Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Molecular / cytogenetics images | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1Cite this page: Smith MH. Ectomesenchymal chondromyxoid tumor. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/oralcavityect.html. Accessed December 26th, 2024.
Definition / general
- Rare, benign soft tissue tumor with striking predilection for the anterior dorsal tongue
- First named by Smith et al. in 1995 (Am J Surg Pathol 1995;19:519)
Essential features
- Most are found on the anterior dorsal tongue
- Fewer than 120 well documented cases have been reported
- Histopathologically demonstrates a well defined, often multilobulated tumor with ovoid, round, fusiform or polygonal cells within a sometimes myxoid, chondromyxoid or mucoid background
- Reticular arrangement of cells is often noted
- Characterized by RREB1::MRTFB (previously MKL2) fusion in 90% of cases (Am J Surg Pathol 2018;42:1297)
- Conservative excision recommended; < 10% have recurred
Terminology
- Ectomesenchymal chondromyxoid tumor of the anterior tongue (Am J Surg Pathol 1995;19:519)
ICD coding
- ICD-10: D10.1 - benign neoplasm of tongue
Epidemiology
- No sex predilection
- Average age ~40 years
- Age range is from 2.3 - 78 years (Cleft Palate Craniofac J 2022;59:932, Am J Surg Pathol 1995;19:519)
Sites
- Striking predilection for anterior dorsal tongue
- Rare cases reported in other oral locations
- Posterior tongue / base of tongue (Am J Surg Pathol 2018;42:1297, Cleft Palate Craniofac J 2022;59:932, Head Neck Pathol 2014;8:329, Oral Oncol 2017;67:192)
- Gingiva / anterior hard palate (Int J Oral Sci 2018;10:4, Oral Surg Oral Med Oral Pathol Oral Radiol 2012;114:154)
- Buccal mucosa (J Am Dent Assoc 2015;146:196)
- Mandible (Head Neck Pathol 2021;15:319)
- Cases with the same RREB1::MRTFB fusion and overlapping morphologic features have been noted in extraoral sites
- It is unclear whether these tumors are completely different entities or if they represent a variation of ectomesenchymal chondromyxoid tumor
- Mediastinum (Histopathology 2020;76:1023)
- Maxillo-ethmoidal angle, reported as a biphenotypic sinonasal sarcoma (Genes Chromosomes Cancer 2021;60:565)
- Oropharynx, reported as a biphenotypic oropharyngeal sarcoma (Genes Chromosomes Cancer 2018;57:203)
Etiology
- Currently considered as tumors of uncertain histogenesis by WHO classification
- Most authors support neural crest origin (Am J Surg Pathol 1995;19:519)
- Supported by the fact that the anterior tongue derives from the neural crest mesenchyme of the first branchial arch (Head Neck Pathol 2015;9:315)
- Pluripotency of the neural crest may explain the significant immunohistochemical variability (Oral Surg Oral Med Oral Pathol Oral Radiol 2021;132:4, Oral Oncol 2006;42:1026)
- Markers for undifferentiated embryonic stem cells (OCT 3/4, SOX2, Nanog, MAP2, CD105 mRNAs) have been found in ectomesenchymal chondromyxoid tumors (Oral Surg Oral Med Oral Pathol Oral Radiol 2013;115:233)
- Some authors cite potential link between ectomesenchymal chondromyxoid tumor and myoepithelioma of soft parts (Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2005;99:581, Histopathology 2016;69:607)
Clinical features
- Slow growing, usually asymptomatic, firm submucosal nodule on anterior dorsal tongue
- Purulent drainage noted in one case report (Anticancer Research 2010;30:4685)
- Tumor size ranges from 0.3 - 4.0 cm (Am J Surg Pathol 1995;19:519, Oral Oncol 2017;67:192)
- Pain is rarely noted (Advances in Oral and Maxillofacial Surgery 2021;1:100006)
Diagnosis
- Diagnosis is made on histopathological examination
Radiology description
- Isointense signal or low intensity signal on T1 weighted MRI and hyperintense signal on T2 weighted MRI (Oral Surg Oral Med Oral Pathol Oral Radiol 2013;115:233, Oral Oncol 2017;67:192, BMJ Case Rep 2019;12:e231278)
- Case detailing CT scan without contrast shows cystic appearing lesion with hemorrhagic areas (Head Neck Pathol 2014;8:329)
Radiology images
Prognostic factors
- 5 cases (< 10% of reported cases with follow up information) are reported to have recurred (Am J Surg Pathol 2018;42:1297, Am J Surg Pathol 1995;19:519, Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009;108:e20)
- Local re-excision appears curative (Oral Dis 2008;14:390)
Case reports
- 26 year old woman with slow growing nodule on the anterior dorsal tongue (Advances in Oral and Maxillofacial Surgery 2021;1:100006)
- 37 year old woman with expansile radiolucency in the body of the mandible (Head Neck Pathol 2021;15:319)
- 43 year old man with mass on posterior dorsal tongue (Head Neck Pathol 2014;8:329)
- 46 year old man with anterior dorsal tongue mass, present for 5 years (BMJ Case Rep 2019;12:e231278)
Treatment
- Conservative surgical excision is recommended (Int J Surg Case Rep 2017;41:162, Oral Dis 2008;14:390)
Gross description
- Firm, well defined tumor
- White, tan, yellow or gray in color (Am J Surg Pathol 1995;19:519, Acta Cytol 2010;54:82, Oral Surg Oral Med Oral Pathol Oral Radiol 2021;132:4)
- Cystic, gelatinous or hemorrhagic areas often are described (Virchows Arch 2003;442:302, Int J Surg Pathol 2016;24:586, Oral Surg Oral Med Oral Pathol Oral Radiol 2021;132:4)
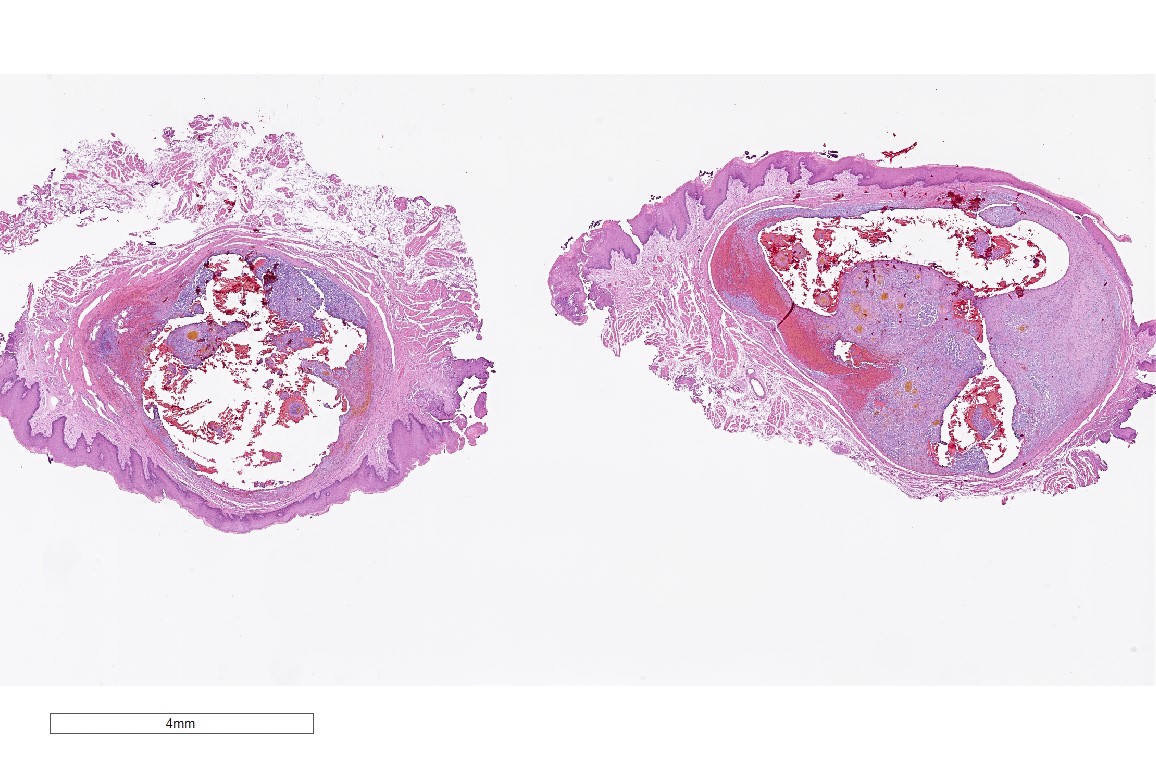
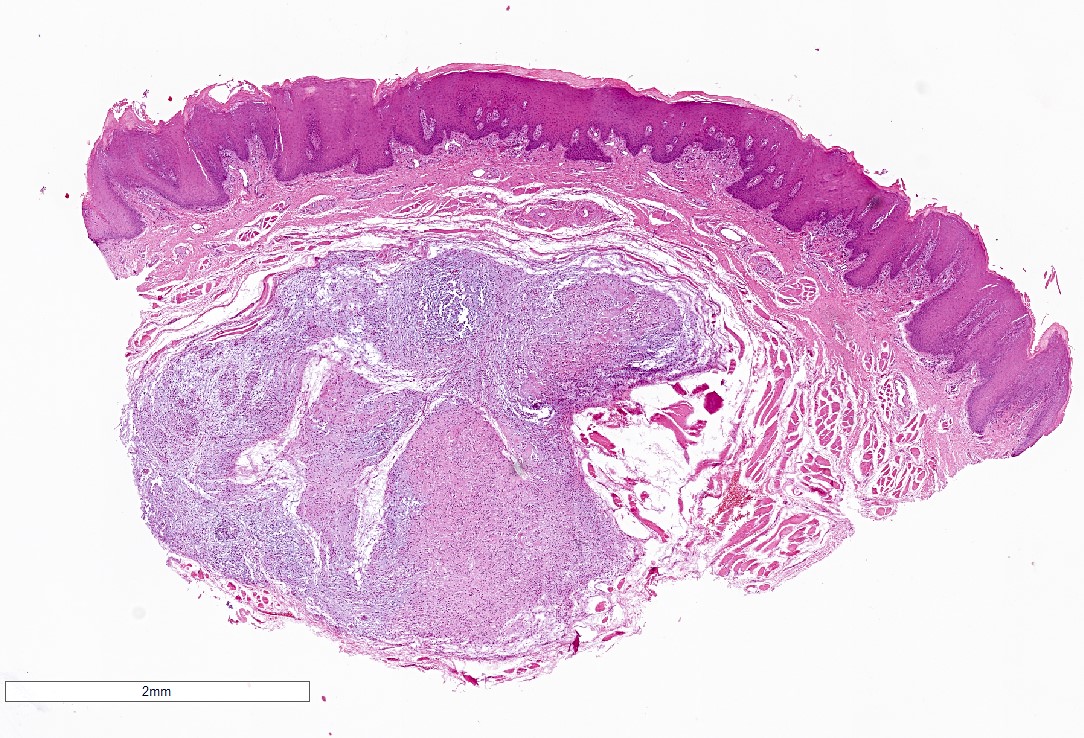
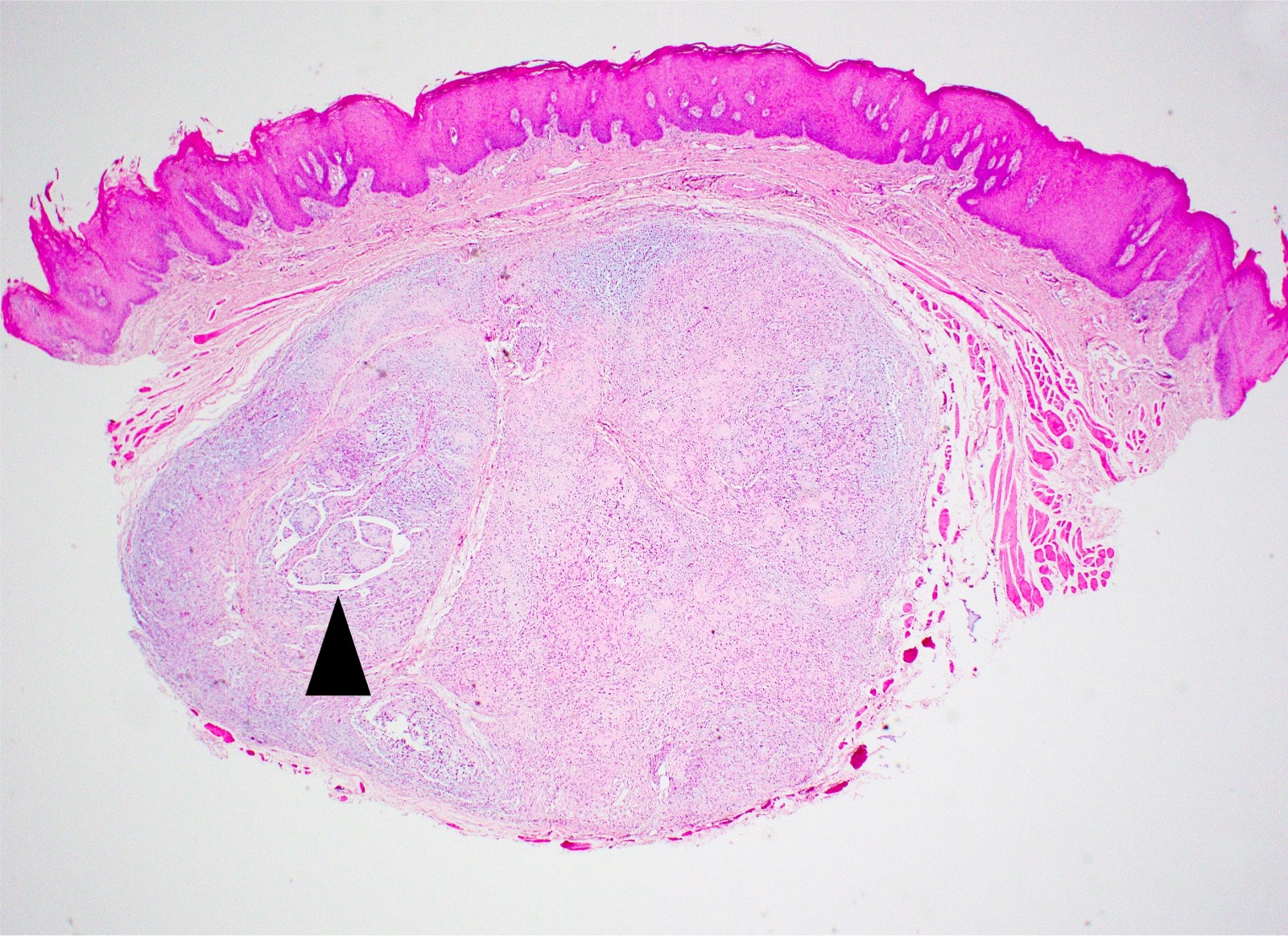
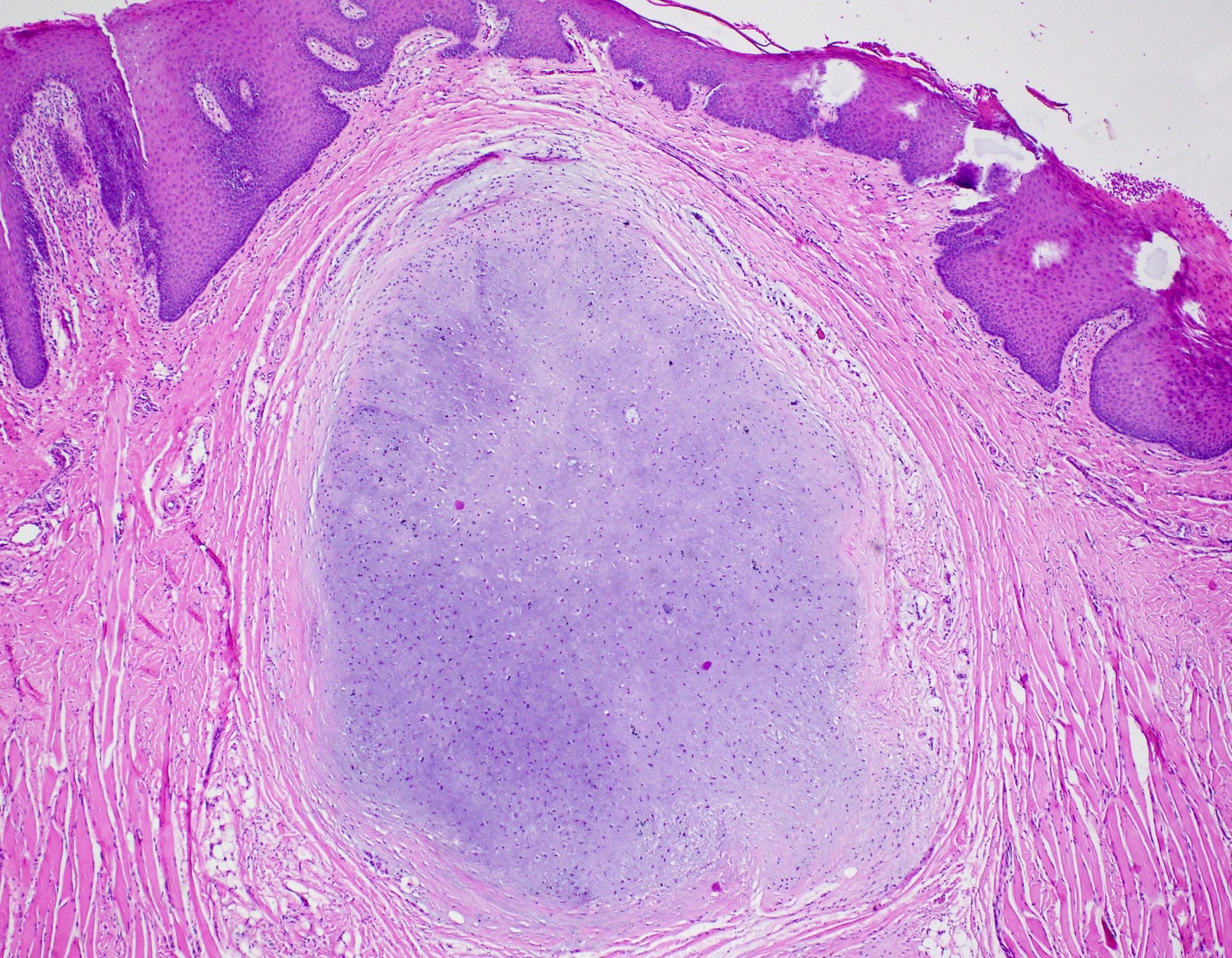
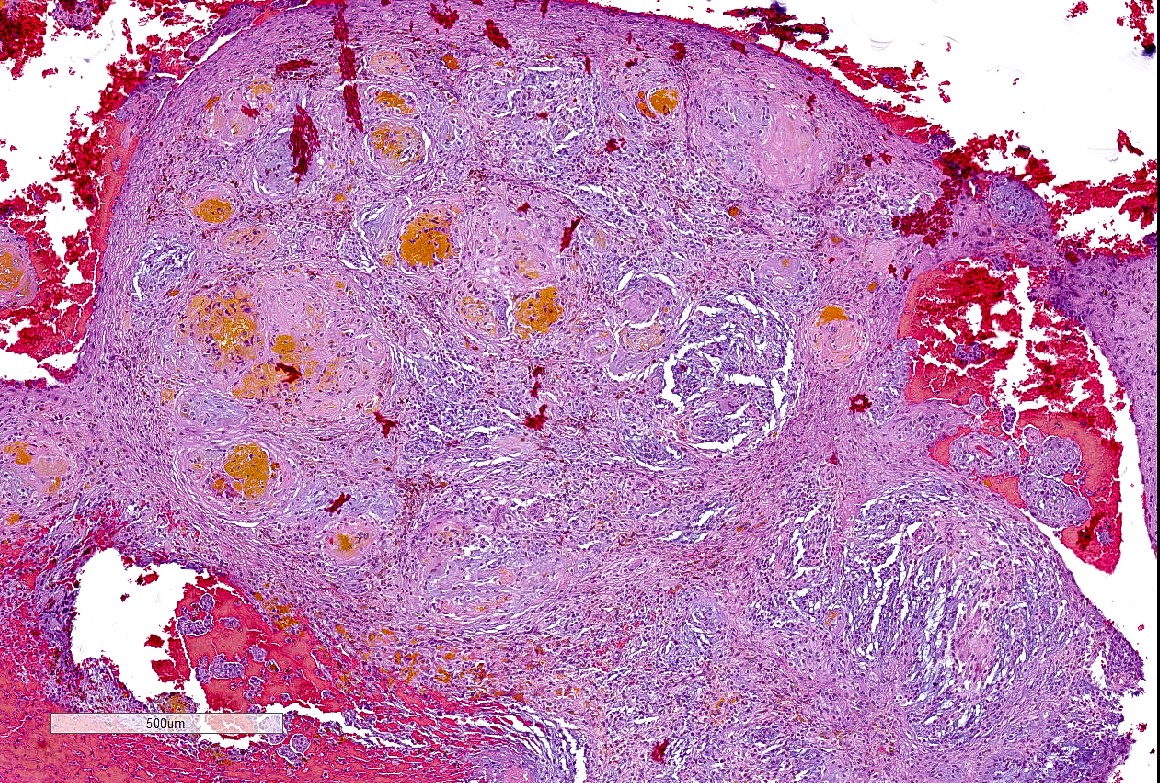
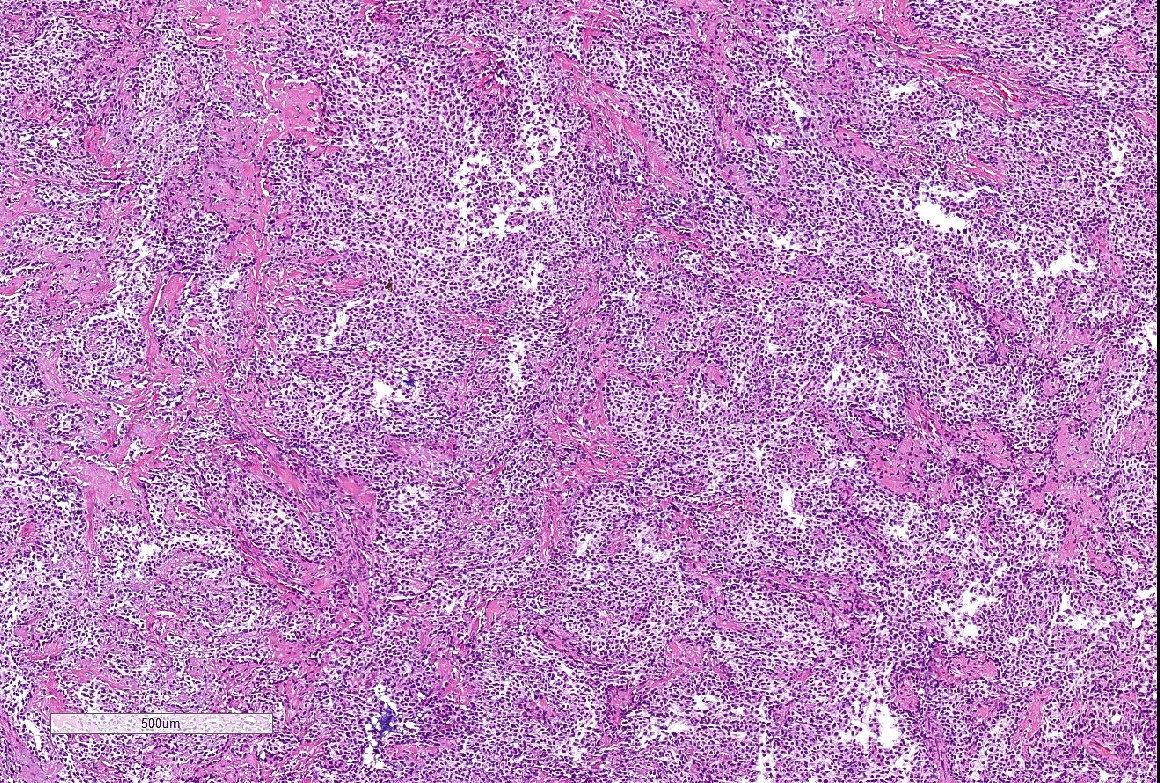
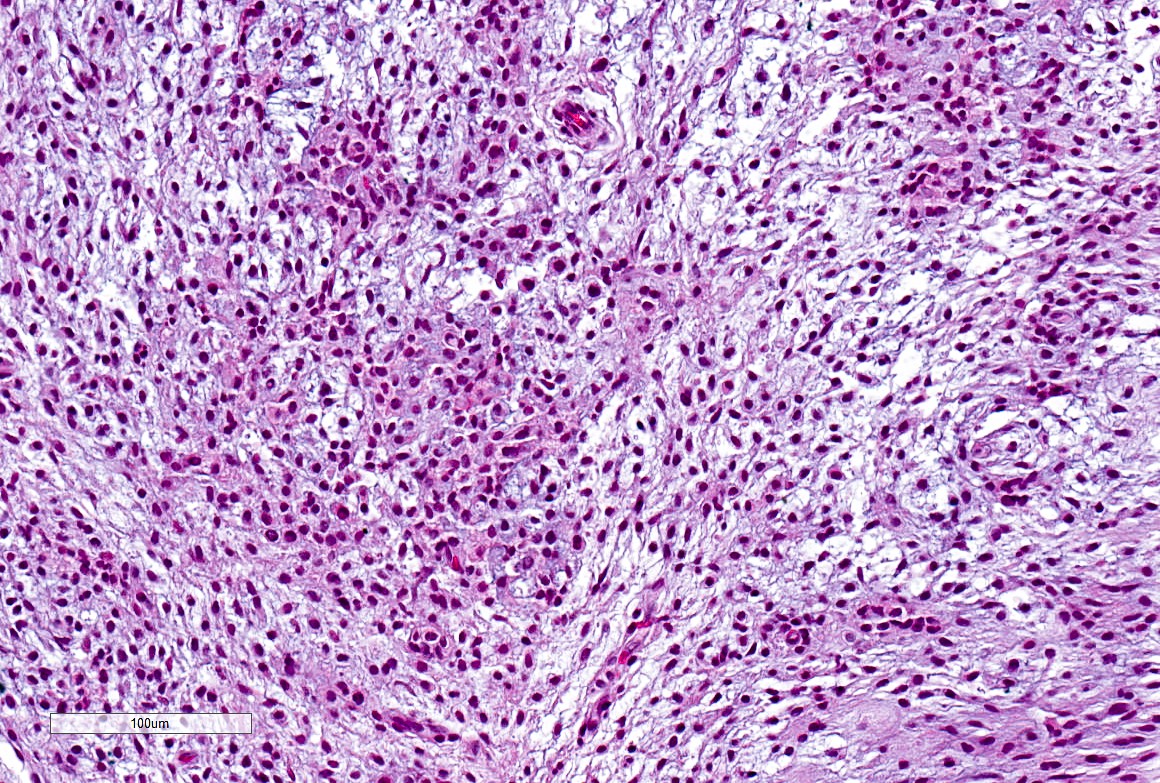
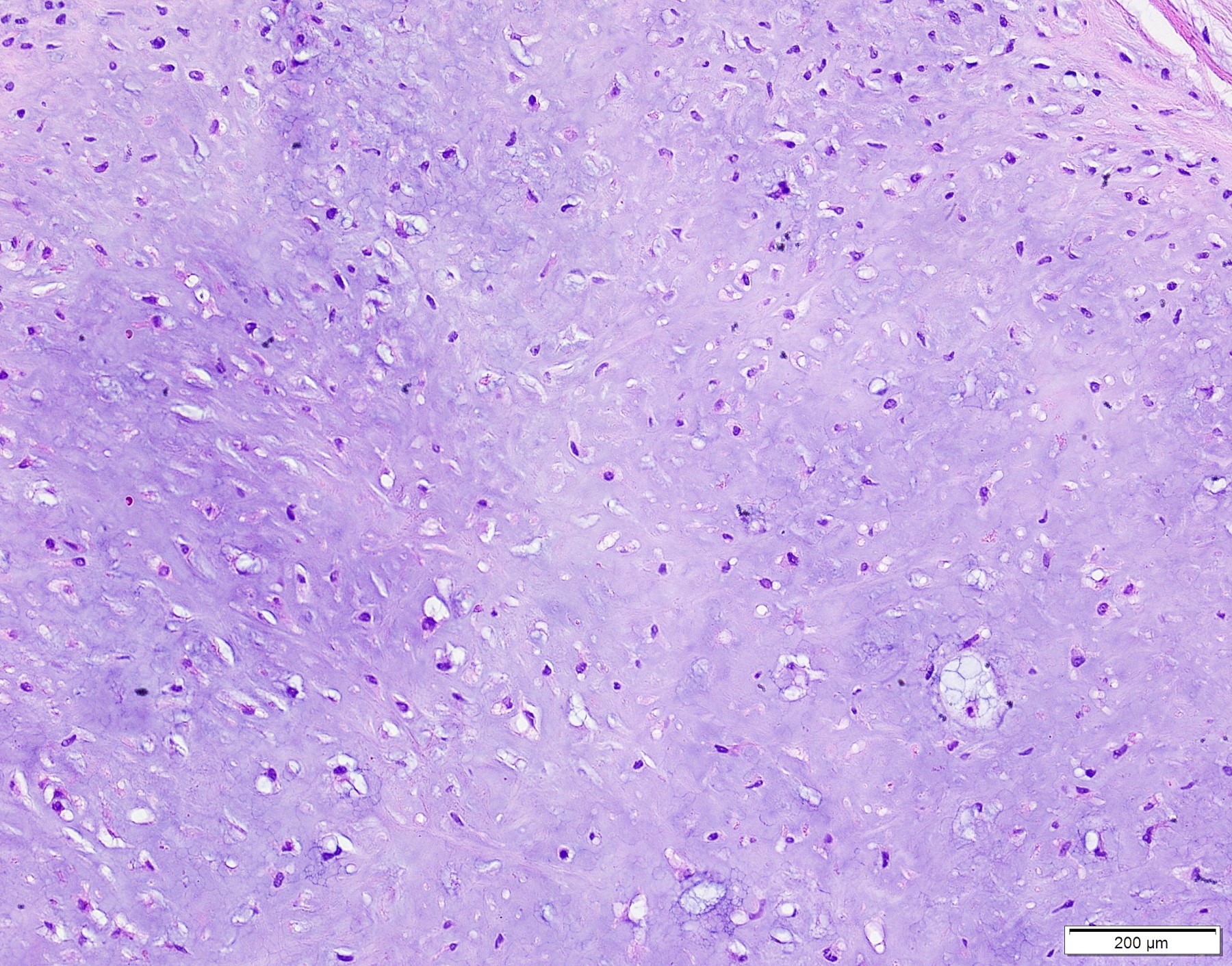
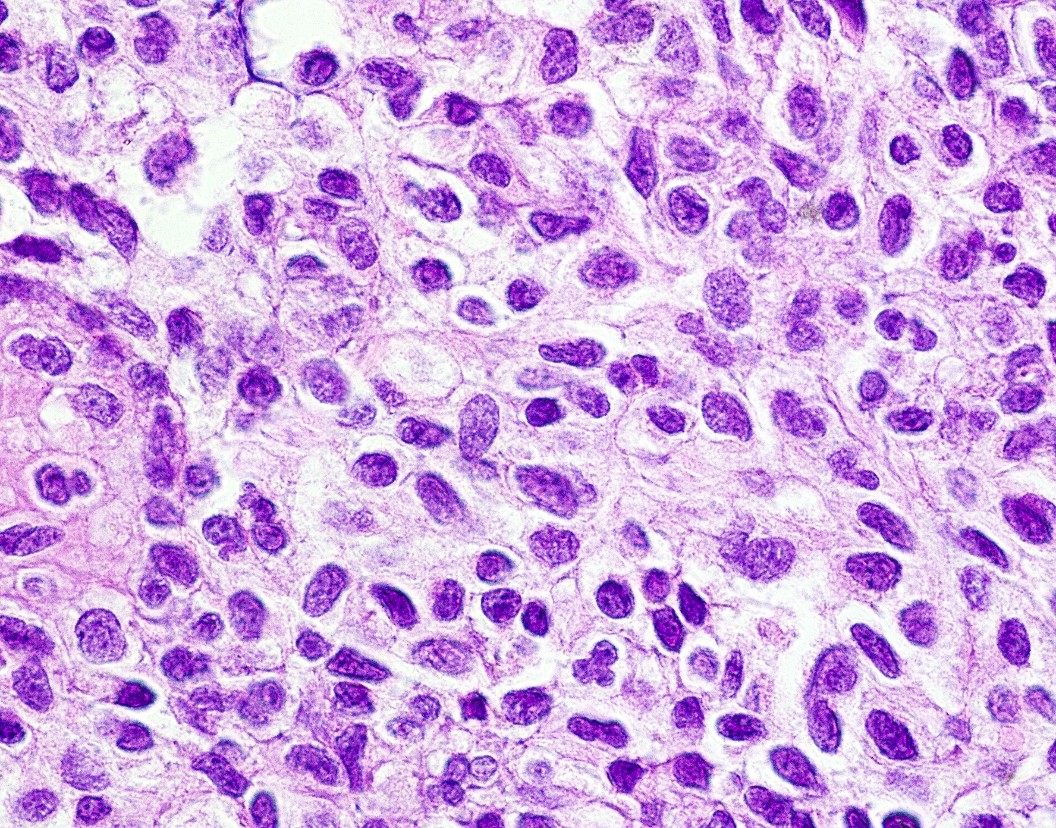
Microscopic (histologic) description
- Well demarcated tumor, often entrapped within skeletal muscle and frequently multilobulated (Am J Surg Pathol 2018;42:1297, Head Neck Pathol 2015;9:315)
- Stromal background may be hyalinized or demonstrate mucoid, myxoid or chondromyxoid areas
- Cords, strands or sheets of oval, round, fusiform or polygonal bland cells, sometimes arranged in a reticular / net-like or globoid pattern (Am J Surg Pathol 2018;42:1297)
- Myxoglobulosis-like changes have been noted (Virchows Arch 2003;442:302)
- May focally demonstrate fine calcifications, cellular atypia, necrosis, multinucleated giant cells (Am J Surg Pathol 2018;42:1297, Head Neck Pathol 2015;9:315, Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1996;82:417)
- Cystic, slit-like spaces or hemorrhagic areas often noted (Head Neck Pathol 2014;8:329)
- Mitotic figures not seen (Head Neck Pathol 2015;9:315)
Microscopic (histologic) images
Cytology description
- Overlapping features with pleomorphic adenoma (Acta Cytol 2010;54:82, Oral Oncol 2003;39:83)
- Cellular, with abundant thick to myxoid fibrillary stromal elements (Acta Cytol 2010;54:82)
- Clusters of oval, spindled or polygonal cells with uniform nuclei (Acta Cytol 2010;54:82)
- Lacking mitotic figures (Acta Cytol 2010;54:82)
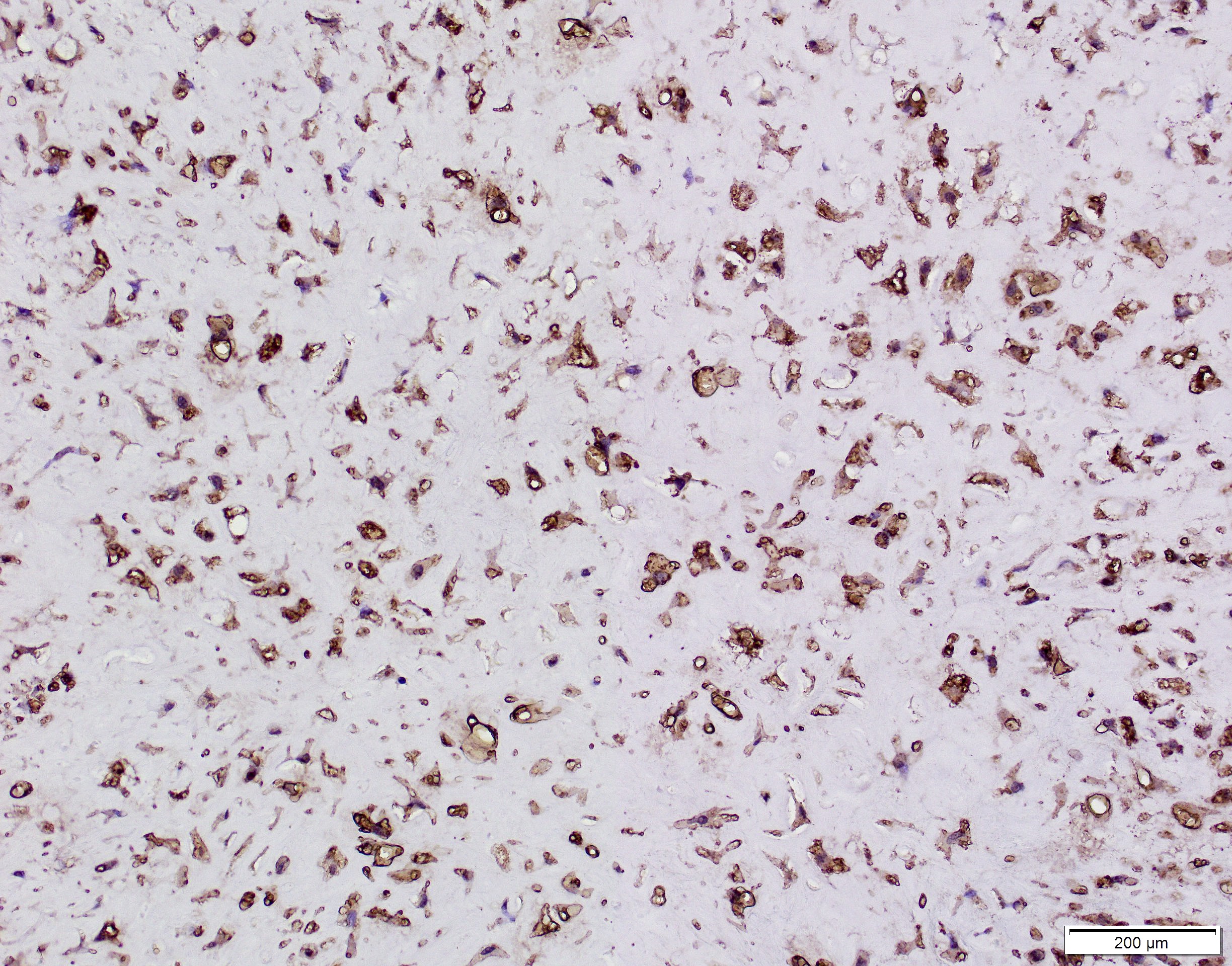
Positive stains
- Glial fibrillary acidic protein (GFAP) ~90% (Head Neck Pathol 2015;9:315)
- S100 protein > 90%
- CD56 and CD57 > 50% (Head Neck Pathol 2015;9:315)
- Authors often attribute the immunodiversity to the pluripotency of the neural crest origin
- Many other markers, such as SMA, p63, cytokeratin, desmin and SOX10, are positive in a subset (< 50%) (Head Neck Pathol 2015;9:315, Int J Surg Pathol 2016;24:586, Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2010;110:e48)
Negative stains
- EMA typically negative
Electron microscopy description
- Electron microscopy is not specific (Int J Surg Pathol 2016;24:586)
- Lobulated, concave nuclei; well developed rough endoplasmic reticulum; intermediate filament bundles (Int J Surg Pathol 2016;24:586, Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1996;82:417)
Molecular / cytogenetics description
- RREB1::MRTFB (previously MKL2) gene fusion (RNA sequencing and FISH) (Am J Surg Pathol 2018;42:1297)
- EWSR1::CREM fusion product found in 1/21 cases and 3/11 cases showed EWSR1 rearrangement on FISH (Am J Surg Pathol 2018;42:1297, Histopathology 2016;69:607)
- Unclear at this point whether EWSR1 rearranged ectomesenchymal chondromyxoid tumors represent a separate entity or part of the spectrum of ectomesenchymal chondromyxoid tumors
Molecular / cytogenetics images
Sample pathology report
- Anterior tongue, excision:
- Ectomesenchymal chondromyxoid tumor
Differential diagnosis
- Soft tissue myoepithelioma:
- Due to the overlapping morphologic, immunohistochemical and molecular findings (EWSR1 rearrangements), some authors note significant overlap or potential link between soft tissue myoepithelioma and ectomesenchymal chondromyxoid tumor (Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2005;99:581, Histopathology 2016;69:607)
- Pleomorphic adenoma / salivary myoepithelioma:
- Do not occur on the anterior dorsal tongue due to the lack of salivary glands in this area
- PLAG1 aberrations not found in ectomesenchymal chondromyxoid tumors (Histopathology 2016;69:607)
- Oral focal mucinosis:
- Stroma positive for PAS and Alcian blue (Head Neck Pathol 2015;9:315)
- Less cellular than ectomesenchymal chondromyxoid tumors
- Most commonly found on the gingiva
- Neurothekeoma:
- Positive with NKI / C3 (CD63), MITF (Head Neck Pathol 2015;9:315)
- Negative with S100, GFAP, CD57, cytokeratin (Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1996;82:417)
- Reticular perineurioma:
- EMA positive (Virchows Arch 2005;447:677)
- GLUT1 and claudin1 often positive
- Negative with S100, GFAP, CD57, cytokeratin
- Clinical differential diagnosis for a submucosal nodule on the dorsal tongue most often includes fibroma / fibrous hyperplasia, granular cell tumor or cartilaginous / osseous choristoma, all of which can easily be differentiated from an ectomesenchymal chondromyxoid tumor by biopsy
- GLI1 altered mesenchymal tumors:
- Both tumors have a propensity to oral tongue location, multilobulated to nodular growth pattern and immunopositivity of SMA, S100 and keratins
- GLI1 altered mesenchymal tumors have epithelioid morphology, arborizing capillary network and show GLI1 amplification or GLI1 translocation at molecular level (Am J Surg Pathol 2020;44:729)
Board review style question #1
Board review style answer #1
A. Ectomesenchymal chondromyxoid tumor. This tumor is well defined and comprised of ovoid cells set within a mucoid background.
B. While glomus tumors may show a similar morphology, the immunohistochemical profile is not compatible with glomus tumor.
C. While the dorsal tongue is a common location for granular cell tumor and S100 is positive, the morphology of the cells is inconsistent with granular cell tumor.
D. While the histomorphology is highly suggestive of pleomorphic adenoma, pleomorphic adenomas do not occur on the anterior dorsal tongue due to the lack of salivary glands in the area.
Comment Here
Reference: Ectomesenchymal chondromyxoid tumor
B. While glomus tumors may show a similar morphology, the immunohistochemical profile is not compatible with glomus tumor.
C. While the dorsal tongue is a common location for granular cell tumor and S100 is positive, the morphology of the cells is inconsistent with granular cell tumor.
D. While the histomorphology is highly suggestive of pleomorphic adenoma, pleomorphic adenomas do not occur on the anterior dorsal tongue due to the lack of salivary glands in the area.
Comment Here
Reference: Ectomesenchymal chondromyxoid tumor