Table of Contents
Definition / general | Essential features | Terminology | ICD coding | History | Biosafety level (BSL) | Laboratory safety program | Safety data sheets (SDSs) | Universal precautions | Engineering changes | Biological spills management | Biohazard waste disposal | Training on biosafety practice | Biosafety in surgical pathology | Biosafety in autopsy | Clinical images | Videos | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Napit AR, Hassell LA. Biosafety for lab and pathology. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/managementlabbiosafety.html. Accessed November 27th, 2024.
Definition / general
- Biosafety refers to the protection of workers, the community and the environment from accidental exposure to infectious agents, toxins and other biological hazards
- To ensure protection, a set of policies, rules and procedures, known as biosafety guidelines, have to be followed by personnel working in lab facilities while handling and disposing of materials containing biological hazards (StatPearls: Biosafety Guidelines [Accessed 11 October 2023])
Essential features
- Biosafety includes implementation of training in practices to protect lab personnel, the community and the environment
- All lab workers should have or may be required to complete biosafety training annually and implement it in the practice
- Laboratory director must monitor compliance with biosafety
- Based on laboratory practices, safety equipment and facility construction, the U.S. Centers for Disease Control and Prevention (CDC) has executed 4 levels of biosafety
- Biosafety guidelines have a crucial role in surgical pathology labs and autopsy as well
Terminology
- Biohazard: biological substances that pose a threat to the health or environment; also called biological hazards and biohazardous agents
- Laboratory biosecurity: the protection, control and accountability for valuable biological material agents and toxins within laboratories, in order to prevent their loss, theft, misuse, diversion, unauthorized access or intentional unauthorized release (Front Bioeng Biotechnol 2020;8:650)
- Biosafety level (BSL): a series of safety precautions based on the potential for harm and spread, intended to minimize the risk of exposure of laboratory personnel and the surrounding environment to potentially infectious biohazardous agents (Methods Mol Biol 2019;1897:213)
- Occupational Safety and Health Administration (OSHA): a part of the United States Department of Labor, established to ensure safe and healthful working conditions for workers by setting and enforcing standards and providing training, outreach, education and compliance assistance
- Safety data sheets (formerly material safety data sheets [MSDSs]): documents that list information relating to occupational safety and health for the use of various substances and products
- Blood borne pathogen: microorganisms such as viruses or bacteria that are carried in blood and can cause disease in people (CDC: Bloodborne Diseases [Accessed 11 October 2023])
- Universal precautions: practice standards for treating all potentially infectious bodily fluids or tissues as infectious, including the use of impermeable items such as medical gloves, goggles and face shields every time one handles such materials
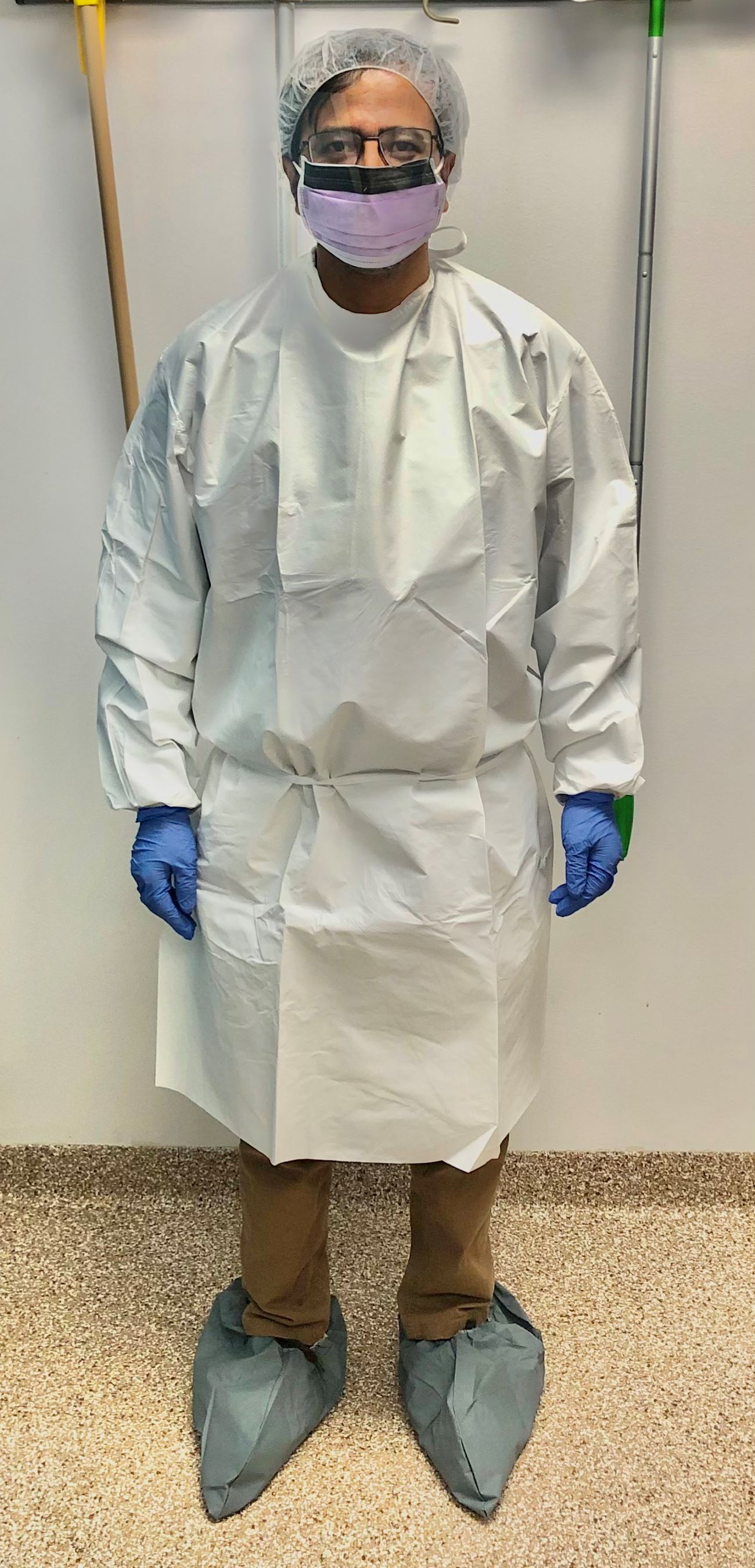
- Personal protective equipment (PPE): equipment worn to minimize exposure to hazards that cause serious workplace injuries and illnesses; includes items such as gloves, safety glasses and shoes, earplugs or muffs, respirators, vests and full body suits (OSHA: Personal Protective Equipment [Accessed 11 October 2023])
ICD coding
- ICD-10: Z91.89 - other specified personal risk factors, not elsewhere classified
History
- Concept of biosafety came into existence at the time of Pasteur and Koch (around 1890)
- In 1910, while studying the disease, Dr. Howard Taylor Ricketts acquired typhus and died; this was followed by many reports of laboratory acquired infection (Curr Protoc Microbiol 2009;13:111)
- Sulkin and Pike (1949 and 1951) and Collins (1990) contributed to the implementation of protective measures against biological agents
- Biosafety measures were first implemented in North America and the United Kingdom in 1970 and accelerated as awareness of risks associated with hepatitis and human immunodeficiency virus (HIV) increased
- Working practices, personnel protection measures and physical containment measures have been designed to restrict the transmission of biological agents (Belgian Biosafety Server: Biosafety Worldwide - Historical Background [Accessed 11 October 2023])
Biosafety level (BSL)
- 4 levels as implemented by CDC based on laboratory practices, safety equipment and facility construction
- Dictates the type of work practices that are allowed to occur in a lab setting and plays a major role in the design of the facility
- BSL 1
- Laboratory settings that involve working with low risk microbes that pose little to no threat of infection in humans (e.g., nonpathogenic strain of E. coli)
- Follow basic safety procedures
- No special equipment or design features are required
- BSL 2
- Laboratories that work with agents associated with pathogenic human diseases and hence pose a moderate health hazard (e.g., HIV, S. aureus)
- Safety measures include using gloves and eyewear, handwashing sinks, waste decontamination facilities and self closing and locking doors
- BSL 3
- Laboratories that work with microbes that are either indigenous or exotic and can cause serious or potentially lethal diseases, which may be spread via inhalation (e.g., West Nile virus, tuberculosis)
- Personnel wear respirators and perform lab manipulations in a gas tight enclosure; other safety features include clothing decontamination, sealed windows and specialized ventilation systems
- BSL 4
- Laboratories that work with highly dangerous and exotic microbes that are often lethal and come without treatment or vaccines (e.g., Ebola, Marburg viruses)
- Lab personnel must wear full body, air supplied suits and shower when exiting the facility; along with BSL 3 features, the lab must be located in a separate building or an isolated and restricted zone of the building (StatPearls: Biohazard Levels [Accessed 11 October 2023])
Laboratory safety program
- Aims to protect lab personnel, clients and the environment by following biosafety guidelines
- Environment health and safety (EHS) division of the institution develops a comprehensive framework that all labs must follow (National Research Council: Prudent Practices in the Laboratory - Handling and Management of Chemical Hazards, Updated Version, 2011)
- Laboratory safety program includes
- Responsibility: chief executive officer, along with all immediate associates, should have a continuing, explicit commitment to the safety program
- Safety plan: clearly defined safety rules that are available in written form and have means of monitoring compliance; should be coordinated with institutional and local community emergency services
- Safety meetings and safety committees: everyone involved in the laboratory should participate
- Safety communications: to alert people to newly recognized hazards, remind them of basic safety principles and instill good attitudes toward safety; safety newsletters containing practical safety advice, safety posters and reference books on laboratory hazards, occupational health and good laboratory practices
- Monitoring safety: observations of individual safety practices, operability of safety equipment and compliance with safety rules should be part of a regular audit (National Research Council: Biosafety In The Laboratory - Prudent Practices for the Handling and Disposal of Infectious Materials, 1989)
Safety data sheets (SDSs)
- Safety data sheets (formerly material safety data sheets [MSDSs]): a system for cataloging information about a particular chemical product, instructions for its safe use and associated potential hazards (Int J Pharm Compd 2017;21:118)
- OSHA's Health Communication Standard, revised in 2012, requires that the chemical manufacturer, distributor or importer provide safety data sheets (SDSs) for each hazardous chemical to communicate information on these hazards to users
- There are 16 sections in SDSs
- Section 1: identification
- Section 2: hazard(s) identification
- Section 3: composition / information on ingredients
- Section 4: first aid measures
- Section 5: firefighting measures
- Section 6: accidental release measures
- Section 7: handling and storage
- Section 8: exposure controls / personal protection
- Section 9: physical and chemical properties
- Section 10: stability and reactivity
- Section 11: toxicological Information
- Section 12: ecological information (not mandatory)
- Section 13: disposal considerations (not mandatory)
- Section 14: transport information (not mandatory)
- Section 15: regulatory information (not mandatory)
- Section 16: other information (OSHA: Hazard Communication Standard - Safety Data Sheets [Accessed 11 October 2023])
Universal precautions
- Standard set of guidelines to prevent the transmission of blood borne pathogens (such as hepatitis A, hepatitis B, HIV and brucellosis) from exposure to blood and other potentially infectious materials (OPIM)
- Implemented by the CDC in 1985, primarily in response to the HIV epidemic
- OPIM
- Semen, vaginal secretions, cerebrospinal fluid, synovial fluid, pleural fluid, pericardial fluid, peritoneal fluid, amniotic fluid, saliva in dental procedures and body fluid that is visibly contaminated with blood
- Any unfixed tissue or organ from human (living or dead)
- Cell, tissue or organ cultures containing HIV
- HIV or hepatitis B virus (HBV) containing culture medium or other solutions
- Blood, organs or other tissues from experimental animals infected with HIV or HBV
- Universal precautions practice includes
- Hand hygiene by hand rubbing with alcohol or hand washing with soap and water
- Use of PPE such as gowns, gloves, masks and goggles
- No mouth pipetting
- No food, drink or lip balm in the lab
- Proper disposal of biohazardous / medical waste
- Use of engineering controls (StatPearls: Universal Precautions [Accessed 11 October 2023])
- Universal precautions must be effectively implemented during autopsies due to documented instances of infection transmission, including but not limited to tuberculosis, AIDS, HBV and SARS-CoV-2, occurring during the procedure (Am J Pathol 2020;190:2180)
Engineering changes
- Set up a hands free sink that includes either an automated faucet with motion detection capabilities or controls operated by your knee or foot
- Automatic door locking system so the door remains closed in the lab
- Having negative airflow into the laboratory or a work cabinet can prevent exposure to splashes and sprays or spread to the external environment
- Using a biosafety cabinet (BSC) to handle fresh tissue (CDC: Guidelines for Safe Work Practices in Human and Animal Medical Diagnostic Laboratories [Accessed 11 October 2023])
Biological spills management
- Spill response is a crucial emergency management process that needs to have its own standard operating procedure (SOP)
- Regular training is needed to ensure lab personnel are well trained in spill management
- Conventional method involves 2 trained staff, one working in the contaminated area and the second providing support from the noncontaminated area
- Steps
- Take appropriate measures to reduce exposure for other lab workers or patients
- Isolate the spill area and vacate it for 30 minutes
- Prepare disinfectant and spill cleanup equipment
- Cover the area with a paper towel and then pour disinfectant
- Collect the paper towel and mop the area with disinfectant (Appl Biosaf 2019;24:141)
- Procedures may vary with larger volume spills
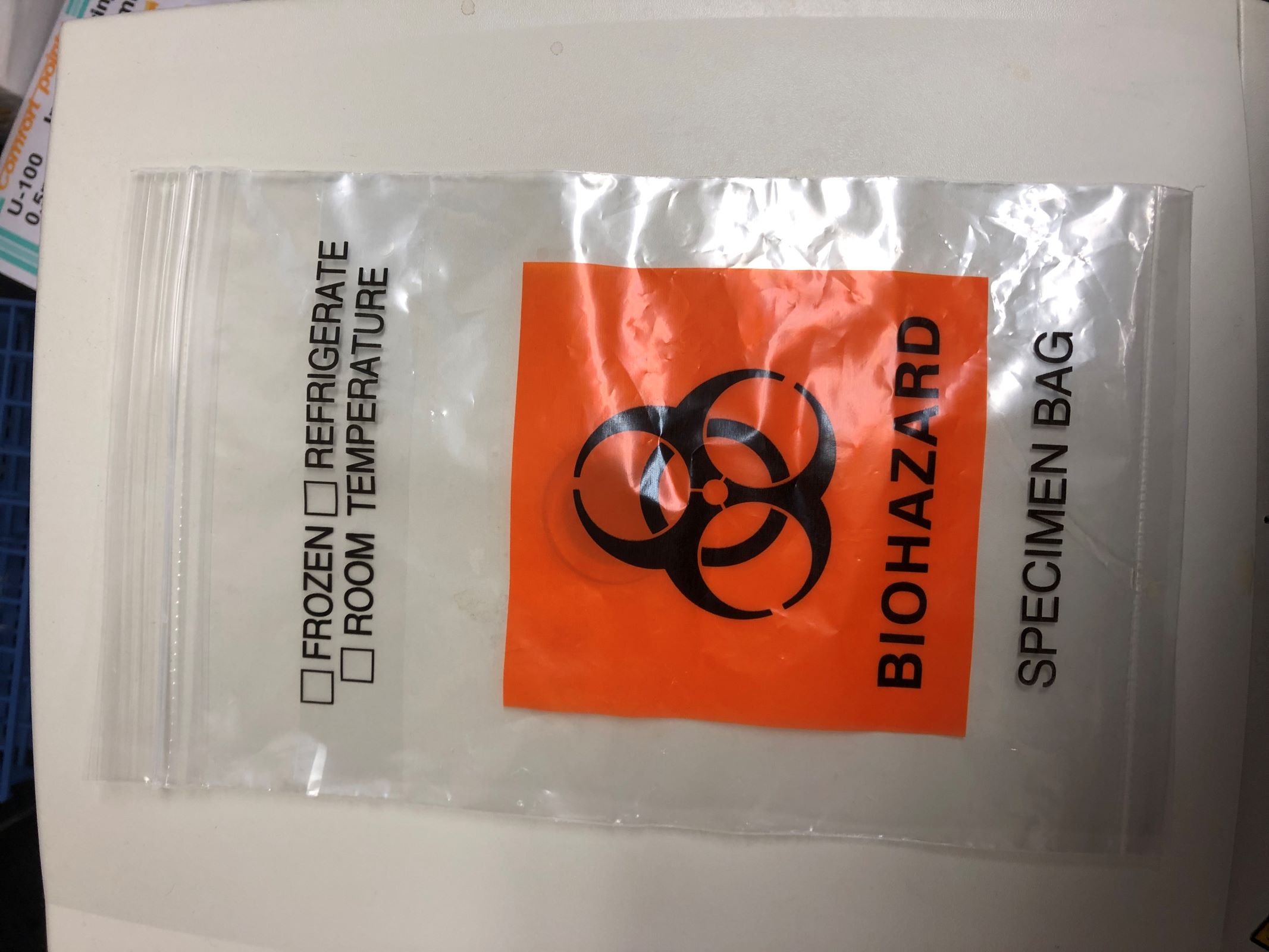
Biohazard waste disposal
- Identify and define all categories of waste generated
- Waste needs to be decontaminated before disposal
- Most clinical laboratories can operate satellite accumulation points and accumulate, store, transport and dispose of waste in accordance with Environmental Protection Agency (EPA) and the Department of Transportation (DOT) regulations (Clin Lab Manage Rev 1990;4:160)
Training on biosafety practice
- Laboratory director must ensure that a laboratory specific biosafety manual is developed, adopted, annually reviewed and is accessible to all laboratory personnel
- Manual or comparable training should be reviewed annually and whenever procedures or policies change
- All lab personnel should take biosafety practice training annually; training must cover the following topics
- Institutional and laboratory safety policies
- Management, supervisor and personnel responsibilities
- Regulations and recommended guidelines
- Routes of exposure in the laboratory
- Risk assessment and reporting of exposures
- Biosafety principles and practices
- Standard precautions for safe handling of infectious materials
- Standard operating procedures
- Hazard communication and biohazard signs
- Engineering controls
- Administrative and work practice controls
- Personal protective equipment (PPE)
- When and how to work in a BSC (biosafety cabinet)
- Transport of biohazardous materials
- Emergency procedures
- Decontamination and disposal of biohazardous waste
- Training program and documentation
- Medical surveillance and exposure evaluation procedures (CDC: Guidelines for Safe Work Practices in Human and Animal Medical Diagnostic Laboratories [Accessed 11 October 2023])
Biosafety in surgical pathology
- Surgical pathology laboratories receive specimens with the same potential exposures as those of other labs
- Needle stick, cut and formalin exposure by splash or prolonged skin exposure are common hazards; hence, the training must include education on needle stick injuries, PPE and the hazards of chemical exposures
- Incident reporting and subsequent follow up training have been reported to be more effective than didactic training alone
- Pathology departments should consider additional biosafety components when initiating and training new residents
- Discomfort caused by certain PPE, such as masks pressing on the skin, face shields obstructing dictation microphones and uncomfortable ventilators and respirators, leads to people not using them correctly or at all; hence, these items should be customized as per the pathologist's requirement (Hum Pathol 2013;44:951)
- Use of freeze spray in the frozen section should be discouraged (MMWR Suppl 2012;61:1)
- Exposure to aerosols generated during frozen sections should be minimized, especially in potentially infectious cases
- Cryostat decontamination procedures should be sufficient for viral, mycobacterial and other pathogens
Biosafety in autopsy
- Autopsy can lead to exposure to infectious agents, toxic chemicals (e.g., formalin, cyanide and organophosphates) and radiation from radionuclides used for patient therapy and diagnosis
- Autopsy generated droplets (> 5 mm in diameter) also potentially transmit infections if inhaled or ingested
- Implantable cardioverter defibrillator can sustain an electrical discharge of 25 - 40 J if manipulated; hence, it needs to be deactivated and manufacturers must have service representatives available to assist with deactivation (Am J Forensic Med Pathol 2002;23:107)
- Autopsy biosafety program must be provided to autopsy staff and visiting personnel with an environment free from hazardous exposure risk (Finkbeiner: Autopsy Pathology, 2nd Edition, 2009)
Clinical images
Videos
Lab safety: biosafety
Biohazard spill management
Biosafety levels
Additional references
Board review style question #1
Board review style answer #1
A. Blood borne pathogens. Splashes from blood borne pathogens is the risk best prevented with such a splash guard. Answer E is incorrect because while plexiglass may halt certain radiation particles, it is generally not effective against most forms of radiation. Answers C and D are incorrect because in the absence of airflow controls, such a shield would not prevent exposure to lyophilized toxins or aerosols. Answer B is incorrect because while chemical toxins could splash, the greater risk with them is spills, which risk would be enhanced in working behind a shield.
Comment Here
Reference: Biosafety for lab and pathology
Comment Here
Reference: Biosafety for lab and pathology
Board review style question #2
A laboratory handling clinical cultures that include evaluation and culture of aerobic, anerobic and mycobacterial samples should follow precautions designated as which of the following levels?
- Biosafety level 1
- Biosafety level 2
- Biosafety level 3
- Biosafety level 4
Board review style answer #2
C. Biosafety level (BSL) 3. While most routine clinical lab samples for routine human pathogens can be safely handled using precautions designated at BSL 2, the addition of mycobacteria such as tuberculosis that are spread through inhalation require more stringent standards and hence are BSL 3. Answer A is incorrect because these samples are potentially infectious to humans. Answer B is incorrect because mycobacteria require more stringent standards than BSL 2. Answer D is incorrect because Biosafety level 4 is for samples that are generally highly dangerous and do not have effective treatments. The samples described here do not meet this definition.
Comment Here
Reference: Biosafety for lab and pathology
Comment Here
Reference: Biosafety for lab and pathology