Table of Contents
Definition / general | Essential features | Epidemiology | Sites | Pathophysiology | Clinical features | Diagnosis | Laboratory | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Molecular / cytogenetics description | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Riegler AN, Leal SM. Streptococcus pneumoniae. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/microbiologystreptococcuspneumoniae.html. Accessed March 28th, 2025.
Definition / general
- Gram positive bacterium
- Taxonomy: order Lactobacillales, family Streptococcaceae
Essential features
- Lancet shaped encapsulated gram positive diplococci
- Alpha hemolytic, optochin (P disk) susceptible, bile soluble
- Negative: catalase, oxidase and indole
- Normal nasopharyngeal flora
- Major cause of pneumonia, bacteremia, meningitis, sinusitis, otitis media
- 2 million infections per year; 6,000 deaths
- Vaccination available for infants, adults > 65 years and immunocompromised individuals, resulting in a drastic reduction in invasive infections
- Emerging antimicrobial resistance (AMR) (Am J Ther 2017;24:e361, Lancet 2022;399:629)
- Macrolide (azithromycin) resistance
- Serious threat category for the CDC Antimicrobial Resistance Report (Lancet 2022;399:629, CDC: 2019 AR Threats Report [Accessed 6 September 2022])
Epidemiology
- Infants, age ≥ 65 years old, immunocompromised
- Unvaccinated individuals or hosts with waning immunity
- Postviral 2° infection (influenza, etc.) (Microbiol Immunol 2022;66:253, Influenza Other Respir Viruses 2016;10:394, J Formos Med Assoc 2022;121:687)
Sites
- Normal nasopharyngeal flora
- Lung
- Sinuses
- Inner ear
- Bloodstream
- Meninges
- Cornea
- Conjunctiva (mBio 2016;7:e01792)
Pathophysiology
- Invasive infection by commensal strains; person to person spread of novel serotypes that evade vaccine mediated protection
- Direct spread from nasooropharynx to sinus, inner ear and brain
- Aspiration into the lower respiratory tract
- Hematogenous spread via oropharyngeal injury, damaged alveolar capillaries and active transit across endothelial cells utilizing host receptors PECAM1, pIgR, laminin receptor and PAFR (J Exp Med 2017;214:1619, J Clin Invest 2009;119:1638)
- Virulence factors aid in immune evasion, colonization and invasion (Nat Rev Microbiol 2018;16:355)
- IgA protease, hemolytic toxin (pneumolysin), biofilm formation, complement sequestering proteins (e.g., PspA, PepO, Eno, Pht), metal binding proteins (PsaA, PiuA and PiaA) and cell binding proteins (e.g., RgrA, CbpA)
Clinical features
- Causative agent for pneumococcal disease
- Pneumonia, bacteremia, meningitis, acute otitis media, sinusitis
- High rates of inappropriate Z-Pak (Zithromax, azithromycin) use in outpatient settings are driving macrolide resistance
Diagnosis
- Dyspnea: chest Xray or CT scan showing lung consolidation, typically lobar pattern, sputum Gram stain and culture, blood culture, urinary antigen test
- Meningismus: head CT or MRI showing meningeal inflammation; CSF Gram stain and culture
- Facial pain and congestion: head CT, culture
- Ear pain / vertigo: head CT, culture
- Reference: StatPearls: Streptococcus Pneumoniae [Accessed 13 September 2022]
Laboratory
- Aerobic growth in routine culture conditions, 37 °C
- Can grow anaerobically
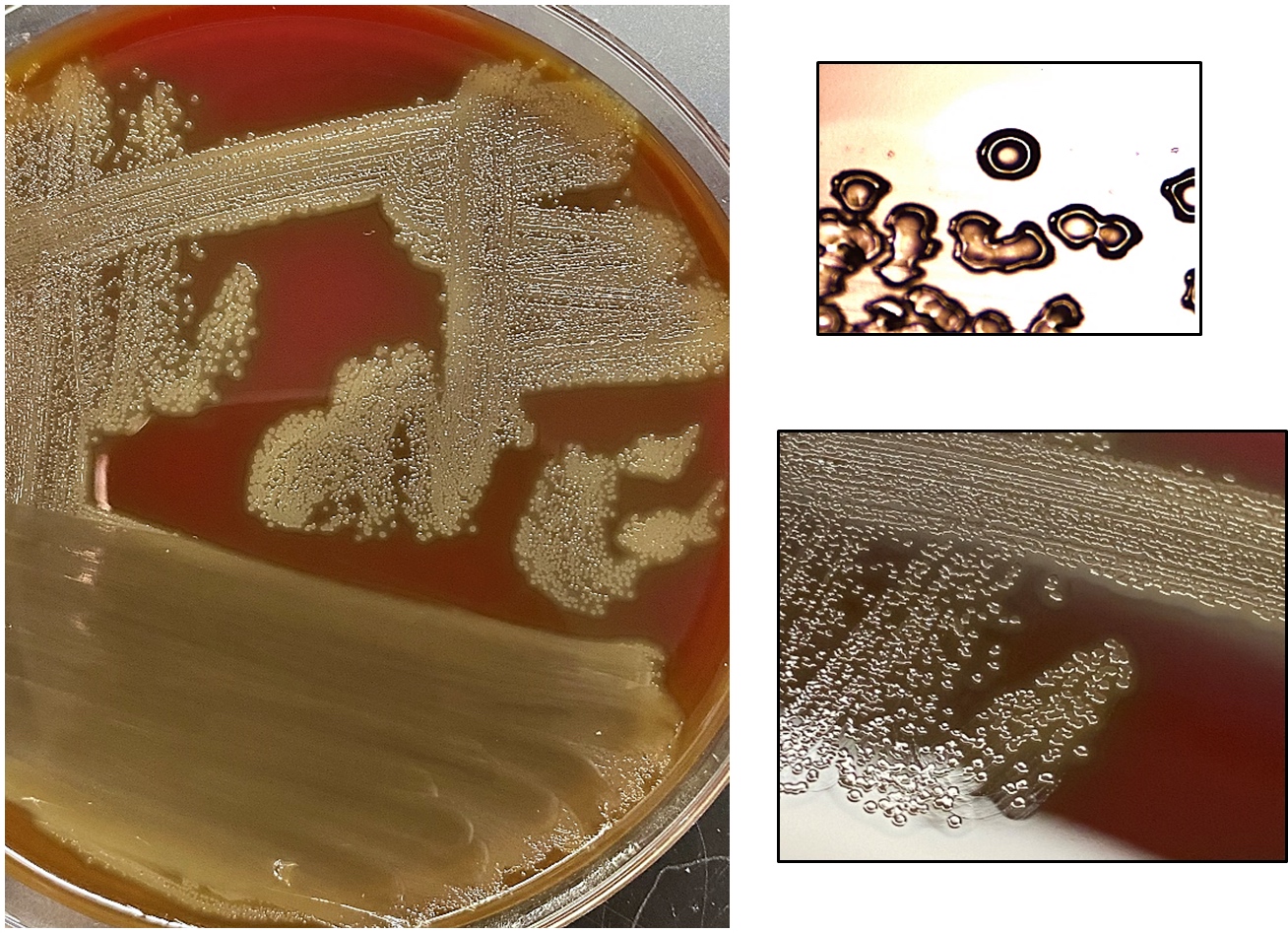
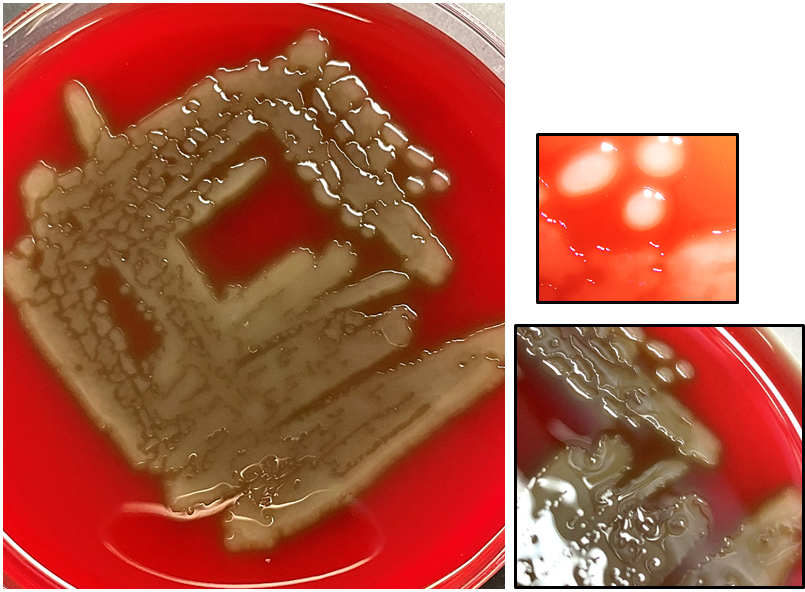
- Gray-white glistening colonies
- Growth on blood agar, α hemolytic
- Optochin (P disk) susceptible, bile soluble*
- *Optochin resistance or bile resistance are rare → sporadic isolation (J Clin Microbiol 2012;50:1326, Clin Lab 2021;67, J Clin Microbiol 2013;51:3242, Lancet 1988;2:281)
- Negative: catalase, oxidase, urease, indole, motility
- Lancet shaped encapsulated gram positive diplococci
- Autolysis occurs in some isolates resulting in a characteristic central depression (dimple) within colony
- Other isolates have a mucoid appearance (Clin Microbiol Rev 2015;28:871)
- Serotype 3: large mucoid colonies
- Serotypes 6, 9, 11, 14, 18, 19 and 23: small mucoid colonies
- Definitive identification by MALDI TOF mass spectrometry
- Positive quellung (Neufeld quellung) reaction or latex agglutination assay to determine capsular serotype
- Urinary antigen test
- Rapid detection of the C polysaccharide antigen (teichoic acid) in patient urine samples (J Clin Microbiol 2018;56:e00787, Clin Infect Dis 2018;66:1504)
Case reports
- 6 month old girl from The Gambia with recurrent meningitis caused by S. pneumoniae serotype 14 (Ann Clin Microbiol Antimicrob 2009;8:3)
- 20 month old girl with lethal disseminated infection with multidrug resistant, nonvaccine S. pneumoniae serotype 15A (Int J Infect Dis 2020;90:219)
- Teenage girl with epilepsy and previous laryngectomy / tracheostomy develops multidrug resistant pneumonia with nonencapsulated S. pneumoniae (J Infect Chemother 2020;26:749)
- 68 year old woman with concurrent necrotizing fasciitis of the lower leg and meningitis caused by S. pneumoniae (BMC Infect Dis 2019;19:358)
- 76 year old diabetic man with pneumonia associated invasive infection with mucoid S. pneumoniae, serotype 3 (BMC Res Notes 2017;10:21)
Treatment
- Typical first line therapy: amoxicillin
- Resistance to 1 or more antibiotic groups is seen in > 3 out of 10 of cases (and is increasing) (Am J Ther 2017;24:e361)
- β lactam resistance in 45% of isolates: mutations in penicillin binding proteins (PBP2b and PBP2x) (Mayo Clin Proc 2000;75:1161)
- Increasing macrolide resistance: mefA gene (drug efflux) or erm gene (methylation of macrolide binding site) (J Clin Microbiol 2004;42:3570)
- Fluoroquinolone resistance is rare (< 2%): mutations in gyrA (DNA gyrase), parC and parE (topoisomerase IV) and increased expression of pmrA (drug efflux) (Antimicrob Agents Chemother 2001;45:3517)
- Tetracycline resistance in 25%: ribosomal protection proteins mediated by tet genes (M and O) (Antimicrob Agents Chemother 2005;49:1636)
- Polysaccharide conjugate vaccines: PCV13 for children < 2 years; PPSV23 for adults > 65 years or immunocompromised
Clinical images
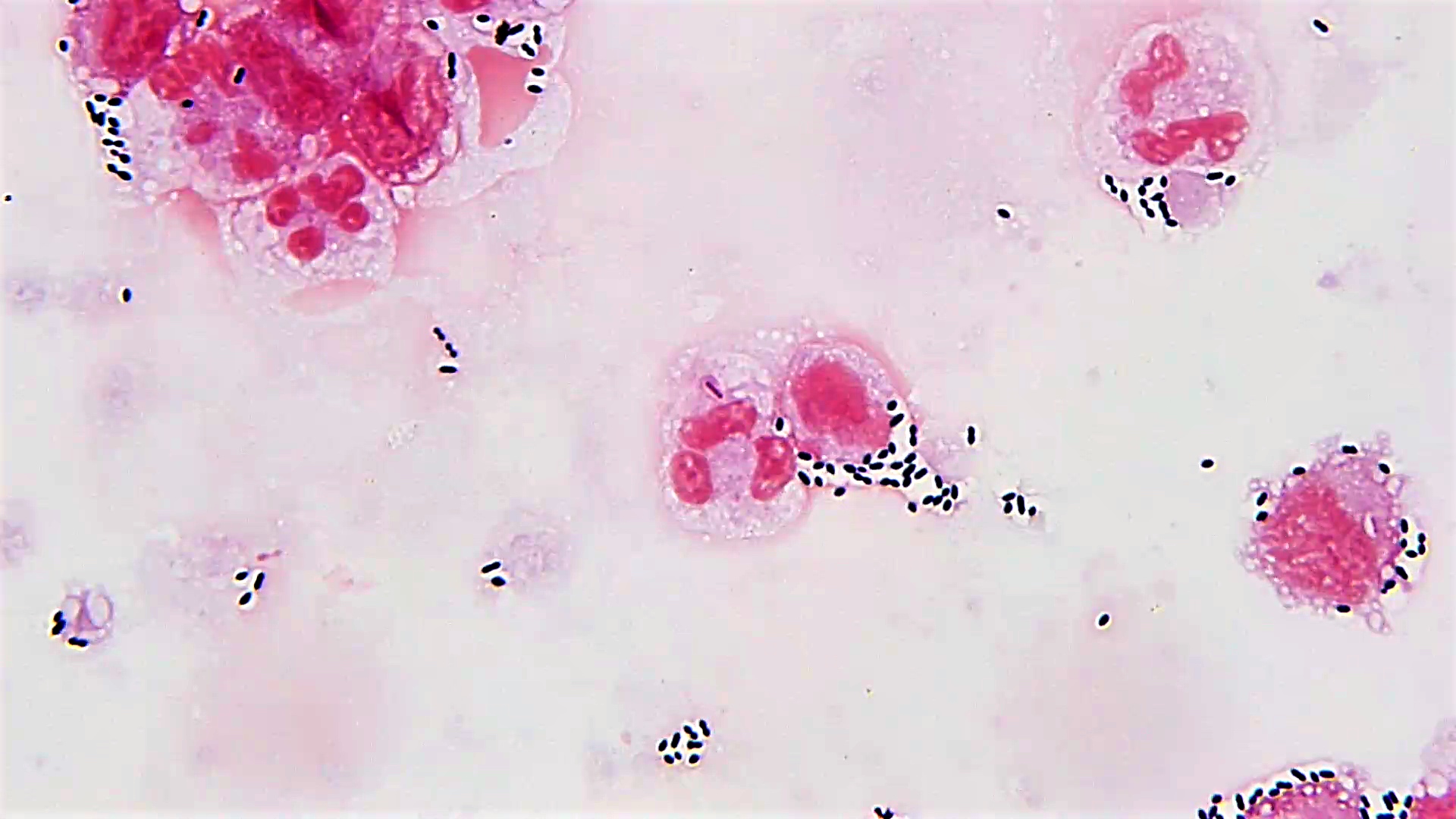
Microscopic (histologic) description
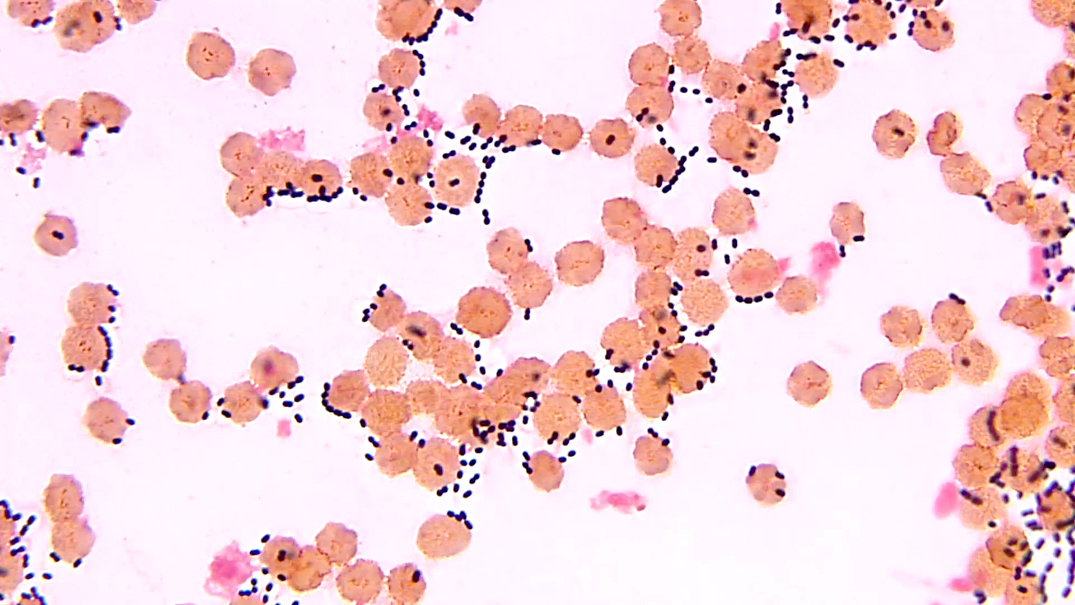
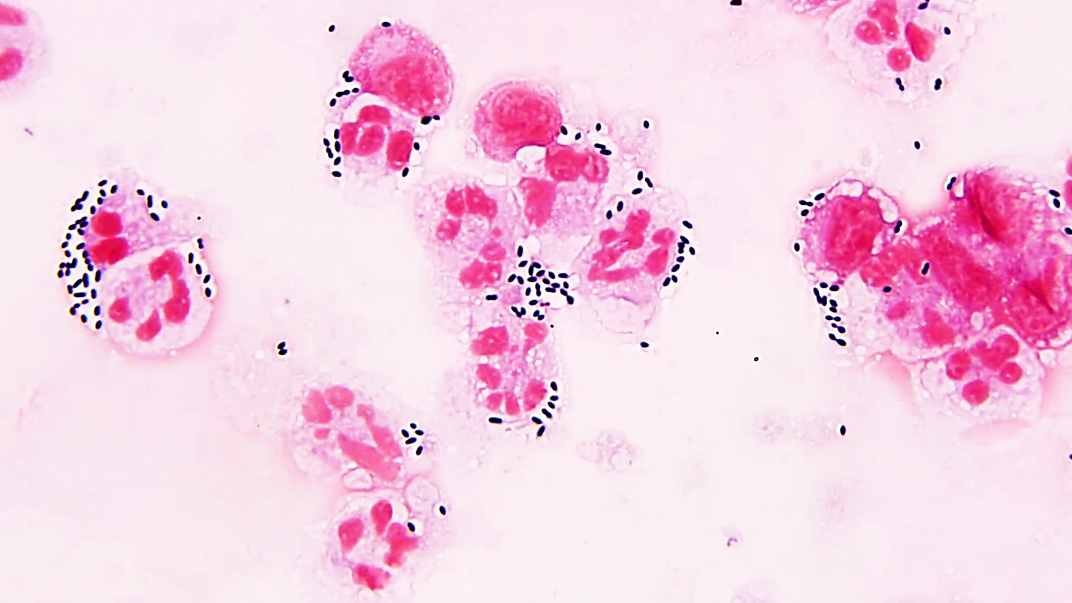
- Lancet shaped encapsulated gram positive diplococci
- Polysaccharide capsule
Microscopic (histologic) images
Positive stains
- It is rare to obtain surgical pathology specimens with S. pneumoniae
- If present, they are basophilic on H&E, black on GMS, and purple on tissue Gram stain
Molecular / cytogenetics description
- Both major commercial FDA approved MALDI TOF mass spectrometry systems enable definitive identification
- 16S rRNA sequencing is the gold standard for bacterial identification (Clin Microbiol Infect 2013;19:1066, J Clin Microbiol 2012;50:4087, J Microbiol Methods 2020;170:105854)
- S. mitis, S. pseudopneumoniae and S. oralis are often misidentified as S. pneumoniae due to similar capsule type; differentiation may require molecular validation (Eur J Clin Microbiol Infect Dis 2020;39:2247)
Differential diagnosis
- Other gram positive cocci:
- S. pseudopneumoniae:
- Also lancet shaped gram positive diplococci but are bile insoluble and optochin (P disk) nonsusceptible
- Streptococcus viridans group:
- Also α hemolytic but are optochin (P disk) and bile resistant (Infect Genet Evol 2011;11:1709)
- Group A and group B streptococci:
- β hemolytic and form long chains
- Staphylococcus spp.:
- Catalase positive and aggregate into grape-like clusters (Baron: Medical Microbiology, 4th Edition, 1996)
- S. pseudopneumoniae:
Additional references
Board review style question #1
An elderly man presents with fever (39 °C), a productive cough with rust colored sputum, headache, dizziness and anorexia. His chest exam showed bibasilar crackles, pO2 was 85 and respiratory rate was 35. A chest radiograph showed dense consolidation of the left lower lobe and opacities throughout both lung fields. One pathogen was predominant on sputum culture. Gram stain (shown in figure) and colony morphology are consistent with S. pneumoniae. What additional biochemical test result helps render a definitive identification?
- Bile soluble
- Catalase positive
- Optochin (P disk) resistant
- Oxidase positive
Board review style answer #1
A. Bile soluble. S. pneumoniae is negative for catalase and oxidase as well as resistant to optochin (P disk). When bile is placed on the culture plate S. pneumoniae colonies will dissolve, whereas colonies from other viridans group streptococci will remain intact.
Comment Here
Reference: Streptococcus pneumoniae
Comment Here
Reference: Streptococcus pneumoniae
Board review style question #2
A sinus culture from a fully vaccinated 4 year old child with facial pain, ear pain and intermittent dizziness, grew 4+ lancet shaped gram positive diplococci forming gray, α hemolytic colonies with central umbilication (dimple) on blood agar. The isolate tested catalase negative and was optochin nonsusceptible. MALDI TOF mass spectrometry rendered the definitive identification. What is the most likely organism?
- Streptococcus agalactiae
- Streptococcus pneumoniae
- Streptococcus pseudopneumoniae
- Streptococcus pyogenes
Board review style answer #2
C. Streptococcus pseudopneumoniae. S. pyogenes (group A streptococci) and S. agalactiae (group B streptococci) are β hemolytic. S. pseudopneumoniae is α hemolytic and can mimic the appearance of S. pneumoniae but will test bile insoluble and optochin resistant.
Comment Here
Reference: Streptococcus pneumoniae
Comment Here
Reference: Streptococcus pneumoniae