Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Molecular / cytogenetics images | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Stone M, Jeon YK, Murga-Zamalloa C. Systemic EBV+ T cell lymphoma of childhood. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lymphomanonBchild.html. Accessed April 1st, 2025.
Definition / general
- Often rapid and fulminant disease within the spectrum of childhood Epstein-Barr virus (EBV) positive T cell lymphomas
Essential features
- Clinically characterized by systemic involvement, including the bone marrow, lymph nodes, spleen and lungs; most patients have a rapid, often fatal, clinical course
- Neoplastic elements are EBV+ T cell lymphocytes identified in biopsies from end organ damage biopsy sites; EBV+ T cell lymphocytes predominantly have a cytotoxic immunophenotype
- Neoplastic elements are mostly small lymphocytes without cytological atypia or effacement of the background tissue architecture
- It occurs in pediatric and young adult immunocompetent patients and there is an overlap in symptoms, clinical outcomes, laboratory findings and histomorphological features with the other 2 EBV+ T / NK lymphoproliferative disorders of childhood: EBV+ hemophagocytic lymphohistiocytosis (EBV+ HLH) and T / NK systemic form chronic active EBV disease (T / NK sCAEBV)
- These 3 entities represent different ends of a spectrum of end organ damage secondary to EBV infected hyperactivated T cell lymphocytes
Terminology
- No longer recommended
- Fulminant T cell lymphoproliferative disease
- Sporadic fatal infectious mononucleosis
- Fatal infectious mononucleosis
- Fulminant EBV+ T cell lymphoproliferative disorder of childhood
- Lethal hemophagocytic lymphohistiocytosis
- Fulminant hemophagocytic syndrome in children
- Severe chronic active EBV disease (CAEBV)
ICD coding
Epidemiology
- More commonly affects people in Asia, Mexico, Central America and South America
- Affects immunocompetent patients
- Most commonly occurs in children and young adults; rare cases have been reported in older adults
- References: Pediatr Blood Cancer 2019;66:e27798, Diagn Pathol 2021;16:48, Leuk Lymphoma 2017;58:53, Blood 2000;96:443, Leuk Lymphoma 2020;61:808
Sites
- Liver (40%), spleen (70%), bone marrow (40%), lung (50%), and lymph nodes (60%) (Pediatr Blood Cancer 2019;66:e27798, Diagn Pathol 2021;16:48, Leuk Lymphoma 2017;58:53, Blood 2000;96:443)
Pathophysiology
- Disease develops from EBV infected T cell lymphocytes (Pediatr Blood Cancer 2019;66:e27798, Diagn Pathol 2021;16:48, Leuk Lymphoma 2017;58:53, Blood 2000;96:443)
Etiology
- Epstein-Barr virus (EBV) is latent in memory type B cells of healthy carriers (Pediatr Blood Cancer 2019;66:e27798, Diagn Pathol 2021;16:48, Leuk Lymphoma 2017;58:53, Blood 2000;96:443, Blood 2001;98:280)
- However, patients who develop aggressive T cell lymphomas associated with EBV infection feature T or NK cells with latent EBV infection
- Mechanisms involved in the proliferation and expansion of T / NK cell types infected with EBV are not understood
- However, it is proposed that a subset of EBV+ T / NK cells may evade immune surveillance
Clinical features
- Symptoms include hepatosplenomegaly, fever, lymphadenopathy, malaise and upper respiratory tract symptoms
- Often, there is rapid development of multiorgan failure, sepsis and death within a few days to a few months in immunocompetent patients
- Proposed as a diagnosis of exclusion in EBV positive T / NK lymphoproliferative disorders of childhood that do not fulfill the criteria for T / NK sCAEBV or EBV positive HLH
- References: Diagn Pathol 2021;16:48, Leuk Lymphoma 2017;58:53, Blood 2000;96:443
Diagnosis
- Histologic, immunohistochemical, molecular and cytogenetic analysis of involved tissues and clinical correlation
Laboratory
- Hyperferritinemia, elevated liver enzymes, elevated lactate dehydrogenase (LDH), bicytopenias or pancytopenias
- Increased EBV DNA in the peripheral blood (> 1 x 102.5 copies/μg)
- References: Diagn Pathol 2021;16:48, Leuk Lymphoma 2017;58:53, Blood 2000;96:443
Prognostic factors
- Overall poor prognosis with a high mortality rate (66 - 90%) (Diagn Pathol 2021;16:48, Leuk Lymphoma 2017;58:53)
Case reports
- 16 year old girl with fatal disease course (Indian J Pathol Microbiol 2020;63:78)
- 30 year old woman with systemic EBV positive T cell lymphoma of childhood developing following systemic CAEBV disease (Diagn Pathol 2023;18:111)
- 68 year old woman with disease involving bone marrow and soft tissue (Pathol Int 2022;72:376)
Treatment
- HLH 2004 protocol or other etoposide containing regimens followed by hematopoietic stem cell transplant (Leuk Lymphoma 2017;58:53, Diagn Pathol 2021;16:48, Pediatr Hematol Oncol 2018;35:121)
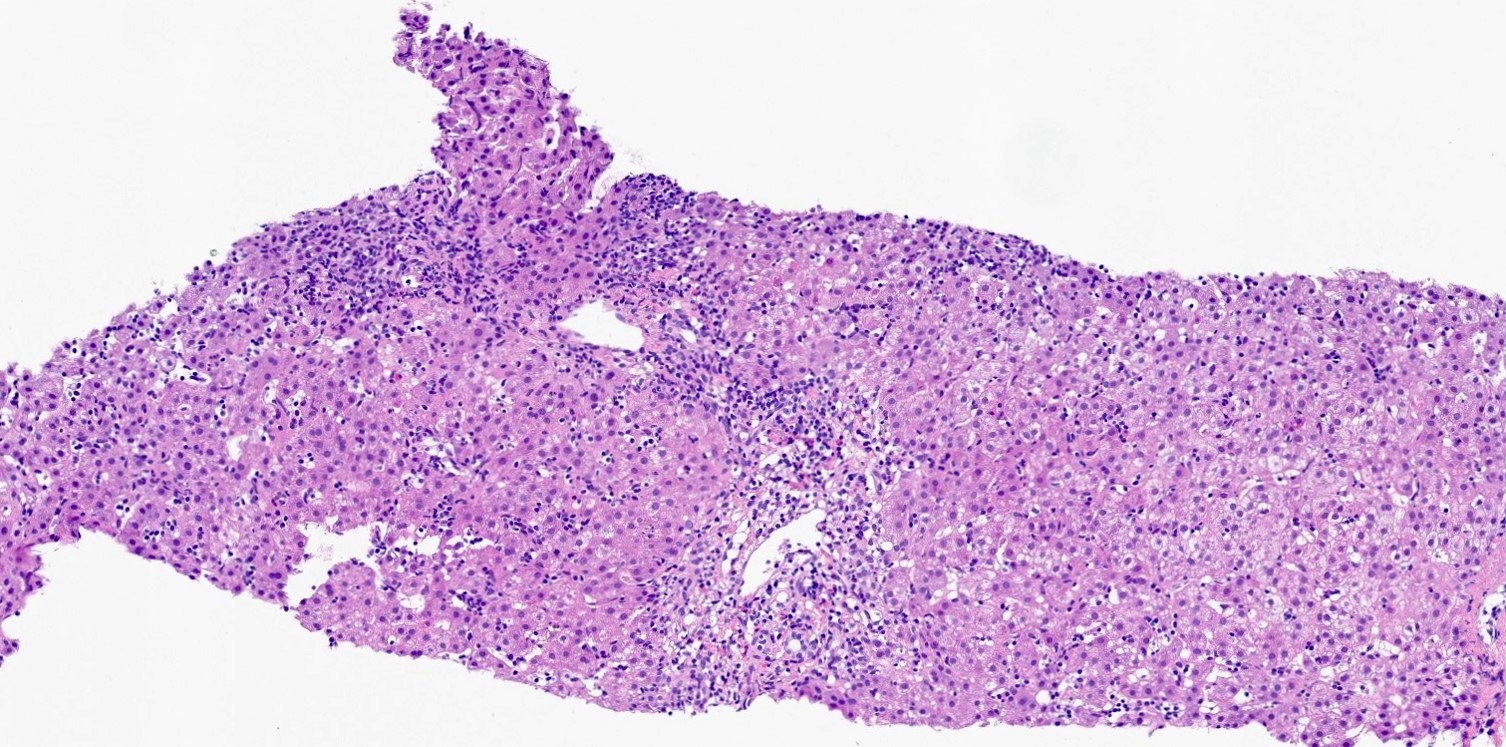
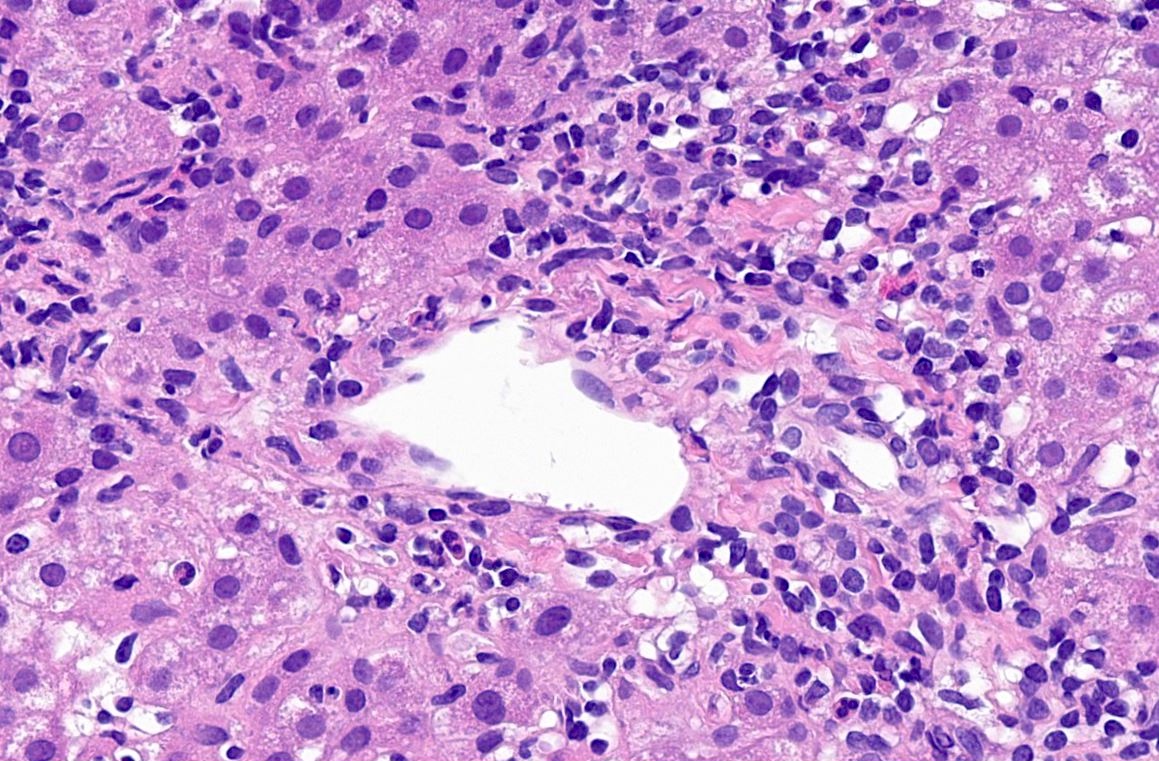
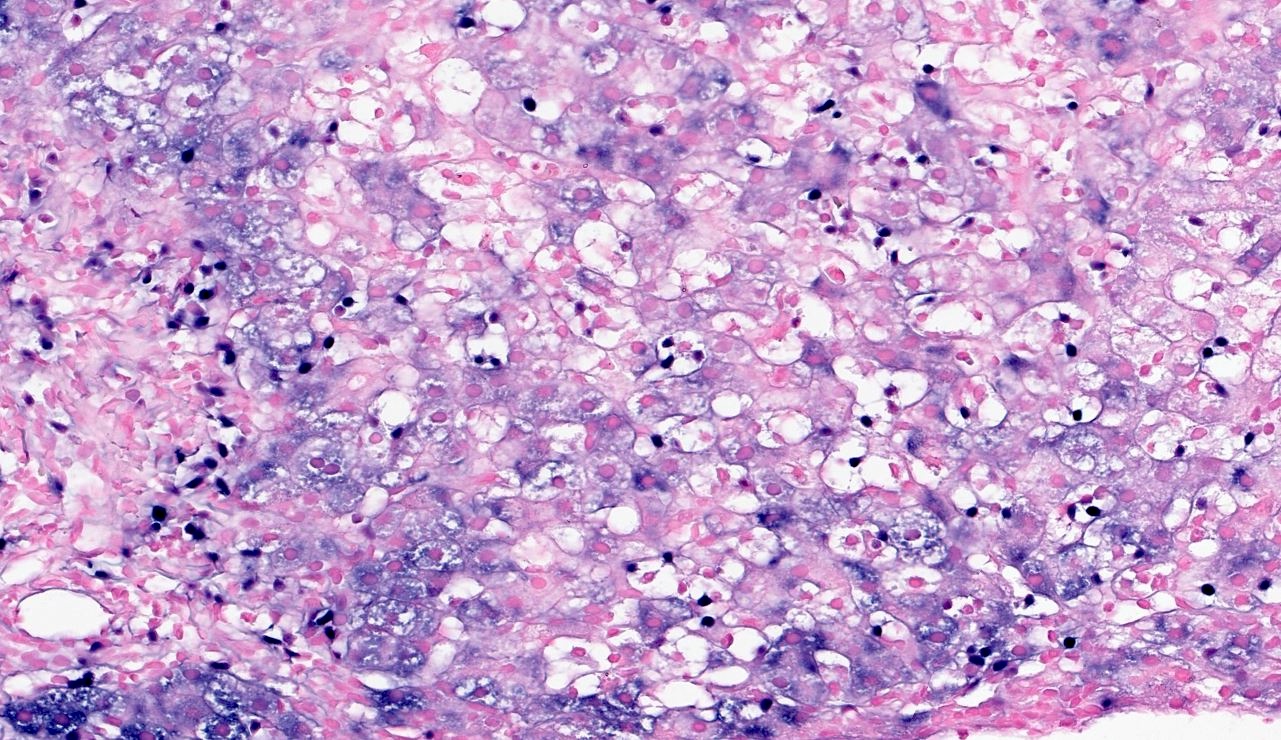
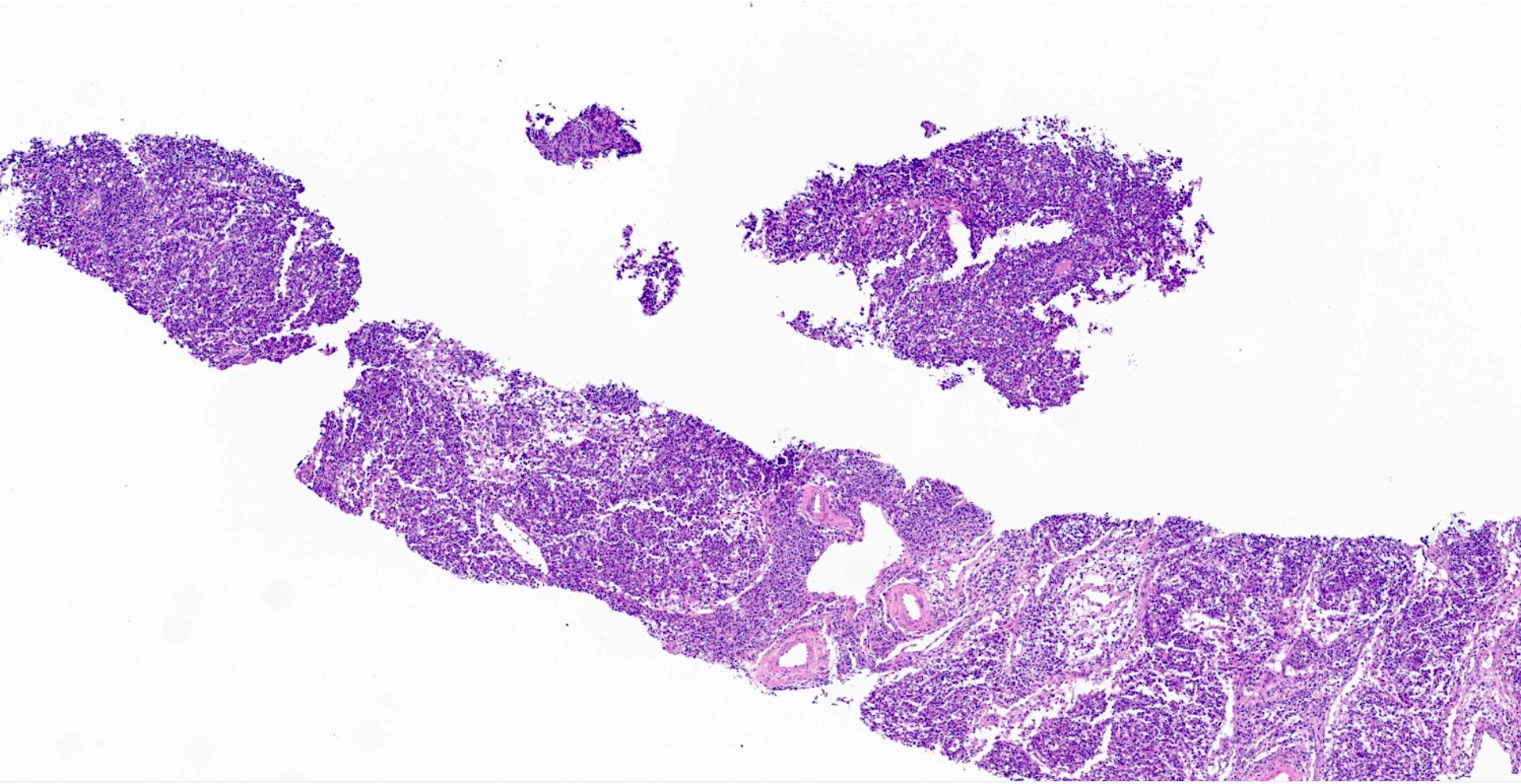
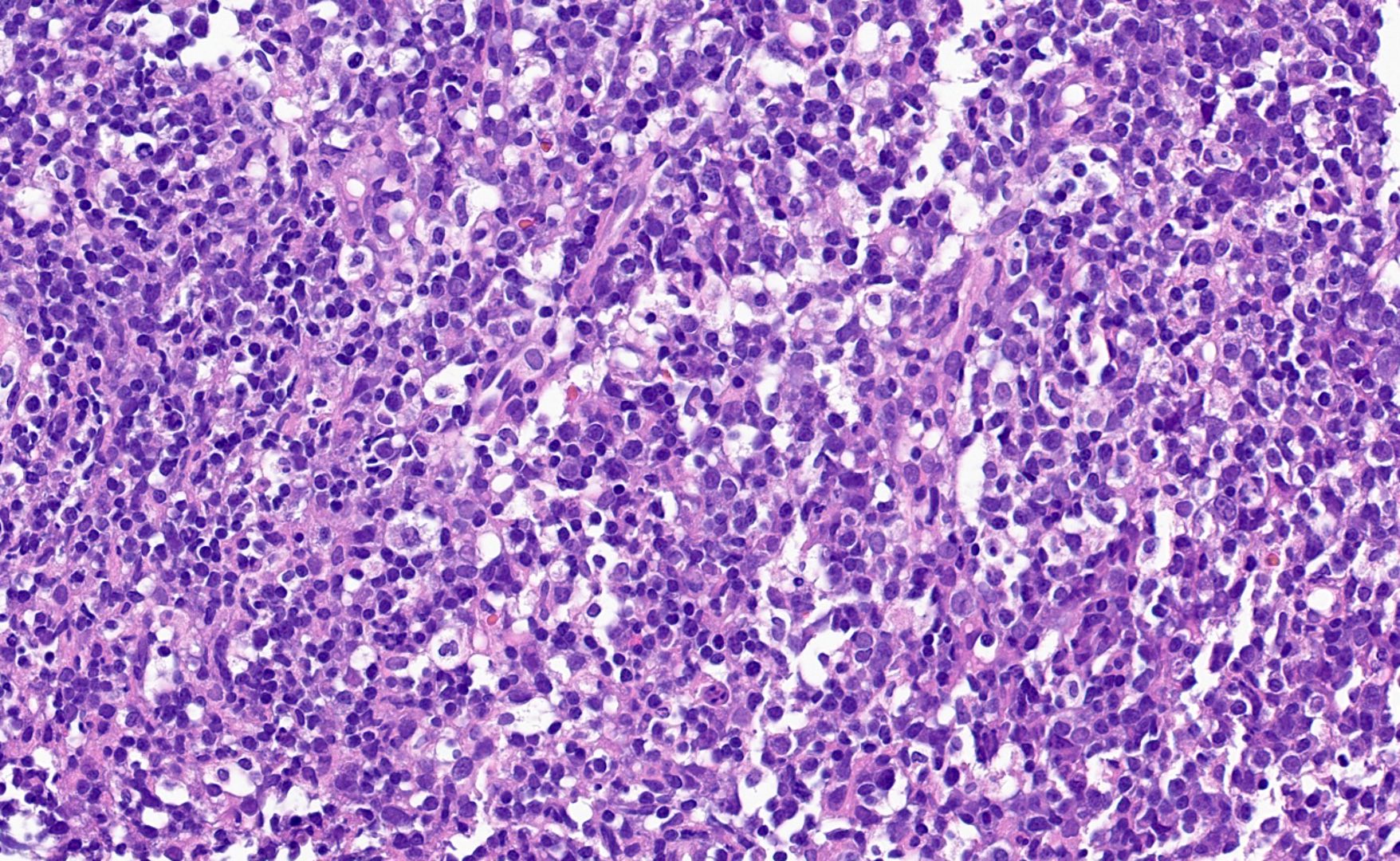
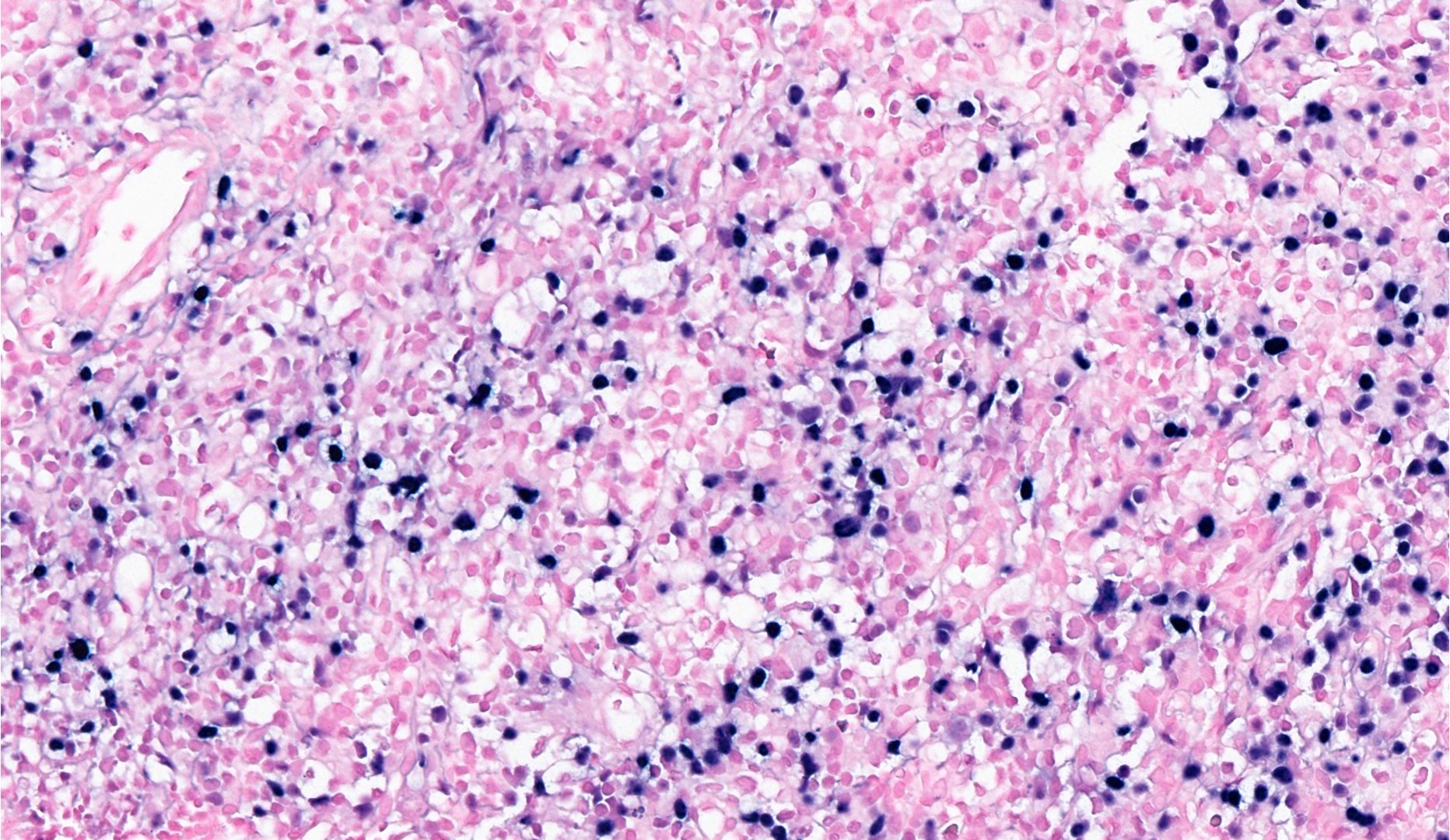
Microscopic (histologic) description
- More frequently, there is a mild expansion of small to medium sized T cell lymphocytes without cytological atypia or effacement of the background target tissue architecture
- When involved, the spleen shows depletion of the white pulp, lymphocyte infiltration of the red pulp and prominent hemophagocytosis
- When the liver is involved, findings include a sinusoidal and portal lymphocytic infiltrate; additional reported findings include cholestasis, steatosis and variable degrees of liver necrosis
- Bone marrow shows a scattered to diffuse, medium / large atypical lymphocytic infiltrate and increased histiocytes and hemophagocytosis
- Lymph nodes, when involved, usually show preserved architecture with open sinuses, expanded paracortical regions, sinus histiocytosis and hemophagocytosis (Pediatr Blood Cancer 2019;66:e27798, Blood 2000;96:443)
- Few cases with diffuse sheets of atypical medium to large lymphocytes involving the liver, bone marrow, spleen, lung or lymph node have been reported
- References: Diagn Pathol 2021;16:48, Leuk Lymphoma 2017;58:53, Blood 2000;96:443, Pediatr Blood Cancer 2019;66:e27798
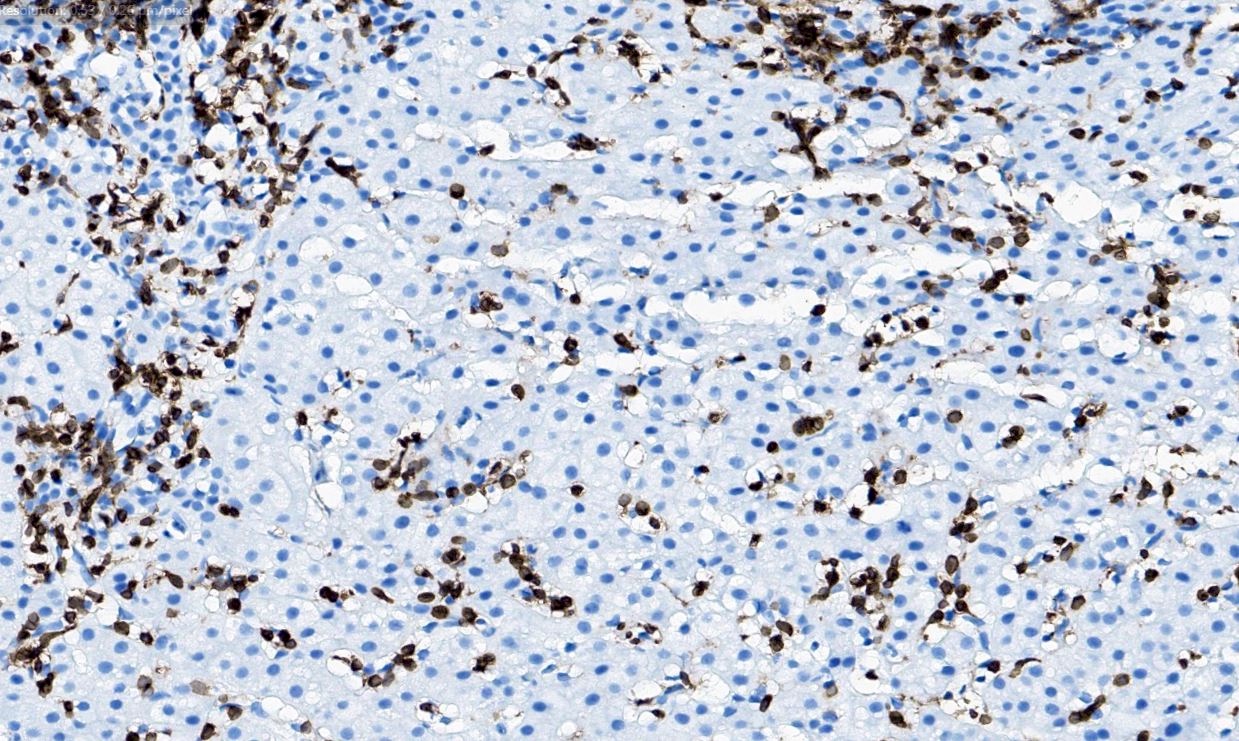
Microscopic (histologic) images
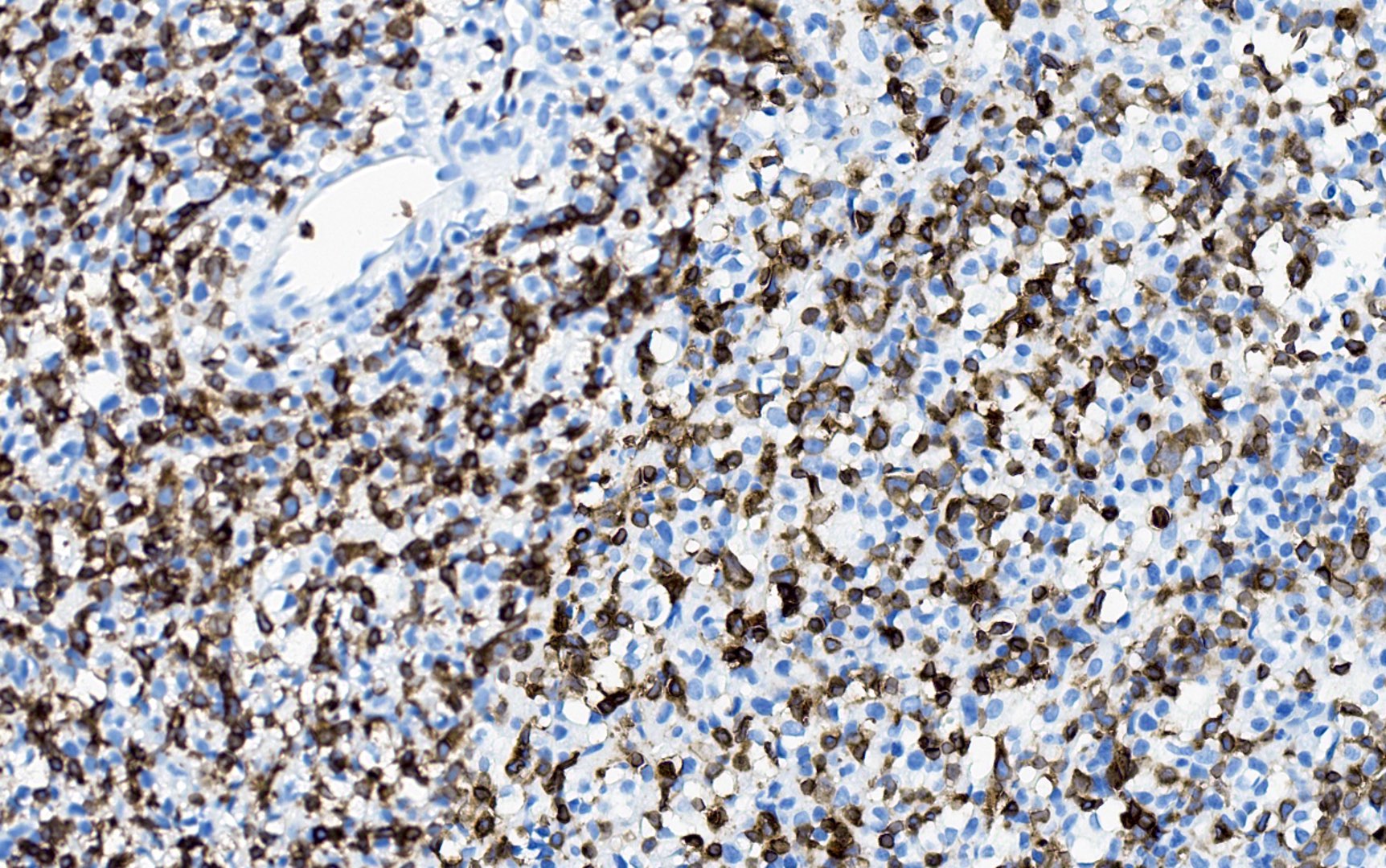
Positive stains
- CD3+ / CD8+
- CD3+, CD4+ (CD8 negative) in cases following systemic CAEBV disease
- EBER in situ hybridization (ISH)
- TIA1
- CXCR3 (60% of cases)
- CD2
- References: Leuk Lymphoma 2017;58:53, Blood 2000;96:443, Diagn Pathol 2021;16:48, Pediatr Blood Cancer 2019;66:e27798, Indian J Pathol Microbiol 2020;63:78, Diagn Pathol 2023;18:111
Negative stains
Molecular / cytogenetics description
- Monoclonal TCR gene rearrangements by PCR or EBV clonality testing (Int J Clin Exp Pathol 2014;7:5738, Blood 2000;96:443, Diagn Pathol 2021;16:48)
- Clonal cytogenetic abnormalities have been reported including inv(7) (Int J Clin Exp Pathol 2014;7:5738)
Sample pathology report
- Bone marrow core biopsy, touch imprints, aspirate and clot:
- Hypercellular bone marrow with atypical EBV positive T cell lymphocytic infiltrates (see comment)
- Comment: The T cell lymphocytic infiltrates feature aberrant loss of CD5 and concurrent T cell receptor rearrangement studies are consistent with a monoclonal T cell population. In the proper clinical context, these findings can be consistent with systemic EBV positive T cell lymphoma of childhood.
Differential diagnosis
- Aggressive natural killer cell leukemia (ANKL) (Cancers (Basel) 2020;12:2900, Blood Cancer J 2017;7:660, Blood 2012;119:673):
- Primarily a leukemic disease by definition, with secondary hepatosplenomegaly and bone marrow involvement
- Positive expression of CD56, CD16, EBER and cytoplasmic CD3ε with lack of surface CD3 expression
- Lack of expression of surface T cell receptor and monoclonal TCR gene rearrangements
- Aggressive clinical course, overall survival is < 1 year after diagnosis
- Chronic active EBV disease of T / NK cell type, systemic form (T / NK sCAEBV) (Blood Adv 2020;4:2918, Blood 2012;119:673, Pathogens 2018;7:28, Semin Diagn Pathol 2020;37:32, Am J Clin Pathol 2024 Feb 12 [Epub ahead of print]):
- Persistent high EBV titers and infectious mononucleosis symptoms for > 3 months
- Positive EBV infection of T or NK cells in peripheral blood or involved tissues
- Most commonly, it involves the spleen, liver and bone marrow
- By definition, EBV infected T or NK cells lack cytological atypia and do not efface the background tissue architecture
- T cell type (59% of cases) (CD4 > CD8)
- NK cell type (CD56 positive of 41% of cases)
- It often shows monoclonality by TCR gene rearrangement or EBV clonality testing; fewer cases are oligoclonal or polyclonal
- Can develop following EBV negative HLH; it is proposed that cases of EBV+ HLH that do not respond to initial therapies with persistent high EBV counts may constitute T / NK sCAEBV
- EBV+ hemophagocytic lymphohistiocytosis (EBV+ HLH) (J Clin Invest 1993;92:1444, Int J Clin Exp Pathol 2014;7:5738, Br J Haematol 2022;196:31, Semin Diagn Pathol 2020;37:32, Pediatr Blood Cancer 2007;48:124):
- Diagnosis requires meeting the HLH 2004 diagnostic criteria, including 5 out of 9 clinical and laboratory findings
- Hemophagocytosis is detected in the bone marrow, liver or lymph nodes
- Small numbers of EBV+ T cell lymphocytes are identified
- T cells do not show cytologic atypia or effacement of the background architecture
- Lack of clonal cytogenetic abnormality
- EBV+ T cells are CD8+ / CD4-
- Lack of monoclonal TCR gene rearrangement
- EBV+ nodal T and NK cell lymphoma (Hum Pathol 2015;46:981, Am J Surg Pathol 2015;39:462, Int J Hematol 2016;104:591, Histopathology 2012;61:186, J Clin Exp Hematop 2020;60:30, Pathol Res Pract 2013;209:448, Haematologica 2018;103:278):
- Primarily, it is a nodal disease with limited extranodal disease, including the bone marrow, spleen or liver
- Diffuse effacement of the lymph node architecture by lymphocytes with marked cytological atypia; the atypical lymphocytes are most commonly medium to large with pleomorphism
- Most cases show a CD3+ / CD8+ phenotype (~90%)
- Positive for EBER (in at least 30% of the tumor cells) and cytotoxic markers (TIA1, granzyme B)
- Monoclonal TCR gene rearrangement (75 - 85%)
Table 1: Comparison of the clinical and laboratory findings between the entities included in the differential diagnosis of systemic EBV+ T cell lymphoma of childhood (adapted from Am J Clin Pathol 2024 Feb 12 [Epub ahead of print])
| Epstein-Barr virus associated hemolymphohistiocytosis (EBV HLH) | Chronic active EBV disease of T / NK cell type systemic form (T / NK sCAEBV) | Systemic EBV positive T cell lymphoproliferative disorder of childhood | Nodal EBV positive T / NK cell lymphoma | Aggressive NK cell leukemia | |
| Morphological features | Small T cell lymphocytes with no definitive cytological atypia | The infiltrates are predominantly composed by lymphocytes and plasma cells with no effacement or distortion of the background tissue and without morphological atypia; HRS-like cells may be present | Variable expansion of lymphocytic infiltrates composed by small to medium sized T cells with no morphological atypia | Effacement of the nodal architecture by medium to large lymphocytes with marked cytological atypia | Medium sized atypical lymphocytes, frequently with prominent nucleoli |
| Immunophenotype | A subset of T cells are EBV and CD8 positive; loss of pan T cell markers may be observed | The HRS-like cells are CD30 positive with variable expression of PAX5 and CD20; the EBV positive T cells are predominantly CD4 positive with loss of pan T cell markers (rare EBV+ CD8 T cells have been reported) | Majority of cases are composed by CD8 positive neoplastic T cells (CD4+ cases are rare) | A minimum of 30% EBV positive T cell lymphocytes is required; majority of the cases are composed by CD8 positive neoplastic cells | Cytoplasmic CD3 expression and positive expression of CD2, CD56 and CD16; negative for CD57 |
| Anatomical sites of presentation | Bone marrow and liver | Liver, bone marrow and spleen | Bone marrow, liver, lymph nodes, spleen | Lymph nodes | Peripheral blood and bone marrow |
| Age at diagnosis | Predominantly pediatric population | Predominantly pediatric population | Predominantly pediatric population | Adult populations | Peak incidence between 21 and 30 year old |
| Relevant clinical features | Meets diagnostic criteria for HLH; good responses to etoposide based regimens | Persistent mononucleosis-like symptoms and high EBV titers for at least 3 months; good responses to systemic chemotherapy and hematopoietic stem cell transplantation is curative in most of pediatric patients; dismal clinical course in adult populations | Rapid development of multiorgan failure and end organ damage including liver failure, hepatosplenomegaly and pancytopenia, with high mortality rates | Aggressive clinical course and poor responses to current chemotherapeutic agents | Fulminant clinical course with a median overall survival of < 2 months |
| Relevant clinical features and prognosis | Meets diagnostic criteria for HLH; overall good prognosis with good responses to etoposide based regimens | Persistent mononucleosis-like symptoms and high EBV titers for at least 3 months; pediatric patients display good responses to systemic chemotherapy and hematopoietic stem cell transplantation is curative in most of pediatric patients; adult patients are characterized by dismal clinical course and poor prognosis | Rapid development of multiorgan failure and end organ damage including liver failure, hepatosplenomegaly and pancytopenia, with high mortality rates and poor prognosis | Aggressive clinical course, poor responses to current chemotherapeutic agents and bad prognosis | Fulminant clinical course, median overall survival of < 2 months and dismal prognosis |
Board review style question #1
Board review style answer #1
D. Presence of a clonal cytogenetic abnormality. Clonal cytogenetic abnormalities are found in systemic EBV+ T cell lymphoma of childhood but not EBV+ HLH. Answer A is incorrect because both systemic EBV+ T cell lymphoma of childhood and EBV+ HLH show EBER positivity in CD8+ T cells in most cases. Answer B is incorrect because systemic EBV+ T cell lymphoma of childhood and EBV+ HLH show no cytologic atypia; however, the presence of cytologic atypia would favor a diagnosis of systemic EBV+ T cell lymphoma of childhood. Answer C is incorrect because systemic EBV+ T cell lymphoma of childhood and EBV+ HLH most commonly occur in children and young adults (Int J Clin Exp Pathol 2014;7:5738).
Comment Here
Reference: Systemic EBV+ T cell lymphoma of childhood
Comment Here
Reference: Systemic EBV+ T cell lymphoma of childhood
Board review style question #2
Which of the following is correct regarding EBV+ T cell lymphoproliferative neoplasms of childhood?
- An indolent clinical course characterizes EBV+ T cell lymphoproliferative neoplasms
- Diagnosis can be established only after documentation of T cell receptor clonality studies
- Distinction between systemic EBV+ T cell lymphoma and chronic active EBV disease of T / NK cell type, systemic form (T / NK sCAEBV) can be established solely on morphological analysis of the lymphocytic infiltrates
- These groups of diseases constitute a continuum with similar histological features and overlap in clinical and laboratory findings
Board review style answer #2
D. These groups of diseases constitute a continuum with similar histological features and overlap in clinical and laboratory findings. Systemic EBV+ T cell lymphoma, T / NK sCAEBV and HLH EBV overlap in clinical features, are indistinguishable in histological features and can precede one another. Answer A is incorrect because these entities usually have an aggressive clinical course. Answer B is incorrect because T cell receptor clonality studies are not positive in all cases and its presence is not required to establish the diagnosis. Answer C is incorrect because the histological features between systemic EBV+ T cell lymphoma and T / NK sCAEBV are similar (Leuk Lymphoma 2017;58:53, Am J Clin Pathol 2024 Feb 12 [Epub ahead of print]).
Comment Here
Reference: Systemic EBV+ T cell lymphoma of childhood
Comment Here
Reference: Systemic EBV+ T cell lymphoma of childhood