Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Chatzopoulos K. NUT carcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lungtumornutcarcinoma.html. Accessed December 26th, 2024.
Definition / general
- NUT carcinoma is an aggressive malignancy characterized by NUT gene rearrangements
- Monotonous, poorly differentiated morphology with foci of abrupt keratinization
Essential features
- NUT carcinoma is an aggressive malignancy more frequently arising in the thorax or aerodigestive tract, affecting patients of any age with equal gender distribution
- Morphologically it shows diffuse architecture and consists of monotonous cells with frequent cytoplasmic clearing, large nuclei with prominent nucleoli and foci of abrupt keratinization
- Due to its largely nonspecific morphology, the differential diagnosis is broad
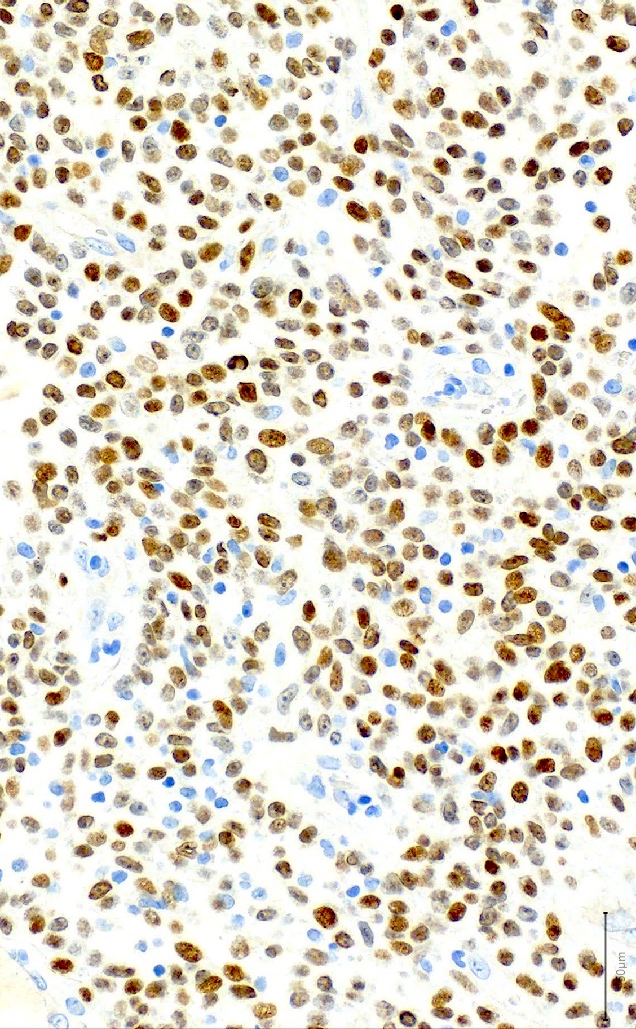
- Speckled nuclear immunohistochemical expression of NUT protein in ≥ 50% of cells is a diagnostic hallmark
- NUT gene rearrangements are present and can be detected by FISH
Terminology
- NUT midline carcinoma (no longer recommended)
ICD coding
- ICD-O: 8023/3 - NUT carcinoma
Epidemiology
- M = F (Clin Cancer Res 2012;18:5773)
- Initially thought to affect younger patients; later proven to affect patients of any age (Clin Cancer Res 2012;18:5773)
Sites
- Mediastinum (Clin Cancer Res 2012;18:5773)
- Upper aerodigestive tract (Clin Cancer Res 2012;18:5773)
- Occasionally: salivary glands, retroperitoneum, pancreas, urinary bladder (Cancer Genet Cytogenet 2010;203:16)
Pathophysiology
- Somatic NUT reciprocal translocation leading to expression of an oncogenic NUT fusion gene (Cancer Genet Cytogenet 2010;203:16)
- See Molecular / cytogenetics description
Etiology
- Definitive environmental or infectious etiology is lacking (Cancer Genet Cytogenet 2010;203:16)
Clinical features
- Symptoms depend on anatomic location and extent of tumor
- Thoracic cases present with cough, shortness of breath, hemoptysis, pericardial or pleural effusion (Lung Cancer 2015;90:484, Diagn Cytopathol 2019;47:594)
- Very aggressive clinical course, leading to death within a few months (Eur Arch Otorhinolaryngol 2018;275:815)
Diagnosis
- Diagnosis of NUT carcinoma can be challenging because of nonspecific morphologic features
- Features may not be uniformly present in small biopsy specimens
- A combination of subtle morphologic changes with NUT immunohistochemistry can aid in the diagnosis (Virchows Arch 2021;478:21)
Laboratory
- Occasional elevation of serum alpha fetoprotein in mediastinal cases (Cancer Res 2003;63:304)
Prognostic factors
- Poor prognosis, with median survival from initial diagnosis ranging 1 - 6.7 months (Clin Cancer Res 2012;18:5773, Eur Arch Otorhinolaryngol 2018;275:815, J Thorac Oncol 2015;10:951)
Case reports
- 26 year old man with a 3 cm sublingual gland mass (Head Neck Pathol 2017;11:460)
- 28 year old man with a tracheal mass, false negative FISH results and long term survival (Head Neck Pathol 2021;15:698)
- 32 year old woman with a 7.6 cm perihilar mass (Int J Surg Pathol 2016;24:85)
- 34 year old pregnant woman with a right pulmonary mass (World J Surg Oncol 2020;18:290)
Treatment
- Surgery, chemotherapy and radiation (Eur Arch Otorhinolaryngol 2018;275:815)
- Surgical options may be limited because of surgical inaccessibility of tumors, particularly those with thoracic anatomic localization (Pathol Int 2018;68:583)
- Radiotherapy seems to produce superior outcomes compared with conventional chemotherapy (Clin Cancer Res 2012;18:5773)
Gross description
- Because of the advanced stage at diagnosis, examination of complete resection specimens is rare
- Tumor can be deceivingly well demarcated from adjacent structures (Int J Surg Pathol 2016;24:85)
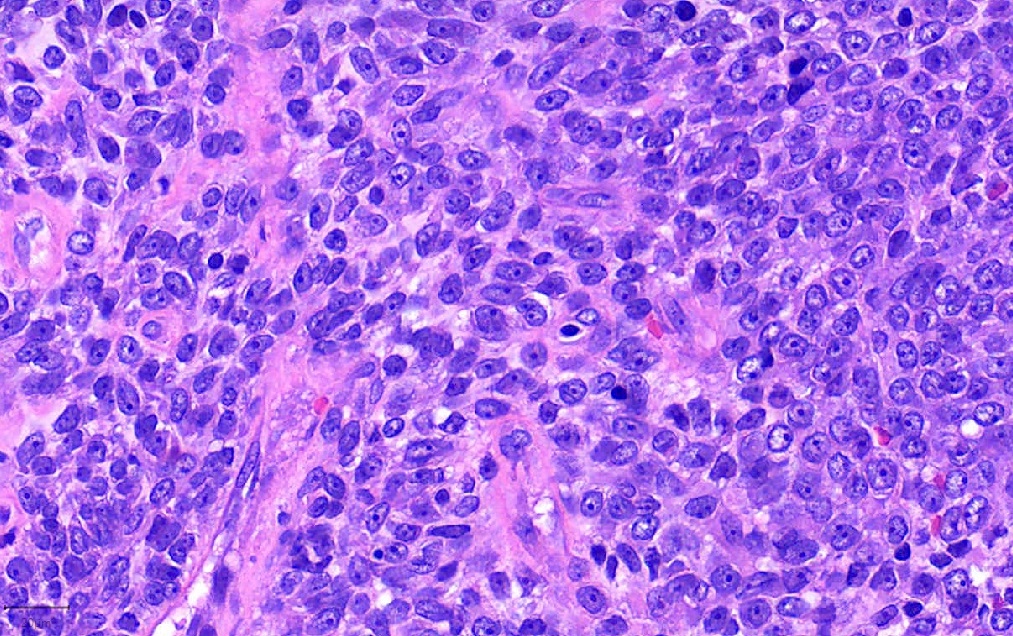
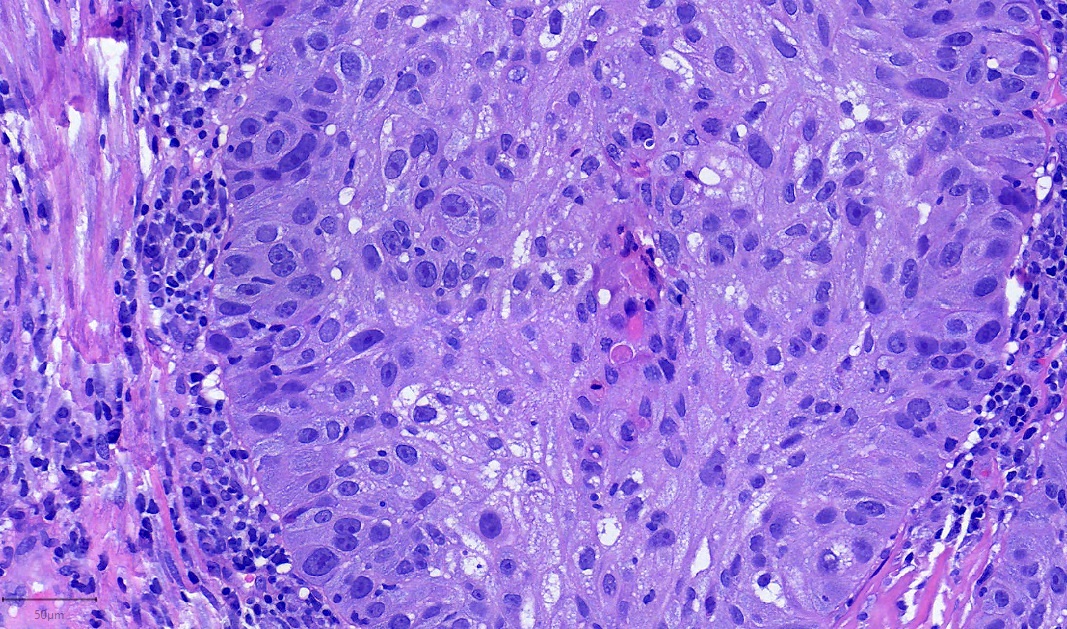
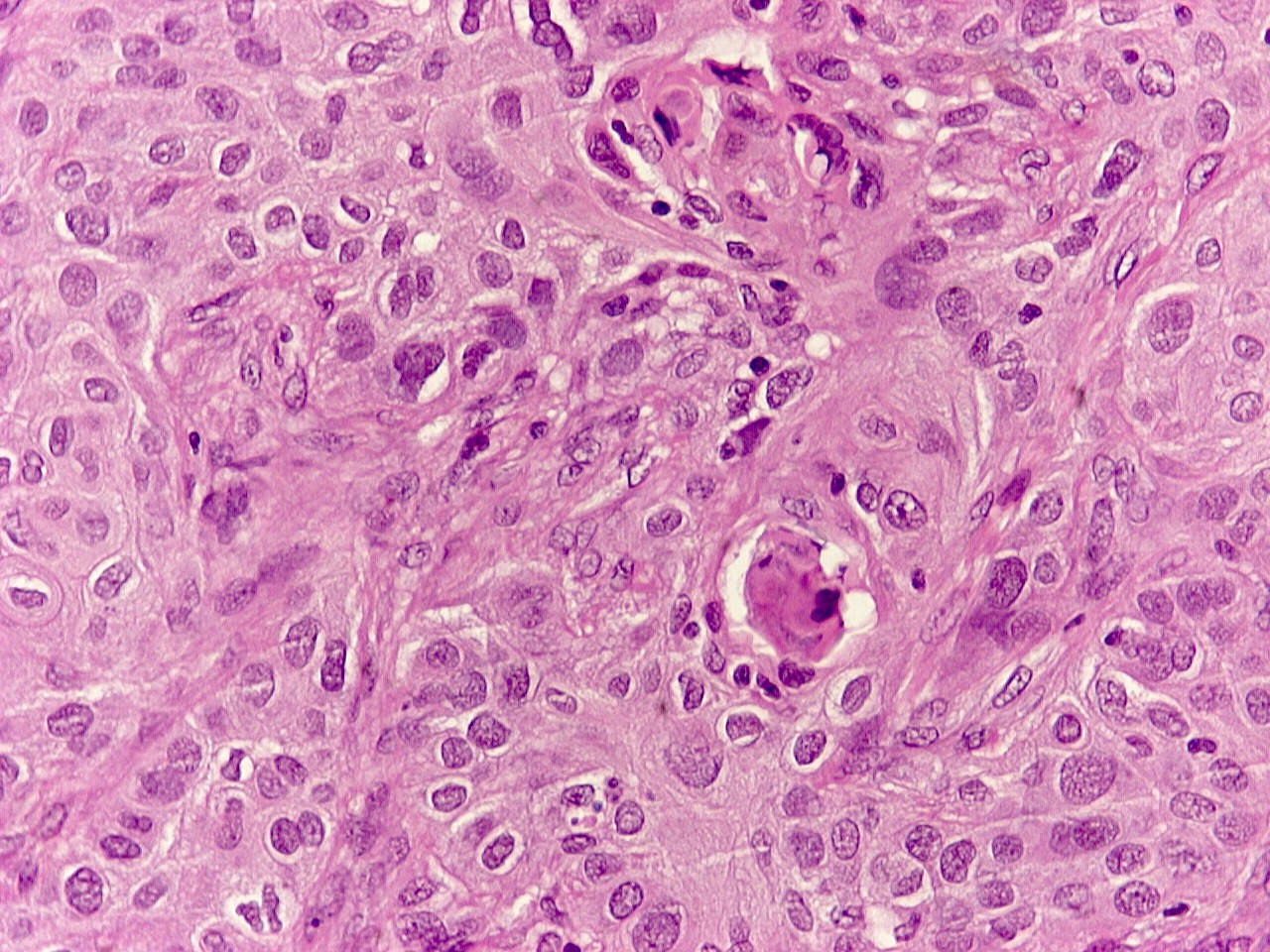
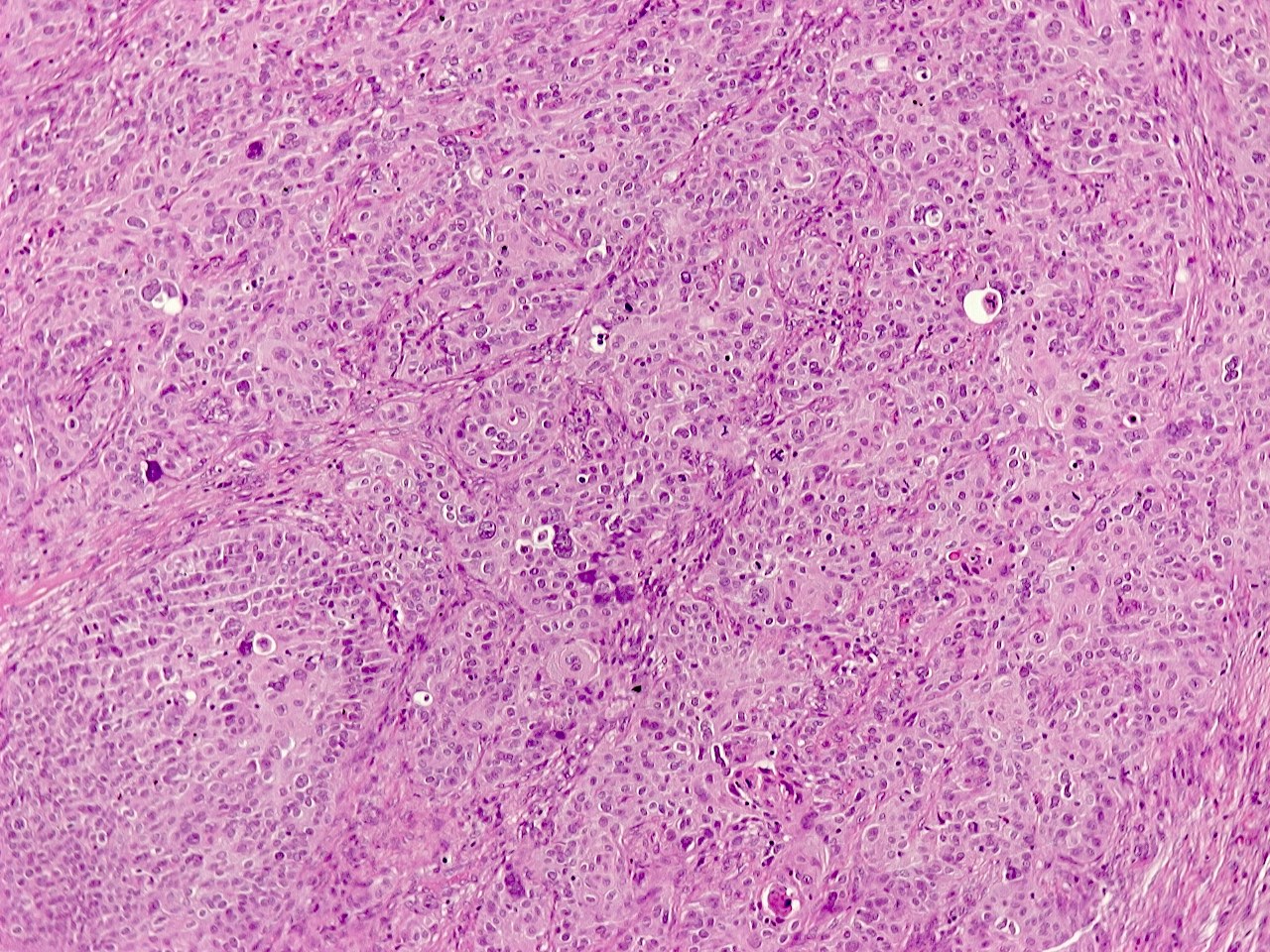
Microscopic (histologic) description
- Primitive looking, monotonous, medium sized cells with frequent cytoplasmic clearing (Cancer Genet Cytogenet 2010;203:16)
- Scattered foci of abrupt keratinization (J Thorac Oncol 2015;10:951)
- Large nuclei with prominent nucleoli (Ultrastruct Pathol 2012;36:280)
- Diffuse architecture with occasional spacing and discohesion of tumor cells (Cancer Cytopathol 2016;124:901)
- Background of necrosis with prominent neutrophils (Cancer Cytopathol 2016;124:901)
- Occasionally, pseudoglandular formations; mucoid stroma, crushing artifact (Int J Surg Pathol 2019;27:225, J Thorac Oncol 2015;10:951)
Microscopic (histologic) images
Cytology description
- Hard to diagnose on cytology because of frequent lack of overt squamous differentiation (Cancer Cytopathol 2016;124:901)
- Scattered dyskeratotic cells may be diagnostically helpful (J Pathol Transl Med 2018;52:349)
Positive stains
- NUT speckled nuclear positivity (sensitivity 87%, specificity 100%) (Am J Surg Pathol 2009;33:984)
- Keratins, particularly high molecular weight (Thorac Cancer 2020;11:1724)
- p63 and p40 (J Thorac Oncol 2015;10:951)
- MYC strongly expressed in primitive component, attenuated in squamoid foci (Oncologist 2019;24:e740)
- p16 can be strongly expressed, without relationship with HPV infection (Appl Immunohistochem Mol Morphol 2014;22:262)
Negative stains
- Negative most of the time but with occasional positive cases (diagnostic pitfalls): CD99, synaptophysin, FLI1, EGFR, HER2, focal TTF1 (Oncologist 2019;24:e740, Biomed Res Int 2020;2020:9791208, J Thorac Oncol 2015;10:951)
Electron microscopy description
- Tumor cells with short microvillous apex, intracellular desmosomes and junctional complexes (Ultrastruct Pathol 2012;36:280)
- Cytoplasmic tonofilaments, polyparticulate glycogen, lipid droplets and electron dense granules (Ultrastruct Pathol 2012;36:280)
Molecular / cytogenetics description
- Reciprocal translocation t(15;19) leading to BRD4::NUT fusion in 70% of cases (Cancer Genet Cytogenet 2010;203:16)
- BRD3::NUT fusion in remaining cases (Cancer Genet Cytogenet 2010;203:16)
- Rare NUT fusion counterpart genes: NSD3, ZNF532, ZNF592 (Cancer Genet Cytogenet 2010;203:16)
- FISH for NUT rearrangements in combination with NUT immunohistochemistry has 100% sensitivity and specificity (Am J Surg Pathol 2009;33:984)
- Next generation sequencing (NGS) or reverse transcription PCR can detect rare NUT fusions nondetectable by FISH (Lung Cancer 2015;90:484)
- TP53 and PIK3CA are frequently mutated genes (Cancer Med 2021;10:5757)
Sample pathology report
- Mediastinum, anterior, excisional biopsy:
- NUT carcinoma (see comment)
- Comment: Infiltrative, poorly differentiated carcinoma, with extensive necrosis and focal keratinization. Immunohistochemically, tumor cells express p63, p40, keratins 5/6 and NUT. Break apart FISH is positive for NUT rearrangement. These findings support the diagnosis.
Differential diagnosis
- Focally keratinizing or basaloid squamous cell carcinoma (Oncologist 2019;24:e740):
- NUT immunohistochemistry is important in differentiating those tumors (Am J Surg Pathol 2009;33:984, Virchows Arch 2021;478:21)
- Thymic carcinoma (Cancer Res 1991;51:3327):
- Thymic carcinomas usually express all of CD5, GLUT1 and CD117 (Am J Surg Pathol 2011;35:1296)
- Small cell carcinoma:
- Occasional positivity for synaptophysin and nuclear molding in NUT carcinoma is a diagnostic pitfall (J Thorac Oncol 2015;10:951)
- NUT immunohistochemistry can help differentiate (Virchows Arch 2021;478:21)
- Ewing sarcoma:
- Occasional positivity for CD99 in NUT carcinoma is a pitfall (Cancer Biol Ther 2019;20:150)
- Ewing sarcomas express NKX2.2 by immunohistochemistry and harbor EWSR1 gene rearrangements (Am J Surg Pathol 2012;36:993, Cancer Genet 2011;204:351)
- Adamantinoma of bone:
- Caution needed when assessing skeletal metastatic lesions (J Clin Oncol 2014;32:e57)
- Adamantinoma of bone almost exclusively arises in the tibia and contains fibro-osseous stroma in addition to epithelial elements; tumor cells harbor EPHB4::MARCH10 gene fusion (Am J Surg Pathol 2019;43:965)
- Mediastinal germ cell tumor:
- Elevated serum alpha fetoprotein is a potential pitfall (BMC Cancer 2016;16:895)
- NUT carcinoma with germ cell-like phenotype has been described in case with ZNF532::NUTM1 gene fusion (Am J Surg Pathol 2022;46:281)
- Immunohistochemistry for NUT protein and molecular pathology for NUT fusions can aid in the differential diagnosis from germ cell tumors (Am J Surg Pathol 2022;46:281)
- Desmoplastic round cell tumor (Lung Cancer 2015;90:484):
- Positive for desmin and WT1 C terminus (Arch Pathol Lab Med 2006;130:728, Am J Surg Pathol 2014;38:1220)
- Harbors EWSR1::WT1 gene fusion (Semin Cancer Biol 2005;15:197)
- Diffuse large B cell lymphoma (Lung Cancer 2015;90:484):
- Positive immunostains for B cell markers and further subclassification by the Hans algorithm (Blood 2004;103:275)
- Porocarcinoma:
- Porocarcinomas may show NUT immunopositivity because of underlying YAP1::NUT fusion (J Cutan Pathol 2021;48:403)
Board review style question #1
A 36 year old man presents with cough and shortness of breath and is diagnosed with a large mediastinal mass and undergoes open surgical biopsy. A low power hematoxylin and eosin microscopic picture is shown above. If the mass undergoes genetic testing, which of the following is the most likely finding?
- BRD4::NUT fusion transcript
- Isochromosome 12p
- MYC amplification
- SMARCA4 point mutation
Board review style answer #1
A. BRD4::NUT fusion transcript
BRD4::NUT fusion transcript is detected in 70% of NUT carcinomas. Answer B is incorrect because isochromosome 12p is a common finding in mediastinal germ cell tumors. Answer C is incorrect: although MYC is overexpressed in NUT carcinoma, this is because it is downstream in the BRD4::NUT fusion transcript cascade and not because of gene amplification. Answer D is incorrect because SMARCA4 point mutations are frequent in SMARCA4 deficient thoracic tumors (Cancer Genet Cytogenet 2010;203:16, Histopathology 2021;78:593, Oncogene 2014;33:1736, Virchows Arch 2021;478:21).
Comment Here
Reference: NUT carcinoma
BRD4::NUT fusion transcript is detected in 70% of NUT carcinomas. Answer B is incorrect because isochromosome 12p is a common finding in mediastinal germ cell tumors. Answer C is incorrect: although MYC is overexpressed in NUT carcinoma, this is because it is downstream in the BRD4::NUT fusion transcript cascade and not because of gene amplification. Answer D is incorrect because SMARCA4 point mutations are frequent in SMARCA4 deficient thoracic tumors (Cancer Genet Cytogenet 2010;203:16, Histopathology 2021;78:593, Oncogene 2014;33:1736, Virchows Arch 2021;478:21).
Comment Here
Reference: NUT carcinoma
Board review style question #2
A 42 year old woman presents with hemoptysis and bone pain. Imaging reveals a right hilar pulmonary mass and multiple lytic bone lesions. The patient mentions a history of facial nodule removed a year ago. Biopsy of a bone lesion reveals metastatic carcinoma with monomorphous morphology and foci of abrupt keratinization. Immunohistochemistry shows nuclear positivity for NUT protein. Which of the following genetic findings would make the diagnosis of NUT carcinoma more likely?
- Detection of YAP1::NUT fusion transcript
- Positive break apart NUT FISH
- Presence of a complex karyotype
- Wild type TP53 gene
Board review style answer #2
B. Positive break apart NUT FISH
Although rare NUT fusions are nondetectable by FISH, the combination of this finding with a positive NUT immunostain has high sensitivity and specificity for diagnosing NUT carcinoma. Answer A is incorrect because a YAP1::NUT fusion, along with the patients reported history of facial nodule would be consistent with the diagnosis of porocarcinoma rather than NUT carcinoma. Answer C is incorrect because most NUT carcinomas have noncomplex karyotypes, with the only finding being a t(15;19) reciprocal translocation. Answer D is incorrect because TP53 is frequently mutated in NUT carcinoma (Lung Cancer 2015;90:484, J Cutan Pathol 2021;48:403, Pathol Int 2018;68:583, Cancer Med 2021;10:5757).
Comment Here
Reference: NUT carcinoma
Although rare NUT fusions are nondetectable by FISH, the combination of this finding with a positive NUT immunostain has high sensitivity and specificity for diagnosing NUT carcinoma. Answer A is incorrect because a YAP1::NUT fusion, along with the patients reported history of facial nodule would be consistent with the diagnosis of porocarcinoma rather than NUT carcinoma. Answer C is incorrect because most NUT carcinomas have noncomplex karyotypes, with the only finding being a t(15;19) reciprocal translocation. Answer D is incorrect because TP53 is frequently mutated in NUT carcinoma (Lung Cancer 2015;90:484, J Cutan Pathol 2021;48:403, Pathol Int 2018;68:583, Cancer Med 2021;10:5757).
Comment Here
Reference: NUT carcinoma