Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Frozen section description | Frozen section images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Positive stains | Negative stains | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Magliocca K. Odontogenic keratocyst. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/mandiblemaxillakeratocyst.html. Accessed November 27th, 2024.
Definition / general
- Odontogenic keratocyst (OKC) is a developmental odontogenic cyst that is thought to arise from dental lamina and is characterized histologically by a thin, uniform parakeratinized stratified squamous epithelial lining with a hyperchromatic basal layer of cells
Essential features
- Intraosseous origin, maxilla or mandible
- Cystic strips of nonneoplastic, nondysplastic epithelium with a fibrous cyst wall
- Epithelial lining composed of parakeratinized stratified squamous epithelium with a hyperchromatic basal cell layer
- Treatment is surgical
- With surgical enucleation, risk of recurrence is 20 - 30% (Oral Surg Oral Med Oral Pathol Oral Radiol 2019;127:282, J Maxillofac Oral Surg 2024;23:145)
Terminology
- Keratocystic odontogenic tumor (KCOT)
- Orthokeratinizing odontogenic cyst: similar name, however, this cyst is unrelated to odontogenic keratocyst
ICD coding
- ICD-11: DA05.0 - developmental odontogenic cysts
Epidemiology
- Third most common odontogenic cyst (Dentomaxillofac Radiol 2011;40:1)
- Broad age range, with peak incidence in second to third decade and second smaller peak in older age (J Craniomaxillofac Surg 2022;50:1)
- Slight male predilection (J Craniomaxillofac Surg 2022;50:1)
- Multiple simultaneous odontogenic keratocysts in the first decade of life raise concern for inherited predisposition (basal cell nevus syndrome [Gorlin syndrome and nevoid basal cell carcinoma syndrome]) (Am J Med Genet A 2011;155A:2091)
Sites
- Mandible is affected more commonly than maxilla (J Craniomaxillofac Surg 2022;50:1)
- Posterior mandible is the most common site of occurrence
Pathophysiology
- Thought to arise from dental lamina
- Involvement of the sonic hedgehog signaling pathway plays a role in the majority of cases (Am J Surg Pathol 2020;44:553)
- Mutations of the tumor suppressor gene PTCH1 (9q22.3-q31) is common in syndrome related OKCs as well as sporadic OKCs (Nat Genet 1996;12:85, Oral Dis 2019;25:1600)
Etiology
- Unknown
Clinical features
- May be small or asymptomatic, incidentally detected on radiographs taken for unrelated reasons or for imaging to investigate delayed tooth eruption (Clin Oral Investig 2023;27:6951)
- Large lesions may produce a painless bony expansion, can displace the involved tooth
- If secondarily infected, may be associated with pain and swelling (Maxillofac Plast Reconstr Surg 2014;36:73)
Diagnosis
- Histopathology supports the diagnosis
- Lesion is intraosseous (within maxilla or mandible but may extend beyond bone borders into maxillary sinus, nasal floor or submucosa to mimic a peripheral lesion)
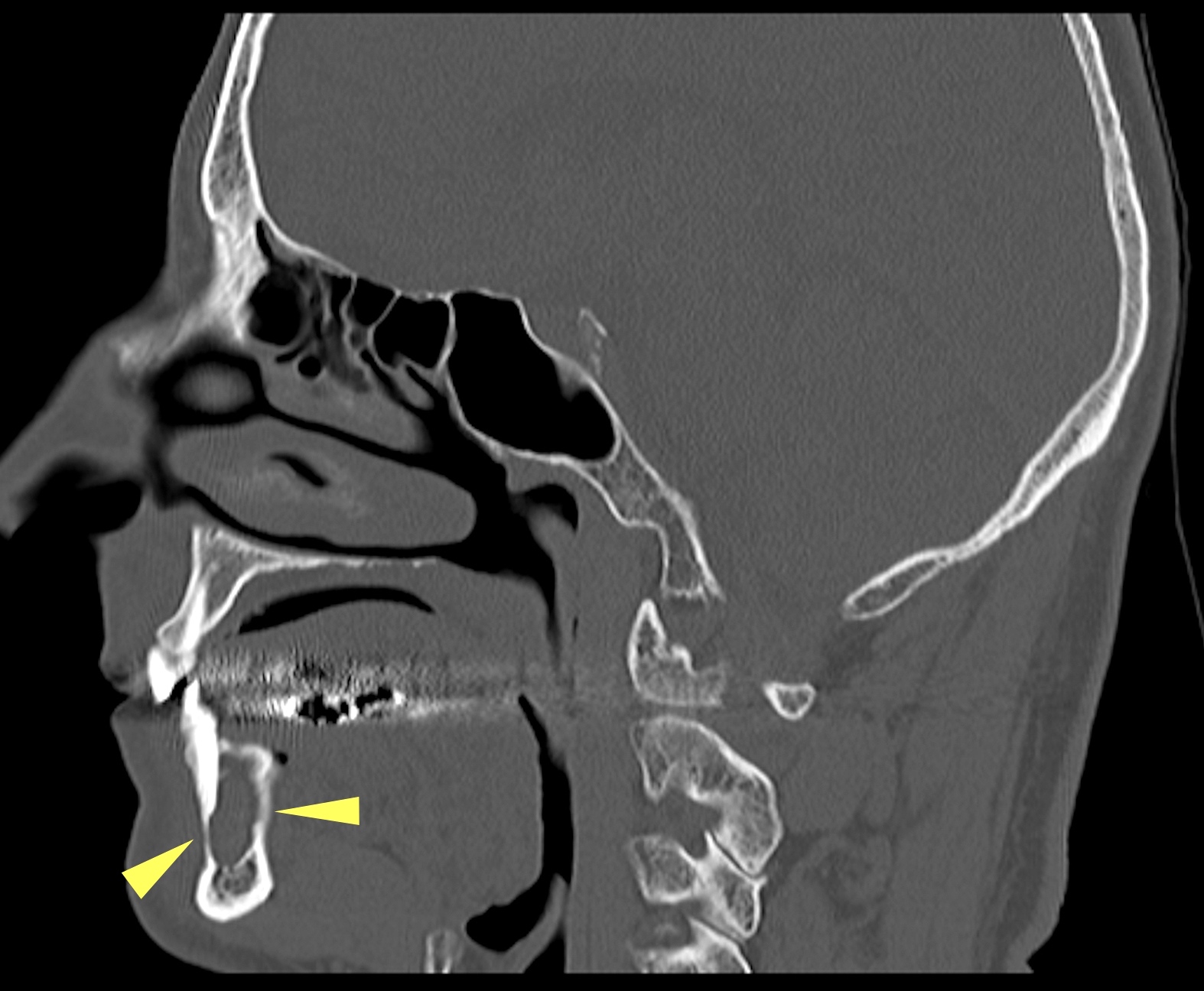
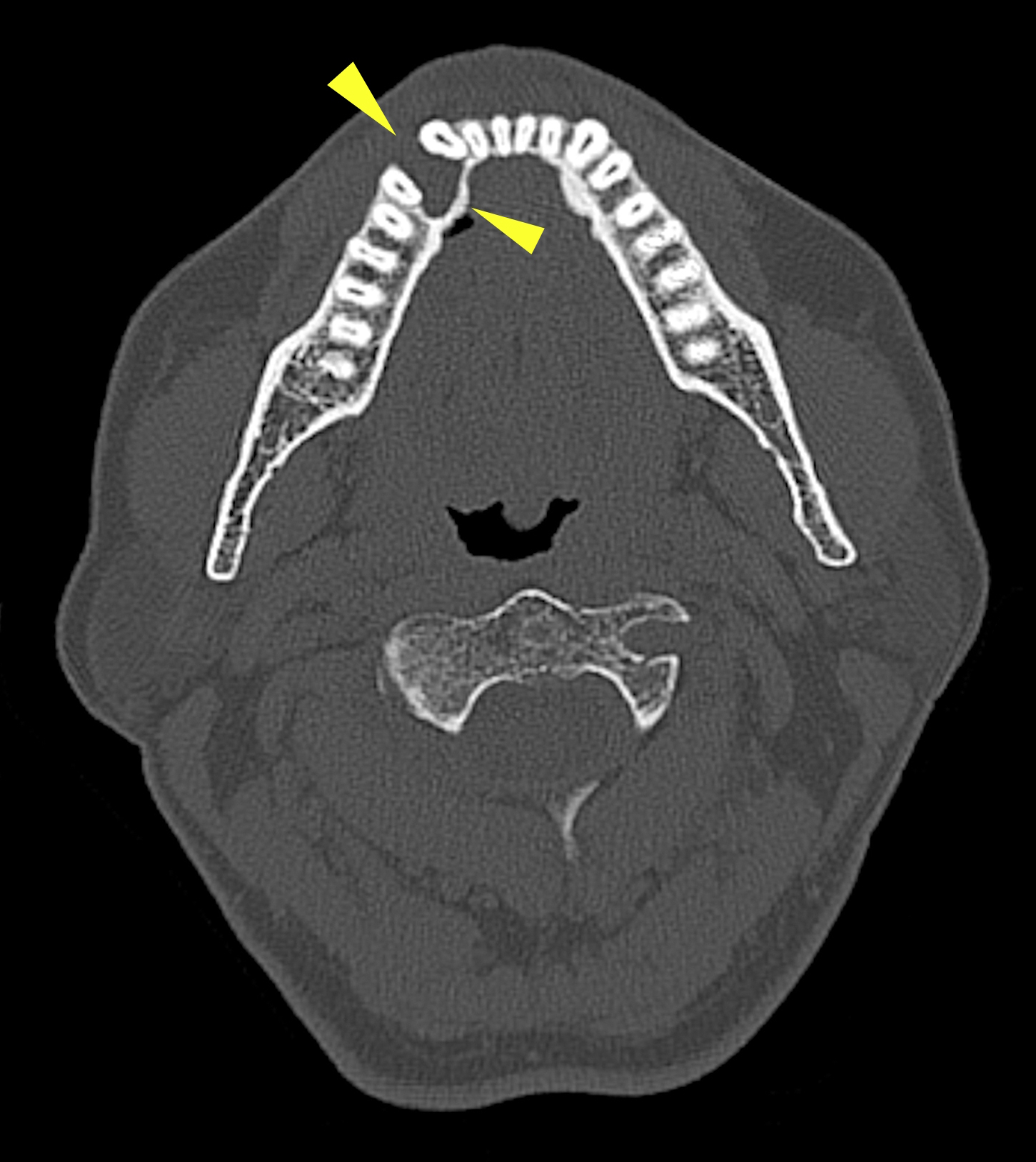
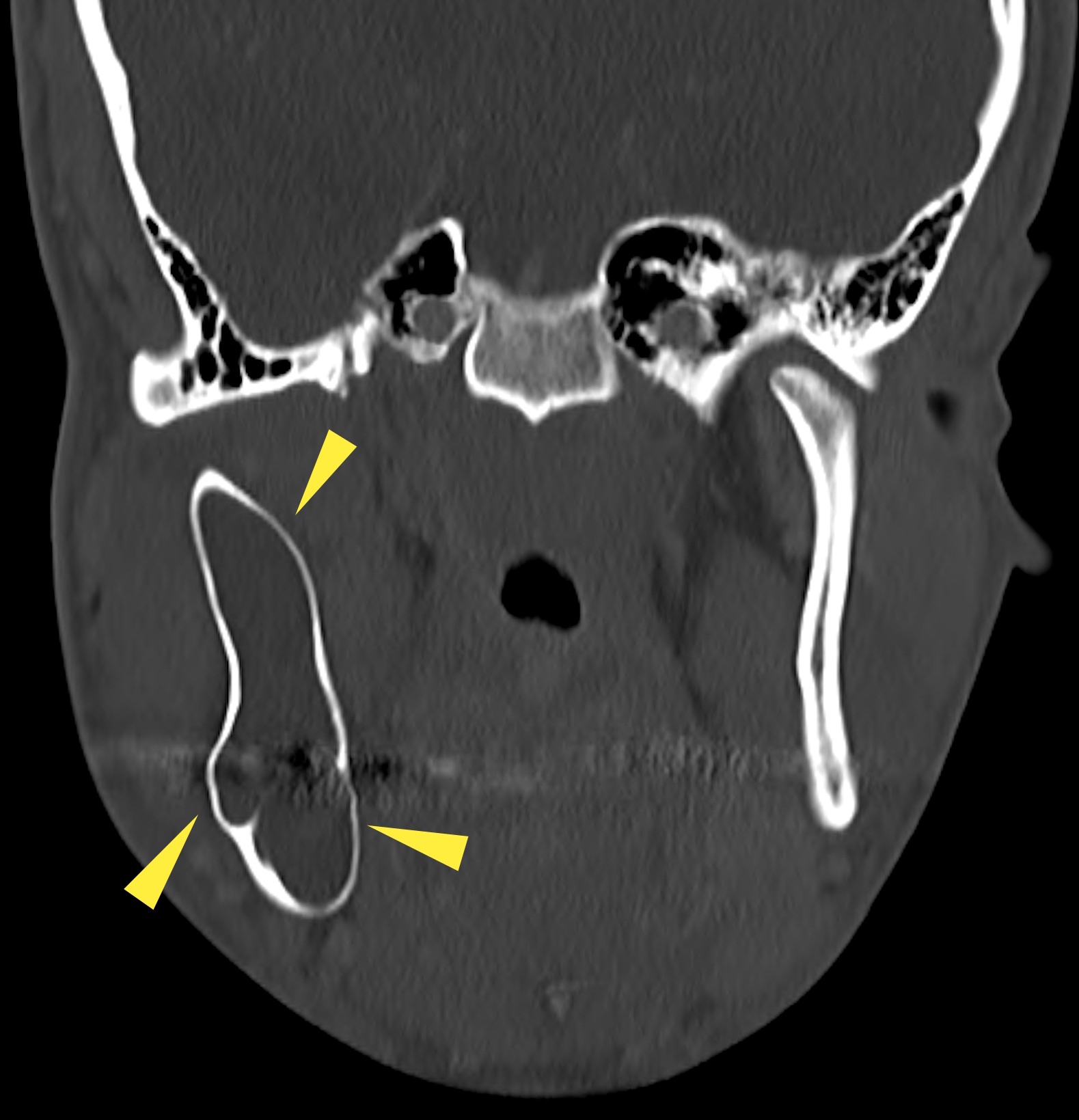
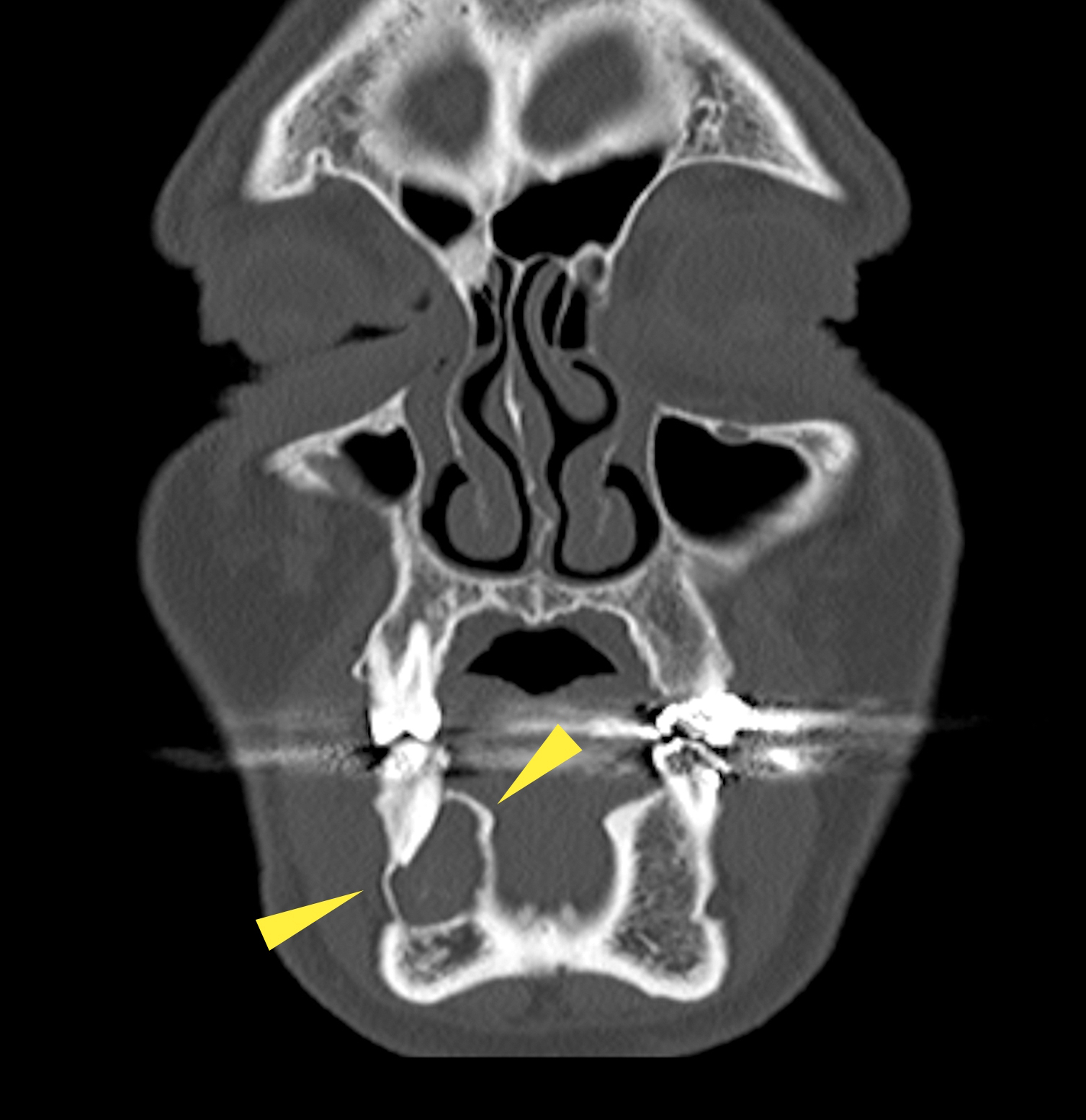
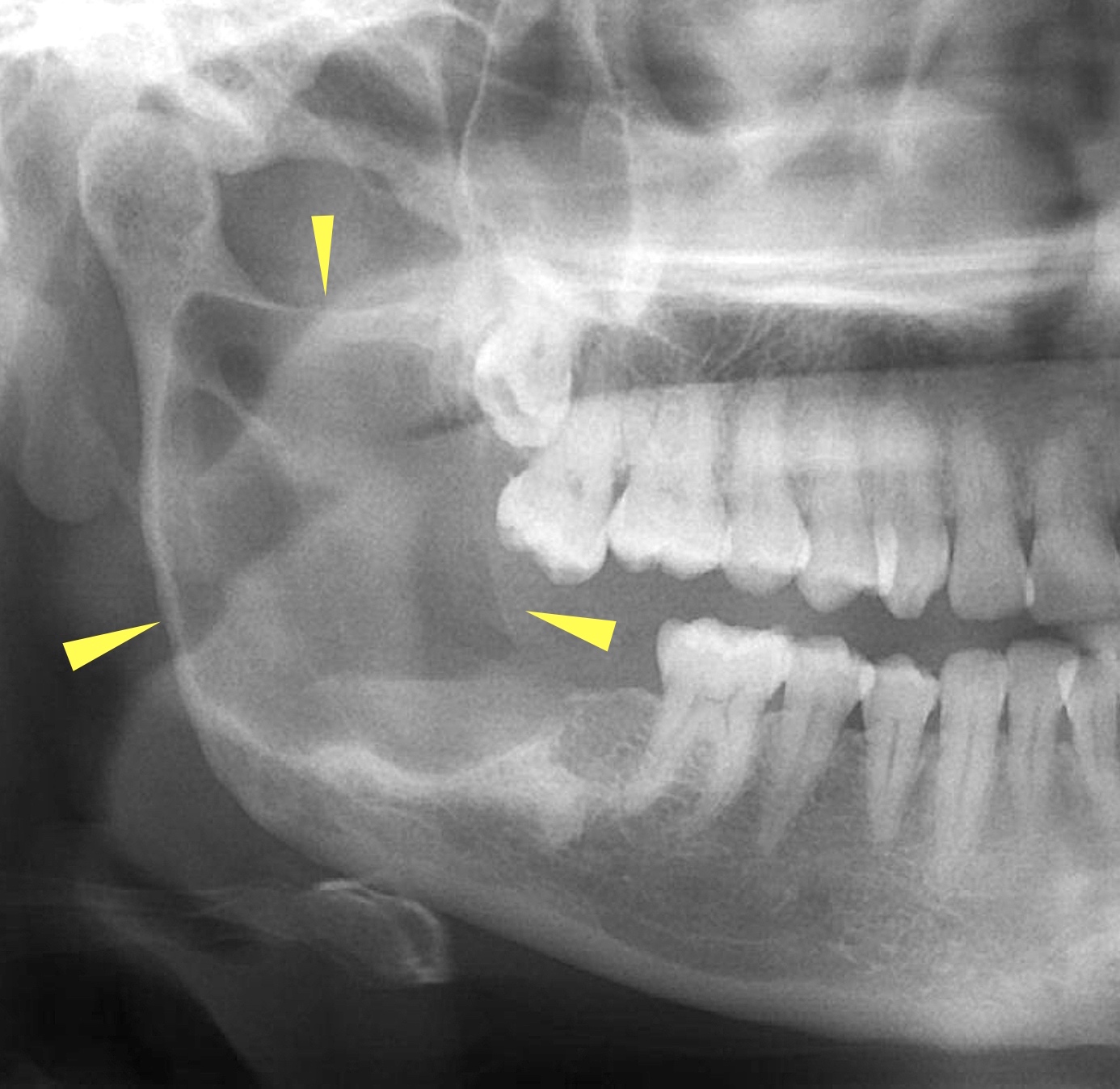
Radiology description
- Radiology is essential to identify landmarks and the extent of disease in the preoperative and follow up setting
- Panoramic radiograph (panorex), intraoral film or cross sectional imaging is useful depending on cyst location and size
- Most commonly a well defined, unilocular radiolucency on Xray
- May have sclerotic border (Dentomaxillofac Radiol 2018;47:20170288)
Radiology images
Prognostic factors
- Overall, excellent prognosis
- Recurrence rate, 20 - 40% following enucleation (J Maxillofac Oral Surg 2024;23:145)
Case reports
- 25 year old man with Lowe syndrome and multiple odontogenic keratocysts (Oral Surg Oral Med Oral Pathol Oral Radiol 2023;136:e171)
- 27 year old man with recurrent odontogenic keratocyst eroding into the floor of the orbit (Orbit 2022;41:368)
- 32 year old woman with carcinoma arising in odontogenic keratocyst (Oral Surg Oral Med Oral Pathol Oral Radiol 2015;120:e204)
Treatment
- Surgical approach varies and factors for consideration include age, maturity, skeletal maturity, anatomic position, history of local recurrence, relative importance of tooth involved (if any), size of cyst, presence of additional pathology including but not limited to pathologic fracture, risk for fracture once removed, patient preference (risk versus benefits, acceptable risk of recurrence, cosmetic and functional considerations) (J Maxillofac Oral Surg 2024;23:145)
- In small lesions, enucleation and curettage of the entire cyst is most common
Clinical images
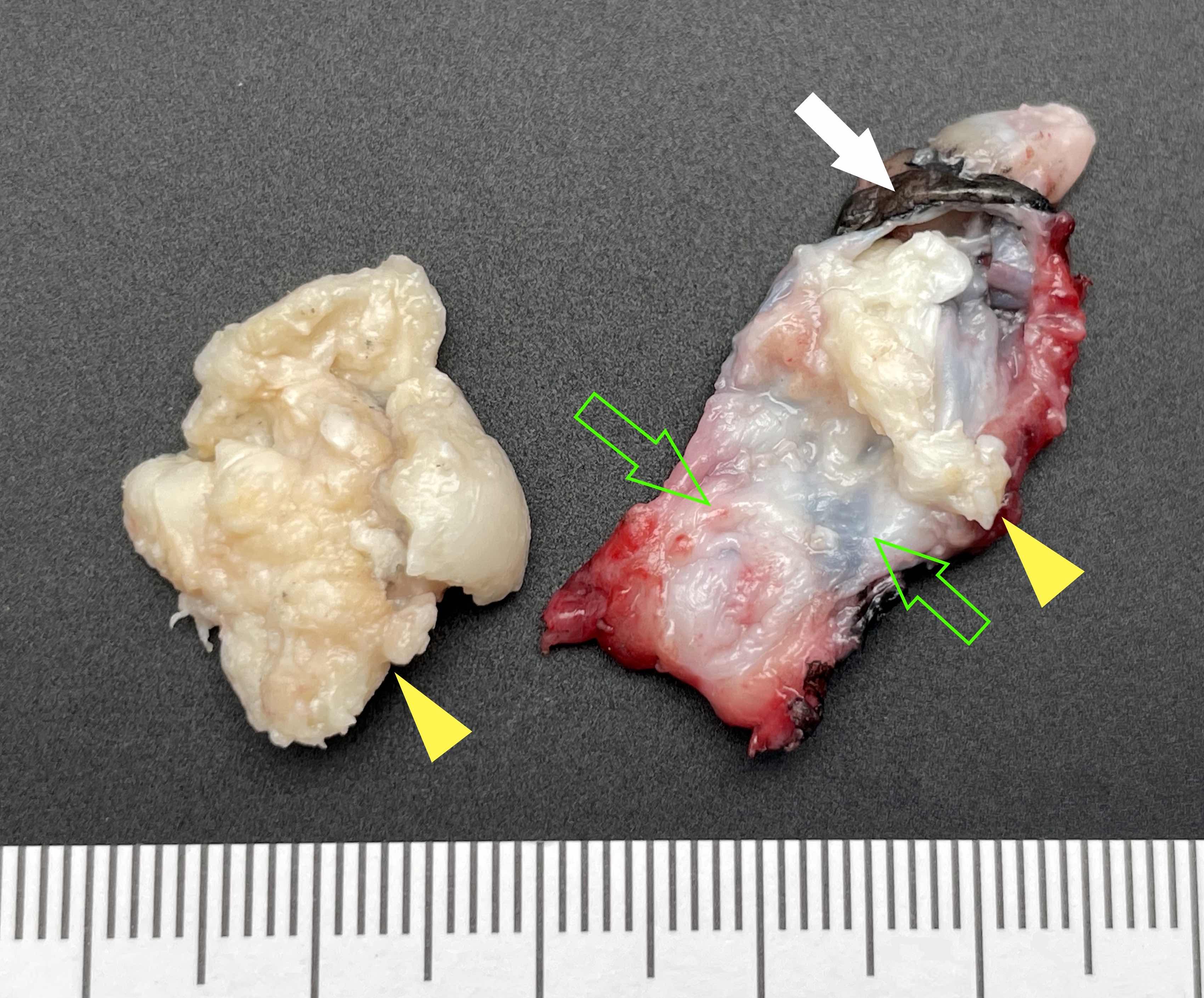
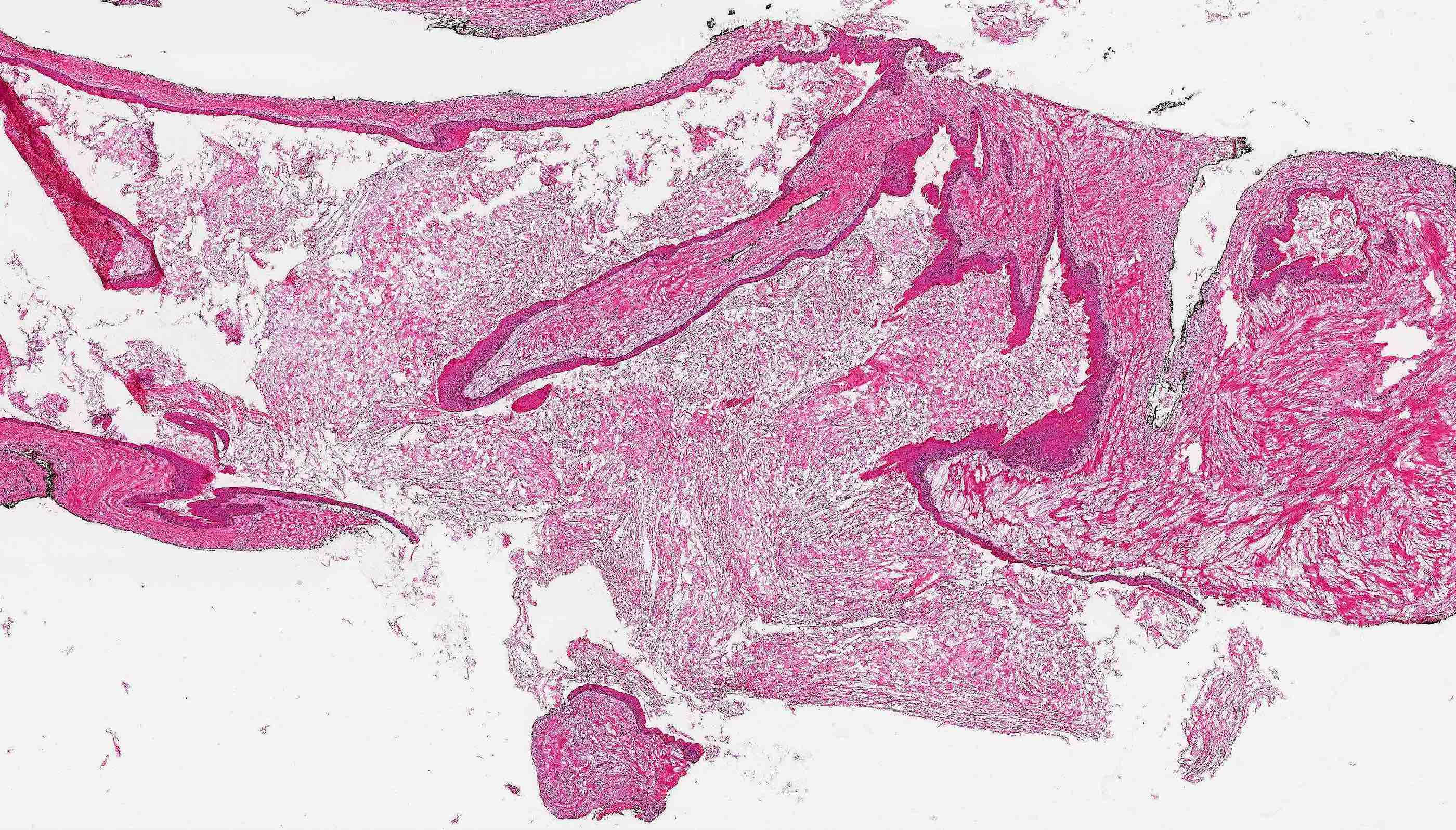
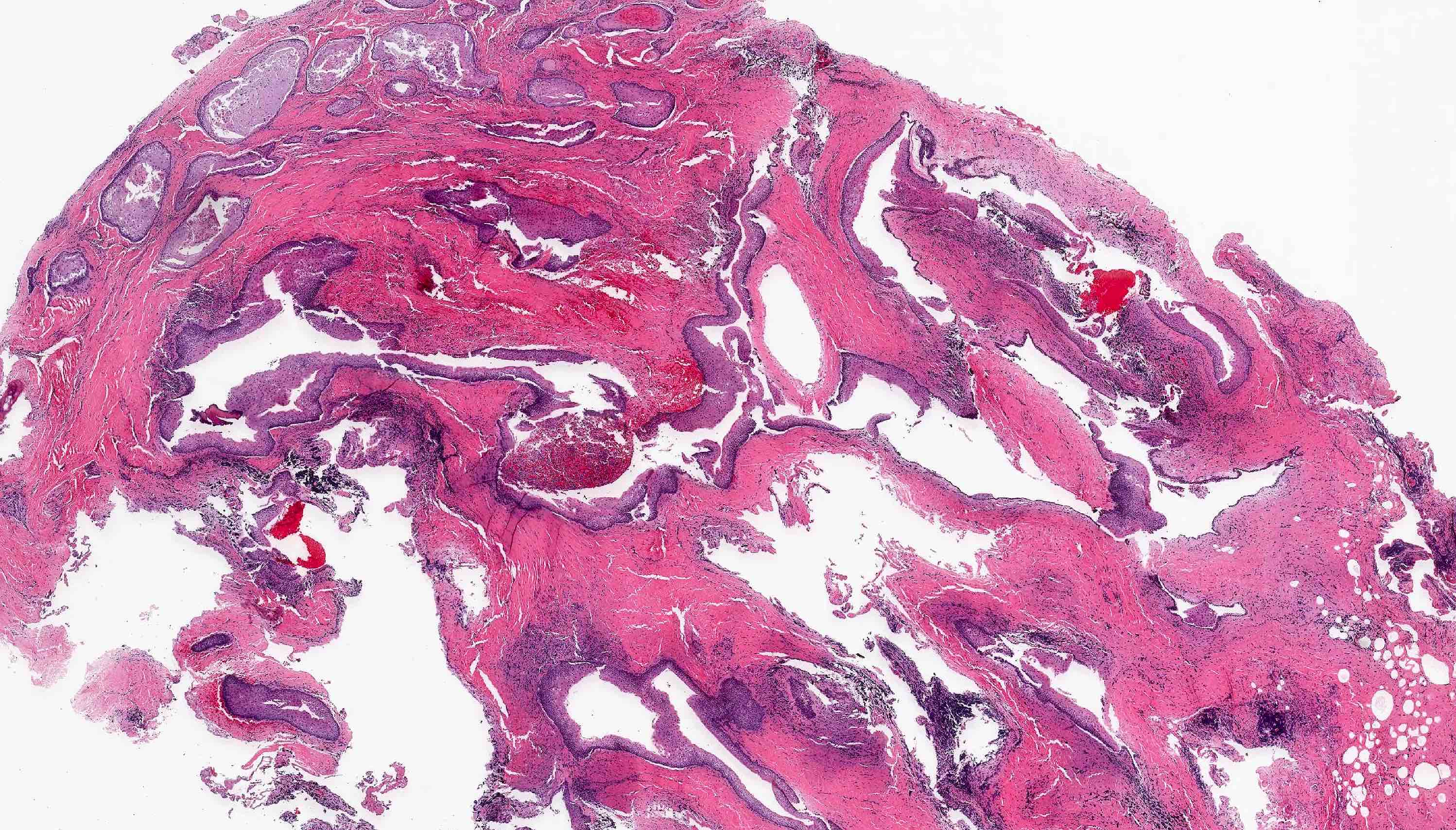
Gross description
- Surgical specimens usually consist of multiple, irregular fragments and may contain white or yellow keratinous debris (Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2002;94:543)
- Possible minute bone fragments
- In cases of curettage type treatment, all mucosal, soft tissue and bone fragments should be submitted for histologic examination to definitively confirm the diagnosis
- In resection cases, sampling surgically sectioned bone margins and relationship of cyst to bone and bone margins
- Cyst lining is generally thin (0.1 - 0.2 cm in thickness), white and may have areas of folds and furrows but lacks papillary excrescences
- Associated tooth received as specimen can be described grossly and supplemented with photographs where equipment is available
Gross images
Frozen section description
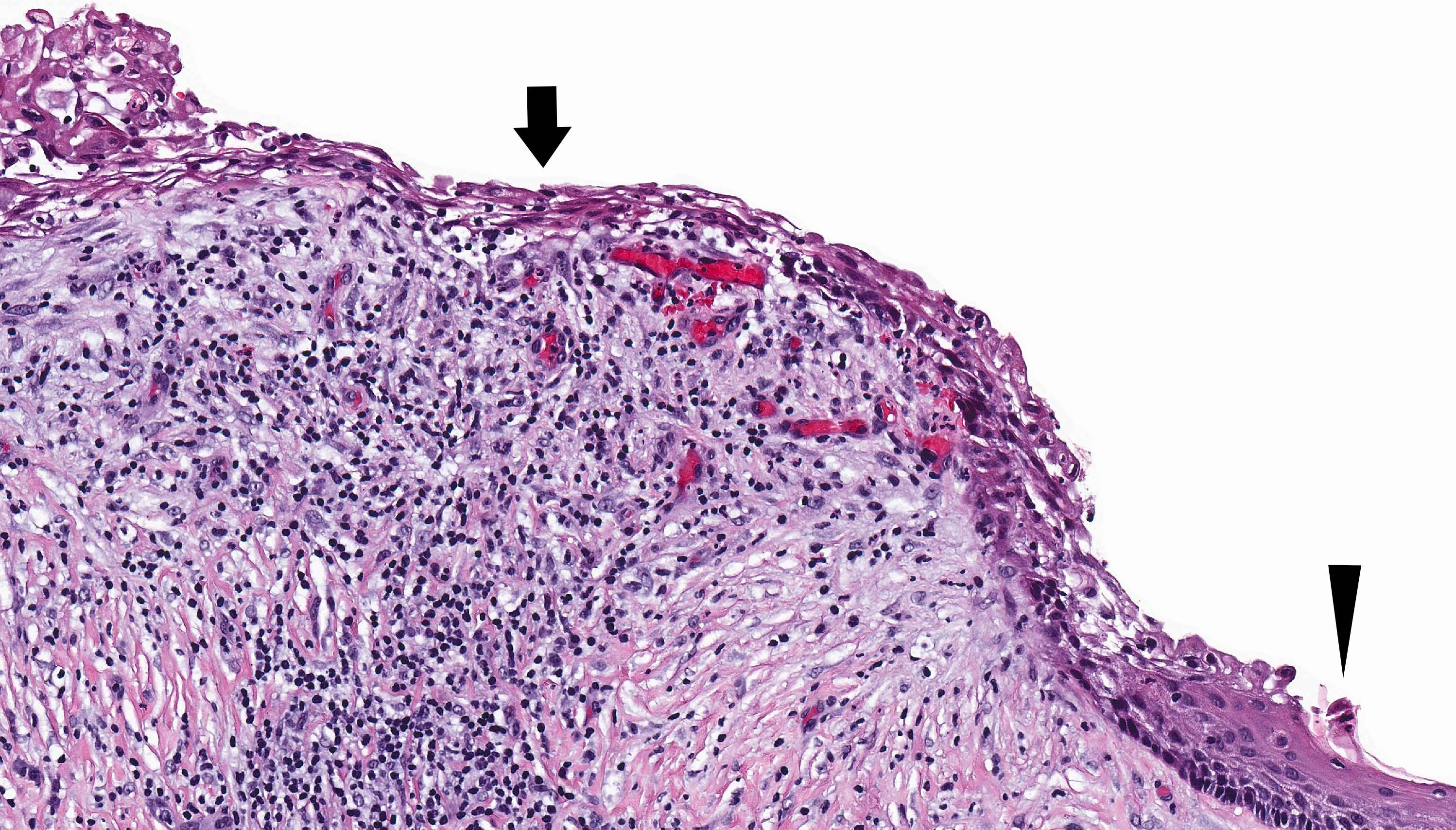
- Uninflamed cysts show characteristic uniform epithelial lining, basal layer hyperchromatism and absent rete ridge formation
- Histologic distortion is possible in the presence of inflammation
- Inflamed cysts may show multilayered stratified squamous epithelium making it difficult to distinguish from unicystic ameloblastoma, luminal subtype or inflamed dentigerous cyst
- Frozen section limitations include sampling bias, frozen section artifact and inability to perform immunohistochemistry such as BRAF V600e (J Oral Maxillofac Surg 2014;72:914)
Frozen section images
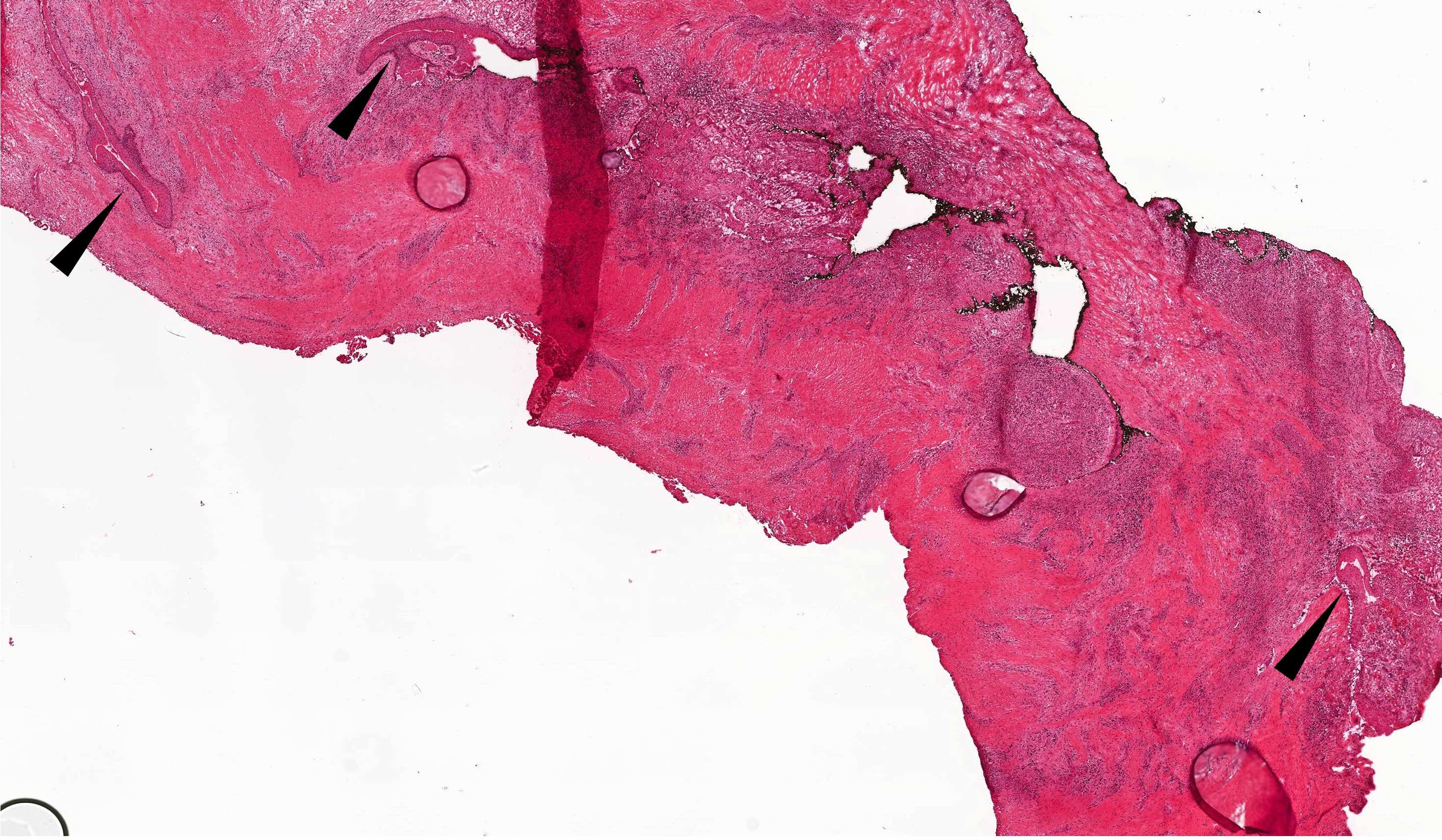
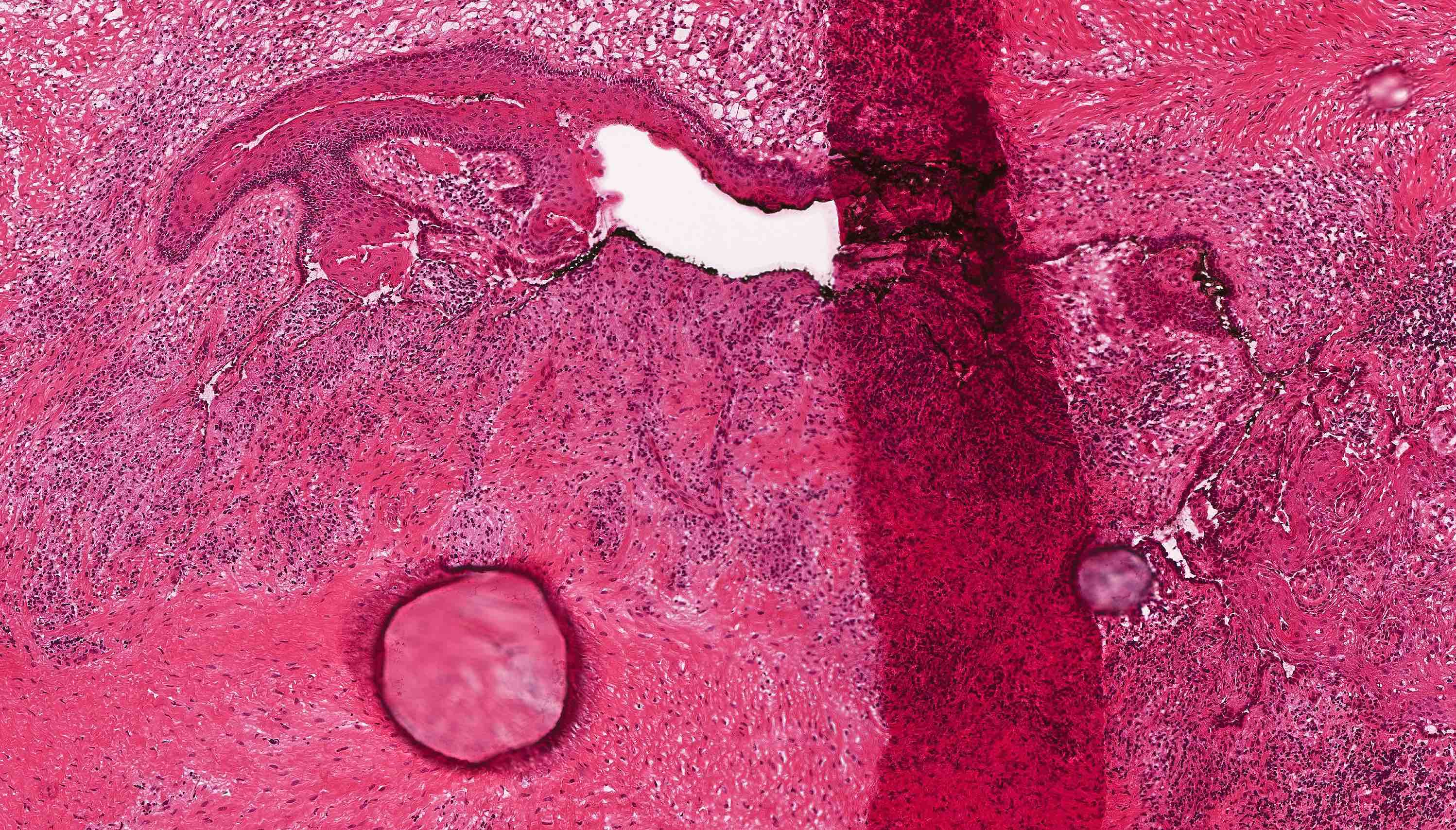
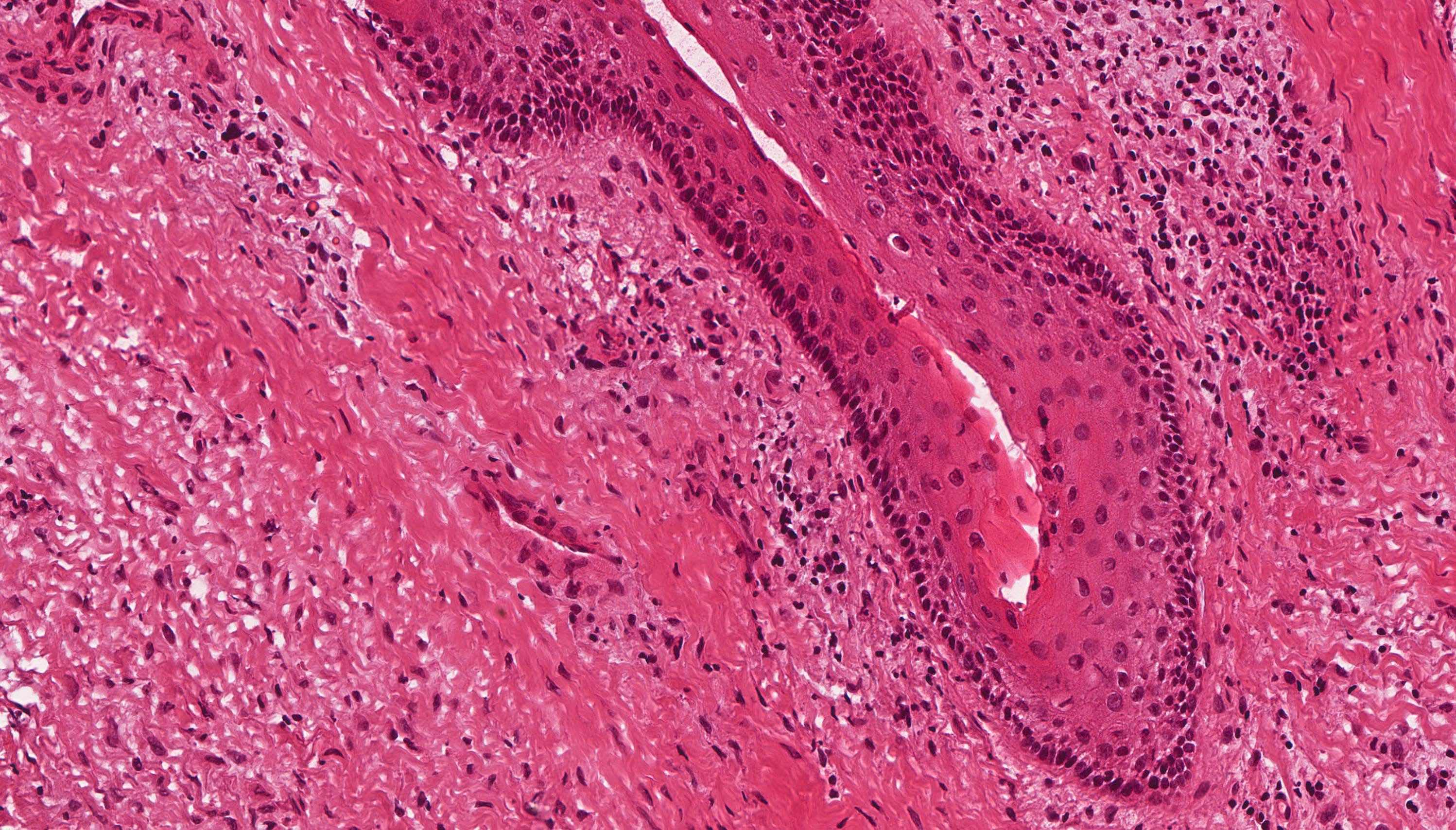
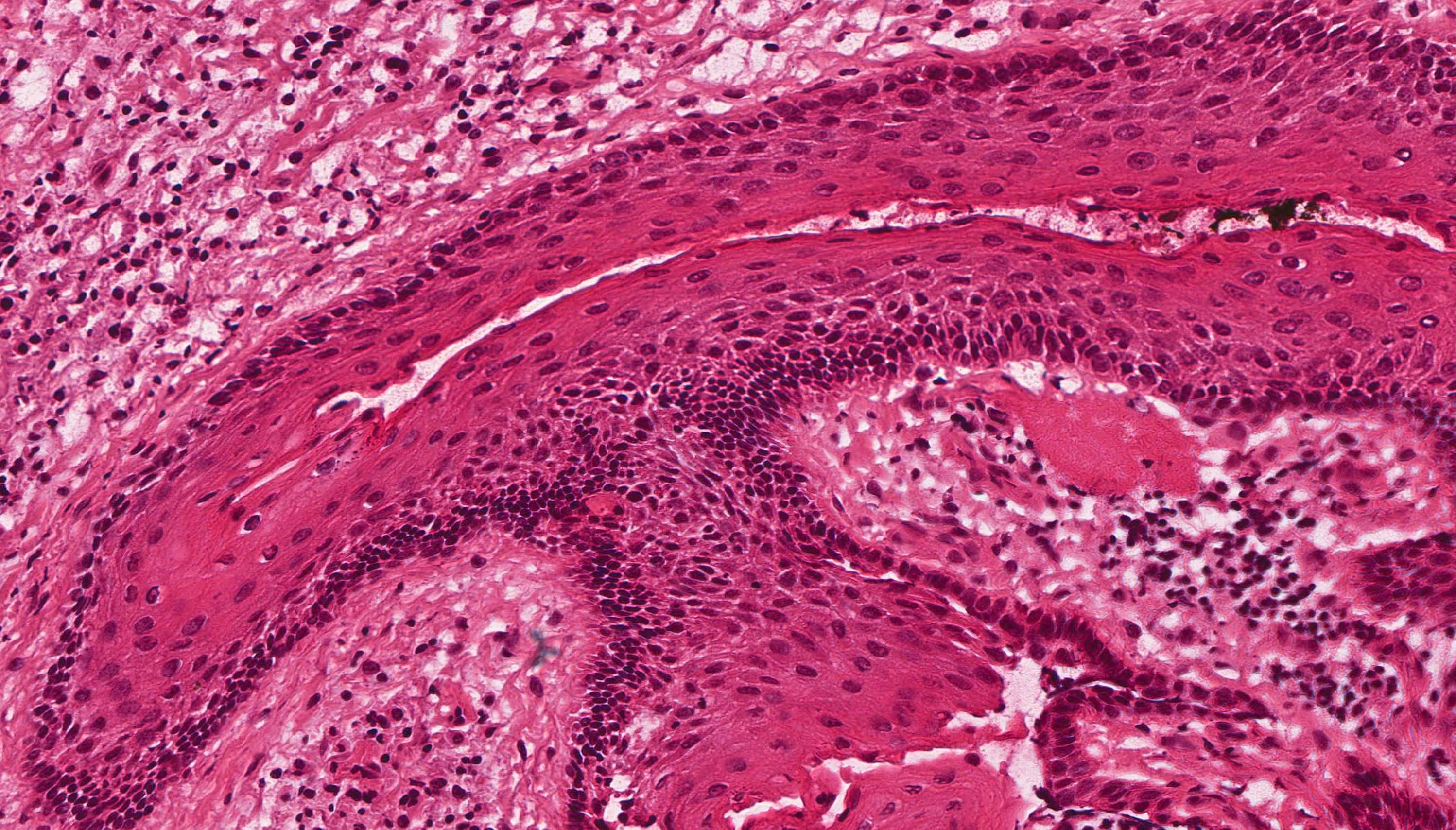
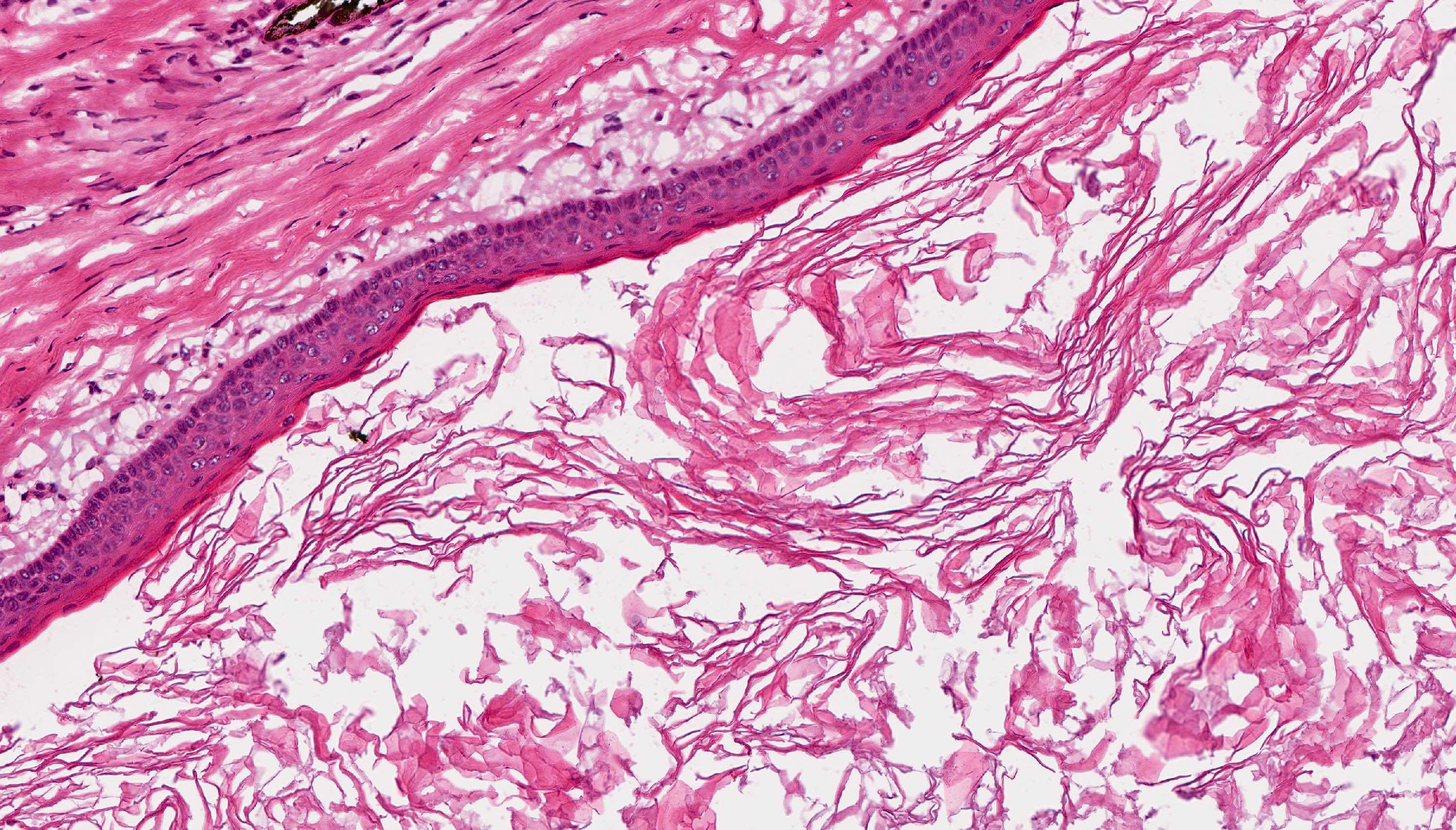
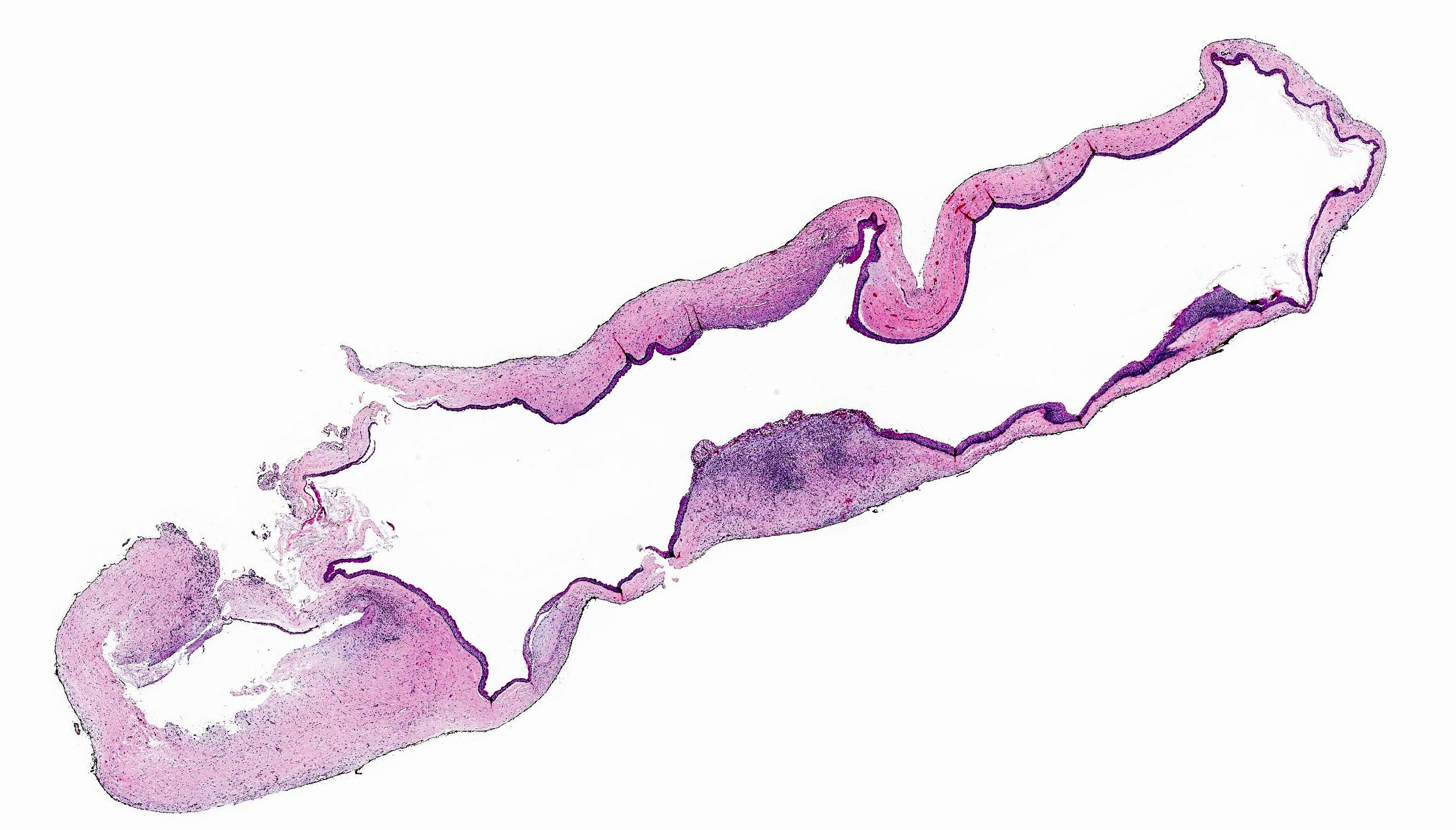
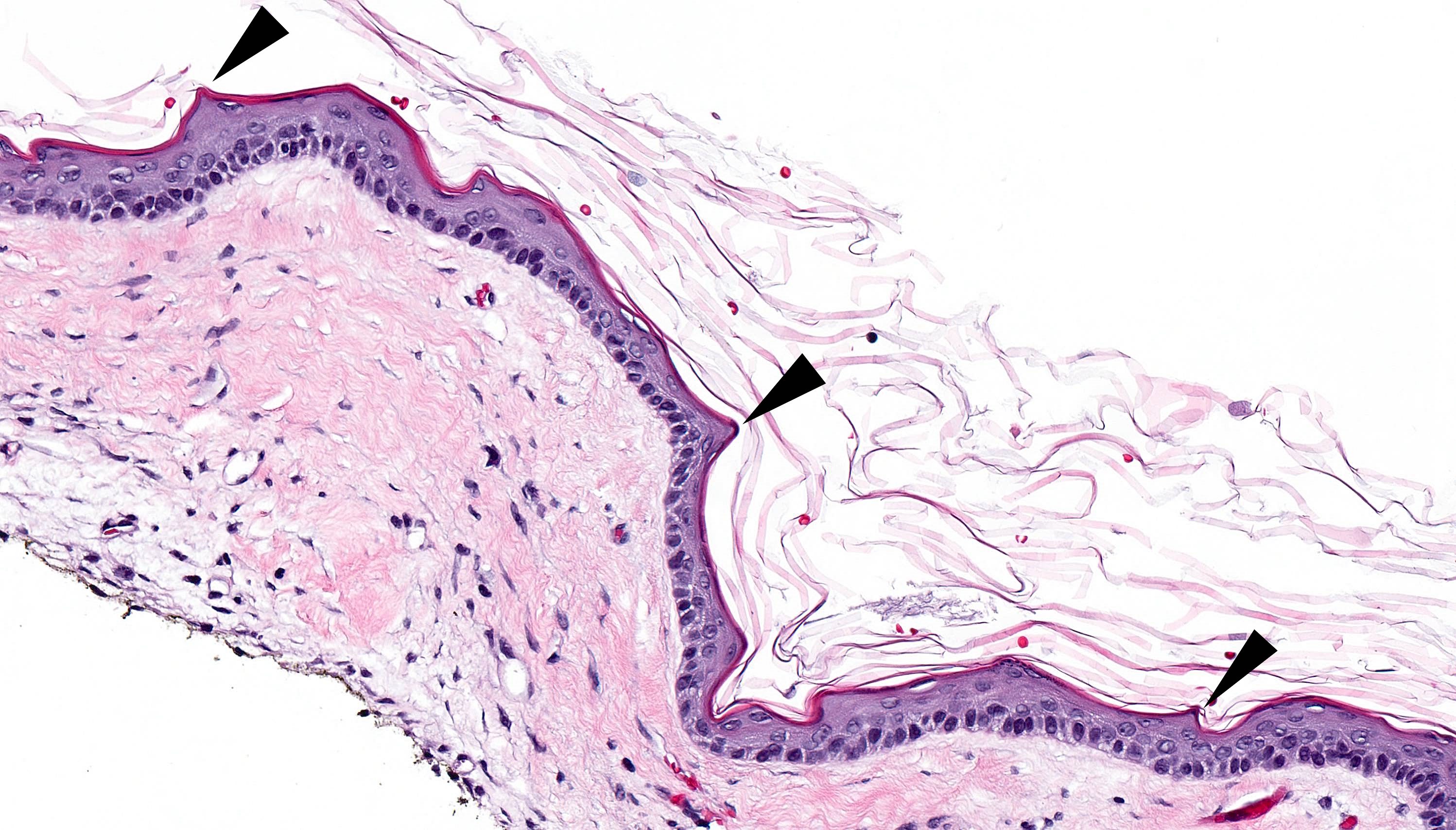
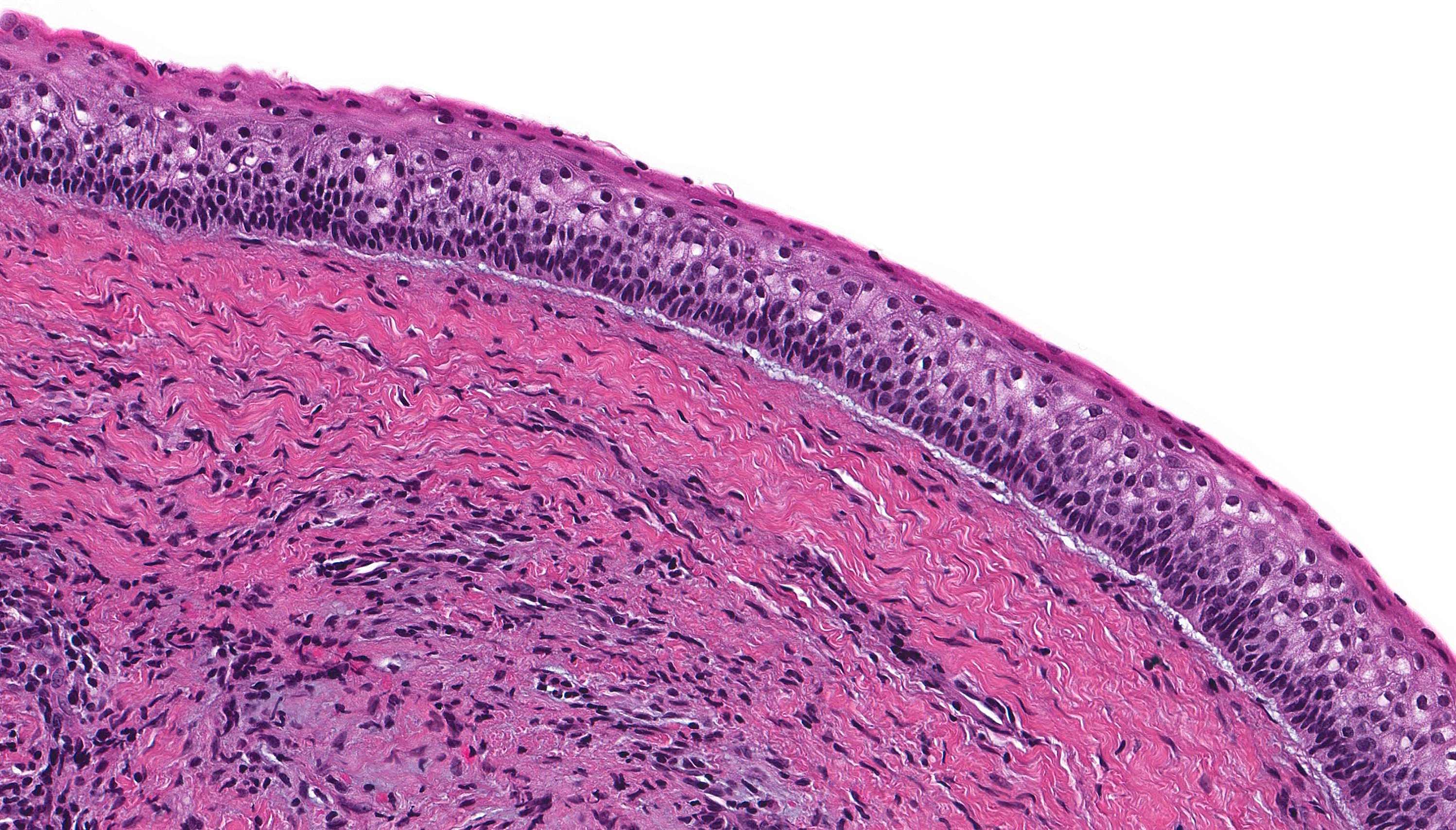
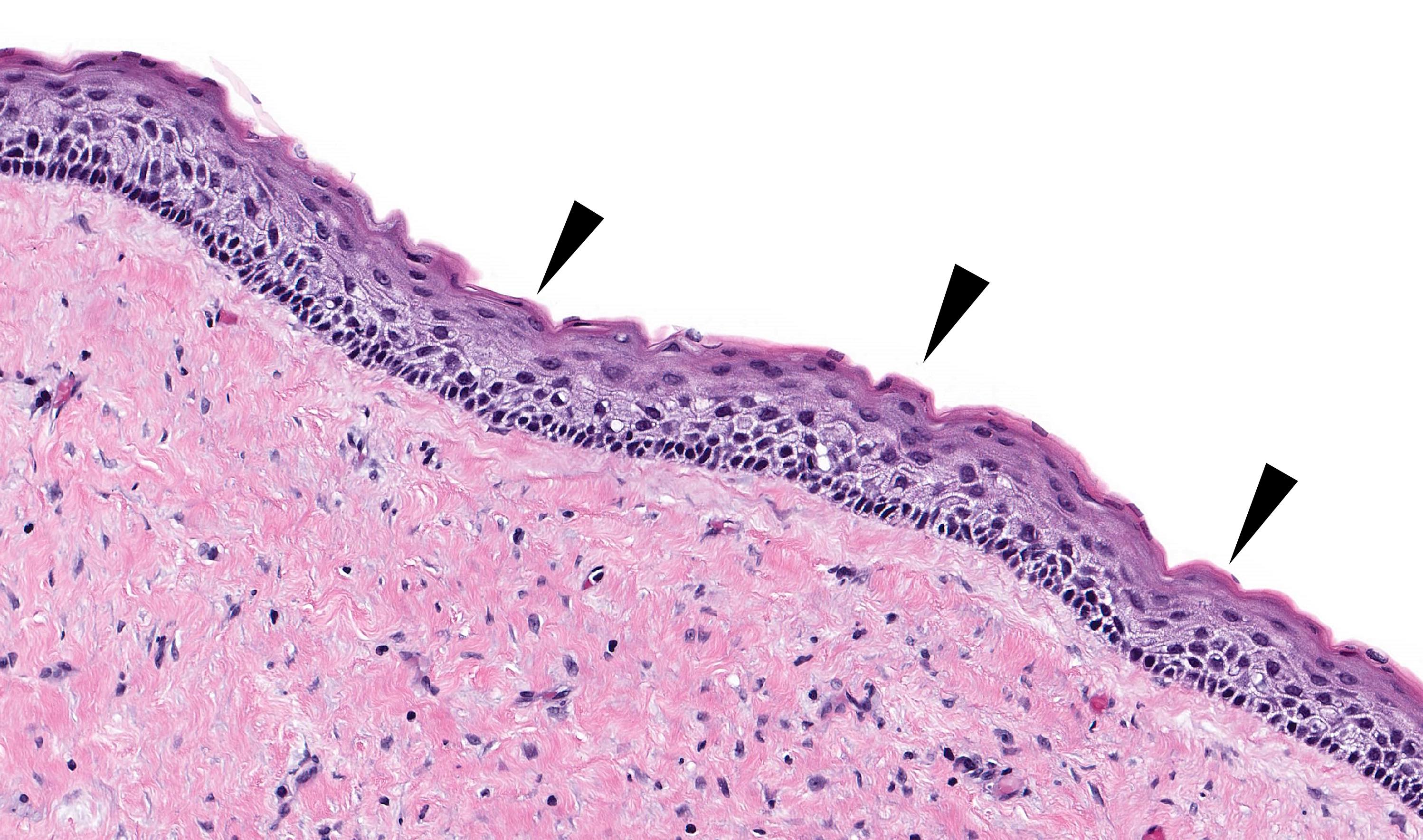
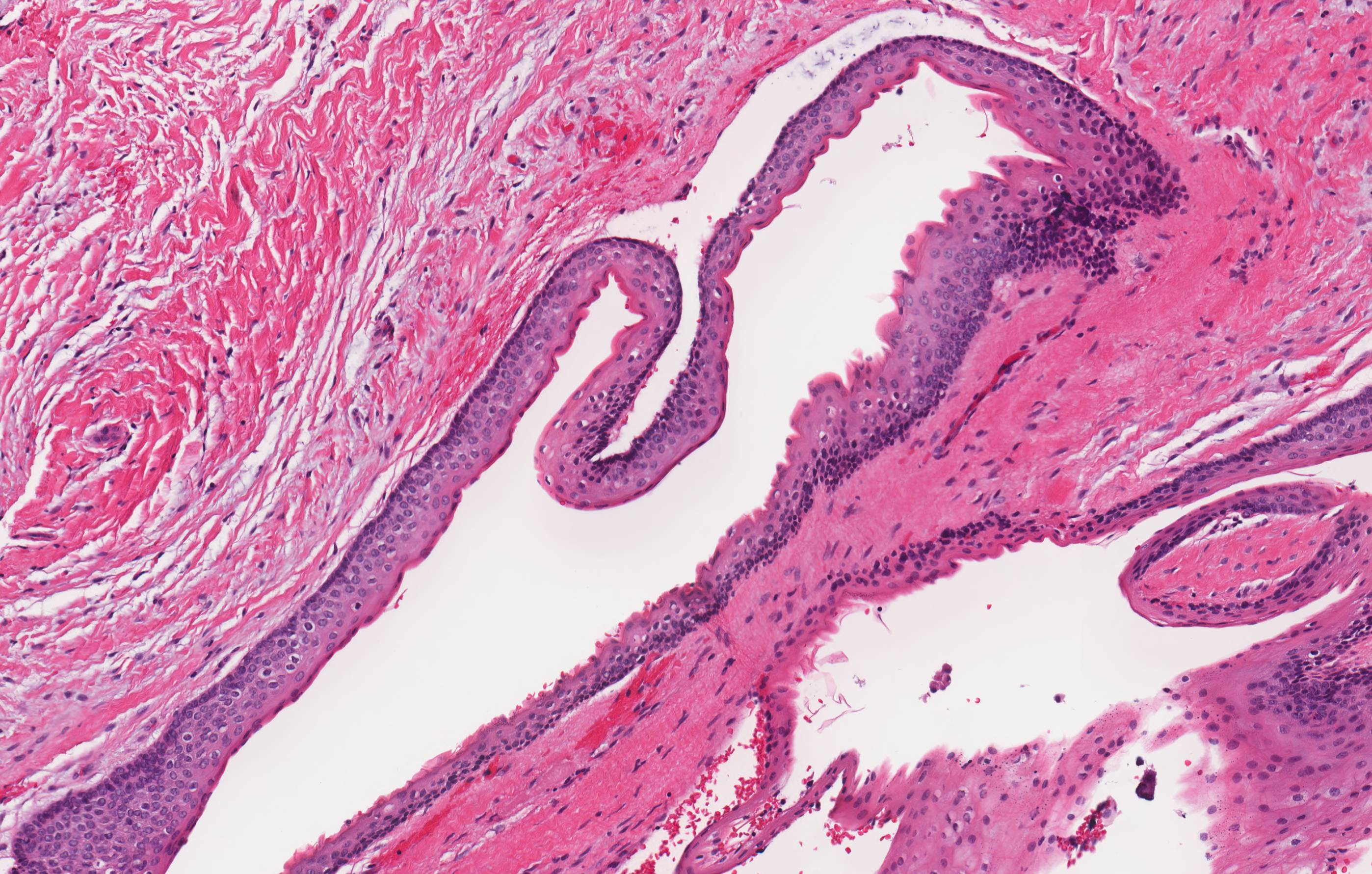
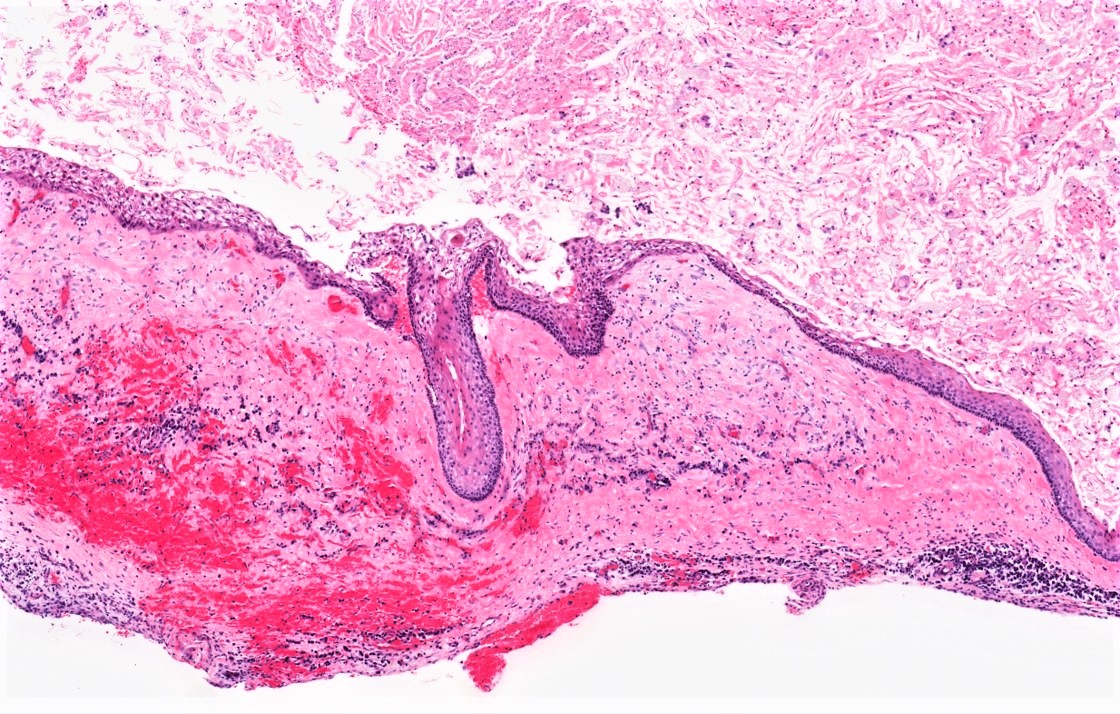
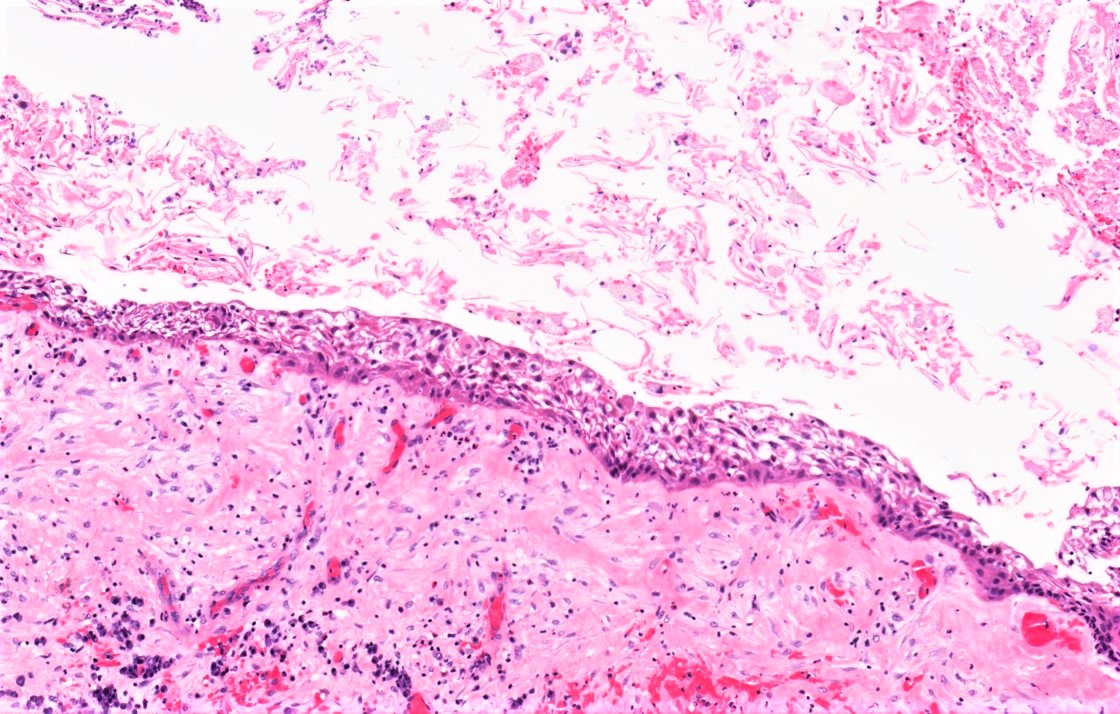
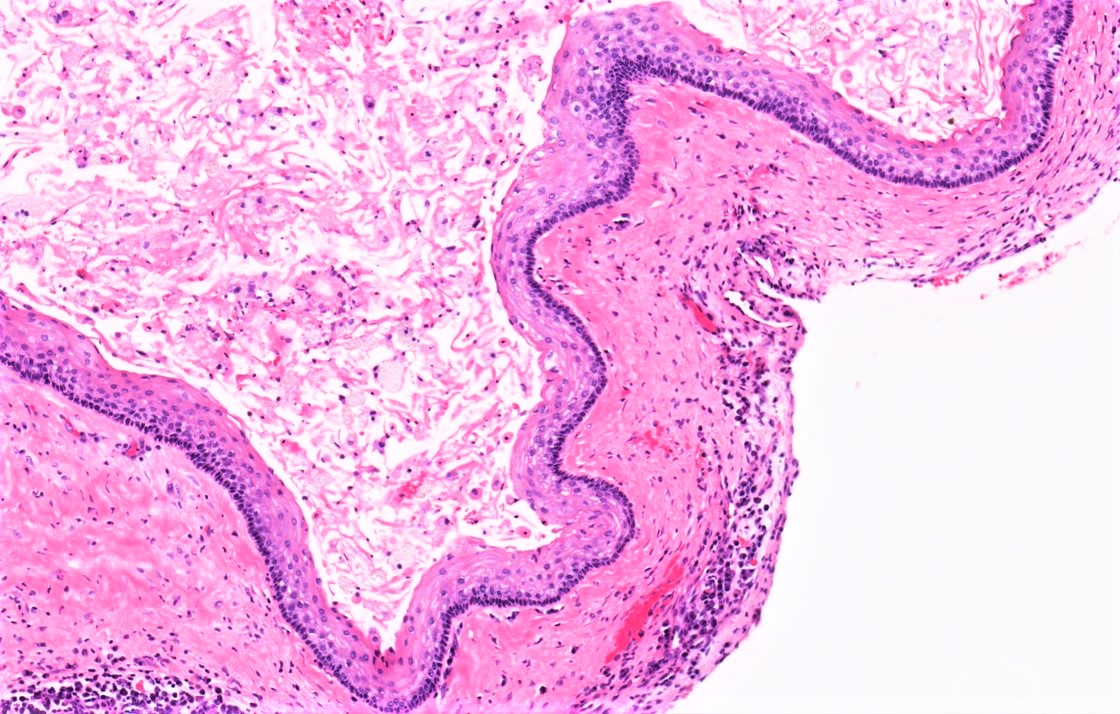
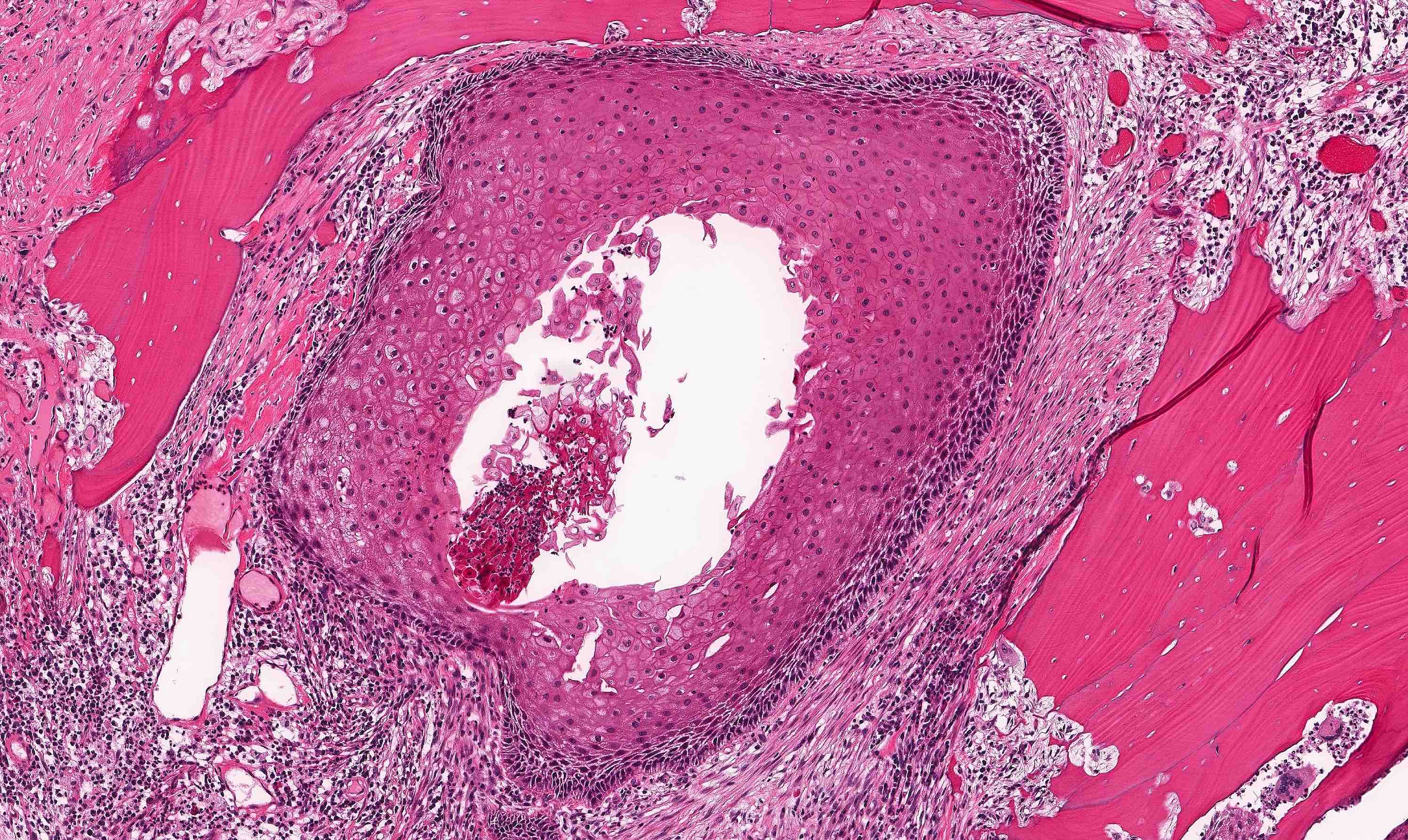
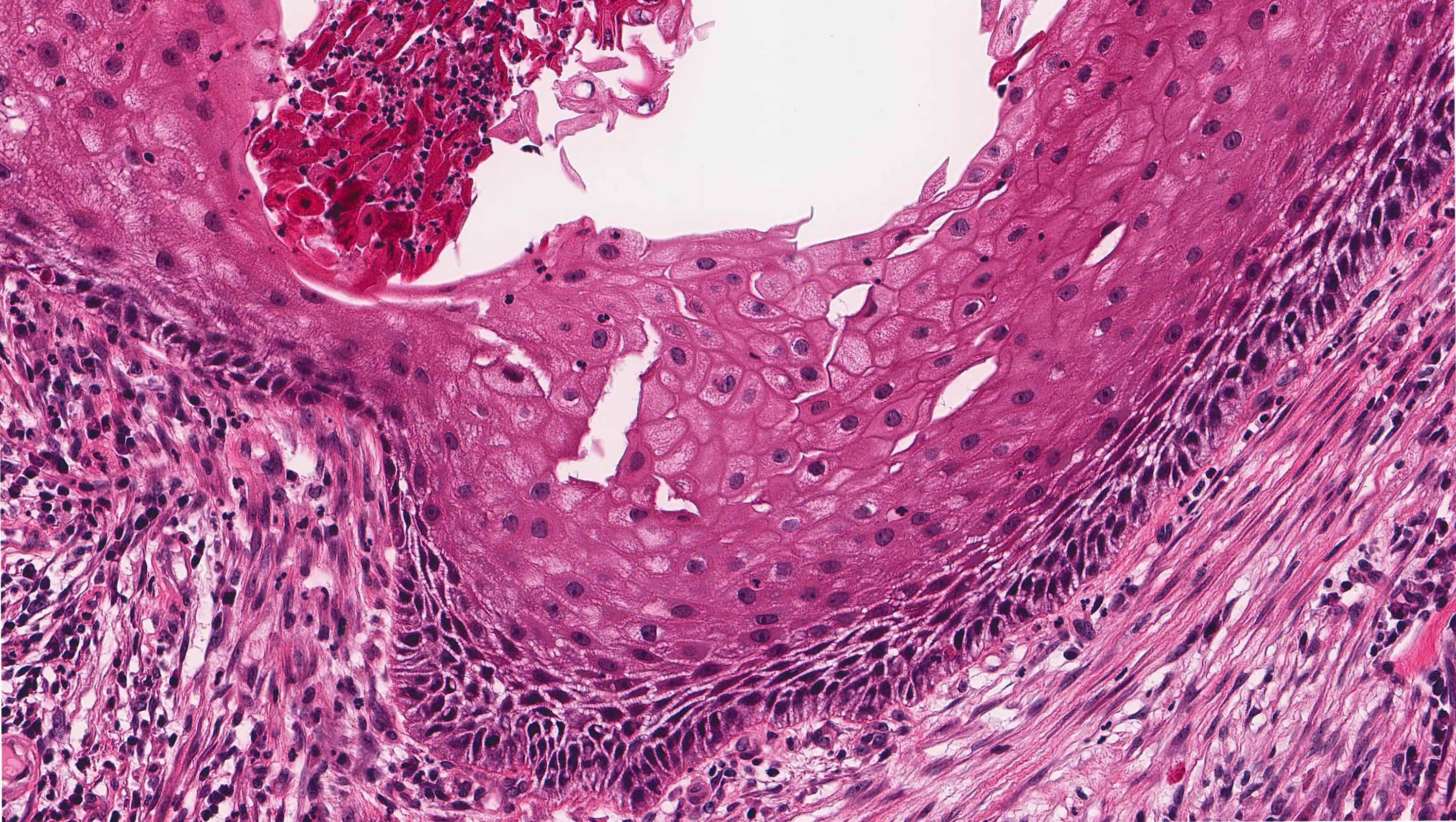
Microscopic (histologic) description
- Uniform epithelial lining 6 - 8 cells thick lacking rete ridges
- May have artifactual clefting between epithelium and underlying fibroconnective tissue
- Epithelium is characterized by palisaded hyperchromatic basal cell layer composed of cuboidal to columnar cells
- May have areas of budding growth from the basal cells
- Luminal surface has wavy (corrugated) parakeratotic epithelial cells
- Lumen may contain keratinaceous debris
- Maxillary cysts can extend into maxillary sinus (Cureus 2022;14:e21002)
- May have satellite cysts (Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2001;91:328)
- Rarely reported in association with psammomatoid calcifications (Oral Oncol 2023;147:106618)
Microscopic (histologic) images
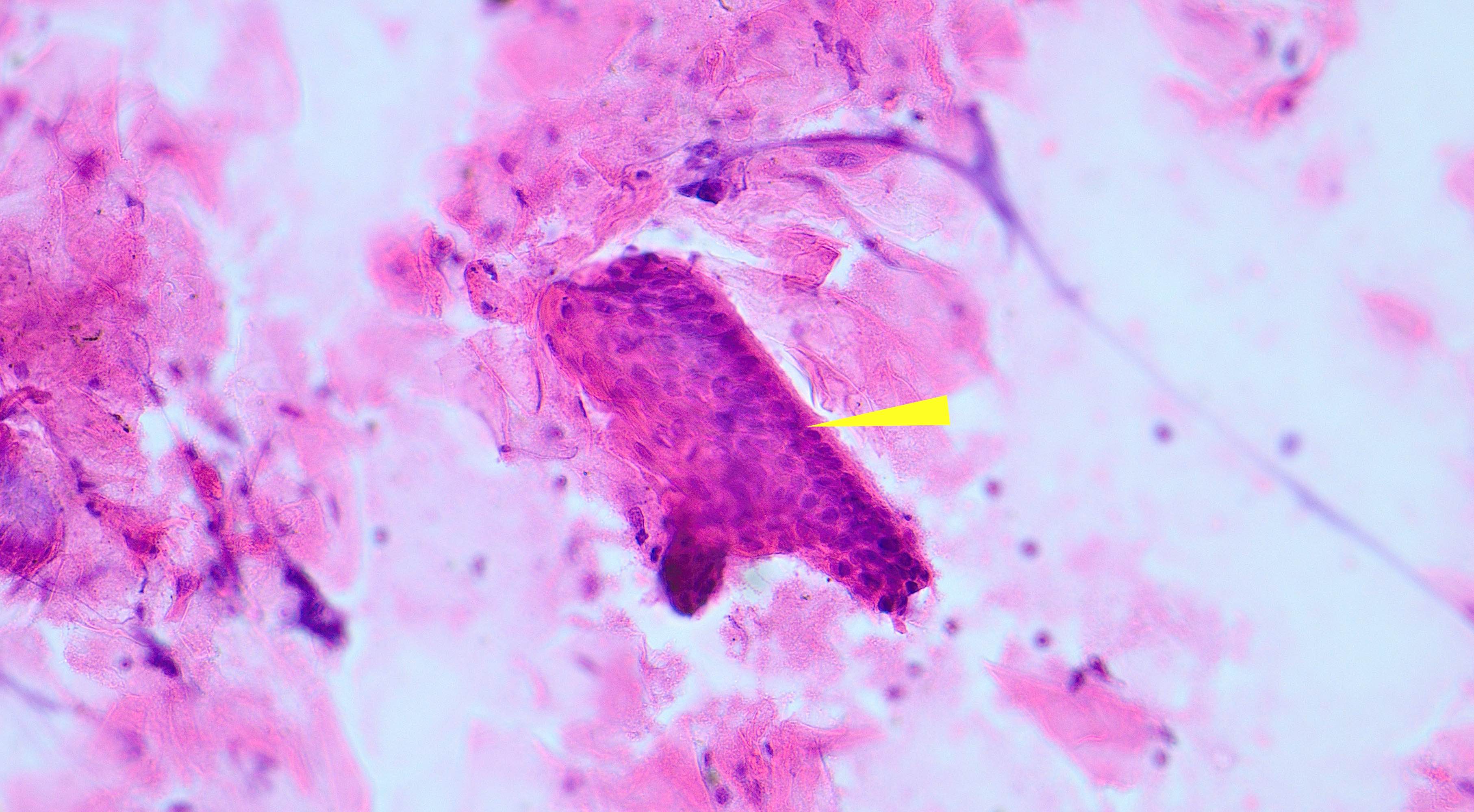
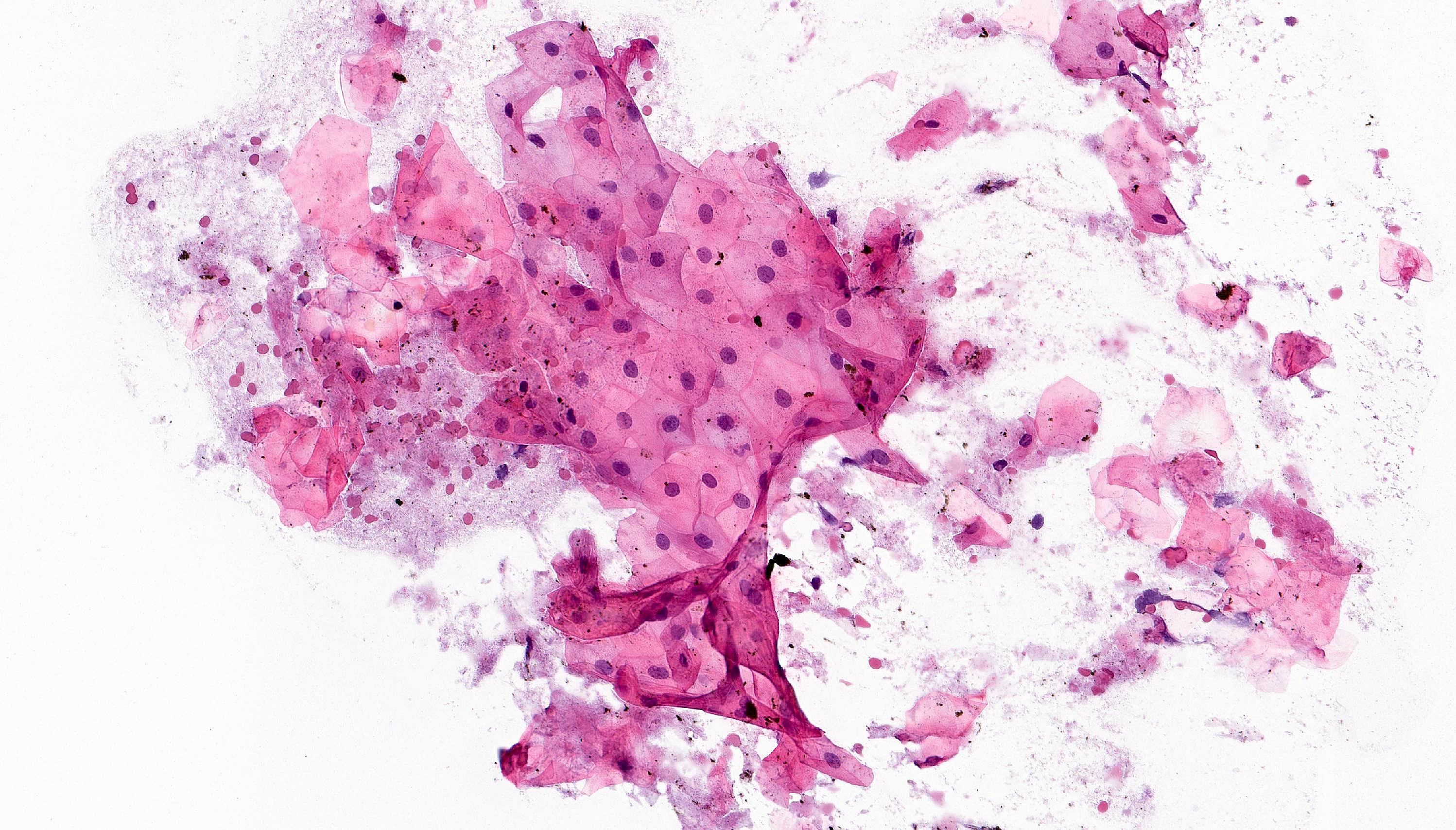
Cytology description
- Isolated groups of keratinocytes with no nuclear atypia in a background of keratin debris (Cytopathology 2007;18:361)
- Full thickness epithelial strips may demonstrate basal layer palisading
Cytology images
Positive stains
- No specific immunohistochemistry required for odontogenic keratocyst
- Squamous epithelium is expected to be immunoreactive for cytokeratin AE1 / AE3, p63 and p40
Negative stains
- BRAF immunostain
- Beta catenin immunostain negative for nuclear staining
Molecular / cytogenetics description
- Sonic hedgehog pathway alterations are common in odontogenic keratocysts, specifically PTCH1 inactivating mutations (Am J Surg Pathol 2020;44:553)
Videos
Odontogenic keratocyst - histopathology
Sample pathology report
- Left mandible lesion, enucleation and curettage:
- Odontogenic keratocyst
Differential diagnosis
- Orthokeratinized odontogenic cyst:
- Similar name, however, this cyst is unrelated to odontogenic keratocyst with limited risk for recurrence and no association with basal cell nevus syndrome
- Uniform stratified squamous epithelium lining with prominent granular layer
- Cuboidal to flat basal layer, no basal palisading
- No surface corrugation
- Thick luminal lamellated keratin (onion skin-like)
- Calcifying odontogenic cyst:
- Cystic basaloid odontogenic epithelium with palisading basal cells, loosely arranged suprabasal epithelial cells resembling stellate reticulum, variable numbers of ghost cells in suprabasilar epithelium
- Dystrophic calcifications
- Paucicellular, eosinophilic partially calcified material (dentinoid)
- Beta catenin nuclear positive
- Unicystic ameloblastoma:
- Palisading of columnar basal cells with hyperchromatic nuclei
- Generally exhibits reverse polarization of nuclei (away from basement membrane)
- Stellate reticulum is often less distinct
- Mandibular lesions often have BRAF p.V600E mutations (Int J Oral Maxillofac Surg 2024;53:122)
- Dentigerous cyst:
- Fibrous to fibromyxoid connective tissue
- No rete ridges, flat interface
- Lining epithelium, 2 - 4 layers of cuboidal epithelium, devoid of superficial keratinization
- Occasional mucous cells; rare ciliated cells
- Occasional dystrophic calcifications
- Odontogenic epithelial rests, small, inactive appearing within fibrous wall
- Radicular / periapical cyst:
- Radicular cyst (RC) is an inflammatory odontogenic cyst associated with the root of a nonvital tooth
- Surfaced by nonkeratinized stratified squamous epithelium
- Often characterized by an arcading pattern
- Cyst wall is composed of inflamed fibrous tissue, may have foamy histiocytes
- Carcinoma cuniculatum:
- Sampling of the more deeply positioned cystic burrows of carcinoma cuniculatum bears resemblance to OKC in some cases
- Very well differentiated subtype of carcinoma
- Prominent intercellular bridges, minimal atypia and rare mitotic figures
- Can have keratin cysts
- May have superficial vacuolated clear cells
- Often associated with inflammatory infiltrate that may obscure tumor stroma boundary
- Intraepithelial abscess formation is common
Additional references
Board review style question #1
Board review style answer #1
D. Well defined layer of palisading hyperchromatic basal cells without reverse polarity. Odontogenic keratocyst has a well defined layer of palisading hyperchromatic basal cells without reverse polarity. Answer C is incorrect because the stellate reticulum-like suprabasal layer is common in ameloblastoma and can also be seen in calcifying odontogenic cyst. Answer B is incorrect because odontogenic keratocyst is a benign lesion; an infiltrative lesion with mitotic activity is concerning for malignancy. Answer A is incorrect because if a granular cell layer is present, consider the possibility of an orthokeratinized odontogenic cyst.
Comment Here
Reference: Odontogenic keratocyst
Comment Here
Reference: Odontogenic keratocyst
Board review style question #2
Which of the following sites is most commonly involved by odontogenic keratocyst?
- Anterior mandible
- Anterior maxilla
- Maxillary sinus
- Posterior mandible
Board review style answer #2
D. Posterior mandible. The posterior mandible is the most common site of involvement for odontogenic keratocyst. Answer B is incorrect because a cystic lesion in the anterior maxilla, specifically in the midline, could represent a nasopalatine duct cyst. Answer A is incorrect because odontogenic keratocyst occurs in the anterior mandible but this is not the most common site. Answer C is incorrect because odontogenic keratocyst occurs in the maxilla with extension into the maxillary sinus but this is not the most common site of occurrence.
Comment Here
Reference: Odontogenic keratocyst
Comment Here
Reference: Odontogenic keratocyst