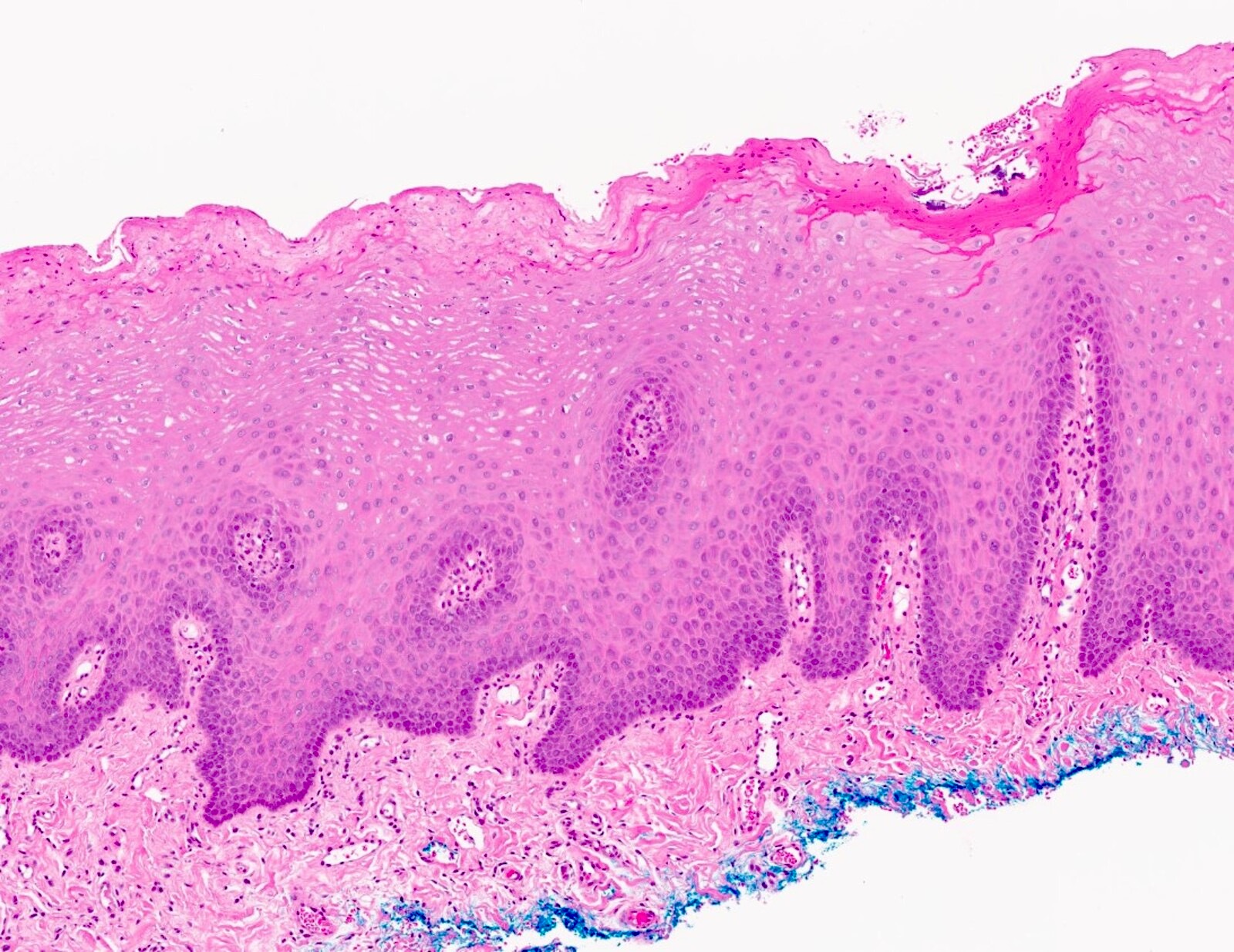
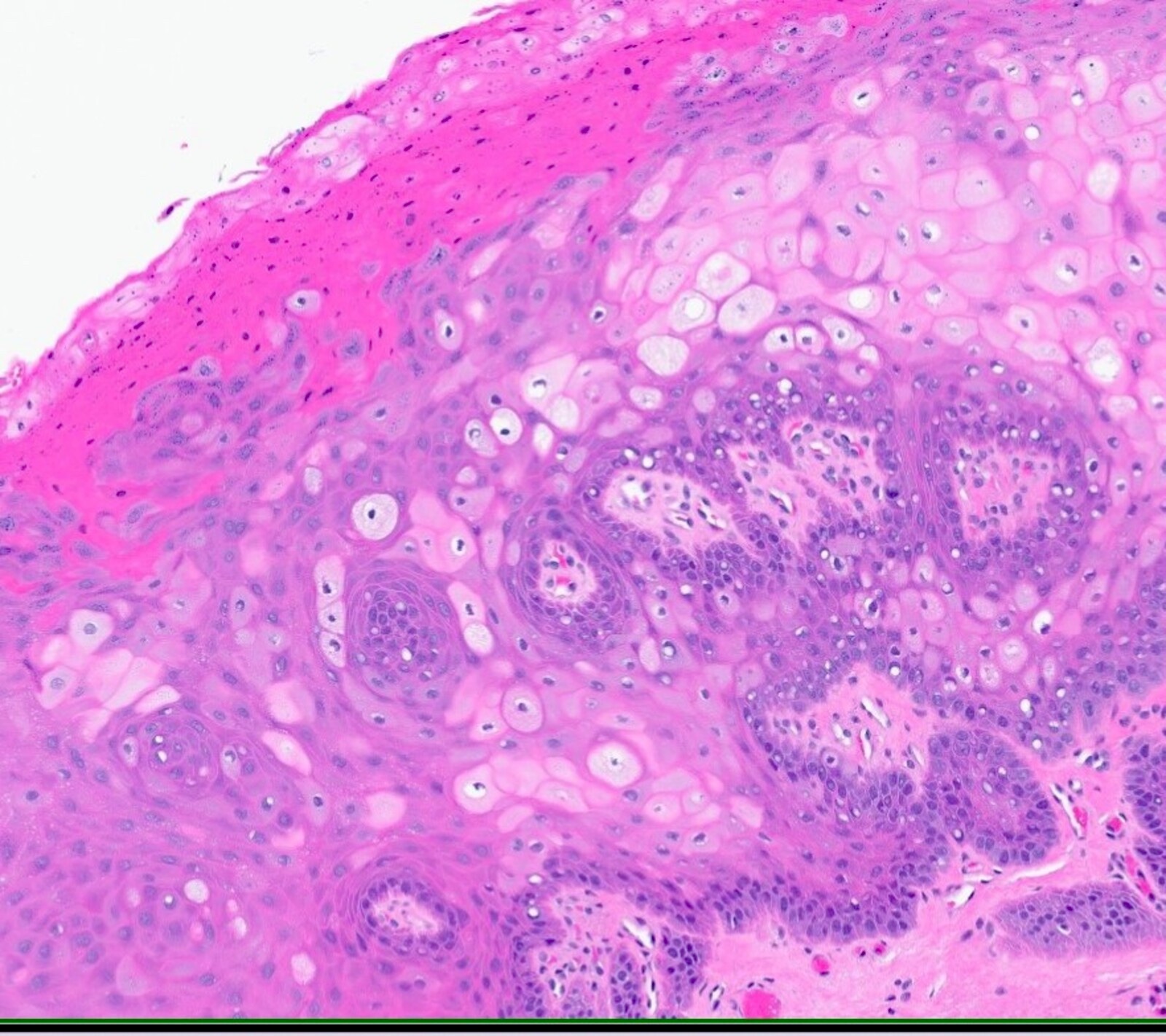
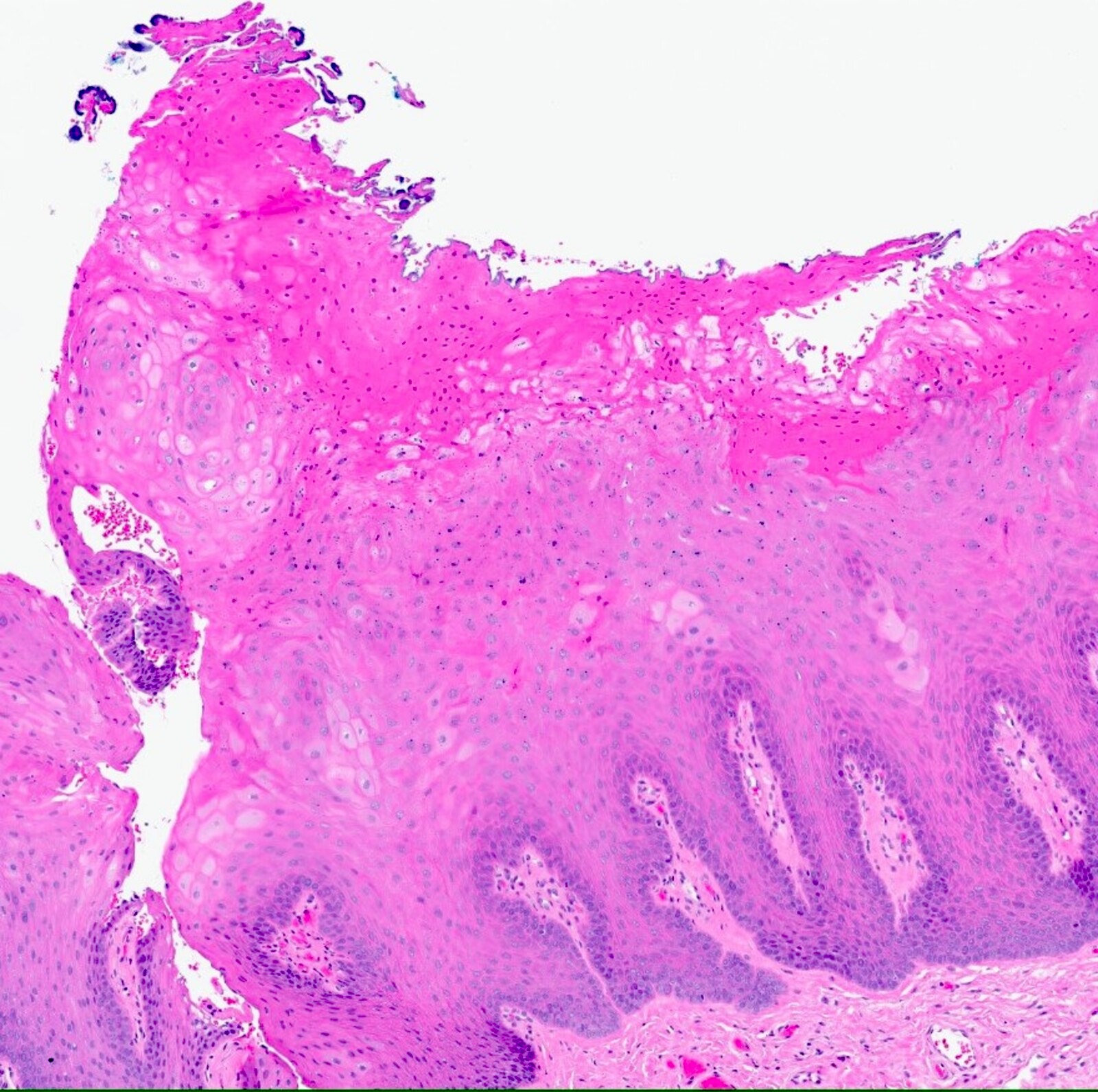
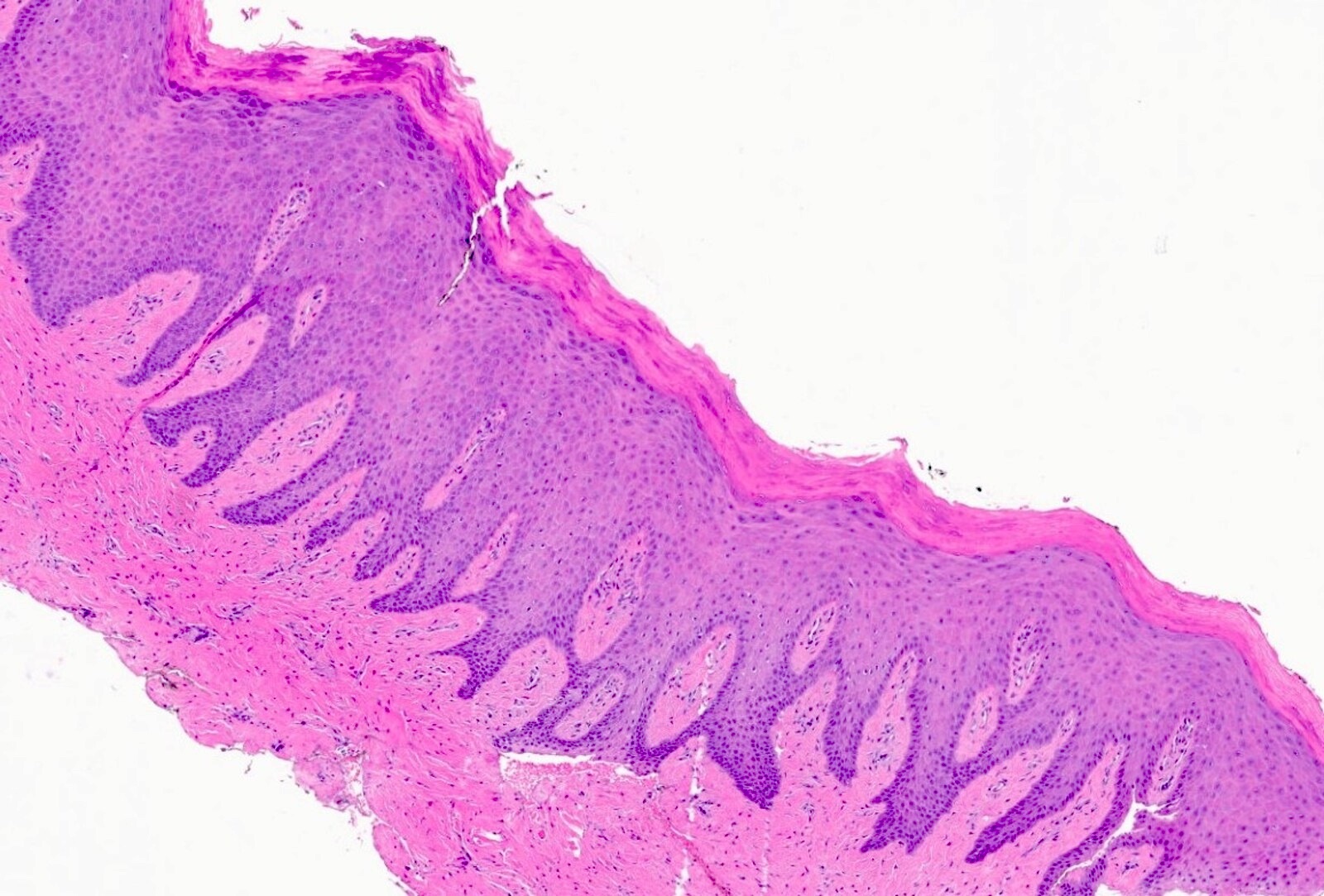
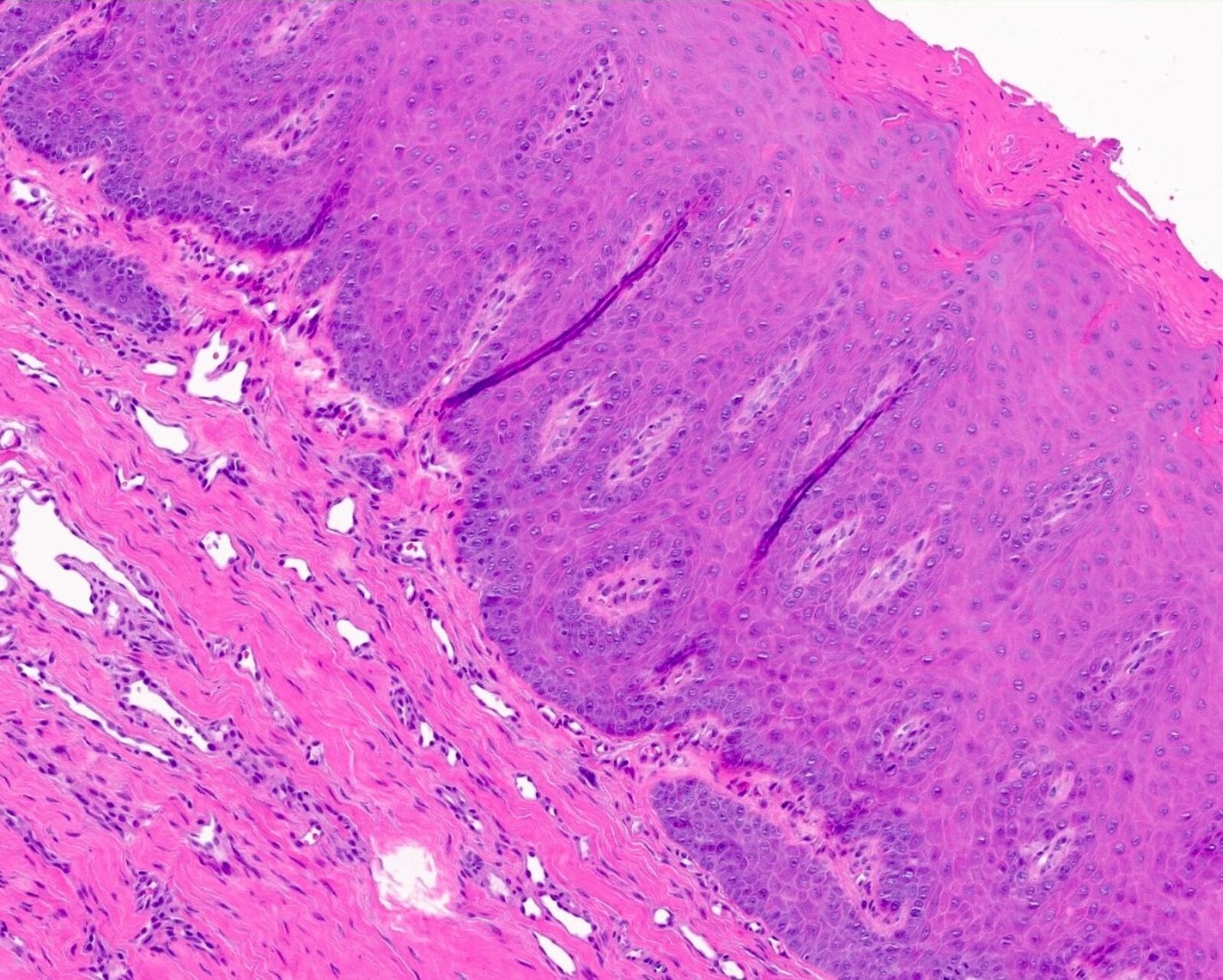
- Benign alveolar ridge keratosis
- Parakeratosis or orthokeratosis and granulosis of the epithelium; the keratin layer may be shaggy and surface bacterial colonization may be observed (Head Neck Pathol 2020;14:915, Head Neck Pathol 2021;15:572)
- Abrupt orthokeratotic / parakeratotic transitions should not be seen
- Rete ridges are elongated, taper from superficial to deep and interconnect at their bases; vascular ectasia may be seen at the tips of the rete and stromal inflammation is scant or absent (Head Neck Pathol 2020;14:915)
- No plasma pools in the superficial epithelium nor edema of keratinocytes are observed (Head Neck Pathol 2021;15:572)
- Parakeratosis or orthokeratosis and granulosis of the epithelium; the keratin layer may be shaggy and surface bacterial colonization may be observed (Head Neck Pathol 2020;14:915, Head Neck Pathol 2021;15:572)
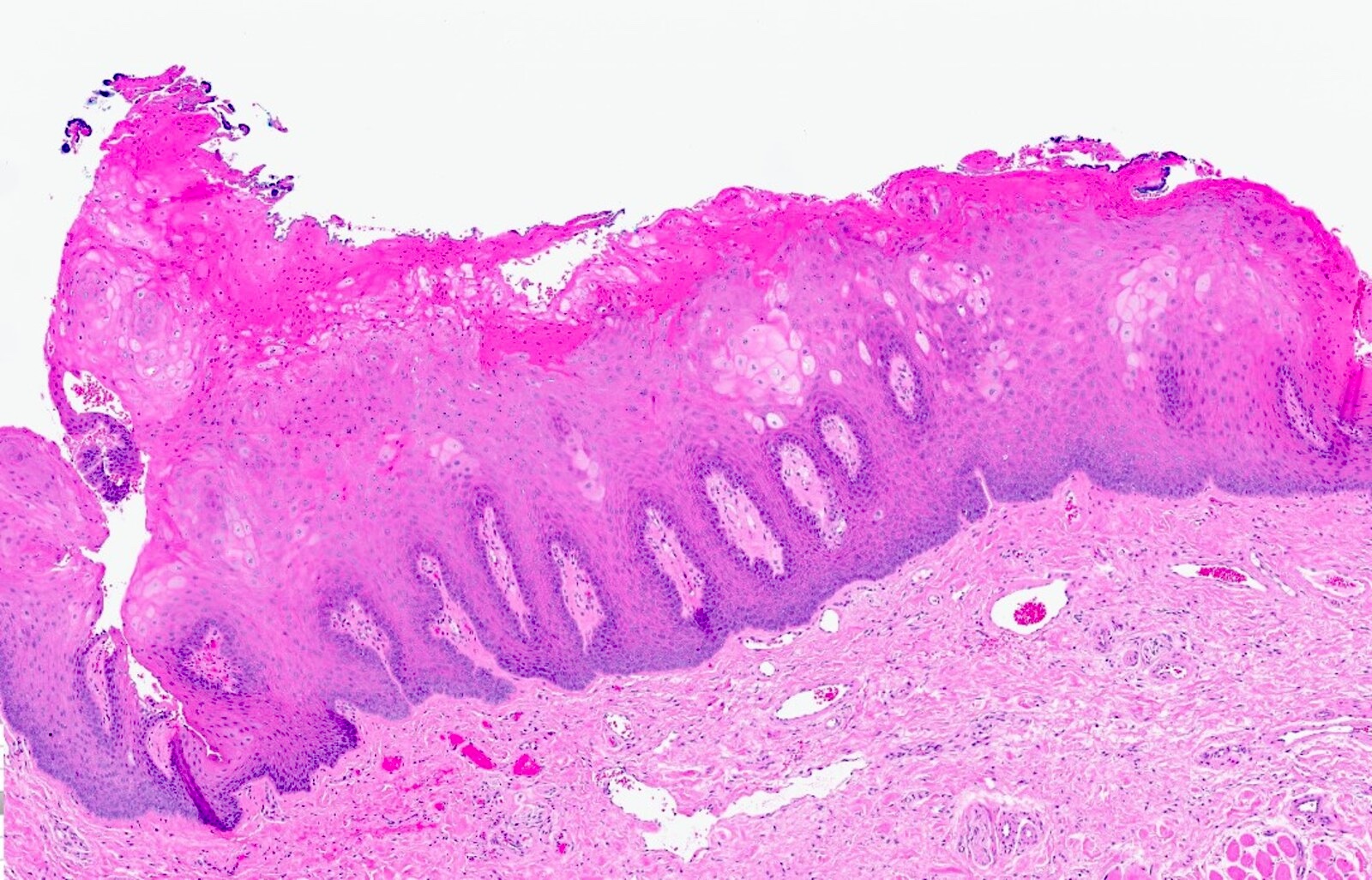
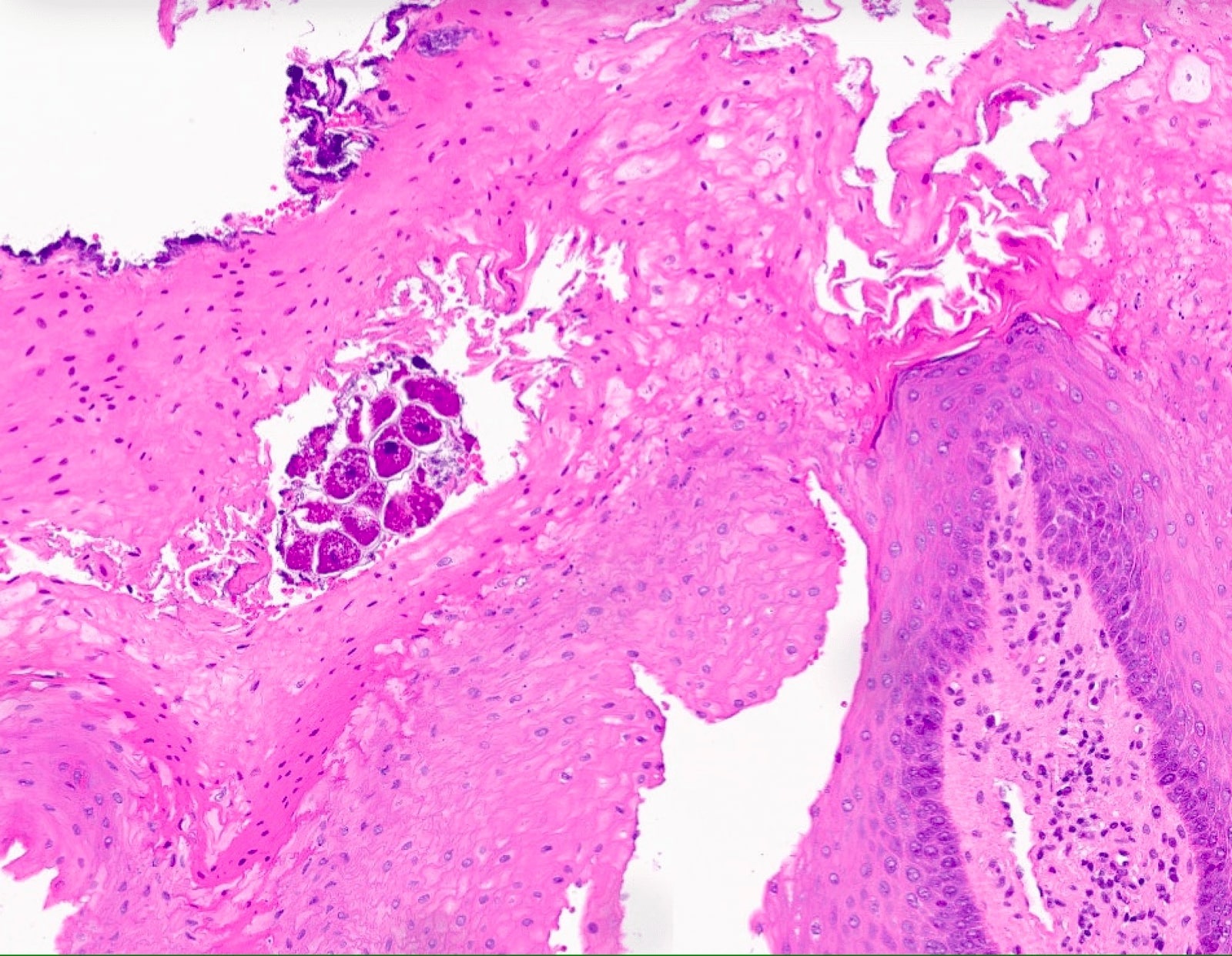
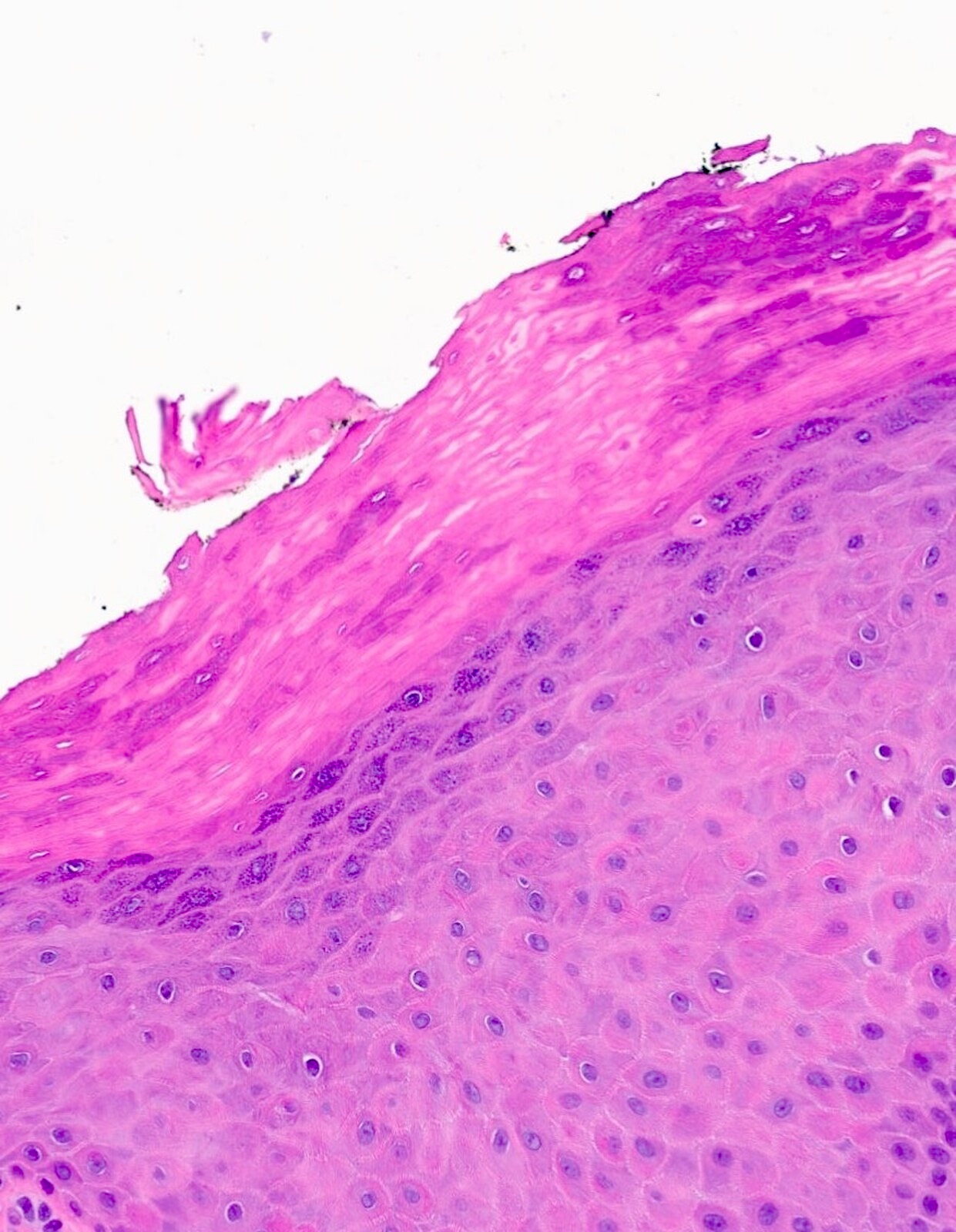
- Morsicatio buccarum / labiorum and morsicatio linguarum
- Acanthosis and parakeratosis with normal maturational changes of keratinocytes
- Edema is present within keratinocytes; plasma pooling may also be noted in superficial epithelium (Head Neck Pathol 2021;15:572)
- Surface parakeratin is ragged / shaggy in appearance; bacterial colonies and food debris may be noted within this ragged keratin
- Stromal inflammatory infiltrate may or may not be present (Head Neck Pathol 2021;15:572)
- Acanthosis and parakeratosis with normal maturational changes of keratinocytes
Microscopic (histologic) images
Contributed by Joshua Seth Goldfaden, D.D.S.
Linea alba, morsicatio buccarum / labiorum and morsicatio linguarum
Benign alveolar ridge keratosis
Positive stains
- p53 exhibits nonextreme staining (nonmutated) in benign, reactive processes including benign alveolar ridge keratosis and morsicatio (Head Neck Pathol 2020;14:915)
Negative stains
Sample pathology report
- Buccal mucosa, left, linea alba, incisional biopsy:
- Hyperkeratosis
- Retromolar pad, right, distal to #31, excisional biopsy:
- Hyperkeratosis
- Buccal mucosa, left, incisional biopsy:
- Ragged keratosis with superficial bacterial colonies (see comment)
- Comment: The histologic findings are consistent with morsicatio buccarum.
- Lateral tongue, right, incisional biopsy:
- Ragged keratosis with superficial bacterial colonies (see comment)
- Comment: The histologic findings are consistent with morsicatio linguarum.
Differential diagnosis
- Materia alba:
- Accumulation of desquamated epithelial cells with bacterial colonies and food debris, such as vegetable matter
- Clinically, materia alba presents as a wipeable plaque that reveals normal, uninflamed underlying attached mucosa
- Accumulation of desquamated epithelial cells with bacterial colonies and food debris, such as vegetable matter
- White sponge nevus:
- Parakeratotic epithelium with acanthosis and spongiosis
- Rete ridges are large and blunted
- Epithelial cells exhibit compact eosinophilic peri and paranuclear condensation
- Leukoedema:
- Parakeratinized, acanthotic epithelium with widened, elongated rete ridges
- Spinous layer keratinocytes demonstrate hydropic degeneration (intracellular edema) with pyknotic nuclei
- Hereditary benign intraepithelial dyskeratosis:
- Parakeratotic epithelium with acanthosis and keratinocyte discohesion in the superficial layers
- Keratinocytes throughout epithelium exhibit dyskeratosis
- The dyskeratotic process of this condition creates the illusion that keratinocytes appear to be engulfed by adjacent keratinocytes creating a "cell within a cell" appearance
- Smokeless tobacco keratosis:
- Parakeratosis or orthokeratosis with acanthosis and church spires (chevroning)
- Basket weaving / hydropic degeneration of the spinous layer epithelium may be seen
- These epithelial cells may exhibit pyknotic nuclei
- Mild chronic inflammation of the underlying connective tissue may be present
- Oral hairy leukoplakia:
- EBER is positive in the spinous cell layer
- Parakeratosis and ballooning degeneration of the spinous keratinocytes
- Margination of chromatin (i.e., nuclear beading) of the spinous keratinocytes is observed; koilocytosis may also be noted
- Both phenomena are cytopathic effects of an Epstein-Barr virus infection
- Candidal organisms may be seen in the superficial epithelium, though an inflammatory response is typically absent
- Dysplasia (unifocal):
- Expansion of basilar compartment and teardrop shaped rete ridges
- Nuclear and cellular pleomorphism with increased N:C ratio
- Nuclei may be hyperchromatic
- Increased mitotic activity, single cell dyskeratosis and glassy appearance of some keratinocytes
- Proliferative verrucous leukoplakia (PVL):
- Skip lesions consisting of sharply demarcated, alternating segments of orthokeratin and parakeratin
- The keratin layer exhibits a verrucous / spiky architecture
- Rete ridges may be bulbous, interconnect and exhibit downward pushing
- This architectural dysplasia may obscure cytologic atypia
- Epithelium may be atrophic in some instances
- Skip lesions consisting of sharply demarcated, alternating segments of orthokeratin and parakeratin
- Verrucous carcinoma:
- Verrucous / papillary keratosis of the surface epithelium
- Chevroning and deep keratin clefting are also noted
- Broad, frond-like, bulbous rete ridges that demonstrate endophytic growth into the submucosa
- Basement membrane remains intact
- Keratinocytes are bland with minimal cytologic atypia
- Verrucous / papillary keratosis of the surface epithelium
- Hyperplastic candidiasis:
- Keratosis and acanthosis of the surface epithelium
- Pseudohyphae are present in the stratum corneum and are oriented perpendicular to the epithelium
- Pseudoepitheliomatous hyperplasia including elongated and bulbous rete ridges with a downward proliferating architecture; no cytologic atypia is observed
- Underlying chronic inflammation with transmigratory neutrophils forming microabscesses in the stratum granulosum
- Lichen planus (plaque form):
- Orthokeratosis or parakeratosis of the surface epithelium with Civatte bodies scattered throughout
- Thickening of the basement membrane and hydropic degeneration of the basal cell layer
- Hydropic degeneration of the basal cell layer may cause the rete ridges to appear saw toothed
- Dense band of lymphohistiocytic inflammation immediately subjacent to the surface epithelium
- Dyskeratosis congenita:
- Orthokeratosis and atrophy of the squamous epithelium
- Over time, the lesions of this condition develop dysplastic changes and evolve into squamous cell carcinoma
Board review style question #1
A 55 year old man presents with a nonwipeable, ill defined white plaque of the right retromolar pad, distal to tooth #31. A biopsy of the lesion reveals stratified squamous epithelium with shaggy surface parakeratin, elongated, tapered rete ridges that coalesce and no cytologic atypia or stromal inflammation. Based on the clinical and histopathologic findings, what is the most appropriate diagnosis?
- Benign alveolar ridge keratosis (BARK)
- Dysplasia
- Lichen planus
- Materia alba
Board review style answer #1
A. Benign alveolar ridge keratosis (BARK). A retromolar pad lesion with shaggy surface parakeratin, elongated, tapered rete ridges that coalesce and no stromal inflammation is consistent with benign alveolar ridge keratosis. Answer B is incorrect because dysplasia exhibits basal cell proliferation and teardrop shaped rete ridges; additionally, cellular and nuclear pleomorphism and increased mitotic activity are also characteristic of dysplasia. Answer C is incorrect because lichen planus exhibits saw toothed rete ridges, hydropic degeneration of the basal cell layer, Civatte bodies within the epithelium, thickening of the basement membrane and a tight band of lymphohistiocytic inflammation. Answer D is incorrect because materia alba is wipeable clinically and is histopathologically characterized by desquamated epithelial cells associated with bacterial colonies and food debris.
Comment Here
Reference: Frictional keratosis
Comment Here
Reference: Frictional keratosis
Board review style question #2
A 22 year old female college student who is anxious about her upcoming final examinations presents with an ill defined white plaque of the lateral tongue. A biopsy is performed. Based on the photomicrograph, what is the most appropriate diagnosis?
- Dysplasia
- Lichen planus
- Morsicatio linguarum
- Oral hairy leukoplakia
Board review style answer #2
C. Morsicatio linguarum. A lateral tongue lesion with ragged surface parakeratin, normal maturational changes of the epithelium, keratinocyte edema and surface bacterial colonization is consistent with morsicatio linguarum; additionally, a cause of trauma based on the patient’s social history is evident. Answer A is incorrect because dysplasia exhibits basal cell proliferation and teardrop shaped rete ridges; additionally, cellular and nuclear pleomorphism and increased mitotic activity are also characteristic of dysplasia. Answer B is incorrect because lichen planus exhibits saw toothed rete ridges, hydropic degeneration of the basal cell layer, Civatte bodies within the epithelium, thickening of the basement membrane and a tight band of lymphohistiocytic inflammation. Answer D is incorrect because oral hairy leukoplakia exhibits positive EBER in situ hybridization, ballooning degeneration of the spinous layer of epithelium and nuclear beading of the chromatin.
Comment Here
Reference: Frictional keratosis
Comment Here
Reference: Frictional keratosis
Board review style question #3
A 13 year old boy with orthodontic brackets and wires presents with bilateral, shagged, diffuse, white plaques of the buccal mucosae. An incisional biopsy reveals ragged surface parakeratin with surface bacterial colonization, normal maturational changes, superficial keratinocyte edema and minimal stromal inflammation. Based on the histopathologic findings, what is the most appropriate diagnosis?
- Hereditary benign intraepithelial dyskeratosis
- Leukoedema
- Morsicatio buccarum
- White sponge nevus
Board review style answer #3
C. Morsicatio buccarum. Bilateral buccal mucosa lesion with ragged surface parakeratin, normal maturational changes of the epithelium, keratinocyte edema and surface bacterial colonization are consistent with morsicatio buccarum; additionally, a source of trauma (i.e., orthodontic appliances) is readily identifiable. Answer A is incorrect because hereditary benign intraepithelial dyskeratosis exhibits discohesion of the superficial layers of the epithelium and individual keratinocyte dyskeratosis that may create a "cell within a cell" appearance of the epithelium. Answer B is incorrect because the histopathologic appearance of leukoedema consists of widened, elongated rete ridges and hydropic degeneration of the spinous layer with pyknotic nuclei. Answer D is incorrect because white sponge nevus exhibits spongiotic epithelium with large, blunted rete ridges and epithelial cells with peri and paranuclear eosinophilic condensation.
Comment Here
Reference: Frictional keratosis
Comment Here
Reference: Frictional keratosis