Table of Contents
Definition / general | Essential features | Epidemiology | Sites | Pathophysiology | Clinical features | Diagnosis | Laboratory | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Garrett EM. Neisseria meningitidis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/microbiologynmeningitidis.html. Accessed December 24th, 2024.
Definition / general
- Gram negative bacterium associated with invasive disease including meningitis and sepsis
Essential features
- Common mucosal colonizer but rarely can cause invasive meningococcal disease (IMD) including meningitis and bacteremia
- Polysaccharide capsule is necessary for invasive disease and contributes to immune evasion
- First line antibiotic therapy is penicillin but resistance can occur
Epidemiology
- Colonizes mucosal surfaces, especially oropharynx and nasopharynx (Carroll: Manual of Clinical Microbiology, 12th Edition, 2019)
- Colonization rates are highest among young adults (~16 - 23 years old)
- Only found in humans
- Invasive meningococcal disease occurs in < 1/100,000 in the U.S. but has a case fatality rate of nearly 15% (Clin Infect Dis 2018;66:1276)
- Risk factors for development of invasive disease include complement deficiencies, immunosuppression (e.g., eculizumab) and asplenia or functional asplenia
- Disruption of mucosa such as by concomitant viral infection or smoking may increase risk of disease
- Outbreaks of invasive disease are associated with transmission of certain serogroups (Methods Mol Biol 2012;799:1)
- Only 6 serogroups cause invasive meningococcal disease: A, B, C, W135, X, Y
- Serogroups B, C and Y are the most common in the U.S.
- Serogroup A is most common in sub-Saharan African countries (meningitis belt region), with attack rates that can exceed 1/1,000 (Ann Trop Med Parasitol 1997;91:777)
- Hyperinvasive lineages identified in several large outbreaks (Clin Infect Dis 2003;36:679)
Sites
- Invasive infection occurs most commonly as meningitis or bacteremia (meningococcemia)
- Rarely causes infection in other sites including pneumonia, septic arthritis, conjunctivitis
- Recent (~2015) spread of novel lineage associated with male urethritis in the U.S. and Europe (Proc Natl Acad Sci U S A 2017;114:4237)
Pathophysiology
- Person to person transmission likely by inhalation of respiratory droplets
- Type IV pili, outer membrane proteins (Opa, Opc, PorA, PorB) and lipooligosaccharide (LOS) mediate adhesion and contribute to colonization of epithelial surfaces (Clin Sci (Lond) 2010;118:547)
- Also mediate intracellular uptake and survival, allowing subepithelial spread and dissemination
- Most strains produce capsules, which are composed of variable polysaccharides that determine the serogroup
- Capsules aid in immune evasion, especially of the complement system (Front Cell Infect Microbiol 2022;12:1020201)
- Strains that do not produce capsules rarely cause disease
Clinical features
- Can present as meningitis with or without meningococcemia or as meningococcemia alone (Procop: Koneman’s Color Atlas and Textbook of Diagnostic Microbiology, 7th Edition, 2017)
- Meningicoccemia often occurs with petechial lesions starting on mucosal surface and spreading to trunk and limbs
- Can rapidly develop into septic shock, disseminated intravascular coagulation, myocarditis
- Highest mortality (~15%) associated with septicemia
- Seasonal, peaking in winter months
- Highest incidence < 1 year of age; second peak in adolescence (CDC: Meningococcal Disease Surveillance [Accessed 26 June 2023])
- Long term sequelae can include brain damage and deafness
Diagnosis
- Culture and Gram stain of the affected site (blood, cerebrospinal fluid [CSF], synovial fluid)
- Gram stain of CSF showing gram negative diplococci is sufficient for presumptive diagnosis of meningococcal meningitis
- Colonization can be identified by culture of a pharyngeal swab
- BioFire FilmArray Meningitis / Encephalitis multiplex PCR panel (BioMèrieux)
- Reference: Intern Med J 2018;48:1294
Laboratory
- Positive cultures should always be handled in a class II biological safety cabinet to avoid exposure and laboratory acquired infection
- Fastidious organism; avoid desiccation and limit transportation time of specimens to maximize recovery
- Culture (Carroll: Manual of Clinical Microbiology, 12th Edition, 2019)
- Can be recovered on sheep blood and chocolate agar grown at 35 °C with 3 - 7% carbon dioxide
- Does not grow on MacConkey agar
- Growth in blood culture media may be inhibited by sodium polyanethole sulfonate (SPS), a common media additive
- For nonsterile sources such as respiratory, can culture on selective media such as Thayer-Martin, New York City agar
- Identification
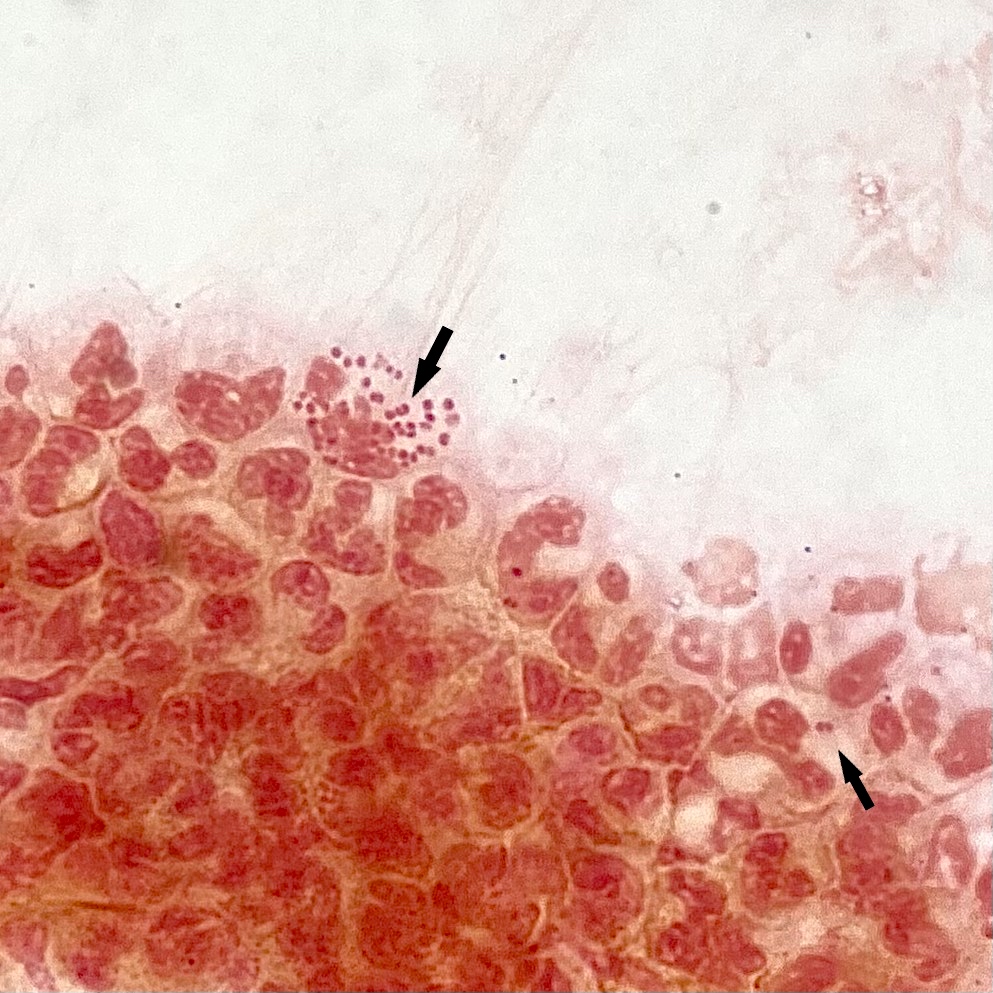
- Gram stain: gram negative diplococci, coffee bean appearance; may appear intracellular
- Colony morphology: smooth, gray, convex, nonhemolytic
- Oxidase test positive
- Identification of Neisseria species by matrix assisted laser desorption ionization time of flight (MALDI TOF) mass spectrometry should be confirmed by an additional identification method such as carbohydrate utilization test
- Carbohydrate utilization tests (e.g., CarboFerm Neisseria Kit, Hardy Diagnostics) assess differential ability to oxidize glucose, maltose, sucrose, lactose
- N. gonorrhea: glucose positive only
- N. meningitidis: glucose and maltose positive
- Serogrouping may be done by latex or slide agglutination
- Invasive meningococcal disease is a nationally reportable condition
Case reports
- 2 year old boy with meningococcal meningitis (World J Clin Cases 2019;7:636)
- 26 year old man with urethritis (Sex Transm Dis 2011;38:439)
- 58 year old smoking woman with community acquired pneumonia (Chest 2017;152:e95)
Treatment
- First line antibiotic therapy is penicillin G; susceptibility should be determined (CDC: Detection of Ciprofloxacin Resistant, β Lactamase Producing Neisseria meningitidis Serogroup Y Isolates [Accessed 11 May 2023])
- Resistance to penicillin is rare; can be due to altered penicillin binding protein 2 (PBP2) or beta lactamase production
- Also frequently susceptible to third generation cephalosporins (ceftriaxone), which can be used for empiric therapy until penicillin susceptibility is determined
- Ciprofloxacin or rifampin for penicillin allergic patients
- 5 meningococcal vaccines available in the U.S.
- 3 quadrivalent (serogroups A, C, W and Y) and 2 recombinant serogroup B
- Vaccination has significantly reduced invasive meningococcal disease in the U.S.
- Prophylactic antibiotic therapy recommended for people in close contact of infected patient within 7 days of symptom onset
Microscopic (histologic) description
- See Laboratory
Differential diagnosis
- Other causes of acute bacterial meningitis (Intern Med J 2018;48:1294):
- Streptococcus pneumoniae, Streptococcus agalactiae (group B):
- Gram positive cocci in pairs or chains
- Listeria monocytogenes:
- Short gram positive rods
- Most common in patients > 50 years old
- Haemophilus influenzae:
- Gram negative coccobacilli, not predominantly in pairs
- Does not grow on blood agar
- Streptococcus pneumoniae, Streptococcus agalactiae (group B):
- Other gram negative diplococci:
- Infrequent causes of acute bacterial meningitis; can be identified by MALDI TOF
- Moraxella catarrhalis
- Commensal Neisseria species
- Neisseria gonorrhea:
- Confirm identification by carbohydrate utilization test
Board review style question #1
A 19 year old man with functional asplenia presents to the emergency department with headache, nausea, fever and hypotension. Blood cultures are negative but a Gram stain on cerebrospinal fluid shows small, gram negative diplococci. Which of the following is a significant virulence factor of this organism?
- Coagulase
- Hemolysin
- Peptidoglycan
- Polysaccharide capsule
Board review style answer #1
D. Polysaccharide capsule. This organism’s description is consistent with Neisseria meningitidis which are gram negative diplococci that may not grow in blood cultures in a patient with possible sepsis and meningitis. N. meningitidis may or may not produce capsule; however, capsule is produced by nearly all isolates that cause invasive disease and is a significant virulence trait that allows immune evasion.
Answers A and B are incorrect because N. meningitidis does not produce coagulase and is nonhemolytic. Answer C is incorrect because peptidoglycan is a component of bacterial cell walls and is not a virulence factor.
Comment Here
Reference: Neisseria meningitidis
Answers A and B are incorrect because N. meningitidis does not produce coagulase and is nonhemolytic. Answer C is incorrect because peptidoglycan is a component of bacterial cell walls and is not a virulence factor.
Comment Here
Reference: Neisseria meningitidis
Board review style question #2
A 25 year old woman rapidly develops septic shock, including petechiae on her palate, conjunctiva and trunk. Blood cultures grow gram negative diplococci that appear encapsulated. On subculture, the organism grows on sheep’s blood agar and chocolate agar but does not grow on MacConkey plates. Which of the following is a significant risk factor for infection by this organism?
- CARD9 deficiency
- Chronic granulomatous disease
- Terminal complement pathway deficiency
- Thalassemia
Board review style answer #2
C. Terminal complement pathway deficiency. This organism’s description is consistent with Neisseria meningitidis which are gram negative diplococci that may appear encapsulated, grows on sheep’s blood and chocolate but not MacConkey agar and may cause fulminant septic shock including petechiae. Defects in the terminal complement pathway, including congenital or as a result of immunosuppressive drugs such as eculizumab, increase the risk of infection by encapsulated bacteria including N. meningitidis, Haemophilus influenzae and Streptococcus pneumoniae.
CARD9 deficiency, chronic granulomatous disease and thalassemia can increase a patient’s risk for infection but have no specific association with N. meningitidis. Answer A is incorrect because CARD9 deficiency confers susceptibility to fungal infections such as candidiasis. Answer B is incorrect because chronic granulomatous disease can lead to recurrent infections most commonly in the lung by common pathogens including Staphyloccocus aureus, Serratia, Nocardia and Aspergillus. Answer D is incorrect because thalassemia can increase the overall risk of infection but not specifically N. meningitidis infection unless the patient has undergone a splenectomy.
Comment Here
Reference: Neisseria meningitidis
CARD9 deficiency, chronic granulomatous disease and thalassemia can increase a patient’s risk for infection but have no specific association with N. meningitidis. Answer A is incorrect because CARD9 deficiency confers susceptibility to fungal infections such as candidiasis. Answer B is incorrect because chronic granulomatous disease can lead to recurrent infections most commonly in the lung by common pathogens including Staphyloccocus aureus, Serratia, Nocardia and Aspergillus. Answer D is incorrect because thalassemia can increase the overall risk of infection but not specifically N. meningitidis infection unless the patient has undergone a splenectomy.
Comment Here
Reference: Neisseria meningitidis