Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Peripheral smear description | Positive stains | Negative stains | Flow cytometry description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Klairmont MM, Choi JK. Peripheral T cell lymphoma, NOS. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lymphomanonbperipheral.html. Accessed April 1st, 2025.
Definition / general
- Mature T cell lymphoma that does not meet WHO classification criteria for other mature T cell lymphoma entities
Essential features
- Mature T cell lymphoma that does not meet criteria for other T cell lymphomas in the current WHO classification system
- Usually has aggressive clinical behavior
- CD4 > CD8, CD30 variable (if positive, heterogenous staining), EMA-, ALK-, negative for T follicular helper markers (CD10, BCL6, PD1, CXCL13, etc.), EBER-
Terminology
- T cell lymphoma, NOS
- Lymphoepithelioid lymphoma
- Lennert lymphoma
ICD coding
- ICD-O: 9702/3 - Mature T cell lymphoma, NOS
Epidemiology
- Accounts for 30% of PTCL in Western countries
- Most commonly a disease of adulthood
- Can rarely occur in children (J Pediatr Hematol Oncol 2012;34:611)
- M:F = 2:1
Sites
- Most commonly presents with peripheral lymphadenopathy (87%) but can involve any site; extranodal disease present in 62% (Blood 2011;117:3402)
- Most common extranodal sites: skin, gastrointestinal tract; lungs and central nervous system less common
- Majority (69%) present with advanced stage disease (Blood 2011;117:3402)
- Advanced stage disease associated with secondary involvement of marrow, liver, spleen and other extranodal sites
- Can involve peripheral blood
Pathophysiology
- Not definitively established
Etiology
- Cell of origin: activated mature T cell (typically CD4+ memory T cell)
Diagrams / tables
Clinical features
- B symptoms (35%) (J Clin Oncol 2006;24:2472)
- Can be associated with eosinophilia, pruritis and hemophagocytic syndrome (rare)
Diagnosis
- Diagnosis established by a combination of morphologic and immunophenotypic findings on tissue biopsy (i.e. lymph node) which demonstrate a mature T cell lymphoma that does not meet criteria for other mature T cell lymphomas in the 2016 WHO classification (Swerdlow: WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues, 4th Edition, 2017)
- Bone marrow biopsy for staging
- Peripheral blood may be involved but not typically a presenting site
Laboratory
- ↑ LDH (47%) (J Clin Oncol 2006;24:2472)
Radiology description
- Lymphadenopathy
Prognostic factors
- Stage and international prognostic index (IPI) score are the most well established prognostic factors
- 5 year overall survival for low IPI is 50 - 59% versus 9 - 18% for high IPI
- Other high risk prognostic features: bone marrow involvement, Ki67 > 80%, thrombocytopenia, GATA3 subtype by gene expression profiling or IHC (Blood 2014;123:2915)
- Prognostically significant molecular subtypes evaluable by IHC (Blood 2019;134:2159):
- GATA3 subtype (35% of PTCL, NOS):
- ≥ 50% tumor cells positive for GATA3 or CXCR3 by IHC
- Associated with monomorphic morphology with minimal inflammatory background
- Very poor overall survival (5 year overall survival = 19%)
- TBX21 subtype (58% of PTCL, NOS):
- ≥ 20% tumor cells positive for TBX21 or CCR4 by IHC
- Associated with polymorphous morphology
- Longer overall survival than GATA3 subtype (5 year overall survival = 38%)
- GATA3 subtype (35% of PTCL, NOS):
Case reports
- 50 year old woman with skin plaques and hypereosinophilia (JAAD Case Rep 2018;4:651)
- 52 year old man with fever and lymphadenopathy (BMJ Case Rep 2018;2018:bcr2017220858)
- 61 year old man with ascites (PTCL, NOS diagnosed by cytology) (J Gastrointest Oncol 2016;7:S96)
- 68 year old man with right upper lung mass and lymphadenopathy (Respir Med Case Rep 2018;23:176)
- 76 year old man with aberrant expression of CD79a and CD20 (Mod Pathol 2001;14:105)
Treatment
- Induction: CHOP (cyclophosphamide, doxorubicin, vincristine and prednisone) or other anthracycline based regimens (CHOEP, EPOCH)
- Consolidation: autologous stem cell transplantation for responders
- Approved second line drugs for relapsed / refractory disease: pralatrexate, romidepsin, belinostat and brentuximab vedotin
- Reference: Blood 2017;129:1103
Gross description
- Enlarged lymph node
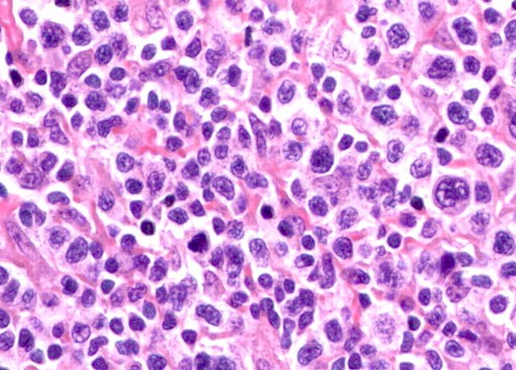
Microscopic (histologic) description
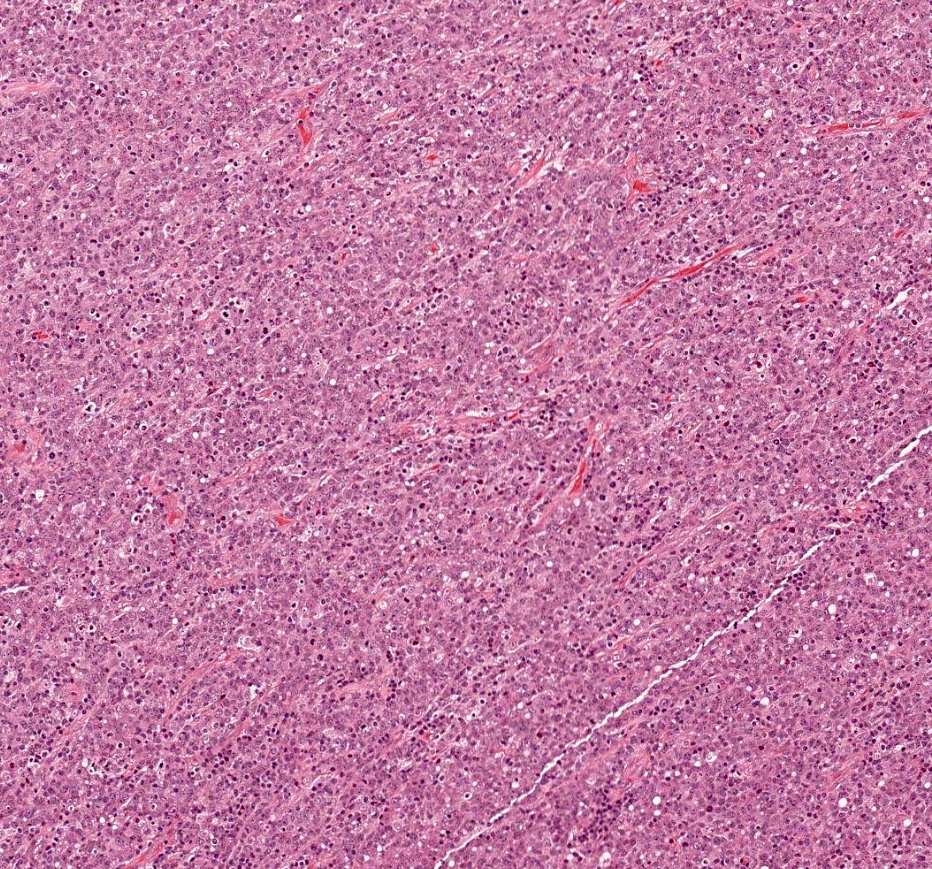
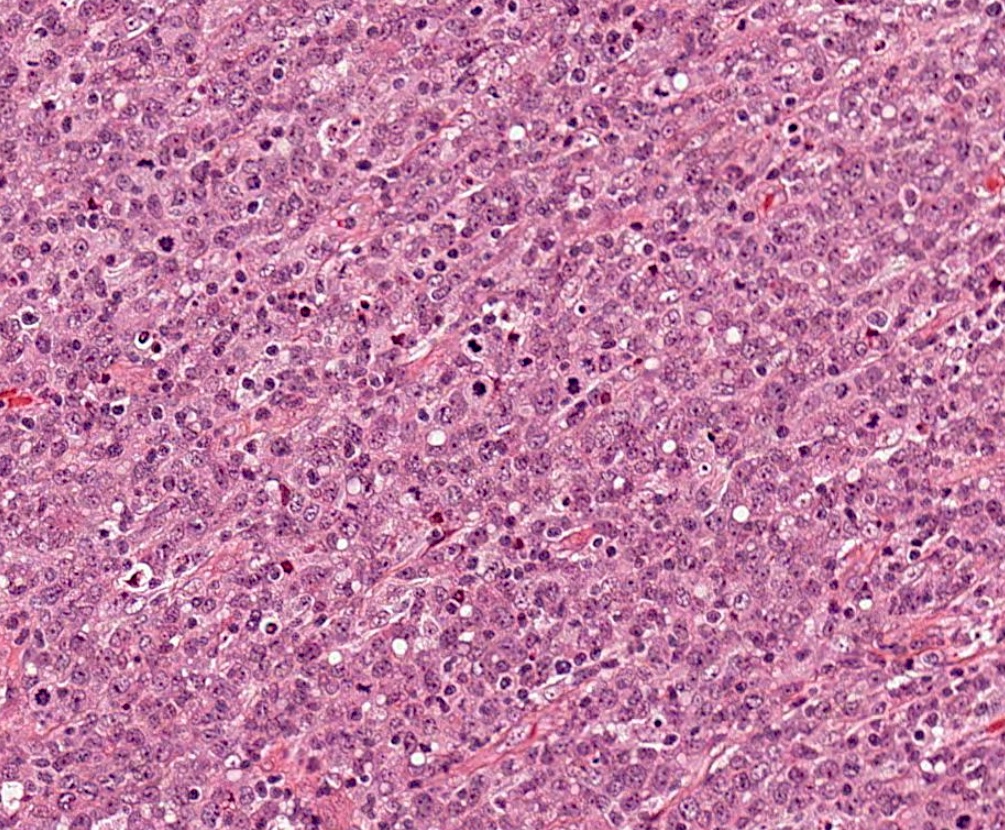
- Lymph node:
- Paracortical or diffuse infiltrate with effacement of the normal architecture by medium to large sized cells with pleomorphic nuclei, vesicular chromatin, prominent nucleoli and frequent mitoses
- Clear cells and Reed-Sternberg-like cells can be seen
- TBX21 subtype associated with a polymorphous inflammatory background composed of small lymphocytes, eosinophils, plasma cells, large B cells and epithelioid histiocytes (Blood 2019;134:2159)
- GATA3 subtype associated with with monomorphic morphology with minimal inflammatory background (Blood 2019;134:2159)
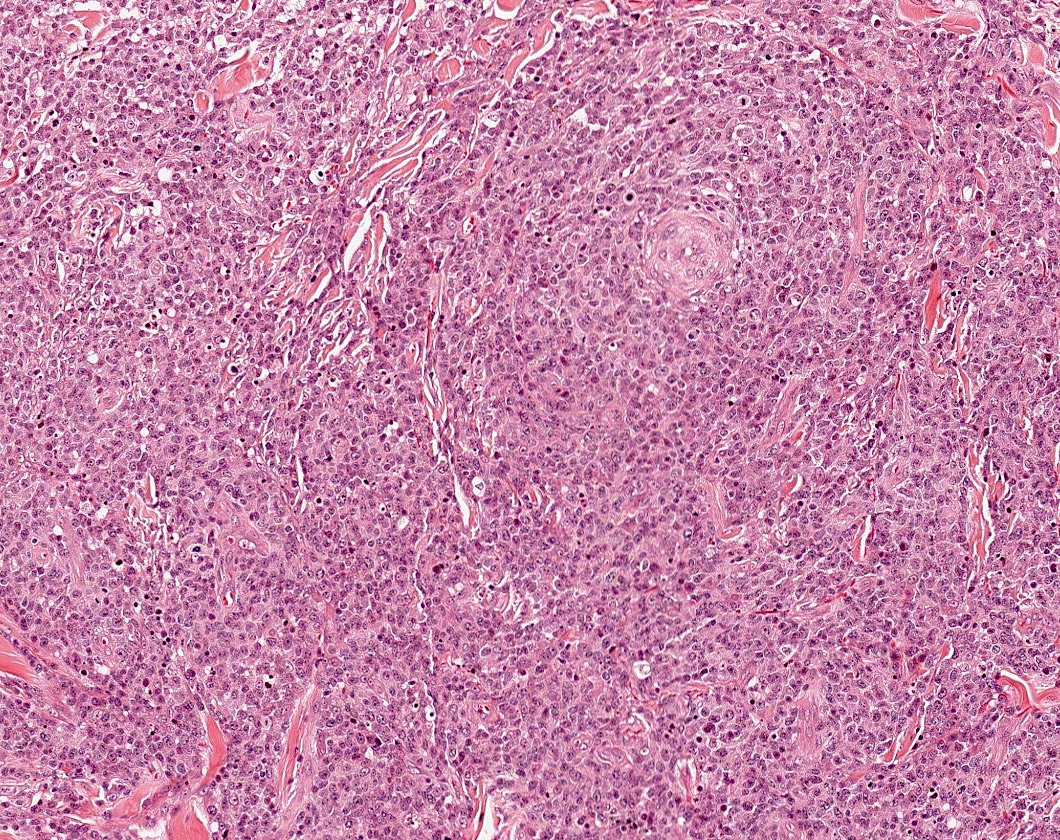
- Lymphoepithelioid variant (Lennert lymphoma)
- Typically shows a diffuse (less commonly paracortical) infiltrate of small cells with subtle nuclear atypia (typically CD8+ with expression of cytotoxic markers), numerous epithelioid histiocytes which often form clusters and occasional immunoblasts
- Correlates with TBX21 molecular subtype
- May have better prognosis than other PTCL, NOS subsets
- Paracortical or diffuse infiltrate with effacement of the normal architecture by medium to large sized cells with pleomorphic nuclei, vesicular chromatin, prominent nucleoli and frequent mitoses
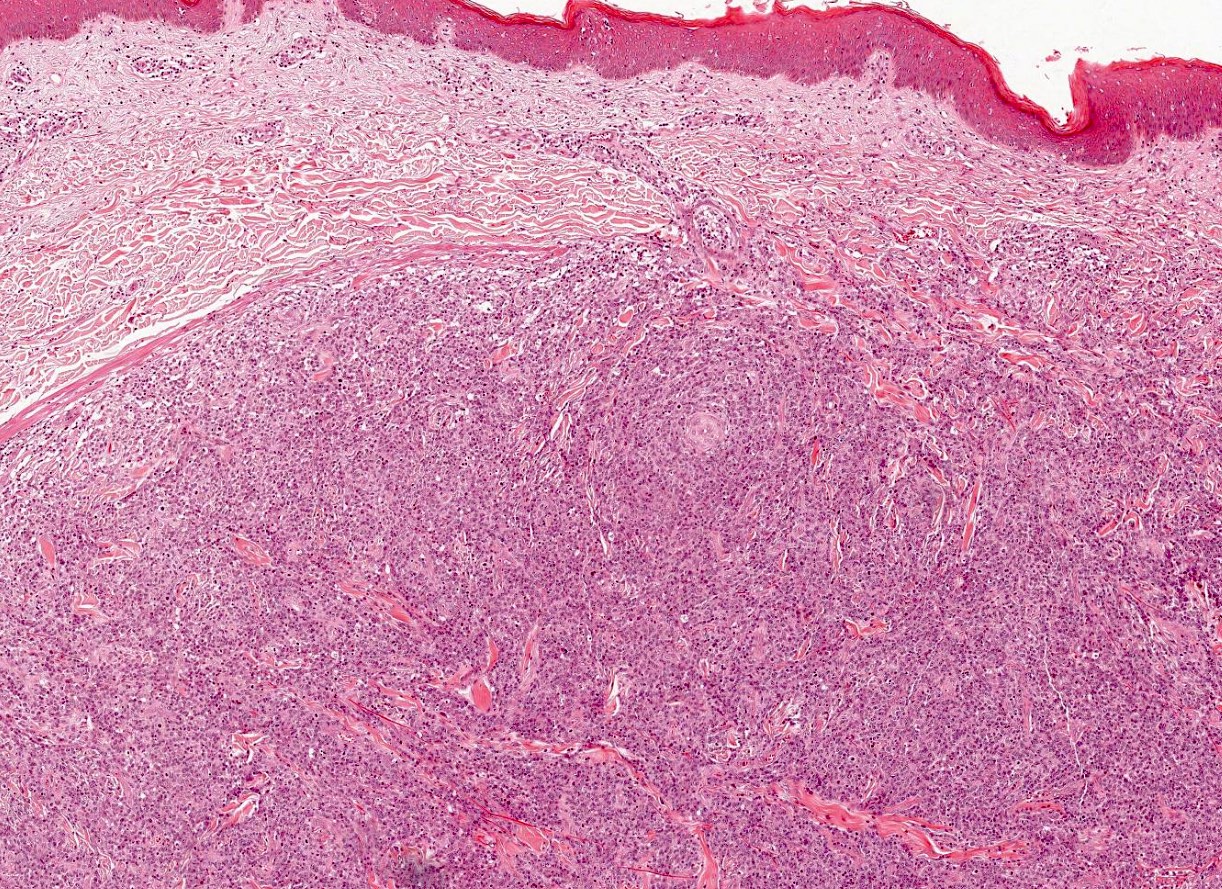
- Skin:
- Lymphoma cells infiltrate the dermis and subcutis; often form nodules which can undergo central necrosis
- Epidermotropism, angiocentricity and adnexal involvement can be seen
- Clinical correlation is needed to exclude mycosis fungoides, anaplastic large cell lymphoma, lymphomatoid papulosis
Microscopic (histologic) images
Cytology description
- Broad cytologic spectrum, cannot diagnose based on cytology alone
- Medium to large tumor cells with irregular, pleomorphic, hyperchromatic or vesicular chromatin; prominent nucleoli; numerous mitotic figures; polymorphous inflammatory background
Cytology images
Peripheral smear description
- Peripheral blood involvement can occur and presents with circulating medium to large tumor cells with nuclear atypia, vesicular chromatin and prominent nucleoli
Positive stains
- Variable expression of pan-T cell markers: CD2 (70%), CD3 (86%), CD5 (20%), CD7 (19%) (J Clin Oncol 2006;24:2472)
- Any combination of CD4 / CD8 expression can be seen: CD4+ / CD8- (38%), CD4+ / CD8+ (8%), CD4- / CD8- (47%), CD4- / CD8+ (7%) (J Clin Oncol 2006;24:2472)
- TCRβF1 (97%), which is negative in gamma delta T cell lymphoma and NK lymphomas (J Clin Oncol 2006;24:2472)
- CD30 can be variably expressed in a subset of tumor cells (~50% cases show > 25% CD30+ cells) (Haematologica 2013;98:e81)
- Intensity of CD30 staining in PTCL, NOS typically heterogenous whereas in ALK- anaplastic large cell lymphoma it is strong and uniform
- CD52 (40%) (Haematologica 2007;92:566)
- TIA1 (27%), CD56 (6%), granzyme B (2%), perforin (J Clin Oncol 2006;24:2472)
- CD15 (4%): when present, often coexpressed with CD30 (J Clin Oncol 2006;24:2472)
- EBER ISH (5%): more commonly involves background B cells (J Clin Oncol 2006;24:2472)
Negative stains
- B cell markers (i.e. CD20, CD79a) typically negative but can be aberrantly expressed in rare cases (J Clin Oncol 2006;24:2472)
- PAX5 represents the most specific B cell marker in these circumstances but gene rearrangement studies are indicated to resolve lineage
- Most markers of a T follicular helper phenotype should be negative (CD10, BCL6, PD1, CXCL13, CXCR5, CD278 (ICOS) and SAP); positivity of 2 or more precludes the diagnosis of PTCL, NOS (Am J Surg Pathol 2019;43:1282, Swerdlow: WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues, 4th Edition, 2017)
- ALK
- EMA (positive in a subset of anaplastic large cell lymphoma)
- TdT
Flow cytometry description
- Flow cytometry may be helpful in identifying aberrant loss of pan-T cell antigens but is typically not sufficient to classify tumor as PTCL, NOS
Molecular / cytogenetics description
- PCR demonstrates clonal rearrangement of TCR genes
- Next generation sequencing shows recurrent alterations of TP53 (> 40%), TET2 (> 40%), RHOA (~35%), CDKN2A (~20%), CD28 (~20%), HLA-A (~20%), SETD1B (~20%) and DNMT3A (~10%), as well as numerous other less prevalent alterations (Leukemia 2019;33:2867)
- Cytogenetics: typically shows a complex karyotype but specific recurrent abnormalities very uncommon
- t(5;9)(q33;q22) / ITK-SYK associated with a follicular growth pattern (rare)
Sample pathology report
- Lymph node, left axillary, biopsy:
- Peripheral T cell lymphoma, NOS (see comment)
- Comment: H&E sections demonstrate effacement of the normal nodal architecture by a diffuse infiltrate of large, pleomorphic lymphoid cells with vesicular chromatin and prominent nucleoli. By paraffin immunohistochemistry, the tumor cells are positive for CD3, CD4, CD5 and CD30 (subset, variable intensity) while negative for CD20, CD7, CD8, CD15, TIA1, granzyme B, perforin, CD10, BCL6, PD1, CXCL13, CXCR5 and EBER ISH. PCR studies are positive for clonal TCR gene rearrangement. These findings are diagnostic for peripheral T cell lymphoma, NOS.
Differential diagnosis
- Classic Hodgkin lymphoma:
- As PTCL, NOS can present with Reed-Sternberg-like cells and CD30 expression (as well as occasional coexpression of CD15), misclassification as classic Hodgkin lymphoma is an important pitfall to consider, particularly on limited needle biopsies
- Careful immunophenotyping of the tumor cells to establish lineage is essential to avoid misclassification (Hodgkin / Reed-Sternberg cells may have aberrant T cell antigen expression but should be CD3 negative, though PTCL, NOS can also be CD3 negative)
- Classic Hodgkin lymphoma should be CD43 negative and weakly PAX5 positive
- PCR clonality assays can help resolve lineage (PTCL, NOS should show clonal rearrangement of TCR genes)
- T cell lymphoma subtypes defined by WHO classification (Swerdlow: WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues, 4th Edition, 2017):
- ALK negative anaplastic large cell lymphoma:
- T cell lymphomas with a T follicular helper phenotype (angioimmunoblastic T cell lymphoma, nodal peripheral T cell lymphoma with T follicular helper phenotype and follicular T cell lymphoma):
- Adult T cell leukemia / lymphoma:
- Adult T cell leukemia / lymphoma associated with positive HTLV1 serology or demonstration of HTLV1 integration in tumor cells
- CD25 positive in adult T cell leukemia / lymphoma but variable in PTCL, NOS
- PTCL, NOS often has polymorphous inflammatory background
- Involvement by mycosis fungoides:
- Clinical history and staging critical to separating nodal involvement by mycosis fungoides from PTCL, NOS
Board review style question #1
A 60 year old man presents with diffuse lymphadenopathy. Lymph node biopsy shows complete effacement of the normal lymph node architecture by a diffuse infiltrate of medium to large pleomorphic lymphoid cells with vesicular chromatin and prominent nucleoli. Immunostains show the tumor cells are positive for CD3, CD5 and CD4 while negative for CD8, CD7, CD20, ALK. Which of the following findings would support the diagnosis of PTCL, NOS?
- Coexpression of BCL6, PD1 and CD10
- EMA positivity
- Heterogenous CD30 positivity
- Strong and uniform CD30 positivity
Board review style answer #1
C. Heterogenous CD30 positivity
Comment Here
Reference: Peripheral T cell lymphoma, not otherwise specified
- PTCL, NOS should not coexpress multiple T follicular helper (TFH) markers. Expression of > 2 TFH markers in addition to CD4 (PD1, CD10, BCL6, CXCL13, CXCR5, CD278, SAP) would suggest nodal peripheral T cell lymphoma with a TFH phenotype.
- EMA should be negative in PTCL, NOS but can be expressed in ALCL.
- Heterogenous CD30 positivity can be a feature of PTCL, NOS. Strong and uniform CD30 positivity in this case would support the diagnosis of ALK negative anaplastic large cell lymphoma.
- Strong and uniform CD30 positivity in this case would support a diagnosis of ALK negative anaplastic large cell lymphoma. CD30 is positive in a subset of PTCL, NOS but the staining is heterogeneous and of variable intensity.
Comment Here
Reference: Peripheral T cell lymphoma, not otherwise specified
Board review style question #2
A 65 year old woman presents with lymphadenopathy. Lymph node biopsy shows effacement of the normal lymph node architecture by a diffuse infiltrate of medium to large pleomorphic tumor cells with vesicular chromatin and prominent nucleoli. By paraffin immunohistochemistry, the tumor cells are positive for CD3, CD8, CD5, PD1, granzyme B and CD30 (subset, variable intensity) while negative for CD4, CD7, ALK, perforin, EMA, CD10, BCL6, CXCR5 and CXCL13. EBER ISH shows rare positivity in small background lymphocytes with benign cytology. CD21 shows focal areas with small residual follicular dendritic cell meshworks. The best classification for this lesion is
- ALK negative anaplastic large cell lymphoma
- Angioimmunoblastic T cell lymphoma (AITL)
- Nodal peripheral T cell lymphoma with TFH phenotype
- Peripheral T cell lymphoma, NOS
Board review style answer #2
D. Peripheral T cell lymphoma, NOS
Comment Here
Reference: Peripheral T cell lymphoma, not otherwise specified
- ALK negative anaplastic large cell lymphoma would have strong and uniform CD30 expression.
- Angioimmunoblastic T cell lymphoma (AITL) is typically CD4+ and expresses > 2 TFH markers (this case only appears to express one, PD1). Further, AITL characteristically has expanded follicular dendritic cell meshworks which can be visualized with a CD21 immunostain.
- Like AITL, there must be expression of > 2 TFH markers to qualify for the classification of nodal peripheral T cell lymphoma with TFH phenotype.
- PTCL, NOS is the best classification for this T cell lymphoma which does not meet the criteria for any other category of mature T cell lymphoma. Although PTCL, NOS is typically CD4+ / CD8-, it can present with any pattern of CD4 / CD8 expression.
Comment Here
Reference: Peripheral T cell lymphoma, not otherwise specified