Nasal cavity, paranasal sinuses, nasopharynx
General
Staging-nasal cavity & sinuses
Editor-in-Chief: Debra L. Zynger, M.D.
Last author update: 26 September 2019
Last staff update: 18 August 2022
Copyright: 2004-2025, PathologyOutlines.com, Inc.
PubMed Search:
Staging nasal cavity paranasal sinuses
See also:
Staging terminology
Page views in 2024: 1,219
Page views in 2025 to date: 289
Cite this page: Magliocca K. Staging-nasal cavity & sinuses. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/nasalTNM.html. Accessed March 28th, 2025.
Definition / general
- Staging of definitive resections for carcinoma (squamous cell carcinoma, neuroendocrine carcinoma and minor salivary gland carcinoma) of the nasal cavity and paranasal sinuses should use this system (AJCC: Cancer Staging [Accessed 24 September 2018], CAP: Protocol for the Examination of Specimens from Patients with Cancers of the Nasal Cavity and Paranasal Sinuses [Accessed 24 September 2018])
- Cancer of the maxillary sinus is the most common of the sinonasal malignancies
- Ethmoid sinus and nasal cavity cancers are equal in frequency but considerably less common than maxillary sinus cancers
- Tumors of the sphenoid and frontal sinuses are rare
- Staging protocols such as those of CAP are to document procedure, tumor site, tumor laterality, tumor focality, tumor size, histologic type, histologic grade where applicable, margin status, lymphovascular invasion, perineural invasion, regional lymph node findings and summarize these pathologic findings using TNM system
Clinical features
- Cancers of the maxillary sinuses are the most common sinonasal malignancies, followed by cancers of the ethmoid sinuses, which are much less common
- Cancers of the frontal and sphenoid sinuses are rare
- When considering the nasal cavity and paranasal sinuses, 60% of malignant neoplasms originate from the maxillary sinus, 20 - 30% from the nasal cavity, 10 - 15% from the ethmoid sinus and 1% from the sphenoid and frontal sinuses
- When only considering the paranasal sinuses, 77% of malignant neoplasms originate from the maxillary sinus, 22% from the ethmoid sinus and 1% from the sphenoid and frontal sinuses
- Location as well as the extent of the mucosal lesion in the maxillary sinus has prognostic importance
Primary tumor (pT) - maxillary sinus
- pTX: Primary tumor cannot be assessed
- pTis: Carcinoma in situ
- pT1: Tumor limited to maxillary sinus mucosa with no erosion or destruction of bone
- pT2: Tumor causing bone erosion or destruction including extension into the hard palate or middle nasal meatus, except extension to posterior wall of maxillary sinus and pterygoid plates
- pT3: Tumor invades any of the following:
- Bone of the posterior wall of maxillary sinus
- Subcutaneous tissues
- Floor or medial wall of orbit, pterygoid fossa, ethmoid sinuses
- pT4: Moderately advanced or very advanced local disease
- pT4a: Moderately advanced local disease; tumor invades any of the following:
- Anterior orbital contents, skin of nose or cheek, minimal extension to anterior cranial fossa, pterygoid plates, sphenoid or frontal sinuses
- pT4b: Very advanced local disease; tumor invades any of the following:
- Orbital apex, dura, brain, middle cranial fossa, cranial nerves other than maxillary division of trigeminal nerve (V2), nasopharynx or clivus
Primary tumor (pT) - nasal cavity and ethmoid sinus
- pTX: Primary tumor cannot be assessed
- pTis: Carcinoma in situ
- pT1: Tumor restricted to any 1 subsite, with or without bone invasion
- pT2: Tumor invading 2 subsites in a single region or extending to involve an adjacent region within the nasoethmoidal complex, with or without bone invasion
- pT3: Tumor extends to invade the medial wall or floor of the orbit, maxillary sinus, palate or cribriform plate
- pT4: Moderately advanced or very advanced local disease
- pT4a: Moderately advanced local disease; tumor invades any of the following:
- Anterior orbital contents, skin of nose or cheek, minimal extension to anterior cranial fossa, pterygoid plates, sphenoid or frontal sinuses
- pT4b: Very advanced local disease; tumor invades any of the following:
- Orbital apex, dura, brain, middle cranial
Pathological regional lymph nodes (pN)
- pNX: Regional lymph nodes cannot be assessed
- pN0: No regional lymph node metastasis
- pN1: Metastasis in a single ipsilateral lymph node, ≤ 3 cm in greatest dimension and extranodal extension negative (ENE-)
- pN2a: Metastasis in:
- Single ipsilateral lymph node that is ≤ 3 cm and ENE+ or
- Single ipsilateral lymph node that is > 3 cm but ≤ 6 cm in greatest dimension and ENE-
- pN2b: Metastasis in multiple ipsilateral lymph nodes, none > 6 cm in greatest dimension and ENE-
- pN2c: Metastasis in bilateral or contralateral lymph node(s), none > 6 cm in greatest dimension and ENE-
- pN3a: Metastasis in a lymph node that is > 6 cm in greatest dimension and ENE-
- pN3b: Metastasis in:
- Single ipsilateral lymph node, > 3 cm and ENE+ or
- Multiple ipsilateral, contralateral or bilateral lymph nodes, any with ENE+ or
- Single contralateral lymph node of any size and ENE+
Notes:
- Designation of "U" or "L" may be used for any N category to indicate metastasis above the lower border of the cricoid (U) or below the lower border of the cricoid (L)
- A selective neck dissection will ordinarily include 10+ lymph nodes and a comprehensive neck dissection (radical or modified radical neck dissection) will ordinarily include 15+ lymph nodes
- Negative pathologic examination of a smaller number of nodes still mandates a pN0 designation
- Midline nodes are considered ipsilateral nodes
AJCC prognostic stage grouping
| Stage 0:
| Tis
| N0
| M0
|
| Stage I:
| T1
| N0
| M0
|
| Stage II:
| T2
| N0
| M0
|
| Stage III:
| T3
| N0
| M0
|
|
| T1 - 3
| N1
| M0
|
| Stage IVA:
| T4a
| N0 - 1
| M0
|
|
| T1 - 4a
| N2
| M0
|
| Stage IVB:
| Any T
| N3
| M0
|
|
| T4b
| Any N
| M0
|
| Stage IVC:
| Any T
| Any N
| M1
|
Registry data collection variables
- Extranodal extension (ENE) clinical (present versus absent)
- ENE pathological (present versus absent)
- Extent of microscopic ENE (distance of extension from the native lymph node capsule to the farthest point of invasion in extranodal tissue)
- Perineural invasion
- Lymphovascular invasion
- Performance status
- Tobacco use and pack years
- Alcohol use
- Depression diagnosis
Histologic grade
- GX: Cannot be assessed
- G1: Well differentiated
- G2: Moderately differentiated
- G3: Poorly differentiated
Notes:
- For histologic types of carcinomas that are amenable to grading, 3 histologic grades are suggested, as shown above
- For conventional squamous cell carcinoma, histologic grading as a whole does not perform well as a prognosticator
- Nonetheless, it should be recorded when applicable, as it is a basic tumor characteristic
- Selecting either the most prevalent grade or the highest grade for this synoptic protocol is acceptable
- Variants of squamous cell carcinoma (i.e. verrucous, basaloid, etc.) have an intrinsic biologic potential and currently do not appear to require grading
- Histologic (microscopic) grading of salivary gland carcinomas has been shown to be an independent predictor of behavior and plays a role in optimizing therapy
- However, most salivary gland carcinoma types have an intrinsic biologic behavior and attempted application of a universal grading scheme is merely a crude surrogate
- Thus a generic grading scheme is no longer recommended for salivary gland carcinomas
- Carcinoma types for which grading systems exist and are relevant are incorporated into histologic type
- 3 major categories that are amenable to grading include adenoid cystic carcinoma, mucoepidermoid carcinoma and adenocarcinoma, not otherwise specified
- In some carcinomas, histologic grading may be based on growth pattern, such as in adenoid cystic carcinoma, for which a histologic high grade variant has been recognized based on the percentage of solid growth
- Those adenoid cystic carcinomas showing ≥ 30% of solid growth pattern are considered to be histologically high grade carcinomas
- Histologic grading of mucoepidermoid carcinoma includes a combination of growth pattern characteristics (e.g. cystic, solid, neurotropism) and cytomorphologic findings (e.g. anaplasia, mitoses, necrosis)
- Adenocarcinomas, not otherwise specified do not have a formalized grading scheme and are graded intuitively based on cytomorphologic features
- For nonsalivary sinonasal adenocarcinoma, intestinal type adenocarcinoma grading is based on growth pattern
- Generally, papillary patterns correspond to low grade tumors, colonic to intermediate grade and solid to high grade
- Mucinous and mixed types have variable behavior
- Nonintestinal type adenocarcinomas are graded intuitively into low, intermediate and high grade tumors
Histologic type
- CAP protocol applies only to carcinomas and melanomas and does not apply to lymphomas, sarcomas or neuroectodermal tumors (e.g. olfactory neuroblastoma, primitive neuroectodermal tumor [PNET], others)
- Nasal cavity and paranasal sinuses
- Squamous cell carcinoma, keratinizing
- Squamous cell carcinoma, nonkeratinizing
- Adenosquamous carcinoma
- Basaloid squamous cell carcinoma
- Papillary squamous cell carcinoma
- Spindle cell squamous cell carcinoma
- Verrucous squamous cell carcinoma
- Lymphoepithelial carcinoma (nonnasopharyngeal)
- Sinonasal undifferentiated carcinoma (SNUC)
- NUT carcinoma
- Adenocarcinoma, non salivary gland type
- Intestinal type
- Nonintestinal type
- Carcinomas of minor salivary glands
- Mucoepidermoid carcinoma, low grade
- Adenoid cystic carcinoma
- Acinic cell carcinoma
- Polymorphous adenocarcinoma
- (Mammary analogue) secretory carcinoma
- Salivary duct carcinoma
- Carcinoma ex pleomorphic adenoma
- Epithelial myoepithelial carcinoma
- (Hyalinizing) clear cell carcinoma
- Adenocarcinoma, not otherwise specified
- Neuroendocrine carcinoma
- Large cell neuroendocrine carcinoma
- Small cell neuroendocrine carcinoma
Board review style question #1
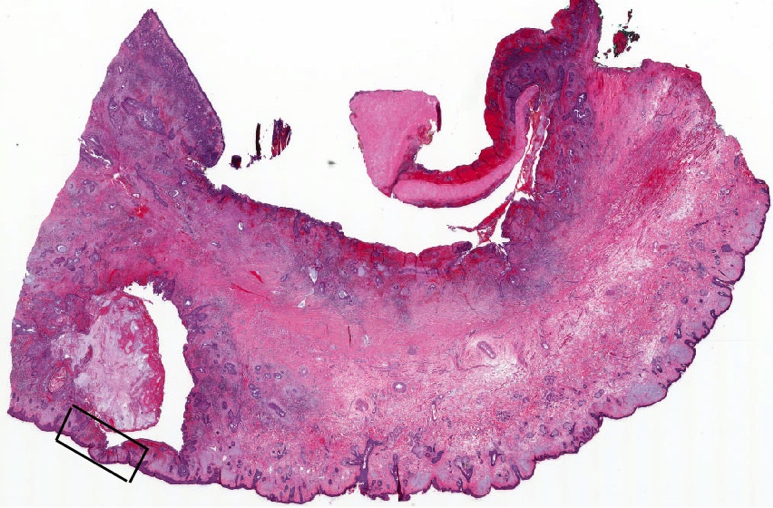
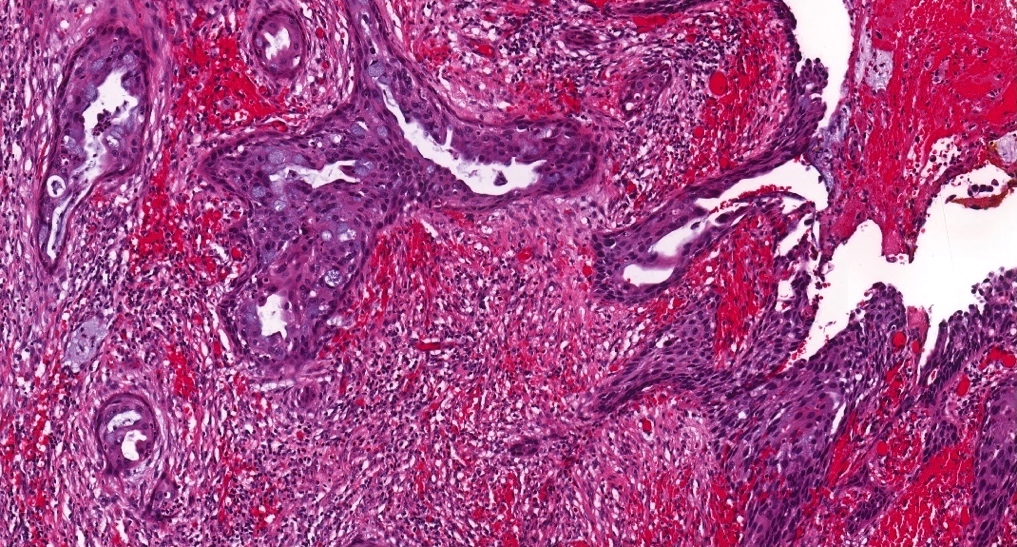
Based on the gross and microscopic examination of the 2.2 cm nasal cavity adenosquamous carcinoma originating along the right nasal septum in the following images, which of the pT category criteria in the 8th edition AJCC staging guide is satisfied?

Image 1
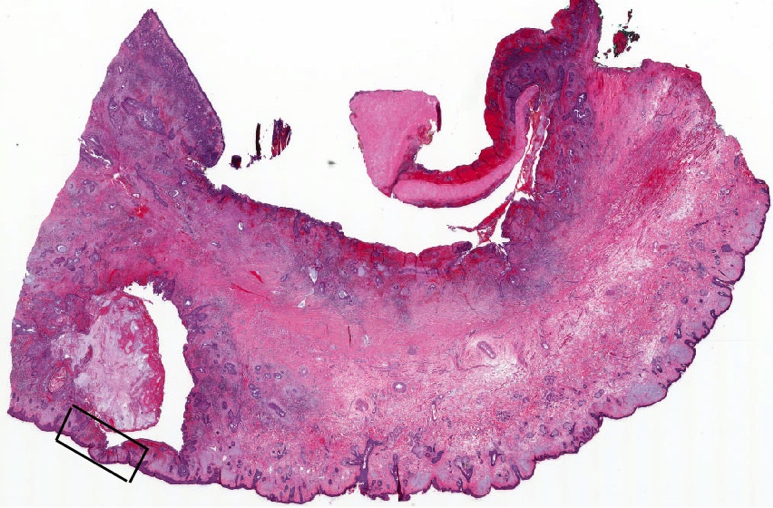
Image 2

Image 3
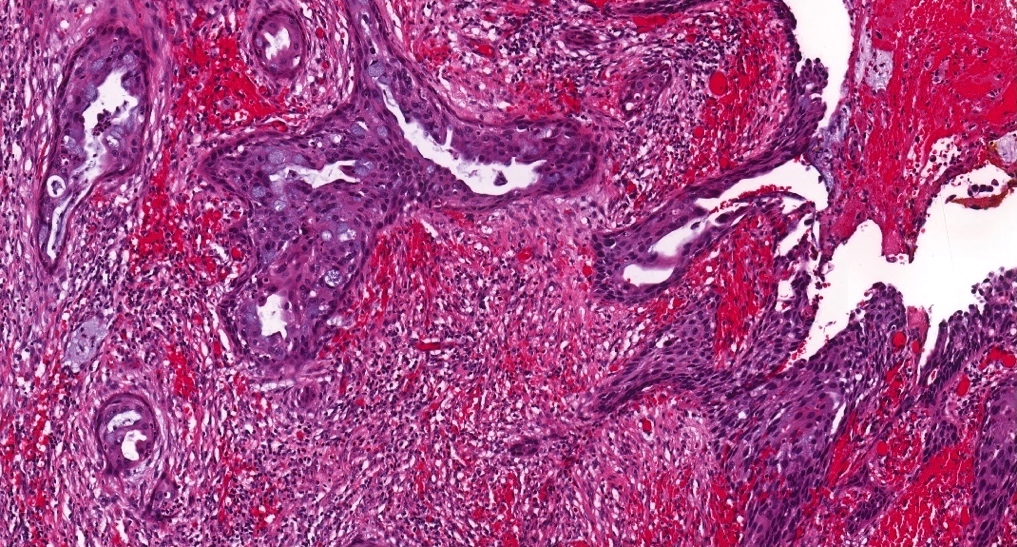
Image 4
- pT1 due to tumor size
- pT2 due to tumor size
- pT3 due to extension to overlying nasal skin
- pT4 due to extension to overlying nasal skin
Board review style answer #1

Back to top