Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Negative stains | Videos | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Smith MH. Periapical (dental) granuloma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/mandiblemaxilladentalgranuloma.html. Accessed April 3rd, 2025.
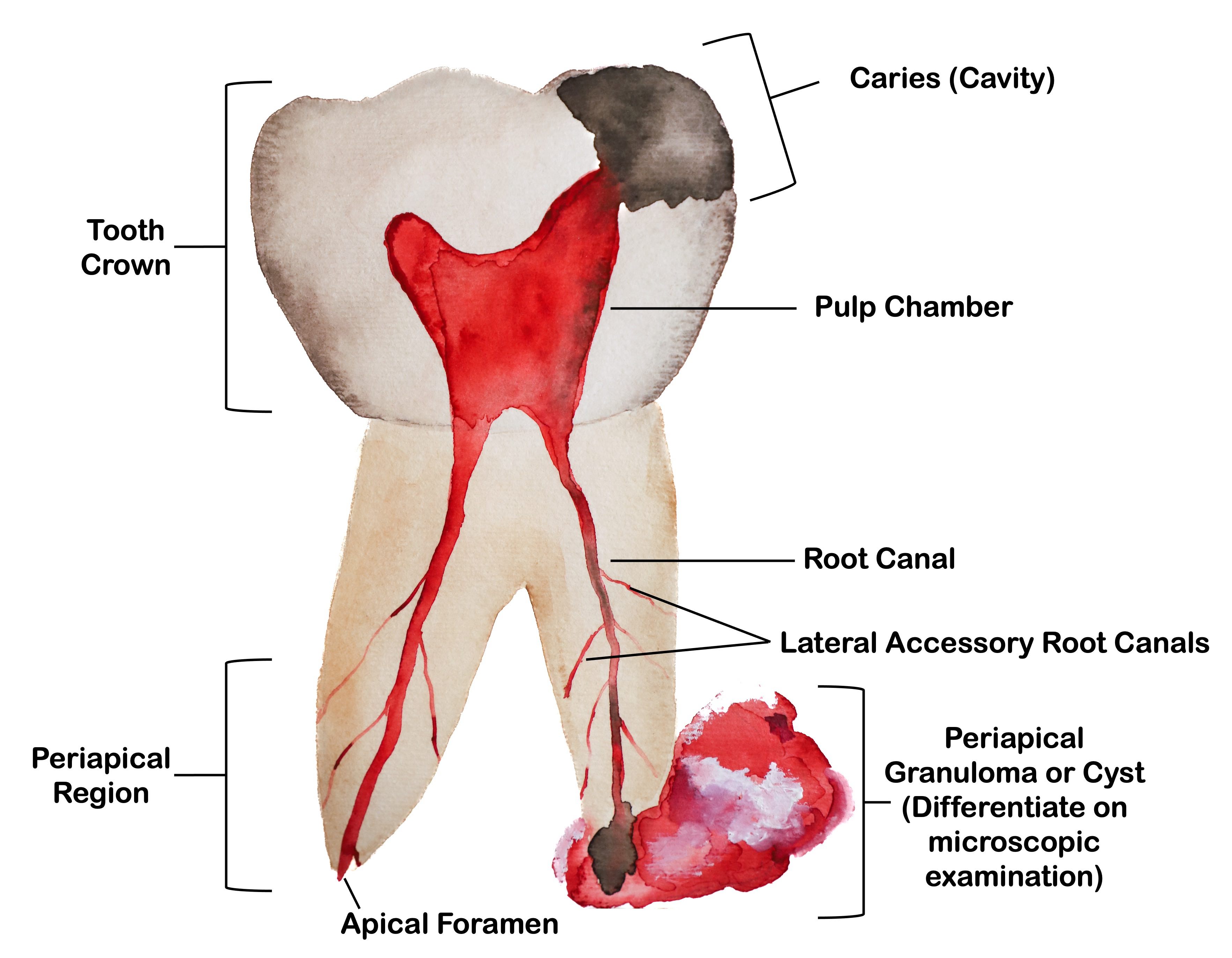
Definition / general
- Inflamed granulation or fibrous connective tissue in the periapical region (or less commonly laterally along the tooth root) of a necrotic or infected tooth
- Devoid of cystic lining epithelium, which histologically distinguishes it from a periapical inflammatory cyst (apical periodontal cyst)
Essential features
- Inflamed granulation or fibrous connective tissue near the apex of an infected tooth
- Diagnosis requires clinical and radiographic correlation
- Lacks cystic epithelium; histopathologic examination is necessary to differentiate from periapical inflammatory cyst
- Treatment entails endodontic therapy (root canal) or extraction
Terminology
- Periapical granuloma: may be referred to as dental granuloma, chronic / acute apical periodontitis or as granulation tissue
- Terms periapical granuloma and dental granuloma are both misnomers, as they are not necessarily composed of granulomatous inflammation
- Dental pulp
- Loose connective tissue within the central pulp cavity of tooth
- Contains vascular, lymphatic and nervous elements (Int J Mol Sci 2021;22:1480)
- Related terminology
- Pulpitis: inflammation of dental pulp tissue; may manifest as a toothache
- May be caused by trauma or bacteria accessing dental pulp
- Reversible pulpitis: may resolve spontaneously, with medication or by correcting / removing the cause
- Irreversible pulpitis: possibility of restoration to a healthy, disease free pulp is not possible
- Treatment limited to root canal therapy or removal of the tooth, depending on the clinical and radiographic presentation
- Apical foramen
- Small opening at the apex (toward root tip) of the tooth root that allows passage of neural and vascular supply of tooth
- Periapical region
- Also called periapex
- Localization around the apical foramen or region of root tip
- Pulpitis: inflammation of dental pulp tissue; may manifest as a toothache
ICD coding
Epidemiology
- Any dentate person may be affected
- No significant sex predilection (J Dent Res Dent Clin Dent Prospects 2008;2:63)
Sites
- Tooth bearing regions of the maxilla or mandible, most often involving the anterior maxillary teeth (J Dent Res Dent Clin Dent Prospects 2008;2:63)
- Occurs around the apex of the tooth or rarely along the lateral aspect of the tooth when lateral accessory root canals are present and involved
- May also affect dental implant sites (PLoS One 2022;17:e0277387)
Pathophysiology
- Degradation of the protective enamel tooth coating is initiated by acid, either directly from acid in the diet or more commonly, from acidic metabolites from certain bacteria within a carious lesion (cavity)
- Bacteria then penetrate the dentin and enter the pulp of the tooth, inciting a complex inflammatory response in which regulatory components of the odontoblasts, fibroblasts and perivascular cells in the dental pulp produce proinflammatory cytokines and chemokines, which recruit dendritic cells and other immune cells in an attempt to neutralize the bacterial toxins (Int J Mol Sci 2021;22:1480)
- While some teeth create tertiary dentin to form a mineralized barrier as a feature of pulpal defense / wound healing, stronger stimuli or prolonged insult can lead to complete necrosis and breakdown of the defensive mechanisms, populating the root canal system with toxins which, in turn, can migrate through the apical foramen to the surrounding tissues (Int J Mol Sci 2021;22:1480)
- To prevent the spread of the bacterial infection from the root canal to the surrounding bone and soft tissue, periapical granulomas (no cyst lining) or periapical cysts (with cyst lining) are formed
- Within the periapical region, bacterial components (e.g., lipopolysaccharides) make contact with antigen presenting cells (e.g., macrophages), which then stimulate the formation of pro or anti-inflammatory cytokines, inducing formation of the periapical granulomas or cysts (Int J Mol Sci 2021;22:1480, Eur Endod J 2020;5:54)
- In the early stages of infection, neutrophils predominate and radiographic alterations of the tooth bearing areas of the jaws are not present; this phase of periapical inflammatory disease is termed acute apical periodontitis
- Over time, osteoclasts resorb gnathic bone, leading to a radiographically detectable periapical radiolucency
Etiology
- Inciting events include caries or trauma (including trauma from operative procedures or tooth wear) (Eur Endod J 2020;5:54)
- Inflammatory reactions may be more pronounced in patients with certain chronic conditions, such as diabetes mellitus in a patient with poor glycemic control (Int J Mol Med 2023;52:60)
- Use of metformin and statins has been found to promote healing of periapical inflammatory disease in diabetic patients (J Am Dent Assoc 2021;152:434)
Clinical features
- Variable; patients with pulpal necrosis may be asymptomatic or may demonstrate pain, swelling, tooth mobility or fistulous tract formation
- May have clinically evident caries / large restorations, evidence of a traumatic tooth injury, abnormality in tooth form (e.g., dens invaginatus, dens evaginatus) or periodontal compromise involving the affected tooth
- Nonvital reaction to electric pulp testing (although the tooth may test vital if the dental granuloma involves only 1 root of a multirooted tooth)
- In cases when actinomyces is involved, purulent discharge containing sulphur granules may be present (BMJ Case Rep 2012;2012:bcr2012006218)
Diagnosis
- Although an inflammatory source can be suspected based on radiographic and clinical findings (patient symptoms, tooth vitality testing), definitive diagnosis is made on histopathologic examination of the excised periradicular lesion
- Cannot reliably differentiate periapical granuloma from periapical cyst clinically or radiographically, although some believe that large lesions most likely represent periapical cysts (Eur Endod J 2020;5:54)
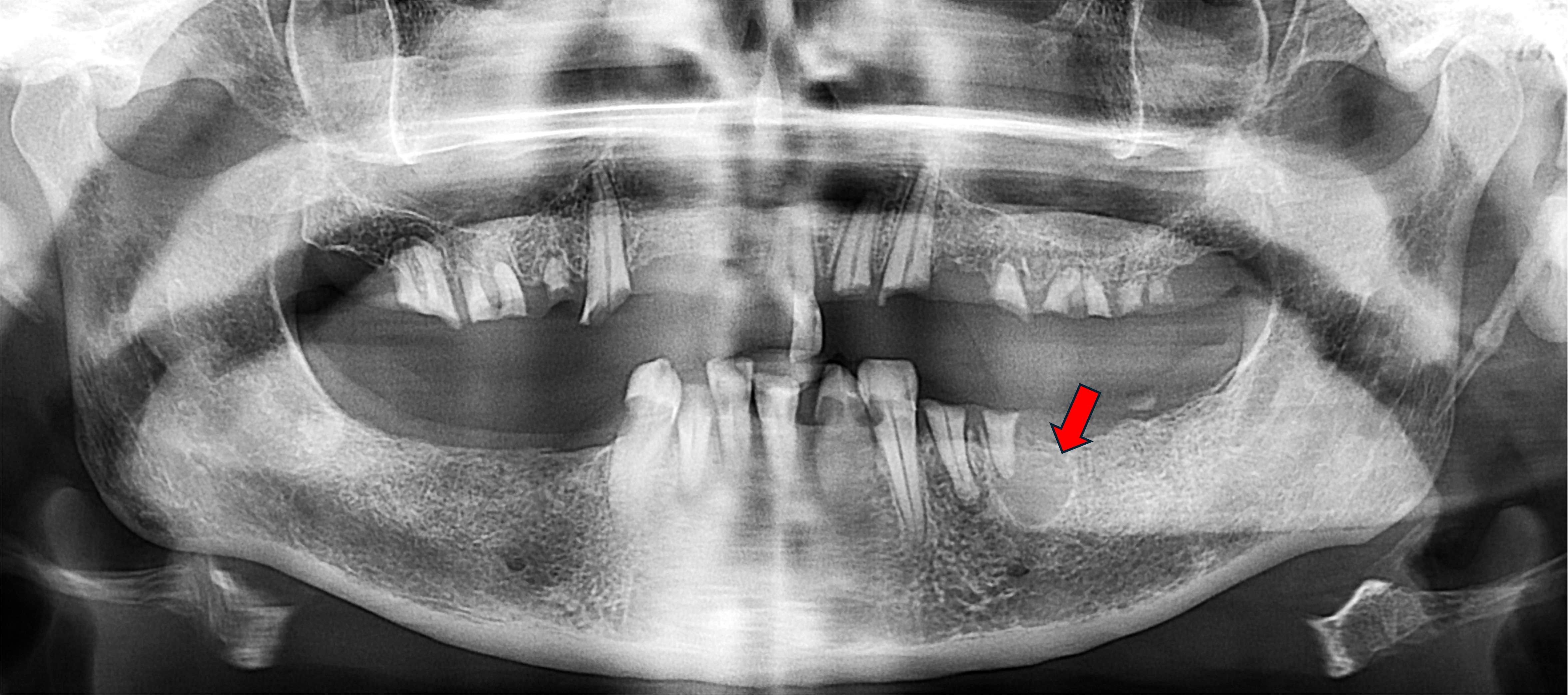
Radiology description
- Radiolucency around the apex of a tooth or rarely on the lateral aspect of a tooth when a lateral accessory pulp canal is involved
- Size ranges from barely perceivable to large lytic lesion rarely measuring > 2 cm
- Circumscribed or ill defined
- Indistinguishable from periapical cysts and other odontogenic or nonodontogenic lesions (Iran Endod J 2021;16:150)
- Affected teeth often show loss of apical lamina dura
- Root resorption is not uncommon
- Intraosseous fibrous scars may occur, especially when both cortical plates have been lost; this can give the appearance of a radiographic persistent radiolucent lesion
- Radiographically detectable lesions in the periapical region of a root canal treated tooth may have failed to resolve for several reasons
- Residual cyst / granuloma formation
- Persistent pulpal infection
- Extraradicular infection (usually localized periapical actinomycotic colonization)
- Accumulation of endogenous debris (e.g., cholesterol crystals)
- Periapical foreign material
- Associated periodontal disease
- Penetration of the adjacent maxillary sinus
- Fibrous scar formation
- All soft tissue removed during periapical surgical procedures should be submitted for histopathologic examination, as unexpected findings are not rare, including neoplasms (Iran Endod J 2021;16:150)
Radiology images
Prognostic factors
- After elimination of the pathogens in the root canal system through root canal therapy or extraction, the periradicular bone should heal and return to its normal function and integrity
- Chronic conditions that impair wound healing, such as diabetes mellitus, may compromise or slow the healing process (Int J Mol Med 2023;52:60, J Am Dent Assoc 2021;152:434)
Case reports
- 29 year old man shows healing and realignment of displaced tooth roots after microsurgical endodontic therapy using mineral trioxide aggregate (Cureus 2024;16:e52020)
- 45 year old woman presents with a granuloma around dental implant (J Oral Implantol 2018;44:287)
- 63 year old woman receives dental implant in the site of chronic residual periapical granuloma (Am J Case Rep 2023;24:e941877)
Treatment
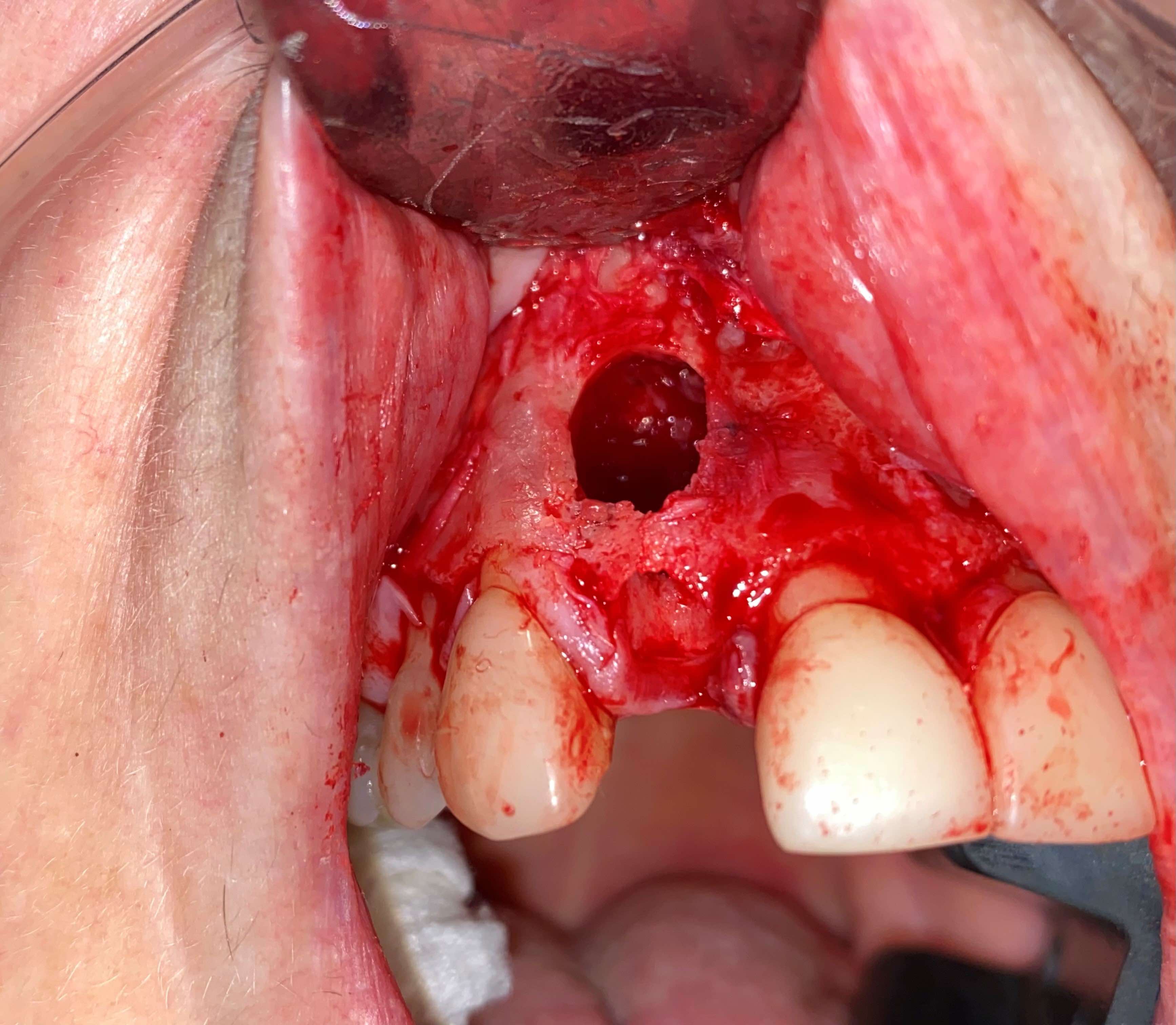
- Pathogen removal via extraction or endodontic (root canal) therapy if the tooth structure is restorable / salvageable
- Patient age, cost of treatment and patient wishes are factors that weigh into treatment of choice
- Follow up at 6 and 12 month intervals after root canal therapy is generally recommended in order to assess healing (Eur Endod J 2020;5:54)
- Periapical surgery (removing a portion of the tooth root when the apex cannot be completely sealed using nonsurgical approaches) may be considered in cases with complex root anatomy or when conventional root canal therapy fails (Eur Endod J 2020;5:54)
- Large periapical lesions (over 8 - 10 mm) often are excised via surgical intervention (Cureus 2024;16:e52020, J Oral Maxillofac Surg 2007;65:1526)
Clinical images
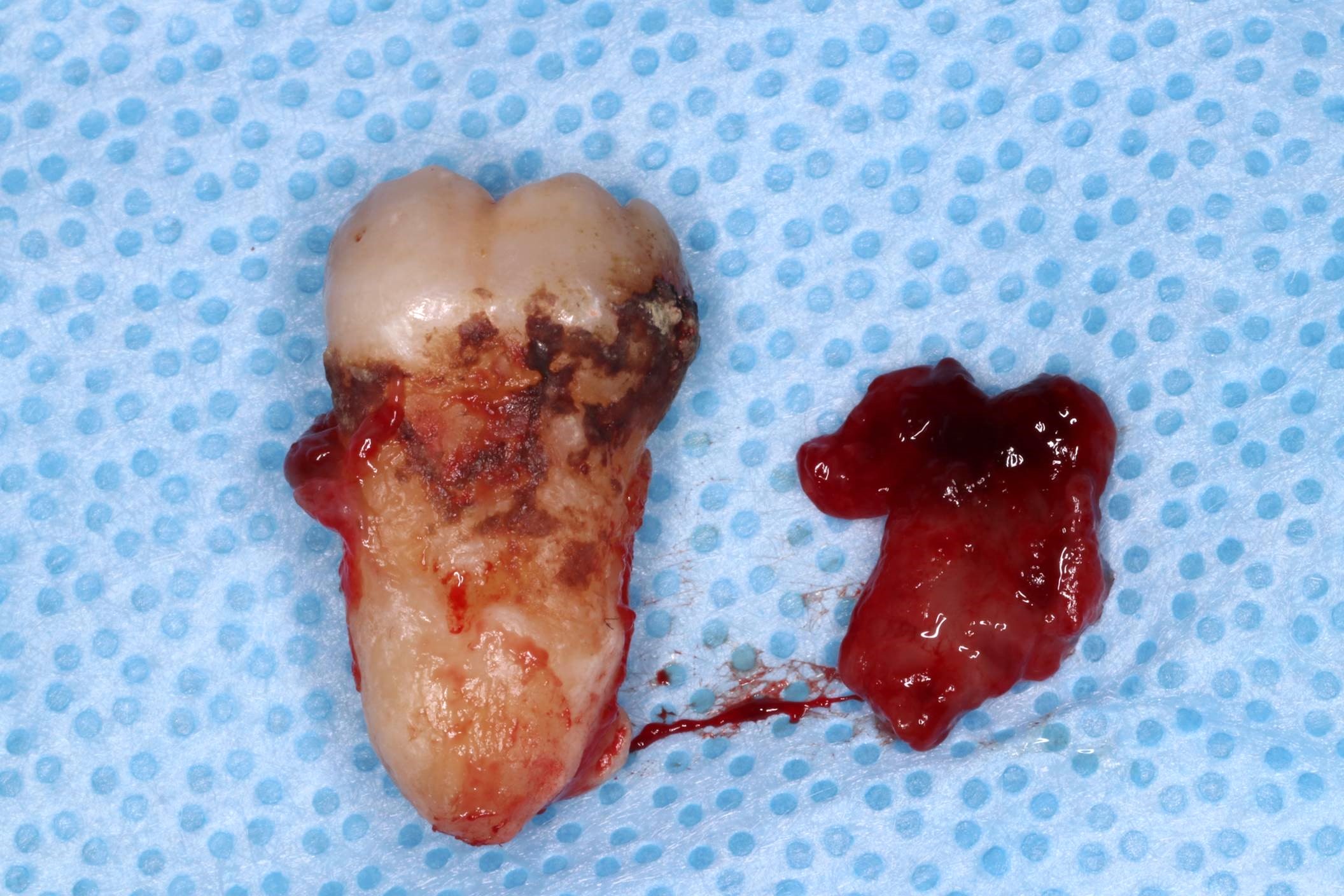
Gross description
- Tan, brown or white soft tissue may be adherent to the root apex of an extracted tooth
- May be firm, soft, friable, granular or hemorrhagic (with extensive vascular proliferation)
- May show cholesterol crystals
Gross images
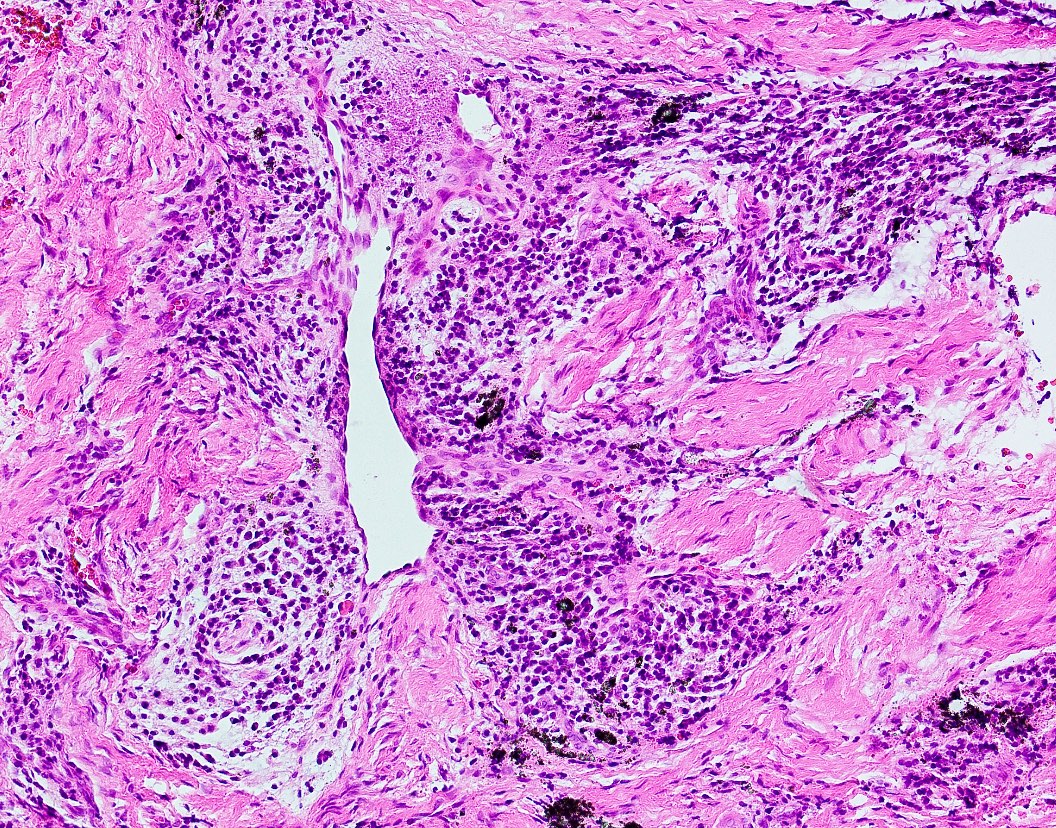
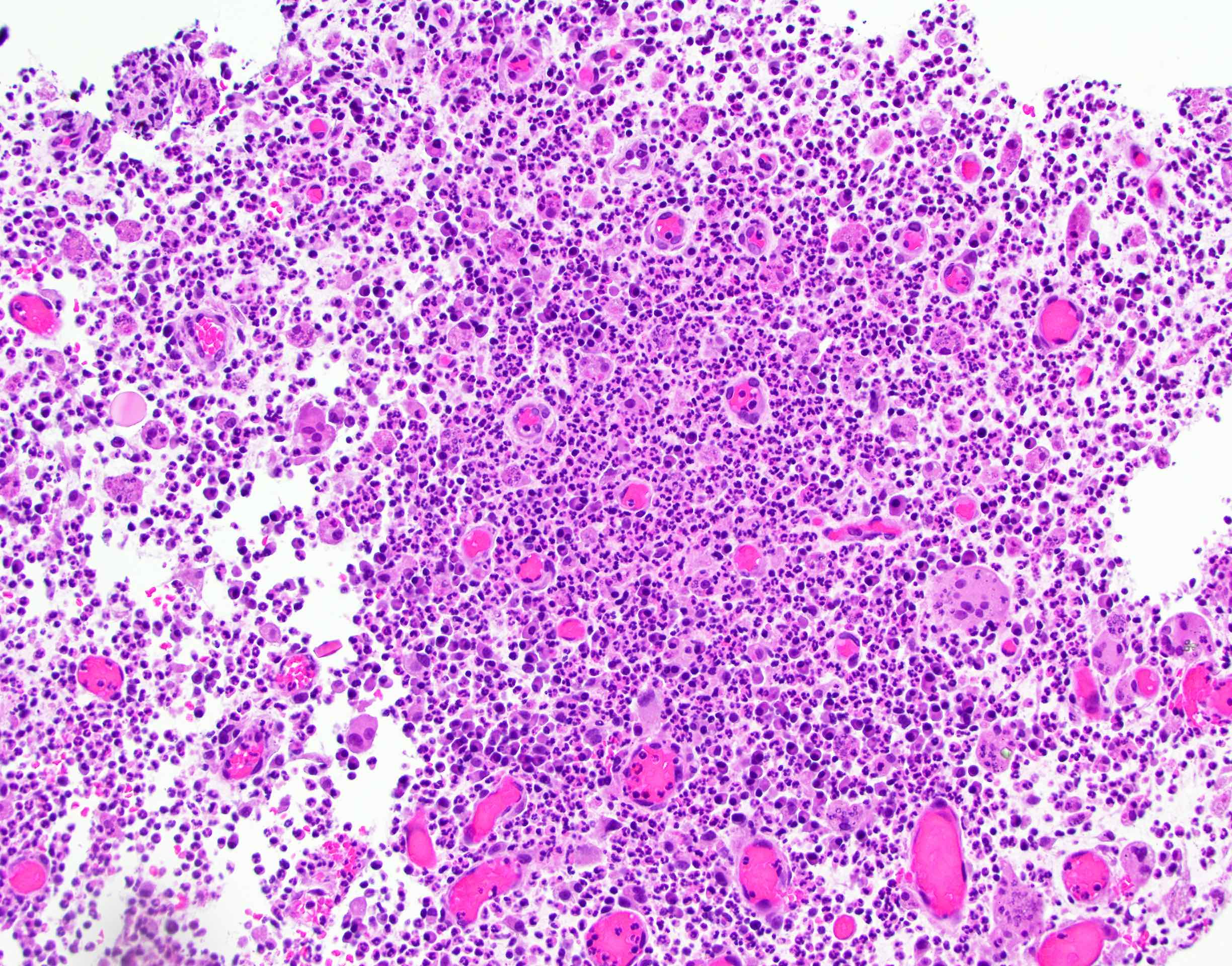
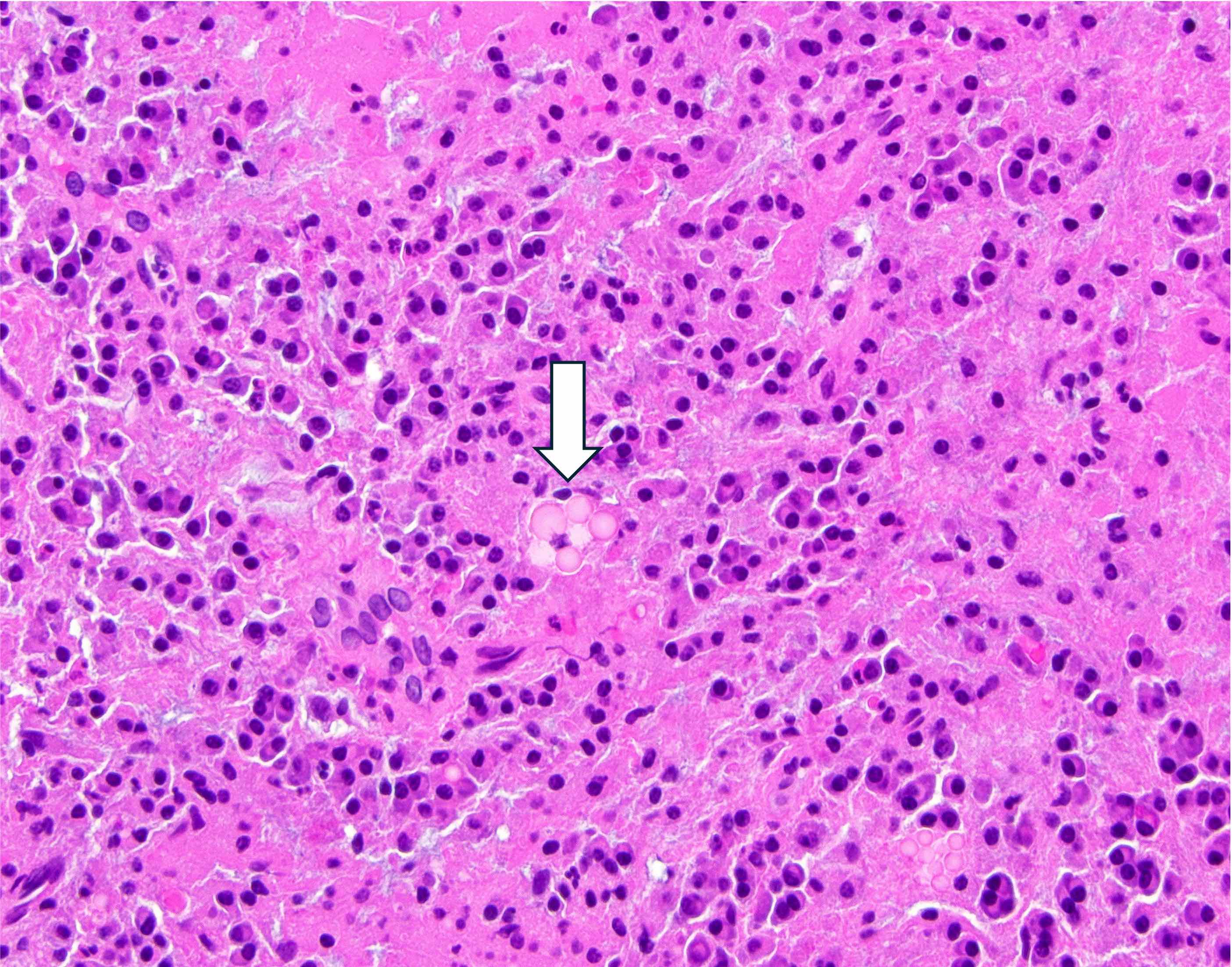
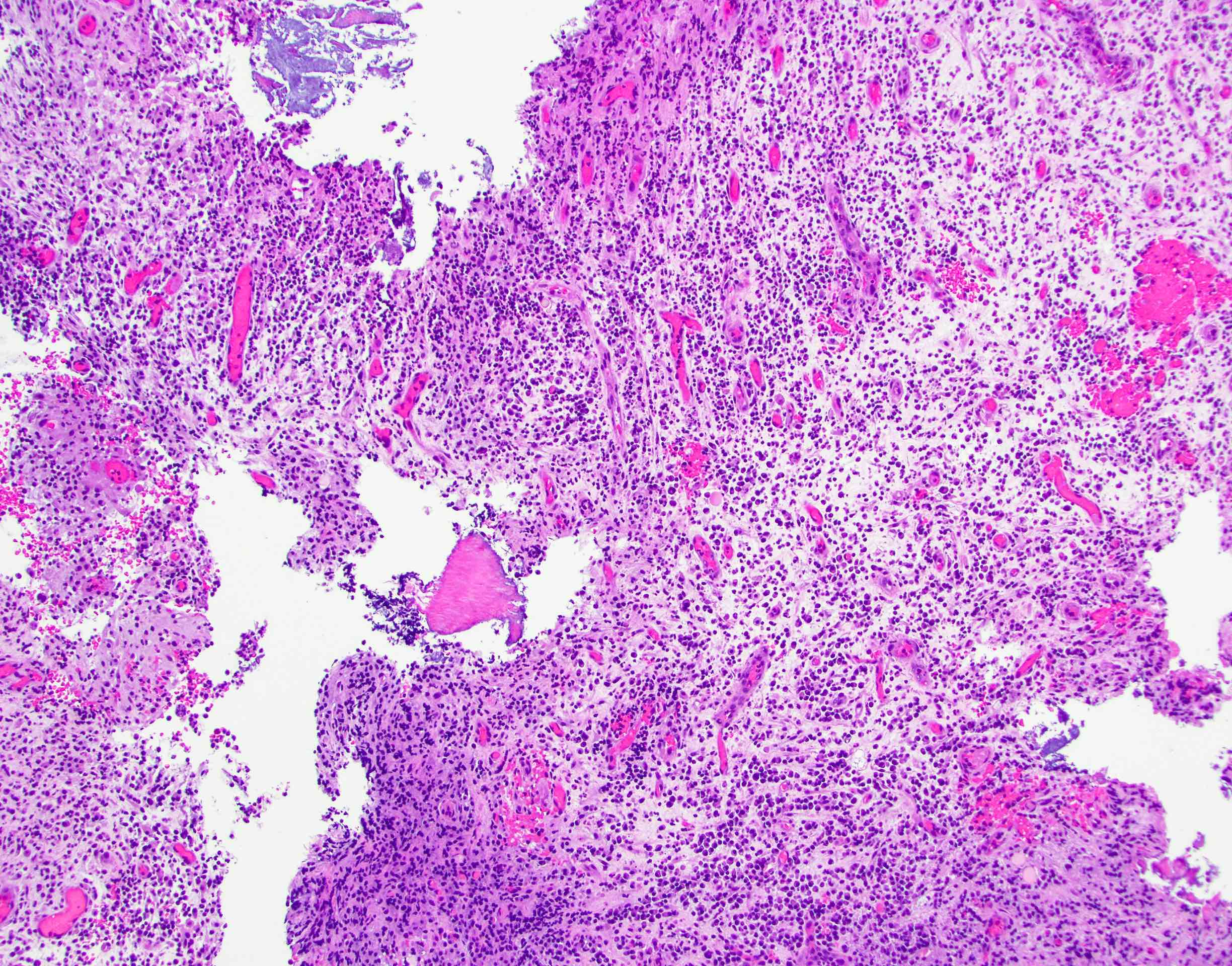
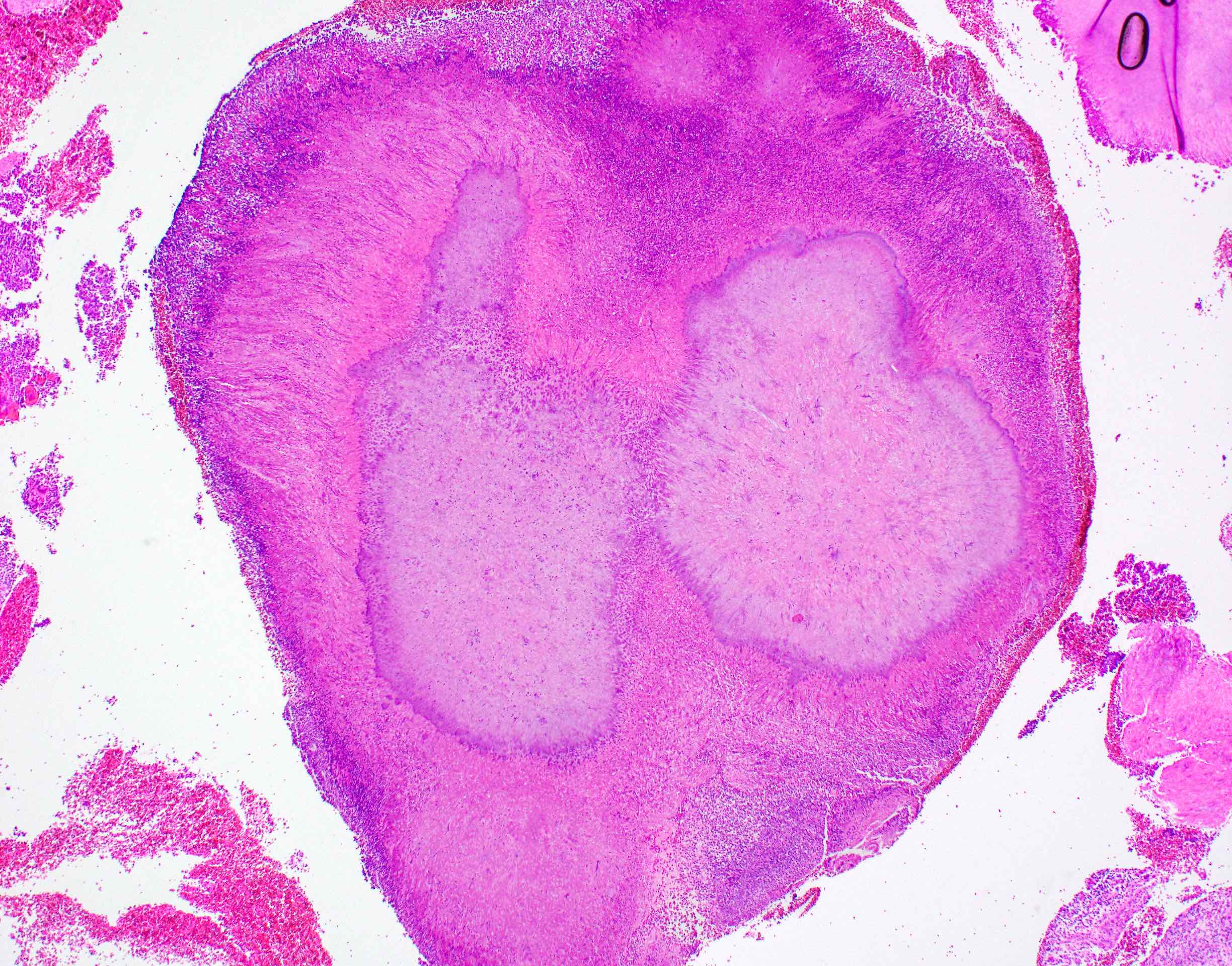
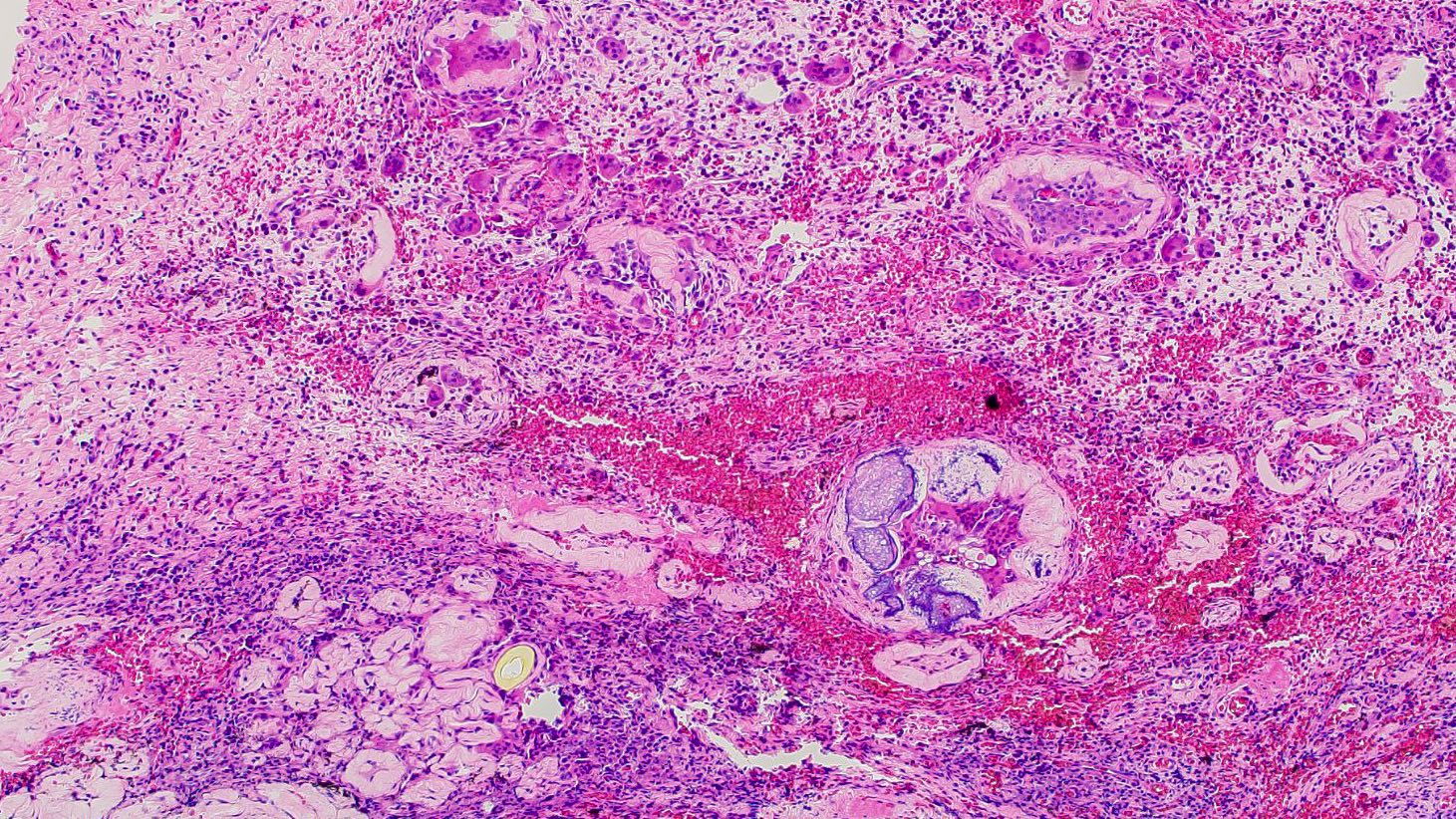
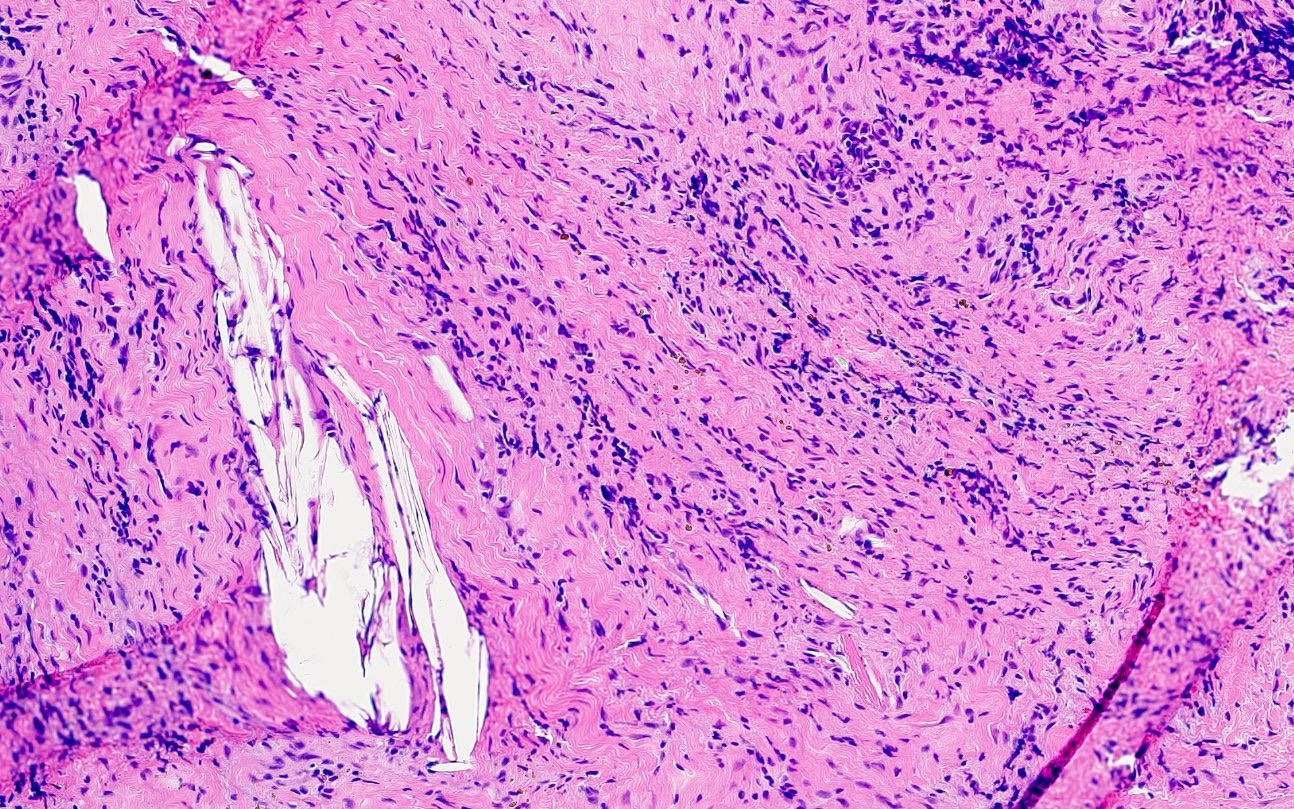
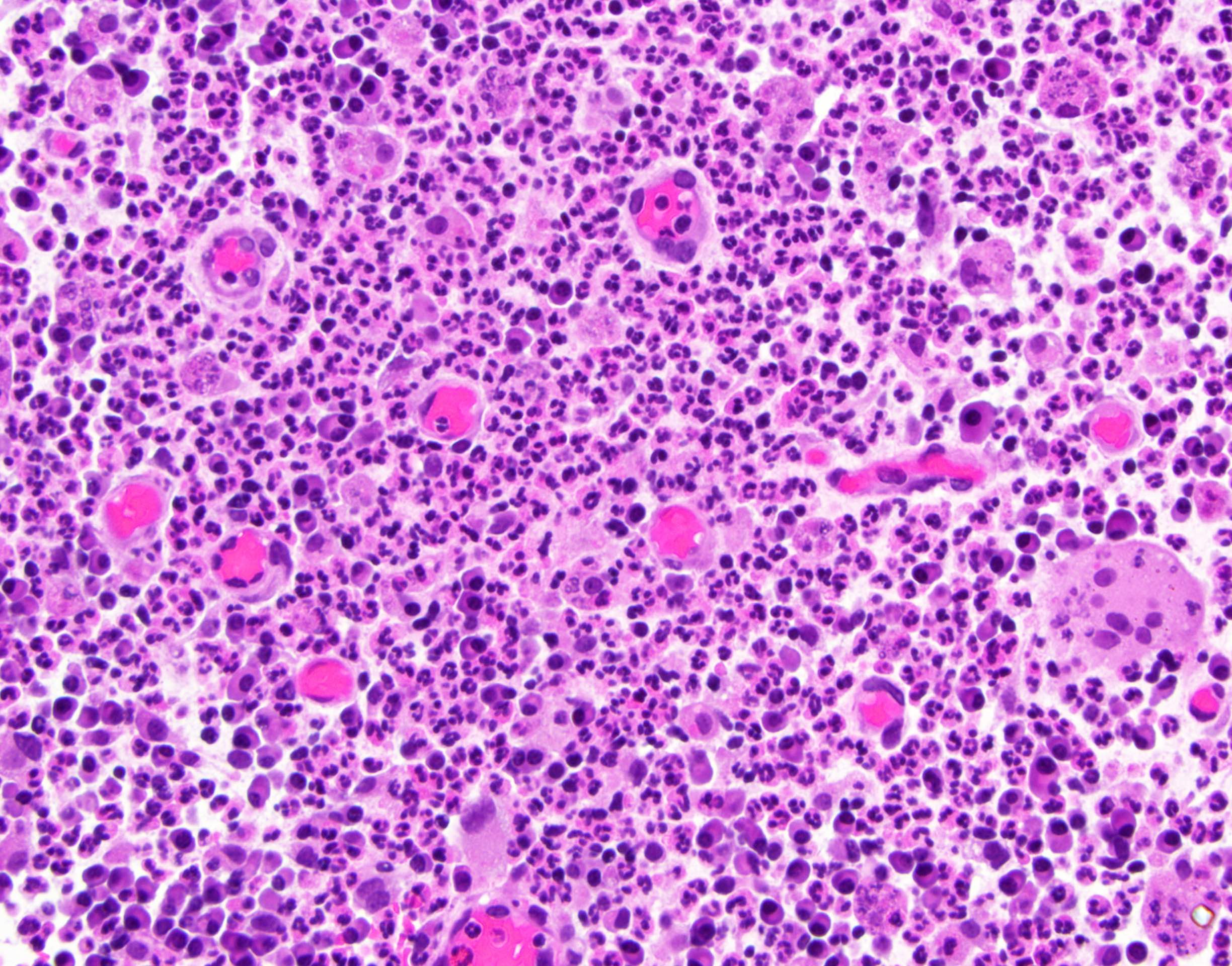
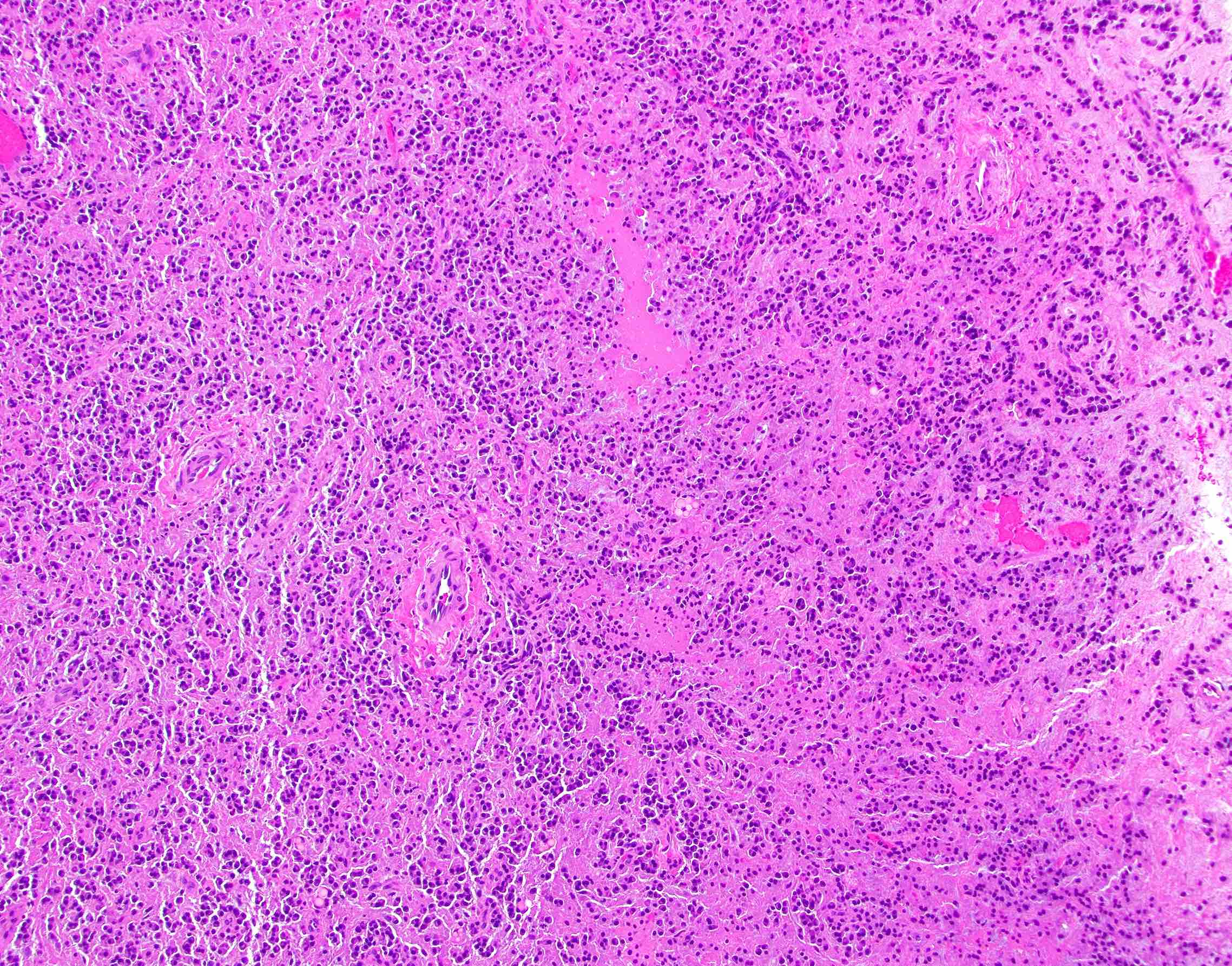
Microscopic (histologic) description
- Microscopic appearance depends on how long the lesion has been present, whether the tooth had prior treatment or whether there is a superimposed abscess
- Inflamed granulation or fibrous connective tissue
- May demonstrate
- Cholesterol aggregates with surrounding multinucleated giant cells, red blood cells and hemosiderin
- Pulse granulomas (giant cell hyaline angiopathy, hyaline bodies): pools of eosinophilic material with a corrugated periphery of condensed collagen, often surrounded by lymphocytes and multinucleated giant cells
- Thought to represent foreign body reaction to vegetable foreign material (J Indian Soc Periodontol 2015;19:327)
- Russell bodies or pyronine bodies: products of plasma cells, not specific to periapical granulomas (Oral Surg Oral Med Oral Pathol 1974;38:584)
- Spicules of bone, tooth or dystrophic calcifications
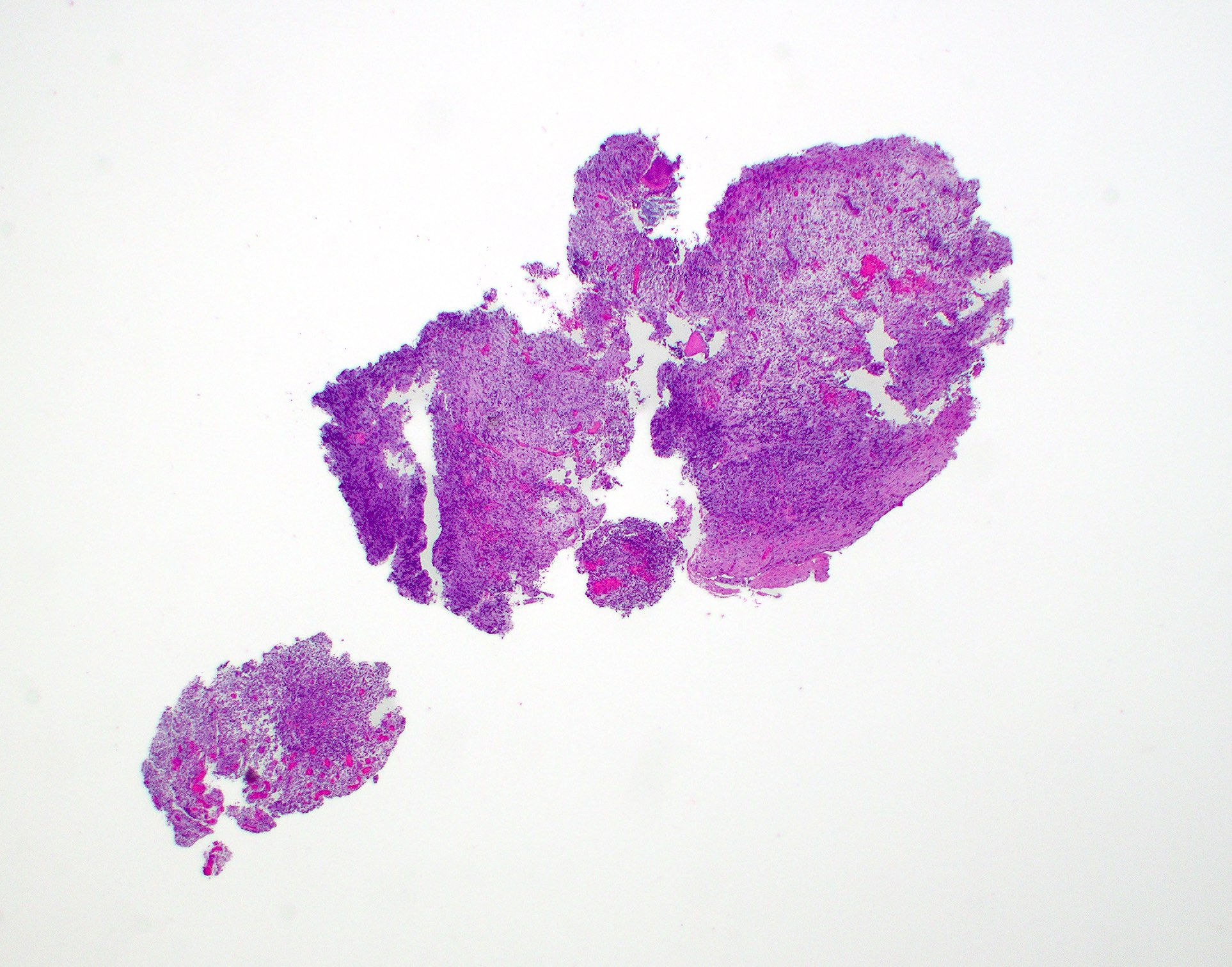
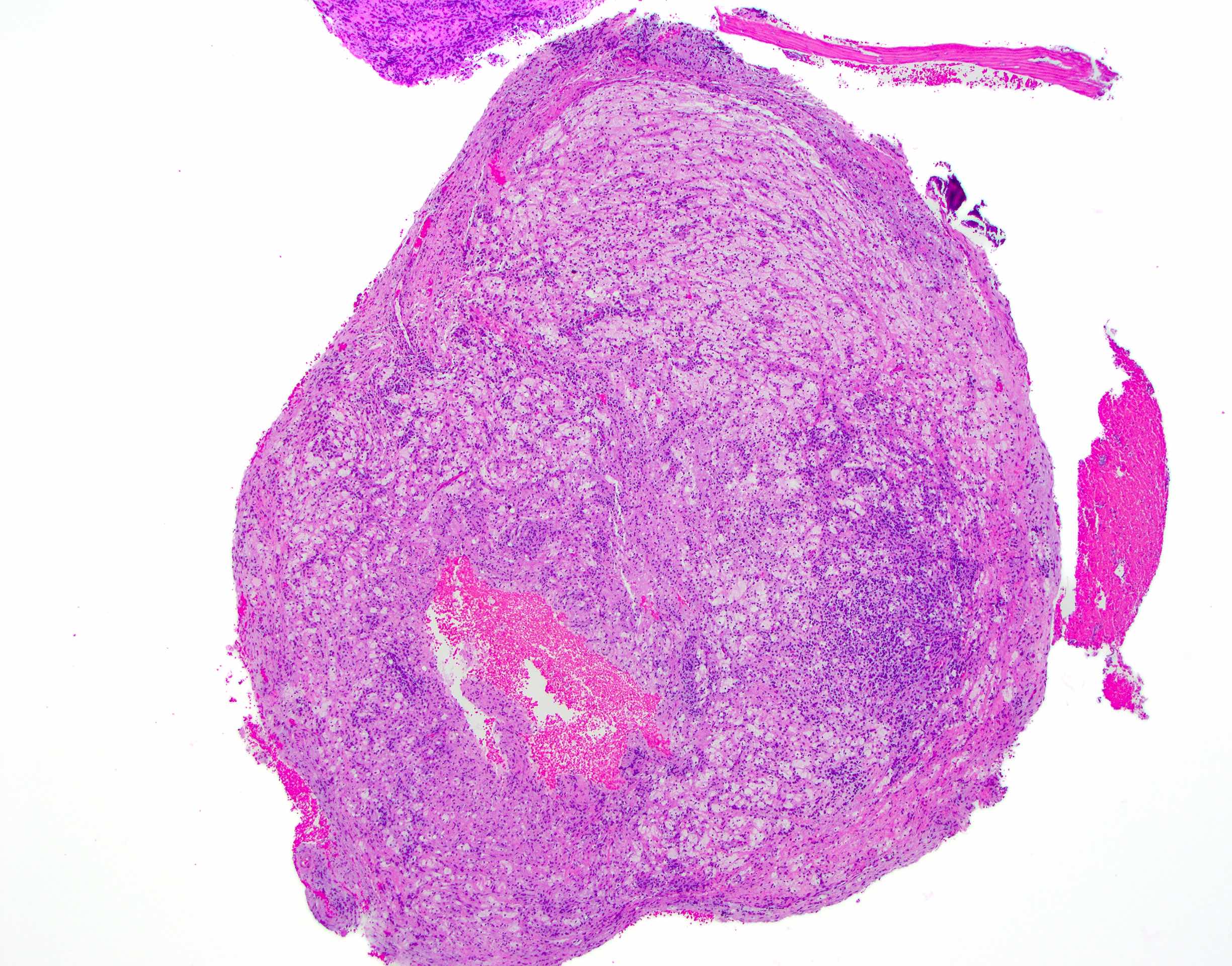
Microscopic (histologic) images
Negative stains
- Lacks prominent, diffuse staining with CD1a, langerin and S100 protein (Natl J Maxillofac Surg 2022;13:294)
- Polyclonal on immunostaining or in situ hybridization with kappa and lambda (while not necessary for diagnosis, may be useful in cases that demonstrate a dense plasmacytic population)
Videos
Etiology and clinical / radiographic characteristics
Sample pathology report
- Maxilla, apical to tooth #10:
- Subacutely inflamed fibrous connective tissue (see comment)
- Comment: When combined with the biopsy location and clinical symptom of dental pain, the histomorphology is compatible with a periapical granuloma.
Differential diagnosis
- Radiographic differential diagnosis is broad and may include a variety of inflammatory or noninflammatory, odontogenic or nonodontogenic lesions (cysts, tumors or nontumors) (Iran Endod J 2021;16:150)
- Primary histopathologic differential diagnosis:
- Periapical cyst (apical periodontal cyst):
- Identical to a periapical granuloma except that there is evidence of cystic lining
- Langerhans cell histiocytosis:
- Inflammatory infiltrate often contains an abundance of eosinophils
- Langerhans cells exhibit elongated nuclei with nuclear grooves / folds and a fine chromatin pattern
- Langerhans cells are reactive with CD1a, langerin and S100 (Natl J Maxillofac Surg 2022;13:294)
- Many cases are clonal and exhibit driver mutations associated with RAS / MAPK pathway
- Multiple myeloma / plasmacytoma:
- Kappa or lambda light chain restriction
- Periapical cyst (apical periodontal cyst):
Board review style question #1
A patient presents with dental pain on biting. The tooth tests nonvital and a radiolucency was noted around the apex of a tooth. Surgical removal of the lesion revealed loose, inflamed granulation tissue devoid of cystic epithelium. What is the most likely diagnosis?
- Langerhans cell histiocytosis
- Odontogenic keratocysts
- Periapical cyst
- Periapical granuloma
Board review style answer #1
D. Periapical granuloma. The histopathology shows loose, inflamed granulation tissue that contains a mixed inflammatory cell infiltrate, comprising neutrophils and plasma cells with scattered lymphocytes and a focal multinucleated giant cell. No evidence of epithelial lining or Langerhans cells are appreciated. Answer A is incorrect because Langerhans cell histiocytosis would demonstrate a proliferation of eosinophils and Langerhans cells, which have elongated nuclei, nuclear groves and a fine chromatin pattern. Answer C is incorrect because this lesion lacks overt epithelial lining. Answer B is incorrect because this lesion lacks an epithelial lining. Odontogenic keratocysts exhibit a regular epithelial lining with peripheral palisading of the basal cell layer and a luminal layer of corrugated parakeratin.
Comment Here
Reference: Periapical (dental) granuloma
Comment Here
Reference: Periapical (dental) granuloma
Board review style question #2
Board review style answer #2
D. Root canal therapy of the involved tooth. Root canal therapy or extraction treats the underlying cause of the problem. The inflamed bony lesion should heal after treating the etiology; however, in some cases, the inflamed tissue must be removed surgically (via apicoectomy) if the bony lesion does not heal. Answer A is incorrect because, while the antibiotics may calm the patient’s symptoms and temporarily reduce some of the inflammation, they do not treat the underlying cause of the problem. Answer B is incorrect because chemotherapy is inappropriate treatment for a benign infection. Answer C is incorrect because an en bloc resection is gross overtreatment.
Comment Here
Reference: Periapical (dental) granuloma
Comment Here
Reference: Periapical (dental) granuloma