Table of Contents
Definition / general | Essential features | Epidemiology | Sites | Pathophysiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Case reports | Treatment | Clinical images | Gross description | Molecular / cytogenetics description | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Gao NJ, Putnam NE. Shigella. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/microbiologyshigella.html. Accessed March 31st, 2025.
Definition / general
- Taxonomy: order Enterobacterales, family Enterobacteriaceae
- Shigella spp. and Escherichia coli represent a single genomospecies but are classified as separate genera for medical purposes due to distinctive disease
- Highly infectious, virulent gram negative bacilli that cause diarrheal diseases, with progression to dysentery
Essential features
- Gram negative bacilli easily spread via fecal-oral transmission and highly infectious due to low infectious dose
- Shigellosis typically presents as self limiting watery or bloody diarrhea but can also cause severe disease, such as hemolytic uremic syndrome
- Difficult to distinguish from E. coli due to high genomic and proteomic similarity
- Children and the immunocompromised have the highest risk of severe disease
Epidemiology
- Shigella spp. has 4 subgroups (species); these infect humans as the major reservoir but can also infect nonhuman primates:
- Group A: S. dysenteriae, 15 serotypes
- S. dysenteriae type 1: severe infections due to the production of Shiga toxin type 1 by the stx1 gene
- Group B: S. flexneri, 8 serotypes
- Group C: S. boydii, 19 serotypes
- Group D: S. sonnei, 1 serotype
- S. sonnei disease is generally less severe
- Group A: S. dysenteriae, 15 serotypes
- Transmitted via direct or indirect fecal-oral route
- Direct contact with an infected person or indirect transmission through food or water contaminated with human feces containing Shigella spp.
- Shigella spp. are easily transmitted due to very low infectious dose
- Fewer than 100 viable bacterial cells need to be ingested to cause infection, in part, due to their resistance to the low pH of the stomach
- Associated with poor hygiene and poor sanitation
- Use of chlorinated water can decrease contamination rates
- Direct contact with an infected person or indirect transmission through food or water contaminated with human feces containing Shigella spp.
- Worldwide, endemic in tropical and temperate climates; reported cases represent only a small proportion of cases
- 180 million human infections annually (StatPearls: Shigella [Accessed 14 March 2022])
- Only 1.5 million cases annually in developed countries
- 450,000 cases annually in the U.S.
- 1 million deaths annually
- S. sonnei (77%), S. flexneri: first and second most common in U.S.
- S. flexneri, S. dysenteriae, S. boydii: most common in developing countries
- 180 million human infections annually (StatPearls: Shigella [Accessed 14 March 2022])
- Risk groups:
- Children < 5 years of age in low / middle income countries
- Immunocompromised hosts
- Advanced age
- Malnourished
- Institutional environments: day care setting or nursing home
- Developing areas that lack running water or indoor plumbing
- Risky sexual behaviors
- Individuals with HLA B27 antigen are predisposed to develop post infection reactive arthritis
- Immunity:
- Little innate immune protection
- Convalescent antibody response to O antigen (LPS) are thought to offer type specific protection
- Breastfeeding is protective for infants and young children
- Prevention:
- Proper hand hygiene and food handling
- Up to 40% attack rate within an infected household
- Antibiotics may be used to reduce length of shedding / transmission
- No vaccine available
- Proper hand hygiene and food handling
Sites
- Gastrointestinal: infection descends from distal small intestine to the large intestine (main site of infection)
- Locally invasive but rarely penetrates beyond the lamina propria
Pathophysiology
- 1 - 4 day incubation period but may be up to 1 week (Heymann: Control of Communicable Diseases Manual, 20th Edition, 2014)
- Shigella spp. harbor a large plasmid with virulence factors that encode the proteins necessary to invade intestinal epithelial cells, including invasion plasmid antigens (IpaB, IpaC and IpaD) (Gilligan: Cases in Medical Microbiology and Infectious Diseases, 4th Edition, 2014)
- Organisms bind M cells and invade the lamina propria, then invade enterocytes from the basolateral surface (Baron: Medical Microbiology, 4th Edition, 1996)
- Lateral spread to infect adjacent cells in intestinal epithelium; bacteria use host cell actin for intercellular actin polymerization to propel into neighboring cells, avoiding extracellular exposure
- Invasion of macrophages induces cellular apoptosis and inflammation
- Presence of white blood cells (WBCs) in feces indicates that the patient has an inflammatory type of diarrhea (suggestive of enteroinvasive bacteria or select protozoans)
- Inflammation can lead to ulceration, a characteristic of shigellosis
- Integrity of the intestinal epithelial barrier breaks down
- Impairs absorption of fluids and nutrients
- Loss of fluids and intestinal bleeding causes bloody diarrhea
- Shigella dysenteriae serotype 1 toxin (Shiga toxin):
- AB5 toxin with a catalytic A chain and 5 B chains; works by inhibiting protein synthesis
- Causes direct cellular damage to intestinal epithelium
- Cause of Shigella associated complications, such as hemolytic uremic syndrome (HUS) which can be fatal
- Drives cytotoxicity and development of vascular lesions
Diagrams / tables
Clinical features
- Mild and asymptomatic infections are usually self limiting, lasting 4 - 7 days
- Inflammatory diarrhea (dysentery), characterized by visible blood and white blood cells in stool
- Often accompanied by abdominal pain and high fever
- Diarrhea causes dehydration / hyponatremia, attributable to severe electrolyte imbalance
- Lethargy, altered mental status
- Common in children
- Rare complications or presentation in immunocompromised or patients with chronic underlying conditions:
- Bacteremia
- Intestinal perforation
- Ekiri syndrome
- Lethal / toxic encephalopathy
- Seizures
- Postinfectious manifestations (Clin Infect Dis 2017;65:e45):
- HUS, characterized by anemia, destruction of platelets and acute kidney injury
- Often associated with Shigella dysenteriae serotype 1 but can be due to other Shiga toxin producing strains of Shigella or E. coli
- Reactive arthritis / Reiter syndrome (Shigella flexneri)
- Erythema nodosum
- Glomerulonephritis
- Postinfectious inflammatory bowel syndrome (IBS)
- HUS, characterized by anemia, destruction of platelets and acute kidney injury
Diagnosis
- Nonspecific or suggestive diagnostic tests; recommend additional microbiologic work up (Gilligan: Cases in Medical Microbiology and Infectious Diseases, 4th Edition, 2014)
- Fecal occult blood test: positive
- Fecal leukocyte examination: positive
- Imaging / colonoscopy (see Colon - Shigella)
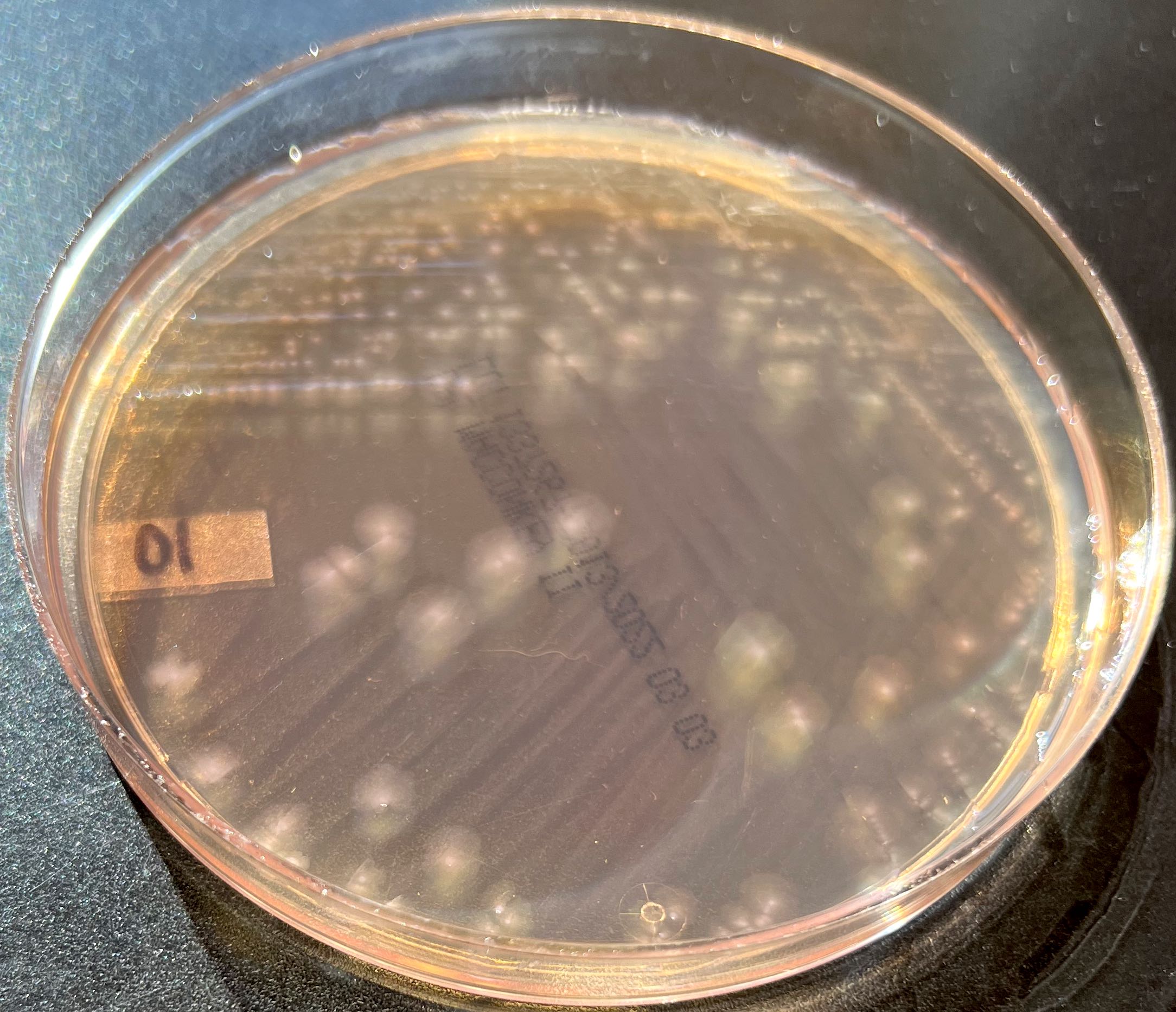
- Stool culture and isolate identification, rule out pathogens with similar growth (Heymann: Control of Communicable Diseases Manual, 20th Edition, 2014, Carroll: Manual of Clinical Microbiology, 12th Edition, 2019)
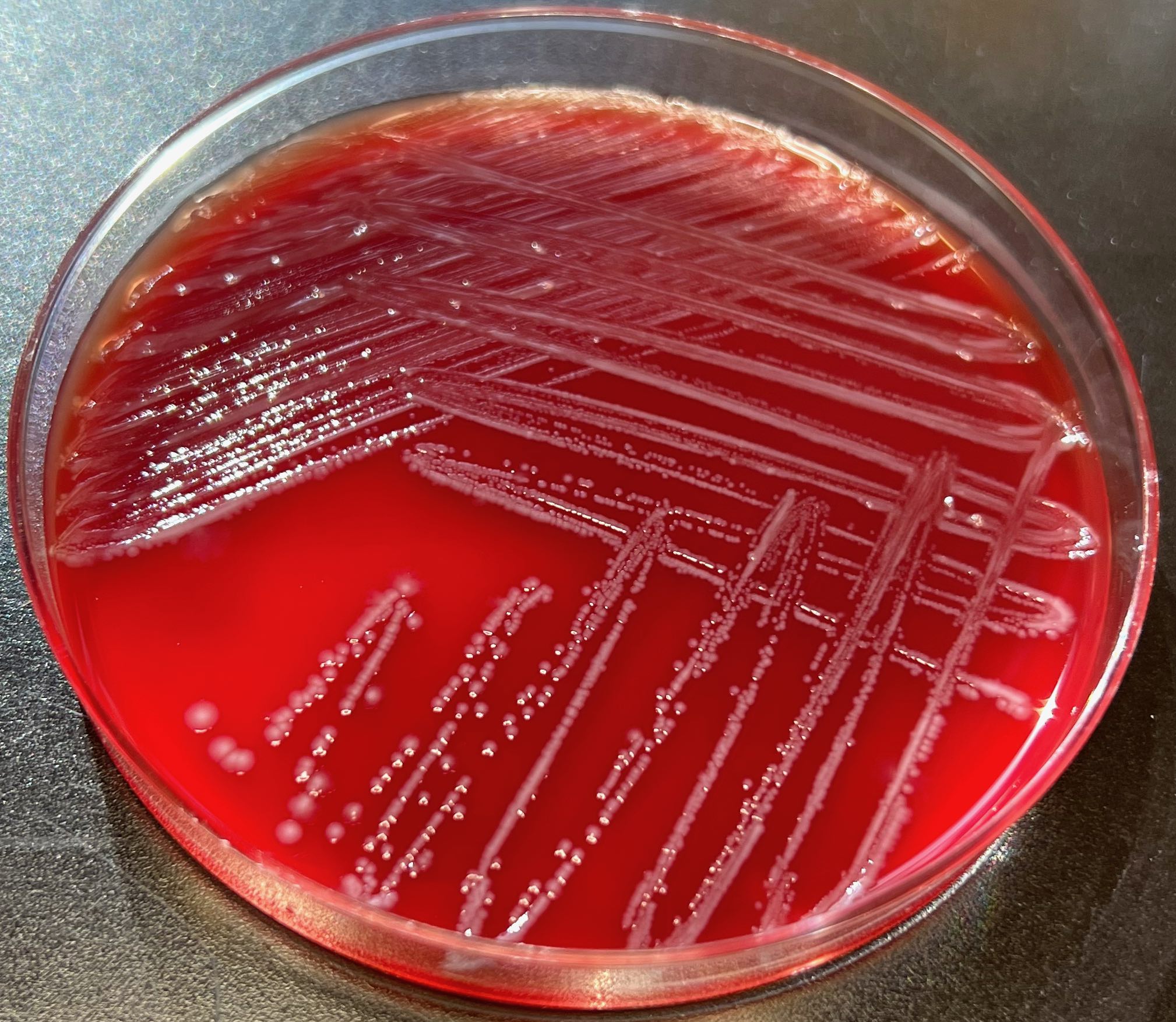
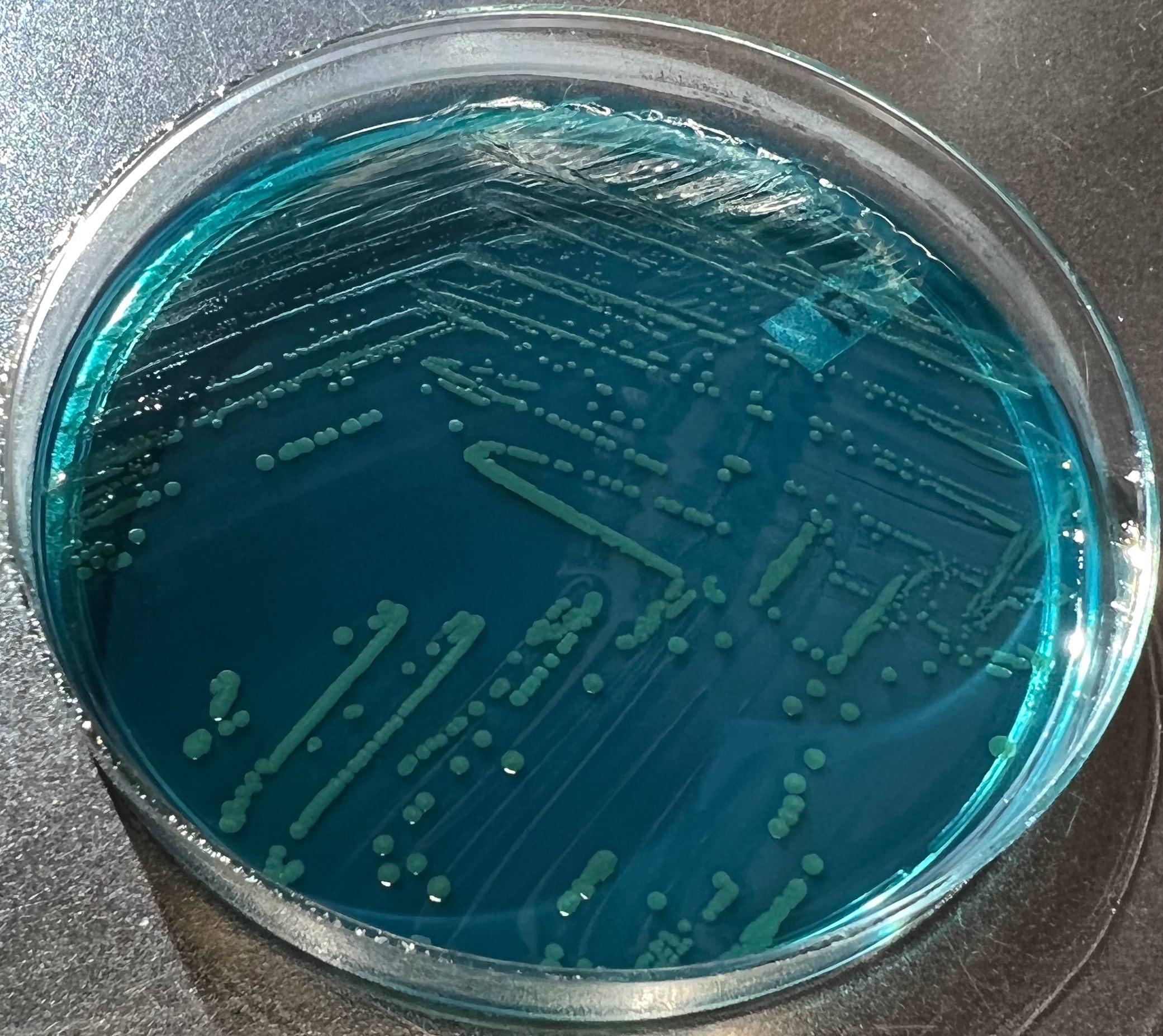
- Hektoen enteric (HE) agar: green colonies
- Xylose lysine deoxycholate (XLD) agar: red colonies
- GN broth (BD) for enrichment
- VITEK 2 gram negative ID card (BioMérieux)
- Shiga toxin enzyme immunoassays (EIAs)
- Stool gastrointestinal pathogen PCR multiplex panels (advantage: faster than culture) (Carroll: Manual of Clinical Microbiology, 12th Edition, 2019)
- BioFire FilmArray Gastrointestinal Panel (BioMérieux)
- BD MAX Enteric Bacterial Panel (BD)
- Prodesse ProGastro SSCS Assay (Hologic)
- NxTAG Gastrointestinal Pathogen Panel (Luminex)
Laboratory
- Shigella spp. are considered serologically defined biotypes of E. coli but are classified as a separate genus for medical purposes, due to distinctive disease
- Conventional matrix assisted laser desorption / ionization time of flight (MALDI TOF) mass spectrometry cannot distinguish Shigella from E. coli (New Microbes New Infect 2017;21:58)
- Gram negative rod, nonmotile, facultative anaerobes
- Lactose nonfermenting on MacConkey agar, consistent with some other diarrheal pathogens
- Triple sugar iron (TSI) agar slant: glucose fermenter (acid producing at bottom), no fermentation of sucrose or lactose and use of amino acids (alkaline at top)
- Expect: K / A, gas negative, hydrogen sulfide negative
- IMVIC biochemicals (J Bacteriol 2004;186:7460, Procop: Koneman's Color Atlas and Textbook of Diagnostic Microbiology, 7th Edition, 2016):
- Indole: variable
- Methyl red: positive
- Voges-Proskauer: negative
- Citrate: negative
- Shigellosis is a notifiable disease in the U.S.; local public health laboratories may perform additional tests for epidemiologic purposes, including Shigella serotyping and antimicrobial susceptibility testing to follow resistance patterns
Case reports
- 2 year old girl with Shigella dysenteriae type 1 and HUS (J Med Microbiol 2005;54:997)
- 29 year old man with Shigella sonnei bacteremia (Praxis 2014;103:245)
- 40 year old man with reactive arthritis (Oxf Med Case Reports 2017;2017:omx070)
- 45 year old man with shigellosis associated encephalopathy (BMJ Case Rep 2018;2018:bcr2017222372)
- Shigella sonnei outbreak involving 158 cases likely caused by person to person contact (Am J Public Health 2020;110:842)
Treatment
- Rehydration is effective in shigellosis where stool volume is relatively low
- Oral: low cost, easy to administer
- IV: can be used if patient is vomiting or severely dehydrated
- Antibiotic therapy in patients that are severely ill
- Controversial if antibiotics should be used in mild cases who usually recover without antibiotics in 5 - 7 days (CDC: Shigella [Accessed 18 April 2022])
- Shortens disease course and reduces time frame that organisms are shed
- Always refer to local antibiogram to determine appropriate empiric antibiotics
- Azithromycin
- First choice oral therapy for children
- Most clinical laboratories do not test azithromycin susceptibility
- Ceftriaxone
- First choice parenteral therapy for children
- For suspected / confirmed invasive disease
- Achieves high concentrations in serum and stool (Ann Intern Med 1997;126:697)
- Ciprofloxacin
- Antimicrobial resistance is increasing
- Achieves high concentrations in serum and stool (Ann Intern Med 1997;126:697)
- Alternative therapies: trimethoprim sulfamethoxazole or ampicillin, if susceptible
- Antidiarrheal medication is contraindicated (StatPearls: Shigella [Accessed 14 March 2022])
- E.g., loperamide, paregoric and diphenoxylate
- Delays clearance of organisms
- Can prolong / worsen symptoms
- Antimicrobial treatment with ciprofloxacin and trimethoprim sulfamethoxazole may increase Stx production (Antimicrob Agents Chemother 2010;54:3790)
- Development of HUS can be characterized by various symptoms that may be treated with supportive therapy (e.g., care for anemia, thrombocytopenia, fluid and electrolyte disturbances, acute kidney injury and hypertension)
Clinical images
Gross description
- Indistinguishable from other causes of ulcerative colitis
- Acute onset of rectosigmoidal lesions (Baron: Medical Microbiology, 4th Edition, 1996):
- Erythema
- Edema
- Focal hemorrhage
- Adherent layers of purulent exudate
- Biopsy examination (Baron: Medical Microbiology, 4th Edition, 1996):
- Edematous
- Capillary congestion
- Focal hemorrhage
- Crypt hyperplasia
- Goblet cell depletion
- Mononuclear and polymorphonuclear cell infiltration
- Shedding of epithelial cells and erythrocytes
- Microulcerations
Molecular / cytogenetics description
- 16S rRNA gene sequencing will not differentiate Shigella spp. from E. coli due to > 99% sequence similarity (New Microbes New Infect 2017;21:58)
- Molecular assays targeting virulence genes are successful for detecting Shigella / enteroinvasive E. coli and serotypes
- Genes: ipaH, ipaB, ipaC, inv, ial
- Primarily for epidemiology purposes rather than diagnostics
- E.g., BioFire FilmArray Gastrointestinal Panel uses gene targets to differentiate Shigella from E. coli, where Shigella is positive for ipaH and stx1
- stx1 / stx2, can indicate Shiga-like toxin producing E. coli (STEC) or Shigella, this marker cannot distinguish alone
- ipaH, invasion plasmid antigen detected in Shigella and enteroinvasive E. coli (EIEC), this marker alone cannot distinguish
Differential diagnosis
- Invasive diarrheal disease similar to that caused by Shigella can be differentiated by symptomatic multiplex molecular tests and the following characteristics:
- Enteroinvasive E. coli (EIEC):
- Also encodes for genes that allow for invasion of enteric epithelial cells
- Most E. coli isolates can be differentiated from Shigella based on their motility and ability to ferment lactose
- Shiga toxin producing E. coli (STEC):
- Also encodes for Shiga toxin
- E. coli O157:H7 can often be identified on Sorbitol MacConkey (SMAC) agar as a nonsorbitol fermenter (J Clin Microbiol 1986;23:869)
- Salmonella:
- Hydrogen sulfide production on TSI slant or XLD agar
- May also be recovered for other systemic sites
- Campylobacter jejuni:
- Growth at 42 °C in microaerophilic conditions
- May also be recovered for other systemic sites
- Yersinia enterocolitica:
- Recovery and characteristic bullseye colony appearance with red center and pale border on the Yersinia selective agar cefsulodin irgasan novobiocin (CIN) agar (BD)
- May also be recovered for other systemic sites
- Entamoeba histolytica:
- Can be identified using a stool ova and parasite exam
- Clostridioides difficile:
- Strict anaerobe that can be identified through detection of C. difficile toxins A and B
- Enteroinvasive E. coli (EIEC):
- Noninfectious diseases with chronic diarrhea, including lactose intolerance, celiac disease, irritable bowel syndrome and ulcerative colitis, will not be associated with positive microbiologic findings
Additional references
- Centers for Disease Control and Prevention: Shigella - Shigellosis [Accessed 16 March 2022], Centers for Disease Control and Prevention: National Notifiable Diseases Surveillance System [Accessed 16 March 2022], Centers for Disease Control and Prevention: National Antimicrobial Resistance Monitoring System for Enteric Bacteria [Accessed 16 March 2022], UpToDate: Treatment and Prognosis of Shiga Toxin-Producing Escherichia coli (STEC) Hemolytic Uremic Syndrome (HUS) in Children [Accessed 16 March 2022]
Board review style question #1
A nonlactose fermenting, nonmotile gram negative rod was isolated from the stool culture of a 3 year old boy currently experiencing low volumes of bloody diarrhea, now several days after fever and diarrhea presented. The organism colony was red on XLD agar and MALDI TOF MS identified the organism as E. coli. What is the organism?
- E. coli
- Salmonella
- Shigella
- Yersinia
Board review style answer #1
C. Shigella. The observation of red colonies on XLD agar or xylose lysine deoxycholate agar are suggestive of an enteric organism that can grow in the presence of deoxycholate (inhibits gram positive organisms) and cannot ferment xylose. Most enteric organisms can ferment xylose but Shigella cannot. Another organism that may appear red on XLD agar is nonhydrogen sulfide producing Salmonella, due to lysine decarboxylation that alkalinizes the media. E. coli can be nonlactose fermenting and nonmotile in some cases, which may align with the organism identification given by MALDI TOF MS; however, E. coli is ruled out due to appearance on XLD agar (E. coli colonies appear yellow due to fermentation of excess lactose and sucrose in the agar). It is important to remember that MALDI TOF MS is unable to discriminate between Shigella and E. coli. These colony characteristics and biochemicals, along with the child's age and clinical picture, support a diagnosis of shigellosis.
Comment Here
Reference: Shigella
Comment Here
Reference: Shigella
Board review style question #2
A 27 year old man presents to primary care with fever, chills, abdominal pain, vomiting and several loose dark colored stools. Lab results show the patient was thrombocytopenic with low hemoglobin levels, elevated lactate dehydrogenase (LDH) and elevated creatinine. Which would be the most appropriate treatment?
- Antidiarrheal medication
- Ciprofloxacin
- Intravenous rehydration
- Trimethoprim sulfamethoxazole
Board review style answer #2
C. Intravenous rehydration. This patient presented with clinical labs indicative of hemolytic uremic syndrome (HUS), characterized by hemolytic anemia, acute kidney failure and low platelet counts. Rehydration for diarrheal illness and supportive therapy for anemia, thrombocytopenia and renal dysfunction are recommended. Intravenous rehydration may be optimal compared with oral rehydration when a patient is vomiting or severely dehydrated. While the cause of loose stools had not yet been identified, the stx genes have been observed in Shigella dysenteriae and enterohemorrhagic E. coli and less commonly in S. sonnei. Some antimicrobials, including ciprofloxacin and trimethoprim sulfamethoxazole, can increase the production of stx genes or trigger a bacteriophage to enter a lytic phase, which may transfer stx genes to nontoxigenic bacterium in the gut. In order to prevent HUS or an increase in symptom severity, treatment with ciprofloxacin is not recommended. This question is based loosely on the case study of a 27 year old man with S. sonnei and HUS (IDCases 2017;8:6).
Comment Here
Reference: Shigella
Comment Here
Reference: Shigella