Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2 | Board review style question #3 | Board review style answer #3Cite this page: Rohr BR, Hossler EW. Scabies (mite). PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skinnontumorscabies.html. Accessed December 26th, 2024.
Definition / general
- Scabies are 8 legged mites that infest the stratum corneum
- Cause intense pruritus accompanied by a variety of cutaneous findings; infestation may lead to secondary impetiginization and psychological sequelae
Essential features
- Obligate ectoparasite
- Burrows into the stratum corneum of acral and intertriginous sites
- Diagnosis is through visualization of burrows on clinical exam or through identification of mites, eggs or scybala on microscopy
Terminology
- Itch mite, Sarcoptes scabiei var. hominis
ICD coding
- ICD-10: B86 - scabies
Epidemiology
- Prevalence: ~200 million people worldwide (J Am Acad Dermatol 2020;82:533, PLoS Negl Trop Dis 2018;12:e0006549)
- Low and middle income tropical countries (J Am Acad Dermatol 2020;82:533)
- Increased risk with population crowding: homeless, children, displaced groups (J Am Acad Dermatol 2020;82:533)
- Crusted scabies in elderly and immunosuppressed
- Sexual transmission
Sites
- Finger and toe webs
- Volar surfaces of wrists
- Intertriginous areas
- Areas under occlusion (i.e. waistbands)
- Areola (females), genitalia (males)
- Spares head (high sebaceous areas) in adults, immune competent (Dermatol Ther 2020;33:e13746)
- May affect head in infants, immunocompromised
Pathophysiology
- Skin to skin transmission or fomites
- Classic scabies: mite load 5 - 15 mites (J Am Acad Dermatol 2020;82:533)
- Th1 / Th2 immune response
- Crusted scabies: 100s - 1,000s of mites
- Th2 response
- Mites burrow into stratum corneum
Etiology
- Sarcoptes scabiei var. hominis
- Obligate ectoparasite
- Burrows into stratum corneum
- 0.5 - 5 mm per day (Dermatol Ther 2020;33:e13746)
- Life cycle 14 - 21 days (Dermatol Ther 2020;33:e13746)
- Female mite lives 4 - 6 weeks, lays 40 - 50 eggs (Dermatol Ther 2020;33:e13746)
- Mites survive 24 - 36 hours off host at room temperature (Dermatol Ther 2020;33:e13746)
- Longer possible if colder temperature
- Transfer via skin to skin
- Minimal transfer time: 5 minutes (Dermatol Ther 2020;33:e13746)
- Fomite transfer possible
Clinical features
- Initial symptom onset 4 - 6 weeks post initial infection (J Am Acad Dermatol 2020;82:533)
- Subsequent infection symptom onset within days (J Am Acad Dermatol 2020;82:533)
- Classic presentation:
- Extreme pruritus, nighttime worsening
- Burrows
- Small white serpiginous scaly linear papules on finger and toe webs
- Erythematous scaly papules on intertriginous, areolar and genital skin and areas under occlusion
- Excoriations common
- Genital / scrotal erythematous nodules (IDCases 2020;22:e00947)
- With or without pruritus in infants, immunosuppressed and patients on topical steroids (J Am Acad Dermatol 2020;82:533)
- With or without secondary impetiginization or autoeczematization
- Crusted scabies
- Yellow to white hyperkeratotic plaques
- With or without postscabetic pruritus for 4+ weeks posttreatment
- Use topical corticosteroids, education
Diagnosis
- Mineral oil scraping (low sensitivity)
- Clinical exam (burrows on finger and toe webs, genital nodules)
- Dermoscopy (delta wing jet sign) (Tidsskr Nor Laegeforen 2020;140:1)
- Other noninvasive techniques: videodermoscopy, confocal microscopy, optical coherence tomography (J Am Acad Dermatol 2020;82:533)
- Skin biopsy (shave or punch)
Laboratory
- Not required for diagnosis
- Eosinophilia
- Elevated IgE (Dermatol Ther 2020;33:e13746)
Prognostic factors
- Favorable with adequate treatment
- High recurrence risk:
- If close contacts not treated
- Resistance to permethrin
- Oral ivermectin
- New agents in development (Dermatol Ther 2020;33:e13746, Acta Derm Venereol 2020;100:adv00112)
Case reports
- 10 month old with scabies incognito mimicking urticaria pigmentosa (Pediatr Dermatol 2002;19:409)
- 5 year old with bullous scabies (J Pediatr 2016;179:270)
- 26 year old man with scabies presenting as chronic urticaria (Mil Med 2020;185:e1854)
- 55 year old man with history of HIV and injection drug use with erthrodermic presentation of crusted scabies (Infez Med 2019;27:332)
- 76 year old man with scabies mimicking bullous pemphigoid (Clin Cosmet Investig Dermatol 2017;10:317)
Treatment
- Permethrin 5% cream
- First line
- Close contacts treated simultaneously
- FDA approved for > 2 months age
- Oral ivermectin
- Less commonly used (J Am Acad Dermatol 2020;82:533):
- Benzyl benoate 10 - 25%
- Precipitated sulfur 2 - 10%
- Can be used in infancy and pregnancy (Dermatol Ther 2020;33:e13746)
- Crotamiton 10%
- Malathion 0.5%
- Lindane 1%
Clinical images
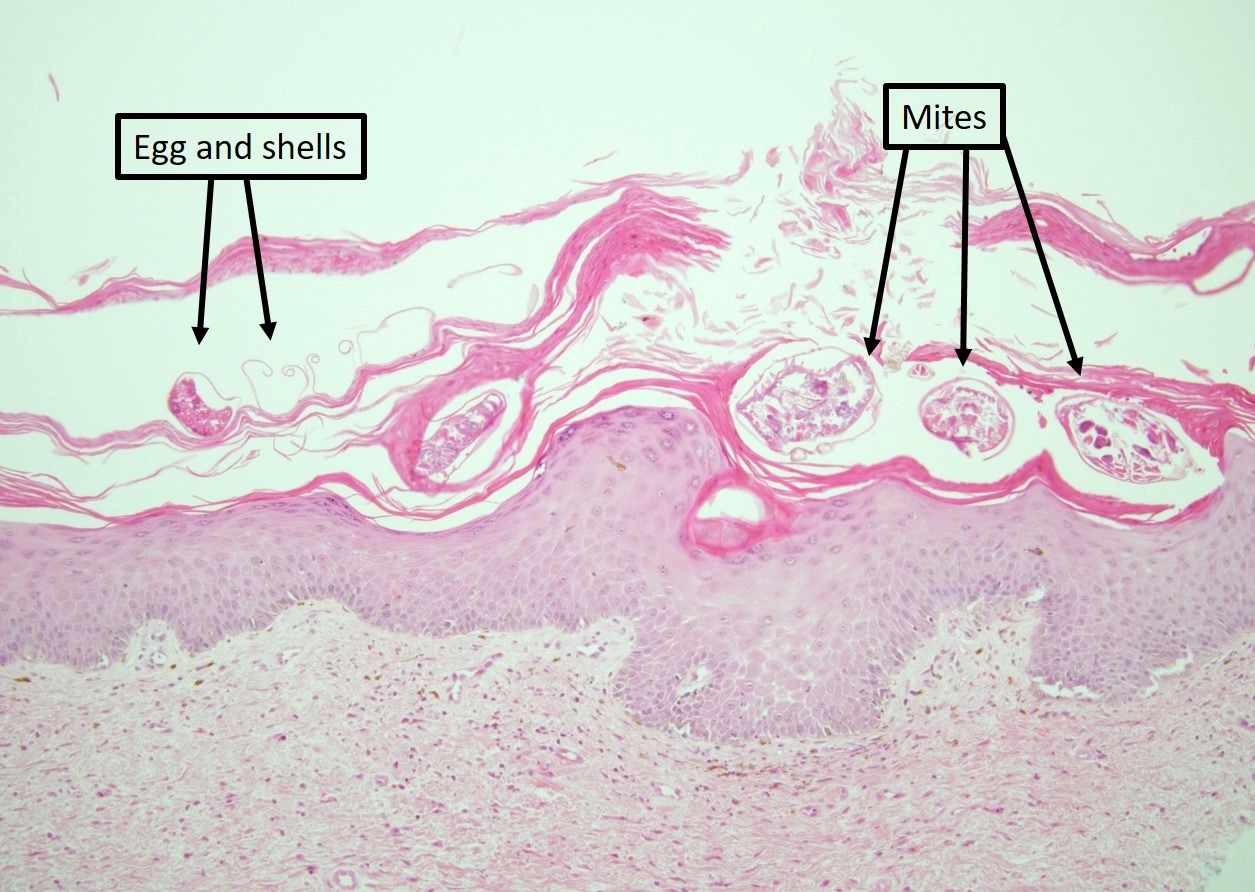
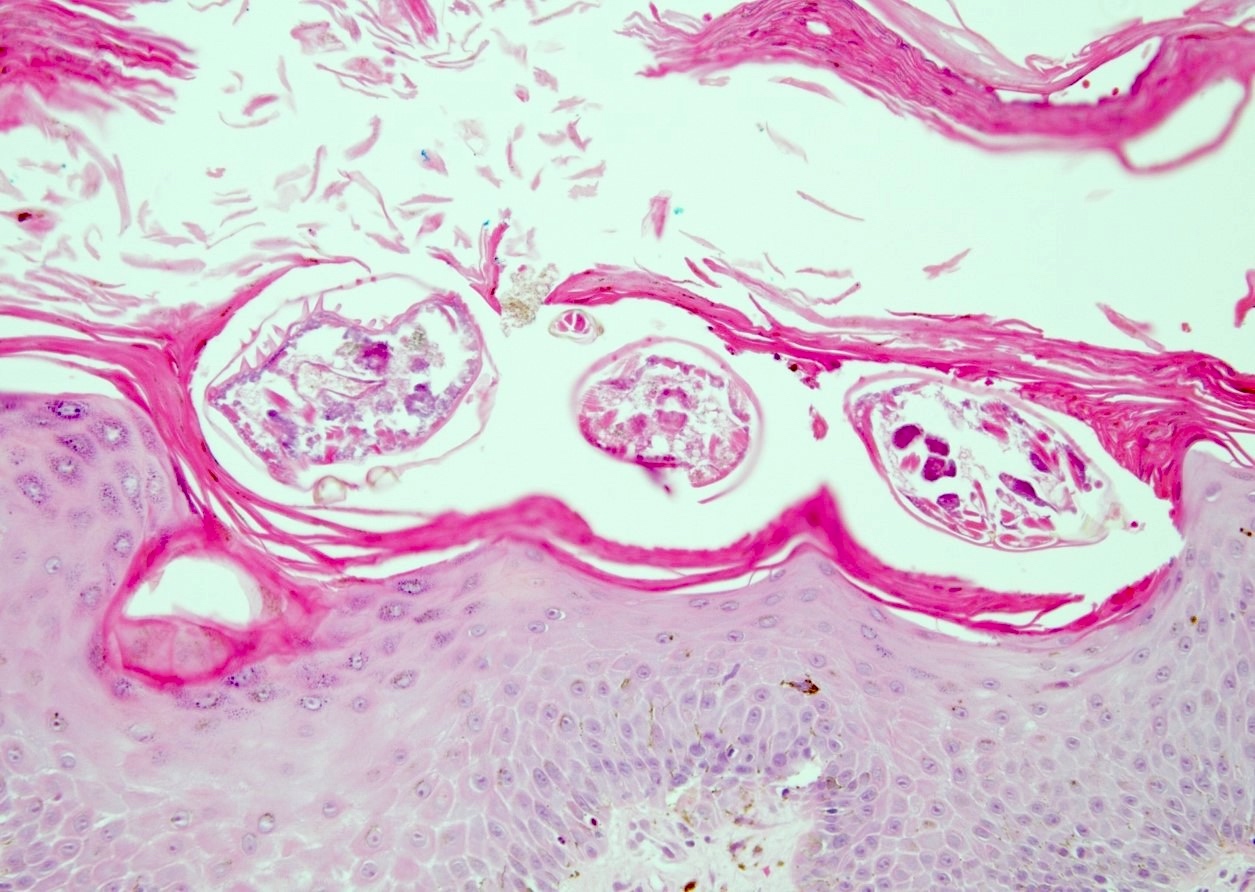
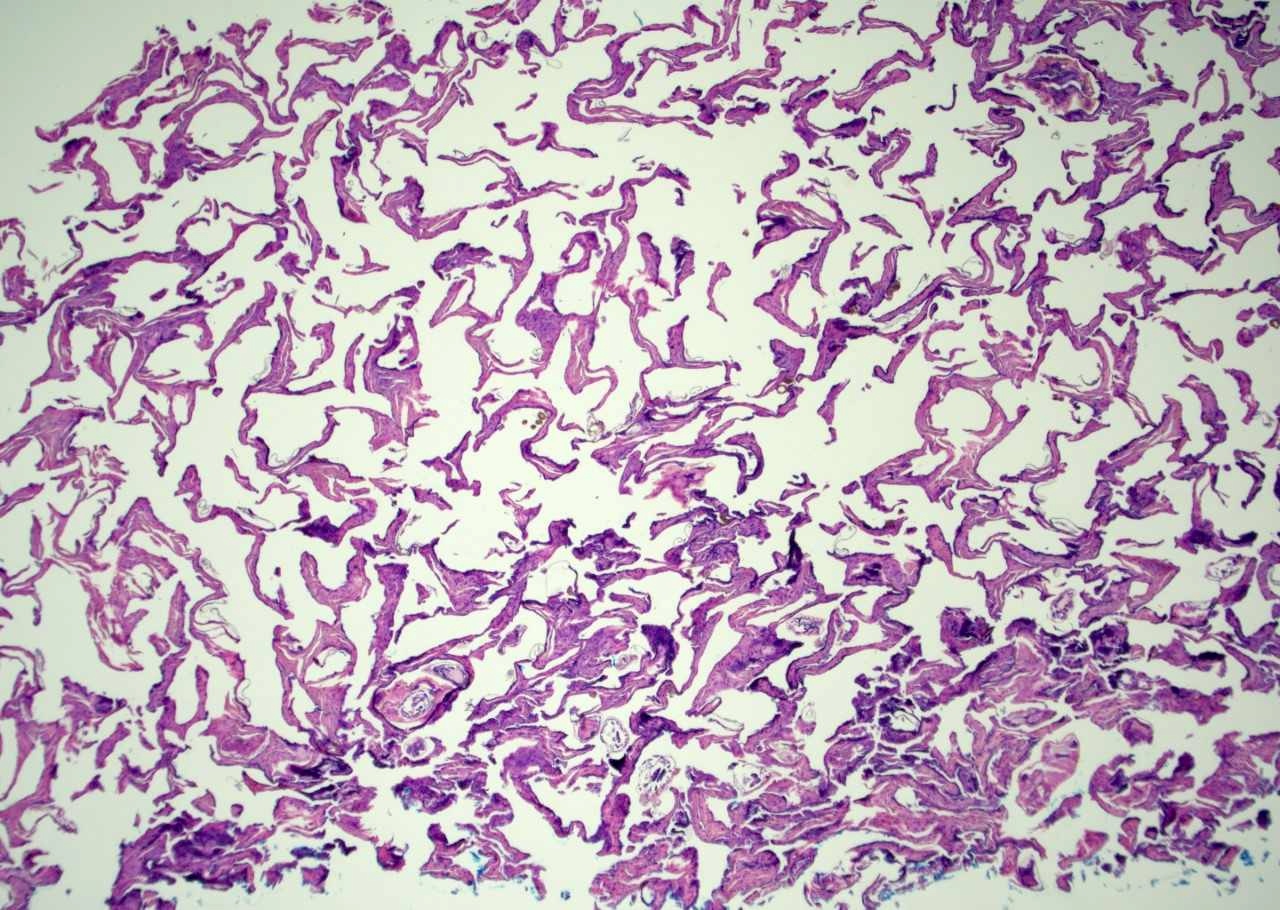
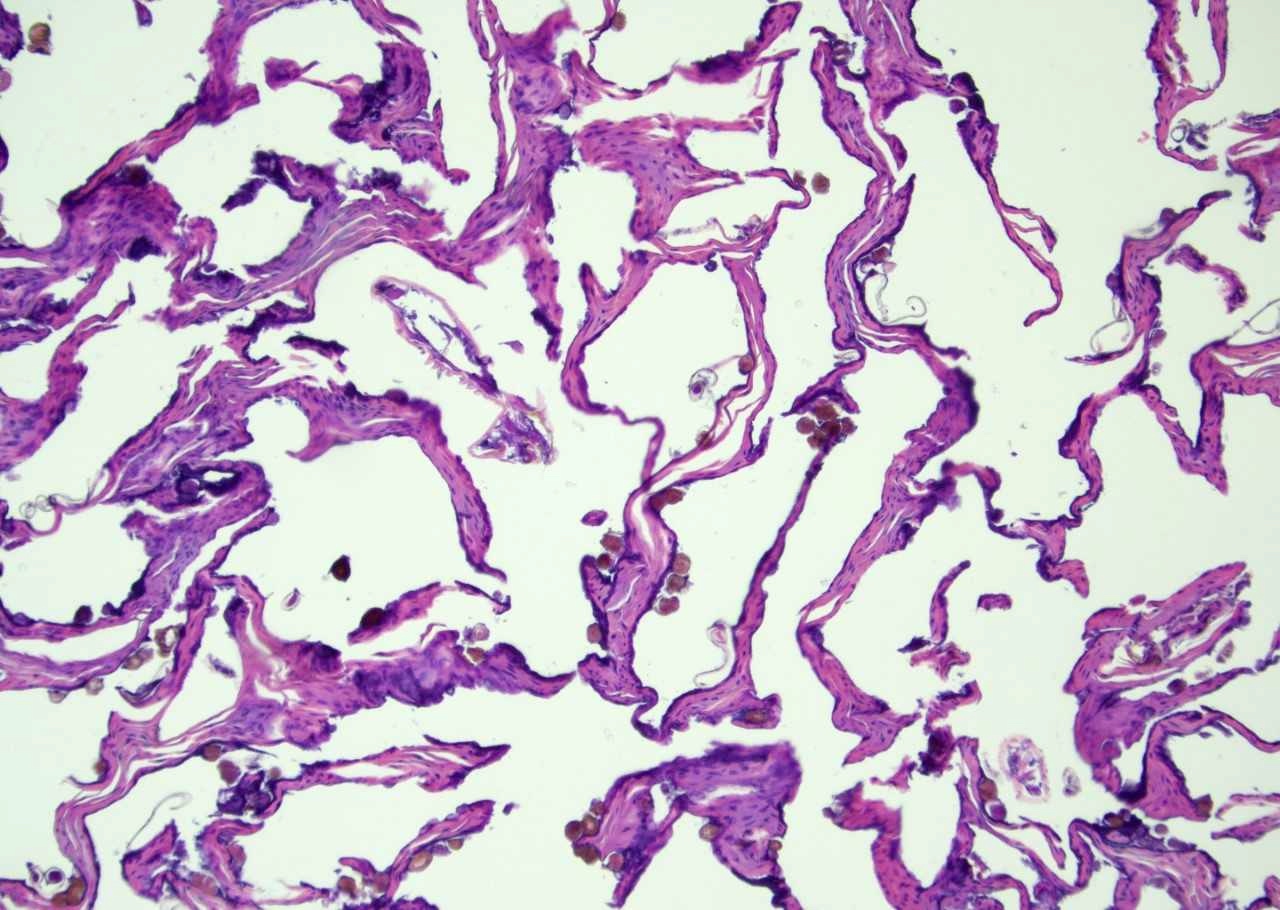
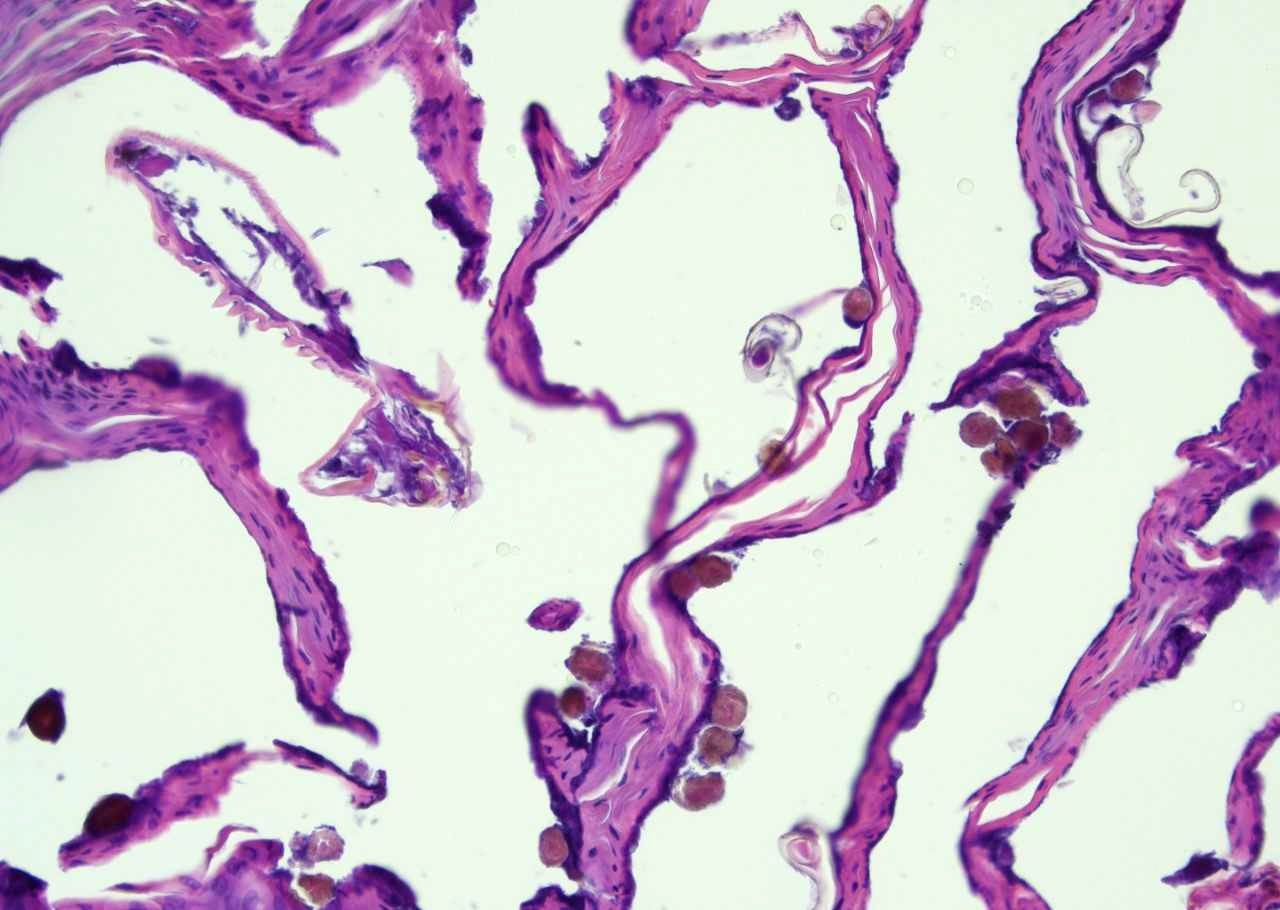
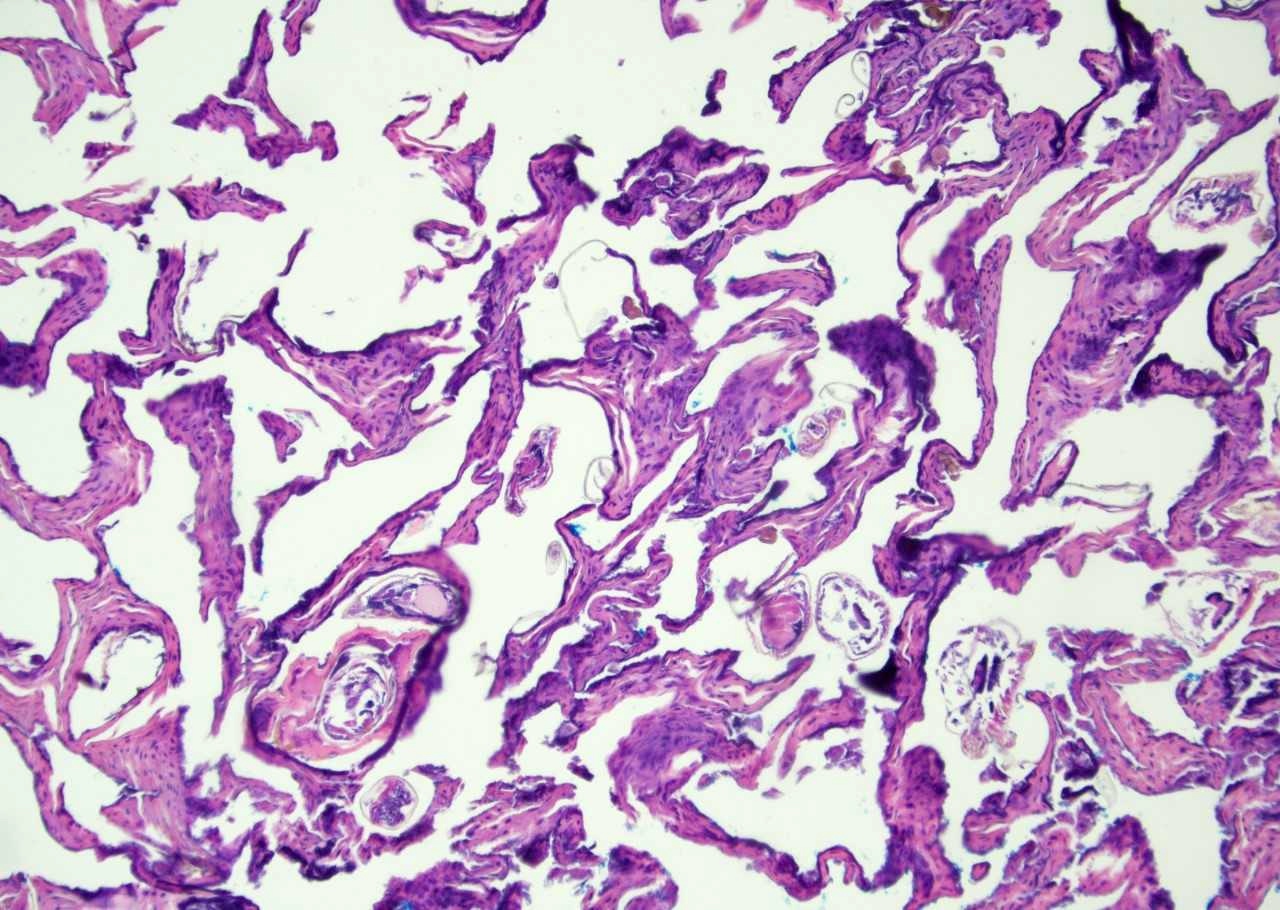
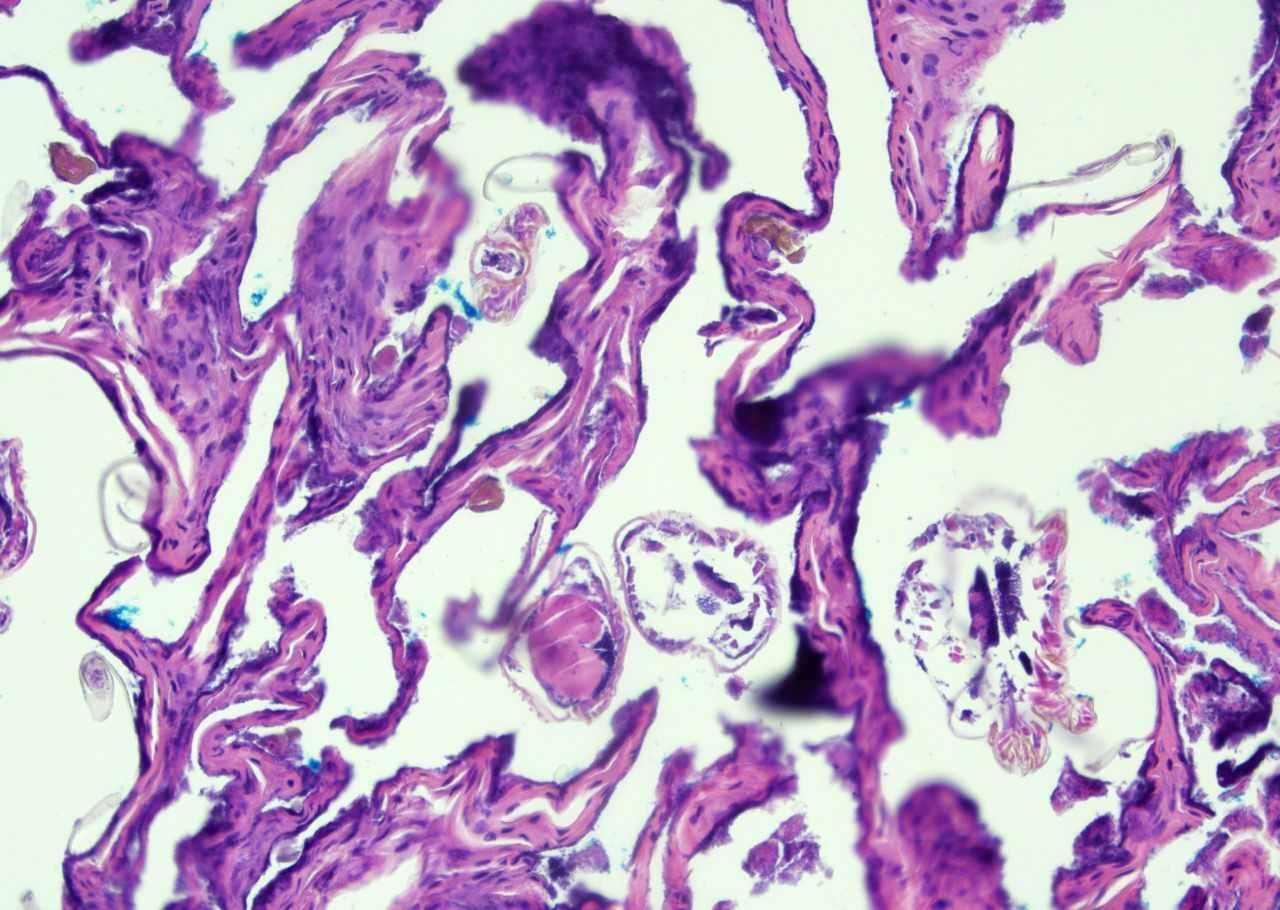
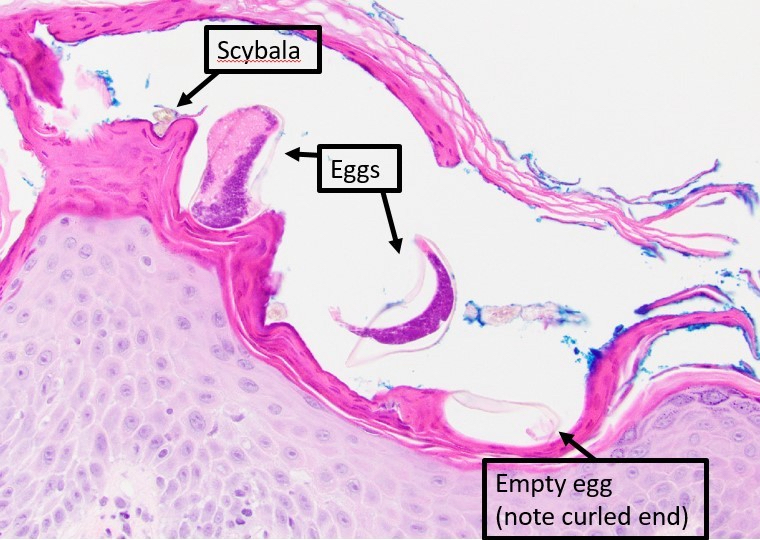
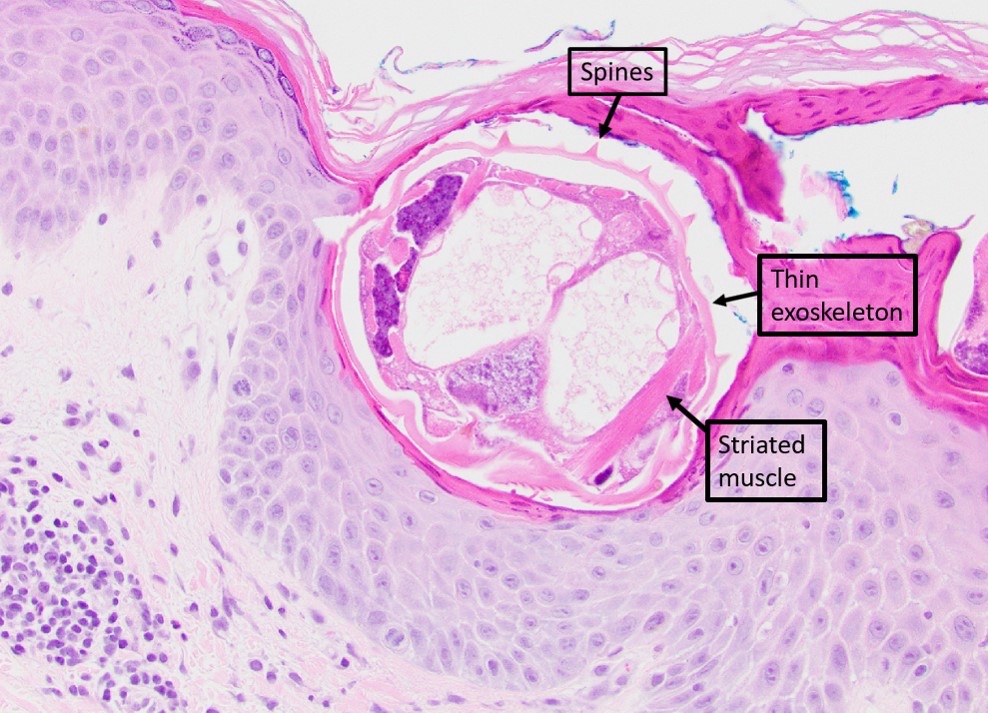
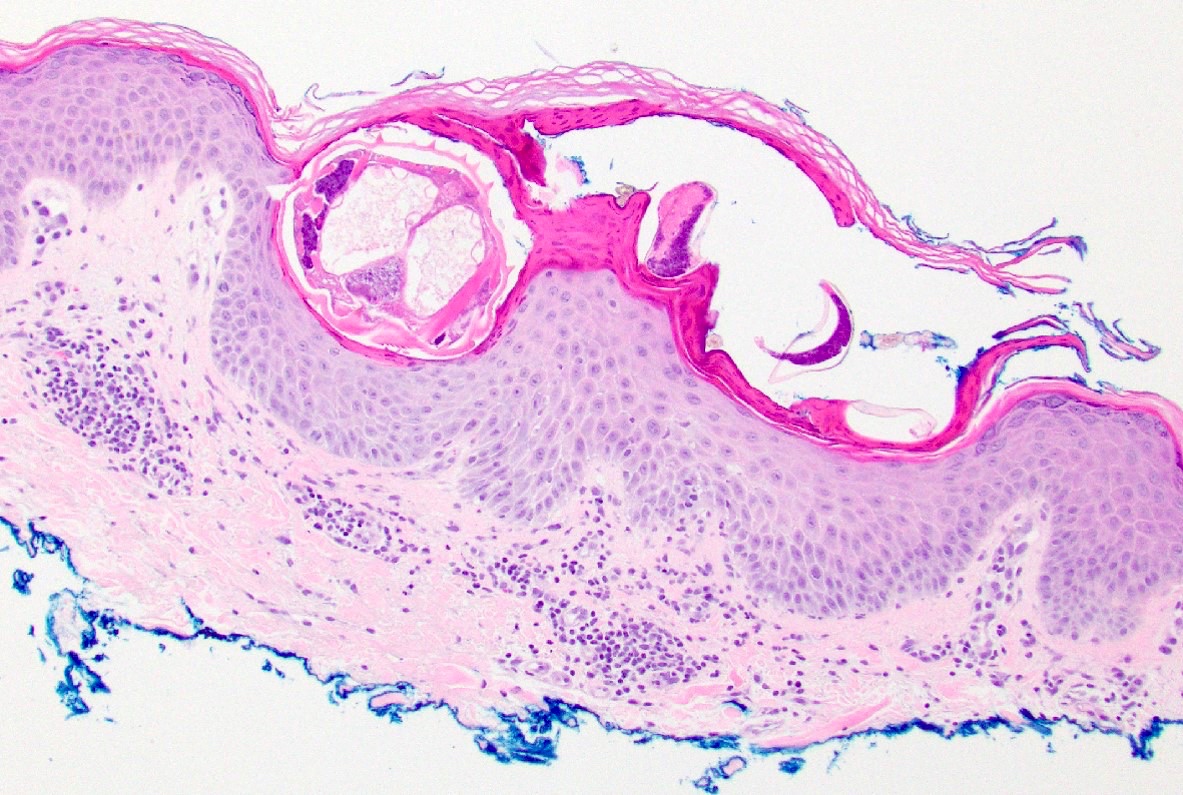
Microscopic (histologic) description
- Classic scabies
- Identification of intracorneal mites, ova or scybala (feces)
- Mites: 0.2 - 0.4 mm length (Dermatol Ther 2020;33:e13746, Clin Microbiol Rev 2014;27:48)
- Oval bodies with rudimentary legs (Clin Microbiol Rev 2014;27:48)
- Exoskeleton with striations, dorsal spines (Clin Microbiol Rev 2014;27:48)
- Long hair-like (setae) on hind legs (Clin Microbiol Rev 2014;27:48)
- Oval eggs: 0.1 - 0.2 mm (Clin Microbiol Rev 2014;27:48)
- Superficial perivascular lymphoeosinophilic infiltrate with histiocytes and possible neutrophils
- Possible epidermal spongiosis with or without features of excoriation (ulceration, erosion) and crust
- CD30+ infiltrate possible
- Identification of intracorneal mites, ova or scybala (feces)
- Crusted scabies
- Hyperkeratosis with numerous mites, eggs and scybala
- Nodular scabies
- Epidermal acanthosis
- Denser dermal infiltrate: lymphocytes with or without follicle centers, eosinophils, plasma cells (Indian J Dermatol Venereol Leprol 1997;63:170)
- Vasculitis possible
- Bullous scabies
- Subepidermal bulla with eosinophils
Microscopic (histologic) images
Contributed by Eric W. Hossler, M.D. and Bethany R. Rohr, M.D.
Virtual slides
Positive stains
- Not required for diagnosis
- CD30 positive infiltrate possible in nodular scabies (J Cutan Pathol 2008;35:1100)
Videos
Probe of scabies burrow under dermoscopy
Ask a dermatologist: how do I get rid of scabies?
Sarcoptes scabiei var. hominis
Sample pathology report
- Skin, anatomic location, (punch or shave) biopsy:
- Scabies
Differential diagnosis
- Classic scabies (J Am Acad Dermatol 2020;82:533):
- Arthropod bites
- Folliculitis:
- Folliculocentric infiltrate of neutrophils with or without eosinophils and histiocytes
- Papular urticaria
- Prurigo nodularis:
- Irregular epidermal hyperplasia with hypergranulosis and vertically oriented papillary dermal fibrosis
- Delusional parasitosis:
- Diagnosis of exclusion
- Features of excoriation (erosion, ulceration) on histology
- Dermatitis (atopic, nummular, contact)
- Lice infestation:
- Localized to coarse hair bearing areas
- Urticarial stage of bullous pemphigoid:
- See direct immunofluorescence (DIF) findings below
- Dermatitis herpetiformis:
- Gluten sensitivity
- DIF with basement membrane zone and papillary dermal granular IgA
- Tunga penetrans:
- Flea (larger than mite)
- Embeds in stratum corneum of sole of foot / between toes most commonly
- Demodex mites:
- Commensal mite found in folliculosebaceous units
- Head / neck location most common
- No spines
- Lymphomatoid papulosis:
- CD30+ infiltrate
- Lacks diagnostic mites, ova or scybala
- Crusted scabies (J Am Acad Dermatol 2020;82:533):
- Psoriasis:
- Regular acanthosis without significant spongiosis or eosinophils
- Pityriasis rubra pilaris:
- Regular acanthosis without significant spongiosis or eosinophils
- Palmoplantar keratoderma
- Seborrheic dermatitis:
- Seborrheic distribution, parakeratotic shouldering of follicular ostia
- Erythrodermic mycosis fungoides / Sézary syndrome
- Atopic or contact dermatitis
- Darier disease:
- Seborrheic distribution
- Acantholysis with dyskeratosis on histology
- Psoriasis:
- Infantile scabies (J Am Acad Dermatol 2020;82:533):
- Arthropod bites
- Papular urticaria
- Atopic dermatitis
- Infantile acropustulosis
- Langerhans cell histiocytosis:
- CD1a+ collections of epitheliotropic Langerhans cells
- Bullous scabies
- Bullous arthropod bites
- Bullous impetigo:
- Presence of bacterial cocci
- Bullous pemphigoid:
- DIF with linear IgG and C3
- Serum enzyme linked immunosorbent assay (ELISA)
- Pemphigus vulgaris:
- Suprabasal layer acantholysis with extension down follicular epithelium
- DIF with net-like IgG
- Incontinentia pigmenti (inflammatory stage):
- Dyskeratosis present
Additional references
Board review style question #1
A biopsy from a patient with crusted scabies is likely to reveal which findings compared with typical scabies?
- Few mites
- Few ova
- Many ova but few mites
- Mites present in the upper dermis
- Numerous mites, ova and scybala
Board review style answer #1
E. Numerous mites, ova and scybala. Crusted scabies occurs in immunosuppressed patients and characteristically contains hyperkeratosis with numerous mites, ova and scybala. Scabies mites reside in the epidermis only.
Comment Here
Reference: Scabies (mite)
Comment Here
Reference: Scabies (mite)
Board review style question #2
Board review style answer #2
Board review style question #3
Scabies mites avoid which anatomic region, except in infants and immunosuppressed patients?
- Acral sites
- Genitals
- Head (face, scalp)
- Intertriginous areas
- Volar wrists
Board review style answer #3
C. Head (face, scalp); scabies typically avoid the face / scalp (highly sebaceous areas) in immunocompetent adults. The other listed sites are typical areas of involvement.
Comment Here
Reference: Scabies (mite)
Comment Here
Reference: Scabies (mite)