Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Flow cytometry description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Marques-Piubelli ML, Miranda RN. Nodal T follicular helper lymphoma, angioimmunoblastic type. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lymphomanonbaitl.html. Accessed April 1st, 2025.
Definition / general
- Nodal based, mature T cell lymphoma derived from CD4+ T follicular helper (TFH) cells admixed with a polymorphous infiltrate of reactive cells and prominent proliferation of high endothelial venules and follicular dendritic cells
- Patients usually present with lymphadenopathy, systemic disease and immunodysregulation
- References: Blood 2017;129:1095, Am J Surg Pathol 2016;40:335, Histopathology 2014;64:171, Blood 2014;123:1293, Leukemia 2020;34:2592, Am J Clin Pathol 2021;156:1
Essential features
- Nodal based, mature T cell lymphoma derived from CD4+ T follicular helper (TFH) cells admixed with a polymorphous infiltrate of reactive cells and prominent proliferation of high endothelial venules and follicular dendritic cells
- Patients usually present with lymphadenopathy, systemic disease and immunodysregulation (Blood 2017;129:1095, Am J Surg Pathol 2016;40:335, Histopathology 2014;64:171, Blood 2014;123:1293, Leukemia 2020;34:2592, Am J Clin Pathol 2021;156:1)
- Expression of TFH markers (Blood 2017;129:1095, Am J Surg Pathol 2016;40:335, Histopathology 2014;64:171, Nat Genet 2014;46:371, Hum Pathol 2010;41:79, Mod Pathol 2009;22:753, Am J Clin Pathol 2007;128:854, Am J Surg Pathol 2007;31:1077, Br J Haematol 2007;138:733, Leukemia 2006;20:296, Leukemia 2022;36:165, Blood 2008;111:4463, Am J Surg Pathol 2007;31:1068, Haematologica 2007;92:1059, Am J Surg Pathol 2004;28:54):
- εCD3, CD4, CXCL13, CD10, PD-1 (CD279), ICOS, BCL6, CD200, CXCR5, cMAF, SAP, TIGIT, CD27
- Unique mutational profile (Blood 2017;129:1095, Am J Surg Pathol 2016;40:335, Blood 2014;123:1293, Nat Genet 2014;46:371, Blood 2015;126:1741, Leukemia 2020;34:2592, Blood 2014;123:2915, Haematologica 2015;100:e505, Blood 2012;120:1466, Blood 2014;123:1293, Nat Genet 2014;46:166):
- Most common mutations are TET2, DNMT3, IDH2 and RHOA
Terminology
- Angioimmunoblastic lymphadenopathy with dysproteinemia (AILD)
- Immunoblastic lymphadenopathy
- Lymphogranulomatosis X
ICD coding
Epidemiology
- Represents 15 - 20% of all peripheral T cell lymphomas and 1 - 2% of all non-Hodgkin lymphomas (Leuk Lymphoma 2016;57:2804, Blood 2017;129:1095, Am J Surg Pathol 2016;40:335, Leukemia 2020;34:2592, J Clin Oncol 2013;31:240)
- Usually affects patients in the sixth and seventh decades; median of 65 - 69 years old (Leuk Lymphoma 2016;57:2804, Blood 2017;129:1095 Am J Surg Pathol 2016;40:335, Blood 2014;123:1293, J Clin Oncol 2009;27:3951, Medicine (Baltimore) 2007;86:282)
- Sex predominance varies but usually shows slight male predominance (Leuk Lymphoma 2016;57:2804, Blood 2017;129:1095, Am J Clin Pathol 2007;128:854, Am J Surg Pathol 2007;31:1077, Leukemia 2006;20:296, Medicine (Baltimore) 2007;86:282)
- Geographic distribution: more common in Europe than Asia (Blood 2017;129:1095, Br J Haematol 2007;138:733, Leukemia 2020;34:2592, Blood 2008;111:4463, Haematologica 2015;100:e361)
- In Asia, T / NK lymphomas are more frequent than angioimmunoblastic T cell lymphoma (AITL)
- No specific ethnic predisposition
Sites
- Common involvement of mediastinal and retroperitoneal lymph nodes (Medicine (Baltimore) 2007;86:282)
- Bulky disease is rare
- Bone marrow involvement in ~60% of cases (Medicine (Baltimore) 2007;86:282)
- Extranodal involvement is variable (Blood 2017;129:1095, Mod Pathol 2009;22:753, Medicine (Baltimore) 2007;86:282, Am J Surg Pathol 2007;31:1068)
- Skin, spleen and liver are the most common extranodal sites
- Peripheral blood involvement is rare (Blood 2017;129:1095)
Pathophysiology
- T follicular helper (TFH) cells are essential checkpoints for the B cell activation and differentiation from centroblast to centrocytes; consequently these cells become either plasma cells or memory B cells (Blood 2017;129:1095)
- TFH tolerance is an important mechanism in the prevention of autoimmune diseases
- Dysregulation of TFH checkpoints may cause a germinal center anarchy and consequent AITL
Etiology
- Somatic mutations (Blood 2017;129:1095, Nat Genet 2014;46:371):
- TET2, DNMT3A, IDH2-R172 and RHOA
- Immunodysregulation (Blood 2017;129:1095, Leukemia 2022;36:165)
- Upregulation of TFH cells promotes a high differentiation of B cells, plasmacytic differentiation and hypergammaglobulinemia
- B cells of the tumor microenvironment decrease the expression of CD73 and CXCR5
- Expansion of a distinct population of CD8+ T cells with exhausted phenotype and upregulation of the chemokines XCL2 and XCL1
- Upregulation of TFH cells promotes a high differentiation of B cells, plasmacytic differentiation and hypergammaglobulinemia
- Possible relationship to Epstein-Barr virus (EBV) with disease progression (Blood 2017;129:1095, Am J Surg Pathol 2016;40:335)
- B cells in AITL usually show active EBV infection
Clinical features
- Patients usually present with advanced disease (stage III / IV) (Leuk Lymphoma 2016;57:2804, J Clin Oncol 2009;27:3951, Mod Pathol 2009;22:753, Am J Clin Pathol 2007;128:854, Am J Surg Pathol 2007;31:1077, Medicine (Baltimore) 2007;86:282, Blood 2008;111:4463)
- B symptoms and lymphadenopathy are the most common findings (~70 - 90%) (Blood 2017;129:1095, Mod Pathol 2009;22:753, Medicine (Baltimore) 2007;86:282)
- Hepatosplenomegaly (~50 - 80%) (Blood 2017;129:1095, Histopathology 2014;64:171, Mod Pathol 2009;22:753)
- Systemic symptoms due to immune dysregulation (Leuk Lymphoma 2016;57:2804, Blood 2017;129:1095, Histopathology 2014;64:171, Leukemia 2006;20:296, Leukemia 2022;36:165, Medicine (Baltimore) 2007;86:282, Blood 2008;111:4463, Am J Surg Pathol 2007;31:1068)
- Anemia (~10 - 80%)
- Warm autoimmune hemolytic anemia
- Thrombocytopenia (~10 - 30%)
- Polyclonal hypergammaglobulinemia (~50 - 80%)
- Monoclonal gammopathy (~10%)
- Hypereosinophilia (~30 - 40%)
- May be associated with infection
- Broad skin manifestations (~20 - 50%)
- Urticarial eruption
- Infiltrated purpura
- Nodules
- Erythroderma
- Maculopapular eruption
- Quincke edema
- Annular rash
- Plaques
- Tumor
- Cavity effusions (~40%)
- Usually neoplastic cells are absent on effusions or obscured by hypereosinophilia
- Arthralgia
- Associated or not associated with chondritis
- Neurological symptoms
- Confusion
- Polyneuritis
- Deafness
- Cerebellar syndrome
- Anemia (~10 - 80%)
Diagnosis
- May be challenging even in excisional biopsies; a precise diagnosis requires integration of clinical, immunophenotypic and molecular data (Leuk Lymphoma 2016;57:2804, Histopathology 2014;64:171, Am J Clin Pathol 2021;156:1)
- Although immune dysregulation is common, it is not mandatory for the diagnosis
- Majority of the diagnoses are made weeks to months after the patients report nonspecific symptoms (Blood 2017;129:1095)
Laboratory
- Elevated lactate dehydrogenase levels and β2 microglobulin, hypergammaglobulinemia, hypereosinophilia, anemia, thrombocytopenia and lymphopenia (Medicine (Baltimore) 2007;86:282, Blood 2012;120:1466)
Radiology description
- CT usually shows low bulky disease, which has variable uptake values on PET (Blood 2017;129:1095)
Prognostic factors
- Variable but usually unfavorable (Leuk Lymphoma 2016;57:2804, Blood 2017;129:1095, Blood 2014;123:1293, J Clin Oncol 2009;27:3951, Leukemia 2020;34:2592, J Clin Oncol 2013;31:240)
- Median overall survival: 18 - 29 months
- 1, 3 and 5 year overall survival of 66%, 64% and 32% respectively
- 5 year progression free survival of 18 - 38%
- Median overall survival: 18 - 29 months
- Alternative prognostic index for AITL (1 point each): low risk (0 - 1 risk points) and high risk (2 - 5 points) (Blood 2017;129:1095)
- Age > 60 years
- Eastern Cooperative Oncology Group (ECOG) performance status > 2
- Involvement of > 1 extranodal site
- B symptoms
- Thrombocytopenia (< 150 x 109/L)
- Factors associated with shorter overall survival (Medicine (Baltimore) 2007;86:282)
- High risk stratification
- Ascites
- Thrombocytopenia
- Hypoalbuminemia
- Renal failure
- Circulating atypical cells
- Hyperuricemia
- Gain of chromosome X
- Factors associated with worse progression free survival (Medicine (Baltimore) 2007;86:282)
- High risk stratification
- Generalized lymphadenopathy
- Thrombocytopenia
- Hypoalbuminemia
- May coexist or progress to EBV associated B cell lymphomas (e.g. EBV+ diffuse large B cell lymphoma) and classic Hodgkin lymphoma (Am J Surg Pathol 2007;31:1077, Br J Haematol 2007;138:733, Am J Clin Pathol 2002;117:368)
- Usually shows a type 2 or 3 of latency
Case reports
- 38 year old woman with peripheral blood involvement by AITL (Am J Blood Res 2020;10:257)
- 47 year old man with an Epstein-Barr virus induced cutaneous diffuse large B cell lymphoma and AITL (Am J Dermatopathol 2019;41:927)
- 75 year old woman with AITL and previous history of acute myeloid leukemia (Clin Case Rep 2020;8:3494)
- 76 year old man with a leukemic relapse of AITL (Br J Haematol 2020;189:592)
- 77 year old man with AITL and pure red cell aplasia (World J Clin Oncol 2020;11:405)
- 78 year old man with AITL after receiving pembrolizumab for metastatic melanoma (JAAD Case Rep 2020;6:1264)
Treatment
- Single agent oral therapies or intensive chemotherapy combination followed by autologous stem cell transplantation (Blood 2017;129:1095, J Clin Oncol 2009;27:3951, Leukemia 2020;34:2592, Blood 2008;111:4463, J Oncol Pract 2019;15:137)
- Good response but short remission duration
- No gold standard chemotherapy, usually anthracycline based regimen
- CHOP (cyclophosphamide, doxorubicin, vincristine, prednisone)
- 53% of complete remission in up front setting
- CHOEP (CHOP + etoposide)
- 51% of complete remission in up front setting
- Romidepsin + CHOP
- 51% of complete remission in relapsed / refractory setting
- Bevacizumab + CHOP
- R-CHOP (rituximab + CHOP)
- Alemtuzumab + CHOP
- ACVBP (doxorubicin, cyclophosphamide, vindestine, bleomycin, prednisone)
- ACVBP (doxorubicin, cyclophaphamide, vindesine, bleomycin, prednisone)
- Bortezomibe + ACVBP
- mBACOD (methotrexate, bleomycin, doxorubicin, cyclophosphamide, vincristine, dexamethasone)
- PEGS (cisplatinum, etoposide, gemcitabine, methylprednisolone)
- ICE (iphosphamide, carboplatin, etoposide), DHAP (dexamethasone, cytarabine, cisplatinum) and ESHAP (etoposide, methylprednisolone, cisplatinum, cytarabine)
- Relapsed / refractory setting
- CHOP (cyclophosphamide, doxorubicin, vincristine, prednisone)
- Single agents
- Used in a relapsed / refractory setting
- Pralatrexate
- Romidepsin
- Brentuximab vedotin
- Belinostat
- Bendamustine
- Lenalidomide
- Hypomethylating agents
- Azacitidine and decitabine
- Counterbalance the DNA hypermethylation caused by TET2 and IDH2 mutation
- Azacitidine and decitabine
- Consolidation with stem cell transplantation
- Able to achieve 70% of complete remission and progression free survival of 42% in 2 years
- Complete remission patients have better survival compared with those with partial remission (PR)
- Graft versus host disease (GVHD) may affect up to 60%
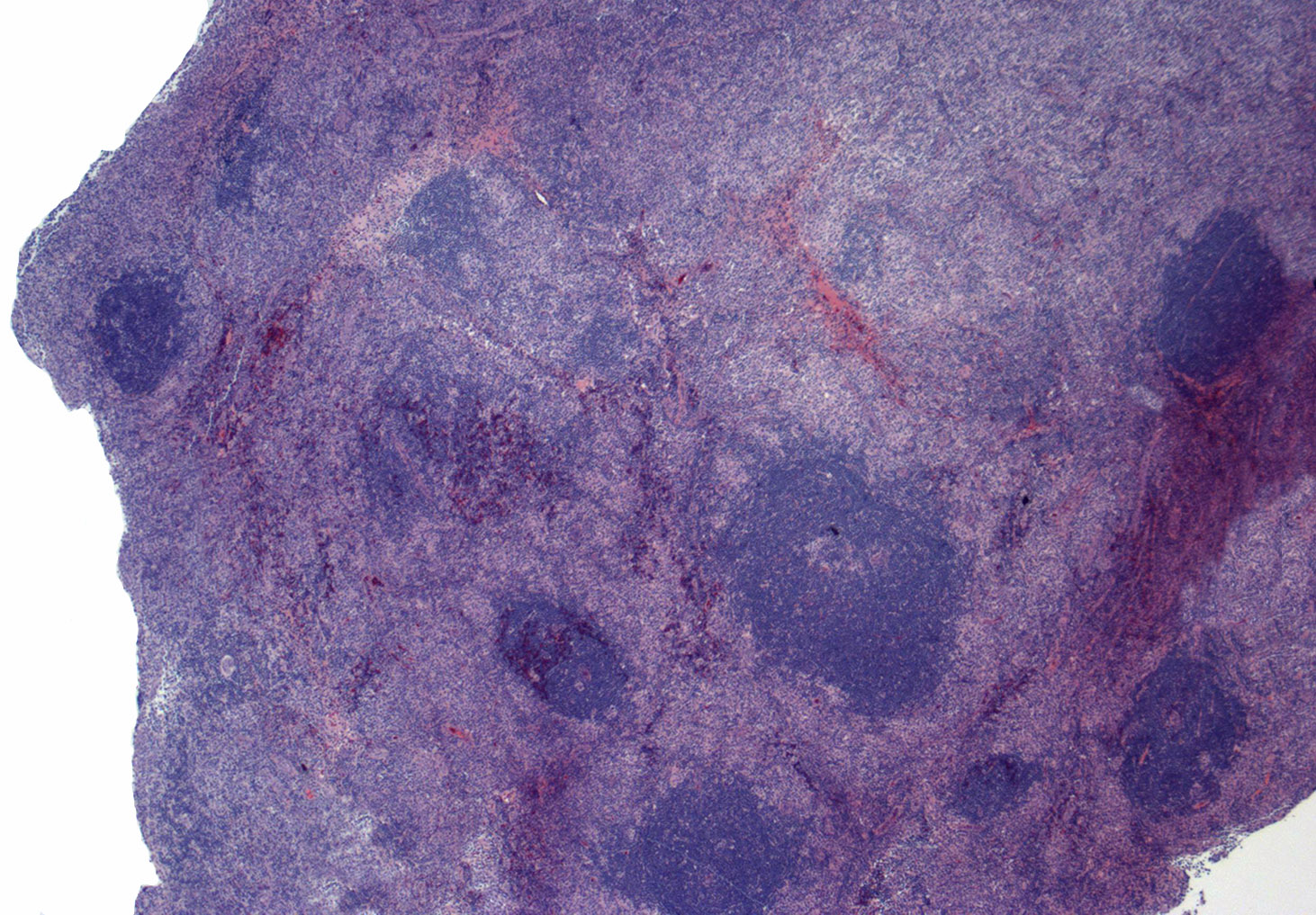
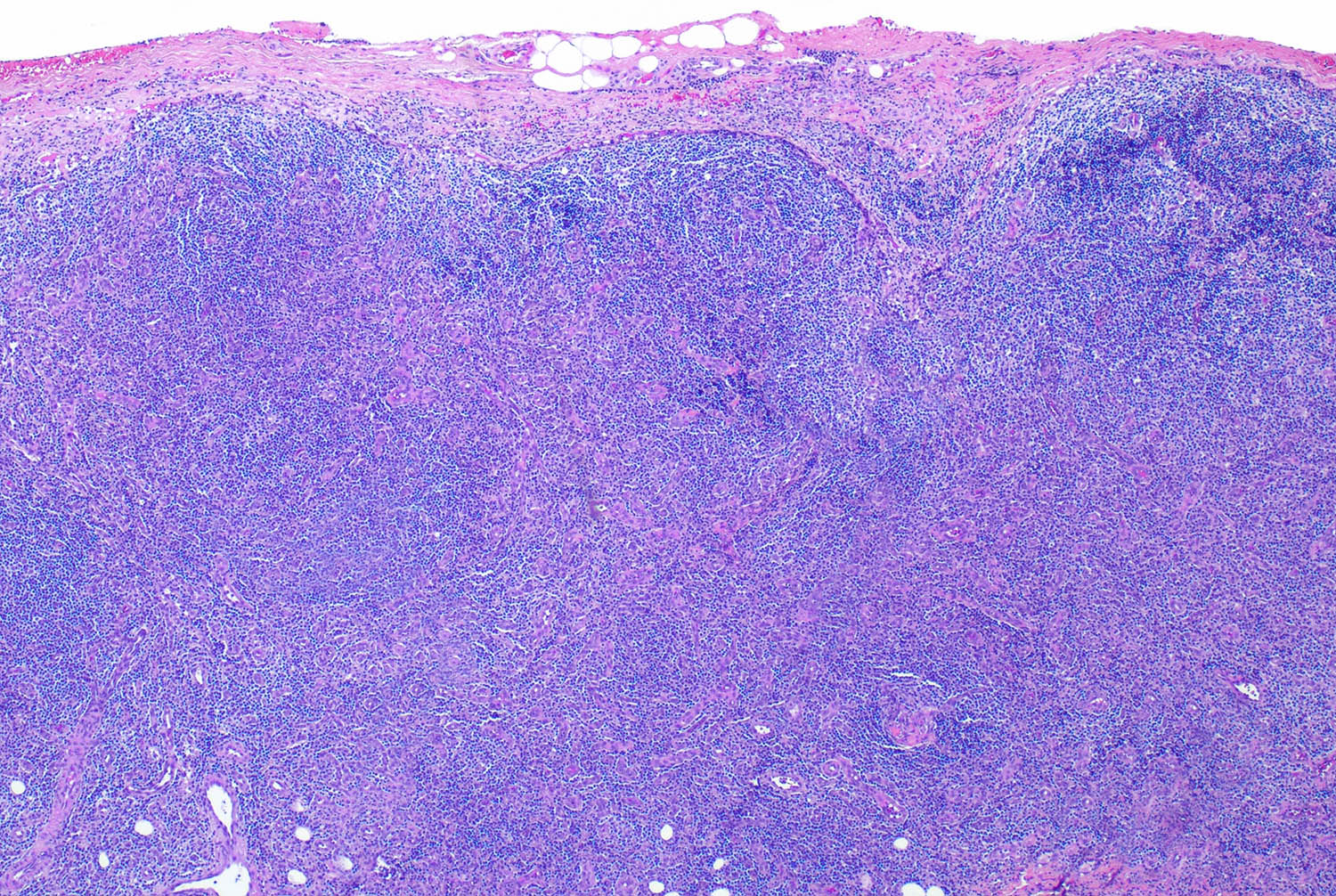
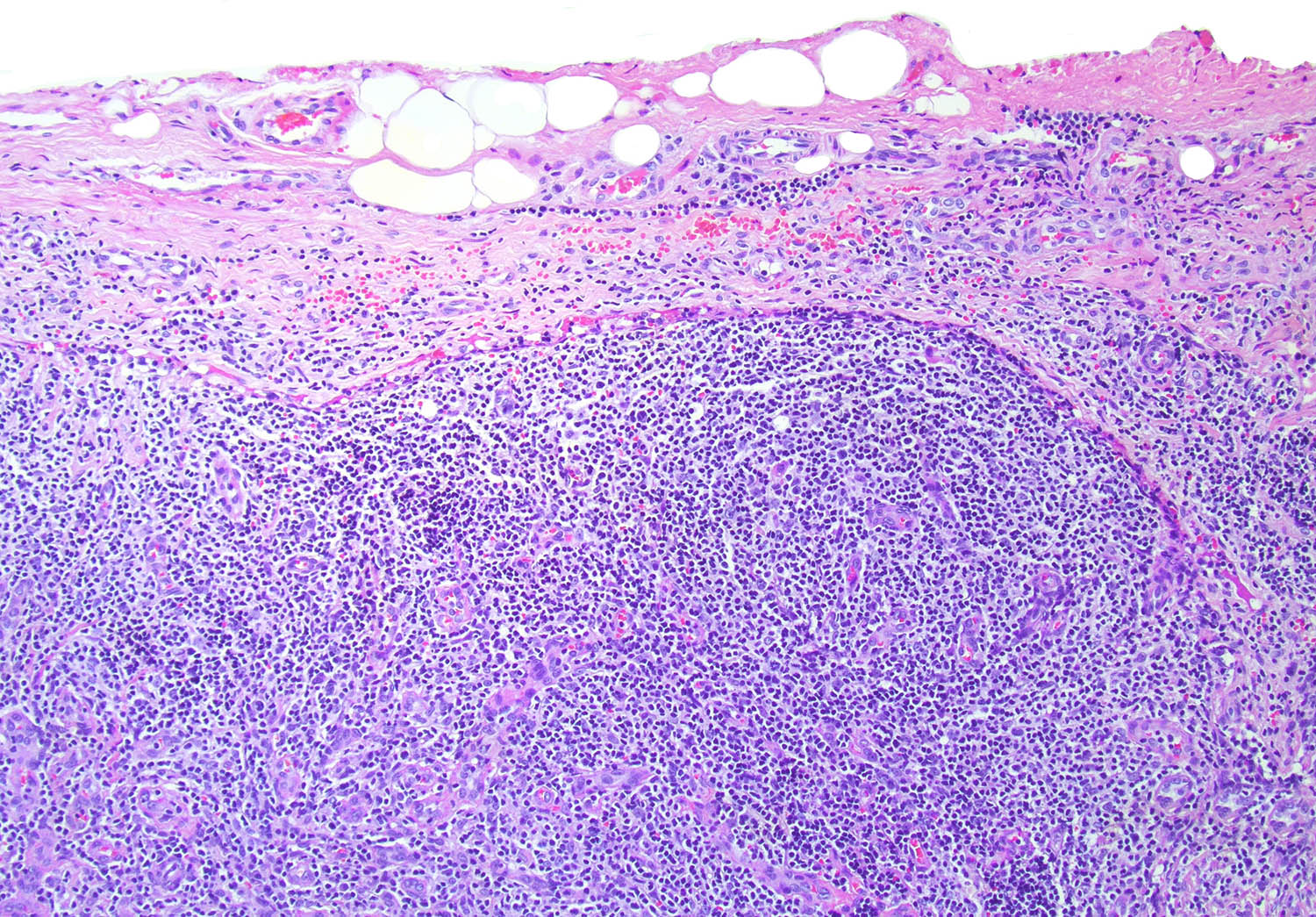
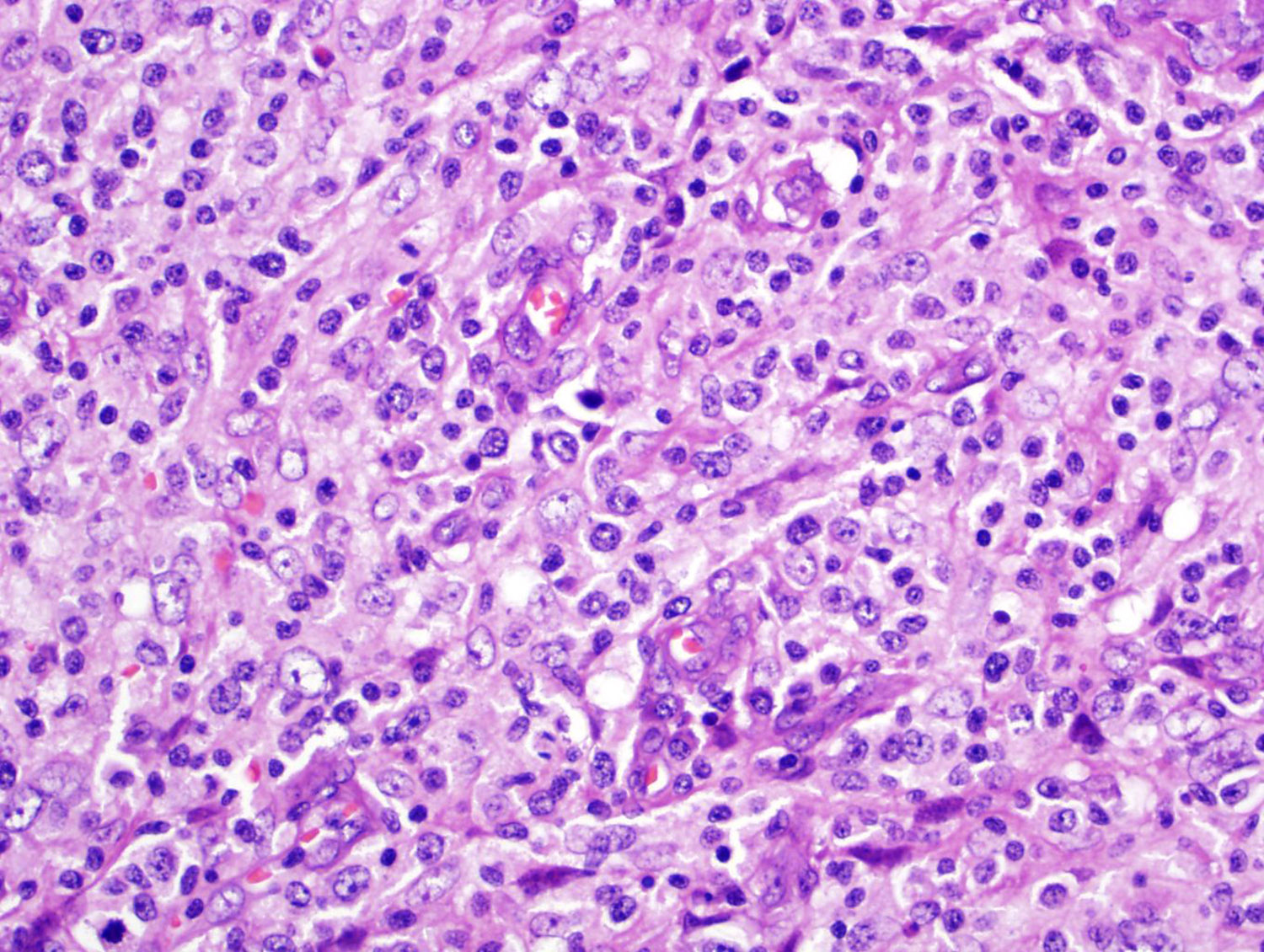
Microscopic (histologic) description
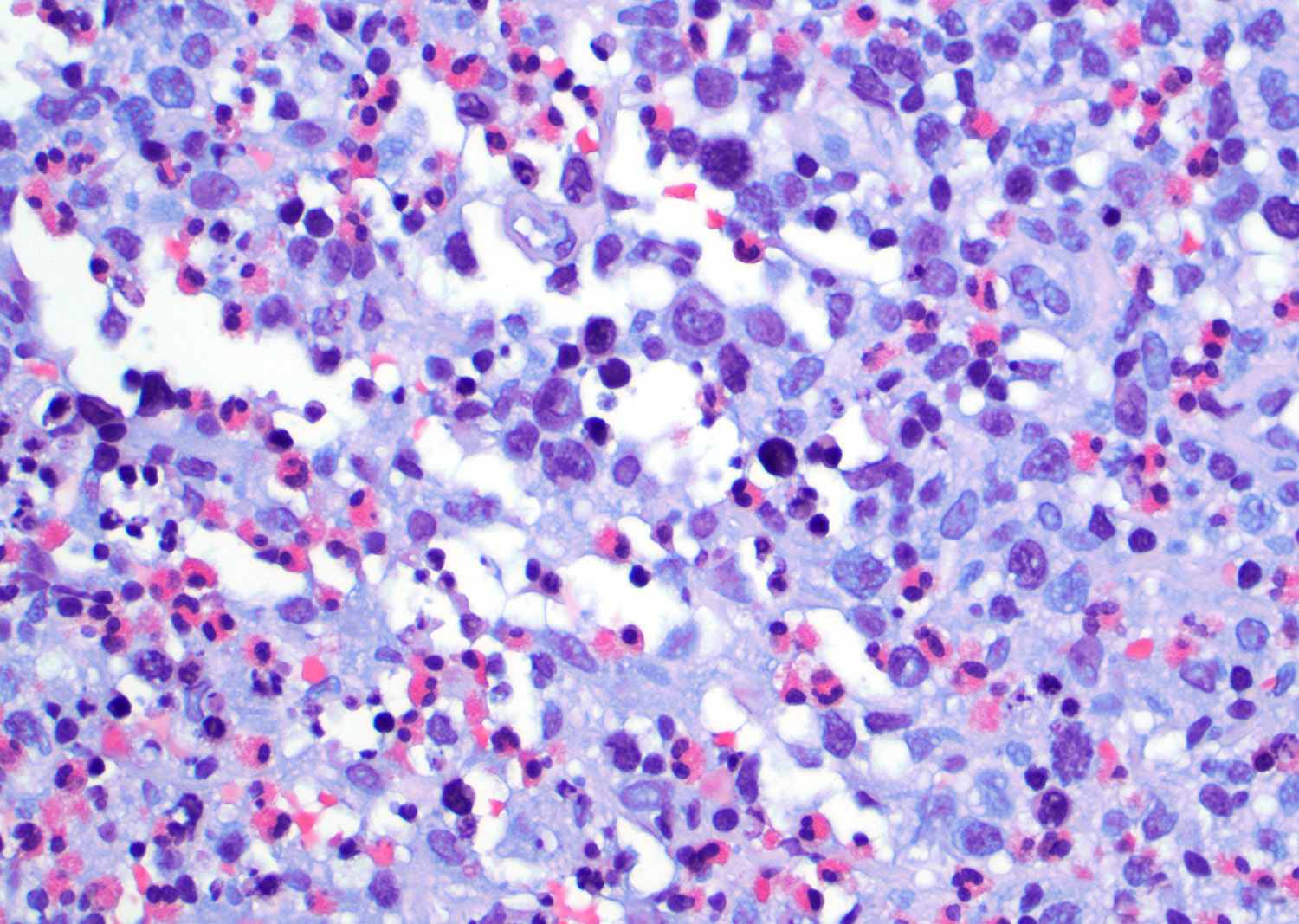
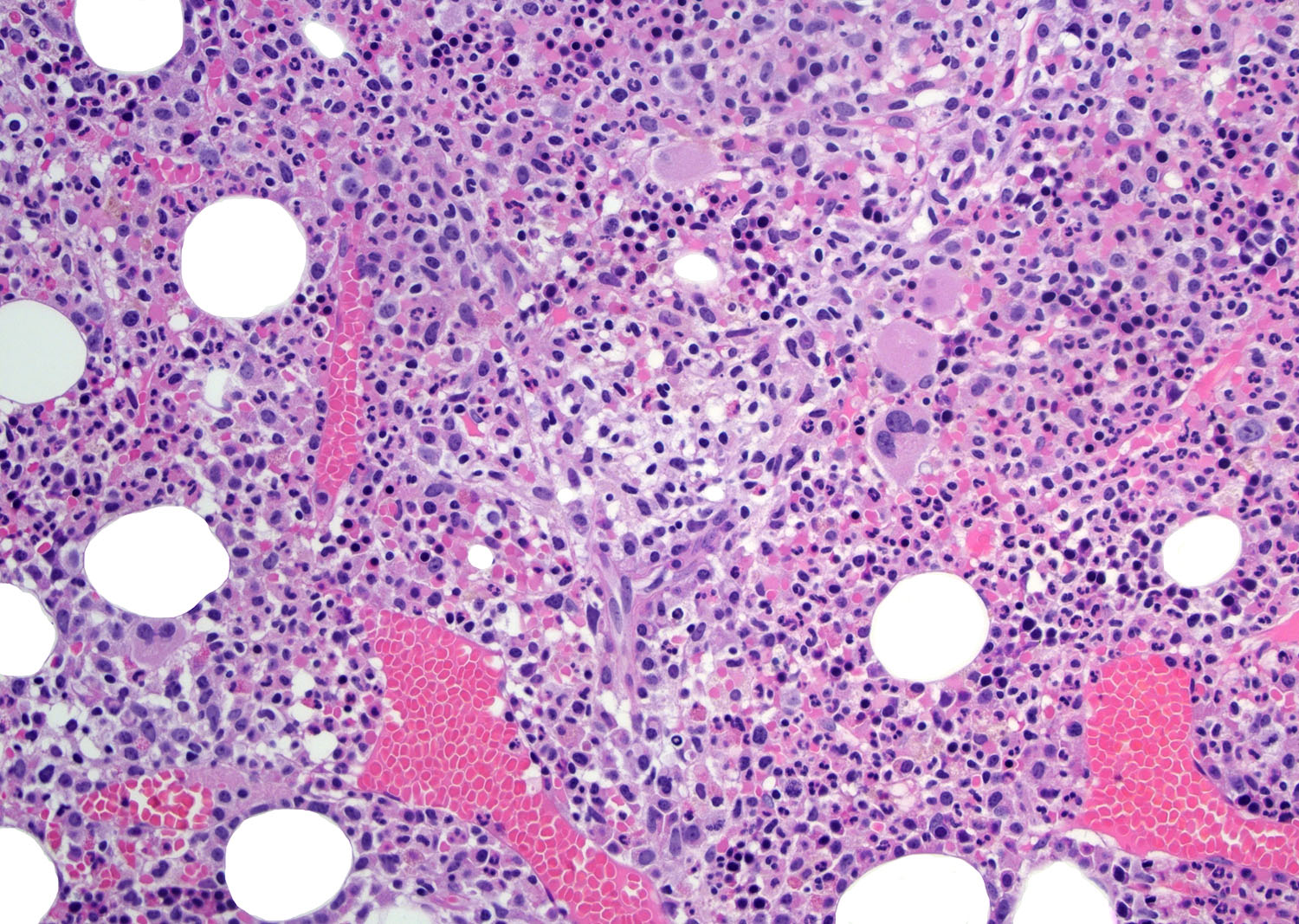
- Lymph node (Leuk Lymphoma 2016;57:2804, Blood 2017;129:1095, Histopathology 2014;64:171, Hum Pathol 2010;41:79, Mod Pathol 2009;22:753, Am J Surg Pathol 2007;31:1077, Leukemia 2020;34:2592)
- Partial or complete architecture effacement
- Pattern I: architecture partially preserved and hyperplastic follicles with tingible body macrophages and indistinct mantle zones
- Pattern II: architecture mostly preserved with residual follicles
- Pattern III: architecture completely effaced without residual follicles
- AITL cells are the minority population and are located adjacent to high endothelial venules (HEV) or around follicles
- Small to intermediate size, clear cytoplasm and minimal atypia
- Clear cytoplasm in ~30% of cases
- Small to intermediate size, clear cytoplasm and minimal atypia
- Polymorphous inflammatory background composed of reactive lymphocytes, histiocytes, eosinophils, plasma cells, reactive B cells, Reed-Sternberg-like cells, immunoblasts and follicular dendritic cells
- Partial or complete architecture effacement
- Peripheral blood (Hum Pathol 2010;41:79, Leukemia 2006;20:296, Medicine (Baltimore) 2007;86:282)
- Limited evaluation
- Lymphopenia
- Cases with pronounced involvement usually show polymorphic lymphoid population composed of few atypical cells, lymphoplasmacytic, immunoblasts, granular lymphocytes and plasma cells; neoplastic cells are small to large sized lymphocytes with regular or slightly indented nuclei, moderated condensed chromatin, small or indistinct nucleoli and abundant basophilic cytoplasm
- Cases with hypergammaglobulinemia may show rouleaux formation
- Bone marrow (Hum Pathol 2010;41:79, Am J Clin Pathol 2007;128:854, Leukemia 2006;20:296, Medicine (Baltimore) 2007;86:282)
- Bone marrow aspirates are not optimal for diagnosis: very few or absent atypical lymphocytes
- Usually multifocal and poorly defined nodular pattern in core biopsies
- Rare cases of paratrabecular pattern
- Minority of cases present with HEV, stromal edema or patent sinusoids
- Heterogeneous cellular background
- Hemophagocytic syndrome is rare
- Reticulin stain is usually disrupted in lymphoid aggregates
- Skin (Medicine (Baltimore) 2007;86:282, Am J Surg Pathol 2007;31:1068)
- Broad histological presentation
- Histologic picture of vasculitis is more common
- Band-like subepidermal, perivascular, periadnexial or diffuse infiltrate
- Epidermotropism not present
- Broad histological presentation
Microscopic (histologic) images
Contributed by Roberto N. Miranda, M.D.
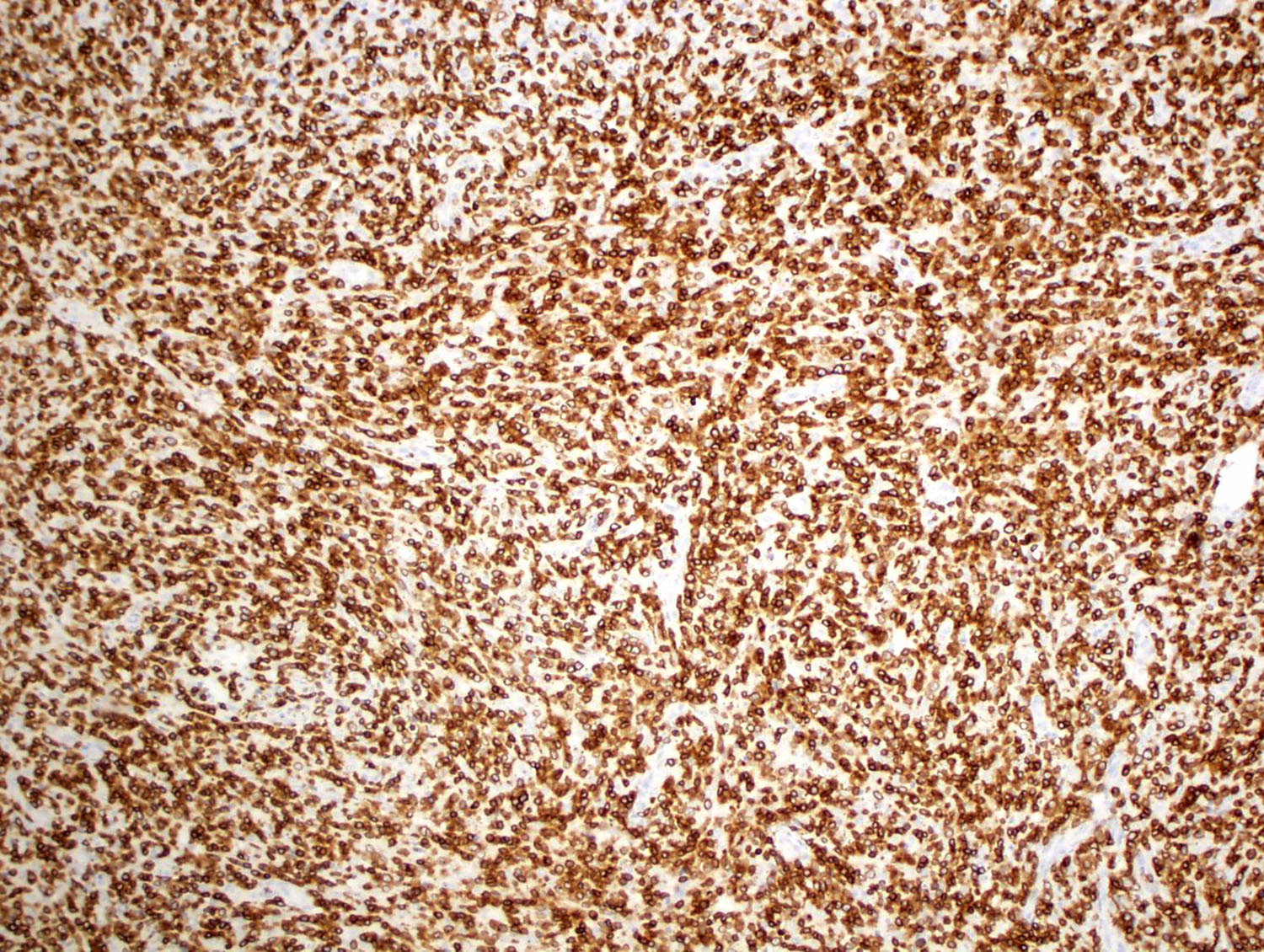
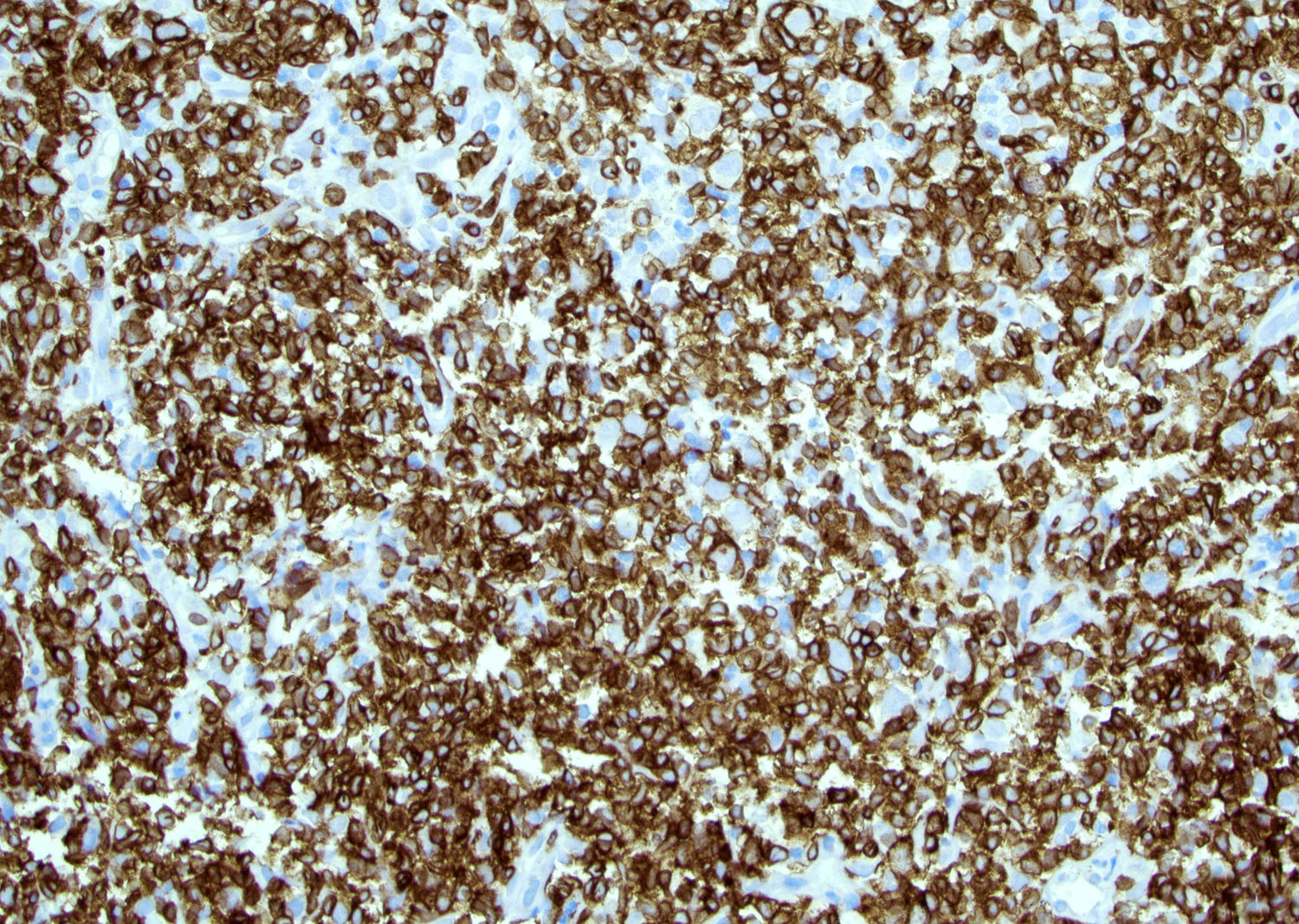
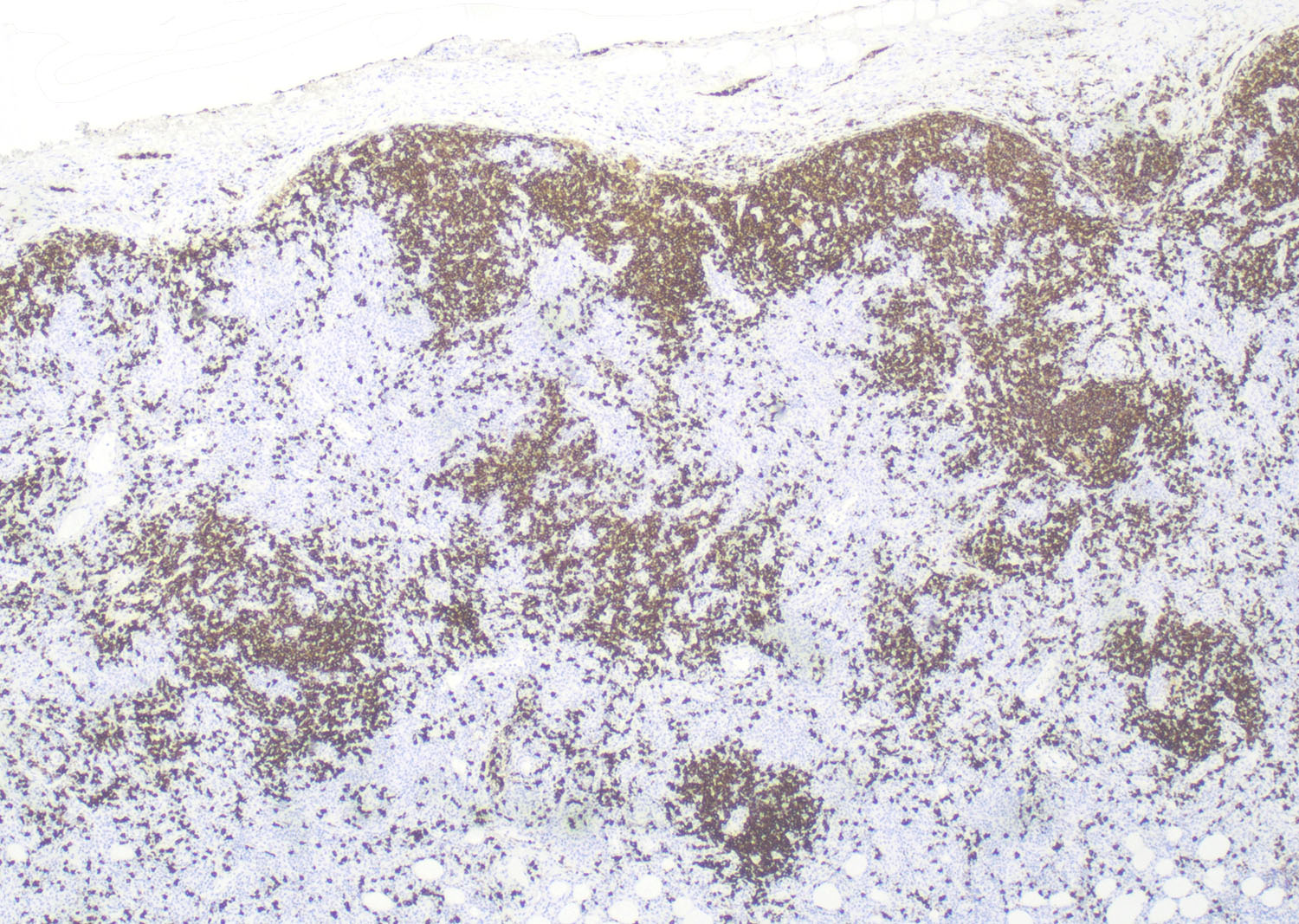
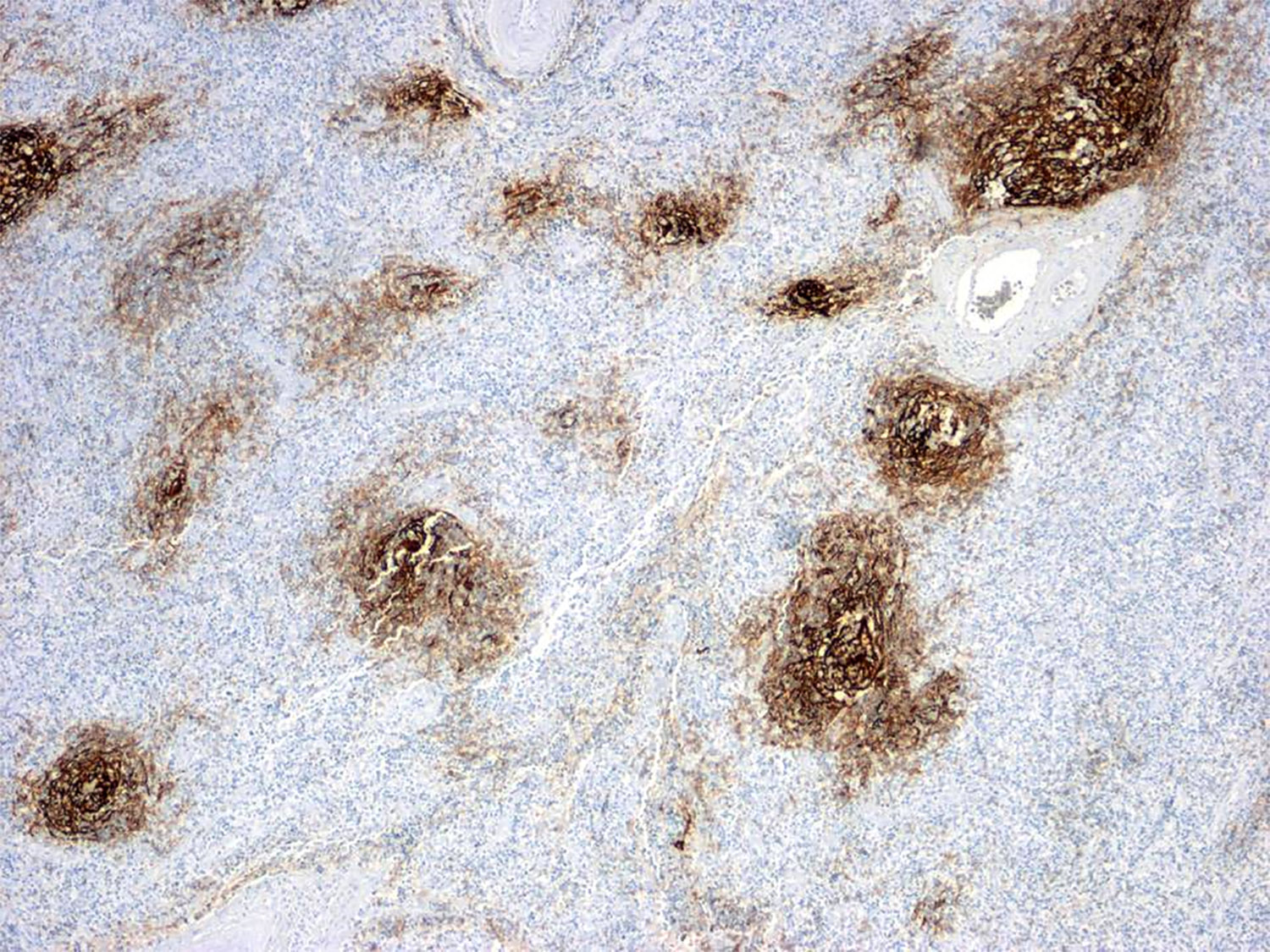
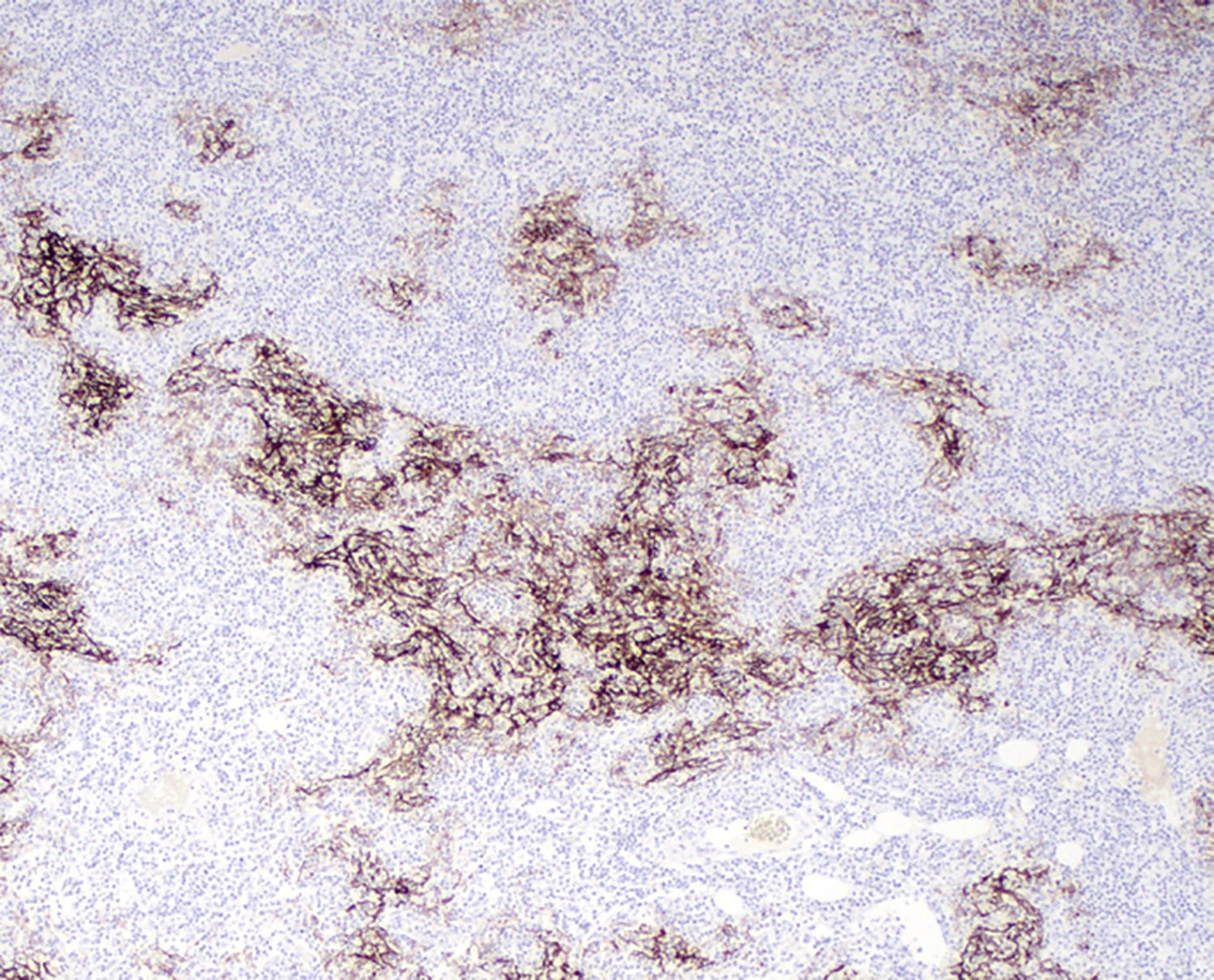
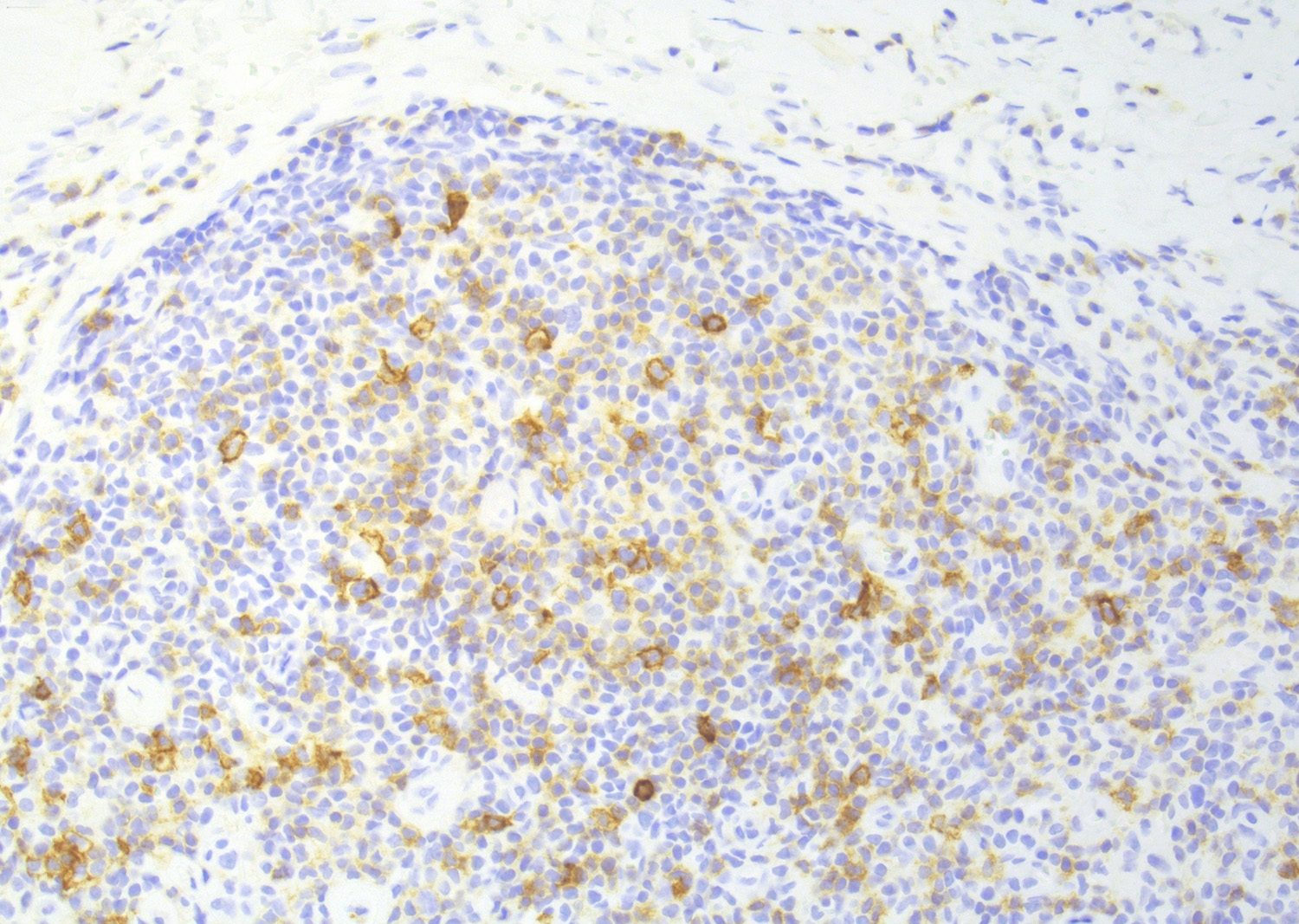
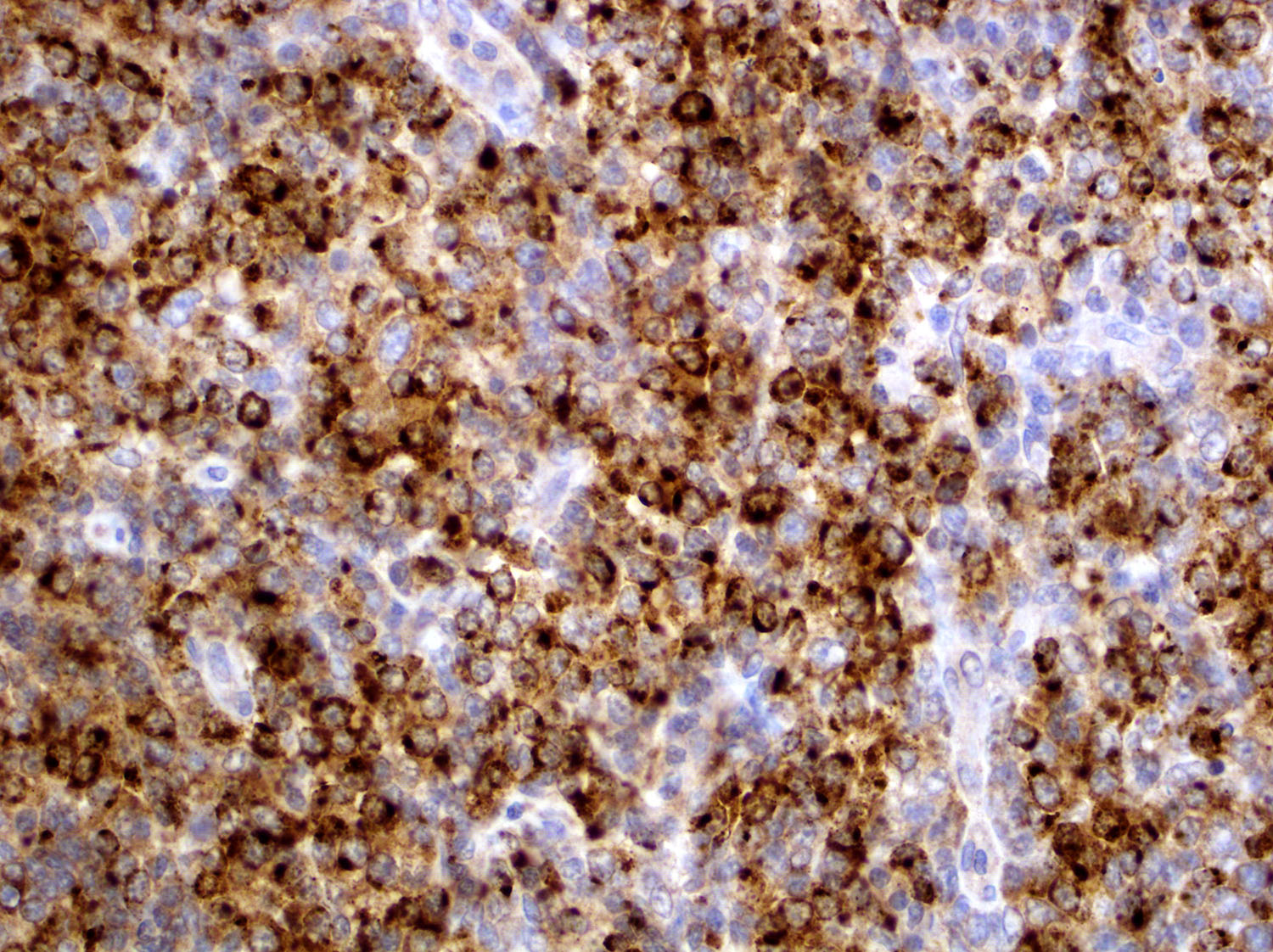
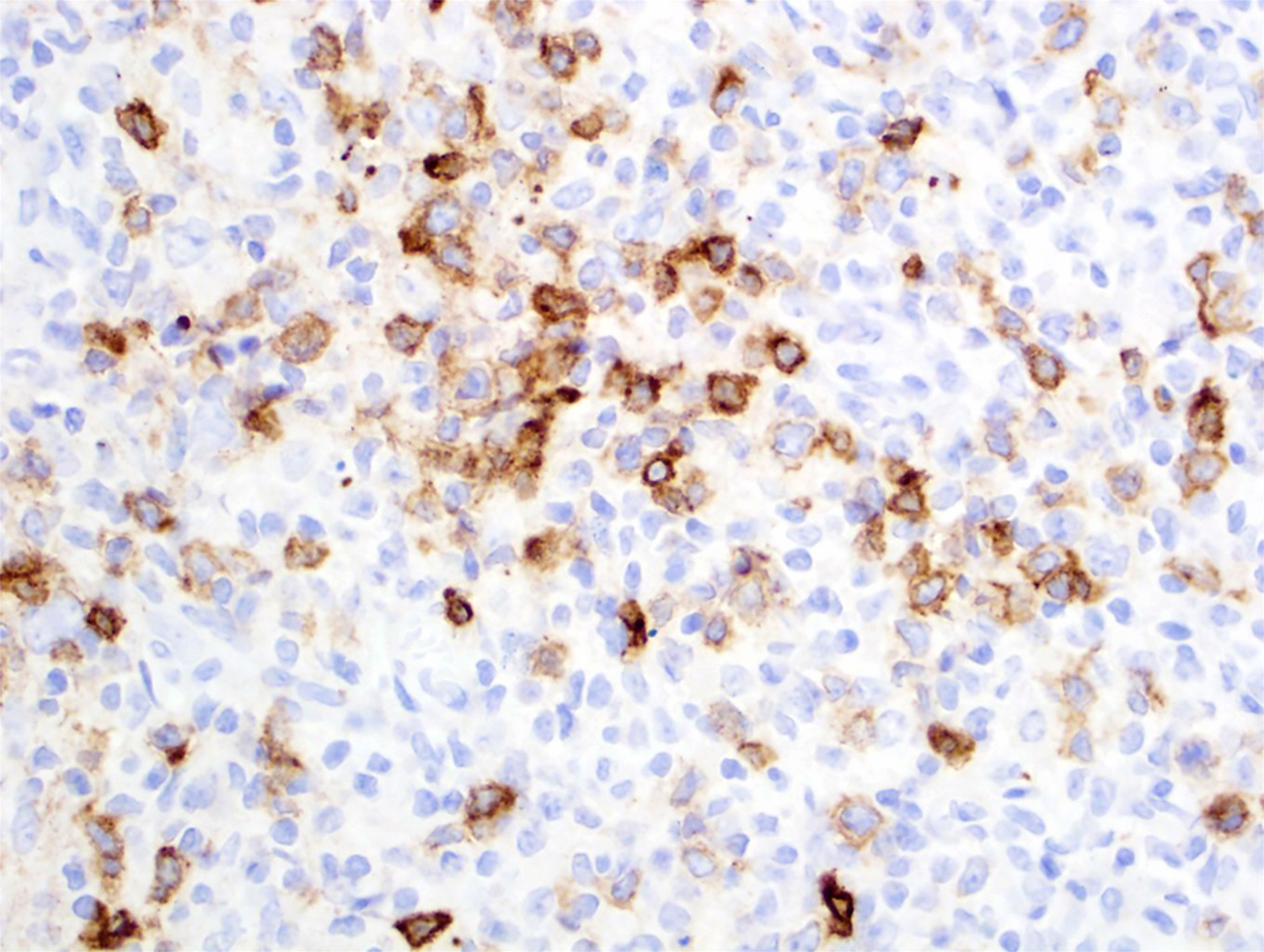
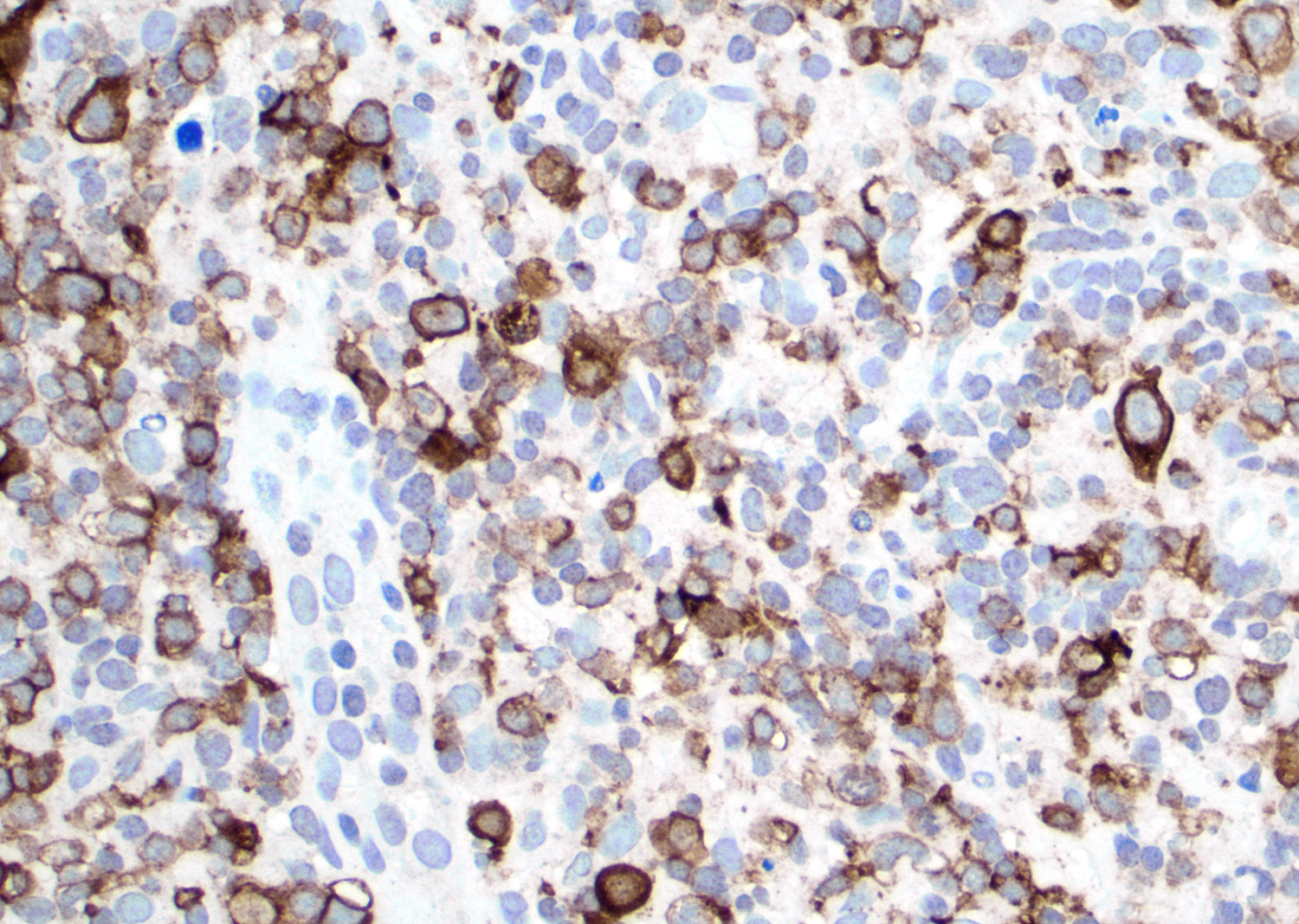
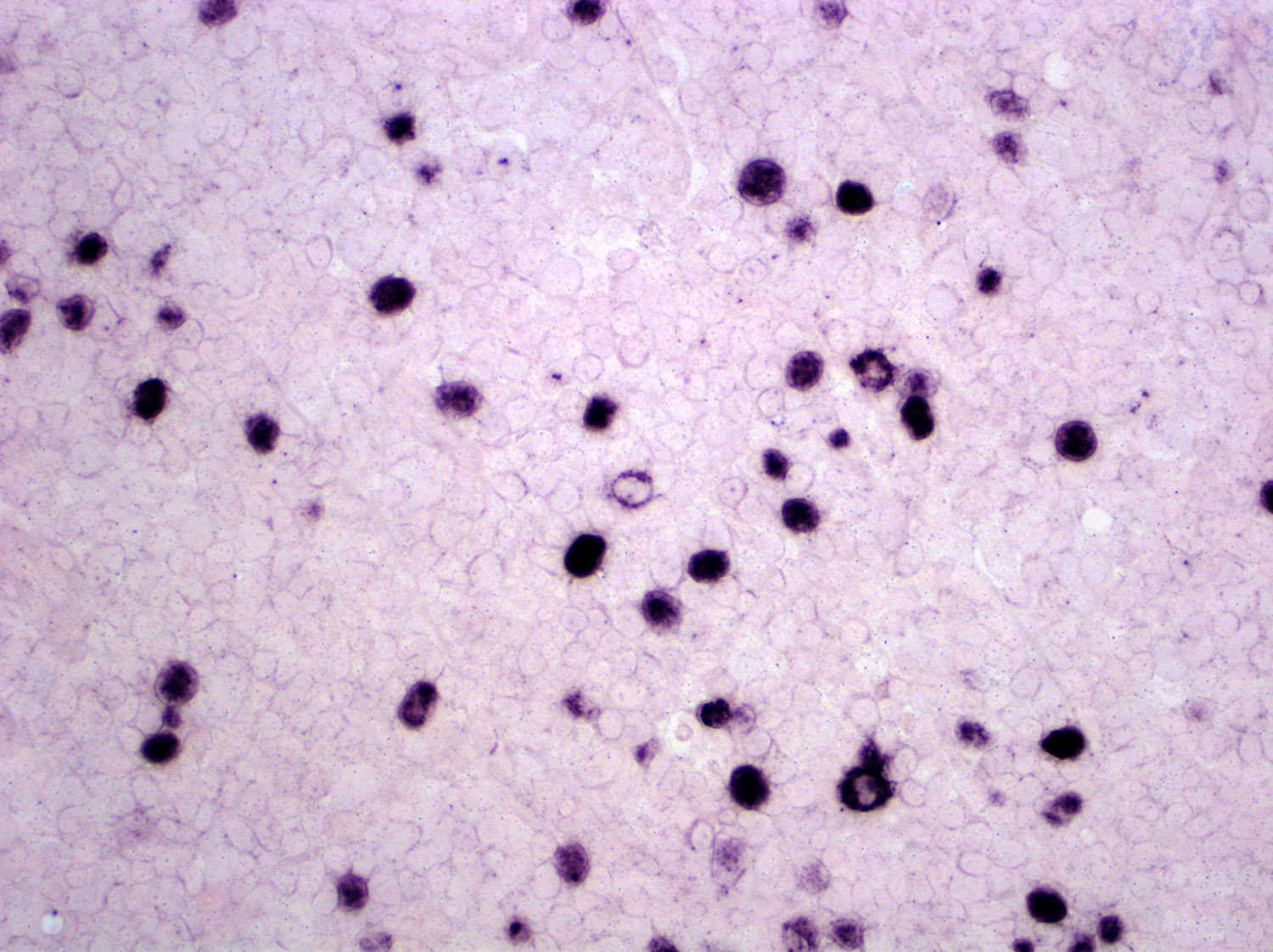
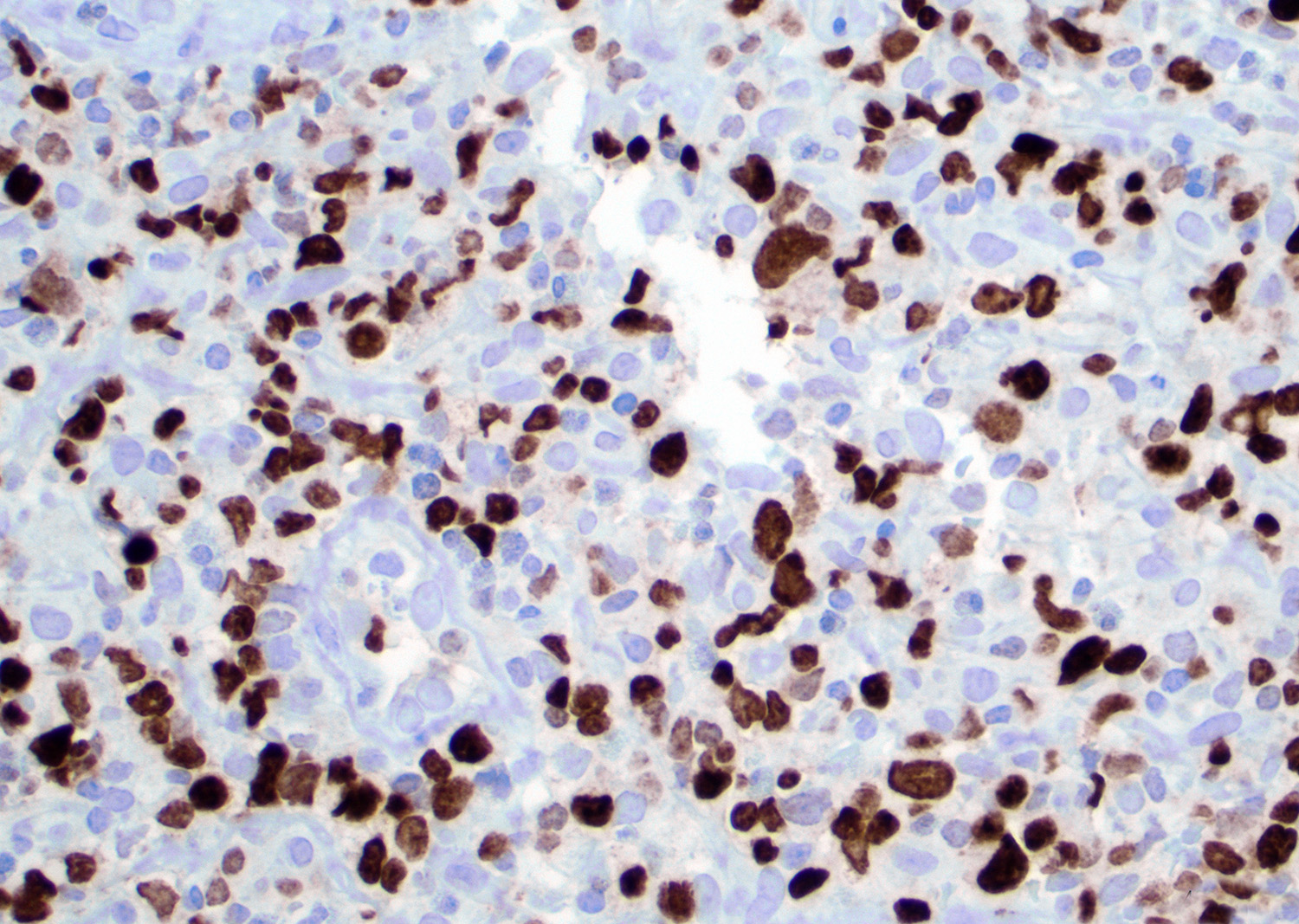
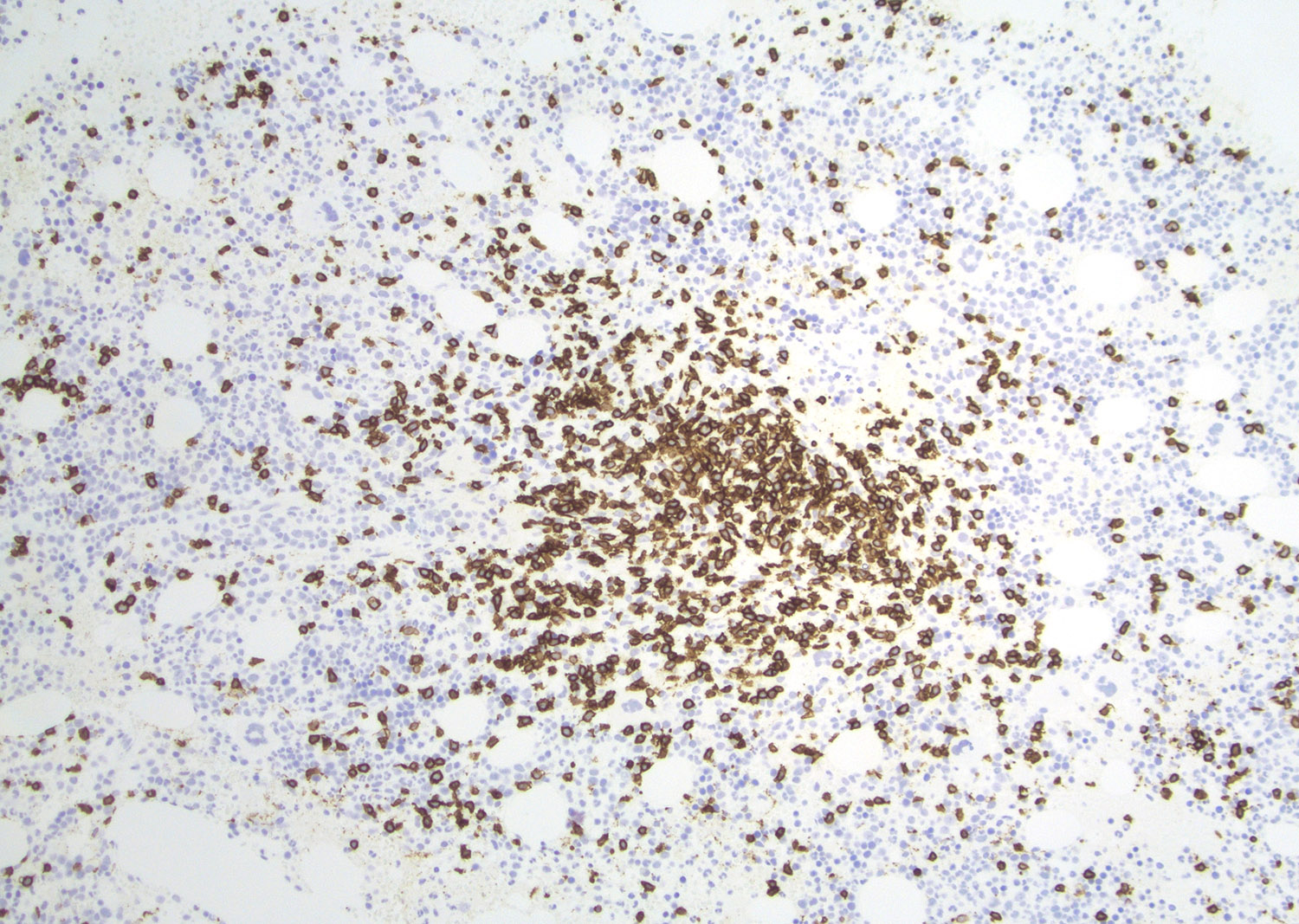
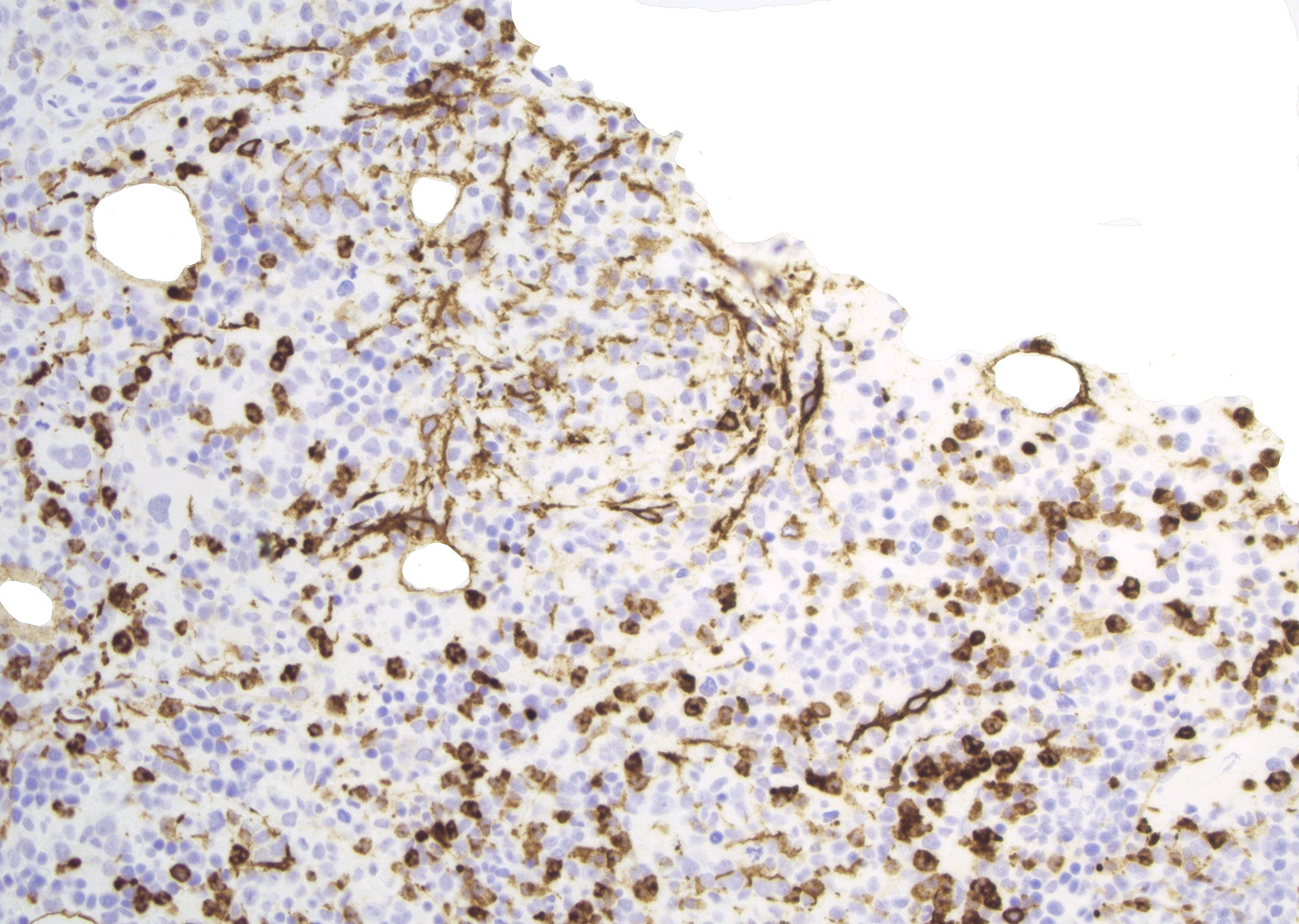
Positive stains
- T cells: εCD3, CD4; CD5 and CD7 (Blood 2017;129:1095, Am J Surg Pathol 2016;40:335, Leukemia 2020;34:2592)
- Follicular dendritic cells: CD21, CD23, CD35 highlight expanded and distorted follicular dendritic cell meshworks (Histopathology 2014;64:171)
- CD21
- Reliable marker to identify the follicular dendritic cells when compared to CD23
- CD35 (Am J Clin Pathol 2007;128:854)
- CD21
- TFH markers (Blood 2017;129:1095, Am J Surg Pathol 2016;40:335, Histopathology 2014;64:171, Nat Genet 2014;46:371, Hum Pathol 2010;41:79, Mod Pathol 2009;22:753, Am J Clin Pathol 2007;128:854, Am J Surg Pathol 2007;31:1077, Br J Haematol 2007;138:733, Leukemia 2006;20:296, Leukemia 2022;36:165, Blood 2008;111:4463, Am J Surg Pathol 2007;31:1068, Haematologica 2007;92:1059, Am J Surg Pathol 2004;28:54)
- CXCL13 and CD10
- Both have good specificity and low sensitivity
- CXCL13 is more specific than CD10
- Limited utility in cases with bone marrow involvement but useful in other extranodal sites
- Cases with skin involvement show more CXCL13 positivity compared with CD10
- CXCL13 has a cytoplasmic with dot-like reinforcement pattern
- PD-1 (CD279) and ICOS (CD278)
- Good sensitivity but less specific
- PD-1 is highly dependent on fixation
- BCL6, CD200, CXCR5, cMAF, SAP, TIGIT, CD27
- CXCL13 and CD10
- Epstein-Barr virus encoded small RNAs (EBER) in situ hybridization (Blood 2017;129:1095, Am J Clin Pathol 2007;128:854, Br J Haematol 2007;138:733, Leukemia 2020;34:2592, Medicine (Baltimore) 2007;86:282, Blood 2008;111:4463, Am J Clin Pathol 2002;117:368)
- ~60 - 90% cases
- Usually positive on scattered B cells and immunoblasts
- CD30 (Blood 2017;129:1095)
- Present in ~20% of cases
Negative stains
- Aberrant loss of T cell markers (Blood 2017;129:1095, Mod Pathol 2009;22:753, Leukemia 2022;36:165, Blood 2008;111:4463)
- B cell markers (CD20, PAX5, CD79a) (Blood 2017;129:1095, Leukemia 2022;36:165)
- May be increased in the microenvironment and usually loss of CD73 as compared with B cells in normal tissues
Flow cytometry description
- Multiparameter flow cytometry is a reliable tool for supporting the diagnosis of AITL in tissues and fluids (Leuk Lymphoma 2016;57:2804, Hematol Oncol 2014;32:16, Am J Clin Pathol 2007;128:854, Leukemia 2006;20:296)
- Positive for CD2, CD4, CD5, CD10, CD42 and CD45
- Negative for sCD3, CD7 (complete or partial), CD8, CD19, CD20, CD38, CD56, CD57, TCRαβ (partial or complete loss), TCRγδ
- CD10 expression is highly sensitive and is a less specific marker for distinguishing from other forms of peripheral T cell lymphoma
- Clonal B cells may be identified in the background of the neoplastic T cells
Molecular / cytogenetics description
- Karyotypic abnormalities are present in 90% of the cases (Blood 2017;129:1095, Medicine (Baltimore) 2007;86:282, Genes Chromosomes Cancer 2007;46:37)
- Trisomy of chromosome 3, 5 and 19
- Gain of chromosome X
- Comparative genomic hybridization (CGH) (Genes Chromosomes Cancer 2007;46:37)
- Gain of 22q, 19 and 11p11-q14(11q13)
- Loss of 13q
- Variable presence of T cell receptor (TCR) gene rearrangement but usually present (Mod Pathol 2009;22:753, Am J Clin Pathol 2007;128:854, Am J Surg Pathol 2007;31:1077, Br J Haematol 2007;138:733, Leukemia 2006;20:296, Medicine (Baltimore) 2007;86:282, Am J Clin Pathol 2002;117:368)
- IGH gene rearrangement is present in cases (~30%) (Am J Clin Pathol 2007;128:854, Br J Haematol 2007;138:733, Leukemia 2006;20:296, Medicine (Baltimore) 2007;86:282, Am J Clin Pathol 2002;117:368)
- ITK / SYK translocation is rare (Am J Surg Pathol 2013;37:1456)
- Unique mutational profile (Blood 2017;129:1095, Am J Surg Pathol 2016;40:335, Blood 2014;123:1293, Nat Genet 2014;46:371, Blood 2015;126:1741, Leukemia 2020;34:2592, Blood 2014;123:2915, Haematologica 2015;100:e505, Blood 2012;120:1466, Blood 2014;123:1293, Nat Genet 2014;46:166)
- Gene signature
- Vascular endothelial cell migration and angiogenic
- Associated with poor prognosis: p53 induced, cytotoxic and monocytic / dendritic signature
- Associated with good prognosis: B cell (germinal center type)
- Loss of function
- ARID1A, CCND3, EP300, FAS, CD58, PRDM1, TNFSF9 and ETV6
- TET2
- ~40 - 80% cases, usually 2 or more mutations
- Majority of the mutations are either frameshift, splice site or premature stop
- May be detected in B cell population of the microenvironment
- Associated with advanced stage, thrombocytopenia, high International Prognostic Index (IPI) and shorter progression free survival
- DNMT3A
- ~20 - 40%
- Associated with older age
- Usually associated with TET2 mutation
- Not accumulated in the methyltransferase domain
- May be detected in B cell population of the microenvironment
- IDH2-R172
- ~20 - 30%
- Unique pattern
- Induces DNA hypermethylation of gene promoters
- RHOA
- p.Gly17Val is a driver mutation identified in ~70% of AITL cases
- Specific mutation for T cell lymphomas
- Substitution of glycine with valine causes activity loss of GTPase
- Median variant allele frequencies (VAF): 14%
- Correlated with B symptoms or splenomegaly and expression of > 2 TFH markers
- No relationship with outcomes
- p.Gly17Val is a driver mutation identified in ~70% of AITL cases
- STAT3 (codons 614 and 661) and JAK2 (V617F and G571S)
- CD28 T195P
- Plays a role in tumorigenesis and tumor progression
- May cause a downstream in T cell receptor signaling
- NOTCH1
- When present, it is detected only in the B cell component
- Gene signature
Sample pathology report
- Axillary lymph node, excisional biopsy:
- Angioimmunoblastic T cell lymphoma (see comment)
- Comment: According to clinical notes, patient is a 65 year old man with generalized lymphadenopathy, B symptoms, splenomegaly, anemia and thrombocytopenia. The peripheral blood shows anemia and thrombocytopenia. H&E sections show a complete effacement of the lymph node architecture by a diffuse and polymorphic infiltrate. Paracortical areas show increased vascularity with an arborizing pattern and the endothelial cells are prominent. The polymorphic infiltrate is composed of small to intermediate size atypical cells with slight nuclear irregular contours admixed with plasma cells, Reed-Sternberg-like cells, neutrophils and reactive small lymphocytes.
- Immunohistochemical studies show a neoplastic population positive for CD2, CD3, CD4, CD5, CXCL13, CD10 and PD-1. The aberrant cells are negative for CD7, CD8, CD20, CD30, CD138 and ALK1. Kappa and lambda highlight polytypic plasma cells. The CD21 marker highlights follicular dendritic cell meshworks, which appear expanded around clusters of vessels. Epstein-Barr virus encoded small RNAs (EBER) in situ hybridization was positive in scattered large cells. Concurrent flow cytometry immunophenotype showed an aberrant T cell population positive for CD2, CD4, CD5 and CD10. The aberrant cells are negative for sCD3, CD7, CD8, CD19, CD20, CD56, TCRαβ (partial loss) and TCRγδ. A next generation sequencing panel demonstrated TET2, DNMT3, RHOA and IDH2 mutations. Polymerase chain reaction for Ig heavy chain (IGH) and T cell receptor gamma (TRG) were germline and T cell receptor beta (TRB) was monoclonal.
Differential diagnosis
- Reactive lymphoid hyperplasia (RLH) (Histopathology 2014;64:171, Am J Clin Pathol 2021;156:1):
- AITL pattern I shows morphological overlap with reactive lymphoid hyperplasia; however, interfollicular expansion is prominent
- Although monoclonal T cell populations support a diagnosis of T cell lymphoma, reactive processes can also show monoclonal T cells and may lead to false positive diagnoses
- Absence of both follicular dendritic cell expansion and high endothelial venule proliferation in paracortex favors reactive lymphoid hyperplasia
- PD-1 shows strong positivity in reactive germinal centers of reactive lymphoid hyperplasia, while PD-1 is positive in interfollicular lymphocytes of AITL
- Classic Hodgkin lymphoma, mixed cellularity type (Histopathology 2014;64:171, Am J Clin Pathol 2021;156:1):
- Absence of atypical CD10+ TFH cells, hyperplastic high endothelial venules and follicular dendritic cells
- Reed-Sternberg cells are positive for CD30 with weak coexpression of PAX5 and negative or variable CD20 in classic Hodgkin lymphoma
- No aberrant T cell immunophenotype or monoclonal T cell rearrangement
- T cell / histiocyte rich large B cell lymphoma (Am J Clin Pathol 2021;156:1):
- Large B cells in a background of normal T cells
- Absence of follicular dendritic cell proliferation and high endothelial venules
- Usually shows IGH gene rearrangement
- Follicular peripheral T cell lymphoma (F-PTCL) (Haematologica 2017;102:e148):
- Pronounced follicular pattern
- TFH phenotype
- Absence of extrafollicular dendritic cells and high endothelial venules
- Distinct gene expression profile
- Nodal peripheral T cell lymphoma with T follicular helper phenotype (Haematologica 2017;102:e148):
- Similar gene signature (mutations of TET2, DNMT3A and RHOA)
- Diffuse and monotonous lymphoid infiltrate
- Absence of follicular dendritic cell meshwork and high endothelial venules
- Peripheral T cell lymphoma, not otherwise specified (Histopathology 2014;64:171):
- Drug reaction with eosinophilia and systemic symptoms (DRESS syndrome) (Case Rep Dermatol 2017;9:74):
- Patients may present with B symptoms, effusion and lymphadenopathy
- Histological overlap
- Presence of high endothelial venules
- Monoclonal T cell rearrangement
- Clear cells absent
- Normal immunophenotype of T cells
- Primary cutaneous CD4+ small / medium T cell lymphoproliferative disorder (Am J Surg Pathol 2020;44:862):
- Provisional entity in current WHO classification
- Localized and solitary skin lesion in head in neck area
- Lymphadenopathy and systemic symptoms usually absent
- TFH phenotype
- EBV+ diffuse large B cell lymphoma, not otherwise specified (Pathology 2020;52:40):
- Both entities may present a polymorphous infiltrate with Reed-Sternberg-like cells and EBV+ large B cells
- No history of immunodeficiency or immunodysregulation
- Absence of follicular dendritic cell proliferation and high endothelial venules
- Activation of NFκB and JAK / STAT pathways
- Kimura disease (Med Pharm Rep 2019;92:195):
- Usually presents as a localized disease (subcutaneous mass of head and neck with cervical lymphadenopathy)
- More common in young women
- Peripheral blood shows eosinophilia and elevated serum immunoglobulin E (IgE)
- Variable hyalinized vessels and increase in paracortical plasma cells and interfollicular eosinophils
- Angiolymphoid hyperplasia with eosinophilia (epithelioid hemangioma) (J Surg Case Rep 2018;2018:rjy145):
- Most common clinical presentation is a single or multiple small papules in head and neck region
- May present with a polymorphous infiltrate
- No evidence of TFH phenotype or T cell receptor (TCR) gene rearrangement
Additional references
Board review style question #1
Board review style answer #1
B. εCD3+ / CD4+ / CD7- / CD8- / CXCL13+ / PD-1+. Angioimmunoblastic T cell lymphoma (AITL) cells are usually positive for εCD3, CD4 and TFH markers (e.g. CXCL13, PD-1, CD10 and ICOS). Loss of CD7 is also observed.
Comment Here
Reference: Angioimmunoblastic T cell lymphoma
Comment Here
Reference: Angioimmunoblastic T cell lymphoma
Board review style question #2
Which of the following is true about angioimmunoblastic T cell lymphoma (AITL)?
- Histologic pattern I is characterized by a complete effacement of the lymph node architecture
- Peripheral blood involvement is common
- The most common clinical presentation is localized disease and type A symptoms
- The most common mutations are TET2, DNMT3A, IDH2 and RHOA
Board review style answer #2
D. The most common mutations in angioimmunoblastic T cell lymphoma (AITL) are TET2, DNMT3A, IDH2 and RHOA. There are 3 histological patterns in the lymph node: pattern I (architecture partially preserved and hyperplastic), pattern II (architecture mostly effaced but residual follicles can be identified) and pattern III (architecture completely effaced). Peripheral blood is involved in a subset of cases. The most common clinical presentation is with advanced stage disease and type B symptoms. The most common mutations are TET2, DNMT3A, IDH2 and RHOA.
Comment Here
Reference: Angioimmunoblastic T cell lymphoma
Comment Here
Reference: Angioimmunoblastic T cell lymphoma