Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Etiology | Pathophysiology | Clinical features | Diagnosis | Laboratory | Radiology description | Staging | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Marques-Piubelli ML, Miranda RN. Enteropathy associated T cell lymphoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lymphomanonBenteropathy.html. Accessed April 1st, 2025.
Definition / general
- Intestinal lymphoma derived from intraepithelial T cells which occurs in patients with celiac disease (Blood 2011;118:148)
Essential features
- Intestinal lymphoma derived from intraepithelial T cells that occurs in patients with celiac disease (Blood 2011;118:148)
- Comprises less than 1% of all non-Hodgkin lymphomas, 10% of all peripheral T cell lymphomas and 10 - 25% of all primary intestinal lymphomas (Blood 2011;118:148, Gut 2003;52:347, Curr Hematol Malig Rep 2016;11:504)
- Small intestine is the most affected (Blood 2011;118:148, Gastroenterology 2005;128:S79, Am J Clin Pathol 2007;127:701, Blood 2012;119:2458)
- Jejunum > ileum / duodenum
- Frequent involvement of mesenteric, para-aortic and iliac lymph nodes
Terminology
- Enteropathy associated T cell lymphoma type I (obsolete)
- Intestinal T cell lymphoma
- Enteropathy type T cell lymphoma (obsolete)
ICD coding
Epidemiology
- Comprises less than 1% of all non-Hodgkin lymphomas, 10% of all peripheral T cell lymphomas and 10 - 25% of all primary intestinal lymphomas (Blood 2011;118:148, Gut 2003;52:347, Curr Hematol Malig Rep 2016;11:504)
- Usually occurs in patients at middle age (sixth to seventh decade) (Blood 2011;118:148, Am J Clin Pathol 2007;127:701, Curr Hematol Malig Rep 2016;11:504)
- Incidence of 0.1 per 100,000 population / year (Scand J Gastroenterol 2008;43:1322, Cancer 2012;118:3786)
- Equal sex distribution but in some series there is female predominance (Blood 2011;118:148, Am J Clin Pathol 2007;127:701, Curr Hematol Malig Rep 2016;11:504)
- Variable geographic distribution and more common in Western countries (Blood 2011;118:148, Hum Pathol 2010;41:1231)
Sites
- Small intestine is the most frequently affected (Blood 2011;118:148, Gastroenterology 2005;128:S79, Am J Clin Pathol 2007;127:701, Blood 2012;119:2458)
- Jejunum > ileum or duodenum
- Frequent involvement of mesenteric, para-aortic and iliac lymph nodes
- Large intestine involvement (isolated or associated with small intestine) is rare (Blood 2011;118:148)
- Less than 10% of the cases affect stomach, lung, liver or spleen (Blood 2011;118:148)
- Bone marrow (BM) involvement is rare (Blood 2011;118:148)
Etiology
- Celiac disease affects ~1% of the world population (Gastroenterology 2005;128:S79, Blood 2012;119:2458, Arch Pathol Lab Med 2013;137:1227, Gastroenterology 2009;136:91)
- 65% of the lymphomas in patients with celiac disease are of T cell lineage
- Increased risk of non-Hodgkin lymphomas
- Gluten free diet has a protective role for lymphoma development
- Delay in the diagnosis of celiac disease may associate with lymphoma progression
Pathophysiology
- Enteropathy associated T cell lymphoma (EATL) has a stronger association with refractory celiac disease (Blood 2011;118:148, Lancet 2000;356:203, Gastroenterology 2005;128:S79, Am J Clin Pathol 2007;127:701, Am J Surg Pathol 2008;32:744, Blood 2012;119:2458, Hum Pathol 2010;41:1231, Curr Hematol Malig Rep 2016;11:504)
- Refractory celiac disease is a form of celiac disease that does not histologically respond to at least 12 months of gluten free diet
- Occurs in 0.6 - 1.5% of patients
- Chronic inflammation leads to an aberrancy in intraepithelial T cell
- Time between the diagnosis of celiac disease and lymphoma is variable and usually ranges from 5 - 10 years
Clinical features
- Aggressive clinical course (Am J Clin Pathol 2007;127:701)
- Gastrointestinal symptoms (Blood 2011;118:148, Lancet 2000;356:203, Gastroenterology 2005;128:S79, Blood 2012;119:2458, Curr Hematol Malig Rep 2016;11:504):
- Abdominal pain
- Diarrhea and vomiting
- Malabsorption
- Complications that may occur in 50% of the cases: bleeding, perforation and obstruction
- Celiac disease can be diagnosed at the same time as the lymphoma diagnosis (Blood 2011;118:148, Lancet 2000;356:203, Gastroenterology 2005;128:S79, Curr Hematol Malig Rep 2016;11:504)
- Fever, fatigue, weight loss, B symptoms, dermatitis herpetiformis and anorexia may be present
- 33% of patients present with infection (Blood 2011;118:148, Curr Hematol Malig Rep 2016;11:504)
- Hepatosplenomegaly and pruritus are rare (Blood 2011;118:148)
Diagnosis
- Diagnosis usually made by surgical resection (Scand J Gastroenterol 2008;43:1322)
Laboratory
- Microcytic anemia and abnormal white blood count (WBC) (Lancet 2000;356:203, Curr Hematol Malig Rep 2016;11:504)
- Antigliadin, antitransglutaminase or antiendomysium IgA or IgG antibodies in peripheral blood (Lancet 2000;356:203)
- HLA genotyping (Lancet 2000;356:203, Virchows Arch 2005;446:416, Gastroenterology 2007;132:1902, Hum Pathol 2010;41:1231, Hum Immunol 1995;43:29)
- HLA-DQ2, HLA-DQ5 or HLA-DQ8
Radiology description
- 18F-Fluoro-deoxy-glucose positron emission tomography (18F-FDG-PET) (Gut 2003;52:347)
- Patients with long standing celiac disease and a standard uptake value > 6 need further investigation for EATL
- Computed tomography (CT) has a higher accuracy than small bowel enema (Blood 2012;119:2458)
- Findings that increase the suspicion for EATL
- Bowel wall thickening
- Mesenteric lymph node cavitation
- Intussusception
- Small sized spleen (< 120 cm3)
- Video capsule endoscopy (Curr Hematol Malig Rep 2016;11:504)
- May determine the extent and the precise location of the lesions
- Useful in cases of intestinal bleeding
- Findings that increase the suspicion for EATL
Staging
- Staging procedures as performed in other lymphomas (Blood 2012;119:2458)
- Bone marrow examination
- CT of thorax, head and neck
- Patients usually present with advanced stage of disease (Blood 2011;118:148)
Prognostic factors
- Poor prognosis (Blood 2011;118:148)
- Median overall survival (OS): 10 months
- 5 year overall survival: 20%
- Prognostic index for peripheral T cell lymphoma (PIT score)
- Predictive of survival
- Parameters: lactate dehydrogenase (LDH), age, bone marrow involvement and performance status
- Factors associated with better overall survival (Dig Liver Dis 2013;45:377):
- Serum albumin level > 21.6 g/L
- Chemotherapy treatment
- Surgical resection
- Factors associated with worse overall survival (Blood 2011;118:148):
- Large tumor mass (> 5 cm)
- Nonambulatory performance status
- Elevated serum lactate dehydrogenase and C reactive protein (CRP)
Case reports
- 54 year old man with concomitant EATL and primary sclerosing cholangitis (Case Rep Oncol Med 2013;2013:838941)
- 62 year old woman with intestinal obstruction as a first manifestation of EATL (J Clin Diagn Res 2014;8:FD10)
- 67 year old man with early colon cancer and EATL (World J Clin Cases 2020;8:5781)
- 73 year old man without evidence of celiac disease with lesion in stomach (Diagn Pathol 2012;7:172)
Treatment
- Surgery (Blood 2012;119:2458)
- Debulking and resection of tumor mass
- Role in complications, mainly in cases of obstruction and perforation
- Standard dose combination chemotherapy (Blood 2011;118:148, Blood 2012;119:2458)
- Less than 50% achieve complete remission
- Common regimes
- Cyclophosphamide, doxorubicin, vincristine, prednisolone (CHOP) or CHOP-like regimen
- Patients who do not respond to first line CHOP usually have poor prognosis
- Bleomycin, doxorubicin, cyclophosphamide, vincristine and prednisone (BACOP)
- Vincristine, doxorubicin, high dose methotrexate and prednisolone (VAMP)
- Prednisolone, doxorubicin, cyclophosphamide, etoposide, mechlorethamine, vincristine and procarzabine (ProMACE-MOPP)
- Cisplatin, cytarabine, etoposide and methylprednisolone (ESHAP)
- Carmustine, etoposide, cytarabine and melphalan (BEAM)
- Cyclophosphamide, doxorubicin, vincristine, prednisolone (CHOP) or CHOP-like regimen
- Combination of high dose chemotherapy followed by consolidation with autologous stem cell transplantation consolidation (Blood 2011;118:148, Blood 2013;121:2529)
- If patient is eligible, may lead to long term remission
- Radiation therapy is controversial (Blood 2012;119:2458)
- Novel treatments (Blood 2012;119:2458)
- Alemtuzumab
- Cladribine
- Romidepsin
Gross description
- Small intestine (Blood 2011;118:148, Gastroenterology 2005;128:S79, Blood 2012;119:2458)
- Multiple ulcerated lesions or 1 large ulcer
- Large mass is less frequent and it is usually transmural
- Enlargement of regional mesenteric lymph nodes
Microscopic (histologic) description
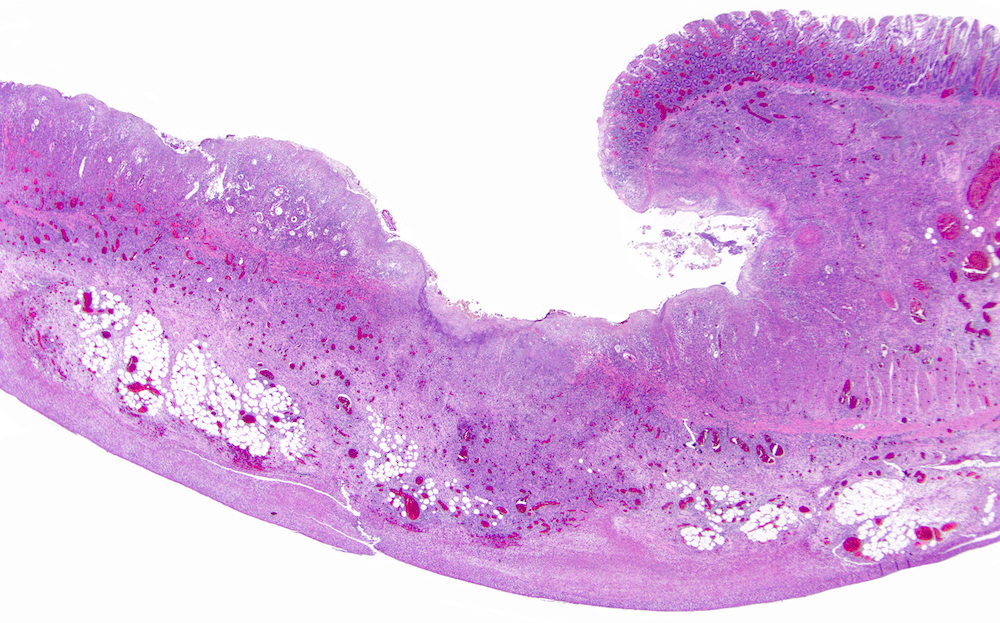
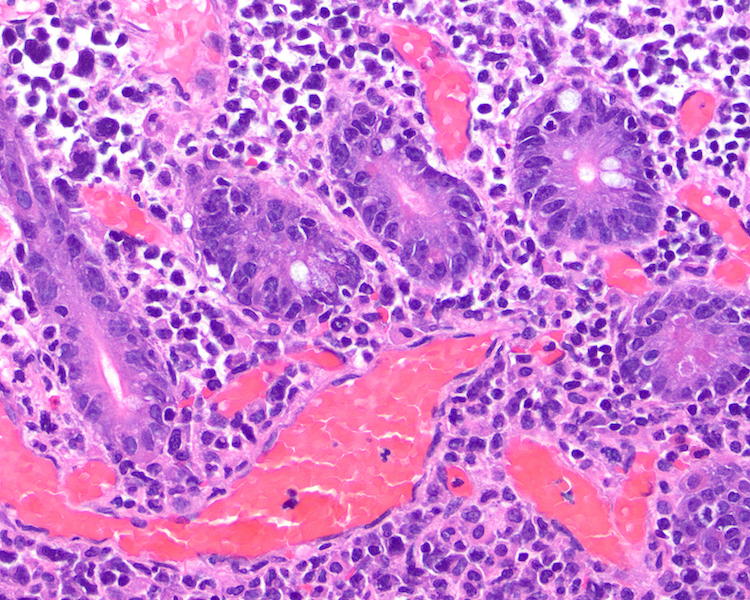
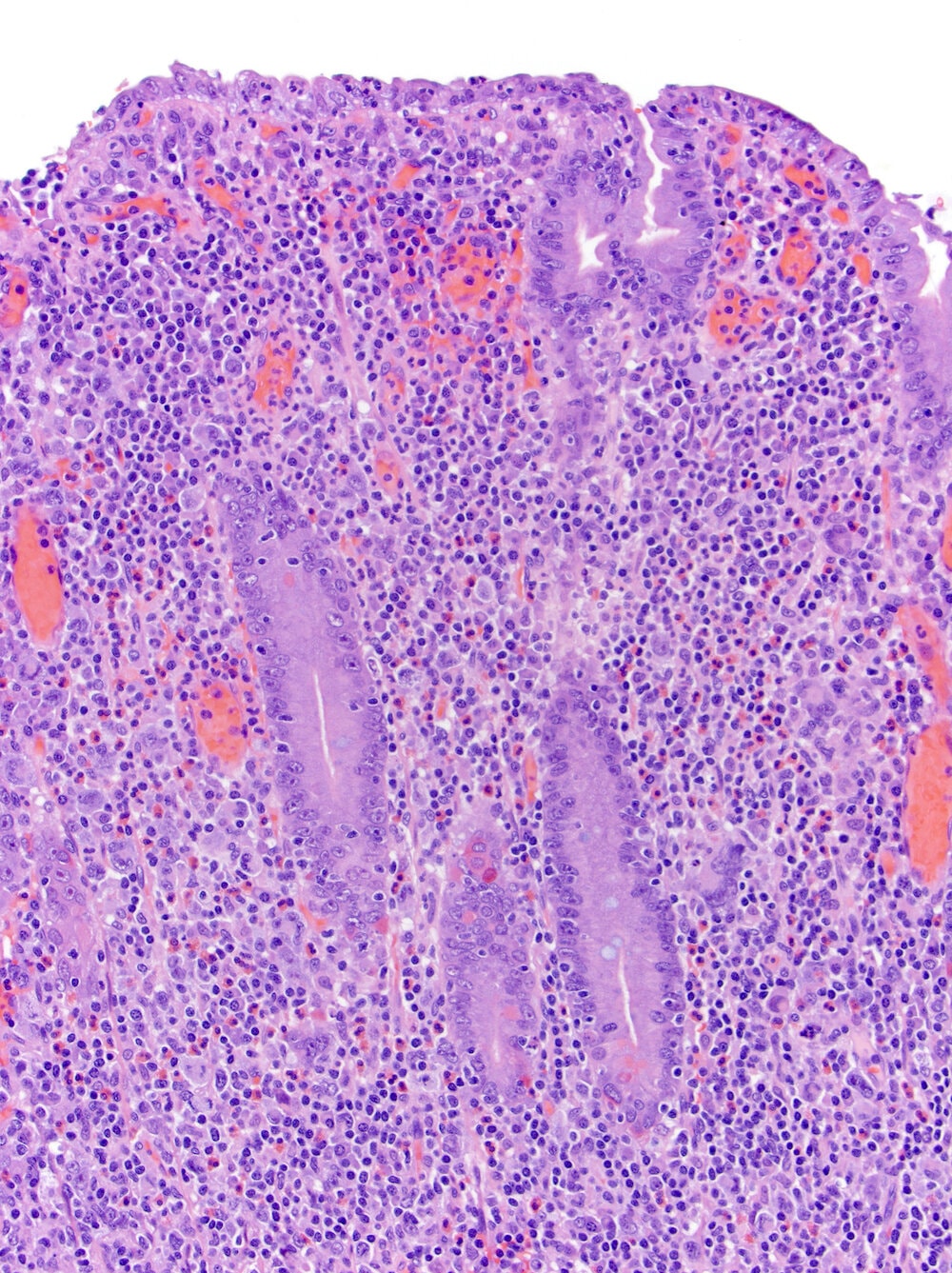
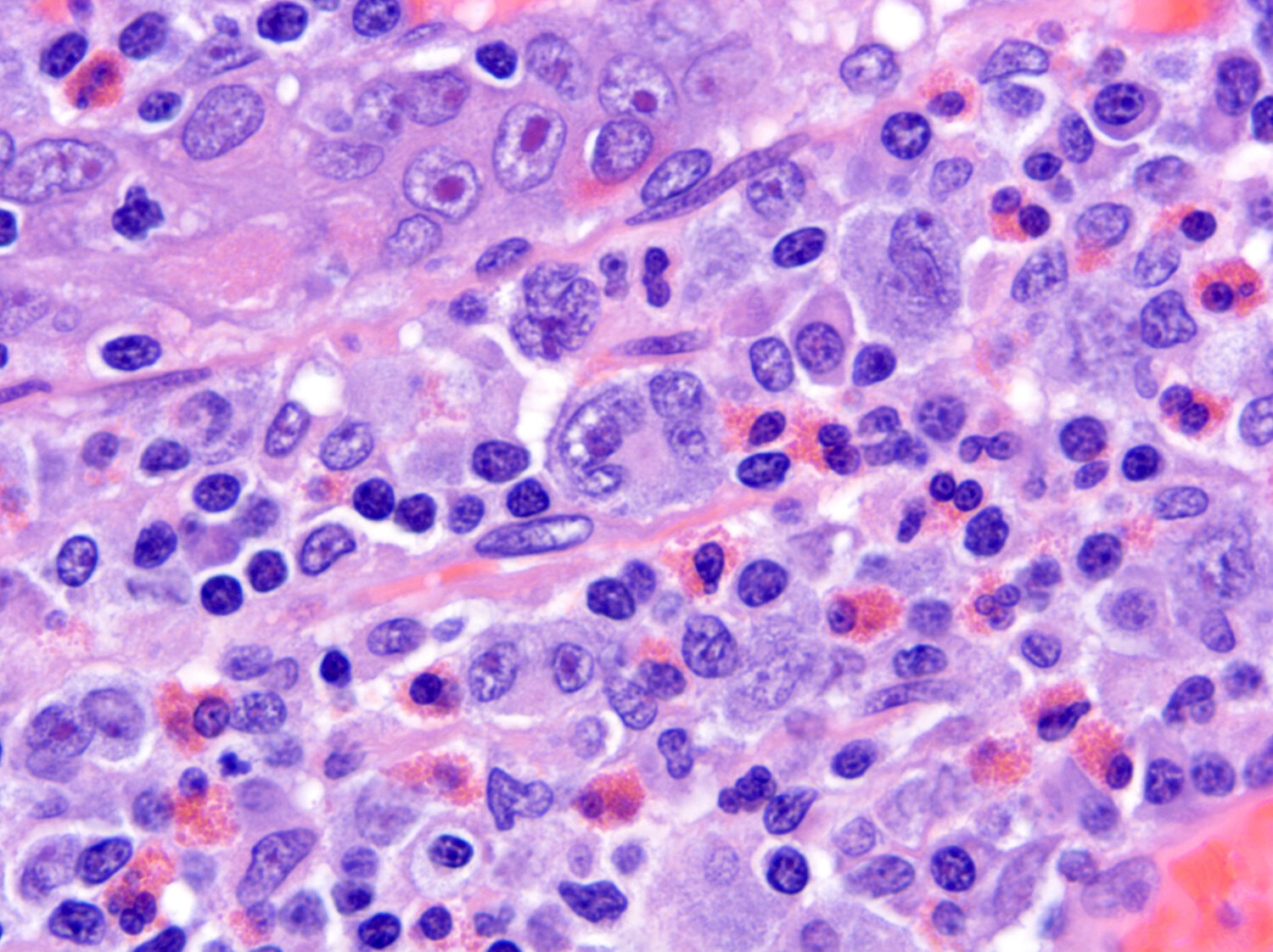
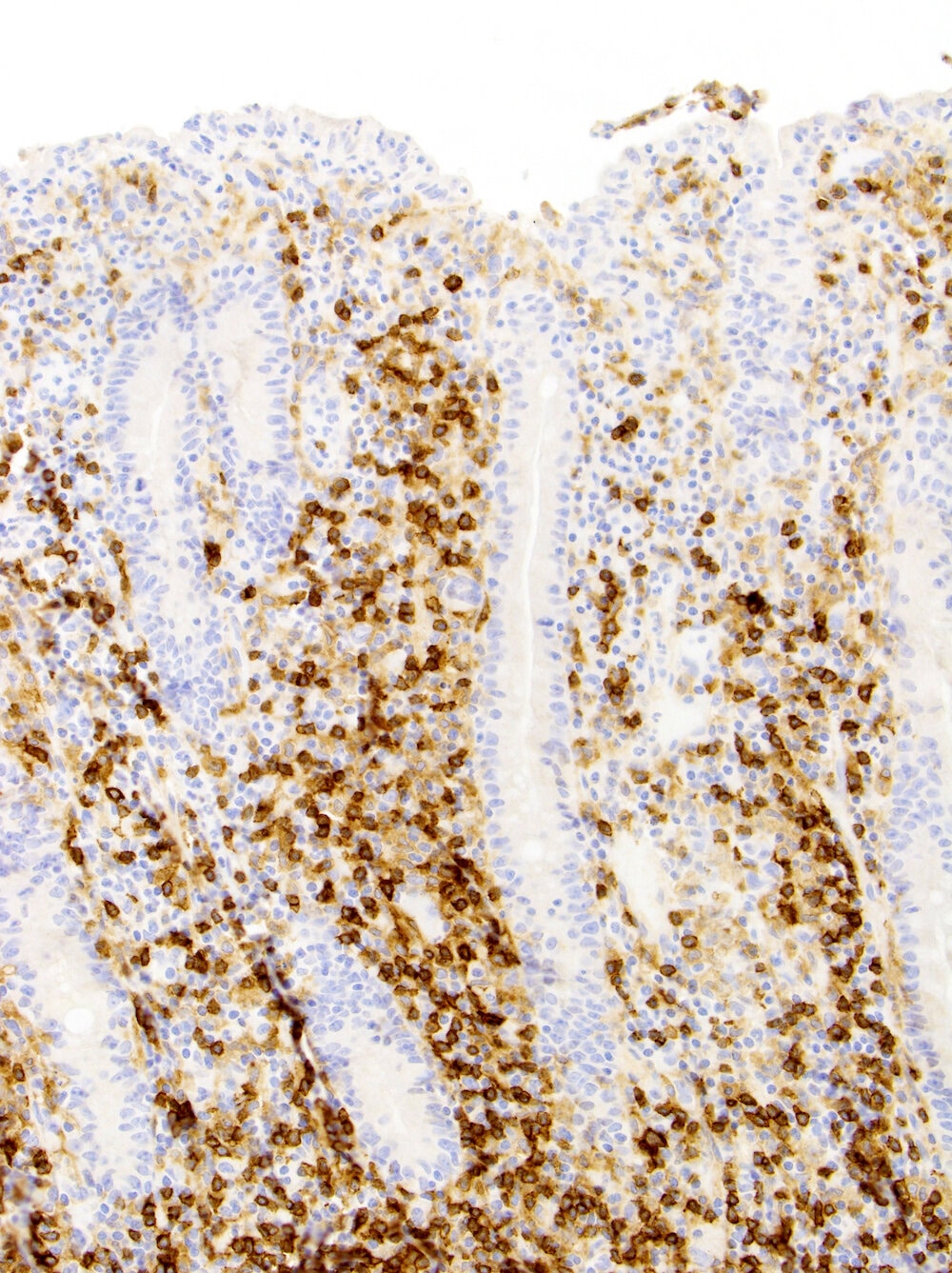
- Intestinal involvement (Blood 2011;118:148, Gastroenterology 2005;128:S79, Am J Surg Pathol 2008;32:744, Hum Pathol 2010;41:1231, Curr Hematol Malig Rep 2016;11:504)
- Ulcerated lesion with diffuse and pleomorphic infiltrate of medium to large cells with angulated nuclei, prominent nucleoli and abundant cytoplasm
- Variable number of anaplastic cells
- Mitotic figures and necrosis are common
- Angiotropism can be noted
- Background with eosinophils, plasma cells, histiocytes and small lymphocytes
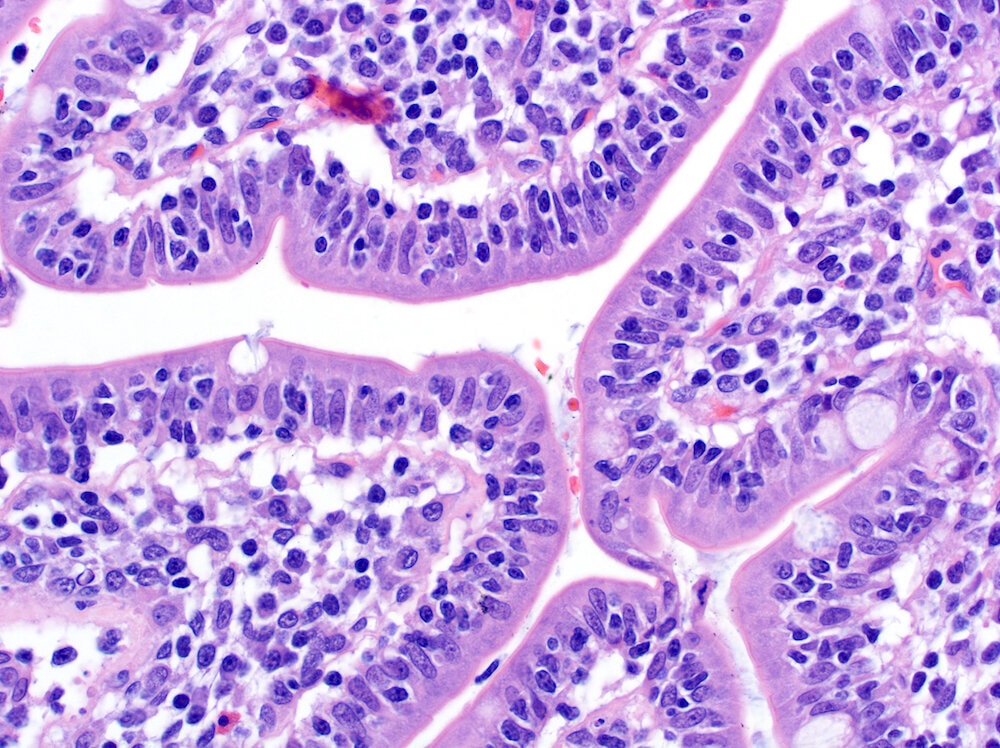
- Features of celiac disease in the adjacent mucosae
- Increased number of intraepithelial lymphocytes (> 30/100 enterocytes)
- Crypt hyperplasia
- Villus atrophy
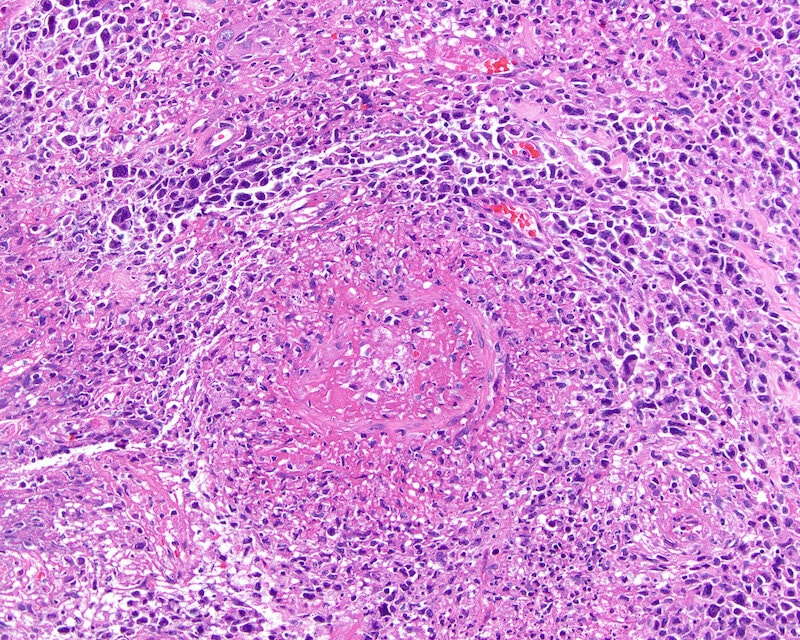
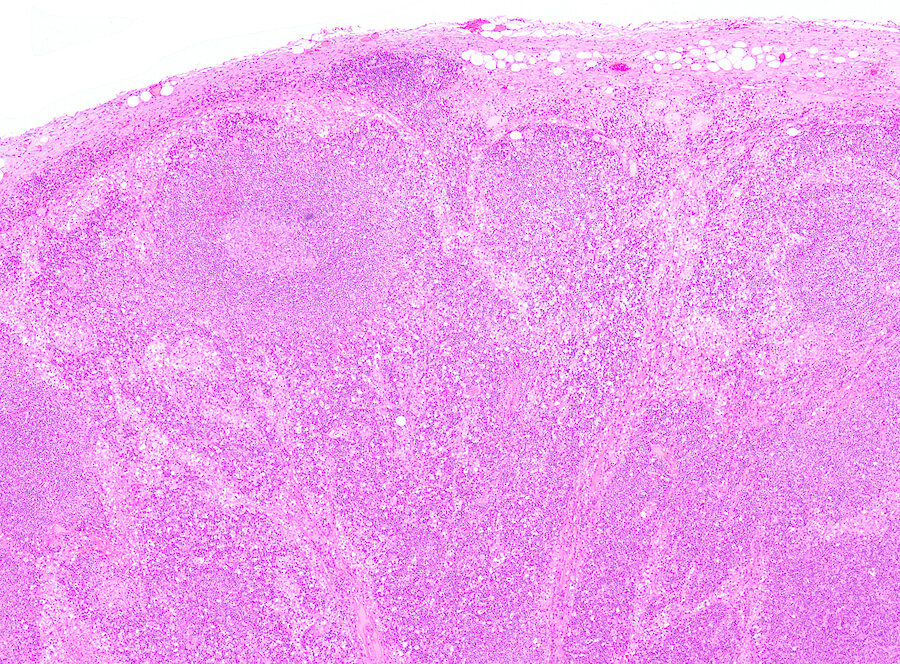
- Lymph node involvement (Curr Hematol Malig Rep 2016;11:504)
- Mainly mesenteric
- Common partial involvement with paracortical or sinusoidal pattern
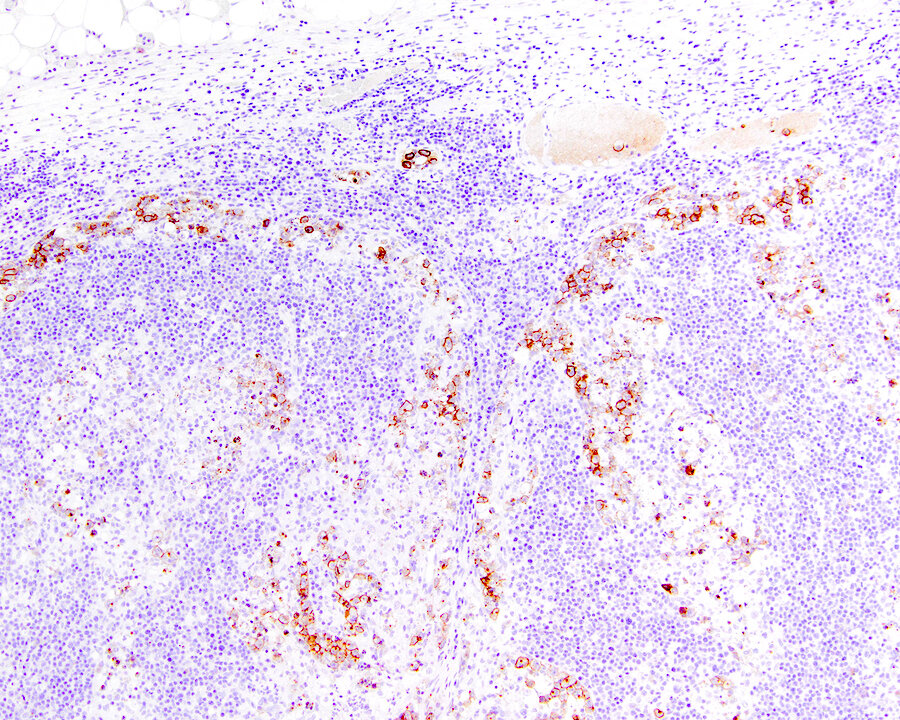
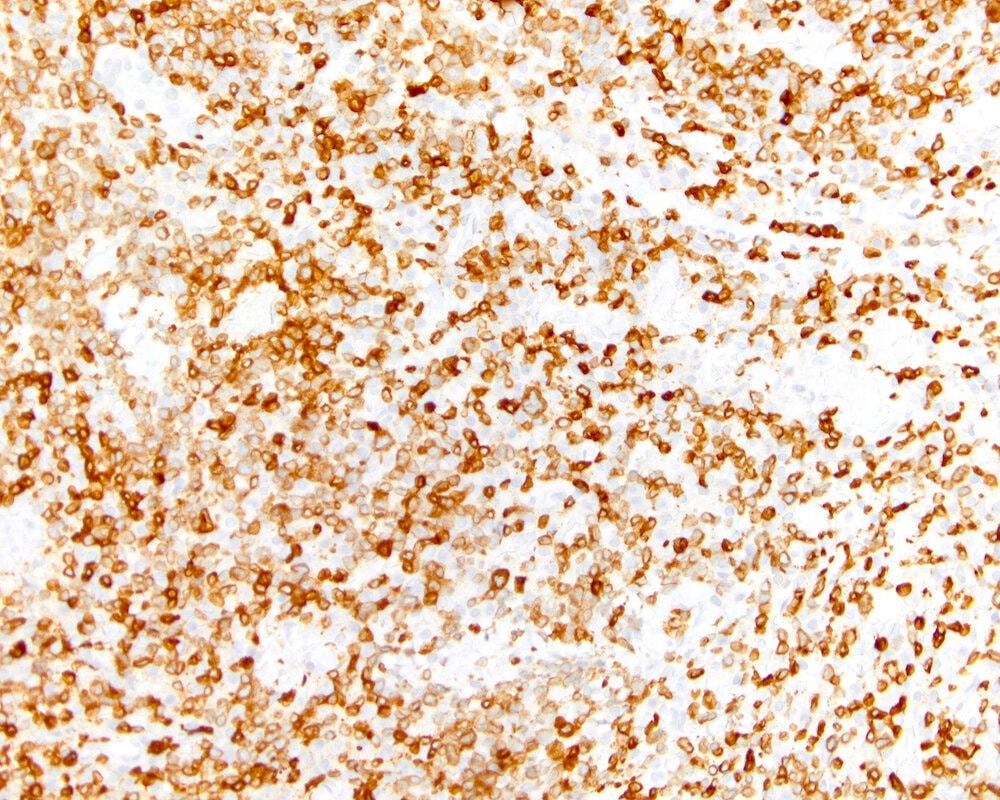
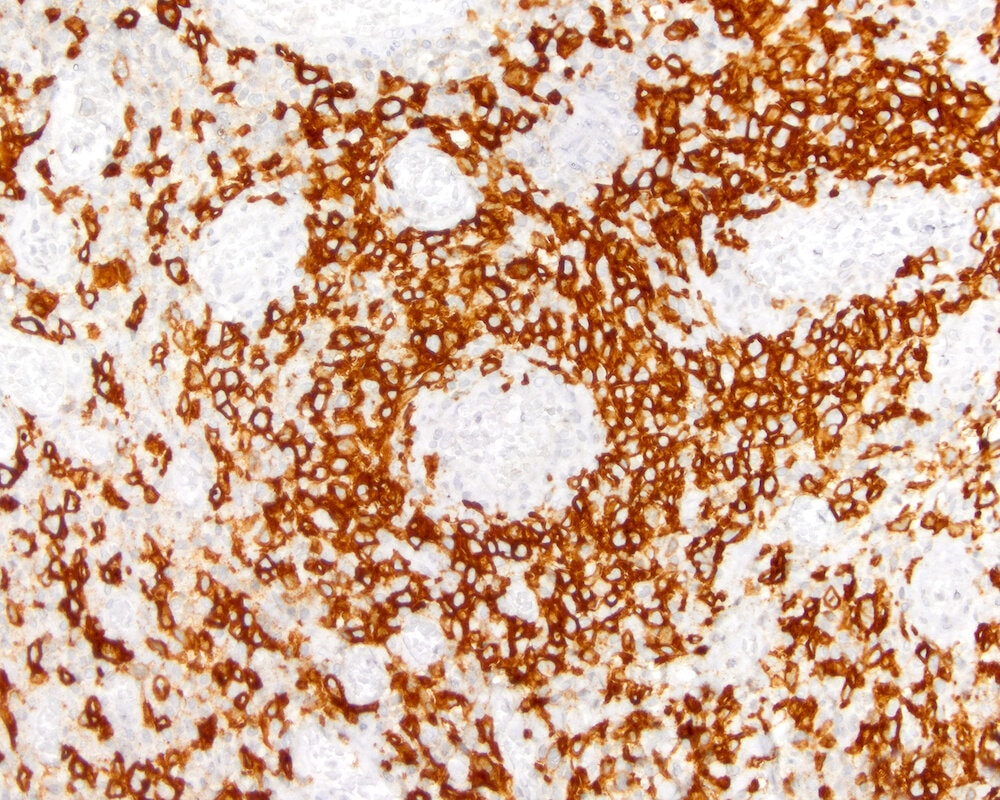
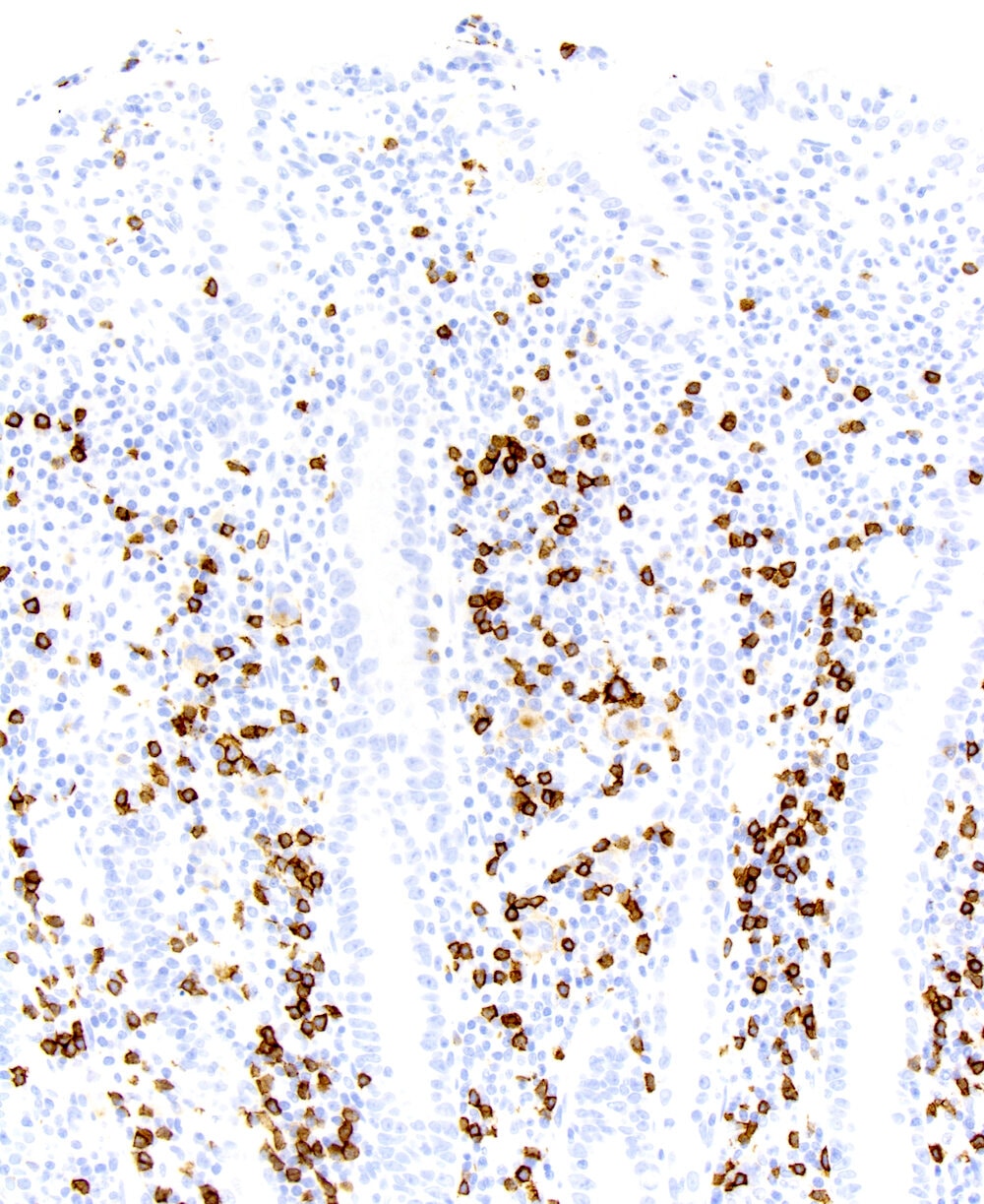
Microscopic (histologic) images
Contributed by Roberto N. Miranda, M.D.
Positive stains
- CD3 and CD7 (Blood 2011;118:148, Gastroenterology 2007;132:1902, Hum Pathol 2010;41:1231)
- TIA1 (Blood 2011;118:148, Hum Pathol 2010;41:1231)
- Perforin and granzyme B (Blood 2012;119:2458)
- CD103 (Gastroenterology 2005;128:S79)
- Overexpression of p53 (J Pathol 2004;202:252)
- Not associated with TP53 mutation
- CD30 (Blood 2011;118:148, Gastroenterology 2007;132:1902)
- May be focal positive, mainly in cases with anaplastic morphology
Negative stains
- Loss of T cell markers: CD2, CD4, CD5 and CD8 (Blood 2011;118:148, Gastroenterology 2005;128:S79, Hum Pathol 2010;41:1231)
- CD56 (Blood 2011;118:148)
- CD20 (J Clin Oncol 2003;21:2760)
- EBER (Blood 2011;118:148)
- TCR-β (Blood 2011;118:148, Mod Pathol 2015;28:1286)
- TCR-γ and δ (Hum Pathol 2013;44:1131)
Molecular / cytogenetics description
- Clonal TCR gene rearrangement (Gastroenterology 2005;128:S79, Am J Pathol 1995;146:509)
- Array comparative genomic hybridization (aCGH)
- Gain of 1q32, 5q35, 7q22 and 8q24 (Am J Clin Pathol 2007;127:701, Gastroenterology 2007;132:1902, Hum Pathol 2010;41:1231)
- Loss of 8p22-p23, 9p21, 13q22 and 18q22 (Am J Clin Pathol 2007;127:701, Gastroenterology 2007;132:1902, Hum Pathol 2010;41:1231)
- Loss of heterozygosity of chromosome 9p21 in around 30% of cases (J Pathol 2004;202:252)
- Associated with loss of p16 expression
- Amplification of 9q33-34 (Virchows Arch 2005;446:416, Am J Clin Pathol 2007;127:701, Hum Pathol 2010;41:1231, Am J Pathol 2002;161:1635)
- Allelic imbalance of NOTCH1 and ABL1
- Allelic variant of MYO9B (Blood 2012;119:2458)
- JAK/STAT and RAS pathways mutation may be detected in up to 50% of cases (Leukemia 2016;30:2245, Pathology 2021;53:349, Virchows Arch 2020;476:667)
Sample pathology report
- Small intestine, jejunum biopsies:
- Enteropathy associated T cell lymphoma (see comment)
- Comment:
- According to clinical notes, the patient has a previous history of celiac disease diagnosed 7 years ago and recently started with anemia, weight loss and diarrhea. Endoscopic examination showed multiple and active ulcers raising mucosal masses in jejunum and mosaic pattern on the adjacent mucosae. A computed tomography realized on the same day showed enlarged mesenteric lymph nodes.
- Multiple biopsies from the jejunum are reviewed. Hematoxylin and eosin sections show an ulcerated lesion and dense infiltration in mucosae and submucosae by atypical lymphocytes. The abnormal lymphocytes are of medium to large size, with prominent nucleoli and moderate to abundant cytoplasm and surrounded by a background with occasional histiocytes, eosinophils and neutrophils. The mucosa adjacent to the atypical infiltrate showed numerous small intraepithelial lymphocytes. Immunohistochemical studies demonstrated that the neoplastic cells are positive for CD3, CD7, TIA1 and TCR-β. The neoplastic cells are negative for CD4, CD5, CD8, CD20, CD56, PAX5, TCRγδ and EBER. The adjacent intraepithelial lymphocytes show a similar reactivity to the lymphoma cells.
- Concurrent polymerase chain reaction for T cell receptor gamma chain demonstrated monoclonal gene rearrangement.
- In summary, the clinicopathologic findings support a diagnosis of enteropathy associated T cell lymphoma in a patient with celiac disease.
Differential diagnosis
- Monomorphic epitheliotropic intestinal T cell lymphoma (MEITL) (Am J Surg Pathol 2011;35:1557, Am J Surg Pathol 2021;45:905, Blood Adv 2020;4:4769):
- Indolent T cell lymphoproliferative disorder of the gastrointestinal tract (Curr Hematol Malig Rep 2016;11:504, BMC Gastroenterol 2020;20:336):
- Lack of transmural involvement and does not form mass
- Not associated with celiac disease
- Majority of cases express CD8
- Peripheral T cell lymphoma, not otherwise specified (PTCL, NOS) (Hum Pathol 2010;41:1231):
- No association with celiac disease
- Most common gastrointestinal lymphoma but it is usually associated with systemic disease
- Most cases are CD4+
- Extranodal NK / T cell lymphoma, nasal type (ENKTCL) (Hum Pathol 2010;41:1231):
- Adult T cell leukemia / lymphoma (ATLL) (BMC Gastroenterol 2020;20:298):
- ALK negative anaplastic large cell lymphoma (ALK- ALCL) (Hum Pathol 2010;41:1231):
- T lymphoblastic lymphoma:
Additional references
Board review style question #1
Which of the following is true about enteropathy associated T cell lymphoma (EATL)?
- It does not associate with celiac disease
- Large and unifocal mass is the most common endoscopic finding
- There is an association with HLA-DQ2.2, HLA-DQ5 and HLA-DQ8
- Usually presents with peripheral lymphadenopathy
Board review style answer #1
C. There is an association with HLA-DQ2.2, HLA-DQ5 and HLA-DQ8. EATL is characteristically associated with celiac disease and in particular persons with major histocompatibility complex expressing HLA-DQ2.2, HLA-DQ5 and HLA-DQ8. Generalized lymphadenopathy is not a feature of intestinal lymphomas. Endoscopically, multiple small ulcerated lesions are noted.
Comment Here
Reference: Enteropathy associated T cell lymphoma (EATL)
Comment Here
Reference: Enteropathy associated T cell lymphoma (EATL)
Board review style question #2
Board review style answer #2
B. CD3+, CD4-, CD5-, CD7+, CD8-, EBER-, TCR-β-. EATL is a T cell lymphoma and thus expresses CD3, usually lacks CD4 and CD8 as well as TCR-β and is negative for Epstein-Barr virus.
Comment Here
Reference: Enteropathy associated T cell lymphoma (EATL)
Comment Here
Reference: Enteropathy associated T cell lymphoma (EATL)