Table of Contents
Definition / general | Essential features | Epidemiology | Sites | Pathophysiology | Clinical features | Laboratory | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Negative stains | Molecular / cytogenetics description | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Amerson-Brown M, Leal SM. Serratia species. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/microbiologyserratiaspecies.html. Accessed December 26th, 2024.
Definition / general
- Gram negative, rod shaped bacteria
- Taxonomy:
- Kingdom: bacteria
- Subkingdom: Negibacteria
- Phylum: Proteobacteria
- Class: Gammaproteobacteria
- Order: Enterobacterales
- Family: Enterobacteriaceae
- Genus: Serratia
- 19 species
- S. marcescens (primary clinical pathogen)
- S. liquefaciens, S. rubidaea, S. plymuthica, S. odorifera, S. ficaria (associated with clinical infection)
- Reference: ASM Press: Approved Lists of Bacterial Names [Accessed 16 February 2022]
Essential features
- Gram negative rod, oxidase negative, indole negative, lactose nonfermenter
- Environmental organism found in water, soil and certain plants
- Opportunistic pathogen infections in neonates and immunocompromised persons
- All body sites
- Nosocomial outbreaks and sporadic infections
- Multiple mechanisms of intrinsic and acquired antimicrobial resistance
Epidemiology
- Opportunistic infections and nosocomial infections in immunocompromised persons
- Outbreaks: neonates / pediatrics > adults
- Outbreaks linked to poor hand hygiene, contaminated medical devices, disinfectants and antiseptics (J Hosp Infect 1997;36:95)
Sites
- Colonizes respiratory tract and gastrointestinal tract
- Lung / lower respiratory tract / ventilator associated pneumonia (VAP)
- Urinary tract / catheter associated urinary tract infections (CAUTIs)
- Surgical site / wounds
- Bloodstream infections / central line associated infections (CLABSIs)
- Endocarditis / left sided endocarditis
- Hospital acquired eye infection, particularly in neonates and pediatric population
Pathophysiology
- Usually acquired through exogenous sources: water, soil, plant, hospital environment
- Pili enhance adherence to epithelial cells of the respiratory tract, gastrointestinal tract and urogenital tract
- Virulence factors include protease activity, hemolytic activity (ShlA and ShlB), biofilm formation, motility, nuclease, lipase, lipopolysaccharide (LPS) and cell surface surfactant (serrawettin) that aids in colonization and invasion (Surg Infect (Larchmt) 2020;21:608, Microbiol Immunol 2005;49:303, J Med Microbiol 1997;46:903, Curr Protein Pept Sci 2005;6:313)
Clinical features
- S. marcescens strains have caused hospital outbreaks, especially among inpatients with extended hospitalization, prolonged antibiotic use and indwelling catheters
- Most commonly causes bloodstream infection, pneumonia, urinary tract infection, etc.
Laboratory
- Aerobic growth 37 °C
- Growth on routine culture media
- Blood agar (nonhemolytic, gray colonies)
- Chocolate agar (large, gray)
- MacConkey agar (lactose nonfermenter)
- Environmental S. marcescens strains are often red due to the production of prodigiosin pigment (Mol Microbiol 2000;36:539)
- Prodigiosin gives growth benefits in the environment
- Protection from physical and chemical stress and growth advantage at ambient temperatures (Arch Microbiol 2018;200:989)
- Most hospital acquired strains are nonpigmented (J Med Microbiol 1997;46:903)
- Nonpigmented due to growth conditions, oxygen requirements and body temperature / incubation temperature 37 °C (FEMS Immunol Med Microbiol 2000;28:143)
- Oxidase negative
- Indole negative
- Motile
- DNase positive, gelatinase positive, lipase positive
- Automated identification instruments, matrix assisted laser desorption / ionization time of flight (MALDI-TOF) mass spectrometry, sequencing
Case reports
- 1 day old girl with neonatal infective endocarditis (Arch Clin Cases 2021;7:40)
- 5 month old boy with biliary atresia received a split liver transplant that was complicated by recurrent portal vein thrombosis (Pediatr Transplant 2018;22:e13180)
- 45 and 50 year old men with panopthalmitis (Am J Ophthalmol Case Rep 2019;16:100531)
- 89 year old man with pseudohemoptysis (Med J Armed Forces India 2018;74:383)
Treatment
- S. marcescens is intrinsically resistant to penicillin, first and second generation cephalosporins, macrolides, tetracycline, nitrofurantoin and colistin
- Mechanism of drug resistance: to fluoroquinolones (gyrA mutations), to aminoglycosides (plasmid mediated aminoglycoside modifying enzymes and 16S methyltransferase enzymes) (Ann Lab Med 2015;35:172)
- Multidrug resistance mechanisms: extended spectrum beta lactamases (ESBLs), ampC beta lactamase, carbapenemases (Eur Rev Med Pharmacol Sci 2017;21:1690, Nat Rev Microbiol 2015;13:42)
Clinical images
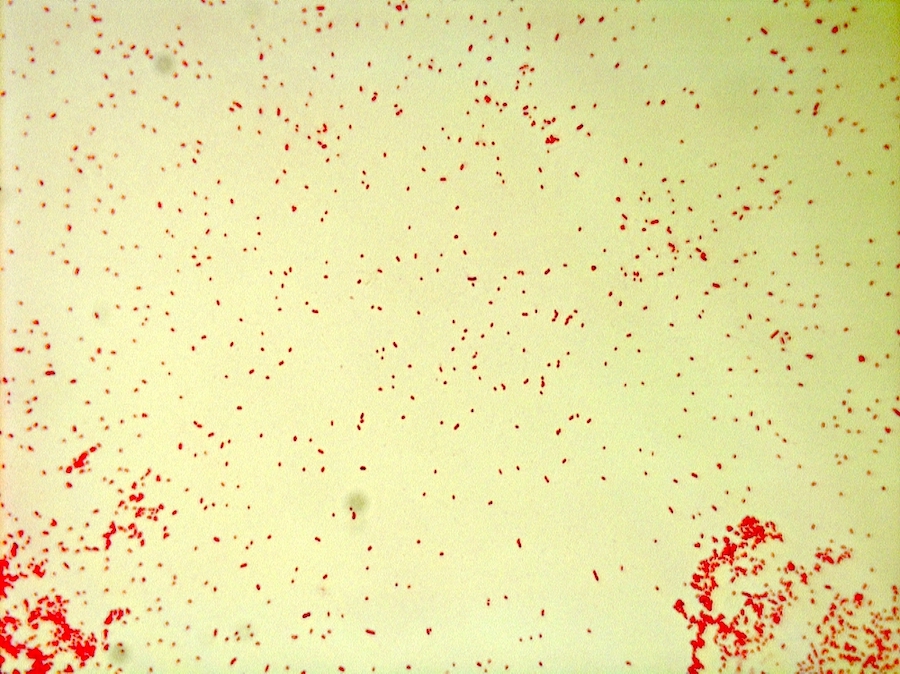
Microscopic (histologic) description
- S. marcescens grows as small, pleomorphic, gram negative rods from solid culture media
Microscopic (histologic) images
Negative stains
- Gram stain, Kinyoun / Ziehl-Neelsen, modified AFB stain, Calcofluor white stain
Molecular / cytogenetics description
- S. marcescens is identified by some rapid molecular blood culture identification systems
- 16S gene sequencing
- Reference: Clin Microbiol Rev 2017;31:e00024
Differential diagnosis
- Other Serratia species:
- S. liquefaciens, S. odorifera, S. plymuthica, S. rubidaea, S. fonticola, S. ficaria, S. entomophila
- Other Enterobacterales:
- Distinguish with MALDI-TOF mass spectrometry, automated identification systems or sequence based identification
- Other oxidase negative, lactose nonfermenters:
- E.g., Stenotrophomonas maltophilia and Acinetobacter species
- Differentiate using automated identification systems or MALDI-TOF mass spectrometry
- Pigmentation can aid differentiation
Additional references
Board review style question #1
A urine culture from a 60 year old kidney transplant patient is growing > 100,000 CFU/mL of a gram negative rod, forming clear colonies on MacConkey agar. The organism is motile and tests negative using oxidase and indole biochemical tests. What is the most likely organism?
- Acinetobacter baumanii
- Escherichia coli
- Pseudomonas aeruginosa
- Serratia marcescens
Board review style answer #1
D. Serratia marcescens. While all the organisms are gram negative rods, S. marcescens is the only lactose nonfermenter that is motile, oxidase negative and indole negative. A. baumanii is nonmotile. E. coli is an indole positive, lactose fermenting organism. P. aeruginosa is oxidase positive.
Comment Here
Reference: Serratia species
Comment Here
Reference: Serratia species
Board review style question #2
Over the course of 3 months, 8 patients in the NICU developed invasive infections with S. marcescens. Initial symptoms of infections were noted in all the patients at least 72 hours postadmission. The isolates showed slight differences in MIC values from in vitro drug susceptibility testing and none of the isolates produced a pigment. Should infection control be notified to perform an outbreak investigation?
- No, the lack of pigmentation indicates these isolates were not acquired in the hospital setting
- No, S. marcescens does not cause outbreaks
- Yes, all lactose nonfermenting, gram negative organisms isolated from the NICU should be reported and investigated regardless of the genus and species
- Yes, the time frame, setting, organism and lack of pigmentation indicates these isolates were likely acquired in a healthcare setting
Board review style answer #2
D. Yes, the time frame, setting, organism and lack of pigmentation indicate these isolates were likely acquired in the hospital setting. Outbreaks with S. marcescens can be slow, linger over the course of months and are more common in NICU settings. The lack of pigmentation of the organism suggests that it was likely acquired in a healthcare setting and not from an external environmental source. Whole genome sequencing should be performed to determine if the organisms are a clonal strain being spread throughout the unit. Surveillance cultures for colonization of S. marcescens would also be recommended for all patients in the unit. While it is important to monitor the prevalence of infections with all organisms in the microbiology lab, an individual outbreak investigation should be limited to organisms of the same genus and species.
Comment Here
Reference: Serratia species
Comment Here
Reference: Serratia species