Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Negative stains | Flow cytometry description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Gibbons K, Perry AM. Pediatric nodal marginal zone lymphoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lymphomapediatricnodalMZL.html. Accessed April 2nd, 2025.
Definition / general
- Rare pediatric non-Hodgkin lymphoma, with characteristic morphologic and clinical features and a typically excellent prognosis
Essential features
- Rare pediatric nodal lymphoma, more common in males
- Typically localized to head and neck lymph nodes with excellent prognosis
- Histologically, expanded marginal zones and interfollicular areas with expanded follicles
- Polymorphous proliferation of monocytoid, centrocyte-like and plasmacytoid cells
ICD coding
- ICD-O: 9699/3 - marginal zone B cell lymphoma, NOS
Epidemiology
- < 2% of childhood non-Hodgkin lymphomas (Pediatr Blood Cancer 2020;67:e28416)
- Most common in adolescents, with a median age of 16 (Virchows Arch 2016;468:141)
- Markedly more common in males, M:F = 20:1
- Rarely seen in adults (Virchows Arch 2016;468:141)
Sites
- Majority of patients have localized (stage I) head and neck lymphadenopathy
- Inguinal / femoral lymph nodes involved in up to 20% of cases (Adv Anat Pathol 2017;24:128)
Pathophysiology
- Arises from postgerminal center memory B cell (Virchows Arch 2016;468:141)
Etiology
- Unknown
Clinical features
- Rare cases of advanced and disseminated disease, stage III / IV, have been reported (Pediatr Blood Cancer 2020;67:e28416)
Diagnosis
- Lymph node biopsy (Pediatr Blood Cancer 2020;67:e28416)
Laboratory
- Normal serum lactate dehydrogenase (LDH) levels (Pediatr Blood Cancer 2020;67:e28416)
Prognostic factors
- Prognosis is excellent, with 5 year overall survival approaching 100% (Pediatr Blood Cancer 2020;67:e28416)
- Very low relapse rate following conservative treatment (Adv Anat Pathol 2017;24:128)
Case reports
- 13 year old boy with inguinal and cervical lymphadenopathy (Pediatr Int 2017;59:358)
- 15 year old girl with generalized lymphadenopathy, splenomegaly and persistent disease (Pediatr Dev Pathol 2015;18:167)
- 18 and 44 year old men with localized cervical lymphadenopathy (Leuk Lymphoma 2010;51:89)
Treatment
- Conservative management; clinical observation after surgical excision in localized disease (Virchows Arch 2016;468:141)
- Systemic therapy reserved for patients with advanced disease, relapse or progression (Pediatr Blood Cancer 2020;67:e28416)
Microscopic (histologic) description
- Partial to complete effacement with sinusoidal obliteration (Adv Anat Pathol 2017;24:128)
- Markedly expanded marginal zones with interfollicular infiltration of lymphoma cells
- Diffuse areas often present (Virchows Arch 2016;468:141)
- Often large follicles with extension of mantle zone into germinal centers, resembling progressive transformation of germinal centers; follicular colonization is sometimes seen (Pediatr Blood Cancer 2020;67:e28416)
- Lymphoid infiltrate is polymorphous including monocytoid cells (small to medium sized, round nuclei, moderate cytoplasm), centrocyte-like cells (irregular nuclei, scant cytoplasm) and plasma cells (Adv Anat Pathol 2017;24:128)
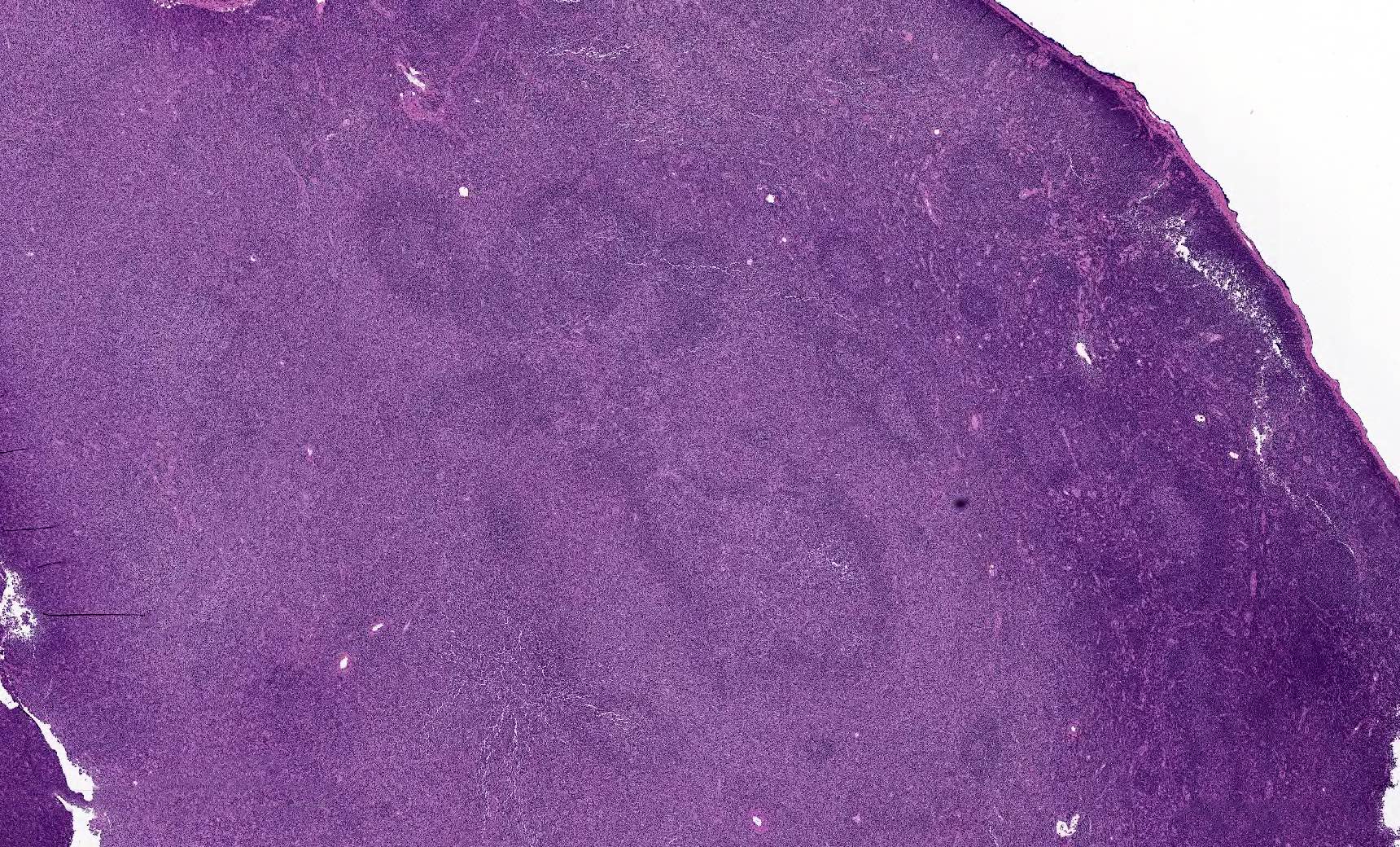
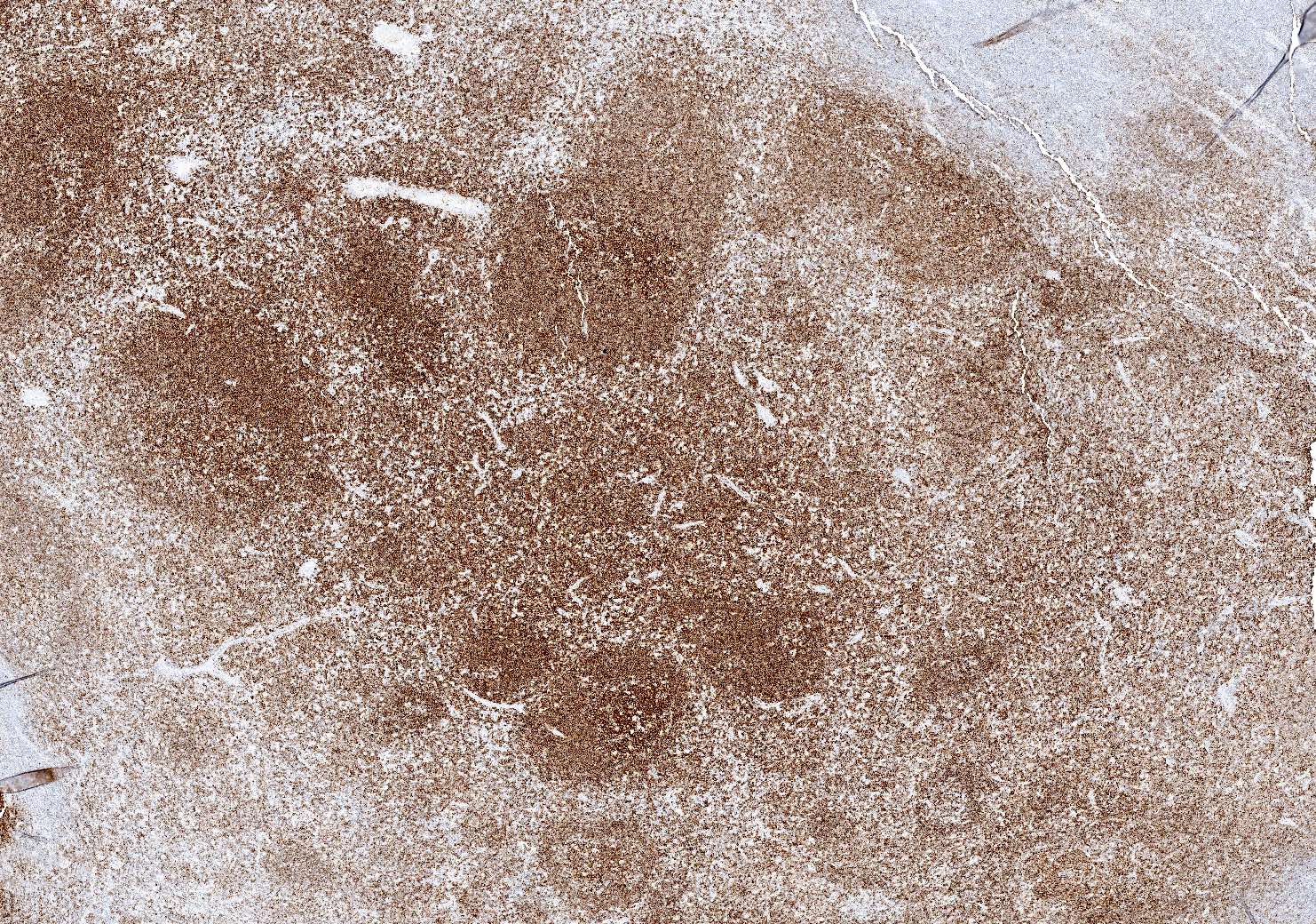
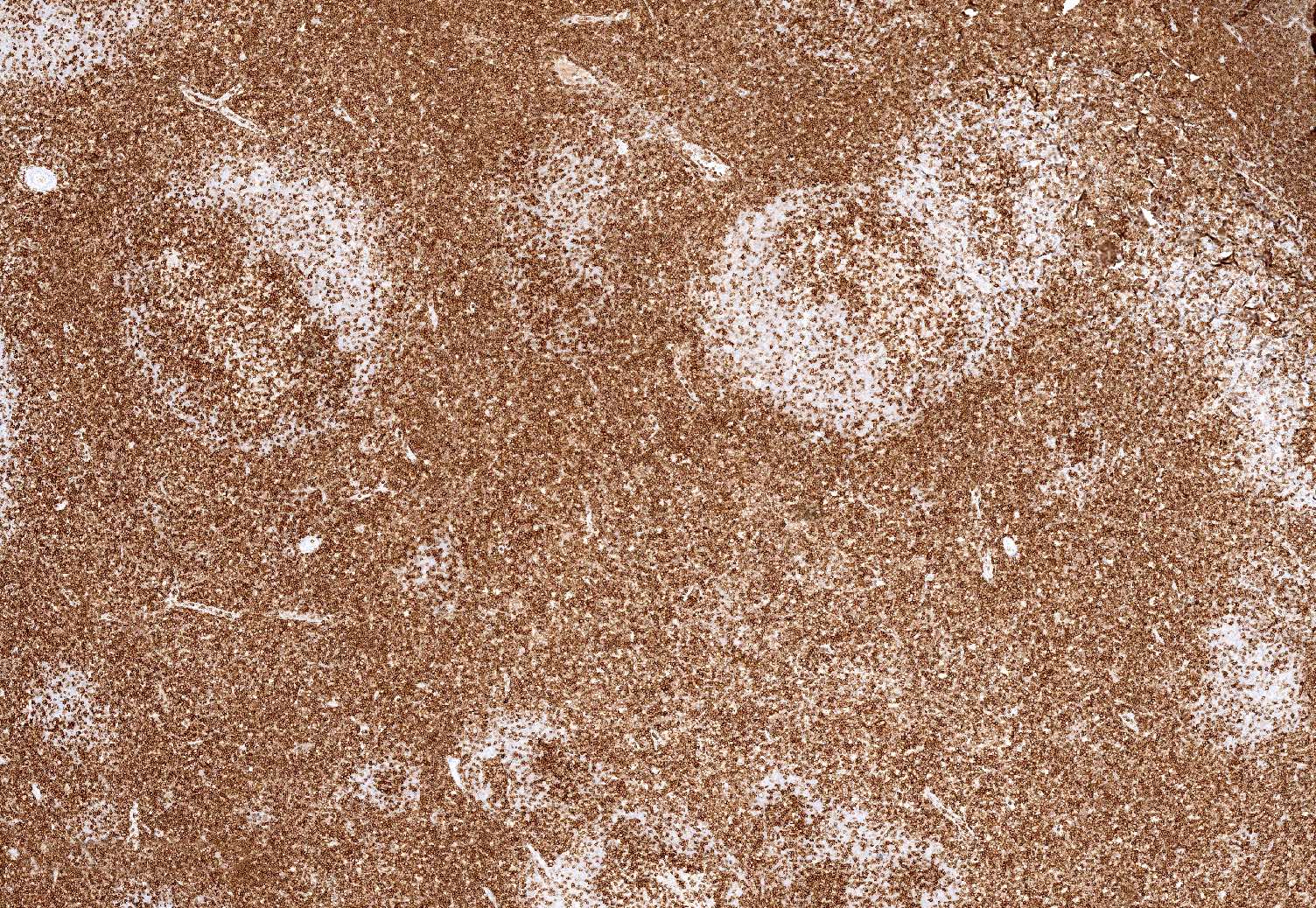
Microscopic (histologic) images
Positive stains
- Positive for CD20, CD19, CD79a, PAX5, CD43 (70 - 100%), MUM1 (plasma cells and lymphoplasmacytic cells), BCL2 (50%) (Adv Anat Pathol 2017;24:128, Virchows Arch 2016;468:141)
- In cases with plasmacytoid differentiation, light chain restriction can be demonstrated by light chain immunohistochemical stains (Pediatr Blood Cancer 2020;67:e28416)
- IgD highlights irregular and expanded mantle zone (Hematol Oncol 2019;37:53)
- Ki67 demonstrates low proliferation rate in interfollicular areas and may demonstrate polarization of follicles (Virchows Arch 2016;468:141, Adv Anat Pathol 2017;24:128)
Negative stains
- CD10 and BCL6 (Pediatr Blood Cancer 2020;67:e28416)
- CD23 is negative but may identify disrupted follicular dendritic cell meshworks (Adv Anat Pathol 2017;24:128)
Flow cytometry description
- Light chain restricted monotypic B cells (Virchows Arch 2016;468:141)
Molecular / cytogenetics description
- Clonal immunoglobulin heavy chain (IGH) gene rearrangements in virtually all cases (Pediatr Blood Cancer 2020;67:e28416)
- Cytogenetic abnormalities include trisomy 18 (21%) and trisomy 3 (Virchows Arch 2016;468:141)
- Mutations identified in pathways important for transcription, intracellular signaling and cellular organization
- Somatic variant in AMOTL1 identified, also implicated in pathogenesis of splenic marginal zone lymphoma (Mod Pathol 2016;29:1212)
- Negative for MYC, BCL2, BCL6 and IRF4 rearrangements (Adv Anat Pathol 2017;24:128)
- Low genetic complexity, recurrent alterations in MAP2K1, TNFRSF14, KMT2C, IRF8 and NOTCH2, which is similar to pediatric type follicular lymphoma (Blood Adv 2022 May 24 [Epub ahead of print], Am J Surg Pathol 2022 Jul 14 [Epub ahead of print])
Sample pathology report
- Cervical lymph node, excisional biopsy:
- Pediatric nodal marginal zone lymphoma
- Histologic description: Sections show lymph node with effaced architecture by large nodules / follicles with markedly expanded marginal zones. Focally, there are large follicles that appear transformed with extension of mantle zones into germinal centers. Lymphoid infiltrate consists predominantly of small monocytoid appearing cells and scattered plasma cells.
- Immunohistochemical stains show the atypical lymphoid cells to be positive for CD20, PAX5, CD43 and BCL2. They are negative for CD10 and BCL6. IgD highlights mantle zone expansion. Ki67 proliferative index is low (< 10%) in the atypical infiltrate.
- Molecular studies are positive for clonal immunoglobulin heavy chain (IGH) gene rearrangement.
Differential diagnosis
- Atypical marginal zone hyperplasia with monotypic immunoglobulin expression:
- Similar clinical and morphologic features (Adv Anat Pathol 2017;24:128)
- Usually occurs in extranodal sites but may occur in lymph nodes (Virchows Arch 2016;468:141)
- Nodal process has been associated with Hemophilus influenzae infection
- Aberrant expression of CD43 (Adv Anat Pathol 2017;24:128)
- Cases show lambda light chain restriction but no molecular evidence of clonality (Virchows Arch 2016;468:141)
- Pediatric type follicular lymphoma:
- Follicles are usually often back to back, with relatively few interfollicular B cells
- More monomorphic cell population consisting of medium to large sized blastoid cells with round to oval nuclei, small nucleoli, fine chromatin and scant cytoplasm
- Germinal center phenotype, with positivity for CD10, BCL6, HGAL and LMO2
- Diffuse areas are not typically present
- Less numerous PD-1 positive cells compared to pediatric NMZL, pushed to periphery of germinal centers (Adv Anat Pathol 2017;24:128)
- Some studies suggest that both (pediatric follicular lymphoma and pediatric NMZL) are histologic variants of same disease due to similar mutational profiles, low genetic complexity in both diseases and similar methylation profiles (Blood Adv 2022 May 24 [Epub ahead of print], Am J Surg Pathol 2022 Jul 14 [Epub ahead of print])
- Adult type nodal marginal zone lymphoma:
- Expanded follicles of pediatric NMZL may resemble adult NMZL (floral variant) (Adv Anat Pathol 2017;24:128)
Board review style question #1
An 18 year old man presents with localized nontender cervical lymphadenopathy. Excisional biopsy was performed and representative images are shown above. Flow cytometry showed a lambda light chain restricted B cell population, while molecular analysis shows a clonal IGH rearrangement. What is the most likely diagnosis?
- Adult marginal zone lymphoma
- Atypical marginal zone hyperplasia
- Pediatric nodal marginal zone lymphoma
- Pediatric type follicular lymphoma
- Progressive transformation of germinal centers
Board review style answer #1
C. Pediatric nodal marginal zone lymphoma. The images show a lymph node with architecture effaced by atypical lymphoid proliferation composed of large follicles and extension of mantle zones into the germinal centers, mimicking progressive transformation of germinal centers. On higher magnification, the lymphoid infiltrate expands the marginal zone and extends into the interfollicular area. Flow cytometry and molecular studies support a lymphoma diagnosis over a benign process. Given the clinical history of a young male with localized nontender cervical lymphadenopathy, morphologic findings, in conjunction with ancillary studies, are most consistent with pediatric nodal marginal zone lymphoma.
Comment Here
Reference: Pediatric nodal marginal zone lymphoma
Comment Here
Reference: Pediatric nodal marginal zone lymphoma
Board review style question #2
Which panel of immunohistochemical stains is most consistent with pediatric marginal zone lymphoma?
- CD20+, CD10+, BCL6+, BCL2+
- CD20+, CD43+, CD10-, BCL6-, BCL2+
- CD20+, CD43-, CD10-, BCL2-, CD5-
- CD20-, CD3+, PD-1+
- CD20+, CD10+, BCL6+, BCL2-
Board review style answer #2
B. CD20+, CD43+, CD10-, BCL6-, BCL2+. In pediatric nodal marginal zone lymphoma, the lymphoma cells are neoplastic B cells, positive for CD20, CD43 and BCL2. They are not derived from a germinal center and are negative for CD10 and BCL6. Therefore, answer B is the best choice. Answer A is consistent with lymphoma of germinal center origin. The stains in answer C are nonspecific. Stains in answer D are supportive of a T cell process. The stains in answer E can be seen in reactive follicular hyperplasia, among other diagnoses.
Comment Here
Reference: Pediatric nodal marginal zone lymphoma
Comment Here
Reference: Pediatric nodal marginal zone lymphoma