Table of Contents
Definition / general | Essential features | Epidemiology | Sites | Pathophysiology | Clinical features | Laboratory | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Molecular / cytogenetics description | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Mruthyunjayappa S, Leal SM. Blastomyces. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/microbiologyblastomyces.html. Accessed April 1st, 2025.
Definition / general
- Taxonomy:
- Class: Eurotiomycetes; order: Onygenales; family: Ajellomycetaceae
- Common species:
- Blastomyces dermatitidis: most common cause of blastomycosis
- Blastomyces gilchristi: northern U.S. and Canada
- Blastomyces helicus: western U.S
- Blastomyces percursus: Africa
Essential features
- Dimorphic mold
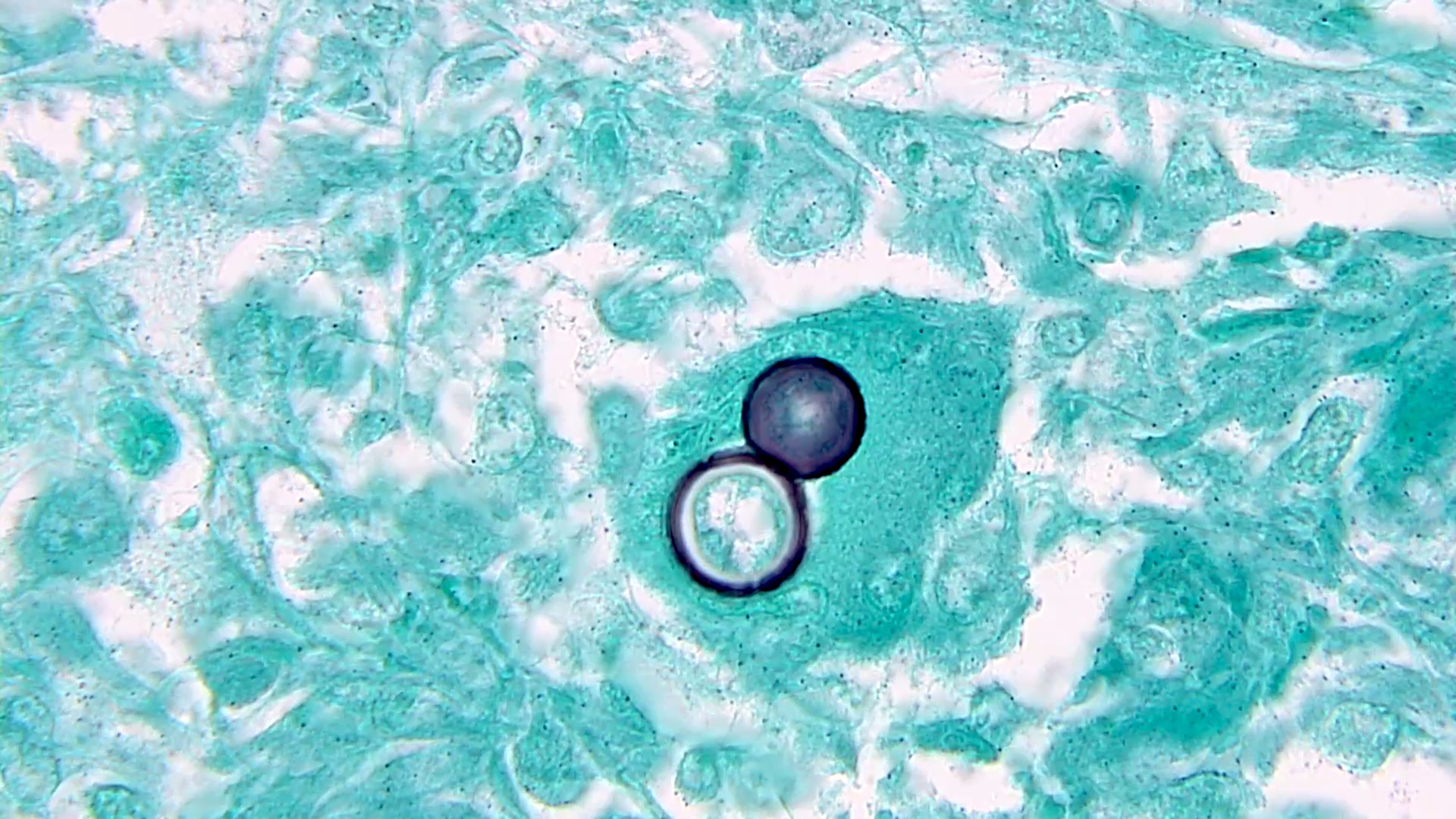
- Body temperature, uniformly sized, extracellular round yeasts with a thick, refractile, double contoured cell wall and broad based budding
- Immunocompetent: a chronic granulomatous and suppurative disease of the lung or skin
- Immunocompromised: disseminated disease with poor prognosis
Epidemiology
- Cause of blastomycosis, a chronic pyogranulomatous inflammatory disease
- Soil organisms, associated with moist areas near riverbeds
- Midwestern, south central and southeastern U.S., particularly in areas surrounding the Ohio and Mississippi River valleys, the Great Lakes and the Saint Lawrence River
- Present in Canada, with a small number of documented cases in Africa and India
- References: J Clin Aesthet Dermatol 2009;2:22, Semin Respir Crit Care Med 2020;41:31
Sites
- Pulmonary blastomycosis: can be asymptomatic or range from self limited pulmonary infection to life threatening (eMedicine: Acute Respiratory Distress Syndrome (ARDS) [Accessed 26 January 2022])
- Extrapulmonary blastomycosis:
- Cutaneous: development of verrucous (wart-like) or ulcerative skin lesions
- Osseous: osteomyelitis along with contagious tissue abscesses and draining sinuses
- Genitourinary (usually male): involvement of the prostate and epididymis
- Central nervous system: brain abscess, cranial or epidural abscess and meningitis
Pathophysiology
- Inhaled spores transform into yeasts resulting in acute and chronic lung inflammation
- Cutaneous lesions can demonstrate pseudoepitheliomatous hyperplasia of the epidermis
- Dissemination to extrapulmonary sites, especially the skin, is presumed to be hematogenous
- Reference: J Clin Aesthet Dermatol 2009;2:22
Clinical features
- Involves the lung in over 90% of cases; infection can range from asymptomatic self limited infection (about 50% of cases) to severe diffuse pneumonia causing respiratory failure
- Extrapulmonary dissemination occurs in approximately 25 - 50% of cases of blastomycosis (Mycopathologia 2009;167:115)
Laboratory
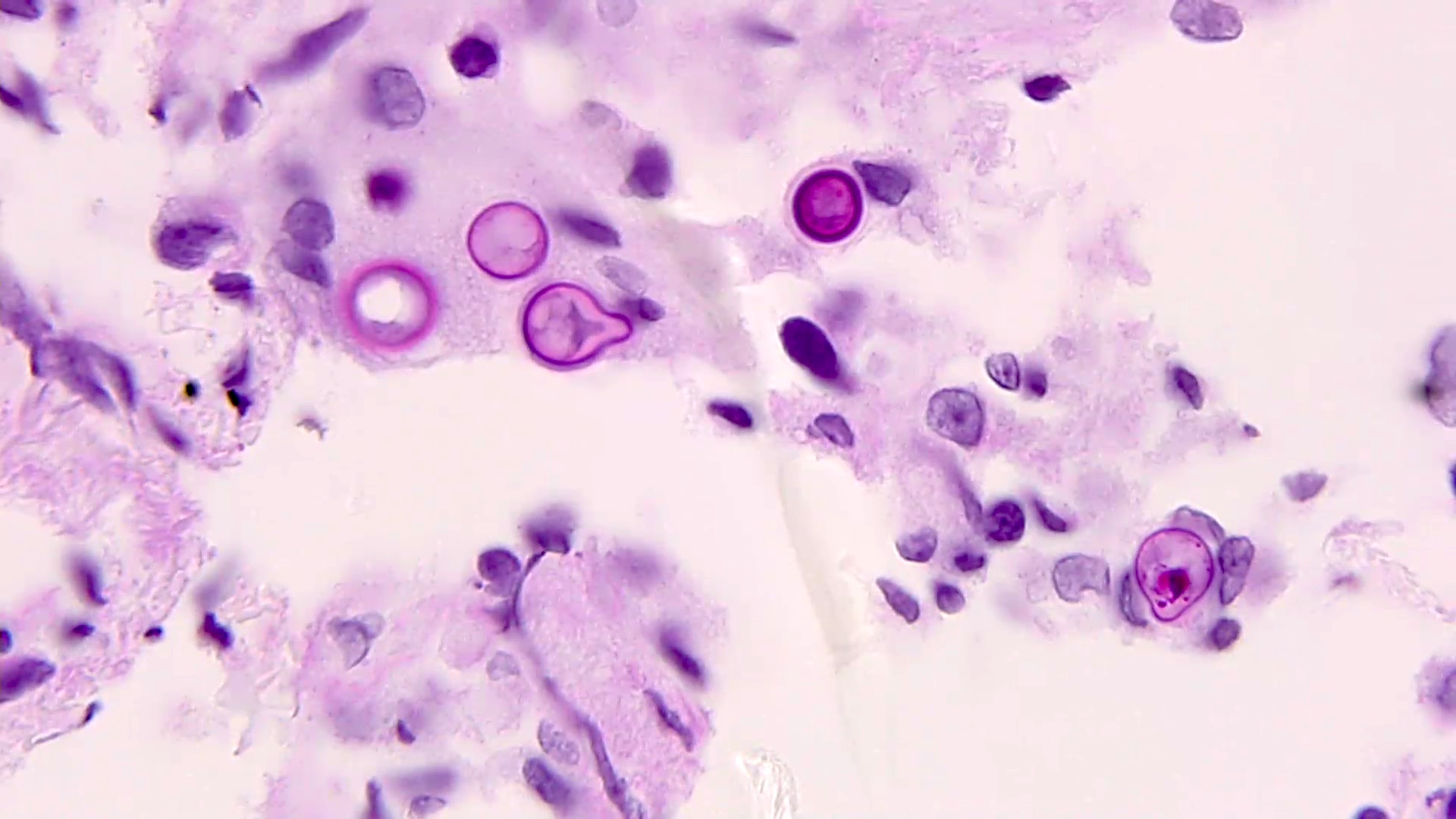
- Direct exam shows large, thick walled, yeast forms with single broad based budding cells (8 - 10 μm)
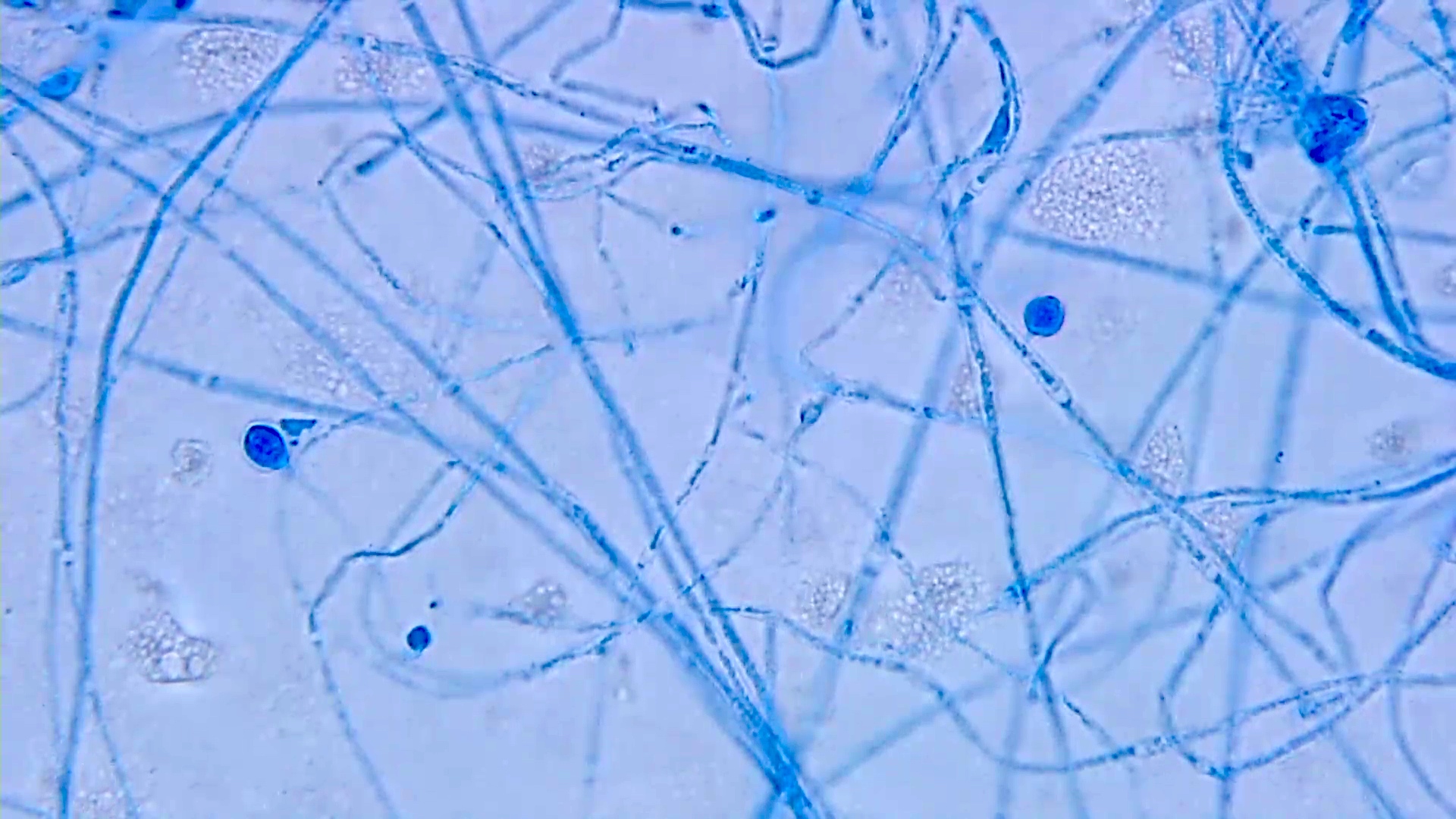
- Slow growing yeasts that transition to a fluffy white mycelium or glabrous, tan, nonsporulating colonies within 1 - 4 weeks
- Microconidia resemble Histoplasma capsulatum but macroconidia are not formed
- Microscopic examination of growth demonstrates thick walled yeast cells with broad based budding
- Conversion to the yeast phase can occur on routine media incubated at 37 °C
- Antibody detection tests
- Immunodiffusion utilizes purified B. dermatitidis A antigen (relatively low sensitivity and specificity)
- Enzyme immunoassays use BAD1 antigen: most sensitive approach (cross reactivity seen with histoplasmosis and other fungal infections)
- Reference: Semin Respir Crit Care Med 2020;41:31
Case reports
- 17 year old South African boy with slow growing lesion of the scalp and neck (Int J Dermatol 2012;51:1090)
- 24 year old man with blastomycosis of nose (Ear Nose Throat J 2016;95:E28)
- 36 year old immunocompetent man with disseminated blastomycosis (Oxf Med Case Reports 2018;2018:omy071)
- 42 year old man with Blastomyces oteomyelitis (Cureus 2020;12:e7417)
- 42 year old man with disseminated blastomycosis infection diagnosed on FNA of the thyroid (Diagn Cytopathol 2011;39:446)
Treatment
- Acute pulmonary blastomycosis can be mild and self limited, not requiring treatment in immunocompetent hosts
- More severe disease, particularly in immunocompromised hosts, requires itraconazole with or without liposomal amphotericin B
- Treatment duration can range from 6 months to 1 year
- References: Clin Infect Dis 2000;30:679, S D Med 2006;59:255
Microscopic (histologic) description
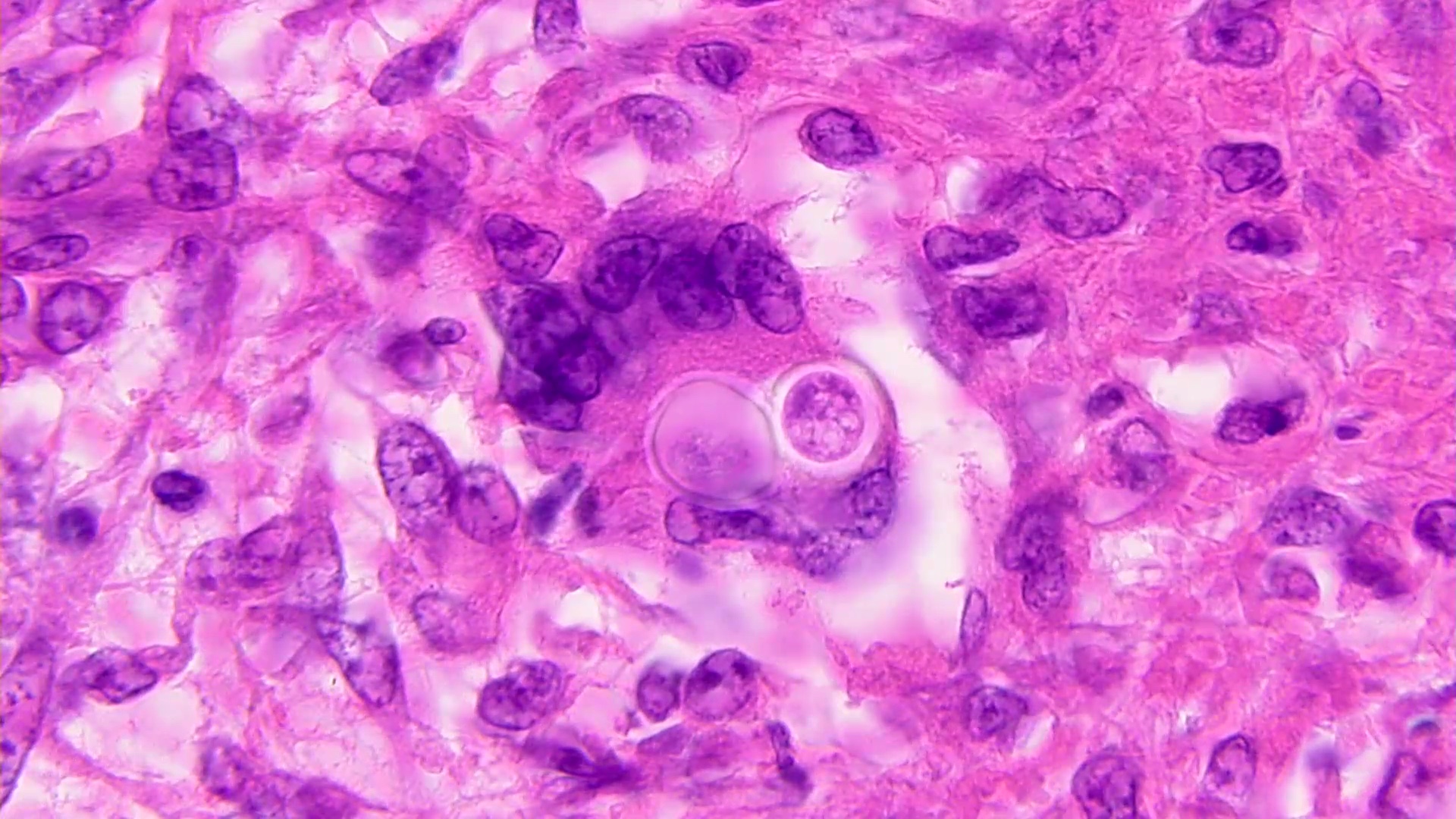
- Pyogranulomatous inflammation: neutrophil infiltration admixed with epithelioid histiocytes and granulomatous inflammation
- Cutaneous lesions demonstrate pseudoepitheliomatous hyperplasia of the epidermis
- Uniformly sized, refractile round yeast cells may be observed at low power in H&E stained tissue sections
- High power may show cell contents within the refractile cell wall but often this material washes away during processing
- Periodic acid-Schiff (PAS) and Gomori methenamine silver (GMS) stains highlight organisms
- Mucicarmine may be weakly positive; contrast with a strongly positive Cryptococcus
- Fontana-Masson stain for melanin: negative
- Reference: Semin Respir Crit Care Med 2020;41:31
Microscopic (histologic) images
Positive stains
- Periodic acid-Schiff (PAS) and Gomori methenamine silver (GMS) stains highlight organisms
- Mucicarmine may be weakly positive; contrast with a strong positive Cryptococcus
Molecular / cytogenetics description
- Nucleic acid probe hybridization assays are commercially available (AccuProbe by Hologic, Inc.) for definitive identification on culture
- Additional lab developed PCR tests, sequencing and matrix assisted laser desorption / ionization time of flight (MALDI-TOF) mass spectrometry (MS) may enable identification
Differential diagnosis
- Acute illness:
- Community acquired pneumonia:
- Viral, bacterial, atypical bacterial
- Community acquired pneumonia:
- Chronic illness:
- Tuberculosis, infection with nontuberculous mycobacteria:
- Acid fast organisms
- Histoplasmosis:
- Small, uniform, narrow based budding yeasts; large tuberculate macroconidia
- Coccidioidomycosis:
- Thick walled spherules with endospores in tissue
- Sarcoidosis:
- Diagnosis of exclusion after ruling out all the infectious agents
- Tuberculosis, infection with nontuberculous mycobacteria:
Additional references
Board review style question #1
A 36 year old Caucasian woman from Tennessee develops flu-like symptoms with fever, headache, diffuse joint pain and cough. She currently takes ibuprofen, which does not alleviate symptoms. An Xray shows diffuse bilateral pneumonia. After 1 week at 30 °C, sputum cultures show unique colonies with central yeast-like creamy morphology and peripheral fuzzy mold-like extensions. At 2 weeks, the colonies are almost entirely mold-like and a tape prep shows thin hyaline septate hyphae with lollipop-like structures called aleurioconidia. No large tuberculate macroconidia are noted at 2 weeks but are spotted at 4 weeks. A molecular test is performed to confirm the diagnosis. What is the most likely cause of respiratory illness?
- Blastomyces dermatitidis
- Coccidioides immitis
- Histoplasma capsulatum
- Paracoccidiodes braziliensis
Board review style answer #1
C. Histoplasma capsulatum. Coccidiodes species exhibit alternating barrel shaped arthroconidia. Paracoccidiodes, Blastomyces and Histoplasma species cultured at 30 °C form lollipop-like aleurioconidia but only Histoplasma proceeds to make large tuberculate macroconidia in late cultures.
Comment Here
Reference: Blastomyces
Comment Here
Reference: Blastomyces
Board review style question #2
Which of the following is true for Blastomyces infection?
- Cutaneous lesions demonstrate pseudoepitheliomatous hyperplasia of the epidermis
- Direct exam shows large, thick walled, refractile yeast forms (8 - 10 μm) with narrow based budding
- Extrapulmonary dissemination does not occur in Blastomyces
- Late cultures show large tuberculate macroconidia
Board review style answer #2
A. Cutaneous lesions demonstrate pseudoepitheliomatous hyperplasia of the epidermis
Comment Here
Reference: Blastomyces
Comment Here
Reference: Blastomyces