Table of Contents
Definition / general | Essential features | Epidemiology | Sites | Pathophysiology | Clinical features | Laboratory | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Molecular / cytogenetics description | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Lieberman JA. Klebsiella oxytoca. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/microbiologyklebsiellaoxytoca.html. Accessed December 26th, 2024.
Definition / general
- Common gram negative bacterium
- Taxonomy: order Enterobacterales, family Enterobacteriaceae (Int J Syst Evol Microbiol 2016;66:5575)
Essential features
- Gram negative, rod shaped, facultatively anaerobic
- Lactose fermenting, indole positive
- Many anatomic and environmental sources
- Opportunistic pathogenic, multiple sites
- Antibiotic associated hemorrhagic diarrhea
- Cytotoxin
- Frequently antibiotic resistant, including extended spectrum beta lactamases (ESBLs)
Epidemiology
- All body sites, feces especially important
- Ubiquitous in environment
- Especially important as hospital associated infection (Klebsiella spp. are ~8% of such infections) (Infect Control Hosp Epidemiol 2016;37:1288)
- Contamination of nonbiological surfaces in hospitals (Emerg Infect Dis 2012;18:1242, J Clin Microbiol 2007;45:3352)
- Opportunistic pathogen, including mild forms of immunocompromise such as old age, metabolic disease / illness, alcoholism
Sites
- Lung / pneumonia
- Blood stream infections
- Enteritis
- Watery diarrhea (J Clin Microbiol 2012;50:1571)
- Hemorrhagic enteritis / colitis, often antibiotic associated (J Clin Microbiol 2010;48:817, N Engl J Med 2006;355:2418, Clin Gastroenterol Hepatol 2003;1:370)
- Important cause of C. difficile negative antibiotic associated diarrhea
- Often resolves with removal of antibiotic pressure
Pathophysiology
- Presence of heat labile cytotoxin important virulence factor for hemorrhagic colitis (J Clin Microbiol 2010;48:817, J Biol Chem 2017;292:19503)
- Gram negative organism, contains immunogenic lipopolysaccharide (LPS) anchored in outer membrane
- Multiple antibiotic resistance mechanisms, of note:
- K. oxytoca specific beta lactamase, blaOXY (J Antimicrob Chemother 2015;70:3230)
- Klebsiella spp. are ESKAPE pathogens (Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa and Enterobacter) which often are multidrug resistant (Clin Infect Dis 2009;48:1)
Clinical features
- Hospital acquired infections are similar to other nosocomial bacterial infections (with gram negative organisms)
Laboratory
- Aerobic growth in routine culture conditions, 37°C
- Growth at 44°C
- Growth on blood agar (nonhemolytic)
- Ferments lactose (pink colonies) on MacConkey agar
- Medium sized, slightly mucoid, yellow to cream colored colonies
- Indole positive, differentiates from other Klebsiella spp.
- MALDI-TOF mass spectrometry
Case reports
- Adolescent patient with antibiotic associated hemorrhagic colitis (Pediatrics 2010;125:e960)
- 50 year old man with chronic pneumonia with cavitary lesion and hemoptysis (Pneumonol Alergol Pol 2015;83:383)
- 73 year old man with endocarditis and pyelonephritis (BMJ Case Rep 2018 Sep 1;2018)
- Patient with unusual carbapenem resistant but ceftriaxone and cefepime susceptible strain (IDCases 2017;11:9)
- Cluster of four cases of nosocomial K. oxytoca bloodstream infections (Infect Control Hosp Epidemiol 2004;25:878)
Treatment
- Likely to harbor multidrug resistance mechanisms (example: extended spectrum beta lactamase [ESBL])
- Carbapenems are typically treatment of choice when ESBL suspected in significantly ill patients
- Empiric treatment guided by local resistance
- Definitive treatment depends on phenotypic antibiotic susceptibility testing
- Pharmacy consultation may be useful, as some drugs (cephalosporins) may be sensitive in vitro but are unlikely useful for clinical treatment in the case of various ESBL carrying organisms, including Klebsiellae (J Clin Microbiol 2001;39:2206)
Clinical images
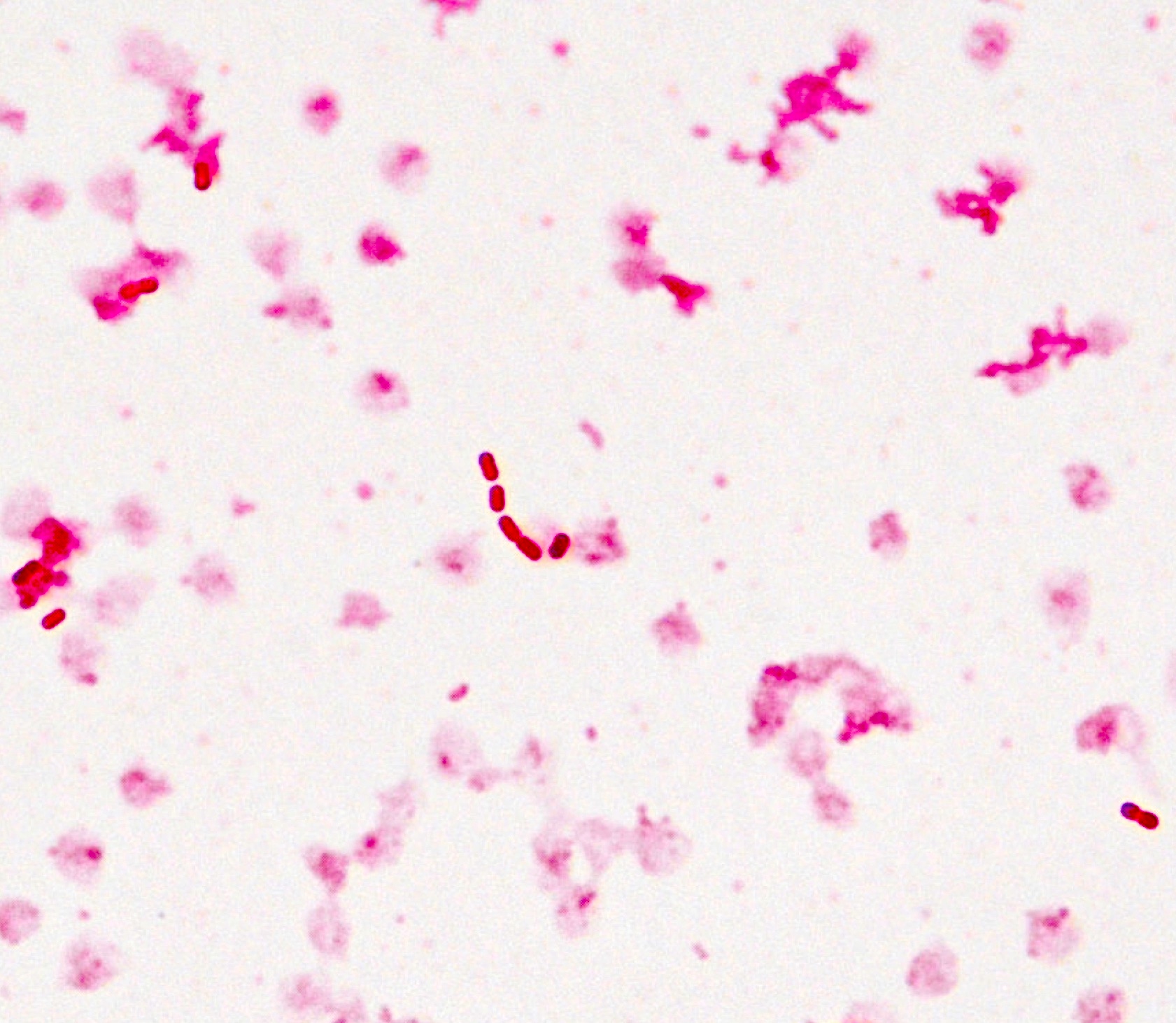
Microscopic (histologic) description
- 2 x 5 micron rod shaped, gram negative bacteria
Microscopic (histologic) images
Molecular / cytogenetics description
- 16S rDNA sequencing does not differentiate from closely related Raoultella spp.
Differential diagnosis
- Klebsiella pneumoniae
- Also gram negative, lactose fermenting organism and member of the same genus
- Indole negative
- Robust polysaccharide capsule
- Raoultella spp.
- Closely related Enterobacteriales member
- Not readily distinguished, even with 16S rDNA amplicon based sequencing
- Other Enterobacteriales
- Includes Citrobacter freundii, Escherichia coli, Shigella spp., Enterobacter spp. and others
- Most commonly MALDI-TOF mass spectrometry or sequence based identification
- Can distinguish with fermentation / metabolic test strips but use of these is rapidly vanishing
- Non-Enterobacteriales nosocomial infections
- Example: Pseudomonas aeruginosa
- Longer and thinner morphology
- Nonlactose fermenting
- Also have mucoid colony appearance
- Example: Pseudomonas aeruginosa
Board review style question #1
The clinical microbiology laboratory has isolated a gram negative rod from the sputum of a homeless, alcoholic patient with a chronic cough. The isolate forms a mucoid colony that turns pink on MacConkey agar and produces a blue spot when placed on filter paper and treated with indole. What is the most likely organism?
- Chlamydia pneumoniae
- Klebsiella oxytoca
- Klebsiella pneumoniae
- Pseudomonas aeruginosa
Board review style answer #1
B. K. oxytoca. Only K. pneumoniae, K. oxytoca and Pseudomonas aeruginosa are gram negative bacilli. Klebsiella spp. ferment lactose (pink on MacConkey's agar), while P. aeruginosa does not ferment lactose. Between K. pneumoniae and K. oxytoca, only K. oxytoca is indole positive. While Chlamydia pneumoniae is gram negative, it is not a bacillus but exists either as a reticulate body (RB) when replicating within host cells (phagolysosomes) or as an infectious elementary body (EB) when passing between cells. C. pneumoniae, like C. trachomatis is therefore not cultured clinically because it requires growth in a eukaryotic cell.
Comment here
Reference: Klebsiella oxytoca
Comment here
Reference: Klebsiella oxytoca
Board review style question #2
For Klebsiella oxytoca, which of the following mechanisms of antibiotic resistance is most important?
- 23S rRNA mutation
- Altered cell wall components
- Drug hydrolyzing enzyme
- Mutation in topoisomerase
Board review style answer #2
C. K. oxytoca carries extended spectrum beta lactamases (ESBLs) which can hydrolyze cephalosporins and other beta lactam antibiotics. Specific resistances vary significantly based on the ESBL identified. In addition, some strains will upregulate drug efflux pumps and ESBL production under antibiotic treatment. Mutation of the 23S rRNA is one mechanism of macrolide resistance. The van operon (especially vanA, vanB) confer vancomycin resistance in Enterococci, as well as Lactobacillus and other anaerobes by changing the peptidoglycan structure to D-Ala-D-Lactate. Fluoroquinolone / quinolone anitbiotics inhibit topoisomerase (DNA gyrase) enzymes and mutations in these genes are an important mechanism of resistance to this class of antibiotics.
Comment here
Reference: Klebsiella oxytoca
Comment here
Reference: Klebsiella oxytoca