Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Molecular / cytogenetics images | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Javeed S, Anjum S, Ahmed A. Cemento-ossifying fibroma / ossifying fibroma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/mandiblemaxillaossifyingfibroma.html. Accessed January 16th, 2025.
Definition / general
- Benign fibro-osseous neoplasm (J Maxillofac Oral Surg 2021;20:240, Oral Dis 2017;23:440, Head Neck Pathol 2020;14:70, J Stomatol Oral Maxillofac Surg 2022;123:364)
- Origin is controversial but is mostly odontogenic in origin and usually arises in jaw (J Maxillofac Oral Surg 2021;20:240, Head Neck Pathol 2022;16:248)
- Characterized by production of bone and cementum-like calcifications in a fibrous stroma
- Usually located in the mandible during third to fourth decade of life (Oral Dis 2017;23:440, Head Neck Pathol 2020;14:70, J Stomatol Oral Maxillofac Surg 2022;123:364)
Essential features
- Cemento-ossifying fibroma (COF) is a fibro-osseous lesion characterized by varied patterns of bone formation in a fibroblastic stroma (Head Neck Pathol 2022;16:991)
- Putatively benign lesion with very rare malignant transformation or metastasis (Head Neck Pathol 2022;16:991, Ear Nose Throat J 2023;102:24)
- Cemento-ossifying fibroma is named because of its usual location in the tooth bearing region of the jaw
Terminology
- Ossifying fibroma, conventional type; cemento-ossifying fibroma; ossifying fibroma; conventional ossifying fibroma; cementifying fibroma
ICD coding
- ICD-O: 9274/0 - cemento-ossifying fibroma
Epidemiology
- Rare lesion that occurs over a broad age range, with peak incidence in third to fourth decade of life (Oral Dis 2017;23:440, Head Neck Pathol 2020;14:70, J Stomatol Oral Maxillofac Surg 2022;123:364)
- Has female predilection (F:M = 5:1)
- Tumor is more prevalent in White people than Black people (Oral Dis 2017;23:440)
Sites
- Mandible is most common, followed by the maxilla
- Mandibular premolar and molar area have more predilection (Head Neck Pathol 2020;14:70)
- Maxillary lesions tend to involve antrum and canine fossa
- Cemento-ossifying fibroma can be classified according to site of origin as (Int J Surg Case Rep 2020;68:257)
- Soft tissue counterpart is referred to as peripheral cemento-ossifying fibroma (PCOF) (Int J Surg Case Rep 2020;68:257)
- Central cemento-ossifying fibroma (CCOF) arises from cells of periodontal ligament in the apical area (Int J Surg Case Rep 2020;68:257)
Pathophysiology
- Multiple cemento-ossifying fibromas rarely show syndromic / inherited association and usually present at a younger age (Case Rep Dent 2023;2023:4664619)
- Hyperparathyroidism jaw tumor syndrome (HPT JT): rare autosomal dominant disease caused by mutation of the tumor suppressor gene CDC73 that encodes for parafibromin resulting in premature truncation of parafibromin protein product; the syndrome predisposes to a triad occurrence: multiple maxillary or mandibular cemento-ossifying fibroma, parathyroid adenoma or carcinoma and renal and uterine tumors (Int J Surg Case Rep 2020;68:257)
Etiology
- Origin of cemento-ossifying fibroma has been suggested as odontogenic or from periodontal ligament progenitor cells (J Maxillofac Oral Surg 2021;20:240)
- Origin of nonodontogenic lesions of similar histology arising from craniofacial bone outside the jaw is unclear (Head Neck Pathol 2022;16:257)
- Periodontal membrane has multipotent cells capable of forming cementum, lamellar bone and fibrous tissue (J Maxillofac Oral Surg 2021;20:240)
- Lesion can present as a component of hyperparathyroidism jaw tumor syndrome; 25 - 50% of patients of this syndrome develop cemento-ossifying fibroma of the jaws with the mandible as a favored site (Case Rep Dent 2023;2023:4664619, J Dent Sci 2020;15:426)
Clinical features
- Smaller lesions are asymptomatic
- Larger / solitary lesions present as painless swelling that causes jaw expansion, facial asymmetry, tooth divergence (Heliyon 2021;7:e07594)
- Grows slowly but can reach a considerable size if left untreated (Head Neck Pathol 2020;14:70)
- Extension to the nasal septum, orbital floor and infraorbital foramen can be seen in larger lesions; rarely associated with the destruction of extraosseous soft tissue components (Heliyon 2021;7:e07594)
- Juvenile variant of lesion occurring at a young age is clinically aggressive and highly recurrent (Heliyon 2021;7:e07594, J Maxillofac Oral Surg 2021;20:240)
Diagnosis
- Diagnosis dependent on clinical, radiologic and pathologic correlation (J Maxillofac Oral Surg 2021;20:240)
Laboratory
- No specific laboratory tests are available
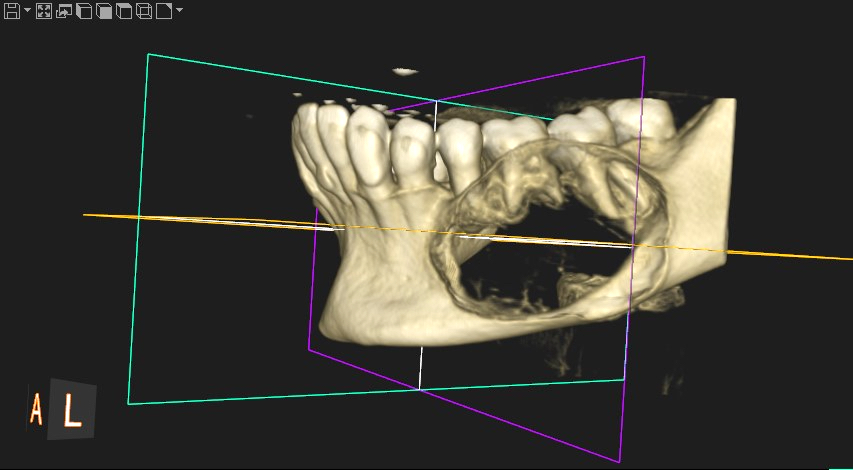
Radiology description
- Radiological findings vary according to maturity of lesion; early lesions show well defined corticated radiolucency and over time, lesion becomes progressively more radiopaque (Heliyon 2021;7:e07594, BMJ Case Rep 2020;13:e239286)
- Well circumscribed, unilocular lesion with centrifugal pattern of growth (Heliyon 2021;7:e07594)
- Can present as lesion with well defined sclerotic borders and is predominantly unilocular (BMJ Case Rep 2020;13:e239286)
- Larger lesions show expansion, thinning and perforation of buccal and lingual cortex and involvement of the lower border of mandible (BMJ Case Rep 2020;13:e239286)
Radiology images
Prognostic factors
- Slow growing, benign neoplasm with no recurrence in majority of cases
- Malignant transformation has been reported in a single case (Ear Nose Throat J 2023;102:24)
Case reports
- 19 year old woman with a large maxillary cemento-ossifying fibroma superimposed with solitary bone cyst (Int J Surg Case Rep 2020;68:257)
- 30 year old man with multiple cemento-ossifying fibromas (Case Rep Dent 2023;2023:4664619)
- 45 year old man with large cemento-ossifying fibroma of the mandible involving the infratemporal and parapharyngeal spaces (Heliyon 2021;7:e07594)
Treatment
- Treated by enucleation and curettage as it shells out easily and recurs rarely (J Maxillofac Oral Surg 2021;20:240)
- Untreated tumors can attain a massive size and rarely require en bloc resection (J Maxillofac Oral Surg 2021;20:240)
Clinical images
Gross description
- Well circumscribed tumor that can be shelled out easily in one piece
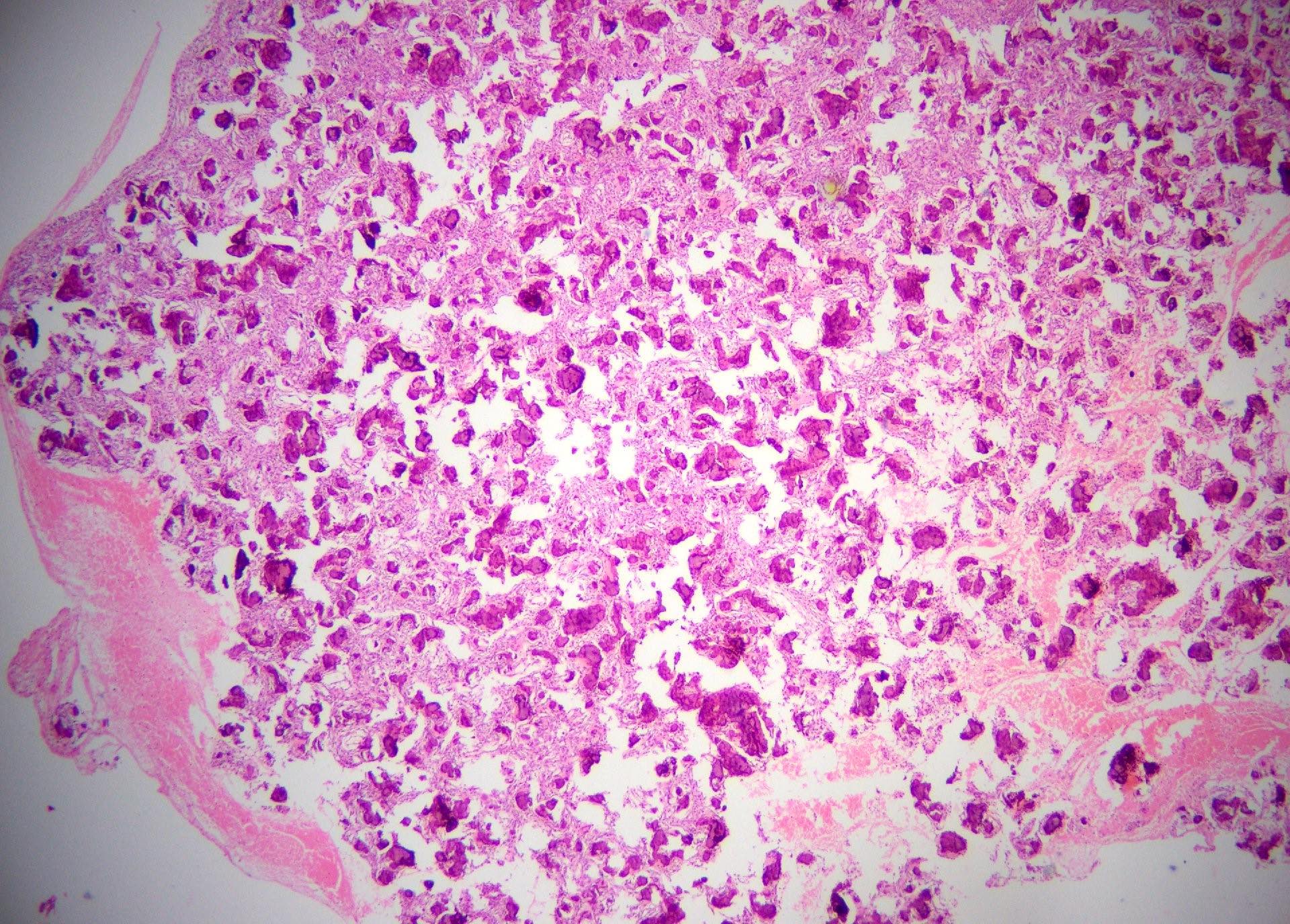
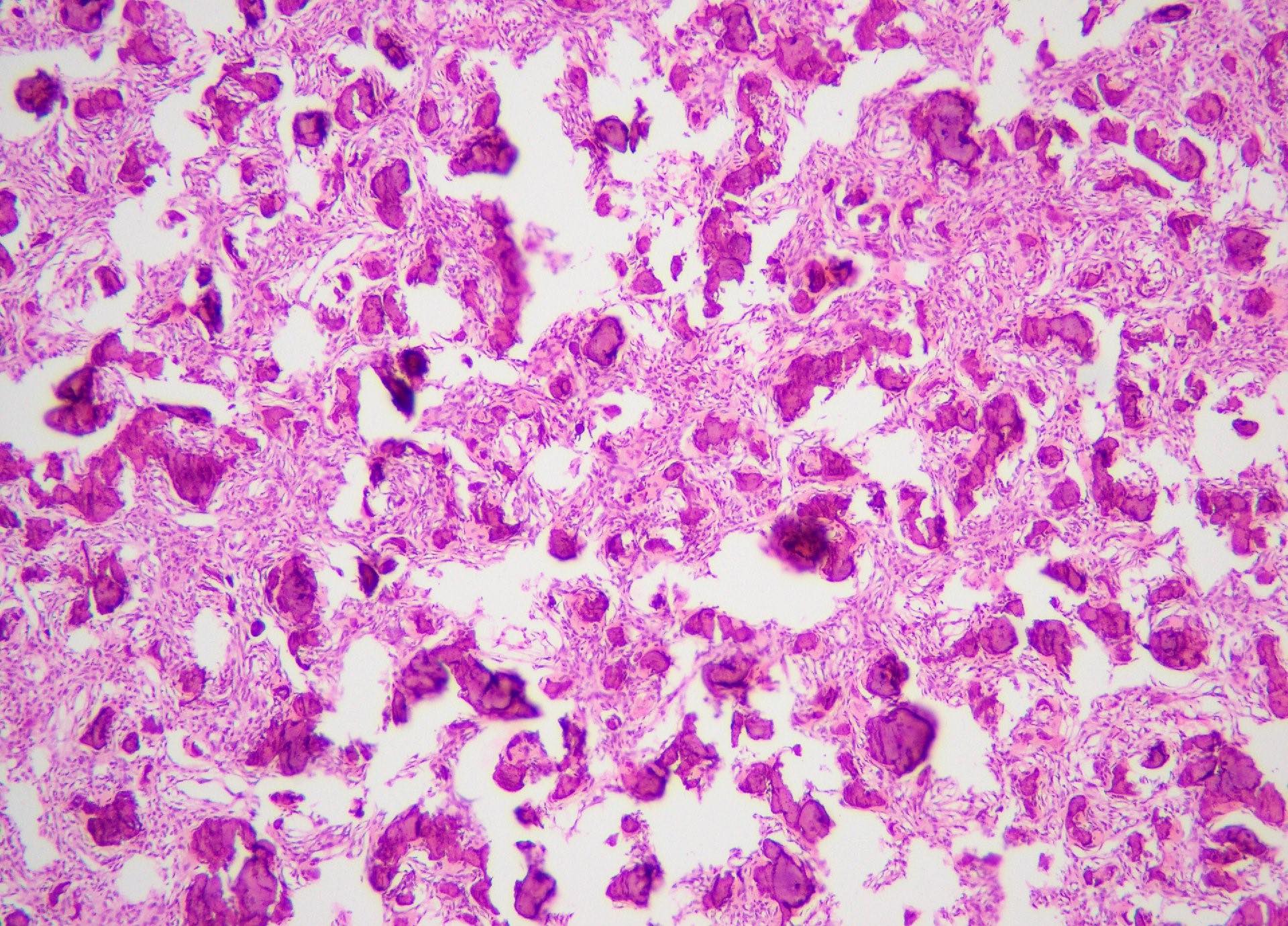
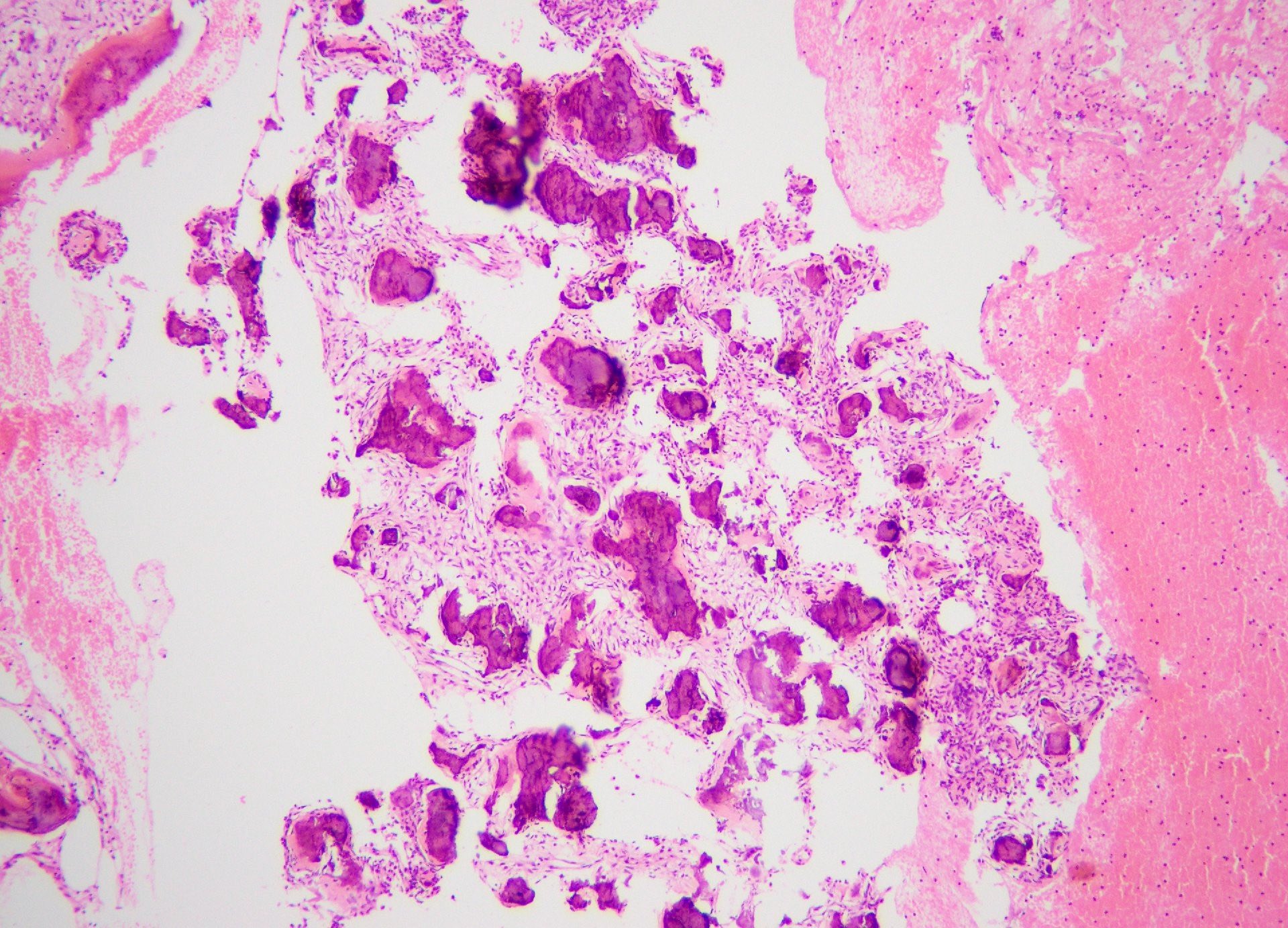
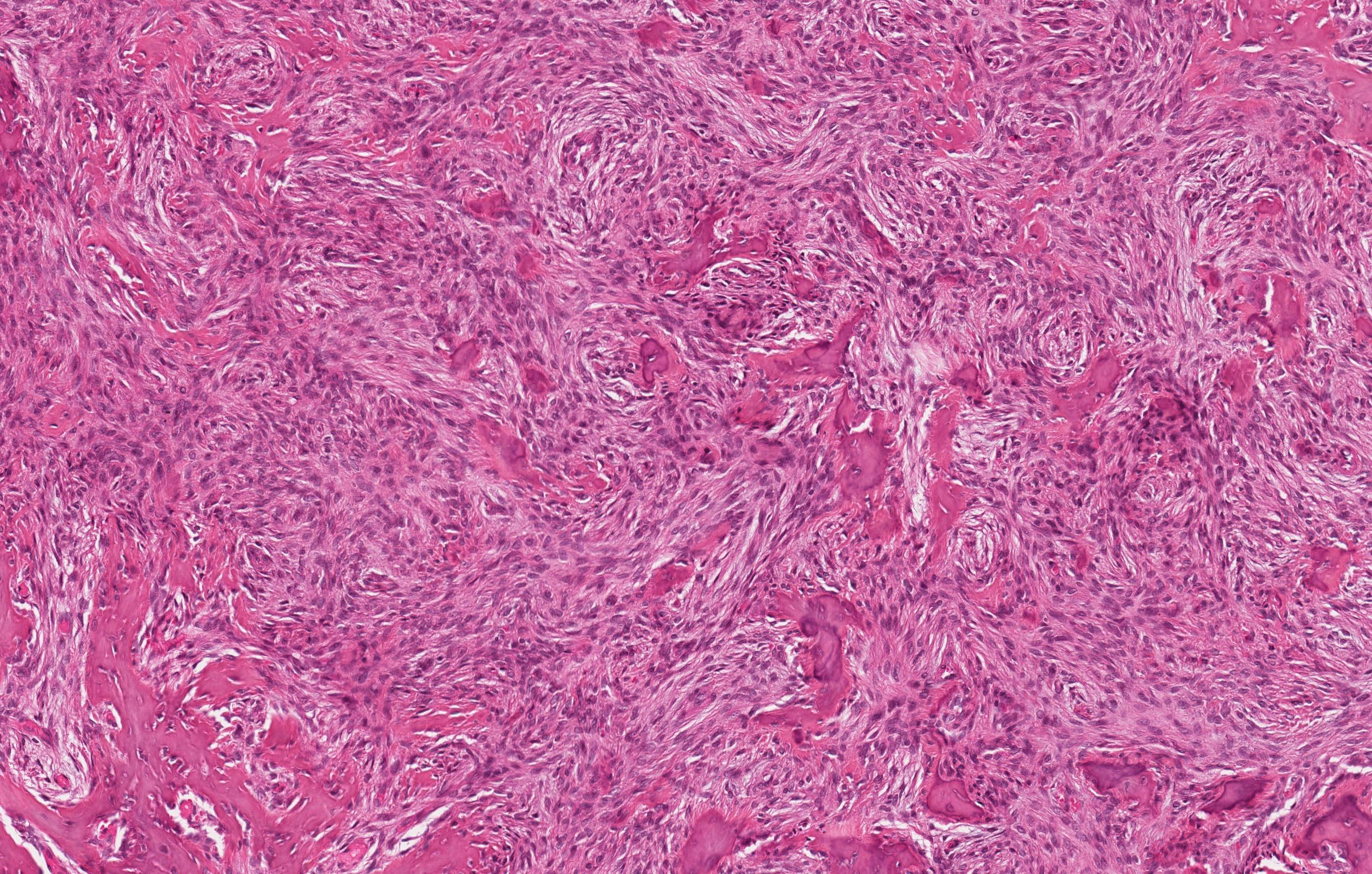
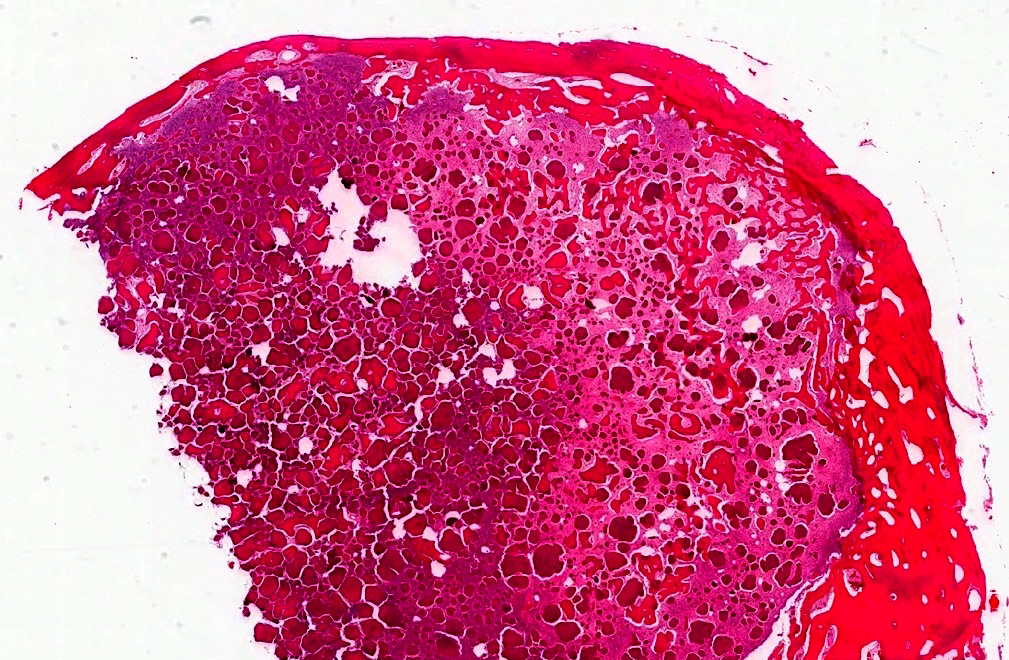
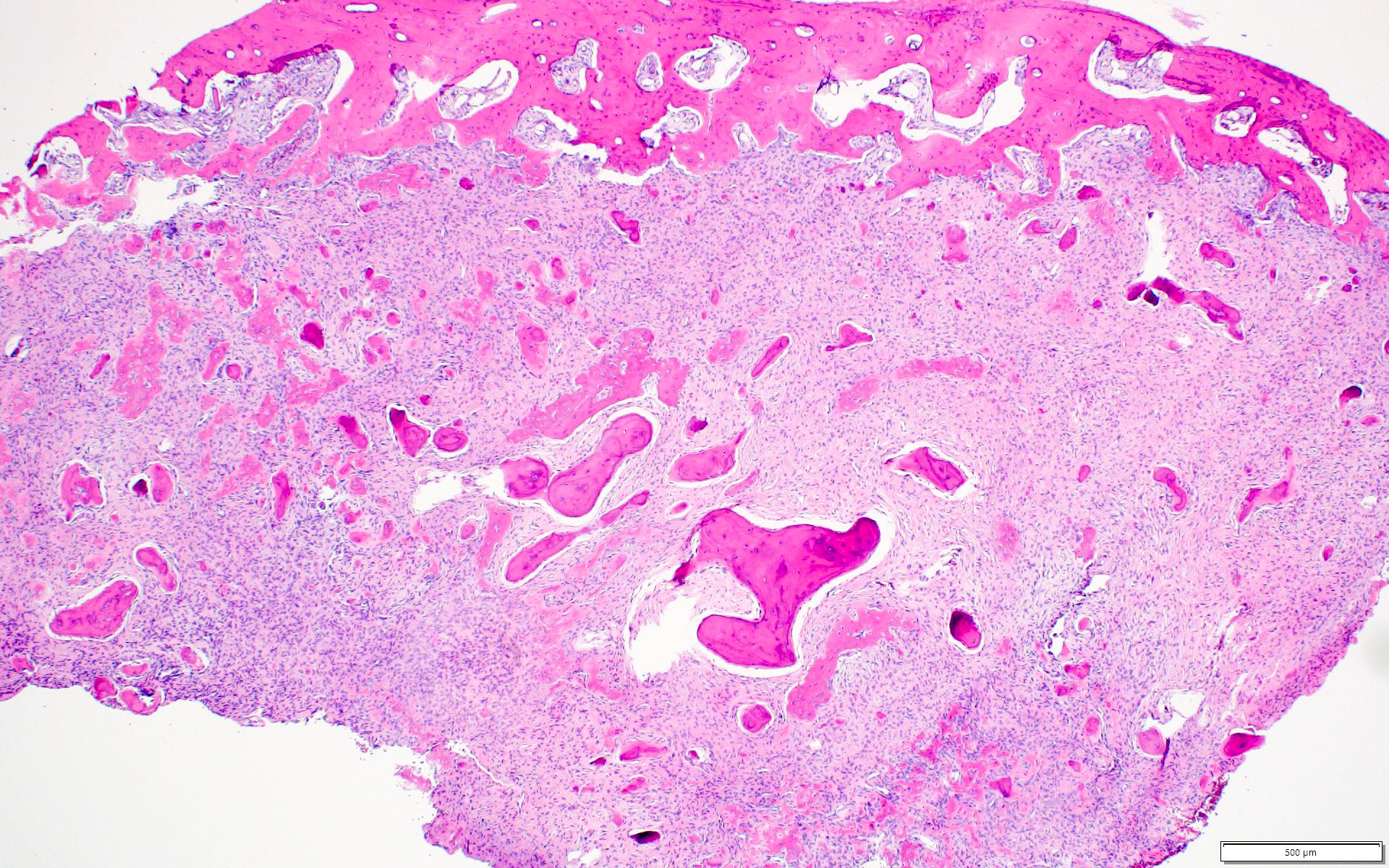
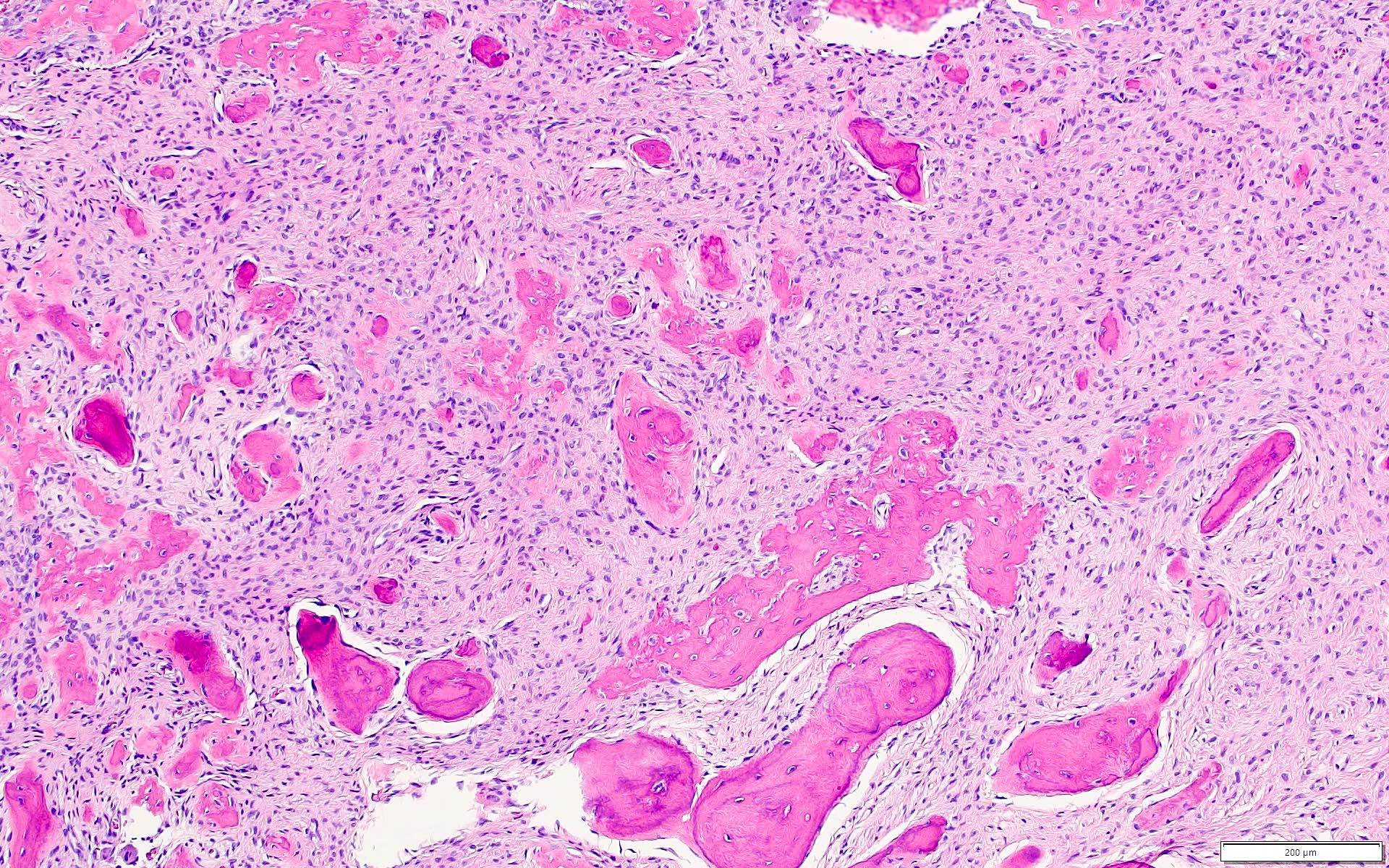
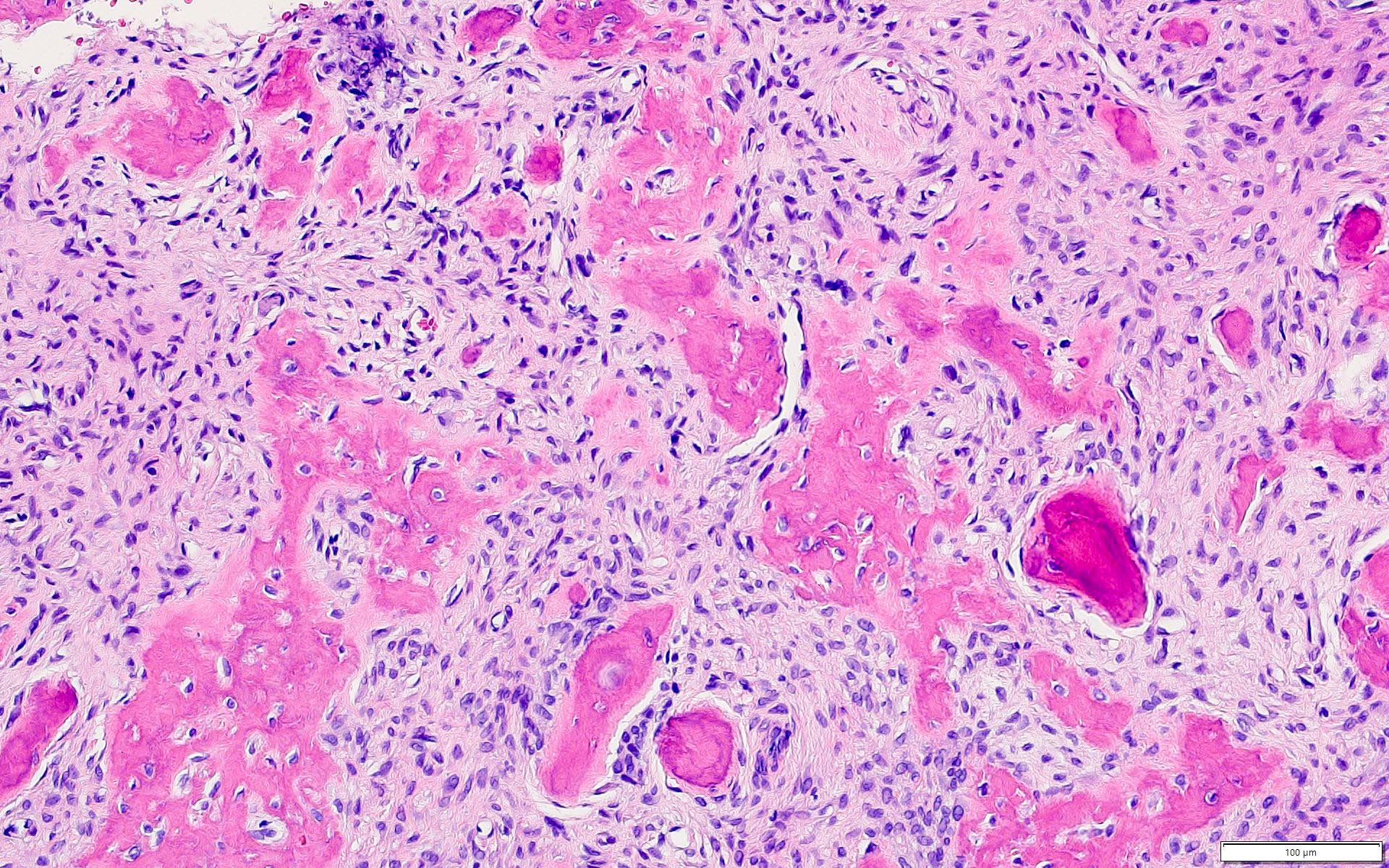
Microscopic (histologic) description
- Well defined lesion; may have thin fibrous capsule
- Well demarcated margin from surrounding normal bone
- Lesion consists of variable proportion of fibrous and mineralized tissue, more heavily mineralized centrally; it shows variation in the amount and type of mineralization, even within a single lesion
- Osteoblastic rimming of bone trabeculae is frequent (J Stomatol Oral Maxillofac Surg 2022;123:364)
- Stroma is fibroblastic with areas of hypercellularity and nuclear hyperchromasia
- No significant atypia and mitoses are infrequent (Head Neck Pathol 2020;14:70)
- Woven to lamellar bone, osteoid and dense acellular or paucicellular basophilic rounded cementum-like calcifications may all be present (Head Neck Pathol 2020;14:70)
- Bony trabeculae may form thick anastomosing strands or fuse into large sheets centrally
- Hemorrhagic cystic degeneration, resembling aneurysmal bone cyst formation, is more often found in juvenile active ossifying fibromas but has been reported in rare COFs (J Stomatol Oral Maxillofac Surg 2022;123:364, Head Neck Pathol 2022;16:248)
- Areas resembling cemento-ossifying fibroma may be seen in psammomatoid and trabecular ossifying fibroma; cemento-ossifying fibroma may contain ossicles like psammomatoid ossifying fibroma
- Cemento-ossifying fibroma with syndromic association has histology similar to that of nonsyndromic cemento-ossifying fibroma
- Cemento-ossifying fibroma in gnathodiaphyseal dysplasia is at the more fibrous end of spectrum with predominantly basophilic rounded islands and droplets of acellular bone (Head Neck Pathol 2014;8:432)
Microscopic (histologic) images
Contributed by Saira Javeed, M.B.B.S., M.Phil., Kelly Magliocca, D.D.S., M.P.H. and Molly Housley Smith, D.M.D.
Positive stains
- Cemento-ossifying fibromas showed significant immune reactivity for keratan sulphate (IHC is not necessary for diagnosis) (J Maxillofac Oral Surg 2021;20:240)
Negative stains
- p53 (J Clin Exp Dent 2022;14:e27)
- MDM2 (25%) and CDK4 (2%) can be seen in a subset of cases but is typically focal (≤ 10% of nuclear staining) (Head Neck Pathol 2022;16:991)
Molecular / cytogenetics description
- None for sporadic cemento-ossifying fibroma
- Syndromic cemento-ossifying fibroma can be identified clinically or by genetic mutations in CDC73 (also known as HRPT2) (J Dent Sci 2020;15:426, Case Rep Dent 2023;2023:4664619)
- Multiple ossifying fibromas can be associated with hyperparathyroidism jaw tumor syndrome (Case Rep Dent 2023;2023:4664619, J Dent Sci 2020;15:426)
- Amplification of MDM2 gene by fluorescence in situ hybridization is rarely (3%) seen in ossifying fibroma (Head Neck Pathol 2022;16:991)
- Positive MDM2 amplification in craniofacial fibro-osseous lesion does not completely exclude ossifying fibroma; however, it should still raise concern for low grade osteosarcoma because this genetic event is much more common in the latter (Head Neck Pathol 2022;16:991)
Molecular / cytogenetics images
Sample pathology report
- Mandible, enucleation and curettage:
- Benign fibro-osseous neoplasm consistent with cemento-ossifying fibroma / ossifying fibroma (see comment)
- Comment: This is a benign fibro-osseous neoplasm that requires clinical and radiological correlation.
Differential diagnosis
- Peripheral ossifying fibroma (Int J Health Sci (Qassim) 2019;13:63, Med Oral Patol Oral Cir Bucal 2022;27:e460):
- Reactive, inflammatory, hyperplastic growth of the gingiva
- It is the soft tissue counterpart to COF; microscopically, it is lined by mucosa and can have identical microscopic appearance
- Cemento-osseous dysplasia:
- Nonneoplastic fibro-osseous lesion of tooth bearing regions
- Most common benign fibro-osseous lesion of jaws, affects middle aged women
- Patients can be managed with follow up and symptomatic treatment
- Radiology: radiolucent, radiodense or mixed, as the lesion matures becomes more radiodense and calcified
- Grossly usually received in multiple gritty fragments with tan brown color
- Microscopically identical to COF
- Unencapsulated with variable cellular fibrous stroma and areas of loose collagen
- Stroma can display osteoid, bone and cementum-like material
- Mature lesion shows more calcification
- Clinical and radiographic correlation is essential to differentiate the two, especially on incisional biopsies
- An expansile variant of cemento-osseous dysplasia exists and can mimic COFs
- Chronic osteomyelitis (Head Neck Pathol 2020;14:842):
- Inflammatory process with a history of trauma and sinus formation
- No age or gender preference
- Treatment includes surgery to remove portions of bone that are infected or dead, followed by intravenous antibiotics given in the hospital
- Microscopically: findings are nonspecific, such as chronic inflammatory cell infiltration, bone marrow fibrosis and sclerotic bone formation
- Desmoplastic fibroma:
- Locally aggressive fibroblastic lesion of bone
- Mostly affects mandible in people younger than 30 (mean: 16 years), no gender predilection
- Excision, recurrence is common
- Radiology: well defined without mineralization
- Grossly: firm, tan-white with rough cut surface, myxoid areas can be seen
- Microscopically
- Infiltrative lesion comprising fascicles of uniform myofibroblasts / fibroblasts having tapering nuclei in a collagenous to myxoid stroma
- Perivascular edema and mitotic figures are present
- Overt bony trabeculae or droplets absent
- IHC: alpha smooth muscle actin (ASMA) and beta catenin positive in some cases
- Associated with activating CTNNB1 gene / APC mutation
- Fibrous dysplasia:
- Skeletal anomaly, a disorder of growing bones
- Monostotic or polyostotic lesion, affects craniofacial bones and femur in children and adolescents, no gender predilection
- Lesions stabilize with skeletal maturation, surgical intervention in younger patients is delayed
- Radiology: radiolucent to sclerotic, ground glass appearance with indistinct borders
- Grossly: affected bone is rubbery, compressible with gritty texture
- Microscopically
- Has bland hypocellular appearance if the lesion is mature; can be hypercellular when the lesion is in actively growing phase
- Lesion fuses with adjacent normal bone
- Irregularly shaped trabeculae of bone in a background fibrous stroma
- Trabeculae of woven bone are elongated and curvilinear, described as Chinese characters or letters in alphabet soup
- Osteoblastic rimming absent or minimal
- Retraction artifact / peritrabecular clefting often present
- Associated with GNAS gene mutation and McCune-Albright syndrome
- Intraosseous meningioma (Surg Neurol Int 2021;12:485):
- Most common benign brain / intracranial tumors, however, intraosseous meningiomas are rare lesions accounting for < 1% of intracranial meningiomas
- Common locations are frontoparietal and orbital regions
- Surgical removal though challenging is curative
- Radiology: depending upon location, usually circumscribed with surrounding bone shell
- Microscopically: morphology is similar to dura based lesions
- Osteoblastoma:
- Benign bone forming tumor
- Rare lesion, mostly affects craniofacial bones specially mandible in people in second to third decade with slight male predominance
- Can be excised however recurrences are reported after incomplete removal
- Radiology: circumscribed rounded of usually > 20 mm in size, radiolucent to radiopaque, sclerotic border; can mimic malignancy
- Grossly: multiple firm tan-white fragments
- Microscopically
- Lesion is composed of haphazard mineralized trabeculae of bone showing prominent osteoblastic rimming, lying in cellular fibrous stroma
- Rare mitotic figures
- Osteosarcoma (J Cancer Res Ther 2018;14:471):
- Malignant bone tumor
- Greatest predilection for the metaphysis (femur and tibia), osteosarcoma of craniofacial bones is infrequent
- Osteosarcoma of the jaws are rare and comprise ~7% of all osteosarcoma cases
- Radiology: irregular mixed radiolucent radiopaque pattern with infiltrative margins
- Microscopically: displays features commonly found in various types of malignant neoplasms
- Reference: J Maxillofac Oral Surg 2021;20:240
Additional references
Board review style question #1
The histologic pattern shown above is from a 32 year old woman who has had small swelling in the mandible for the last 2 weeks. On radiology, the lesion was found to be well circumscribed. What is the most expected behavior of this lesion?
- Benign
- Intermediate, locally aggressive
- Intermediate, rarely metastasizing
- Malignant
Board review style answer #1
A. Benign. This is a slow growing, benign neoplasm with no recurrence in most cases (J Maxillofac Oral Surg 2021;20:240, Oral Dis 2017;23:440, Head Neck Pathol 2020;14:70, J Stomatol Oral Maxillofac Surg 2022;123:364). Answers B, C and D are incorrect because this neoplasm rarely demonstrates malignant transformation or metastasis (Head Neck Pathol 2022;16:991, Ear Nose Throat J 2023;102:24).
Comment Here
Reference: Cemento-ossifying fibroma / ossifying fibroma
Comment Here
Reference: Cemento-ossifying fibroma / ossifying fibroma
Board review style question #2
Which of the following conditions is typically associated with hyperparathyroidism jaw tumor syndrome (HPT JT)?
- Cemento-ossifying fibroma
- Odontogenic keratocyst of jaw
- Ovarian fibromas
- Pits in palms and soles
Board review style answer #2
A. Cemento-ossifying fibroma is associated with hyperparathyroidism jaw tumor syndrome. The syndrome predisposes to a triad occurrence: multiple maxillary or mandibular cemento-ossifying fibroma, parathyroid adenoma or carcinoma and renal and uterine tumors (Int J Surg Case Rep 2020;68:257). Answers B, C and D are incorrect because they are usually associated with basal cell nevus syndrome.
Comment Here
Reference: Cemento-ossifying fibroma / ossifying fibroma
Comment Here
Reference: Cemento-ossifying fibroma / ossifying fibroma