Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Negative stains | Molecular / cytogenetics description | Molecular / cytogenetics images | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Palanthingal Bava E, Szeto W, Mannan R. Squamous cell carcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/nasalscc.html. Accessed April 2nd, 2025.
Definition / general
- Epithelial malignancy originating from sinonasal surface epithelium showing squamous cell differentiation
Essential features
- Sinonasal squamous cell carcinoma (SCC) can be keratinizing (KSCC) or nonkeratinizing (NKSCC)
- Mean: sixth and seventh decades of life
- M:F = 2:1
- Maxillary sinus > nasal cavity > paranasal sinuses
- ~50 - 60% 5 year overall survival
- NKSCC can be associated with human papillomavirus (HPV) or DEK::AFF2 fusion (mutually exclusive)
Terminology
- Keratinizing squamous cell carcinoma
- Nonkeratinizing squamous cell carcinoma
ICD coding
- KSCC
- ICD-O
- 8071/3 - squamous cell carcinoma, keratinizing, NOS
- 8086/3 - squamous cell carcinoma, HPV negative
- 8052/3 - papillary squamous cell carcinoma
- 8051/3 - verrucous carcinoma, NOS
- 8074/3 - squamous cell carcinoma, spindle cell
- 8075/3 - squamous cell carcinoma, acantholytic
- 8560/3 - adenosquamous carcinoma
- 8051/3 - verrucous carcinoma, NOS
- ICD-11
- 2C20.4 & XH4CR9 - squamous cell carcinoma of nasal cavity & squamous cell carcinoma, keratinizing, NOS
- 2C22.1 & XH4CR9 - squamous cell carcinoma of accessory sinuses & squamous cell carcinoma, keratinizing, NOS
- ICD-O
- NKSCC
- ICD-O
- ICD-11
- 2C20.4 & XH6705 - squamous cell carcinoma of nasal cavity & squamous cell carcinoma, large cell, nonkeratinizing, NOS
- 2C22.1 & XH6705 - squamous cell carcinoma of accessory sinuses & squamous cell carcinoma, large cell, nonkeratinizing, NOS
Epidemiology
- ~3% of malignancies of head and neck; < 1% of malignant neoplasms at all sites
- Most common malignant epithelial neoplasm of sinonasal tract (80%)
- More common in Japan than in the West
- M:F = 2:1
- Most patients are in sixth or seventh decade of life
- Rare in patients < 40 years old
- KSCC is the most common type (50 - 60% of all sinonasal tract squamous cell carcinomas)
- NKSCC comprises 40 - 50% of all sinonasal tract squamous cell carcinomas (Head Neck 2012;34:877, Laryngoscope 2015;125:2491)
Sites
- Maxillary sinus (60 - 70%), nasal cavity (12 - 25%), ethmoid sinus (10 - 15%), ethmoid and frontal sinuses (1%) (Head Neck 2009;31:1593)
- ~10% bilateral but may be direct side to side extension
Pathophysiology
- May develop from Schneiderian papilloma and be associated with HPV (20 - 25% of sinonasal carcinomas harbor high risk HPV; NKSCC > KSCC) (Laryngoscope 2001;111:1104, Mod Pathol 2014;27:343)
- Routine HPV testing is not currently mandated for sinonasal carcinomas (Arch Pathol Lab Med 2018;142:559)
- A proportion of virus negative NKSCC may be associated with DEK::AFF2 fusions (mutually exclusive of HPV) (Am J Surg Pathol 2021;45:718)
- Molecular alterations in keratinizing squamous cell carcinoma include
- TP53 and EGFR mutations
- Alterations in PTEN, CDKN2A and KMT2D (Future Oncol 2020;16:1235, Histopathology 2018;73:953)
Etiology
- Reported risk factors include exposure to nickel, chlorophenols, textile dust, thorotrast, chromium, isopropyl alcohol, radium and smoking (Int J Otolaryngol 2013;2013:672621, Head Neck Surg 1979;2:3)
- 36 - 58% of sinonasal NKSCCs are HPV associated (Am J Surg Pathol 2005;29:1367)
Clinical features
- Nasal fullness, epistaxis, rhinorrhea, pain, nasal / facial swelling are common presentations
- Advanced cases may present with proptosis, diplopia or lacrimation (Head Neck Pathol 2016;10:60)
Diagnosis
- KSCC
- Essential: malignant epithelial cells with squamous differentiation and keratinization
- Desirable: p40 immunostain positivity (in selected cases)
- NKSCC
- Essential: morphological or immunohistochemical evidence of squamous differentiation; minimal to no keratinization; active exclusion of mimics, such as NUT carcinoma, SMARCB1 deficient sinonasal carcinoma and adamantinoma-like Ewing sarcoma
Radiology description
- Sinonasal squamous cell carcinoma shows a soft tissue mass characterized by prominent bony destruction on computed tomography (CT) (J Clin Med 2017;6:116, Head Neck Pathol 2016;10:1)
- Magnetic resonance imaging (MRI) shows intermediate T1 signal intensity and hypointense T2 signal
- Variable enhancement on contrast enhanced T1 images is < 50% that of sinus mucosa
- Small lesions are homogenous in signal intensity
- Large tumors are more heterogeneous with areas of necrosis and hemorrhage
Radiology images
Prognostic factors
- Patients with nasal tumors usually present earlier and have a better prognosis than those with maxillary sinus tumors
- Overall, 5 year survival of nasal squamous cell carcinoma is ~60% versus 42% for maxillary sinus tumor
- Prognosis usually correlates with tumor stage and lymph node metastases
- NKSCC usually has a better prognosis than the keratinizing type
- Cohesive or pushing pattern of invasion has a better prognosis than diffuse or single cell invasive pattern (Arch Otolaryngol Head Neck Surg 2007;133:131)
Case reports
- 36 year old woman with basaloid squamous cell carcinoma of nasal cavity (Ear Nose Throat J 2015;94:E27)
- 54 year old man with sphenoid sinus spindle cell carcinoma presented with bilateral vision loss (Oncol Lett 2016;12:401)
- 58 and 60 year old men with postlaryngectomy squamous cell carcinoma (Clin Case Rep 2020;8:630)
- 60 year old man and 85 year old woman with basaloid squamous cell carcinoma of maxillary sinus (Oncol Lett 2013;5:1755)
- 65 year old man with sinonasal squamous cell carcinoma invasive to bone with intracranial extension arising within inverted papilloma (Cureus 2019;11:e4508)
- 67 year old man with verrucous squamous cell carcinoma of nasal cavity and paranasal sinus (J Korean Med Sci 1998;13:662)
Treatment
- Complete surgical resection and adjuvant radiotherapy
Gross description
- Variegated appearance: exophytic, fungating, papillary or inverted; friable, hemorrhagic or necrotic mass
Gross images
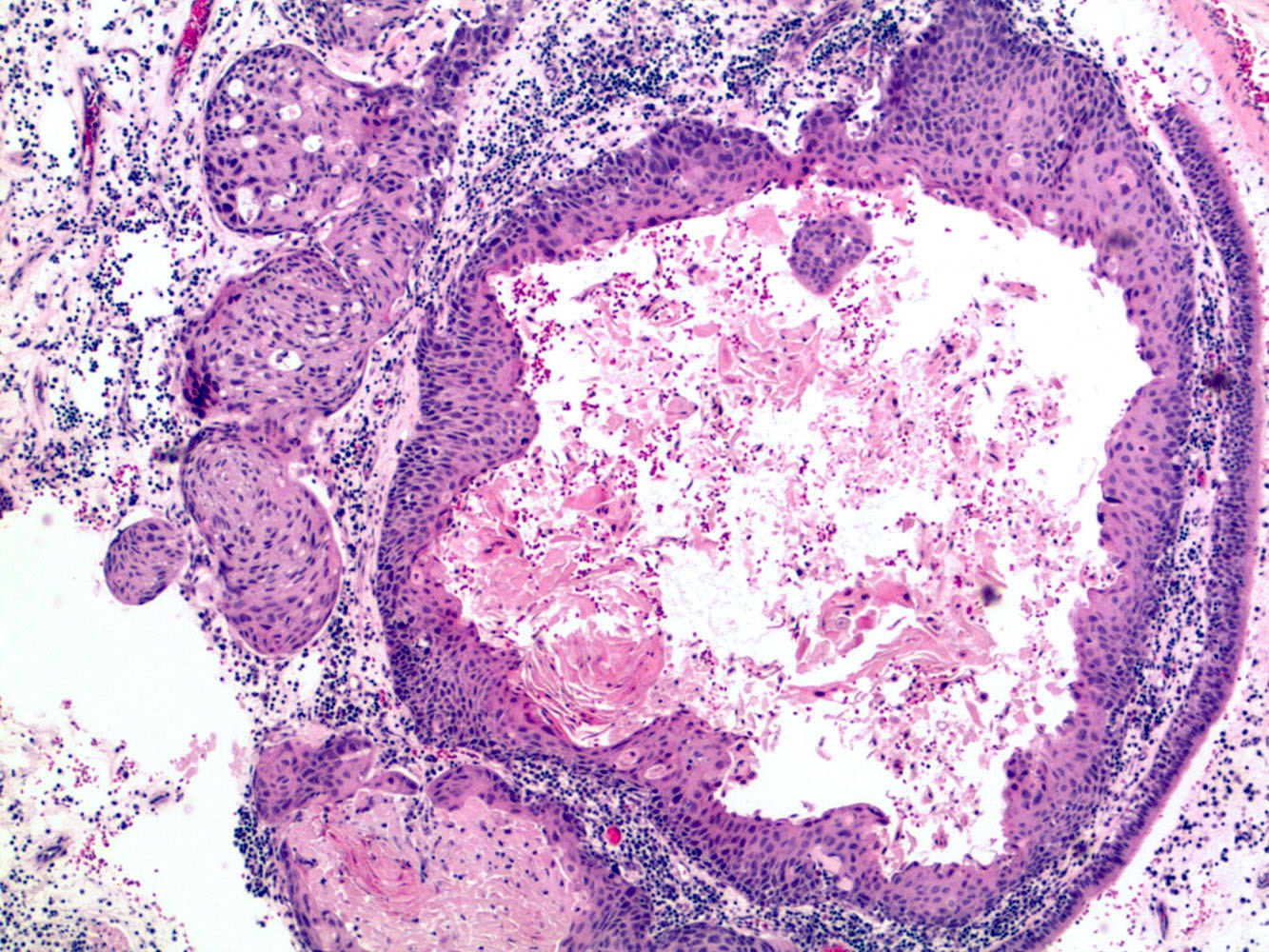
Microscopic (histologic) description
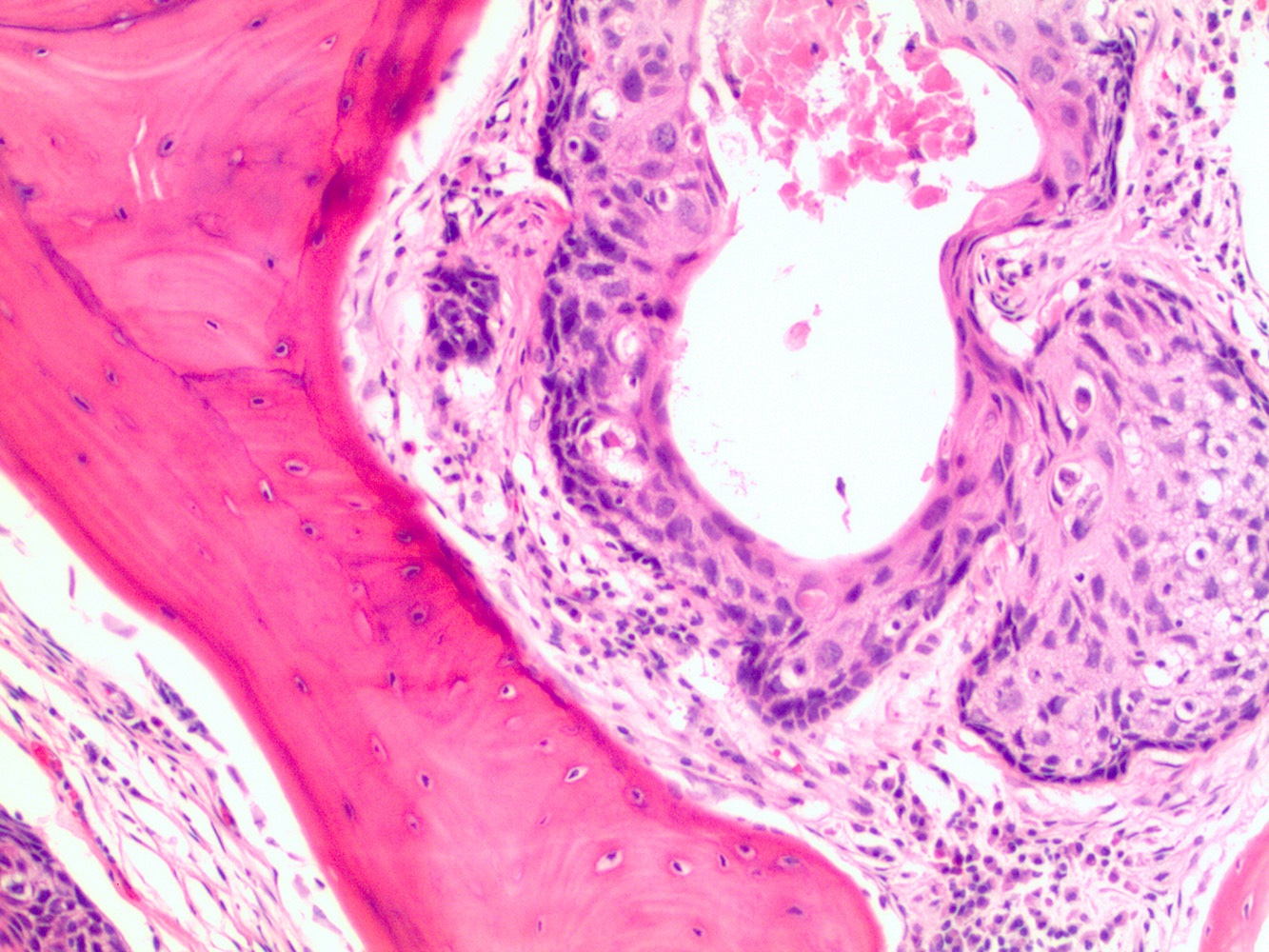
- KSCC
- Destructive stromal infiltration by cohesive nests, cords or single cells
- Stromal desmoplasia and may have associated inflammatory cell reaction
- May have dysplasia of adjacent or overlying surface epithelium
- Polygonal, enlarged cells, with intercellular bridges and pleomorphism
- Keratinization, dyskeratosis, keratin pearl formation and opacified cytoplasm
- Grading KSCC: well, moderately and poorly differentiated carcinomas
- Well to moderately differentiated carcinomas show mild to moderate nuclear atypia with enlarged, hyperchromatic nuclei and low mitotic activity
- Poorly differentiated carcinomas show greater nuclear atypia, increased mitotic activity, atypical mitoses and focal keratinization
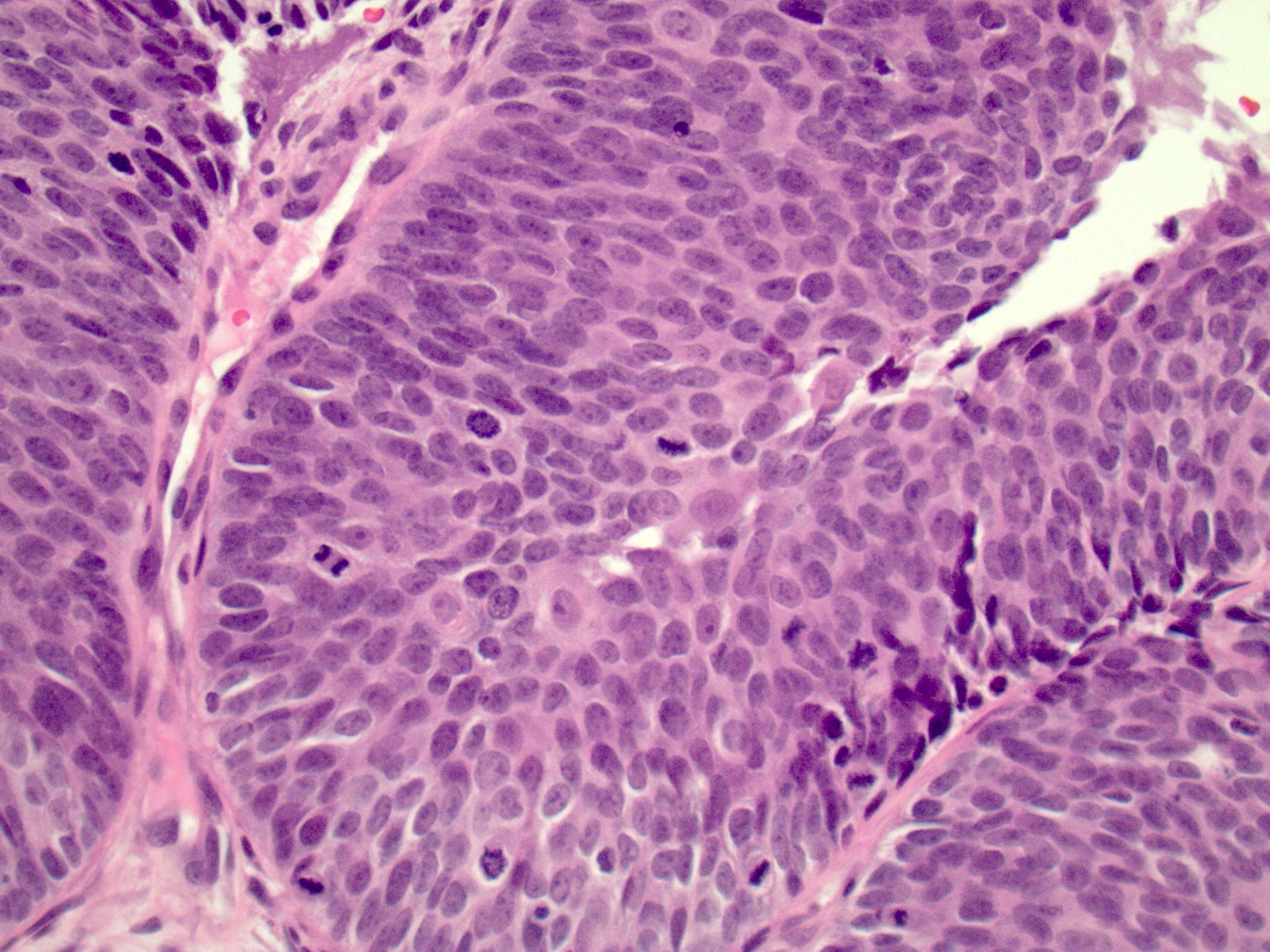
- NKSCC
- Papillary or exophytic growth pattern
- Usually hypercellular tumors showing expansile ribbons, nests and lobules of inverted or endophytic growth of neoplastic epithelium into stroma
- Tumor nests often have smooth border at advancing edge, sometimes with basement membrane-like material but with minimal desmoplasia and mild pleomorphism
- Papillary tumors resemble papillomas but can be differentiated by the complexity, significant pleomorphism, destruction of adjacent epithelium or comedo-like necrosis
- For complex, mass forming papillary tumor with malignant epithelium, invasive growth is not necessary
- Tumor cells have high N:C ratio and show loss of polarity with hyperchromatic, pleomorphic nuclei
- Syncytial appearing morphology can be seen
- Basal, peripherally palisaded, columnar layer may be seen
- Flattened superficial layer may be seen
- Mild to severe pleomorphism can be seen but NKSCC is not graded
- Keratinization is usually absent but may be focal
- Keratinization cannot be a significant component
- Increased mitoses (with atypical forms can be seen)
- Surface epithelium may show dysplasia (any grade)
- Morphologic variants
- Adenosquamous carcinoma
- Basaloid squamous cell carcinoma
- Papillary squamous cell carcinoma
- Spindle cell carcinoma or sarcomatoid carcinoma
- Verrucous carcinoma
- References: Head Neck Pathol 2016;10:60, Head Neck Pathol 2022;16:1
Microscopic (histologic) images
Positive stains
- CK5/6, CK8, CK13, CK14, CK19
- CK7 (60%), CK4 (30%)
- p40, p63 (Appl Immunohistochem Mol Morphol 2009;17:207, Head Neck Pathol 2014;8:141)
- NKSCC
- p16: HPV associated NKSCC should show block-like, diffuse (nuclear and cytoplasmic) pattern in > 70% of neoplastic cells; however, p16 immunohistochemistry alone in a nonoropharyngeal location is less specific
- Performing follow up ISH or PCR for transcriptionally active HPV is needed if HPV status needs to be determined
- p16: HPV associated NKSCC should show block-like, diffuse (nuclear and cytoplasmic) pattern in > 70% of neoplastic cells; however, p16 immunohistochemistry alone in a nonoropharyngeal location is less specific
Negative stains
Molecular / cytogenetics description
- Routine HPV testing is currently not mandated in sinonasal NKSCC but it can sometimes be helpful for diagnosis; if used, HPV specific testing such as in situ hybridization or PCR must be performed because p16 is less specific in sinonasal tumors (Head Neck Pathol 2011;5:349, Am J Surg Pathol 2013;37:185, Virchows Arch 2016;469:277, Histopathology 2020;77:989)
- RNA sequencing and DEK FISH can detect DEK::AFF2 fusions
Sample pathology report
- Mass, maxilla, left, orbital exenteration with left partial maxillectomy:
- Invasive squamous cell carcinoma, keratinizing type, involving maxillary sinus mucosa (see comment)
- Left lateral orbital rim bone margin involved by squamous cell carcinoma.
- Zygomatic arch bone involved by squamous cell carcinoma.
- Perineural invasion is present.
- Comment: Immunostaining shows positive reactivity for p40, supporting the diagnosis (see synoptic report).
Differential diagnosis
- Sinonasal papillomas (Ann Otol Rhinol Laryngol 1971;80:192):
- Lacks invasive growth
- Mild atypia but lacks interconnecting cords of tumor
- Koilocytic change, intraepithelial inflammatory infiltrate, surface mucocytes
- Necrotizing sialometaplasia (Cancer 1973;32:130):
- Reactive healing process centered on minor mucoserous glands
- Infarction or coagulative necrosis of lining of minor mucoserous glands and ducts with ingrowth of metaplastic squamous epithelium
- Maintained lobular growth confined to gland duct outlines
- Verrucous and pseudoepitheliomatous hyperplasia (Pathol Int 1998;48:389):
- Reactive epithelial overgrowth resulting in thickened epithelium
- No destructive infiltrative growth
- Atypical mitoses, comedonecrosis and profound pleomorphism are absent
- NUT carcinoma (JNCI Cancer Spectr 2019;4:pkz094):
- Monotonous carcinoma frequently showing abrupt squamous differentiation and acute inflammation
- NUT1 positive
- SWI / SNF complex deficient sinonasal carcinomas (Am J Surg Pathol 2017;41:458):
- Primarily basaloid cells with scattered rhabdoid cells
- Loss of INI1
- Spindled cell neoplasms (Am J Surg Pathol 2012;36:517):
- For spindled cell squamous cell carcinoma, differential includes leiomyosarcoma, mucosal melanoma, malignant peripheral nerve sheath tumor, biphenotypic sinonasal sarcoma, rhabdomyosarcoma, synovial sarcoma, fibrosarcoma, undifferentiated pleomorphic sarcoma, meningioma, leiomyoma, solitary fibrous tumor, glomangiopericytoma, inflammatory myofibroblastic tumor and fibromatosis (desmoid type)
- Nasopharyngeal carcinoma (Cancer 1979;44:1029):
- Nasopharyngeal carcinoma may be differentiated from sinonasal squamous cell carcinoma by its nasopharyngeal location
- A proportion of nasopharyngeal carcinoma may harbor Epstein-Barr virus (EBV)
Additional references
Board review style question #1
Which of the following is a feature of the sinonasal mass with histology shown in the figure above?
- Cohesive or pushing pattern of invasion has worse prognosis than diffuse or single cell invasive pattern
- Not associated with smoking
- Only of keratinizing type
- Routine human papillomavirus (HPV) testing is not indicated
Board review style answer #1
D. Routine human papillomavirus (HPV) testing is not indicated. Sinonasal squamous cell carcinoma may be associated with high risk HPV. Routine HPV testing is not currently indicated for sinonasal carcinomas, although it can aid in diagnosis. 20 - 25% of sinonasal carcinomas harbor high risk HPV; nonkeratinizing squamous cell carcinoma (NKSCC) more than keratinizing squamous cell carcinoma (KSCC).
Answer C is incorrect because it can be of keratinizing and nonkeratinizing types.
Answer B is incorrect because it has a moderate association with smoking.
Answer A is incorrect because a cohesive or pushing pattern of invasion has a better prognosis than a diffuse or single cell invasive pattern.
Comment Here
Reference: Squamous cell carcinoma
Comment Here
Reference: Squamous cell carcinoma
Board review style question #2
Biopsy from a mass in the maxillary sinus shows histologic features of squamous cell carcinoma with a complex exophytic and endophytic growth pattern with broad papillary fronds. There is minimal keratinization. Which of the following gene rearrangements may be observed in this type of tumor?
- CRTC1::MAML2 fusion
- DEK::AFF2 fusion
- MYB::NFIB fusion
- PPP2R2A::PRKD1 fusion
Board review style answer #2
B. DEK::AFF2 fusion. DEK::AFF2 is a novel fusion identified in a type of nonkeratinizing squamous cell carcinoma (NKSCC) of the sinonasal tract called DEK::AFF2 fusion associated papillary squamous cell carcinoma. This entity exhibits complex exophytic and endophytic growth with broad papillary fronds, anastomosing lobules, ribbons and nests and is detectable with DEK::AFF2 FISH break apart probe or RNA sequencing. Answer C is incorrect because MYB::NFIB fusion is seen in adenoid cystic carcinoma. Answer A is incorrect because CRTC1::MAML2 fusion is seen in mucoepidermoid carcinoma. Answer D is incorrect because PPP2R2A::PRKD1 fusion is seen in cribriform adenocarcinoma.
Comment Here
Reference: Squamous cell carcinoma
Comment Here
Reference: Squamous cell carcinoma