Table of Contents
See also | Definition / general | Terminology | Epidemiology | Sites | Clinical features | Diagnosis | Prognostic factors | Radiology images | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Flow cytometry description | Differential diagnosis | Additional referencesCite this page: Martinez A. Lymphoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/mandiblemaxillalymphoma.html. Accessed April 3rd, 2025.
See also
Definition / general
- More commonly non-Hodgkin lymphoma (NHL) (B or T cell); also Hodgkin lymphoma
- Primary extranodal lymphomas of the mandible and maxilla are rare
Terminology
- Also called intrabony lymphoma or primary osseous lymphoma at this site
Epidemiology
- #2 most common malignant tumor of head and neck after squamous cell carcinoma (3.5% of intra-oral malignancies)
- Mean age for extranodal lymphoma: 5th decade
- Male to female ratio for lymphoma is 1.4:1
- Approximately 16% of NHLs involve the jaw bones
- 2/3 are diffuse large B cell lymphoma (DLBCL)
- Plasmablastic lymphoma, a subtype of DLBCL, more common in the oral cavity of immunocompromised / HIV patients, can also involve the jaw, and can occur in elderly immunocompetent patients
Sites
- Most head and neck lymphomas involve Waldeyer's ring
- ~1/3 of NHLs involve Waldeyer's ring
- The mandible is the most common site for osseous lymphomas followed by the maxilla
Clinical features
- Clinically, patients can present with tooth mobility, swelling, pain or a mass
- Lymphadenopathy and B symptoms (fever, night sweats, weight loss, anorexia, fatigue, etc) can also be present
- May also present as numb chin syndrome (NCS): sensory neuropathy characterized by unilateral hypoesthesia or paresthesia over the lower lip, chin and occasionally gingival mucosa
- Most common non-hematologic cause is breast cancer
- Most common hematologic cause is NHL
Diagnosis
- May be challenging because there is usually a low index of suspicion for lymphoma
- Usually diagnosed at biopsy with flow cytometry, immunohistochemistry and molecular studies to help subclassify the lesion and to help risk stratify the patient
Prognostic factors
-
Diffuse large B cell lymphoma
- Favorable: limited disease (no or <10% marrow involvement), favorable international prognostic index
- Favorable: germinal center gene expression (bcl6+, CD10+, negative for MUM1/IRF4, negative for CD138) versus activated B cell-like profile (Am J Surg Pathol 2004;28:464)
- Unfavorable: p53 mutations present
- Unfavorable: CD10+ and bcl2+ coexpression (Am J Clin Path 2001;116:183)
- Clinical course is very aggressive with most patients dying in the first year after diagnosis
- Outcome may have improved recently due to better management of HIV
- In endemic and sporadic cases, the tumor is highly aggressive but potentially curable
- Poor prognosis if bone marrow involvement, unresected tumor >10 cm and high serum LDH
- Poor prognosis - 1 year survival if multiple lesions and no treatment, but many years if indolent
Plasmablastic lymphoma
Burkitt lymphoma
Multiple Myeloma (MM)
Radiology images
Case reports
- 10 year old boy with T cell lymphoblastic lymphoma (J Clin Diagn Res 2015;9:ZD22)
- 30 year old woman (Natl J Maxillofac Surg 2011;2:210)
- 48 year old woman with involvement of mandible by non-Hodgkin lymphoma (J Postgrad Med 1995;41:90)
- 51 year old woman with non-Hodgkin lymphoma presenting with numb chin syndrome (BMJ Case Rep 2011;2011:bcr0120113712)
- 53 year old man with diffuse large B cell lymphoma of mandible (Case Rep Oncol 2015;8:451)
Treatment
- Managed by chemotherapy, radiotherapy and surgery in various combinations
Microscopic (histologic) description
-
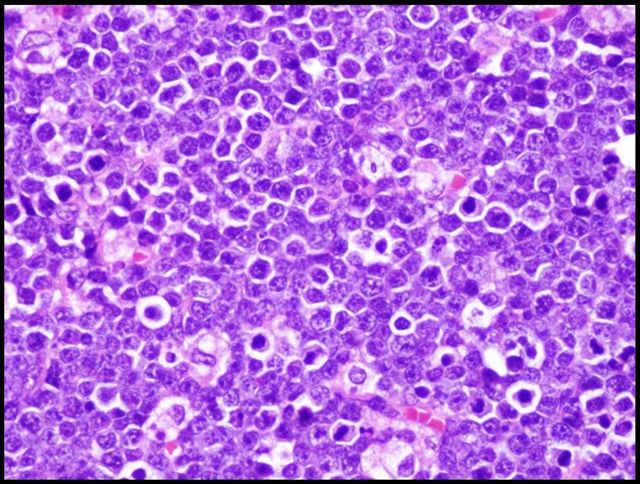
Diffuse large B cell lymphoma
- Monotonous population of large to medium sized lymphoid cells with the morphologic features of centroblasts (large noncleaved cells), immunoblasts (round nuclei with vesicular chromatin and single large nucleolus) or cells with intermediate features
- Subtype of DLBCL most commonly associated with HIV that has predilection for oral cavity
- Characterized by diffuse infiltrate of large lymphoma cells that can also have a “starry sky” pattern like Burkitt lymphoma
- The cells can be plasmacytoid with eccentric nuclei, a single, centrally located prominent nucleoli, abundant basophilic cytoplasm and a paranuclear hof
- "Starry sky" appearance composed of monotonous, medium sized lymphocytes
- The cell size approximates the nuclear size of macrophages
- A so called "squaring off" of the cytoplasm may be encountered, as the cell borders appear to abut one another
- Sheets and aggregates of plasma cells that have abundant basophilic cytoplasm, low N/C ratio, eccentrically placed nucleus with clumped "spoke wheel" or "clock face" chromatin
- The less mature plasma cells show loose reticular chromatin, prominent nucleoli, high N/C ratio
- Mott cells (blue grapelike cytoplasmic inclusions), Russell bodies (cytoplasmic, cherry red, refractive round bodies), Dutcher bodies (intranuclear crystalline rods) can also be present
Plasmablastic lymphoma
Burkitt lymphoma (BL)
Multiple myeloma
Microscopic (histologic) images
Positive stains
-
Diffuse large B cell lymphoma: CD20, CD22, CD79a, PAX5, BCL6 (~60%), CD10 (~40%), CD5 (~10%), CD30 (~10%), BCL2 (~50%)
Plasmablastic lymphoma: CD38, CD138, IRF4/MUM1, VS38c, EBV
Burkitt Lymphoma: CD10, CD19, CD20, CD22, BCL6 and CD79a
Myeloma: Kappa or lambda light chains, CD38, CD79a, CD138, CD56+/-
Negative stains
Flow cytometry description
-
Diffuse large B cell lymphoma: clonally rearranged immunoglobulin genes, BCL2 rearranged in ~20%, BCL6 rearranged in ~30%, BCL6 mutated in ~70%, MYC rearranged in <10%
- del 17p, del 13 or 13q; t(4;14)(p16.3;q32) in 25% of cases, causing increased expression of FGFR3 (fibroblast growth factor receptor 3) and IgH
- t(11;14)(q13;q32) [cyclin D1] is usually part of complex karyotype
- May be missed by routine cytogenetics, particularly if the proliferative rate is low (Am J Clin Pathol 2000;113:831)
- Hyperdiploidy and hypoploidy
Plasmablastic lymphoma: clonal IgH chain gene rearrangement
Burkitt lymphoma: IG-MYC fusions of either t(8;14)(q24;q32), t(2;8)(p12;q24), or t(8;22)(q24;q11); t(8;14) most common
Myeloma
Differential diagnosis
- Because there is usually a low index of suspicion, the differential is broad, mainly based on radiologic findings, and includes:
- Odontogenic cysts
- Benign and malignant odontogenic tumors
- Reactive / inflammatory processes related to odontogenic infection or inflammation
- Other metastases
Additional references