Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Xu B. Allergic fungal rhinosinusitis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/nasalallergicfungal.html. Accessed April 3rd, 2025.
Definition / general
- IgE mediated allergic / hypersensitivity mucosal inflammation to noninvasive environmental fungi in immune competent patients with atopy
- Characteristic pathologic findings are allergic mucin and the presence of fungi without tissue invasion
Essential features
- 1 of the 3 forms of noninvasive fungal infection of the sinonasal tract; the other 2 being saprophytic fungal infestation (localized colonization) and fungal ball (Laryngoscope 2009;119:1809)
- Characterized by thick allergic mucin (with degranulated eosinophils and Charcot-Leyden crystals) and hyphal fragments on GMS stain
- Absence of tissue invasion by fungi
Terminology
- Allergic fungal sinusitis
- Eosinophil related fungal rhinosinusitis
- Eosinophilic mucin rhinosinusitis
- Allergic aspergillosis
Epidemiology
- 6 - 9% of all cases of chronic rhinosinusitis (Clin Rev Allergy Immunol 2006;30:205)
- Some may have a concomitant allergic bronchopulmonary mycosis
- Typically affects young adults with recurrent sinonasal polyps, a history of asthma and a poor response to standard medical treatments, often requiring surgical intervention
Sites
- Nasal cavity or paranasal sinuses, unilateral or bilateral
Pathophysiology
- Antigens released by fungi trapped in the sinus mucin stimulate production of IgE
- Helper T cells (Th2) mediate an eosinophil rich inflammation (Clin Rev Allergy Immunol 2006;30:205)
- Association with MHC class II HLA-DQB1*0301 and DQB1*0302
Etiology
- The most common causal fungi are dematiaceous fungi (including Bipolaris spicifera, Curvularia lunata, Exserohilum rostratum and Alternaria alternata) and Aspergillus species such as A. fumigatus, A. flavus or A. niger (Clin Rev Allergy Immunol 2006;30:205, Med Mycol 2009;47:S324)
- All patients are atopic with type I mediated hypersensitivity
Clinical features
- Nasal obstruction and discharge are the most common symptom (Indian J Otolaryngol Head Neck Surg 2022;74:4640)
Diagnosis
- Proposed diagnostic criteria include (Otolaryngol Head Neck Surg 1994;111:580, Laryngoscope 2009;119:1809)
- Type I hypersensitivity
- Nasal polyposis
- Characteristic computed tomography (CT) and magnetic resonance imaging (MRI) findings
- Fungi identified by stains or culture
- Pathologic findings of eosinophilic (allergic) mucin with fungal elements and no evidence of tissue invasion
Laboratory
- Peripheral eosinophilia
- Elevated serum IgE and fungal specific IgM
- Fungi identified in nasal lavage by stain or by culture
- References: Clin Rev Allergy Immunol 2006;30:205, Med Mycol 2009;47:S324
Radiology description
- CT: opacification of the nasal cavity and one or more paranasal sinuses, with areas of hyperattenuation (increased contrast) as a result of fungal containing allergic mucin (Clin Rev Allergy Immunol 2006;30:205)
- Erosion of bone (skull base and orbit) is seen in 20 - 60% of cases
Prognostic factors
- Failure to surgically remove all sinus disease adequately leads to relapse (Clin Rev Allergy Immunol 2006;30:205)
- Postoperative oral steroid may further reduce recurrence
Case reports
- 20 year old man with allergic fungal rhinosinusitis invading skull base (J Neurosurg Case Lessons 2021;1:CASE2161)
- 34 and 40 year old women with allergic fungal rhinosinusitis (Case Rep Otolaryngol 2019;2019:9598283)
- 42 year old man with allergic fungal rhinosinusitis (Head Neck Pathol 2015;9:488)
Treatment
- Complete endoscopic removal of all inspissated fungal containing allergic mucin and all diseased mucosa is required (Clin Rev Allergy Immunol 2006;30:205)
- Postoperative medical management includes follow up for recurrence, in office debridement and oral or topical corticosteroid
- Systemic antifungal treatment is not effective
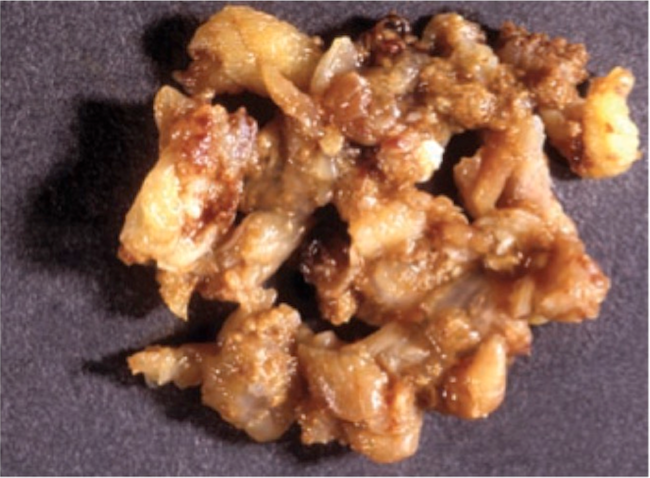
Gross description
- Thick, tenacious mucus similar to peanut butter or wet clay (Head Neck Pathol 2016;10:40)
Gross images
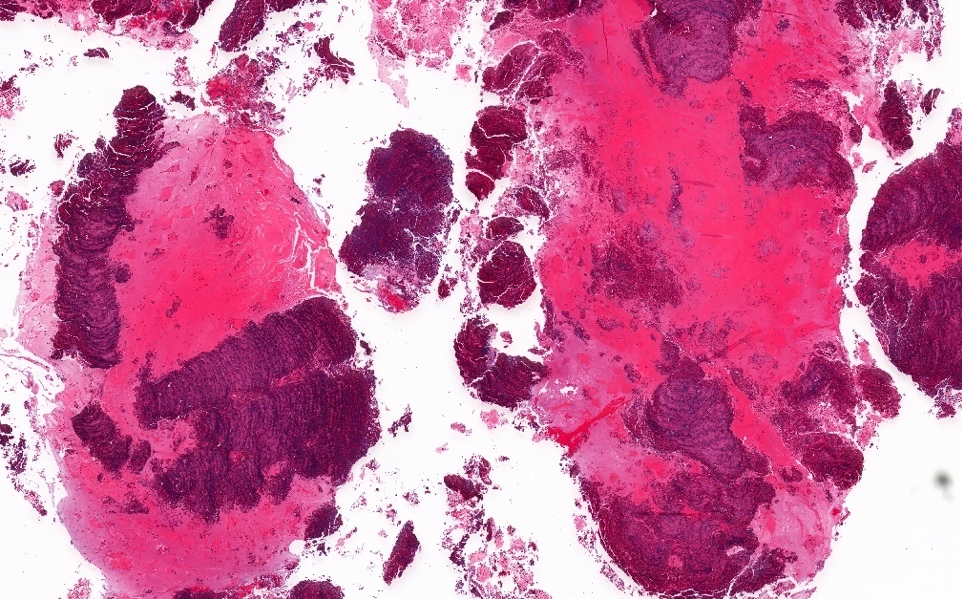
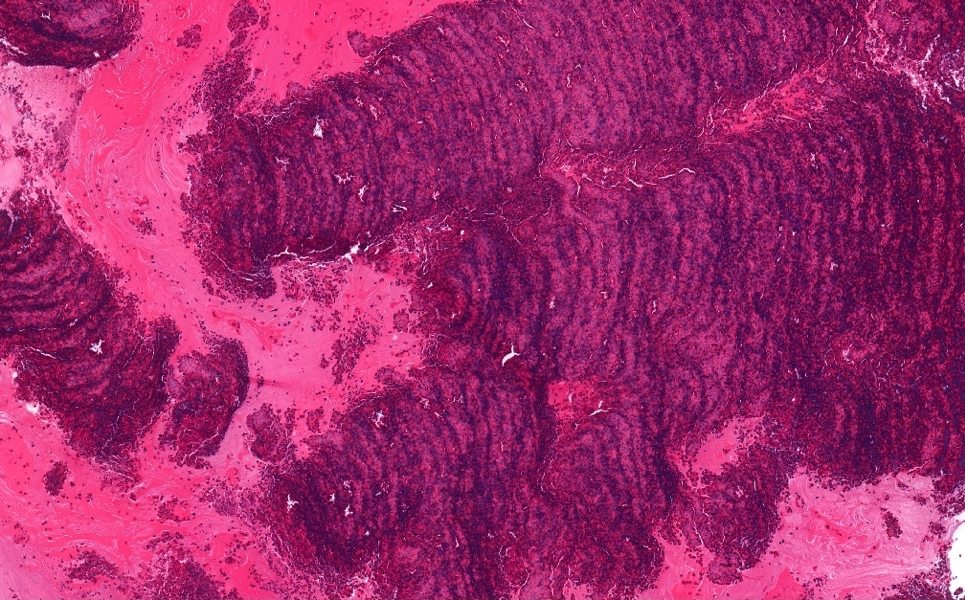
Microscopic (histologic) description
- Eosinophilic mucin (allergic mucin) is diagnostic: layered appearance of mucin admixed with cellular debris, sloughed epithelium, eosinophils (some may be degranulated), Charcot-Leyden crystals and other inflammatory cells (Head Neck Pathol 2016;10:40)
- Scanty fungal hyphae identified in 27 - 91% of cases (often found only with GMS stain) (Indian J Otolaryngol Head Neck Surg 2022;74:4640, Head Neck Pathol 2016;10:40)
- Charcot-Leyden crystals are pink / red refractive and form long needle-like structures
- Eosinophils may have degenerative changes of smudged, elongated or basophilic nuclei
- No evidence of tissue invasion by fungi
Microscopic (histologic) images
Molecular / cytogenetics description
- Fungal polymerase chain reaction (PCR) may be useful to determine specific fungal species (J Clin Diagn Res 2017;11:DC10)
Sample pathology report
- Sphenoid sinus, right, excision:
- Consistent with allergic fungal rhinosinusitis (see comment)
- Comment: The specimen is composed of eosinophilic mucin (allergic mucin) and strips of respiratory mucosa with chronic rhinosinusitis with eosinophilia. GMS stain shows scattered fungal organisms. The overall histologic features are consistent with allergic fungal rhinosinusitis. No evidence of invasive fungal disease is seen.
Differential diagnosis
- Invasive fungal rhinosinusitis:
- Tissue invasion by fungi is the hallmark for invasive fungal rhinosinusitis and is absent in allergic fungal rhinosinusitis
- Invasive fungal rhinosinusitis most commonly impacts immunocompromised hosts, whereas allergic fungal rhinosinusitis occurs in immunocompetent patients with atopy
- Fungal ball:
- Fungal ball has densely packed fungal hyphae, whereas allergic fungal rhinosinusitis contains sparse fungal elements
- Fungal ball lacks abundant allergic mucin
- Allergic fungal rhinosinusitis and fungal ball may coexist (Laryngoscope 2009;119:1809)
Additional references
Board review style question #1
Board review style answer #1
B. Dematiaceous fungi or Aspergillus. The pictures show allergic fungal rhinosinusitis with eosinophilic mucin on H&E and scanty fungal elements on GMS stain. The most common fungal organisms seen in this condition are dematiaceous fungi or Aspergillus. Answers A, C and D are incorrect because Mucor, Histoplasma and Candida are fungal organisms but not the most common cause of allergic fungal rhinosinusitis.
Comment Here
Reference: Allergic fungal rhinosinusitis
Comment Here
Reference: Allergic fungal rhinosinusitis
Board review style question #2
Which of the following statements regarding allergic fungal rhinosinusitis is true?
- It generally occurs in immunocompromised patients with atopy
- It is associated with elevated serum IgG and IgG4
- It is characterized by a neutrophilic rich inflammatory infiltrate in the respiratory mucosa and mucin
- It lacks evidence of tissue invasion by fungi
Board review style answer #2
D. It lacks evidence of tissue invasion by fungi. Allergic fungal rhinosinusitis lacks evidence of tissue invasion, which is characteristic of invasive fungal rhinosinusitis. Answer A is incorrect because allergic fungal rhinosinusitis affects immunocompetent patients with atopy. Answer C is incorrect because this entity is rich in eosinophils, not neutrophils. Answer B is incorrect because allergic fungal rhinosinusitis is associated with elevated serum IgE, not IgG or IgG4.
Comment Here
Reference: Allergic fungal rhinosinusitis
Comment Here
Reference: Allergic fungal rhinosinusitis