Table of Contents
Definition / general | Epidemiology | Pathophysiology | Etiology | Clinical features | Staging / staging classifications | Diagnosis | Laboratory | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Differential diagnosis | Additional referencesCite this page: Soni A, Slominski A. Borrelia burgdorferi / Lyme disease. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/microbiologybburgdorferi.html. Accessed March 31st, 2025.
Definition / general
- Lyme disease is a multisystem disorder caused by spirochete Borrelia burgdorferi
Epidemiology
- In the United States, Lyme disease most commonly occurs in the northeast and upper midwest
- Worldwide, more commonly found in northern Asia and eastern and central Europe
Pathophysiology
- The bite of an infected Ixodes dammini tick causes proliferation of spirochetes in the dermis
- The host dermal inflammatory response causes a rash known as erythema chronicum migrans
- Over days, the spirochetes spread to the nervous system, cardiac tissue and joints via the blood stream
- The spirochetes may induce host cells to produce quinolinic acid, which stimulates NMDA receptors and manifests as malaise in lyme encephalopathy (Neurology 1992;42:43)
- Note: Lyme disease spirochetes are never seen in peripheral blood
Etiology
- Usually transmitted by Ixodes dammini tick
Clinical features
- Causes erythema chronicum migrans (red papule with central clearing that expands slowly), acrodermatitis chronica atrophicans (disease of extremities, usually women, with erythematous, edematous, pruritic phase, followed by sclerosis and atrophy), cutaneous lymphoid hyperplasia of skin
- Also affects heart, joints, nervous system
Staging / staging classifications
- Stage 1: skin lesion (erythema chronicum migrans)
- Stage 2: cardiovascular and nervous system involvement
- Stage 3: arthritis stage characterized by migratory polyarthritis; however, cutaneous lesions and peripheral nervous system involvement are also encountered in this stage
Diagnosis
- Clinical symptoms such as erythema migrans, fever, facial palsy or arthritis
- Biopsy interpretation
Laboratory
- EIA or ELISA for total Lyme titer or IgG and IgM titers
- If EIA / ELISA test results come back positive or equivocal, Western blot IgG and IgM titers are performed
- Lyme titers should be done if the above tests are positive
- PCR in synovial fluid (for spirochetes)
- CSF analysis
- ECG for Lyme carditis
- Darkfield microscopy for spirochetes
Case reports
- Young boy with butterfly rash (Acta Derm Venereol 2010;90:109)
- 17 year old boy with fatal Lyme carditis (Cardiovasc Pathol 2015;24:317)
- 27 year old woman with Lyme disease associated neuroretinitis (Acta Microbiol Immunol Hung 2015;62:403)
- 30 and 50 year old men with "chronic Lyme disease" (JAMA Intern Med 2015;175:132)
- Lyme disease with hearing loss as sole presentation (J Laryngol Otol 2015;129:183)
Treatment
- Early infection: Antibiotics such as doxycycline, amoxicillin, azithromycin
- Late infection: IV ceftriaxone is considered treatment of choice
Clinical images
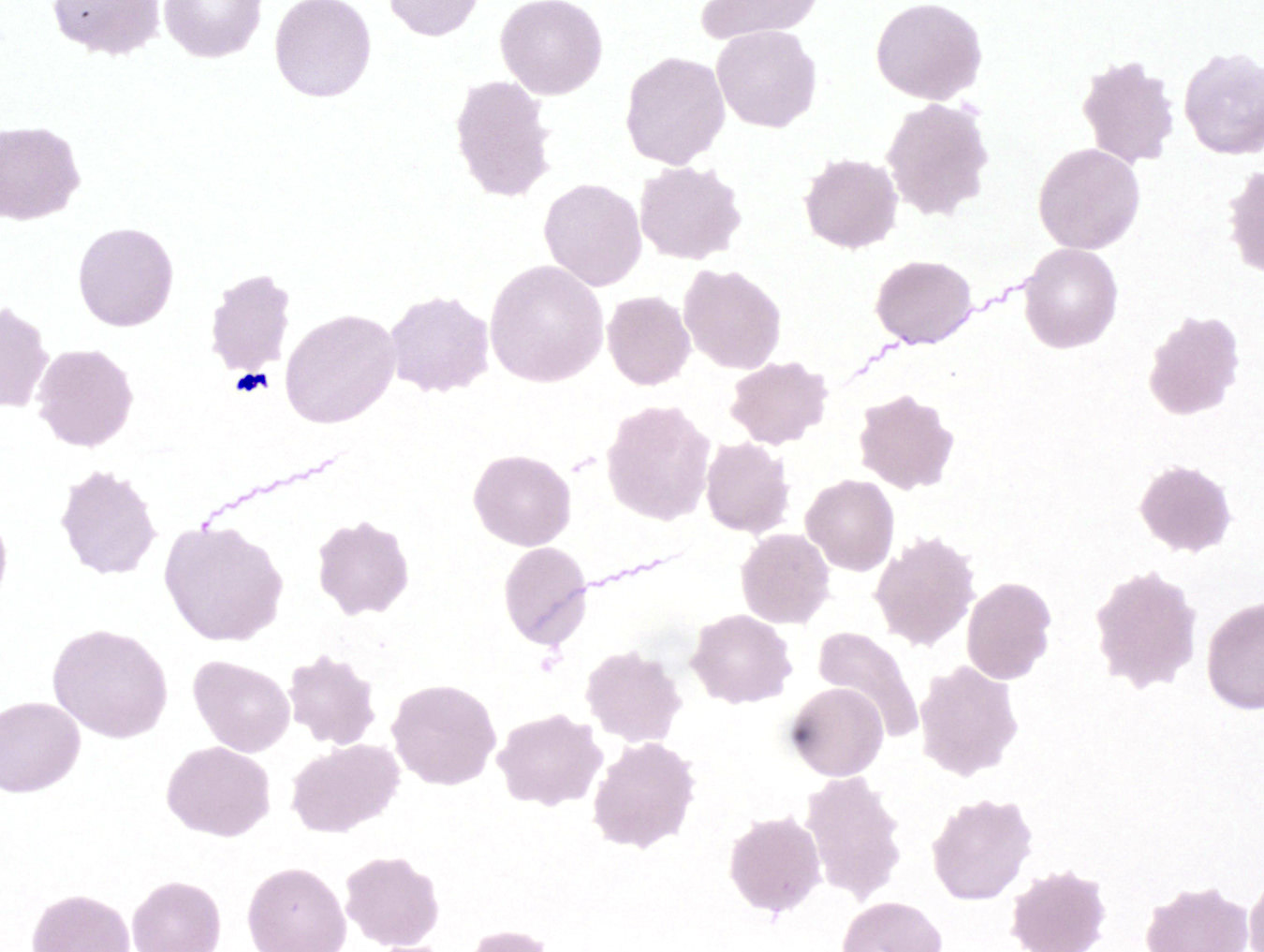
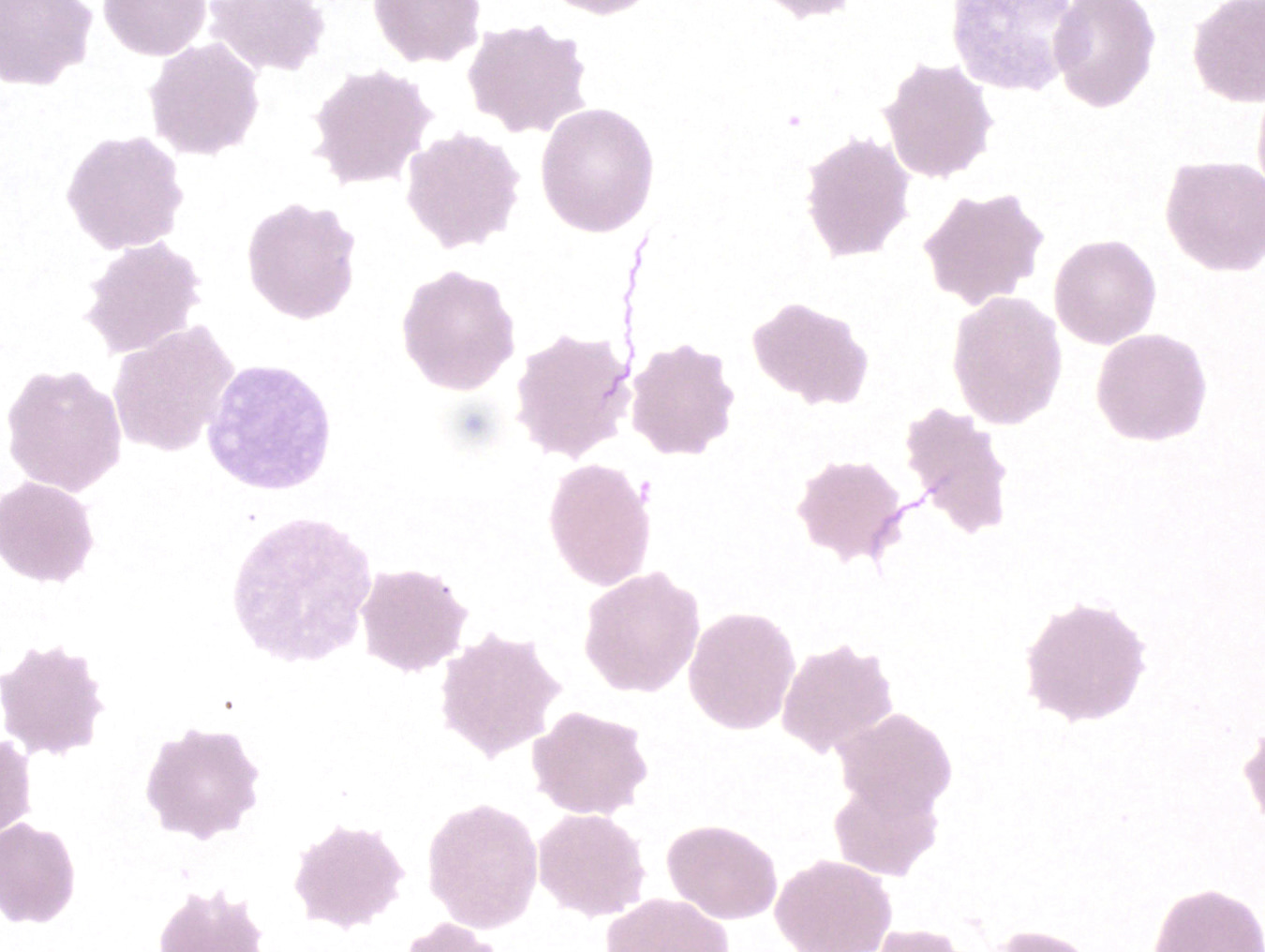
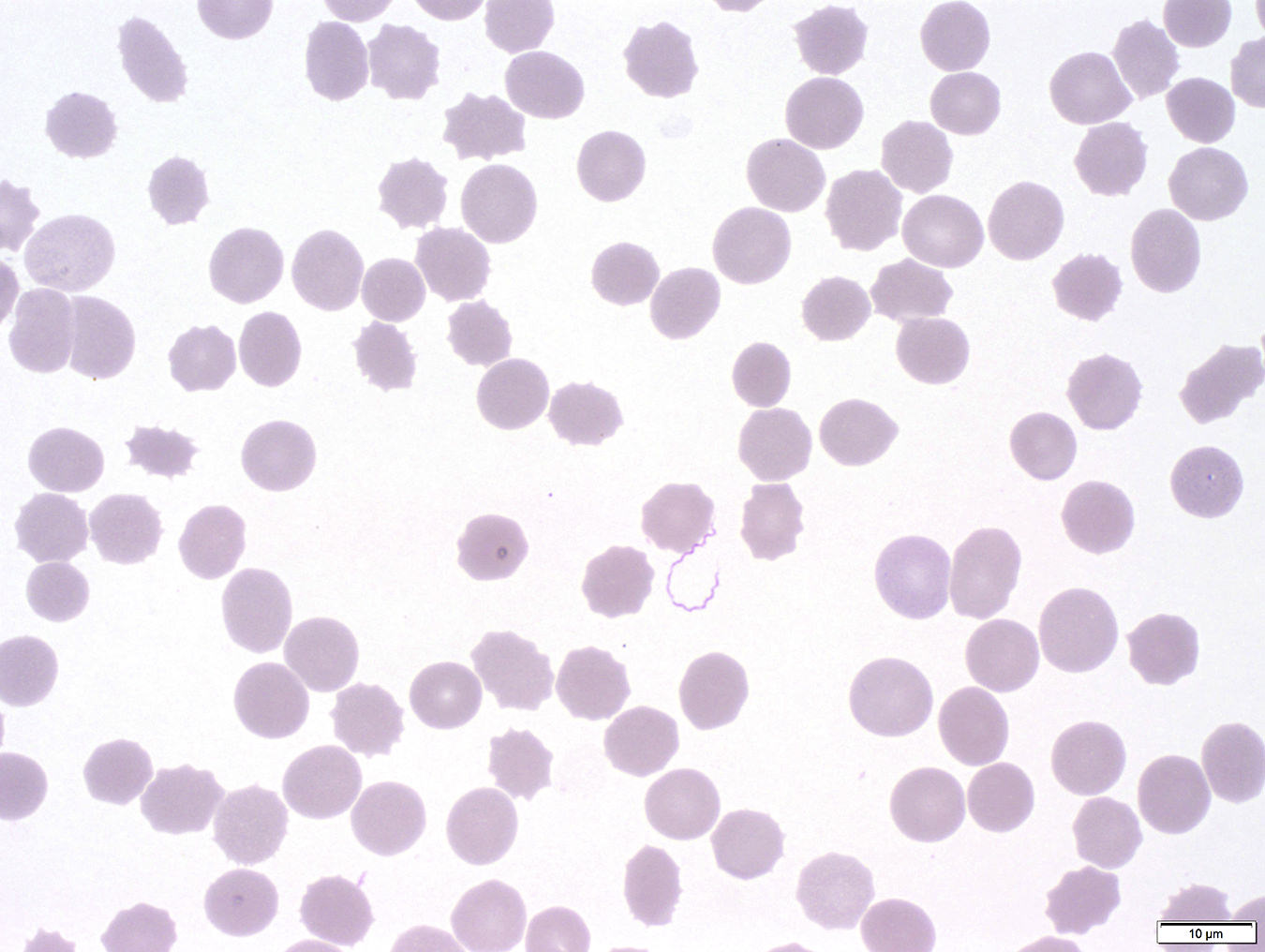
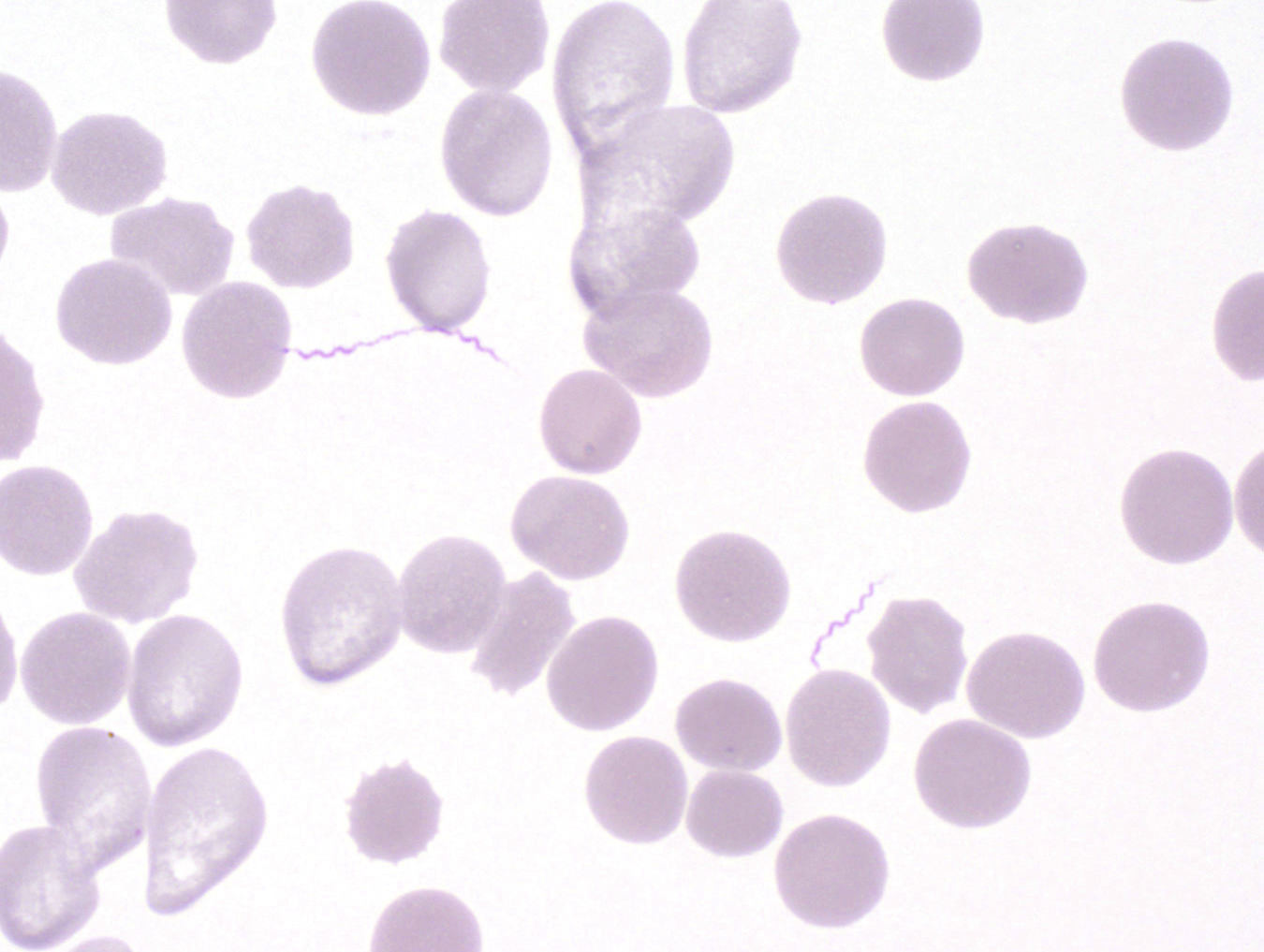
Microscopic (histologic) description
- Superficial and deep perivascular polymorphic infiltrate of neutrophils, lymphocytes, plasma cells, eosinophils and mast cells
- Vascular proliferation and dermal necrosis may be present
- Identification of spirochetes by silver stain or immunocytochemistry is diagnostic
- Borrelia spirochetes are long spiral bacilli (5 - 20 microns in length) with relatively regular undulations
- Typically Borrelia burgdorferi does NOT reach sufficient levels in blood to be seen on peripheral blood smear
- PCR can also be used for diagnosis
Microscopic (histologic) images
Positive stains
- Warthin-Starry (for spirochetes)
- Immunocytochemistry with monoclonal antibodies against Borrelia species
Differential diagnosis
- Bacteria that are not spirochetes but have curved or wavy rods include Vibrio, Campylobacter, Helicobacter
- Other spirochetes include Treponema and Leptospira, but they are not typically seen in blood
Additional references
- WHO: Lyme Borreliosis [Accessed 28 August 2018], eMedicine: Lyme Disease [Accessed 28 August 2018], Wikipedia: Lyme Disease [Accessed 28 August 2018], Rosai: Rosai and Ackerman's Surgical Pathology, 10th Edition, 2011, Johnston: Weedon's Skin Pathology Essentials, 1st Edition, 2012, Emerg Infect Dis 2007;13:436, Pritt: Creepy Dreadful Wonderful Parasites Blog [Accessed 7 August 2018]