Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Frozen section description | Frozen section images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Dermawan JK, Rabinowitz LO. Biphenotypic sinonasal sarcoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/nasalbiphenotypicsarcoma.html. Accessed April 2nd, 2025.
Definition / general
- Low grade sarcoma of the sinonasal tract which features both neural (S100) and myogenic (actin) differentiation and the majority have been associated with PAX3 translocations
Essential features
- Infiltrative, cellular, monomorphic spindled cell neoplasm with herringbone or fascicular architecture
- May have prominent stromal vasculature
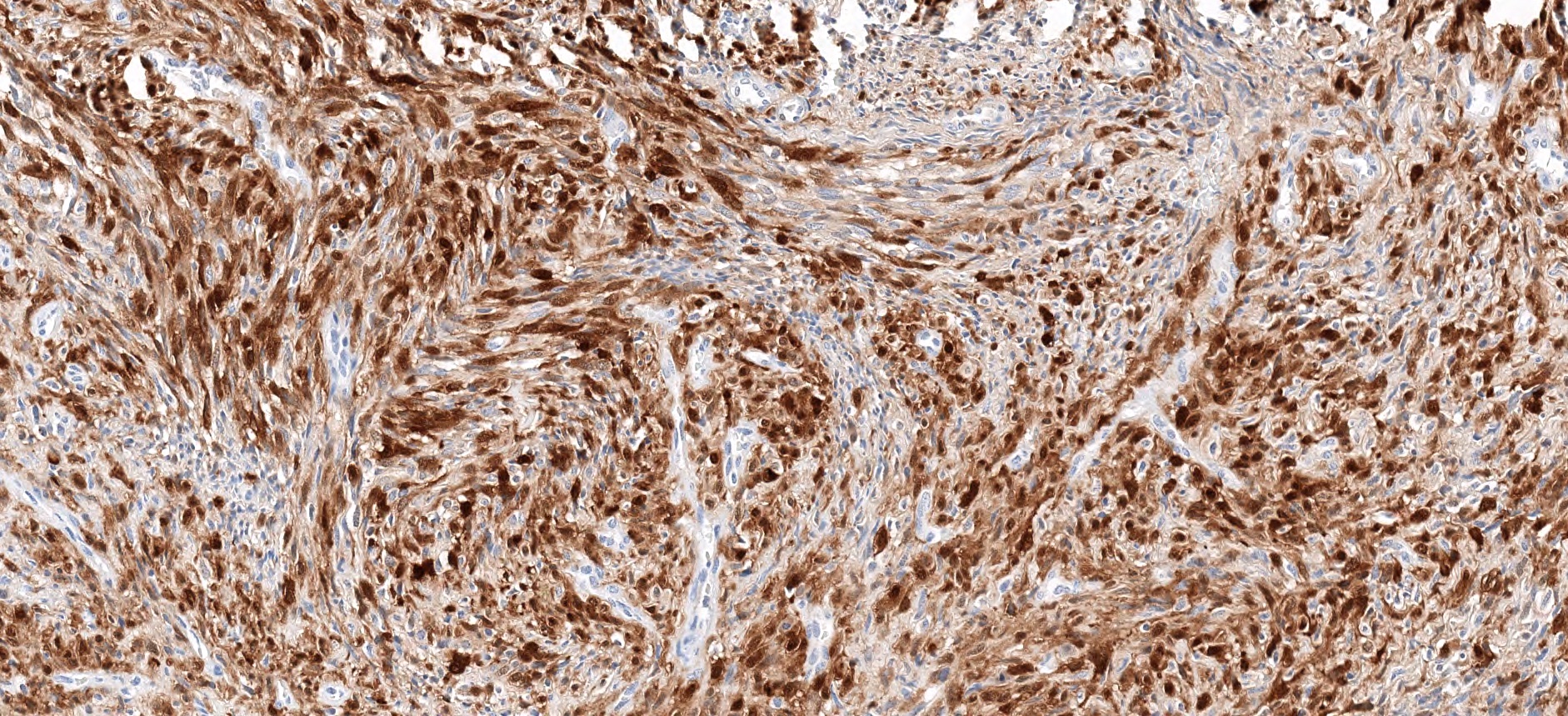
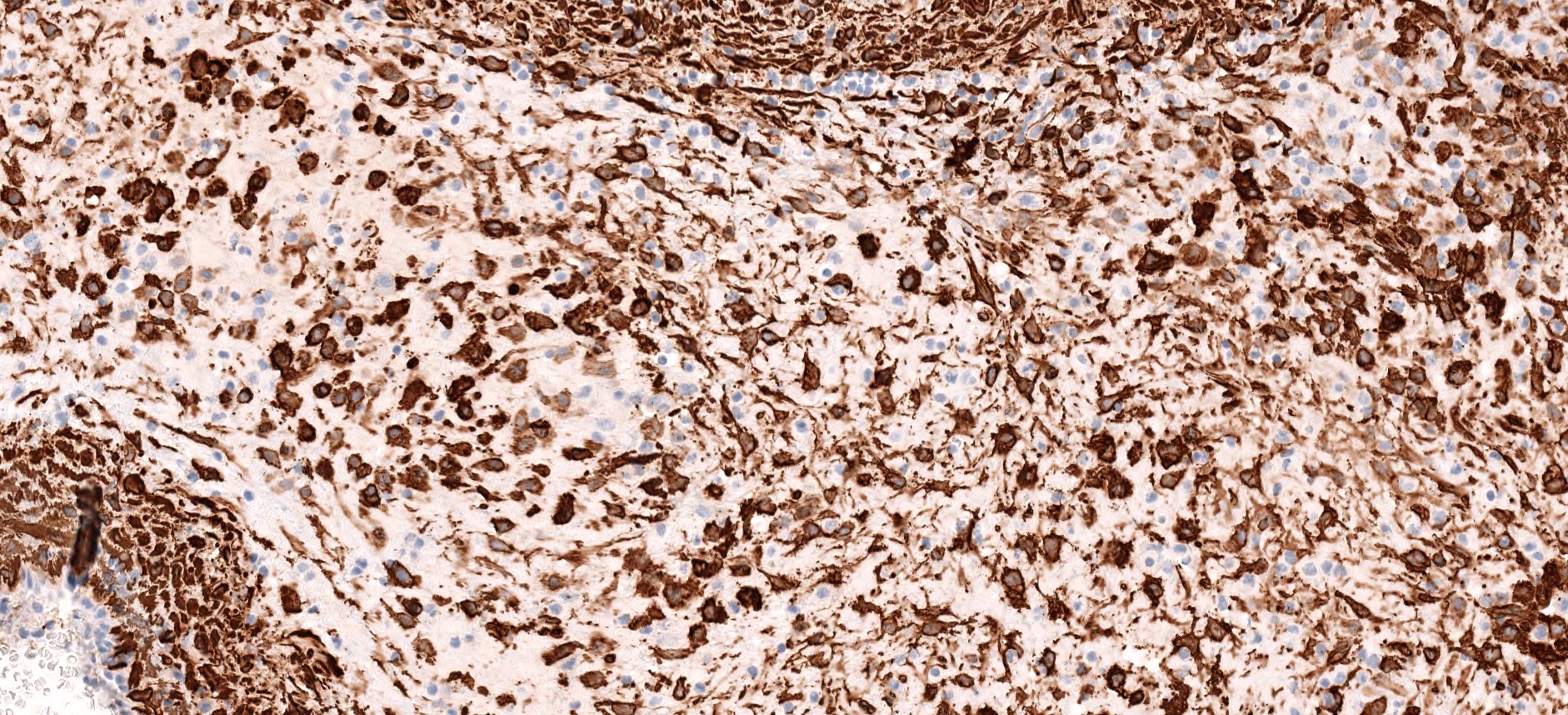
- Positive for S100 (focal to diffuse), SMA/MSA, nuclear beta catenin immunohistochemical stains
- Often recurrent PAX3 translocations most commonly partnered with MAML3
Terminology
- Low grade sinonasal sarcoma with neural and myogenic features (Am J Surg Pathol 2012;36:517)
ICD coding
- ICD-10: C30.0 - Malignant neoplasm of nasal cavity and middle ear
Epidemiology
- M:F = 1:3
- Commonly presents in the fifth decade (range: 24 - 85 years) (Virchows Arch 2018;473:615)
- Rare (likely underreported)
Sites
- Sinonasal tract, with the upper nasal cavity or ethmoid sinus being the most commonly involved
- May extend to cribriform plate or orbit
Etiology
- Unknown
Clinical features
- Nonspecific, usually nasal obstructive symptoms manifesting as difficulty breathing, facial pressure, nasal congestion with or without pain
Diagnosis
- CT or MRI of the nasal sinuses
- Diagnosis is by endoscopic biopsy, debulking or surgical resection
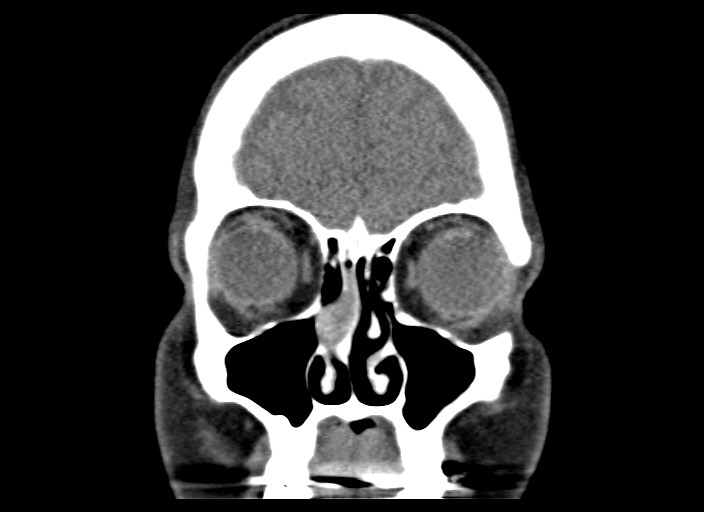
Radiology description
- Heterogenous, enhancing sinonasal tract polyp or mass
- Could present as destructive mass with extension into orbit or anterior skull base (J Neurol Surg Rep 2017;78:e15)
Radiology images
Prognostic factors
- Locally aggressive:
- Local recurrence rate 32 - 44%, majority within 5 years (Am J Surg Pathol 2019;43:747)
- Rare cases of distant metastasis death from disease (~ 2%) (Virchows Arch 2018;473:615)
Case reports
- 35 year old woman with history of right nasal obstruction (Ann Med Surg (Lond) 2018;37:4)
- 39 year old woman with frontal sinus mass who died 8 months after recurrence (Hum Pathol 2016;55:44)
- 47 year old woman with 4.8 cm ethmoid mass (Virchows Arch 2018;473:615)
- 65 year old man presents with epistaxis (Ann Diagn Pathol 2018;33:6)
- 67 year old woman with recurrent nasal polyps (Int J Clin Exp Pathol 2017;10:11743)
Treatment
- Complete surgical resection with or without radiation
Gross description
- Polypoid fragments of tan-yellow to soft gray tissue
Frozen section description
- Diagnostic stromal features could be subtle on frozen sections
- In the presence of benign epithelial proliferation, could be mistaken for an epithelial tumor such as sinonasal papilloma or respiratory epithelial adenomatoid hamartoma on frozen section (Head Neck Pathol 2020;14:33)
Frozen section images
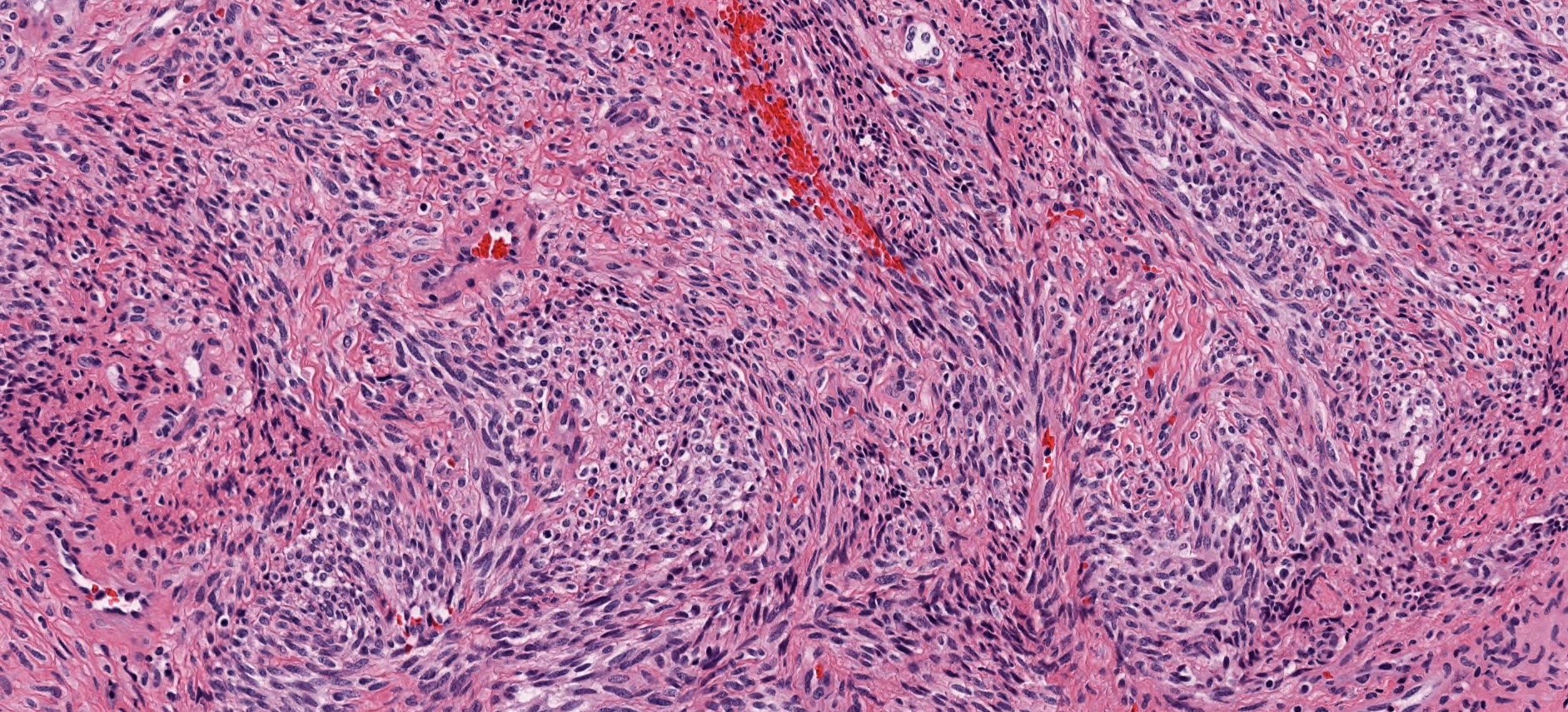
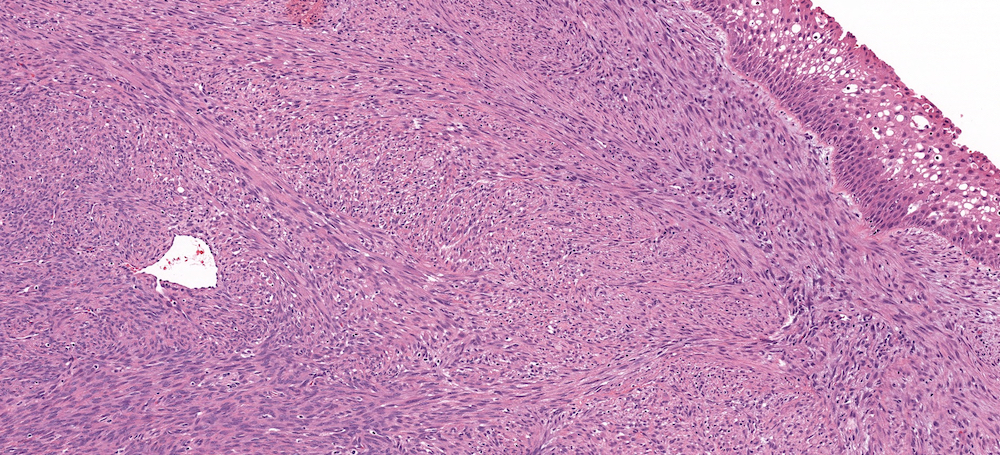
Microscopic (histologic) description
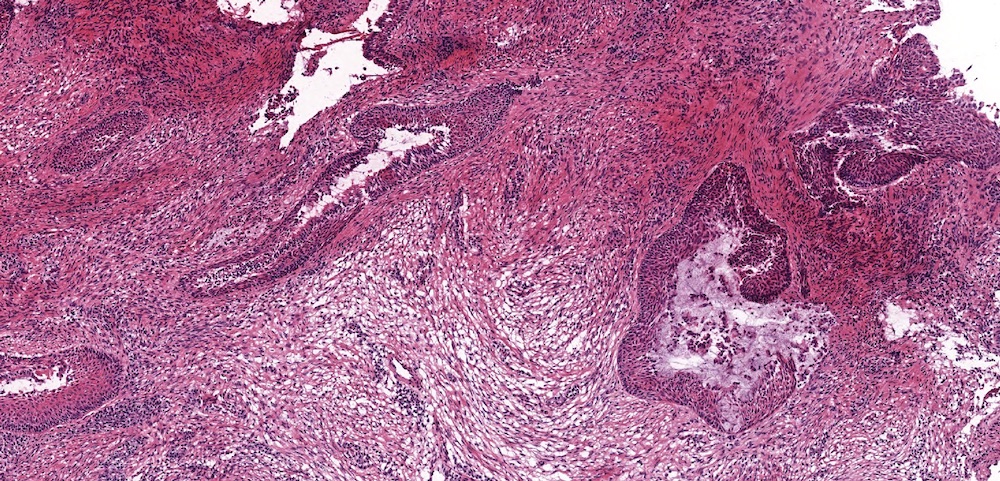
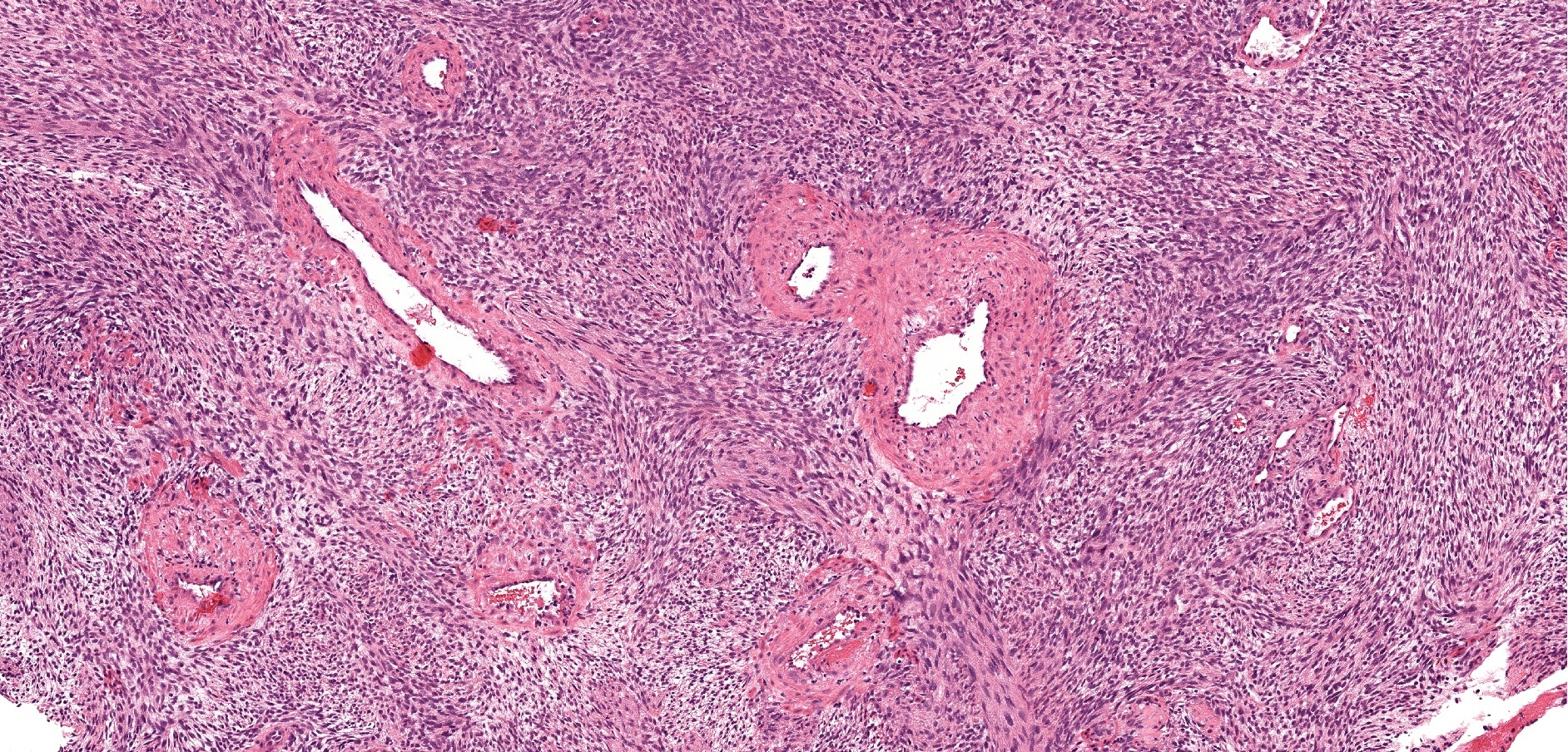
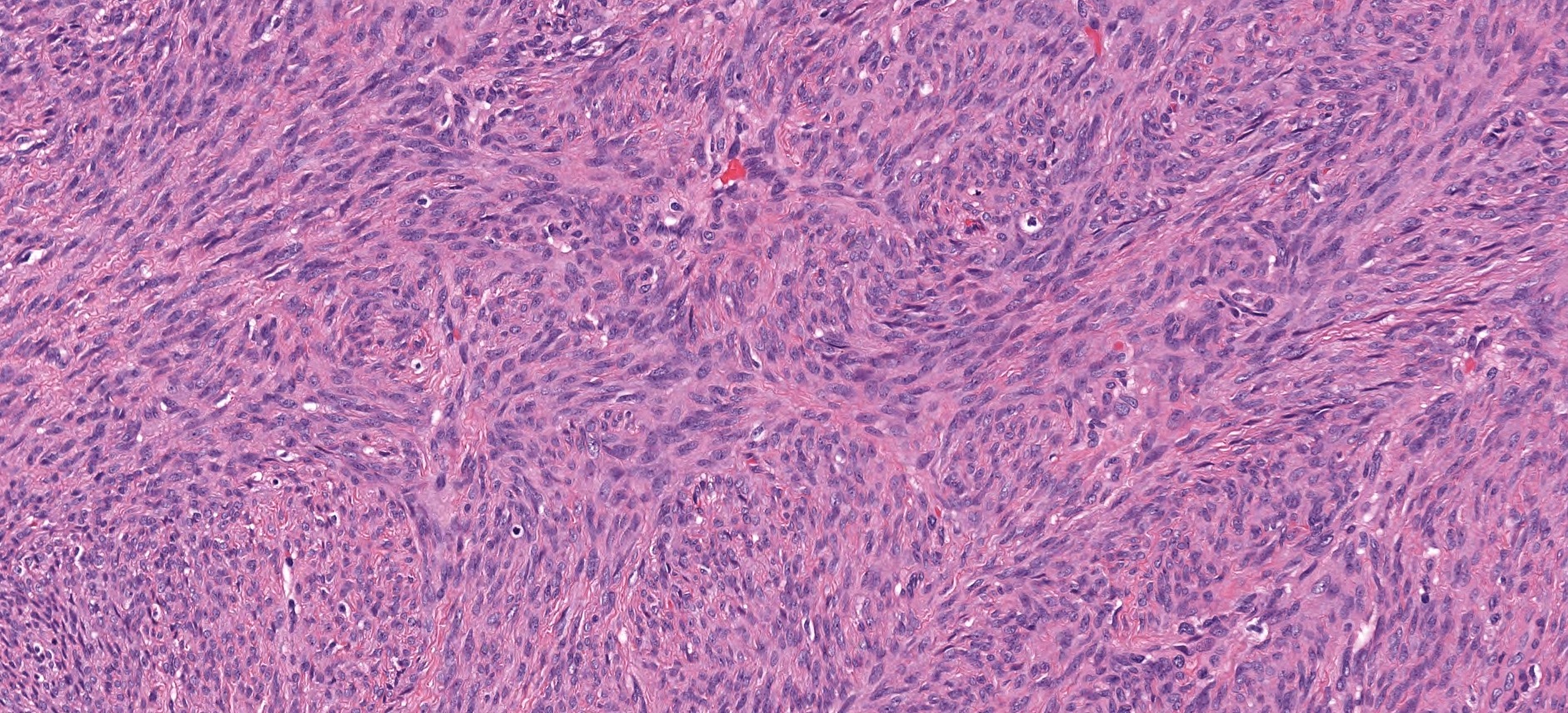
- Infiltrative, cellular spindled cell proliferation
- Medium to long fascicles with areas of herringbone pattern
- Low grade, monotonous spindled cells with ovoid to elongated nuclei and inconspicuous nucleoli
- Usually absence of high grade features such as nuclear pleomorphism, frequent mitoses, significant atypia, necrosis
- Invagination or entrapment of benign surface respiratory epithelial proliferation with or without squamous metaplasia
- Prominent stromal thick walled vasculature, could be hemangiopericytoma-like
- Delicate stromal collagen
- Subset of cases show focal rhabdomyoblastic elements (variable desmin, myogenin, myoD1) (Head Neck Pathol 2020;14:33)
Microscopic (histologic) images
Cytology description
- Bland, uniform population of spindle cells with mildly enlarged, oval to spindle shaped nuclei with fine nuclear chromatin and inconspicuous nucleoli
- Significant nuclear atypia or pleomorphism is typically absent (Diagn Cytopathol 2019;47:507)
Positive stains
- S100 (may be focal), smooth muscle actin (may be diffuse or focal) or calponin, muscle specific actin (patchy to diffuse), nuclear beta catenin (may be focal), desmin (variable), myogenin (variable) (Ann Diagn Pathol 2018;33:6, Hum Pathol 2016;55:44)
- PAX3 (Am J Surg Pathol 2018;42:1275)
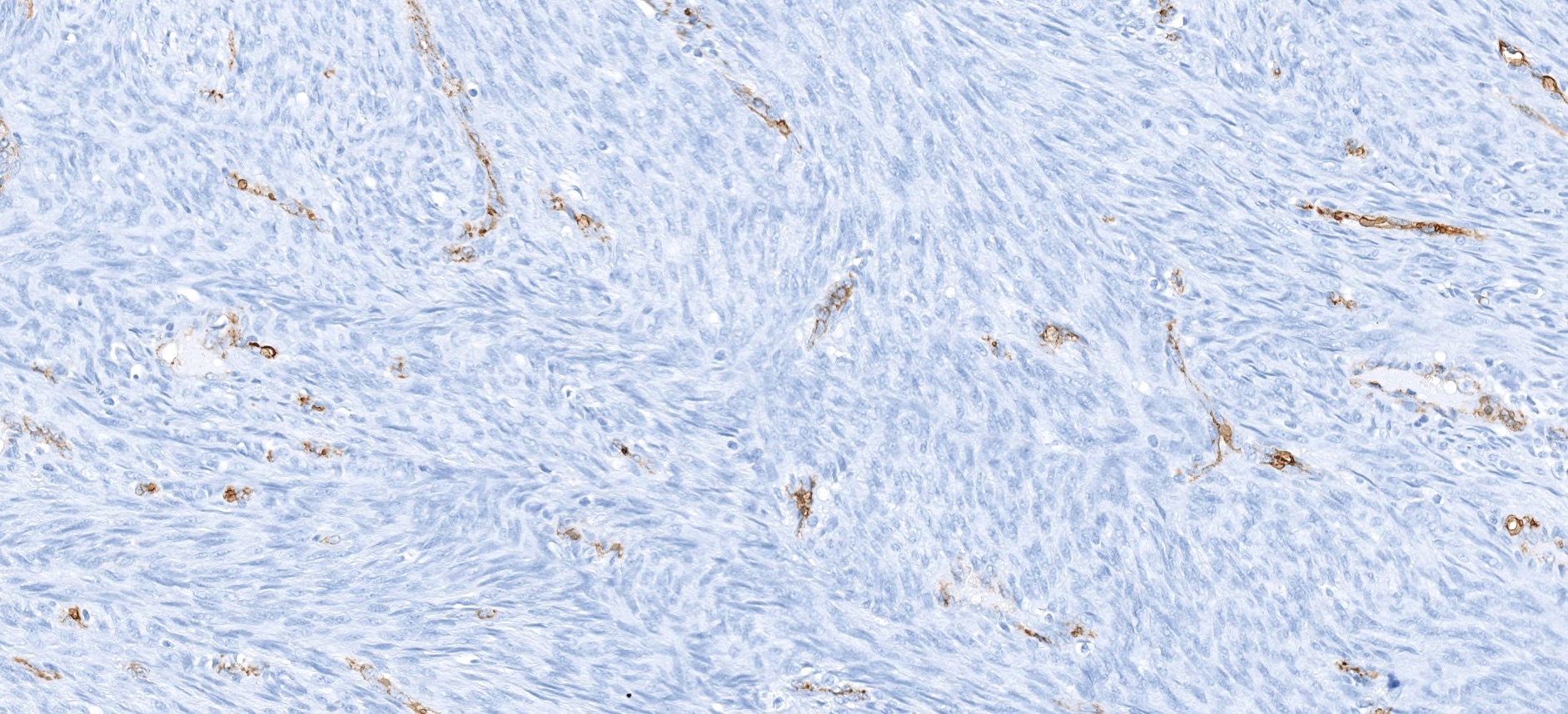
Negative stains
Molecular / cytogenetics description
- Recurrent PAX3 translocations (Am J Surg Pathol 2018;42:1275)
- PAX3 break apart signals on fluorescence in situ hybridization (Histopathology 2016;69:930)
- Most common rearrangement: t(2;4)(q35;q31) resulting in PAX3-MAML3 fusion detected by RNA-seq or RT-PCR (Nat Genet 2014;46:666)
- Other fusions reported: PAX3-NCOA1 (associated with rhabdomyoblastic differentiation), PAX3-FOXO1, PAX3-WWTR1, PAX3-NCOA2 (Am J Surg Pathol 2016;40:51, Genes Chromosomes Cancer 2016;55:25, Am J Surg Pathol 2019;43:747)
Sample pathology report
- Soft tissue mass, right nasal cavity, excision:
- Biphenotypic sinonasal sarcoma (see comment and synoptic report)
- Comment: The nasal cavity mass shows a cellular spindled proliferation with areas showing a herringbone pattern. The spindle cells are low grade with slender to ovoid nuclei and inconspicuous nucleoli. There are invaginations of benign epithelium with squamous metaplasia. The neoplastic spindle cells show patchy S100, SMA and nuclear beta catenin immunohistochemical staining. They are negative for CD34, STAT6, SOX10 and cytokeratin AE1/AE3. These findings support the diagnosis of biphenotypic sinonasal sarcoma, a low-grade spindle cell sarcoma commonly associated with a PAX3-MAML3 gene fusion. This tumor type usually shows slow progressive growth and local invasion. While local recurrence is frequent, distant metastasis is very rare.
Differential diagnosis
- Sinonasal glomangiopericytoma:
- Round to ovoid instead of elongated nuclei
- Diffuse smooth muscle actin and beta catenin nuclear staining positivity
- Absence of herringbone pattern
- Absence of S100 positivity
- Solitary fibrous tumor:
- Schwannoma:
- Malignant peripheral nerve sheath tumor:
- Leiomyoma or leiomyosarcomas:
- Variably cellular proliferation of cells with blunt ended, cigar shaped nuclei
- Positive for smooth muscle actin and desmin
- Absence of S100 positivity
- Spindle cell rhabdomyosarcoma:
- Synovial sarcoma:
- Variable positivity for cytokeratins and TLE1
- Negative for smooth muscle actin and muscle specific actin
- Characterized by t(X;18) SS18-SSX1/2 fusions
- Sinonasal papilloma, inverted type:
- Endophytic growth of markedly thickened squamous epithelial proliferation
- Absence of spindle cell proliferation
- Respiratory epithelial adenomatoid hamartoma (REAH)
- Noninvasive epithelial proliferation with surface invaginations with thickened basement membrane and ciliated respiratory epithelium
- Absence of spindle cell proliferation
Additional references
Board review style question #1
- A 45 year old woman presents with a 3 month history of nasal obstructive symptoms. An MRI of the nasal sinus shows a 3.8 cm polypoid mass in the ethmoid sinus with focal soft tissue extension without bony destruction of the cribriform plate. Histology reveals a low grade, monotonous spindle cell neoplasm. There is patchy immunoreactivity of S100 and SMA and negative staining for CD34, STAT6 and SOX10. Gene rearrangement involving which of the following genes is most commonly associated with this tumor?
- ETV6
- EWSR1
- NUTM1
- NTRK
- PAX3
Board review style answer #1
E. PAX3. Biphenotypic sinonasal sarcoma (shown here) is classically positive for S100 and actin, and is most frequently associated with PAX3 gene rearrangements, most commonly PAX3-MAML3. PAX3-NCOA1 and PAX3-FOXO1 translocations have also been reported.
Comment Here
Reference: Biphenotypic sinonasal sarcoma
Comment Here
Reference: Biphenotypic sinonasal sarcoma
Board review style question #2
- Which of the following features would favor a diagnosis of biphenotypic sinonasal sarcoma?
- Distant metastasis and death within several months of initial diagnosis
- Frequent mitoses and presence of necrosis
- Positive immunohistochemical reactivity for CD34
- Presentation in an adolescent or young male
- Uniform spindle cell proliferation with prominent stromal vasculature
Board review style answer #2
E. Uniform spindle cell proliferation with prominent stromal vasculature. Biphenotypic sinonasal sarcoma typically presents in middle aged women. Histologically, this entity is characterized by a cellular, monotonous spindle cell proliferation with low grade cytology that is positive for S100 and actin but negative for CD34 and STAT6. Prominent stromal vasculature could be present, sometimes reminiscent of hemangiopericytoma. Local recurrence is common but distant metastasis and death from disease remains rare.
Comment Here
Reference: Biphenotypic sinonasal sarcoma
Comment Here
Reference: Biphenotypic sinonasal sarcoma