Table of Contents
Definition / general | Essential features | Terminology | Diagrams / tables | Quality improvement approaches | EPIDEM principles | EPIDEM steps | Examples of EPIDEM | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Zhou Y. Principles of laboratory quality improvement. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/managementlabprincipleslabQA.html. Accessed April 2nd, 2025.
Definition / general
- Quality improvement (QI) is the framework to systematically improve patient care (Agency for Healthcare Research and Quality: Approaches to Quality Improvement [Accessed 11 September 2020])
- Multiple quality improvement models and tools are available but the one that you can remember and use is the best one
Essential features
- Quality assurance ≠ quality improvement (Agency for Healthcare Research and Quality: Table 4.1. Quality Assurance vs. Quality Improvement [Accessed 6 October 2020]
- Principles of quality improvement:
- Good intentions are not good enough
- Set worthwhile goals
- Understand processes and systems
- Go for the high yield
- It doesn't count unless you can measure it
- Your job is never done
- EPIDEM
- Definition: EPIDEMic of healthcare professionals improving patient care
- Exploration, promotion, implementation, documentation, evaluation, modification
Terminology
- Other quality improvement terms to be familiar with
- Total quality management (TQM): organizational / management approach
- Root cause analysis (RCA): tool used in engineering and required for healthcare sentinel events
- Failure modes and effects analysis (FMEA): used by U.S. military and NASA
- Health failure modes and effects analysis (HFMEA): used by VA
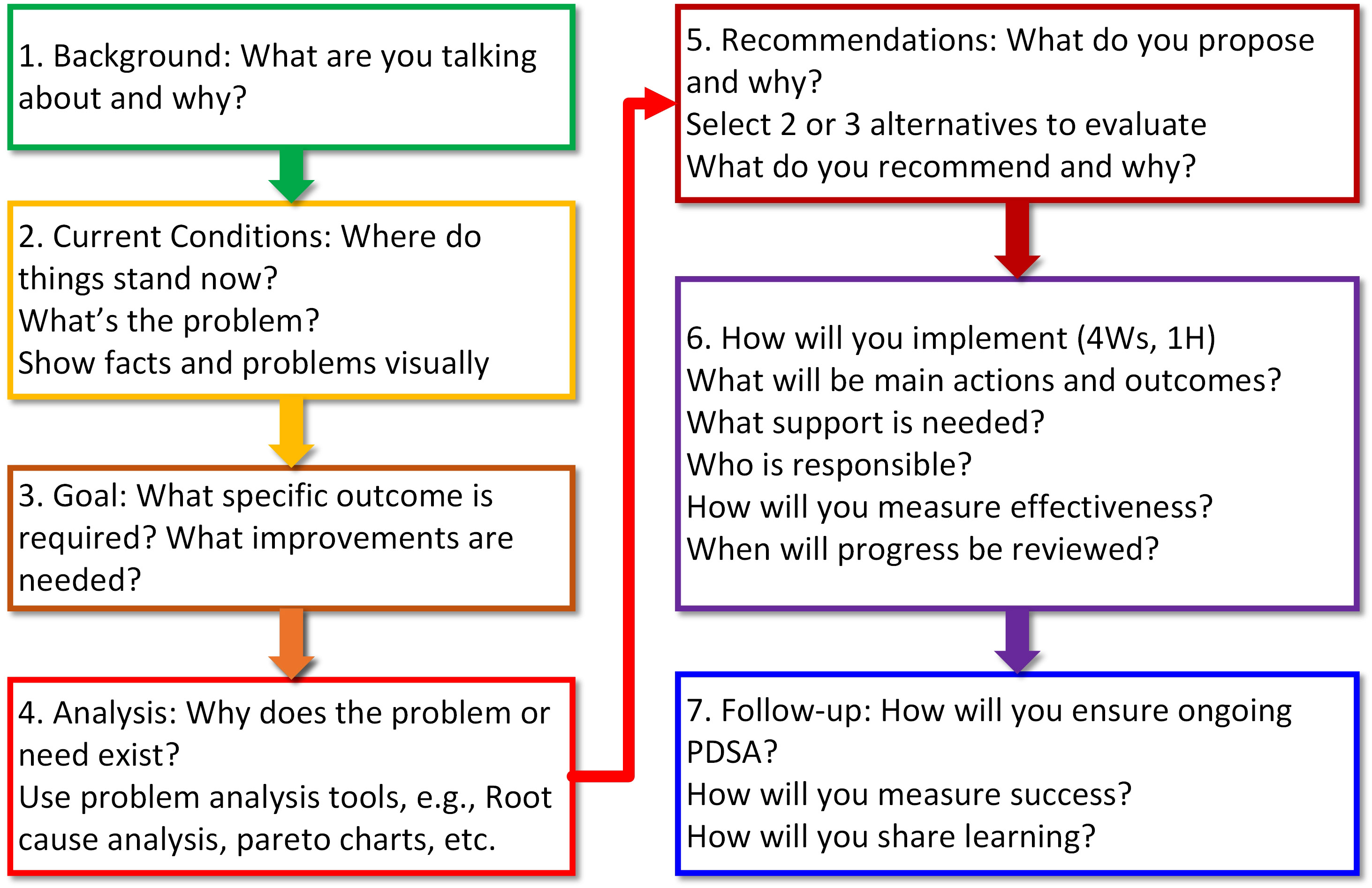
- A3 template: named after the 11 x 17 inch sheet of paper that can be used to lay out the various elements of process improvement (see Diagram 1)
- Kaizen: continuous process improvement
- Gemba: create value
- Poka yoke: mistake proof
- 5 S: sorting, set in order, shine, standardize, sustain
- DMADV: define, measure, analyze, design, verify
Quality improvement approaches
- 6 domains of healthcare quality according to the Institute of Medicine (Institute of Medicine: Crossing the Quality Chasm, 2001)
- Safe
- Effective
- Patient centered
- Timely
- Efficient
- Equitable
- Total Quality Management (TQM) (BMC Exchange: What is TQM? Total Quality Management Explained [Accessed 6 October 2020], ASQ: What is Total Quality Management (TQM)? [Accessed 6 October 2020])
- Management approach focused on improving quality and customer service
- Includes 8 key principles
- Customer focused
- Employee ownership
- Process based
- System integration
- Strategic and systematic approach
- Continuous improvement
- Data driven
- Communication
- Model for improvement: used by Institute for Healthcare Improvement (IHI) (Agency for Healthcare Research and Quality: Approaches to Quality Improvement [Accessed 11 September 2020])
- Combines TQM + rapid cycle improvement (RCI)
- Aim, measures, changes
- RCI: repetitive Plan, Do, Study, Act (PDSA) cycles (see Diagram 2)
- Combines TQM + rapid cycle improvement (RCI)
- Lean Six Sigma: increasingly used in clinical labaoratory
- Combines Lean + Six Sigma (ASQ: What is Six Sigma? [Accessed 11 September 2020])
- Lean: management philosophy on reducing waste
- 8 sources of waste (DOWNTIME)
- Defects
- Overproduction
- Waiting
- Neglected talents
- Transporting
- Inventory
- Motion
- Excess processing
- Lean in clinical laboratory: evaluate workflow and eliminate steps that don't add value
- Six Sigma: statistical control
- Problem solving method to eliminate defects due to process variation
- Sigma describes variability (defects per unit)
- Six Sigma: 99.99966% effective, with only 3.4 defects per million opportunities
- DMAIC: Define, Measure, Analyze, Improve, Control
- Six Sigma in clinical laboratory: focus on error reduction and eliminating variation
- EPIDEM: exploration, promotion, implementation, documentation, evaluation, modification (Lab Med 2019;50:e9)
- Goal = EPIDEMic of healthcare providers working to improve patient care
- 6 principles of quality improvement
- Easy way to remember the steps of quality improvement
- Compatible with other models and tools
EPIDEM principles
- Good intentions are not good enough
- Understand culture, context and resources
- Be self aware and mindful of your surroundings
- Set worthwhile goals
- Establish meaningful goals and measures
- Make sure your goals actually improve patient care in a meaningful way
- Understand processes and systems
- Evaluate systems and simplify processes
- Apply substitution test: would anybody else make a similar mistake?
- Go for the high yield
- Prioritize problem players and interventions
- 20% of the people / mistakes account for 80% of the problems (Pareto principle)
- It doesn't count unless you can measure it
- Measure at baseline and with any changes
- Collect data and document numbers
- Your job is never done
- Adopt a culture of continuous improvement
- Apply lessons learned to other situations
- Reference: Lab Med 2019;50:e9
EPIDEM steps
- Exploration
- Clarifying problem, scope of problem and potential solution
- Understanding local culture, context, resources
- Benchmarking against peers
- Promotion
- Developing a strategy to fix the problem
- Establishing shared goals and QI team
- Promoting to stakeholders and leaders at your institution
- Identifying events and opportunities to fix problem
- Implementation
- Mistake proof (poka yoke) processes
- Performing pilot studies
- Optimizing timing of intervention
- Documentation
- Document at baseline and throughout the process
- Save written correspondence, meeting minutes, important dates
- Document success, challenges and impact
- Evaluation
- Evaluate measures and quantify them
- Solicit feedback
- Modification
- Review for workarounds and outliers
- Seek to expand or improve intervention further
- Reference: Lab Med 2019;50:e9
Examples of EPIDEM
- Reducing BCR-ABL ordering errors (Am J Clin Pathol 2019;151:68)
- Exploration: ordering errors increased steadily from 2011 - 2015 in molecular pathology laboratory
- Promotion: confusion regarding naming of BCR-ABL tests was problematic; obtained buy-in from oncology and hemepath re: new workflow
- Implementation: validated and implemented a BCR-ABL qualitative assay that reflexes to quantitative major, went live in electronic medical record
- Documentation: documented errors before and after intervention
- Evaluation: intervention resulted in a sharp reduction in ordering errors, especially for BCR-ABL minor (acute lymphoblastic leukemia) patients
- Modification: continue to improve electronic medical record ordering to decrease incorrect orders
- Improving molecular testing workflow for surgical pathology specimens (Mod Pathol 2020;33:2025, Mod Pathol 2018;31:764)
- Exploration: surgical pathologist marked areas appeared suboptimal
- Promotion: promoted a research study and educated department residents / faculty on preanalytics of molecular testing (i.e. tumor cellularity)
- Implementation: prior to implementing new workflow, conducted a research study which helped garner buy-in
- Documentation: documented tumor cellularity assessments of surgical pathologists versus molecular pathologists
- Evaluation: compared accuracy of the tumor estimates; measured provider satisfaction and turnaround time
- Modifications: eliminated step of requiring surgical pathologists to review slides
- Improving pregnancy screening and use of urine pregnancy test (J Pediatr Adolesc Gynecol 2020 Jun 11 [Epub ahead of print])
- Exploration: no standardized pregnancy risk assessment in family planning teen clinic
- Promotion: worked with stakeholders to develop new protocol
- Implement: used feedback to train and develop changes
- Document: recorded feedback, documented changes to job aid
- Evaluate: percent uptake increased and urine pregnancy tests decreased
- Modifications: changed design of job aid, modified checklist and adjusted process throughout
Additional references
- Institute for Healthcare Improvement (IHI) has online courses free for individual students, residents and faculty as well as members of the least developed countries (by the United Nations) (Institute for Healthcare Improvement: IHI Open School Online Courses [Accessed 11 September 2020])
- We often default to the idea that individuals lack personal motivation to change but author and social scientist Joseph Grenny describes 6 sources of influence that need to be addressed to make change inevitable; the key sources are classified along the dimensions of motivation versus ability and personal versus social versus structural (Grenny: Influencer - The New Science of Leading Change, 2nd Edition, 2013)
Board review style question #1
You are in charge of the core laboratory and you notice some new clinicians are ordering expensive esoteric tests only available through reference laboratories. What is an appropriate next step using the EPIDEM approach?
- Ask your fellow to manually review every send out test above $1,000
- Gather data from the last 6 months of send out tests to clarify the issue
- Meet with the clinicians and educate them about these unnecessary orders
- Work with the information technology staff to eliminate the ability to order these tests through the electronic medical record
Board review style answer #1
B. Gather data from the last 6 months of send out tests to clarify the issue
Comment Here
Reference: Principles of laboratory quality improvement
Comment Here
Reference: Principles of laboratory quality improvement
Board review style question #2
The internal medicine department at your organization would like to use pediatric blood tubes to reduce patient blood loss. You are concerned that pediatric tubes may result in unintended consequences, such as delayed turnaround time due to special handling requirements. At which step in EPIDEM should this be addressed?
- Exploration
- Promotion
- Implementation
- Evaluation
Board review style answer #2