Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Peripheral smear description | Positive stains | Negative stains | Flow cytometry description | Flow cytometry images | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1Cite this page: Alves de Castro JV, Jaffe ES. Systemic chronic active EBV disease. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lymphomasystemicchronicactiveEBV.html. Accessed April 1st, 2025.
Definition / general
- Systemic chronic active Epstein-Barr virus (CAEBV) disease is a systemic Epstein-Barr virus (EBV) related T / NK cell lymphoproliferative disorder that occurs mostly in children and adolescents
- Manifests as persistent clinical symptoms and high EBV viremia for more than 3 months with a protracted but potentially progressive clinical course
Essential features
- Rare chronic EBV related T / NK cell lymphoproliferative disorder that mainly affects pediatric patients of Asian or Hispanic descent
- Systemic symptoms for at least 3 months, high EBV viremia and absence of immunodeficiency are all essential criteria for the diagnosis
- Demonstration of EBV positive T or NK cells in affected tissues is also required for the diagnosis but affected tissues usually have preserved architectural features
- Cases previously described as B cell type CAEBV have now been excluded from this category, given that they arise mostly in Western countries, affect older adults and usually arise in a background of known immunodeficiency
Terminology
- Chronic active EBV infection
- Severe chronic active EBV infection
- Chronic active EBV disease of T / NK cell phenotype
- Chronic active EBV infection of T / NK cell type, systemic form
- Epstein-Barr virus associated T / NK cell lymphoproliferative disease
ICD coding
- ICD-O: 9725/1 - systemic chronic active EBV positive disease (Int J Hematol 2023;118:568)
- ICD-11: 2B0Y & XH6TZ4 - other specified primary cutaneous mature T cell or NK cell lymphomas and lymphoproliferative disorders & systemic EBV positive T cell lymphoproliferative disease of childhood
Epidemiology
- All cases are associated with EBV by definition
- Worldwide prevalence is unknown but it is rare and most patients are from East Asia (Japan, Taiwan, Korea) and Central / South America (Ann Oncol 2009;20:1472)
- Affects predominantly children and adolescents with a mean age of 8 - 11 years old but has been reported in adults (Blood 2001;98:280, J Infect Dis 2003;187:527, Blood 2012;119:673, Int J Hematol 2011;93:602)
- No gender predilection (Blood 2001;98:280, J Infect Dis 2003;187:527, Blood 2012;119:673)
Sites
- Liver
- Spleen
- Bone marrow and peripheral blood
- Lymph nodes
- Lung
- Eye
- Central nervous system
- References: Blood 2011;117:5835, Ann Oncol 2009;20:1472, Blood 2012;119:673
Pathophysiology
- EBV infects mostly B lymphocytes and epithelial cells during primary infection; it can also infect T and NK cells but this process is less well understood
- CD21 is a receptor used by EBV to infect host cells and it may be expressed in common lymphoid progenitors and precursor T cells (J Immunol 1991;146:865)
- Infection of T lymphocytes and common lymphoid progenitors by EBV has been documented (Blood 1995;85:744, Adv Exp Med Biol 2018;1045:459)
- Cell of origin studies and the presence of divergent phenotypes in CAEBV support the notion that EBV may infect a common lymphoid progenitor in this disease (Nat Microbiol 2019;4:404)
- Cell to cell infection during an attempt to kill infected cells and acquisition of CD21 by NK cells through synaptic transfer have also been suggested as mechanisms of viral acquisition (J Immunol 2003;170:5993)
- It is speculated that the evasion of host immunity by EBV infected T / NK cells is associated with specific human leukocyte antigens (HLA) and genetic background of some patients (Adv Exp Med Biol 2018;1045:459)
- Some HLA alleles might not properly present EBV epitopes and thus impair viral clearance
- Traits related to lymphomagenesis might also be codominantly expressed along with HLA-A26, one of the putative HLA alleles related to EBV T / NK lymphoproliferative disorder (LPD)
- Evasion of host immune response is also facilitated by the latency type II program, which does not express the immunodominant antigens EBNA2 and EBNA3 (Adv Exp Med Biol 2018;1045:459)
- Development and progression of clinically evident disease might be associated with the acquisition of driver gene mutations or epigenetic modifications
- DDX3X and KMT2D mutations have been suggested to be present in the cell of origin models at diagnosis (Nat Microbiol 2019;4:404)
- DDX3X encodes an RNA helicase and loss of function variants alter RNA processing and unwinding
- KMT2D encodes a lysine methyltransferase that participates in chromatin remodeling targeting active chromatin sites involved in transcription and DNA repair (Nat Rev Cancer 2021;21:413)
- DDX3X and KMT2D mutations have been suggested to be present in the cell of origin models at diagnosis (Nat Microbiol 2019;4:404)
- Intragenic deletions in the EBV genome target mostly the BART microRNA clusters 1 and 2 (Nat Microbiol 2019;4:404)
- The most affected microRNAs negatively regulate BZLF1, BRLF1 and BRLF14, which are proteins that function as transcriptional activators of immediate early genes associated with the lytic cycle
- In the lytic cycle, there is a marked reduction of expression of MHC class 1 and class 2 as well as CD74, which may protect the infected cells from EBV specific cytotoxic T lymphocytes
- BZLF1 can also interfere with the activity of CD4 positive T lymphocytes (PLoS Pathog 2011;7:e1002455)
- Transcriptomic studies also imply inflammatory response and cell proliferation genes in the pathogenesis of CAEBV (Pathology 2020;52:111)
- Elevated levels of proinflammatory cytokines may explain the relationship with hemophagocytic lymphohistiocytosis (HLH) (Blood 2018;131:2899)
Etiology
- Precise cause is unknown but an impaired control of EBV due to genetic polymorphisms is suspected
- Association between HLA-A*26 and HLA-B*52 has been reported (Adv Exp Med Biol 2018;1045:459)
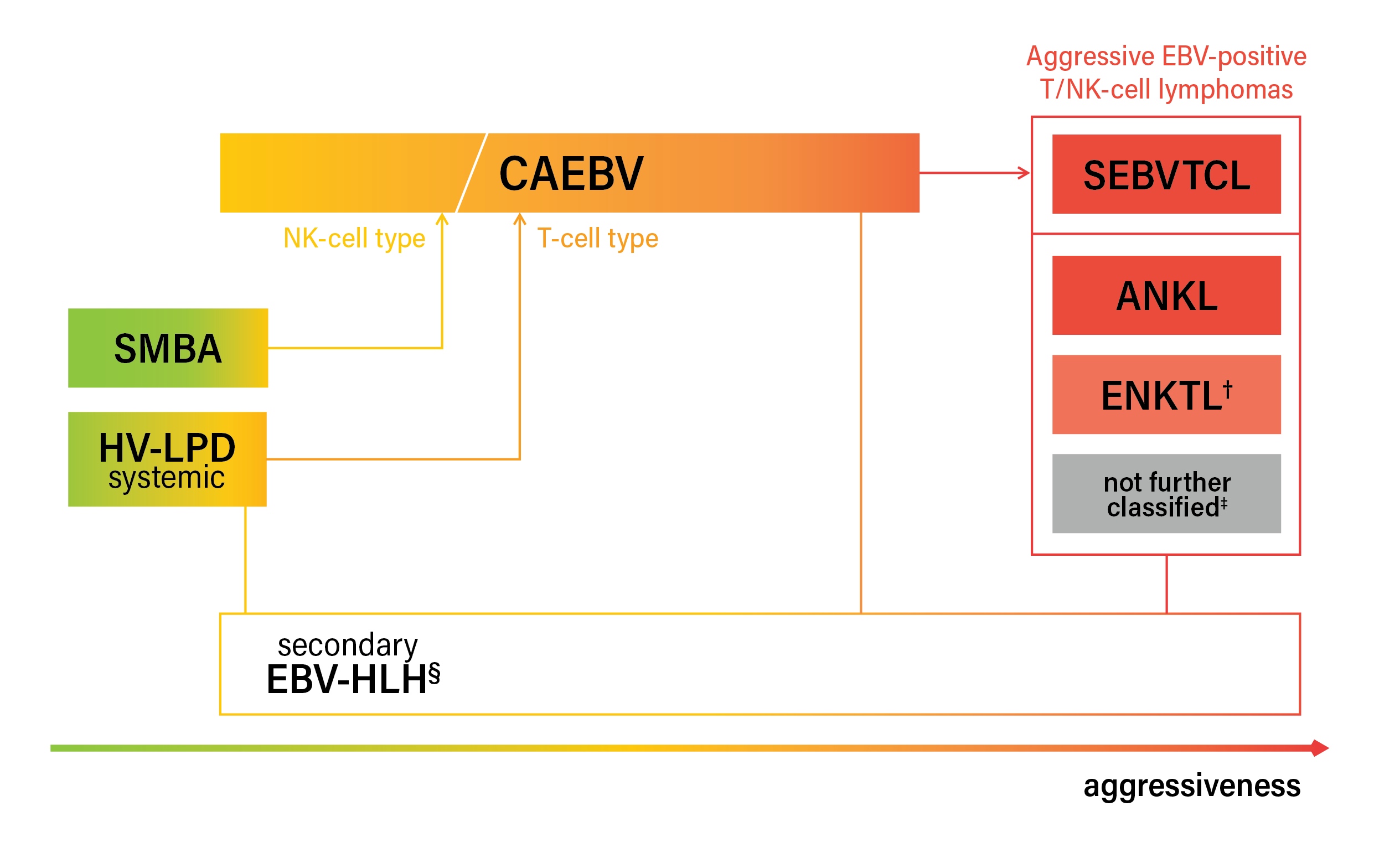
Diagrams / tables
Clinical features
- At presentation (Blood 2018;131:2899)
- Fever
- Liver dysfunction
- Hepatosplenomegaly
- Lymphadenopathy
- Complications (Blood 2018;131:2899)
- Hemophagocytic lymphohistiocytosis
- Coronary artery aneurysms
- Liver failure
- Overt T cell lymphomas, including systemic EBV positive T cell lymphoma of childhood
- Other possible features
- Uveitis, interstitial pneumonia, hydroa vacciniforme-like eruptions (HV LPD) and hypersensitivity to mosquito bites (severe mosquito bite allergy)
- Periorbital face and edema of the face in South American patients reported as hydroa vacciniforme is more consistent with CAEBV (Am J Dermatopathol 2015;37:20)
Diagnosis
- Infectious mononucleosis-like symptoms lasting for at least 3 months (essential)
- High levels of EBV DNA in blood (essential)
- Infiltration of tissues by EBV positive T / NK cells demonstrated by histology (essential)
- B cell type is excluded by both the 5th edition of the World Health Organization Classification of Haematolymphoid Tumours (WHO-HAEM5) and the International Consensus Classification (ICC) 2022 (Virchows Arch 2023;482:227)
- Exclusion of primary or acquired immunodeficiencies, history of transplant, previous malignancies and rheumatic diseases (essential)
- References: Int J Hematol 2023;118:568, Leuk Lymphoma 2020;61:808, Virchows Arch 2023;482:227, Leukemia 2022;36:1720
Laboratory
- Elevation of liver enzymes
- Hypoalbuminemia
- Elevated bilirubin levels
- Cytopenias
- EBV DNA blood levels as measured by polymerase reaction in whole blood or peripheral blood mononuclear cells (preferred over plasma)
- High EBV related IgG titers (viral capsid antigen [VCA] IgG and early antigen [EA] IgG) are often seen but not necessary for the diagnosis (Int J Hematol 2023;118:568)
Radiology description
- For cases with coronary artery involvement, contrast enhanced computed tomography (CT) angiography may show coronary artery dilation (Virol J 2020;17:166)
Prognostic factors
- Overall prognosis is variable but is usually protracted (J Infect Dis 2003;187:527)
- Allogeneic hematopoietic stem cell transplant improves prognosis (Blood Adv 2020;4:2918, Blood 2018;131:2899)
- Unfavorable prognostic factors (J Infect Dis 2003;187:527, Blood Adv 2020;4:2918)
- Age at onset of 8 years old or more
- T cell type over NK cell type: 5 year overall survival of 59% versus 87%
- Thrombocytopenia
- Presence of somatic mutations (Nat Microbiol 2019;4:404)
- Progression to overt T / NK cell lymphoma, including systemic EBV positive T cell lymphoma of childhood
- Importantly, these are not prognostic (Leuk Lymphoma 2020;61:808)
- Degree of atypia
- Clonality status
- Number of EBV positive cells
Case reports
- 9 year old girl with polymyositis and coronary artery dilation (Virol J 2020;17:166)
- 20 year old man with persistent fever, lymphadenopathy and splenomegaly (Am J Transl Res 2021;13:12006)
- 23 year old woman with fever and recurring subcutaneous nodules (Front Med (Lausanne) 2022;9:759834)
- 47 year old man with fever and fatigue (Blood 2020;136:2090)
Treatment
- Standard treatment approach has not been established (Blood 2018;131:2899)
- Treatment of hemophagocytic lymphohistiocytosis, mainly with the HLH-2004 protocol, is the most important once hemophagocytic lymphohistiocytosis is identified (Blood 2018;131:2899)
- Diverse chemotherapy regimens are usually necessary, including high dose systemic corticosteroids or ganciclovir combined with either histone deacetylase inhibitors or bortezomib (Blood 2018;131:2899)
- Hematopoietic stem cell transplant (HSTC) is the only curative approach (Blood 2018;131:2899)
- Early diagnosis and transplant before disease progression might be critical for improving outcomes for these patients (Blood 2018;131:2899)
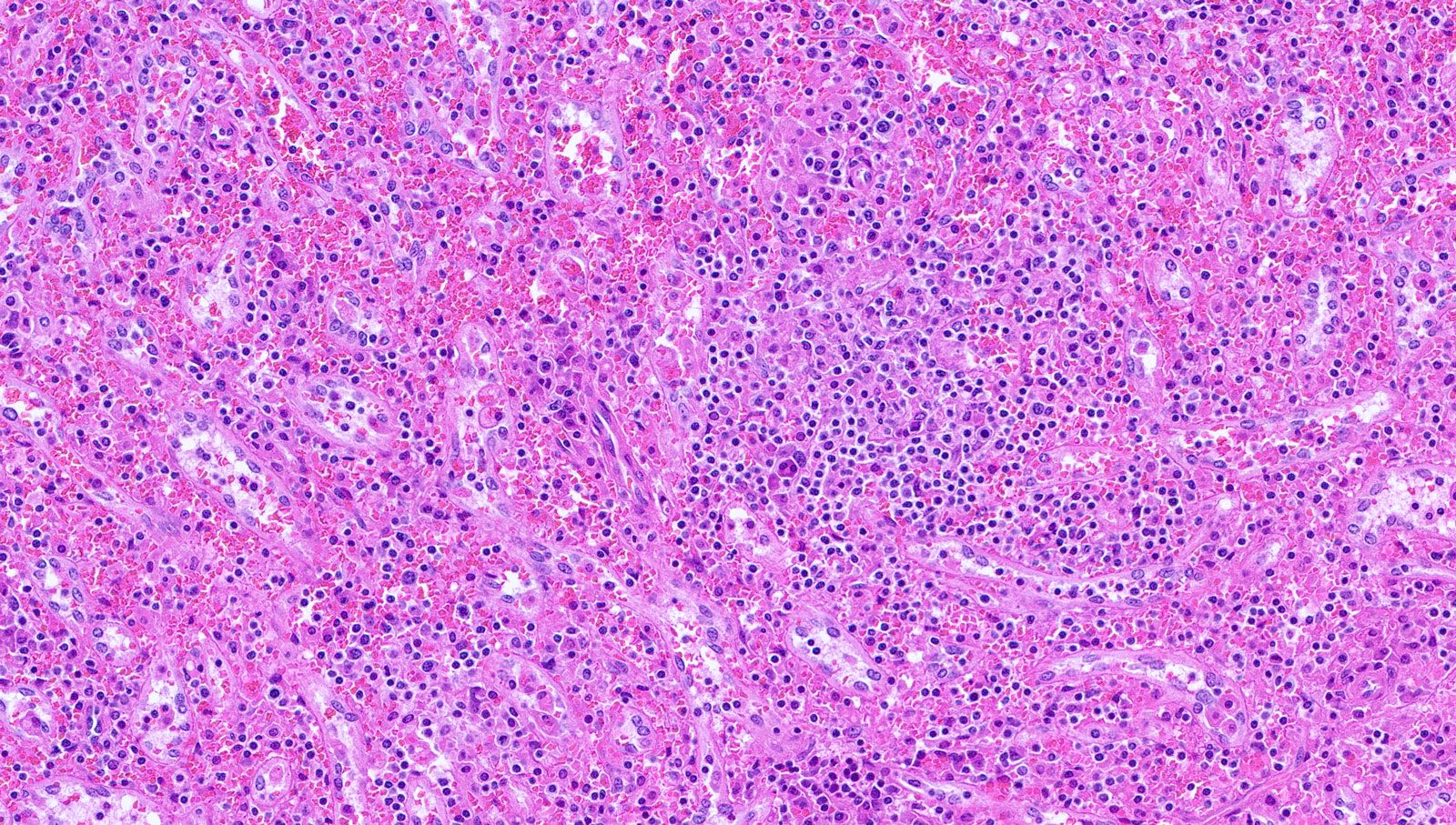
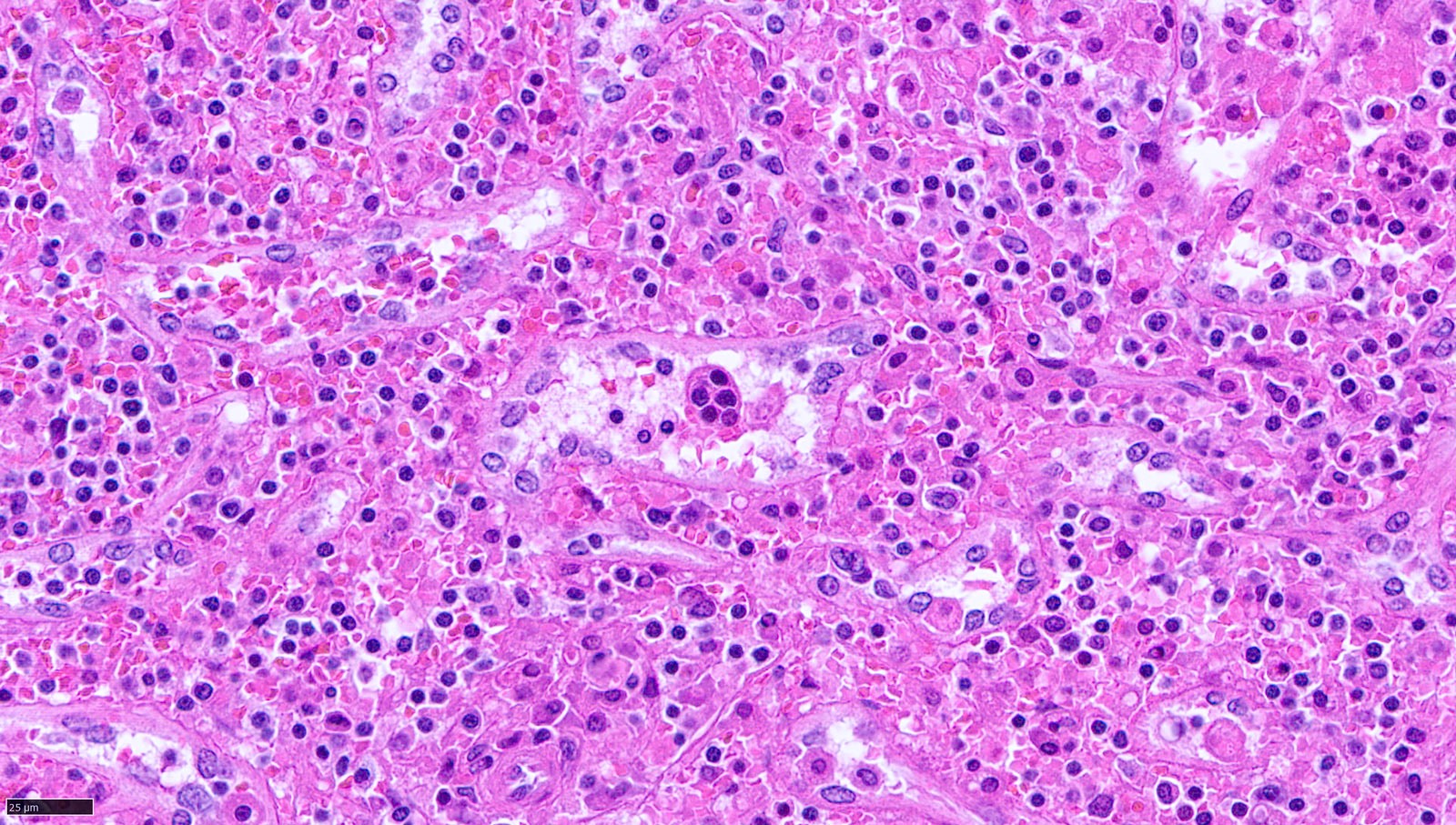
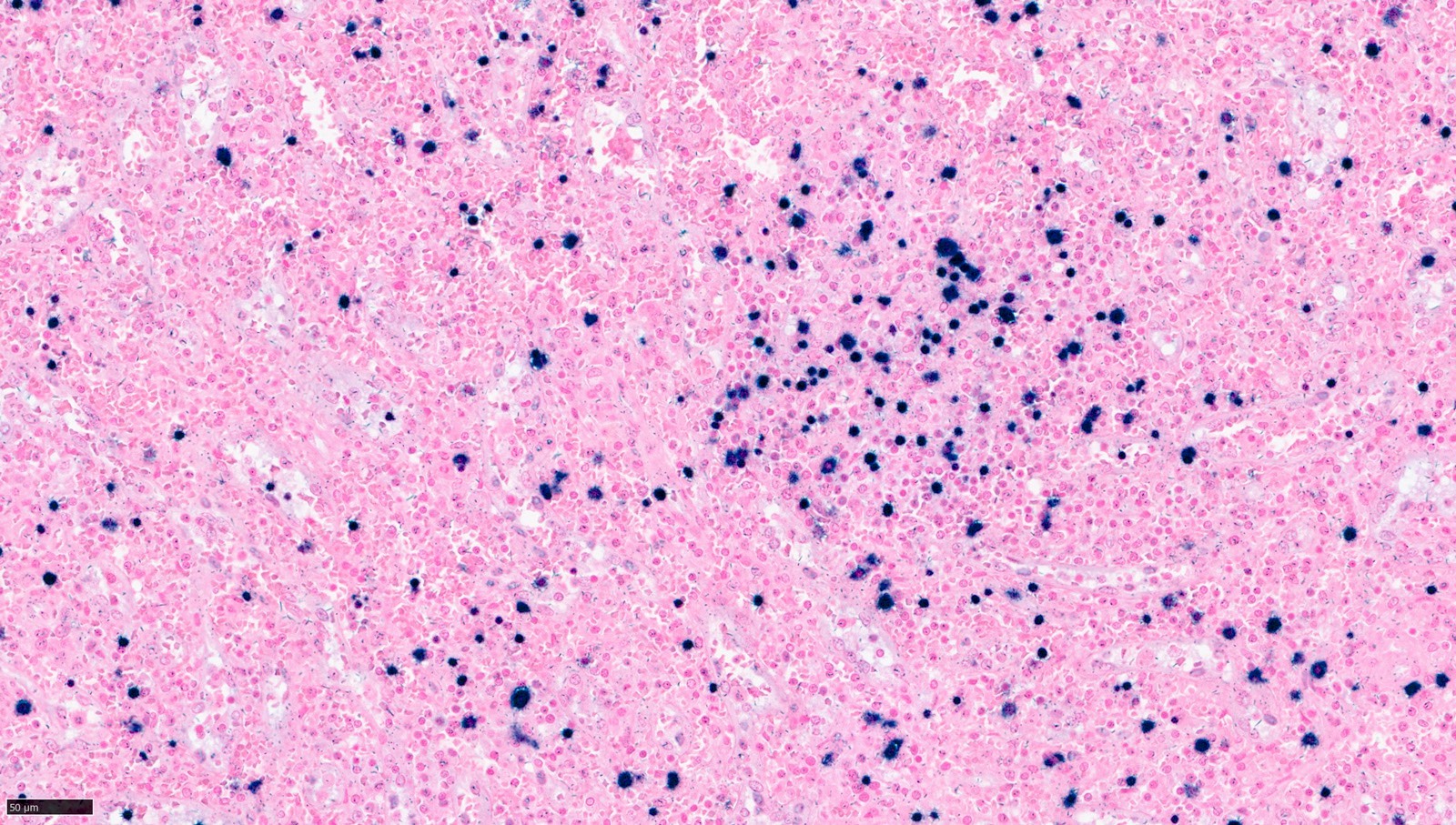
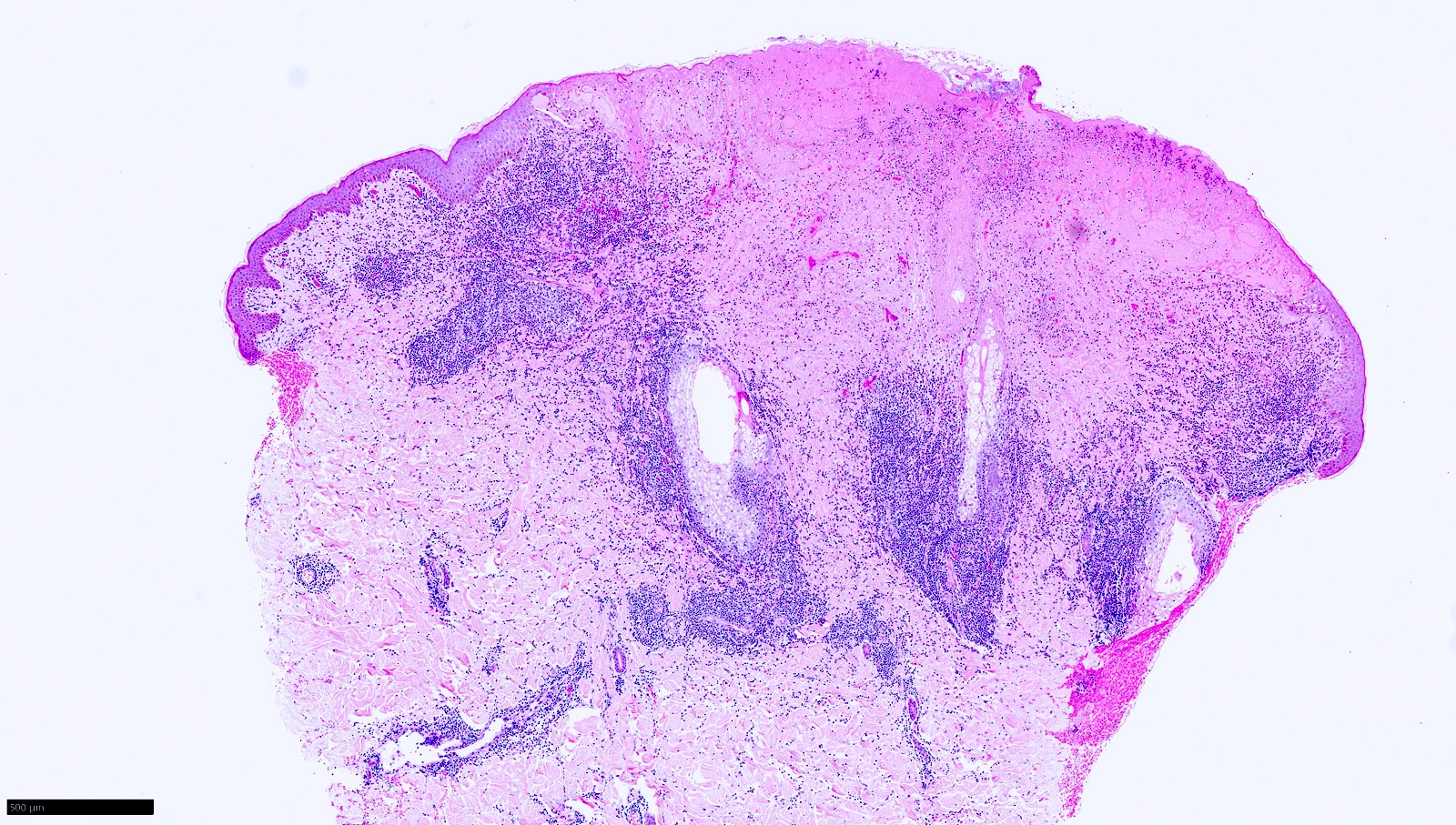
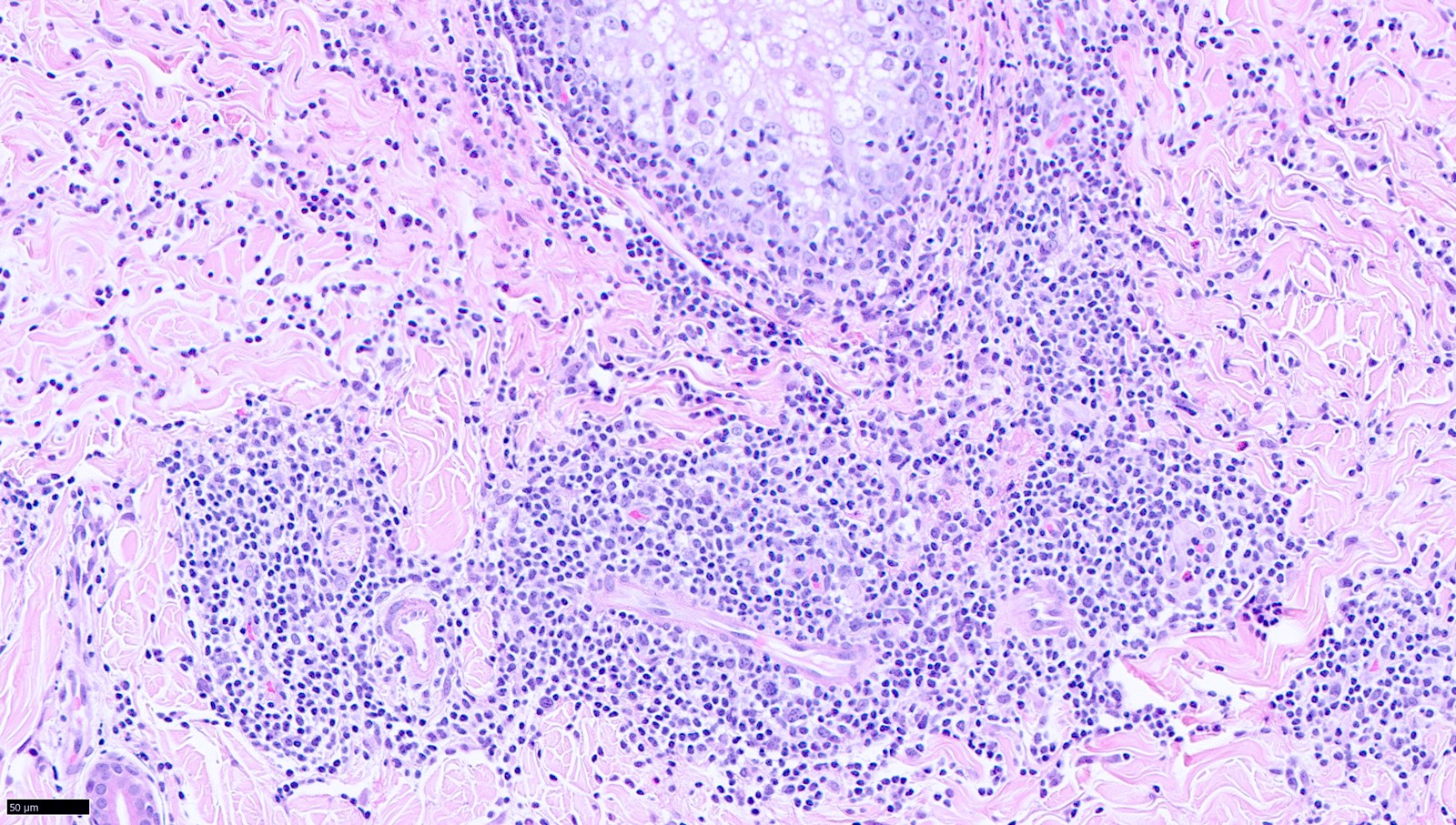
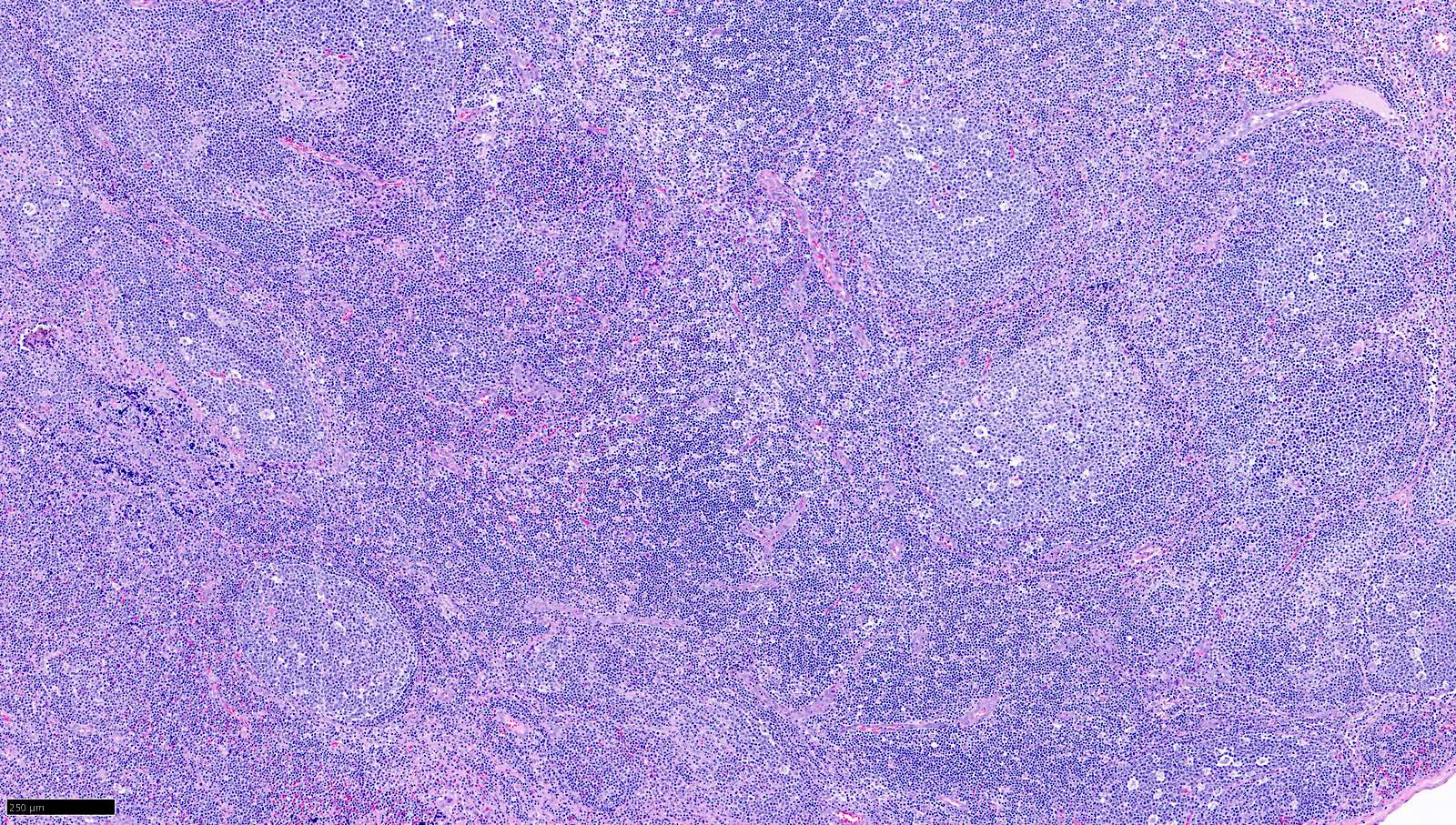
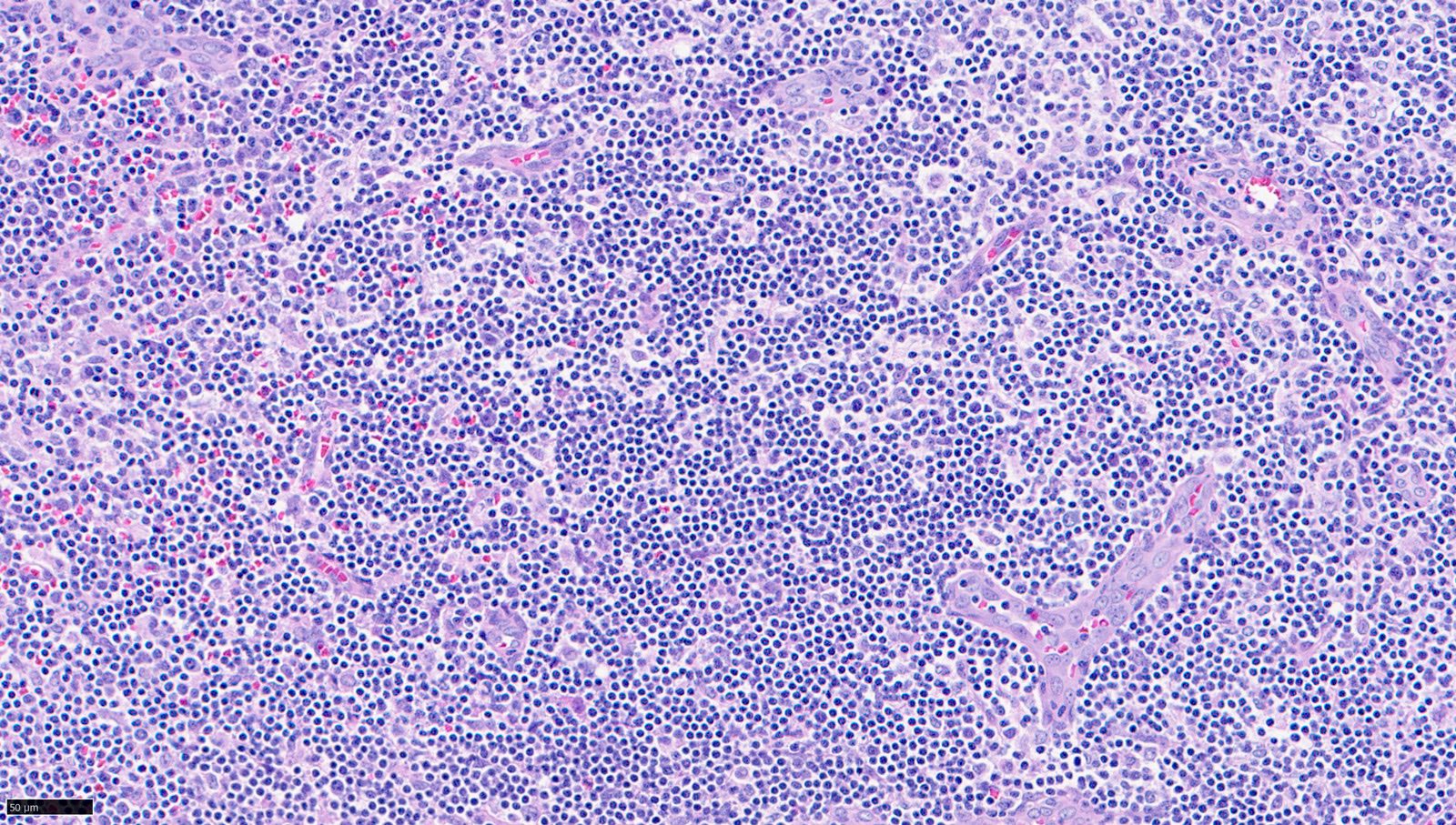
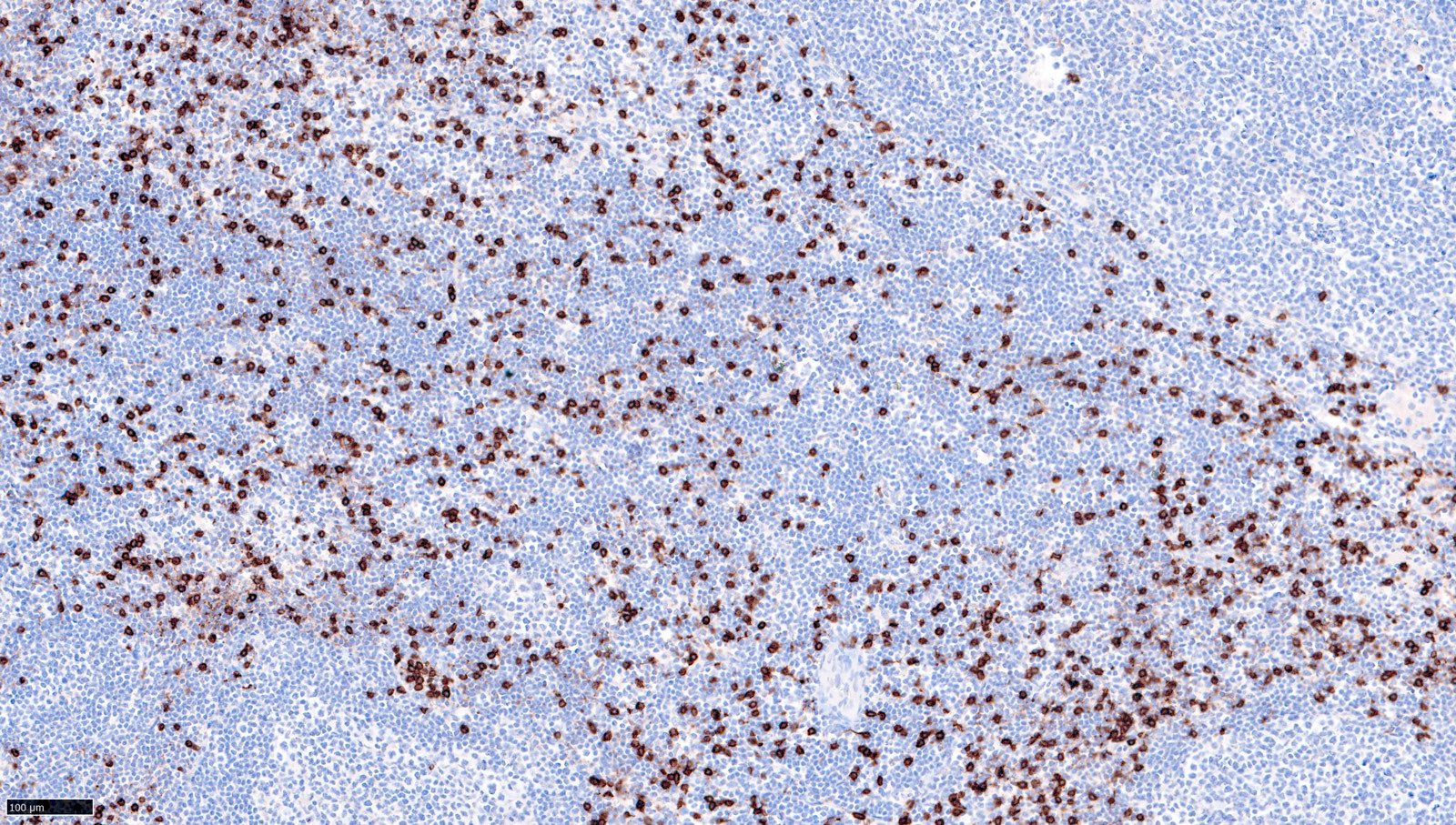
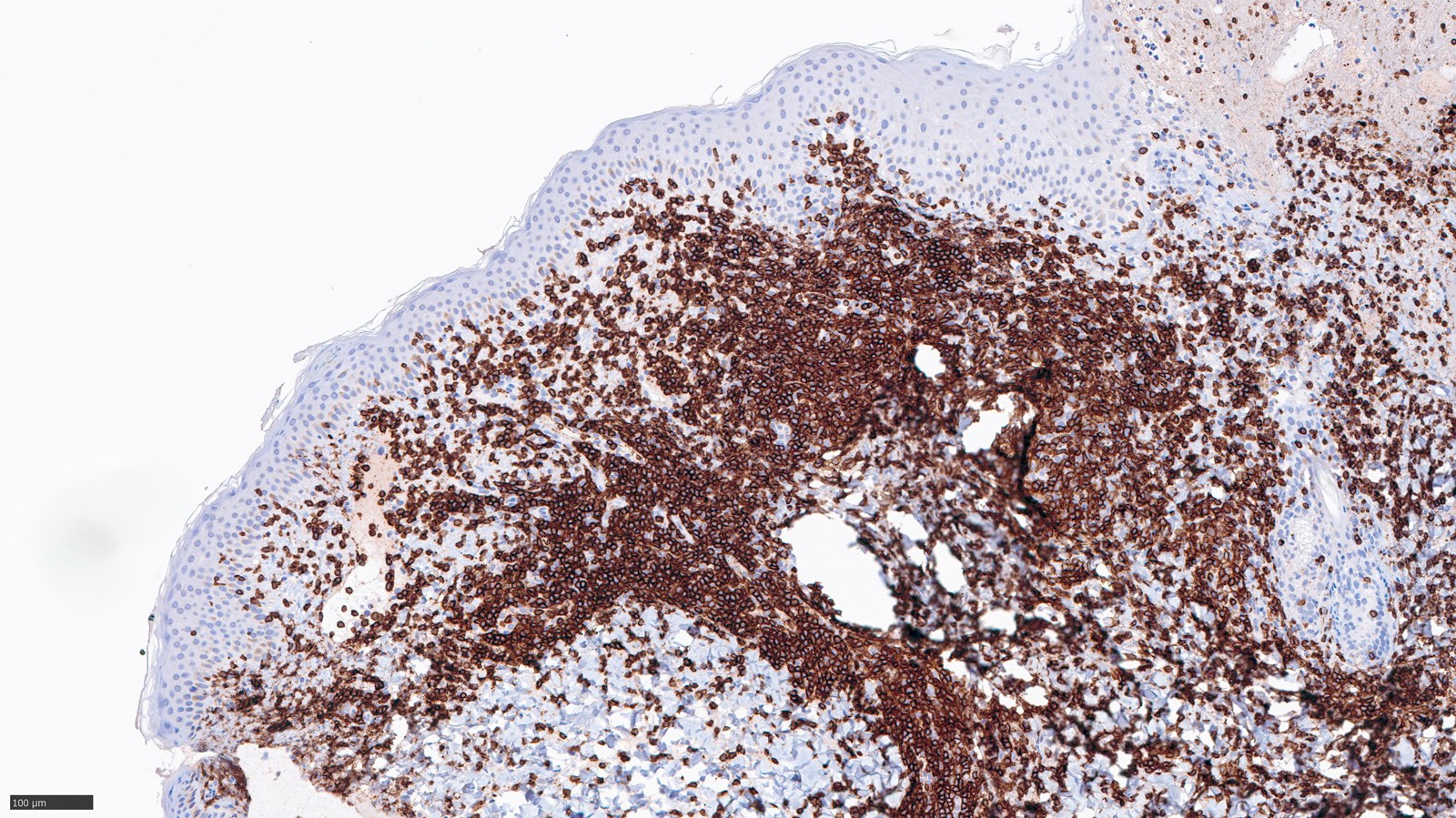
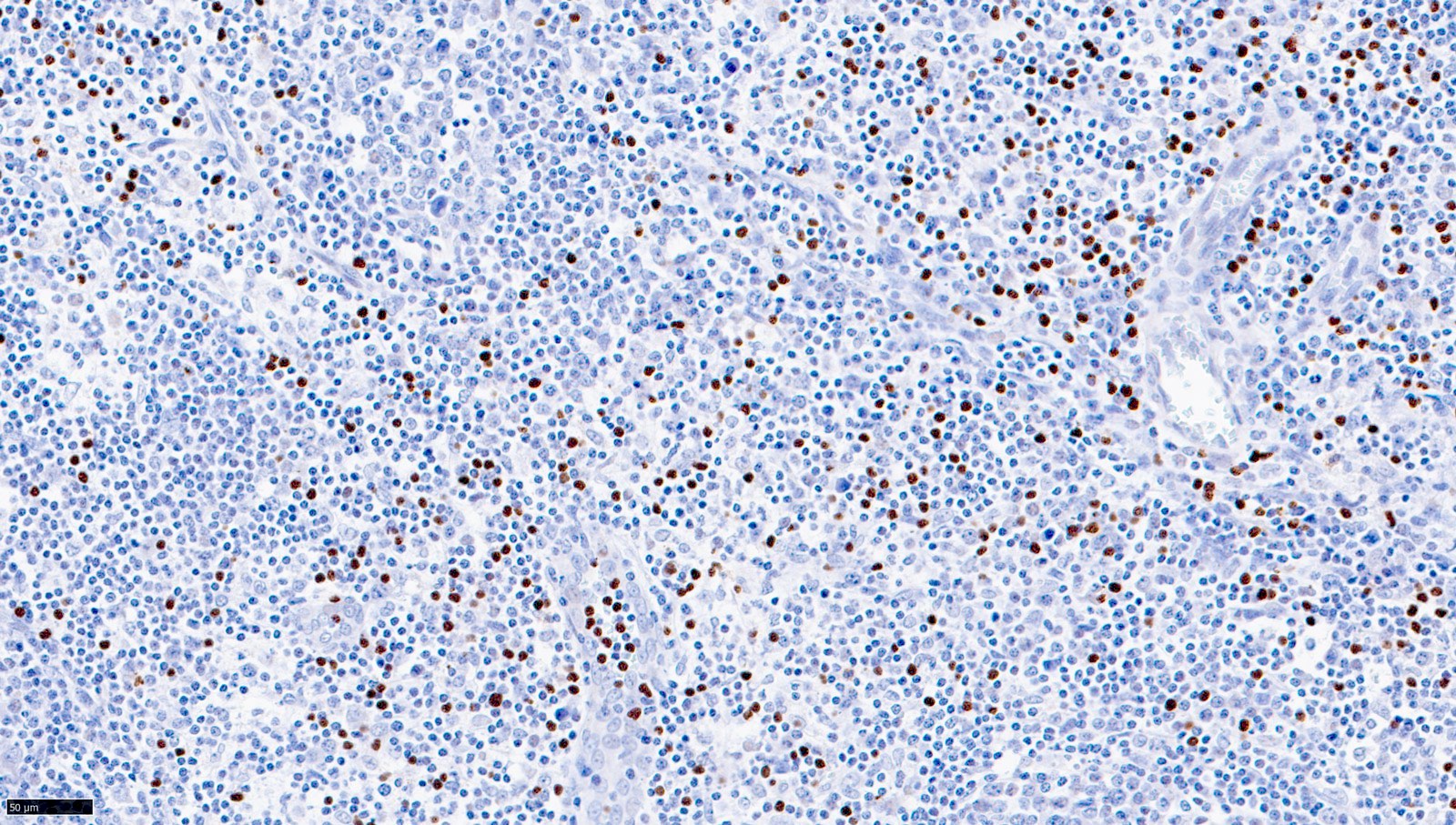
Microscopic (histologic) description
- Affected tissues frequently do not display morphologic features of malignancy (Am J Clin Pathol 2023;159:14)
- Hemophagocytosis can be present in the liver, spleen and bone marrow of cases associated with hemophagocytic lymphohistiocytosis
- Liver
- Predominantly intrasinusoidal lymphocytosis
- Hepatocytes may display features of viral hepatitis
- Spleen
- Mild expansion of the red pulp by lymphocytes arranged singly or in clusters
- White pulp is often preserved
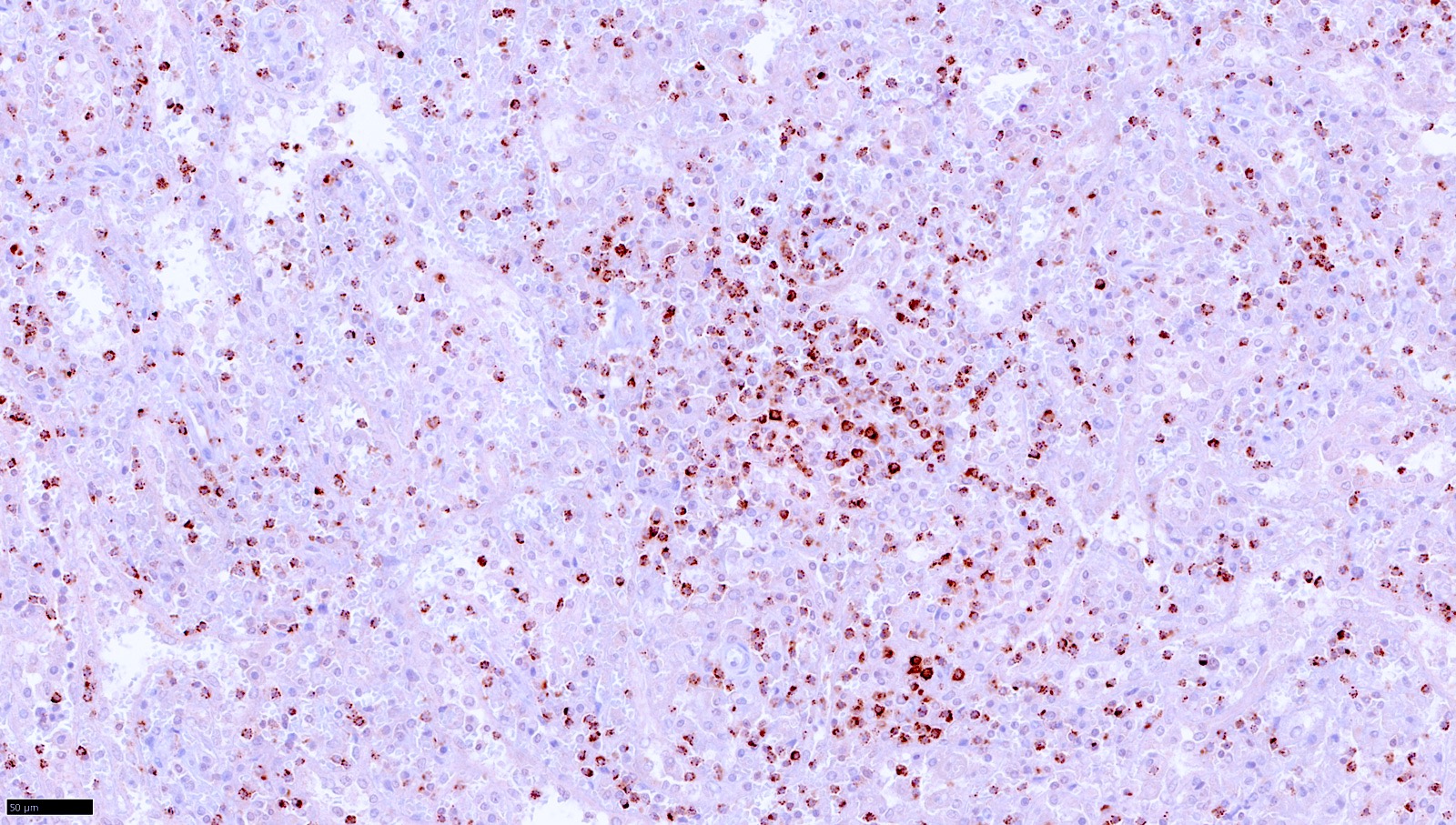
- Lymph node
- Interfollicular / paracortical infiltrate of mildly atypical EBV positive cells
- Architecture is mostly preserved, with follicular and paracortical hyperplasia, open sinuses and a thin capsule
- Bone marrow
- Usually normal
- Discrete interstitial and sinusoidal lymphocytosis may be seen with immunohistochemistry
- Skin (in cases associated with hydroa vacciniforme lesions)
- Dense periadnexal and perivascular dermal and subcutaneous infiltrate of small to medium lymphoid cells
- Epidermal necrosis, ulceration and bullae formation
- Other affected tissues (lung and heart): interstitial pneumonitis and viral myocarditis
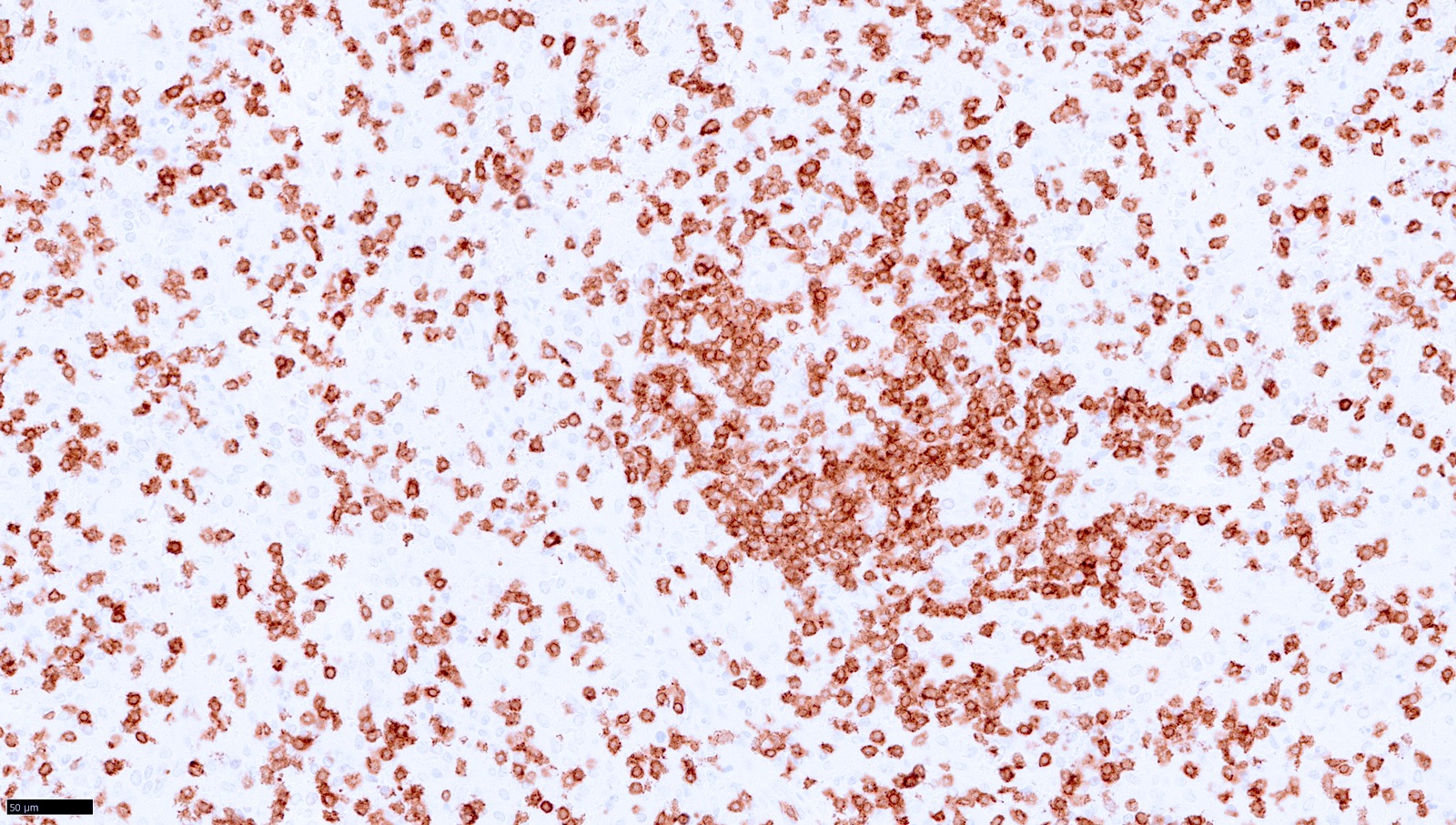
Microscopic (histologic) images
Contributed by Elaine Jaffe, M.D. and João Víctor Alves de Castro, M.D.
Peripheral smear description
- Lymphocytosis with medium sized lymphoid cells showing purple cytoplasmic granules has been reported (Am J Transl Res 2021;13:12006)
Positive stains
Negative stains
- CD20
- EBNA2
- sCD3 (for NK type cases)
- Reference: Blood 2012;119:673
Flow cytometry description
- Cases with T cell phenotype: description not found
- Cases with NK cell phenotype (Am J Transl Res 2021;13:12006)
Flow cytometry images
Molecular / cytogenetics description
- Chromogenic in situ hybridization for EBV encoded RNA (EBER ISH) must be positive
- Demonstration of EBER positivity in T cells by double staining with EBER / CD3 is advisable
- T cell receptor clonality studies by fragment analysis are mostly monoclonal but can be oligoclonal or polyclonal (Ann Oncol 2009;20:1472)
- Abnormal karyotype with 6q deletion has been reported (Int J Cancer 1997;71:943)
- Next generation sequencing (NGS) studies are limited and mostly nondiscriminatory between CAEBV and other EBV positive T / NK cell lymphoproliferative disorders (Nat Microbiol 2019;4:404)
- Somatic mutations are present in 28.75% of 80 cases
- DDX3X is the most frequently mutated gene (87.5%, 14/16 patients)
- Recurrent mutations also involved chromatin modifiers and epigenetic regulators (KMT2D, BCOR, BCORL1, TET2, KDM6A)
- In contrast to extranodal NK / T cell lymphoma (ENKTL), TP53 mutations have not been identified so far (Cancers (Basel) 2021;13:1414)
Sample pathology report
- Spleen, splenectomy:
- EBV positive T cell lymphoproliferative disorder, consistent with chronic active EBV disease of T cell type (see comment)
- Comment: Histologic sections show a preserved splenic architecture. There are mildly atypical lymphoid cells predominantly in the red pulp, while the white pulp is unremarkable. Performed immunohistochemistry stains show that most of the lymphoid infiltrate in the red pulp is composed of T cells positive for CD3, with a slight decrease in CD5 expression. Most of the T cells are positive for CD8, TIA, granzyme B and perforin. Some T cells in the red pulp are also CD4 positive. In situ hybridization for EBV (EBER) is positive in numerous cells in the red pulp, with a distribution similar to the CD8 positive T cells. CD56 is negative. There is evidence of hemophagocytosis on H&E stained sections as well as by CD68 and CD163 immunohistochemistry. TCR clonality by fragment analysis showed a polyclonal pattern. In summary, the overall findings are consistent with chronic active EBV (CAEBV) disease of T cell type.
Differential diagnosis
- Systemic EBV positive T cell lymphoma of childhood (SEBVTCL):
- Hydroa vacciniforme lymphoproliferative disorder (HV LPD), systemic form:
- There is significant clinicopathological overlap between HV LPD, systemic form and CAEBV
- Aggressive NK cell leukemia:
- Usually affects older adults
- Atypia can be more pronounced
- Invariably aggressive
- Infectious mononucleosis:
- EBER positive cells will be B cells
- There is a more pronounced architectural effacement, with a polymorphous paracortical infiltrate
- Always polyclonal for IG and TCR gene rearrangements
- Rare cases can have a more aggressive clinical course but there will be evidence of recent infection by EBV serologic studies
- (Primary) nodal EBV positive T / NK cell lymphoma:
- Affects mostly elderly patients with known immunosuppression
- Primarily a nodal disease
- Usually shows a monomorphic infiltrate of EBV positive cytotoxic T cells effacing the nodal architecture
Additional references
Board review style question #1
A 13 year old Hispanic boy presented with fever, generalized lymphadenopathy, hepatosplenomegaly and cutaneous papules for 4 months. He was previously healthy. After a thorough clinical and laboratory workup, it was shown that he has an elevation of liver enzymes up to 5 times the upper limit of normal range and an EBV viral load of 400,000 copies/mL. Screening for primary and secondary immunodeficiencies is negative. The above image shows the morphological findings of an axillary lymph node excisional biopsy. Which statement about this clinicopathological entity is correct?
- EBV positive cells by in situ hybridization (EBER) should also be positive for CD20 in this lymphoproliferative disorder
- High EBV viral load in this setting confirms the diagnosis of infectious mononucleosis
- Most of the affected patients are elderly and a presentation in childhood is highly unusual
- Preservation of the lymph node architecture, with paracortical and follicular hyperplasia, is not specific but is compatible with the diagnosis of (systemic) chronic active EBV disease (CAEBV)
Board review style answer #1
D. Preservation of the lymph node architecture, with paracortical and follicular hyperplasia, is not specific but is compatible with the diagnosis of (systemic) chronic active EBV disease (CAEBV). The affected tissues in CAEBV usually do not show prominent or specific morphological features and lymph nodes often have a pattern of mixed follicular and paracortical hyperplasia. Answer C is incorrect because CAEBV typically occurs in children and adolescents. Answer B is incorrect because a high EBV viral load is essential for the diagnosis of CAEBV and cannot be used to exclude infectious mononucleosis alone. Answer A is incorrect because the EBV positive cells must be of T or NK cell lineage; B cell type is excluded by current diagnostic criteria.
Comment Here
Reference: Systemic chronic active EBV disease
Comment Here
Reference: Systemic chronic active EBV disease