Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Frozen section description | Frozen section images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Nasri E, Reith JD. Aneurysmal bone cyst. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/boneabc.html. Accessed December 25th, 2024.
Definition / general
- Benign, locally destructive multiloculated blood filled cystic lesion of bone
- Classified as an osteoclastic giant cell rich tumor (WHO 2020)
- Primary and secondary forms
- High rate of local recurrence
Essential features
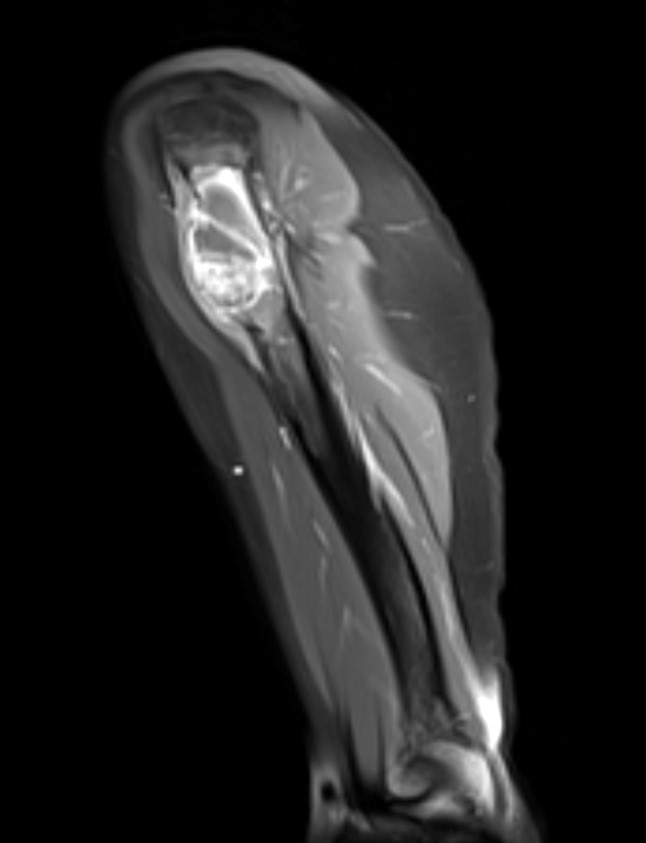
- Imaging: multiloculated lesion with fluid-fluid levels, best appreciated on MRI
- Histology: cyst walls composed of fibroblasts, woven bone and osteoclastic giant cells
- Molecular: rearrangement of USP6 gene (primary form only)
Terminology
- Related term: giant cell lesion of small bones
ICD coding
- ICD-10: M85.50 - aneurysmal bone cyst, unspecified site
Epidemiology
- Rare; 2.5% of all primary bone tumors
- M = F
- In mandible and maxilla, more common in young women
- More common in skeletally immature patients
- Peak incidence in second decade (J Pediatr Orthop B 2004;13:389)
Sites
- Broad skeletal distribution
- Metaphyseal region of long tubular bones, most commonly the femur, tibia and humerus
- Posterior elements of vertebrae
Etiology
- Historically thought to be reactive to underlying vascular events
- Recent molecular data supportive of neoplastic etiology (Genes Chromosomes Cancer 1999;26:265, AJR Am J Roentgenol 1995;164:573)
Clinical features
- Pain and swelling
- Pathologic fracture
- Nerve compression symptoms in cases of vertebral column involvement
- May massively expand the mandible
Diagnosis
- Requires correlation of clinical, radiographic and histologic findings to distinguish primary from secondary aneurysmal bone cyst
- Lack of immunoreactivity for H3G34W (and other histone antibodies) is helpful in excluding giant cell tumor with cystic features
Radiology description
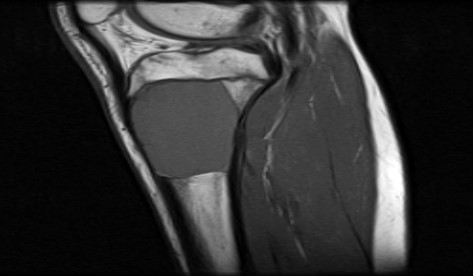
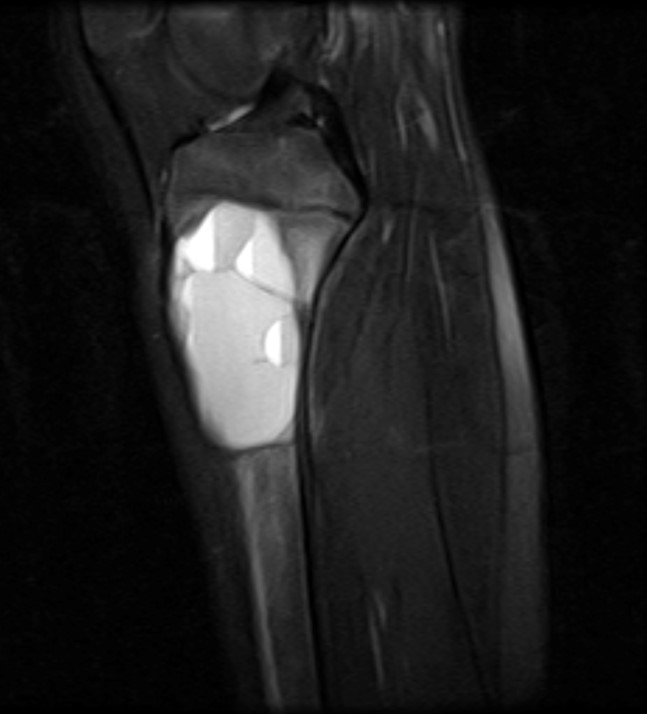
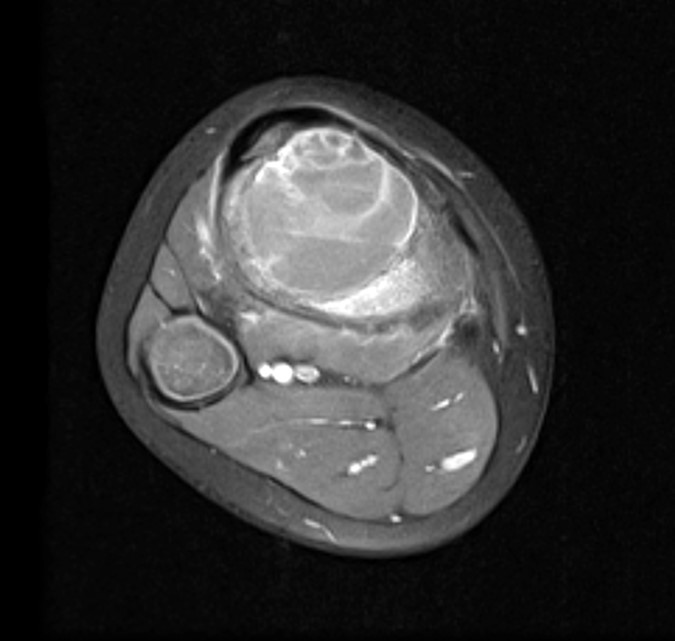
- Xray:
- Eccentric radiolucent lesion with expansile remodeling, involving the metaphysis of long bones
- Finger in the balloon sign possible (Orthop Traumatol Surg Res 2015;101:S119)
- CT scan:
- Well delineated lytic lesion, usually with thin rim of reactive bone
- Fluid-fluid levels occasionally visible
- MRI:
- Multiloculated cyst with characteristic fluid-fluid levels
- Isotope scan:
- Peripheral uptake with central photopenia imparts a donut-like appearances
Radiology images
Prognostic factors
- Up to a third have local recurrence (Clin Orthop Relat Res 2008;466:722)
- Rare case reports of metastatic aneurysmal bone cyst (Virchows Arch 2009;455:455)
Case reports
- 7 year old girl with aneurysmal bone cyst in the cervical spine (BMJ Case Rep 2019;12:e231870)
- 12 year old girl with giant aneurysmal bone cyst of the mandible (Natl J Maxillofac Surg 2013;4:107)
- 22 year old man with fracture of an intertrochanteric aneurysmal bone cyst (Cureus 2019;11:e6461)
- 26 year old man with solid variant of aneurysmal bone cyst of the heel (J Med Case Rep 2011;5:145)
- 48 year old woman with metastatic potential of an aneurysmal bone cyst (Virchows Arch 2009;455:455)
Treatment
- Curettage or en bloc resection
- Percutaneous sclerotherapy with doxycycline (Bone Joint J 2020;102-B:186)
- Arterial embolization
- Steroid or calcitonin injection
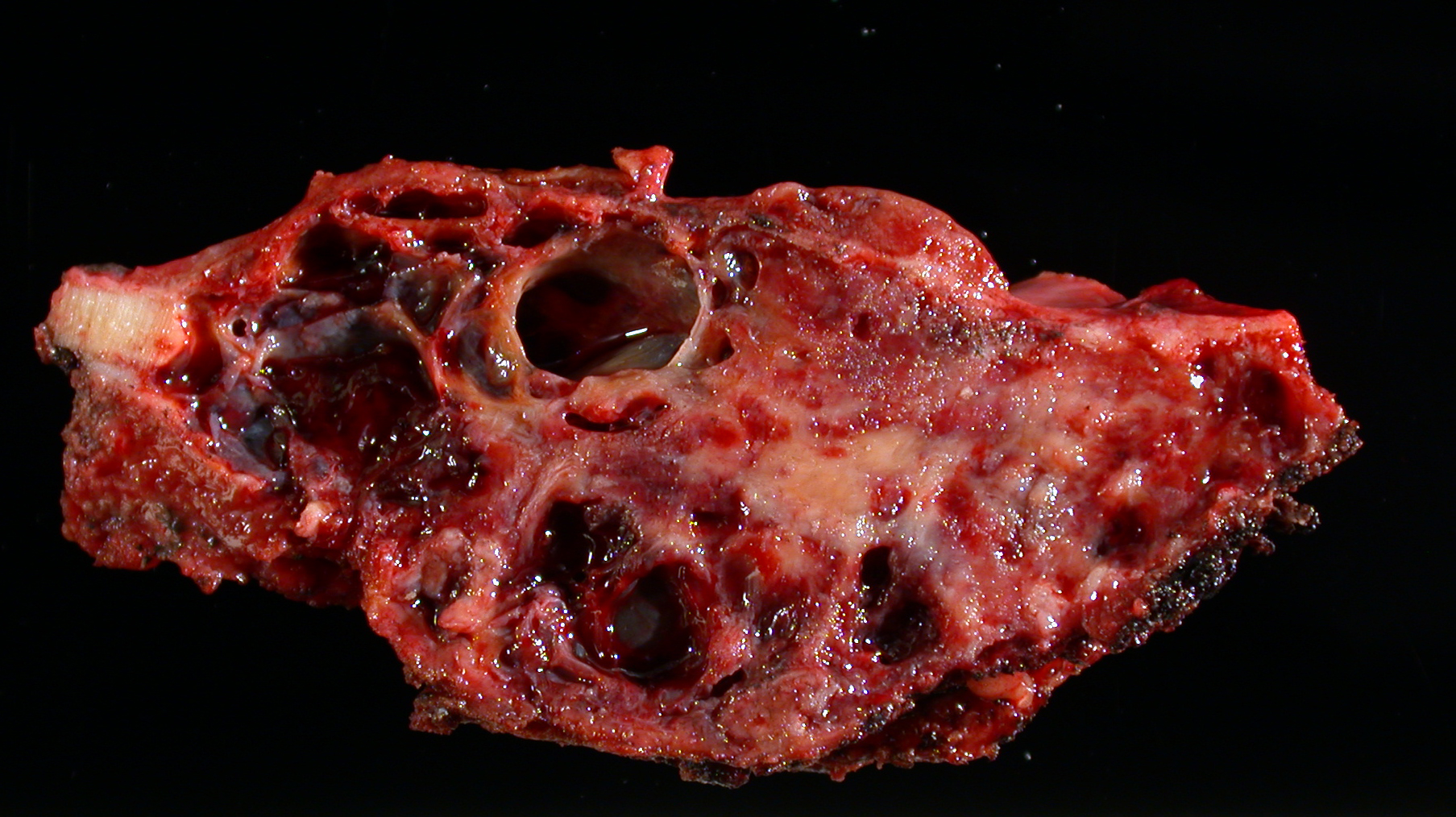
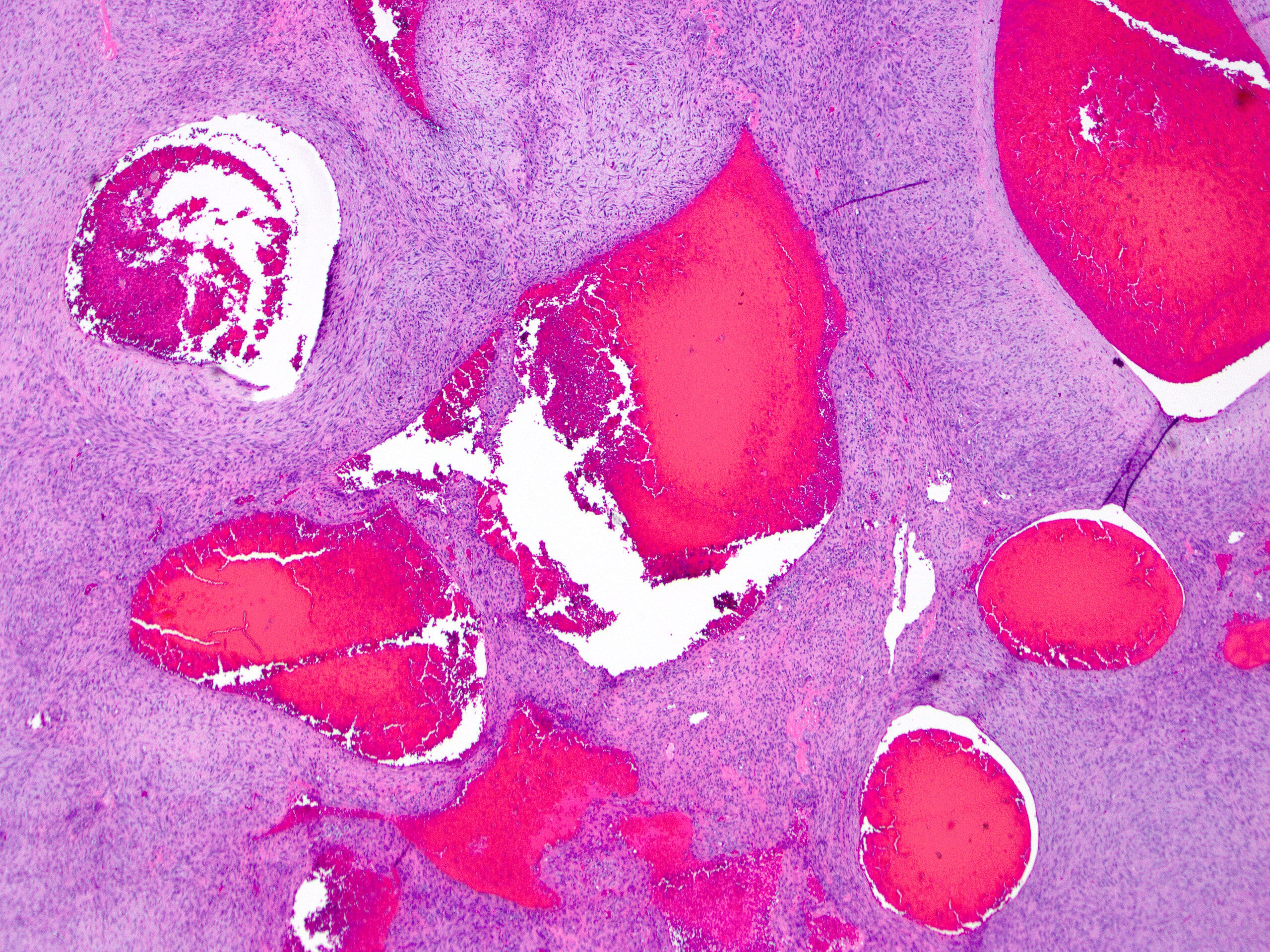
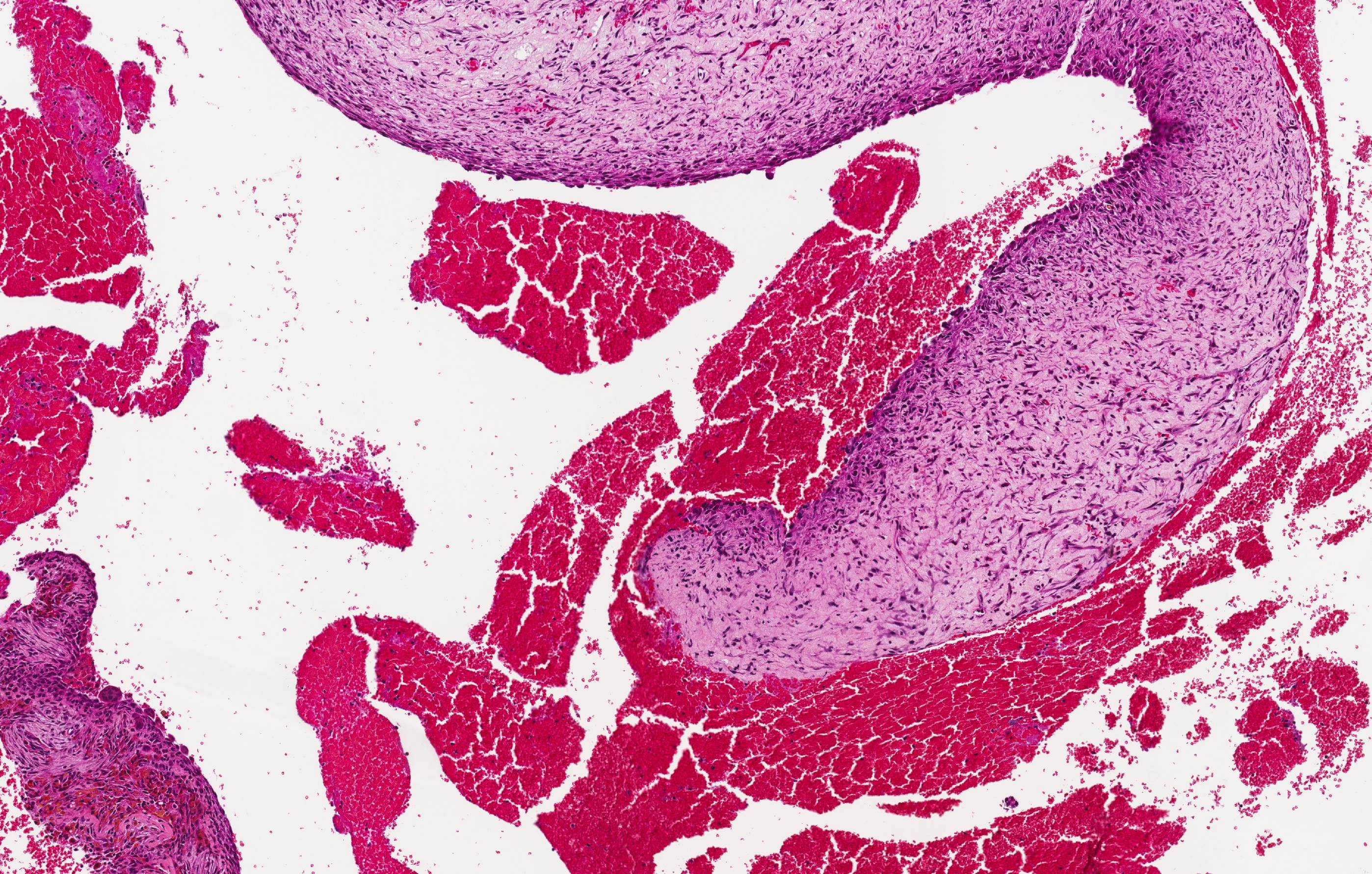
Gross description
- Spongy, multiloculated, hemorrhagic lesion
- Variable size
- Irregular, sharply demarcated borders with thin shell of reactive bone
- Variable amount of solid component
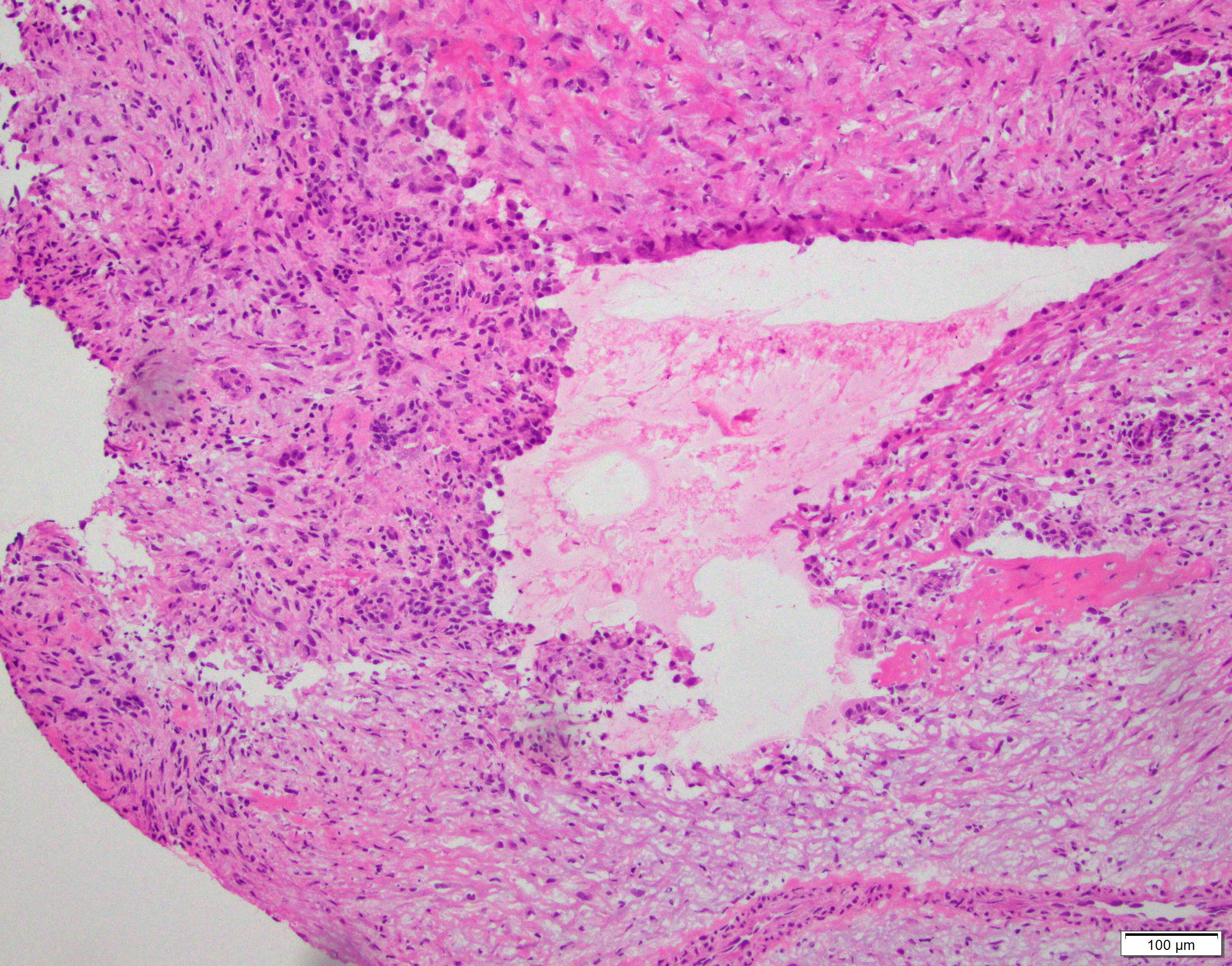
Frozen section description
- Usually small fragments of cellular septa containing:
- Fibroblast-like stromal cells lacking cytologic atypia
- Osteoclast-like giant cells
- Reactive woven bone
- Mitotic activity typically present, no atypical mitoses
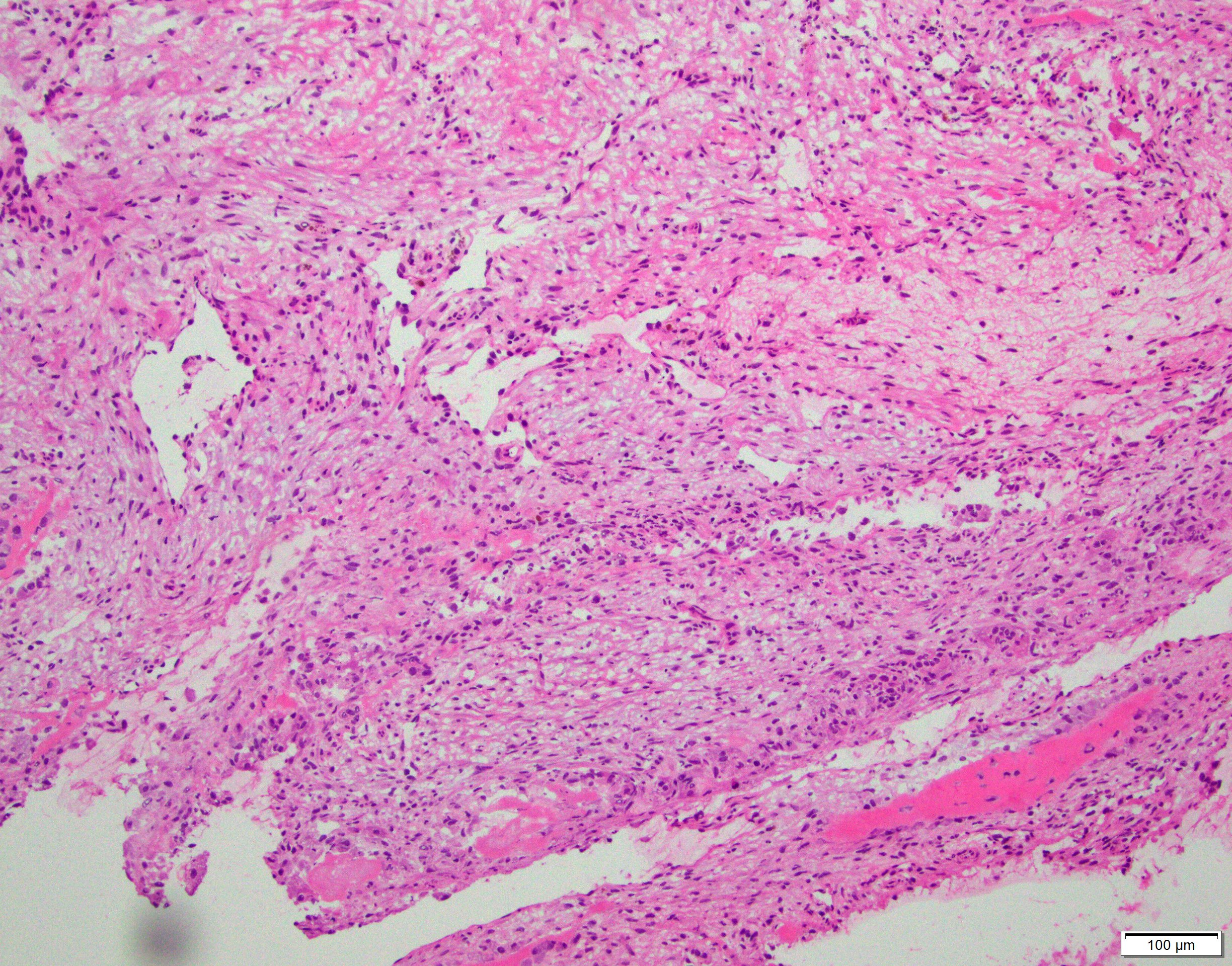
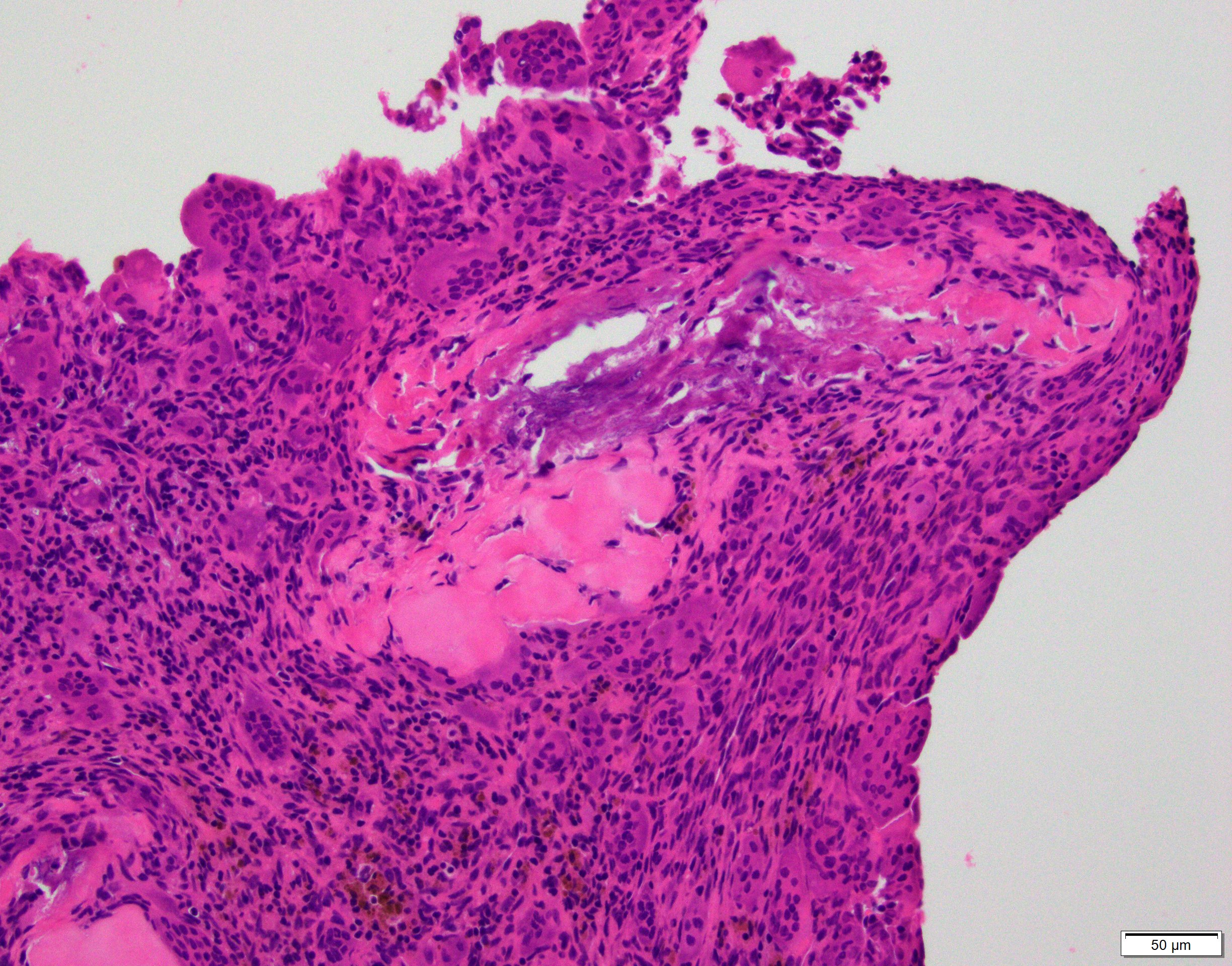
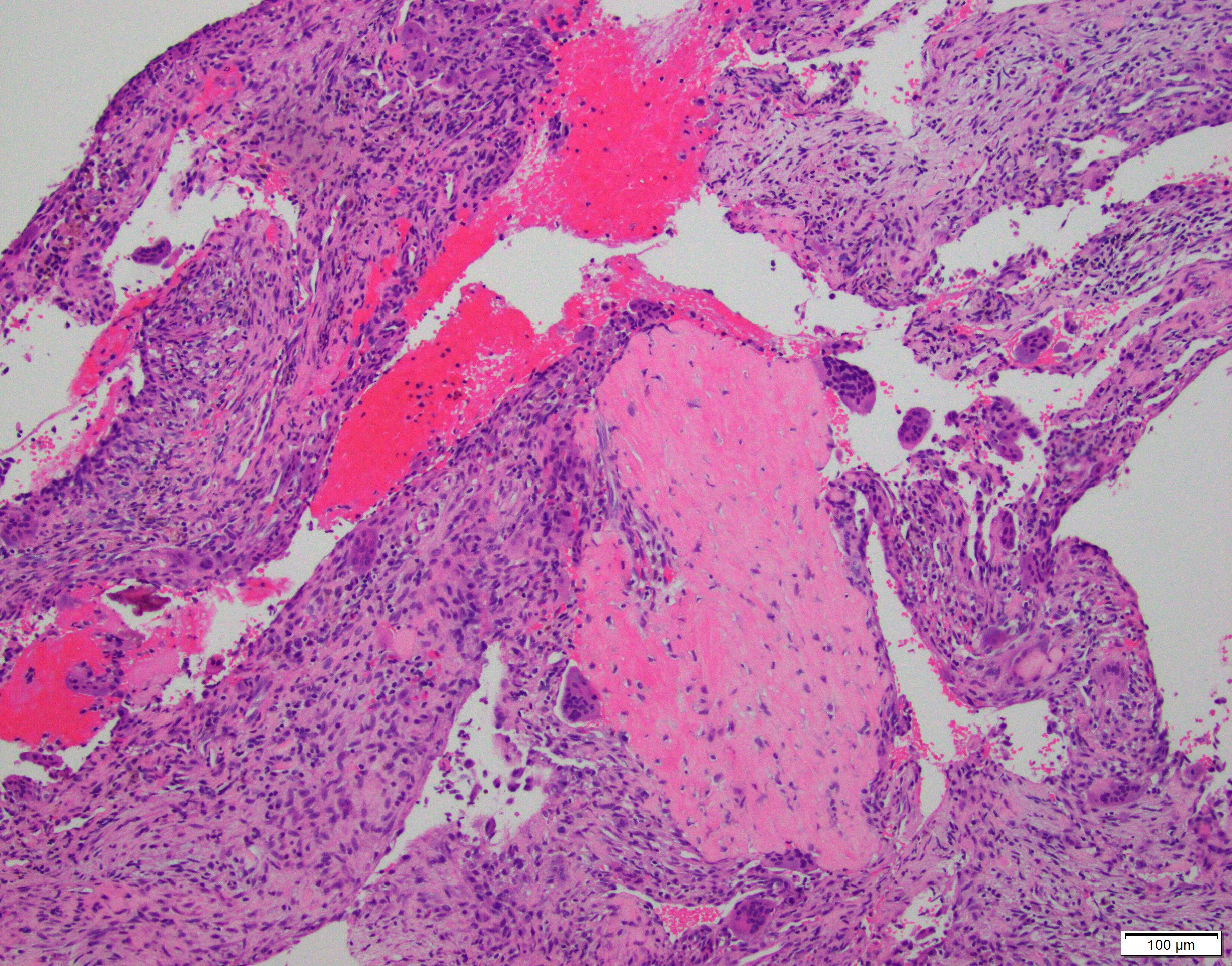
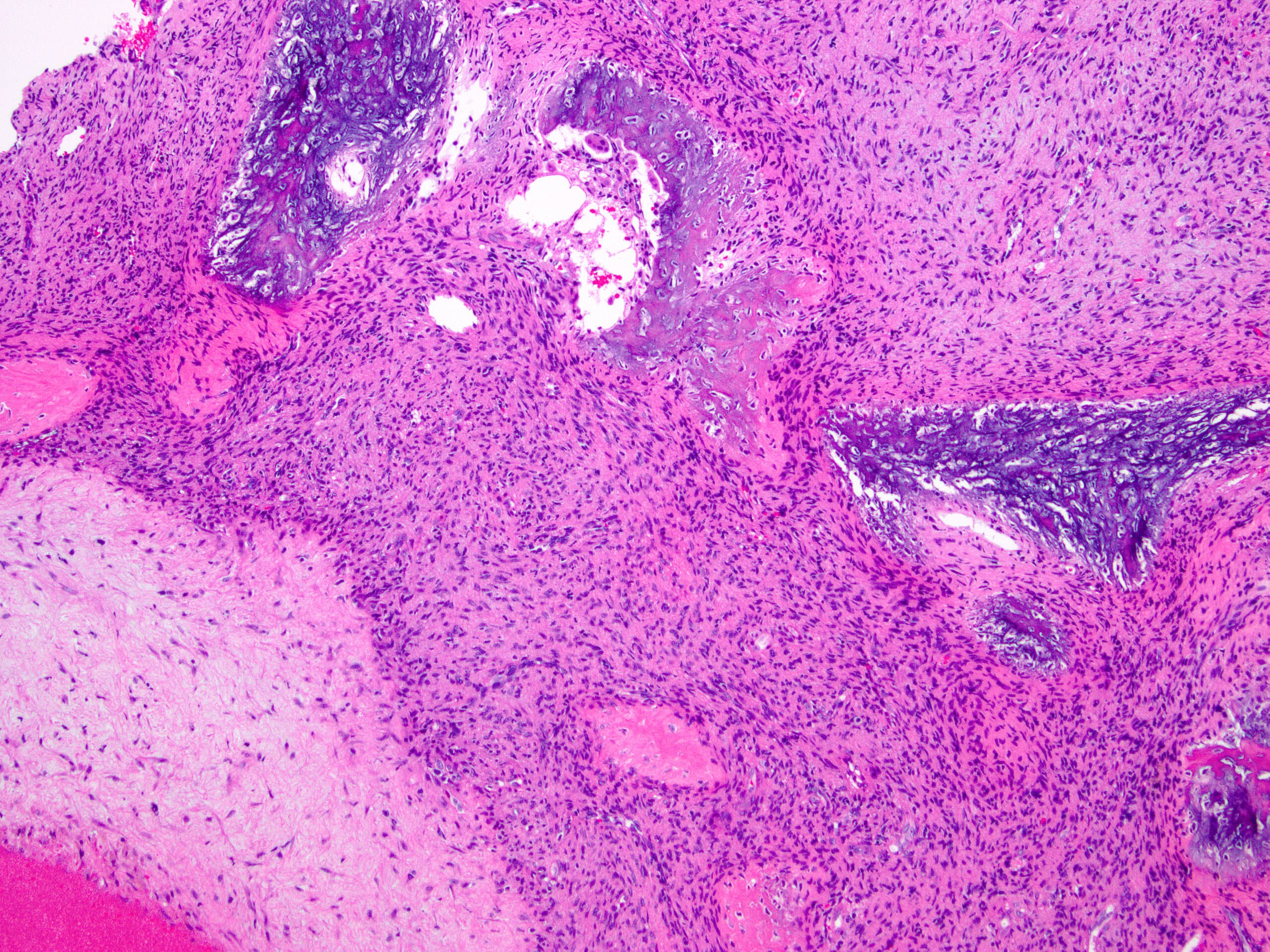
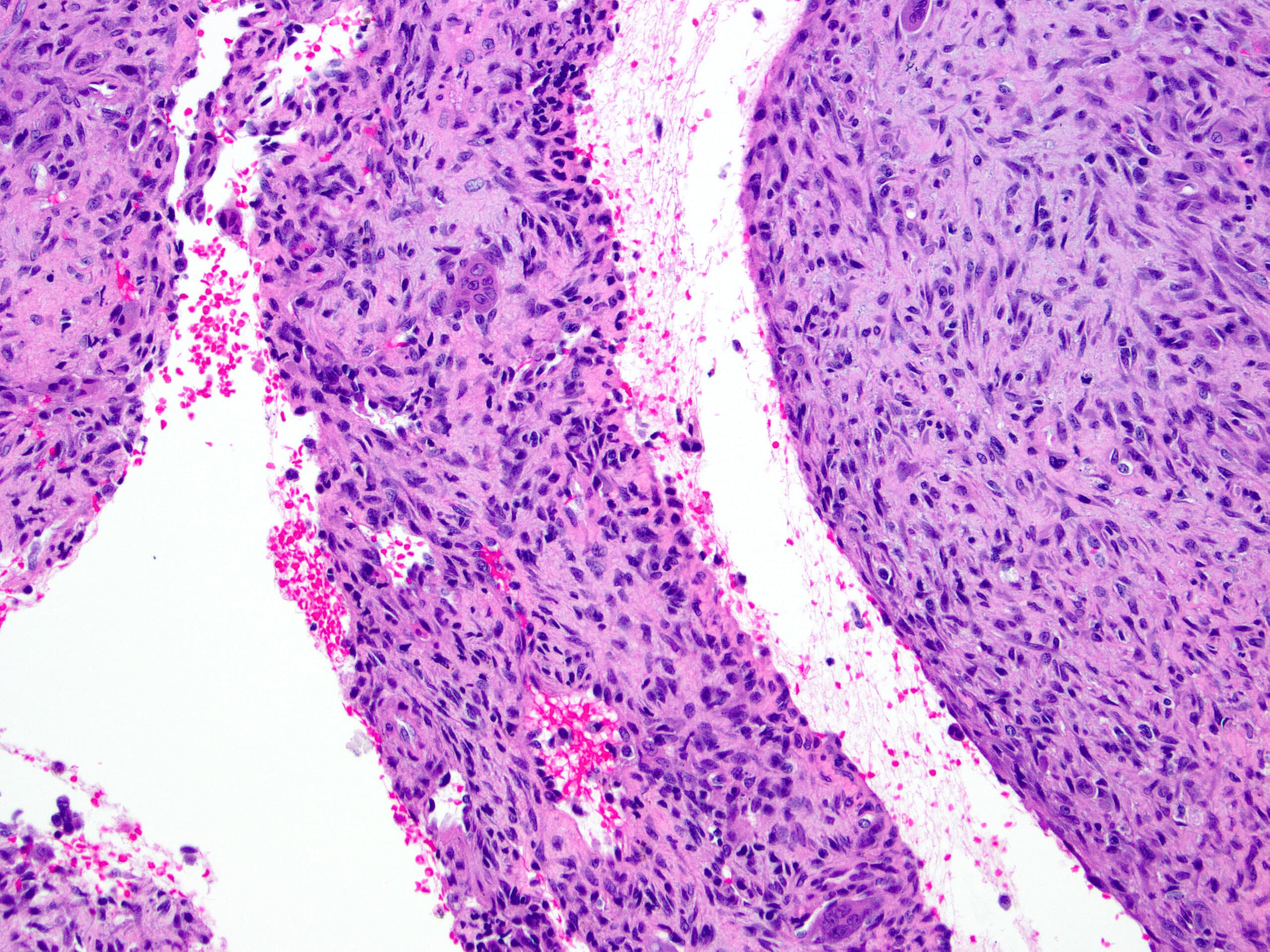
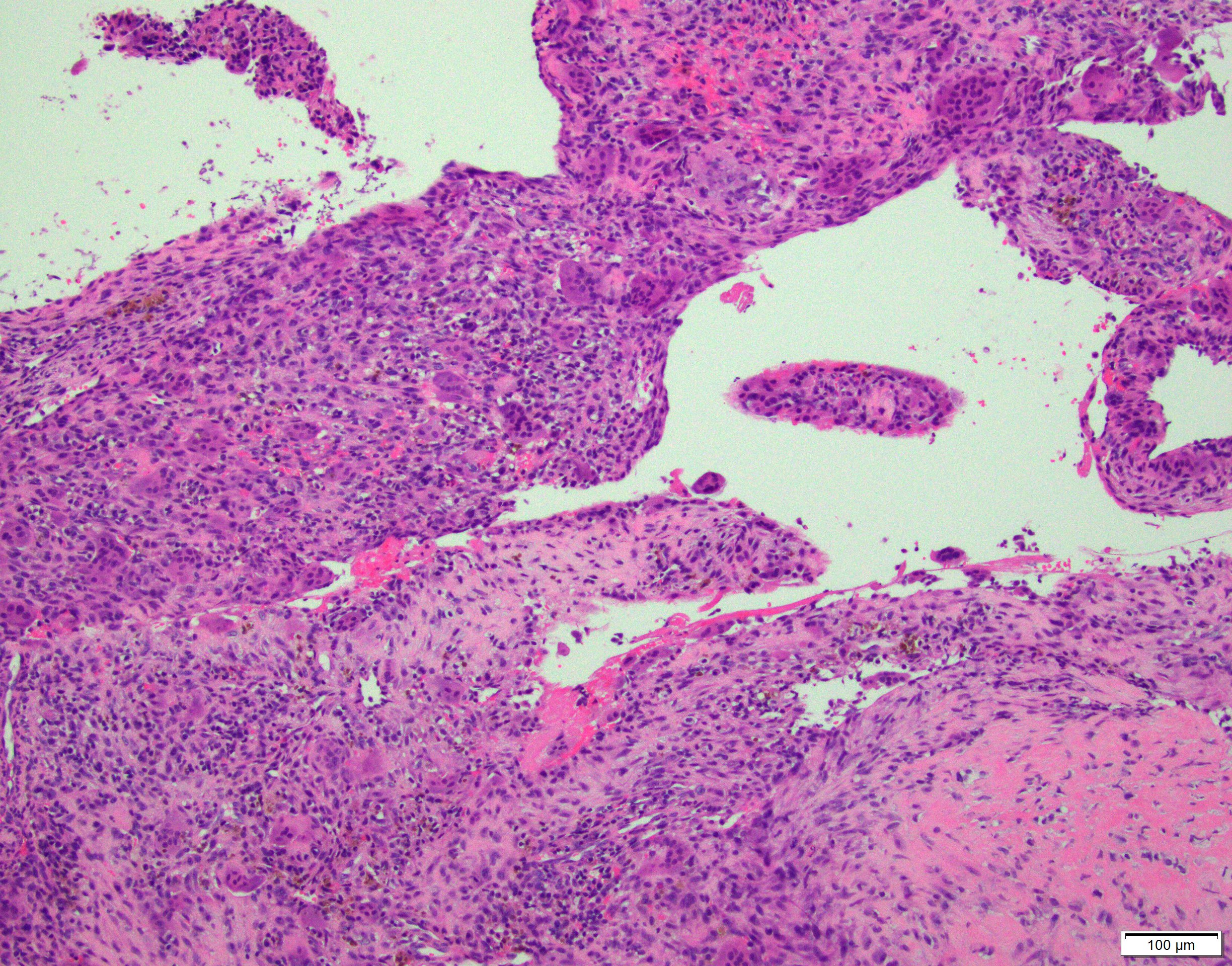
Microscopic (histologic) description
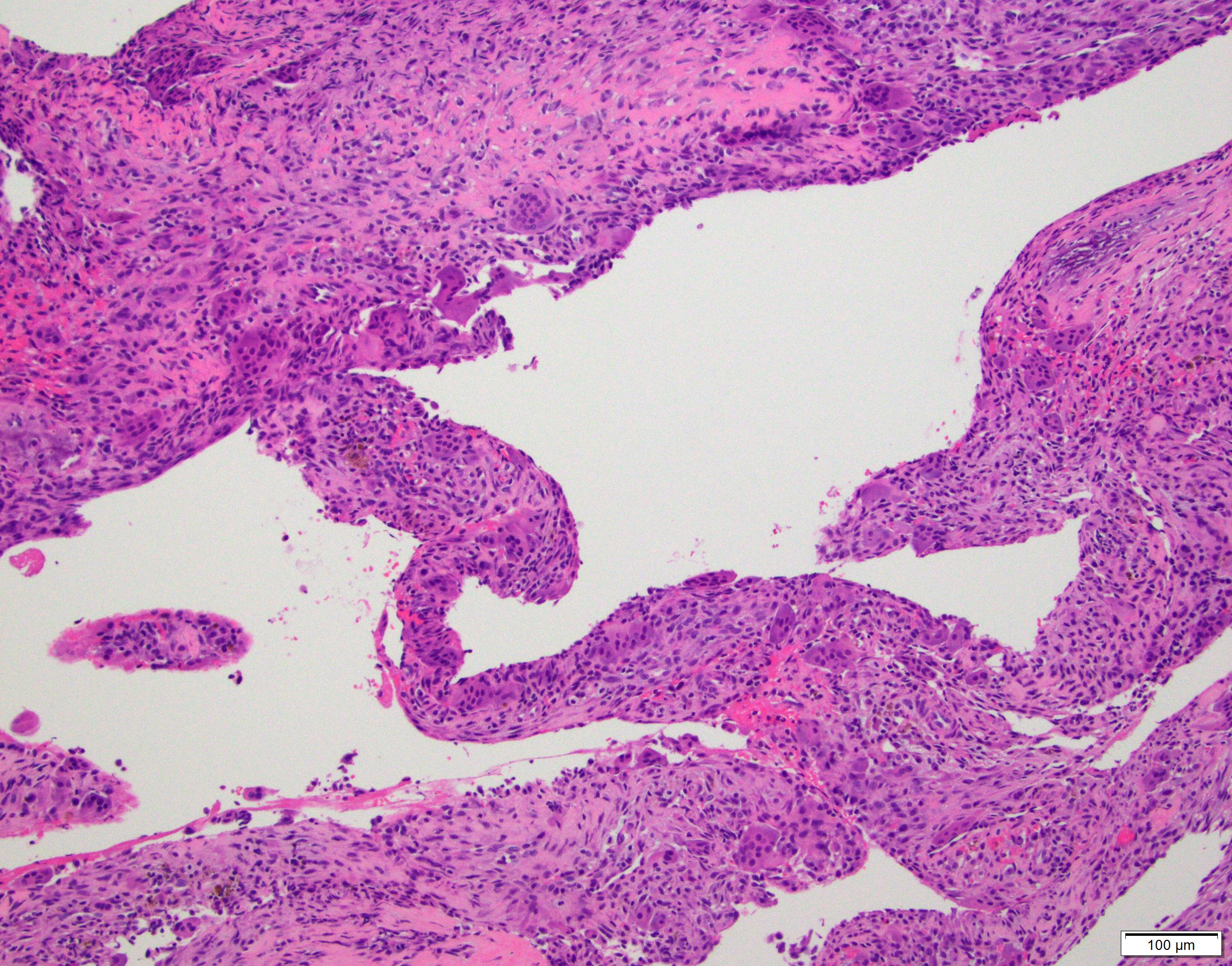
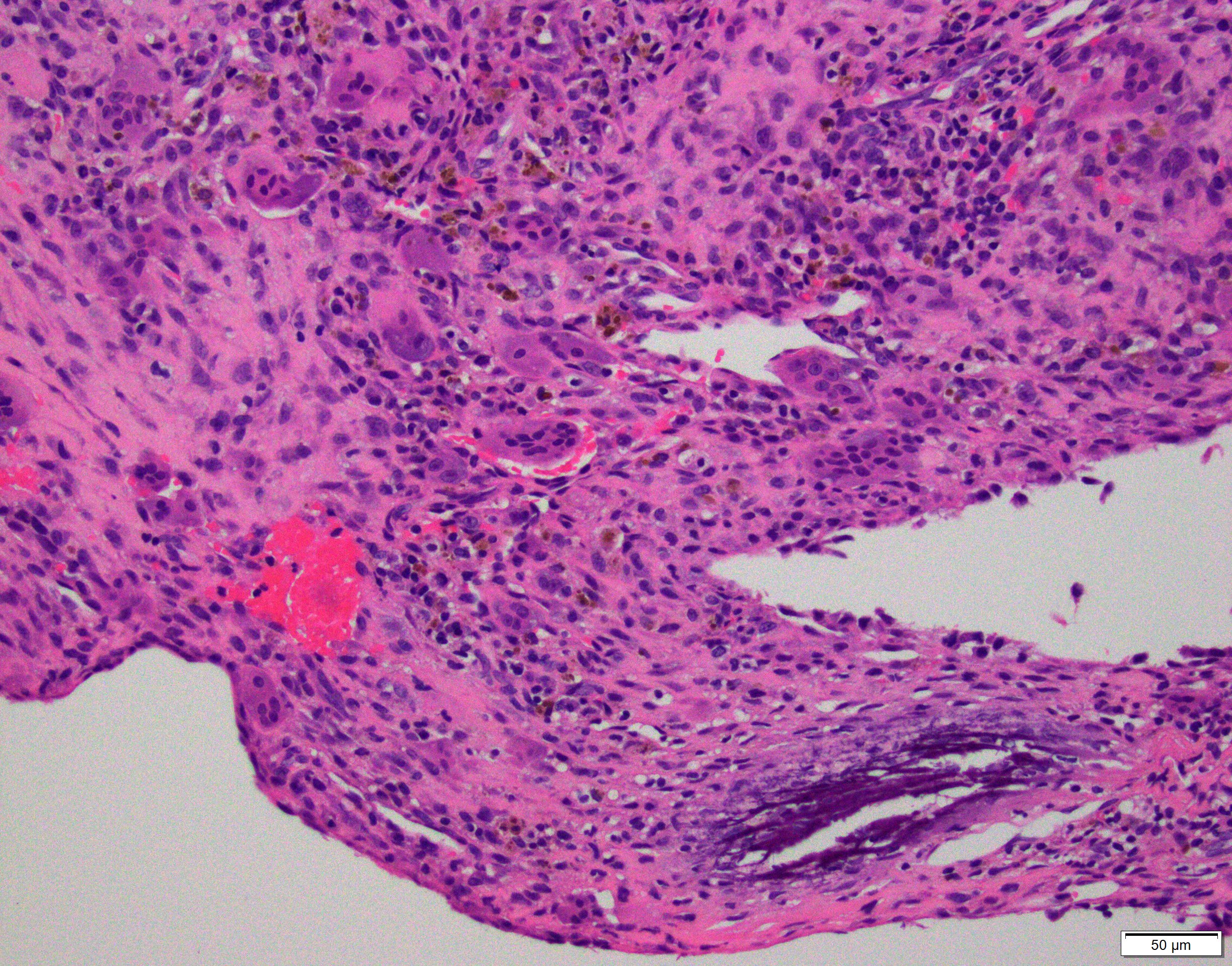
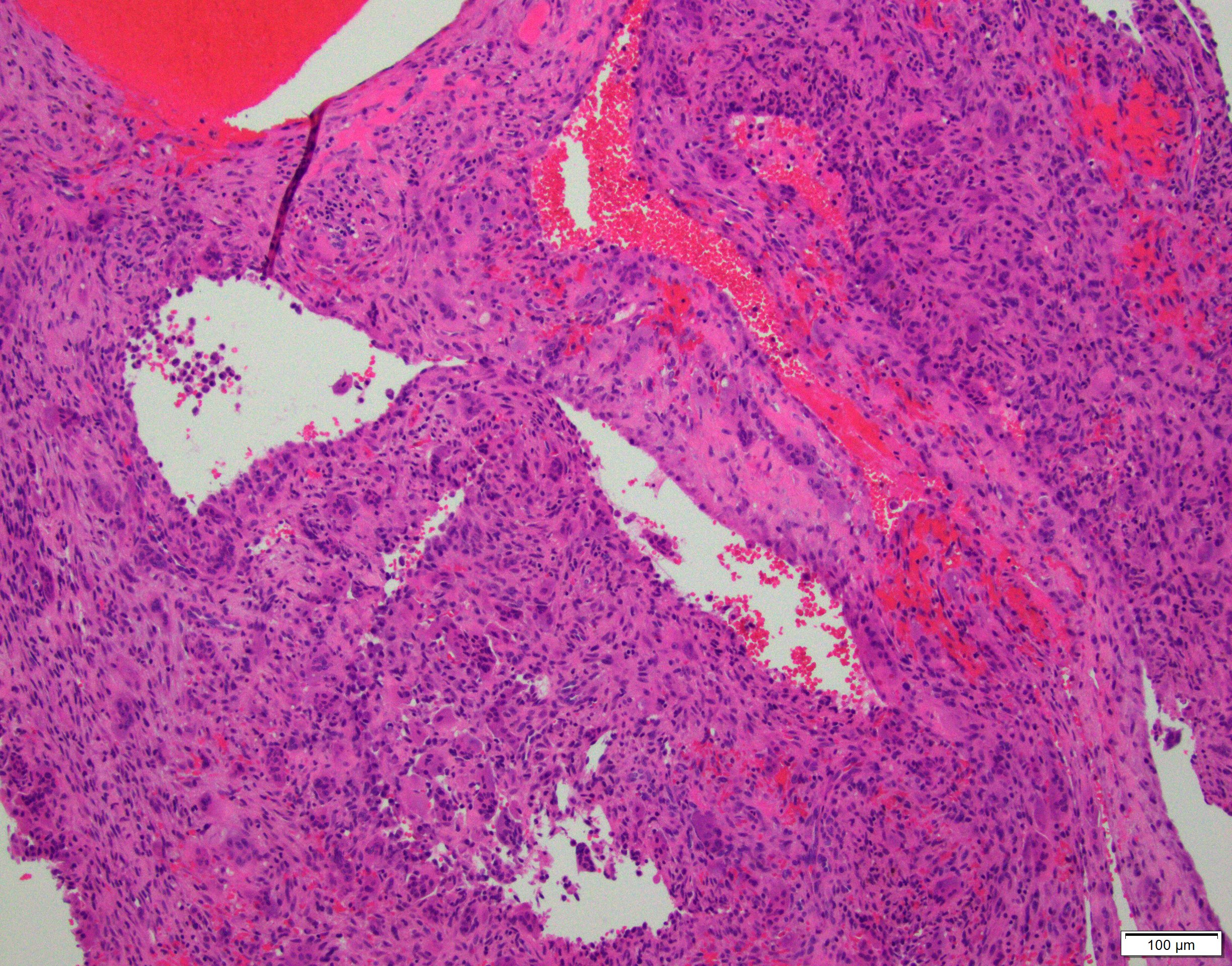
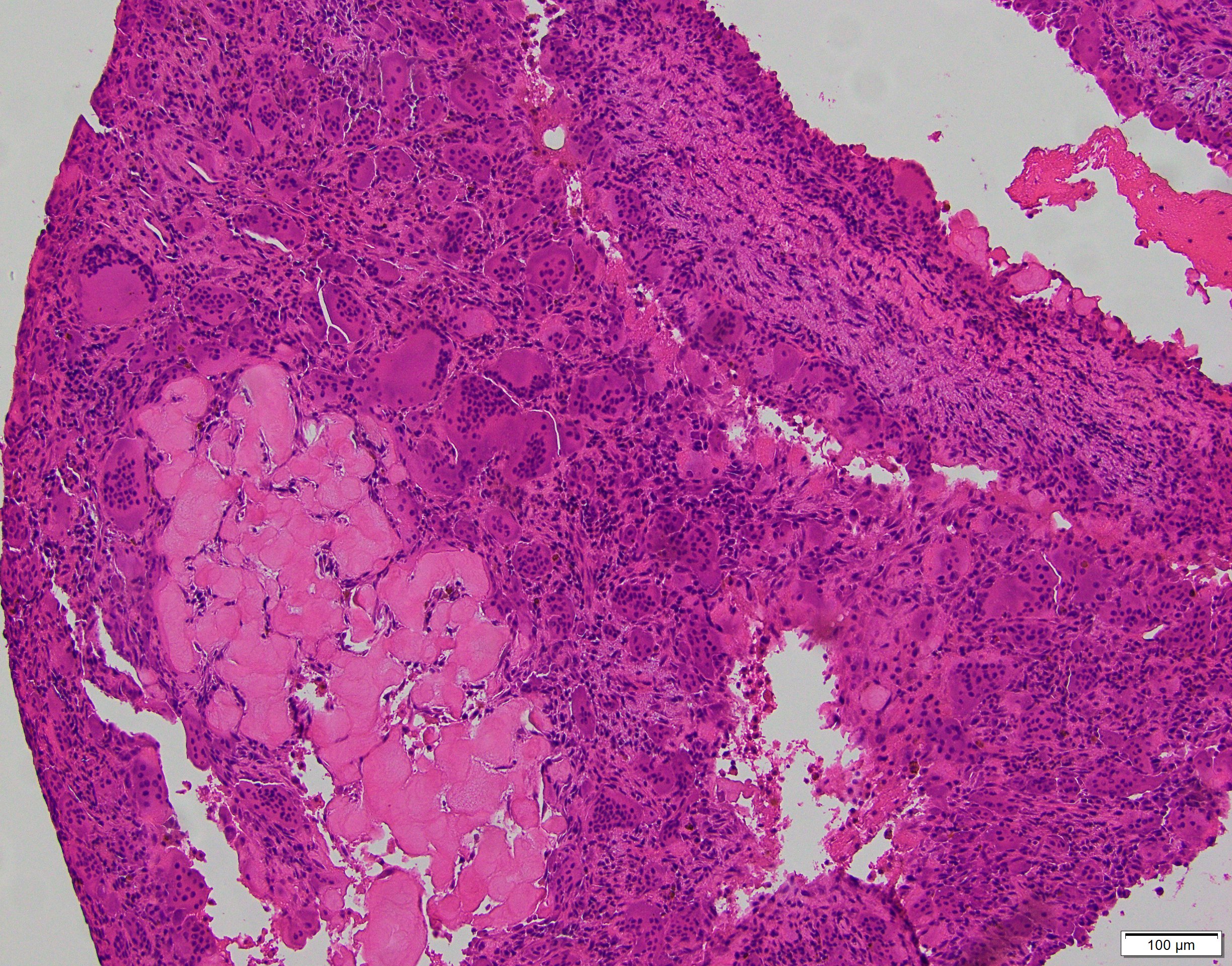
- Multiloculated cystic lesion
- Blood filled cystic spaces separated by cellular septa containing fibroblasts, giant cells and woven bone
- Calcified, basophilic material (blue reticulated chondroid-like material)
- Necrosis not common but mitotic activity is easily identified
- No cytologic atypia (Am J Clin Pathol 2015;143:823)
- Numerous giant cells in connective tissue that line large sinusoidal spaces
Microscopic (histologic) images
Contributed by Elham Nasri, M.D. and Kelly Magliocca, D.D.S., M.P.H.
Positive stains
- There is no specific immunohistochemical stain for aneurysmal bone cyst
Molecular / cytogenetics description
- Abnormalities of 17p13.2 locus in 63% (Mod Pathol 2004;17:518)
- Fusion of USP6 with:
- CDH11 (most frequent, approximately 30%), TRAP150 (THRAP3), ZNF9 (CNBP), OMD, COL1A1, RUNX2, PAFAH1B1, CTNNB1, SEC31A, E1F1, FOSL2, STAT3, USP9X, ASAP1, FAT1, SAR1A, TNC (Genes Chromosomes Cancer 2017;56:266, Genes Chromosomes Cancer 2019;58:589, Genes Chromosomes Cancer 2020;59:357)
- Fusion of USP6 with:
- Rare case report of unusually aggressive aneurysmal bone cyst with RUNX2-USP6 fusion (Cancer Genet 2017;212:13)
- Rearrangement of USP6 gene can be detected by FISH or fusion panel analysis by next generation sequencing
- Other neoplasms with USP6 gene rearrangement: (Pathologe 2018;39:191)
- Myositis ossificans
- Nodular fasciitis
Sample pathology report
- Mass, distal metaphysis, left tibia, curettage:
- Aneurysmal bone cyst
Differential diagnosis
- Telangiectatic osteosarcoma:
- The most important differential diagnosis
- Similar architecture but contains anaplastic stromal cells
- Frequent atypical mitoses
- No specific diagnostic immunohistochemical stain
- Lacks USP6 gene rearrangement (Med Pregl 2015;68:127)
- Central giant cell granuloma:
- Involve gnathic bones
- Usually solid with no / minimal cystic component (mimics solid aneurysmal bone cyst)
- Lacks USP6 gene rearrangement (J Oral Maxillofac Pathol 2018;22:173)
- Secondary aneurysmal bone cyst:
- Lacks USP6 gene rearrangement
- Extensive sampling is critical to rule out an underlying primary lesion
- More common in:
- Fibrous dysplasia
- Giant cell tumor of bone
- Chondroblastoma
- Osteoblastoma
- Osteosarcoma (Am J Pathol 2004;165:1773)
Additional references
Board review style question #1
- Which of the following lesions does not have characteristic rearrangement of USP6 gene?
- Giant cell tumor of bone with secondary aneurysmal bone cyst
- Myositis ossificans
- Nodular fasciitis
- Primary aneurysmal bone cyst
Board review style answer #1
A. Secondary aneurysmal bone cyst lacks USP6 gene rearrangement.
Comment Here
Reference: Aneurysmal bone cyst (ABC)
Comment Here
Reference: Aneurysmal bone cyst (ABC)
Board review style question #2
Board review style answer #2
A. Aneurysmal bone cyst. The H&E shows cystic spaces with stromal giant cells. Rearrangement of USP6 gene confirms the diagnosis in the above clinical and radiographic context.
Comment Here
Reference: Aneurysmal bone cyst (ABC)
Comment Here
Reference: Aneurysmal bone cyst (ABC)