Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Morphologic variants | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Balakrishna J, Jaffe ES. Anaplastic large cell lymphoma, ALK positive. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lymphomanonBanaplastic.html. Accessed December 24th, 2024.
Definition / general
- A peripheral T cell lymphoma usually consisting of large lymphoid cells with abundant amphophilic cytoplasm, often horseshoe shaped nuclei, an ALK (anaplastic lymphoma kinase) gene translocation and expression of ALK protein and CD30 (Swerdlow: WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues, 4th Edition, 2017)
- Affects lymph nodes and extranodal sites (Swerdlow: WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues, 4th Edition, 2017)
- Cases with variant histology (small cells and lymphohistiocytic variants) have a more aggressive clinical course
Essential features
- T cell lymphoma
- Characteristic hallmark cells
- CD30 diffusely and strongly positive
- ALK positive
- ALK gene rearrangement
Terminology
- Also called Ki-1 (CD30+) lymphoma, ALCL (obsolete)
ICD coding
- ICD-10: C84 - mature T / NK cell lymphomas
- C84.6 - anaplastic large cell lymphoma, ALK positive
- C84.60 - unspecified site
- C84.61 - lymph nodes of head, face, and neck
- C84.62 - intrathoracic lymph nodes
- C84.63 - intra-abdominal lymph nodes
- C84.64 - lymph nodes of axilla and upper limb
- C84.65 - lymph nodes of inguinal region and lower limb
- C84.66 - intrapelvic lymph nodes
- C84.67 - spleen
- C84.68 - lymph nodes of multiple sites
- C84.69 - extranodal and solid organ sites
Epidemiology
- 3% of adult and 10 - 20% of childhood non-Hodgkin lymphomas (Orphanet: Anaplastic Large Cell Lymphoma [Accessed 27 January 2020])
- Most frequent in children and young adults (first 3 decades of life) (Orphanet: Anaplastic Large Cell Lymphoma [Accessed 27 January 2020])
- Prevalence 1 - 9/100,000 (Orphanet: Anaplastic Large Cell Lymphoma [Accessed 27 January 2020])
- Male predominance (M:F = 1.5:1) (Swerdlow: WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues, 4th Edition, 2017)
Sites
- Frequent involvement of lymph nodes or extranodal sites (J Clin Exp Hematop 2017;57:120)
- Nodal involvement often not contiguous
- Most common extranodal sites are skin, bone, soft tissues, lung and liver (Blood 2000;96:3681)
- Compared to classic Hodgkin lymphoma, inguinal nodal involvement is more common and mediastinal disease is less common
- Gastrointestinal involvement is rare
- Marrow involvement detected in 10 - 20% of cases; CD30 is helpful in identifying bone marrow involvement (Histopathology 2013;63:13, Hum Pathol 2008;39:1331)
- Central nervous system involvement is more commonly seen with bone marrow involvement and is a poor prognostic finding
- Occasional leukemic presentation in peripheral blood with the small cell variant (Br J Haematol 2014;165:545)
Pathophysiology
- Neoplastic cells are activated mature cytotoxic T cells (Swerdlow: WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues, 4th Edition, 2017)
- Oncogenic translocations result in constitutive activation of the ALK tyrosine kinase
- Resulting fusion proteins are shown to be involved in different downstream signaling pathways including Ras/ERK, PI3K/Akt and JAK/STAT (Cancers (Basel) 2019;11:1074)
Etiology
- Etiology is unknown; the anaplastic lymphoma receptor tyrosine kinase ALK gene (2p23) is overexpressed due to t(2;5)(p23;q35) translocation (Orphanet: Anaplastic Large Cell Lymphoma [Accessed 27 January 2020])
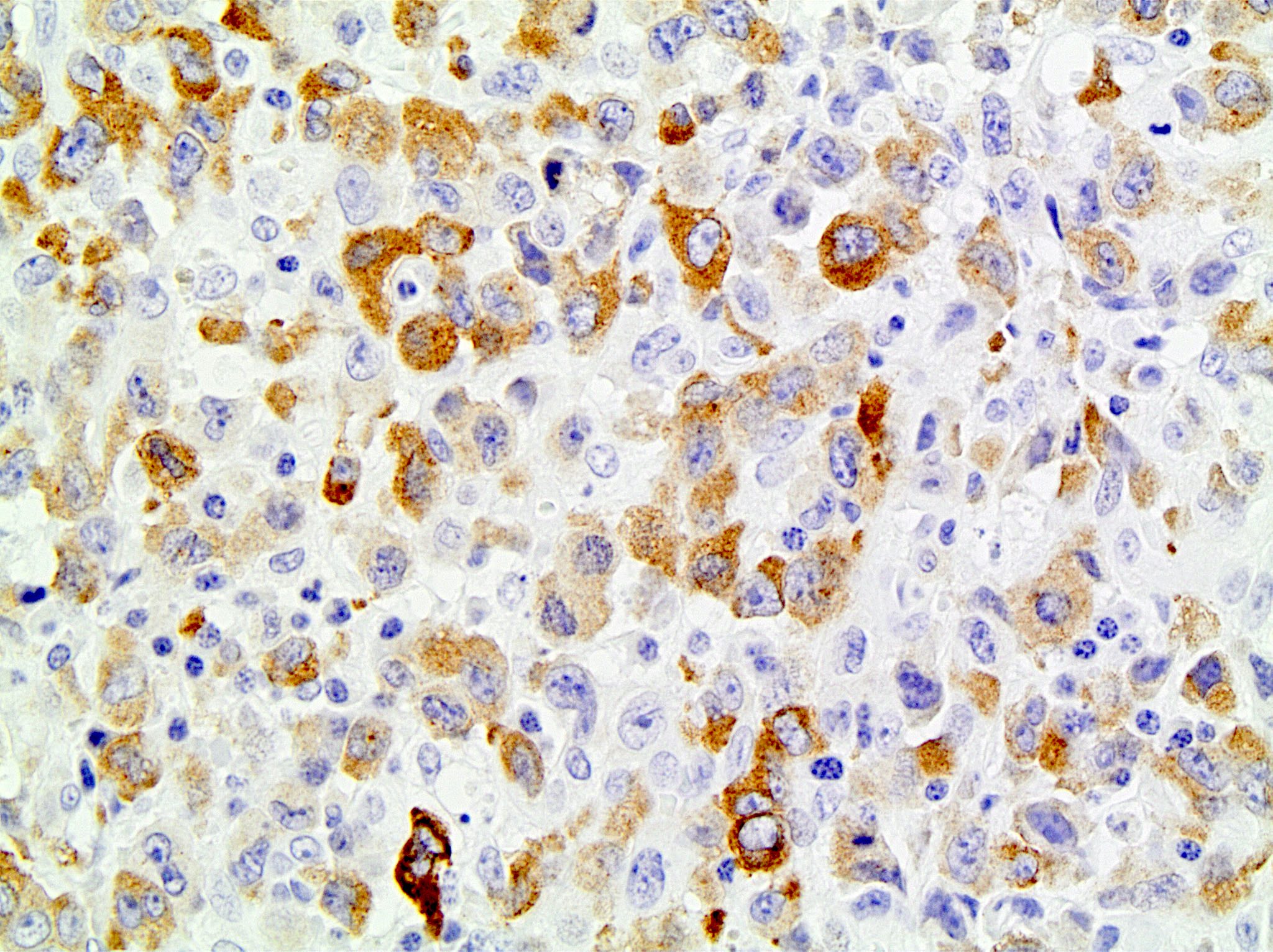
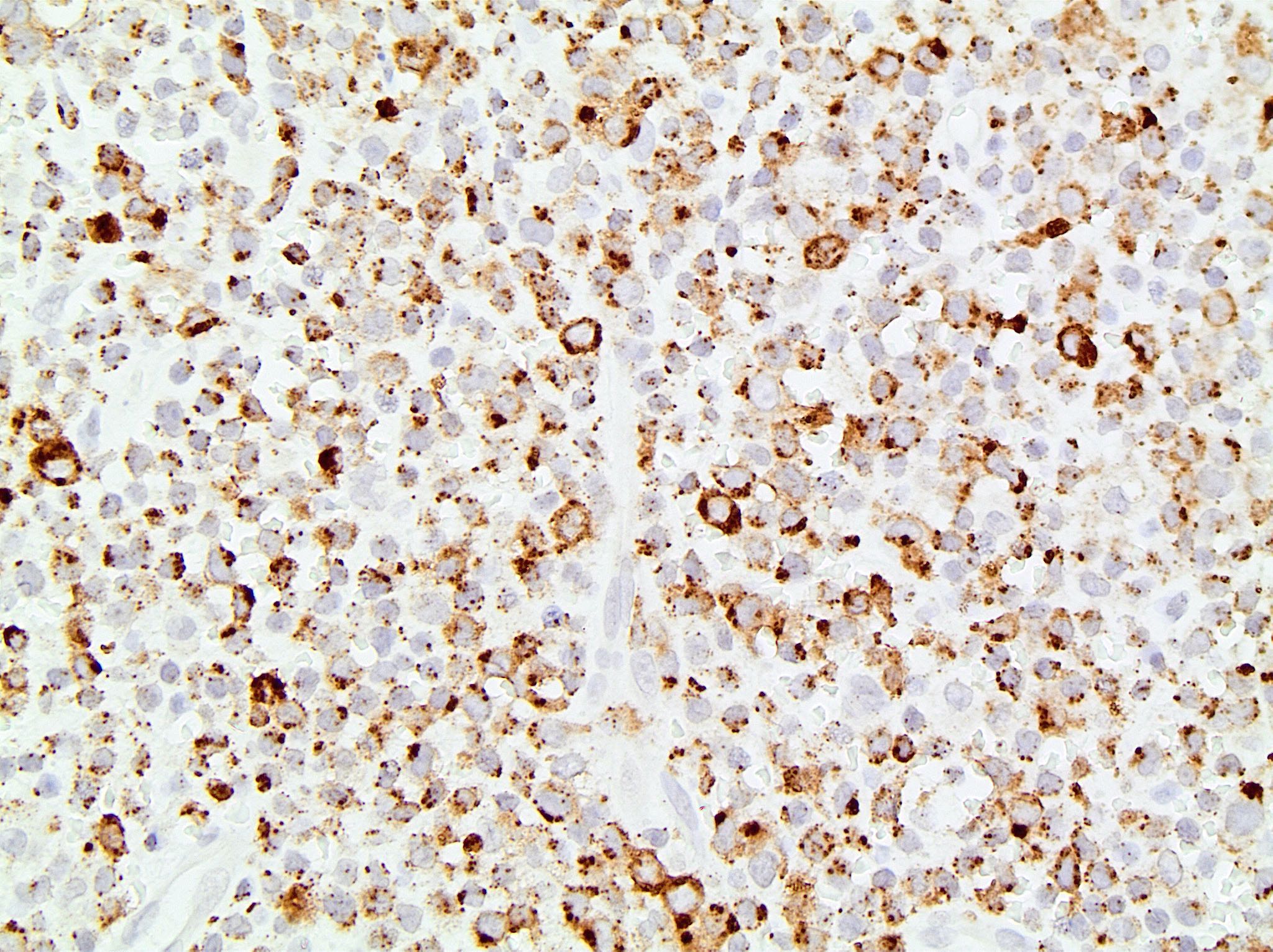
- Cases with the NPM-ALK translocation show both nuclear and cytoplasmic staining for ALK
- Variant translocations involving gene partners other than NPM show mainly cytoplasmic staining
- Not Epstein-Barr virus (EBV) related (Hum Pathol 2004;35:455)
- Clinical presentation following insect bites has been described (Haematologica 2010;95:449)
- This may be related to homing of neoplastic cells to sites of inflammation
Clinical features
- 70% present with stage III - IV disease (J Clin Exp Hematop 2017;57:120)
- Peripheral or abdominal lymphadenopathy, extranodal infiltrates, bone marrow involvement, B symptoms (especially high fever) (Blood 1999;93:2697)
- Anemia, pancytopenia, high lactate dehydrogenase (LDH), occasional eosinophilia (Blood 2008;111:5496)
Diagnosis
- Biopsy of involved lymph node / tissue with immunohistochemistry
- Morphology (see Microscopic description)
- Immunophenotype (see Positive stains)
- Detection of genetic abnormalities and T cell clone (see Molecular / cytogenetics)
Laboratory
- Elevated lactate dehydrogenase, pancytopenia, anemia, thrombocytopenia (Blood 2008;111:5496)
Radiology description
- Enlarged lymph nodes / mass lesion in involved tissue
Prognostic factors
- Moderately aggressive, may be curable; better prognosis than other peripheral T cell lymphomas and ALK- (80% versus 48%) (J Clin Exp Hematop 2017;57:120)
- 5 year failure free survival (FSS) also better than ALK- tumors (60% versus 36%) (Blood 2008;111:5496)
- International prognostic index (IPI) has limited prognostic value compared to other lymphomas
- No prognostic difference between classic and variant translocations
- Small cell or lymphohistiocytic variant morphology often present with disseminated disease at diagnosis (J Clin Oncol 2011;29:4669)
- Circulating tumor cells are associated with poor prognosis (Pathology 2020;52:100)
- 30% relapse, often remain sensitive to chemotherapy (J Clin Exp Hematop 2017;57:120)
Case reports
- 16 month old boy with leukemic presentation with a novel partner to ALK (Haematologica 2019;104:e218)
- 4 year old boy with anaplastic large cell lymphoma of the central nervous system (Pediatr Neurosurg 2007;43:516)
- 10 year old Japanese boy with anaplastic large cell lymphoma of leukemic presentation (J Pediatr Hematol Oncol 2008;30:696)
- 13 year old boy with anaplastic large cell lymphoma with C-MYC rearrangement relapsing in leukemic phase (Am J Hematol 2007;82:59)
- 14 year old boy with skeletal muscle anaplastic large cell lymphoma (Pediatr Hematol Oncol 2009;26:142)
- 16 year old girl with hypocellular lymphohistiocytic variant anaplastic large cell lymphoma (Arch Iran Med 2013;16:424)
- 16 year old girl with ALK positive anaplastic large T cell lymphoma of the breast, not implant related (J Pediatr Hematol Oncol 2010;32:e75)
- 17 year old girl with endobronchial anaplastic large cell lymphoma, T cell phenotype (Arch Pathol Lab Med 2003;127:e430)
- 33 year old woman with anaplastic large cell lymphoma, T cell phenotype, of the breast, implant related (Arch Pathol Lab Med 2003;127:e115)
- 47 year old man with anaplastic large cell lymphoma presenting with spontaneous splenic rupture (Pathology 2004;36:94)
- 71 year old man with stage IE T cell anaplastic large cell lymphoma, monomorphic variant, arising in a bone (Arch Pathol Lab Med 2000;124:1339)
- 2 Chinese women with pulmonary anaplastic large cell lymphoma (Acta Haematol 2007;118:188)
- Leukemic presentation (Pathol Int 2009;59:345)
Treatment
- First line treatment is chemotherapy (CHOP with or without etoposide) (Curr Hematol Malig Rep 2018;13:135, Haematologica 2019;104:e562)
- Allogeneic stem cell transplant is useful in refractory cases (Lancet Oncol 2004;5:127)
- Brentuximab vedotin (anti-CD30) for relapsed cases (Curr Hematol Malig Rep 2018;13:135)
- ALK inhibitors (crizotinib) in relapsed / refractory cases (Cancer Gene Ther 2010;17:633)
- Checkpoint inhibitors (nivolumab) are under trial (J Clin Oncol 2016;34:2698)
Gross description
- Enlarged lymph node
- Firm, fleshy mass
Microscopic (histologic) description
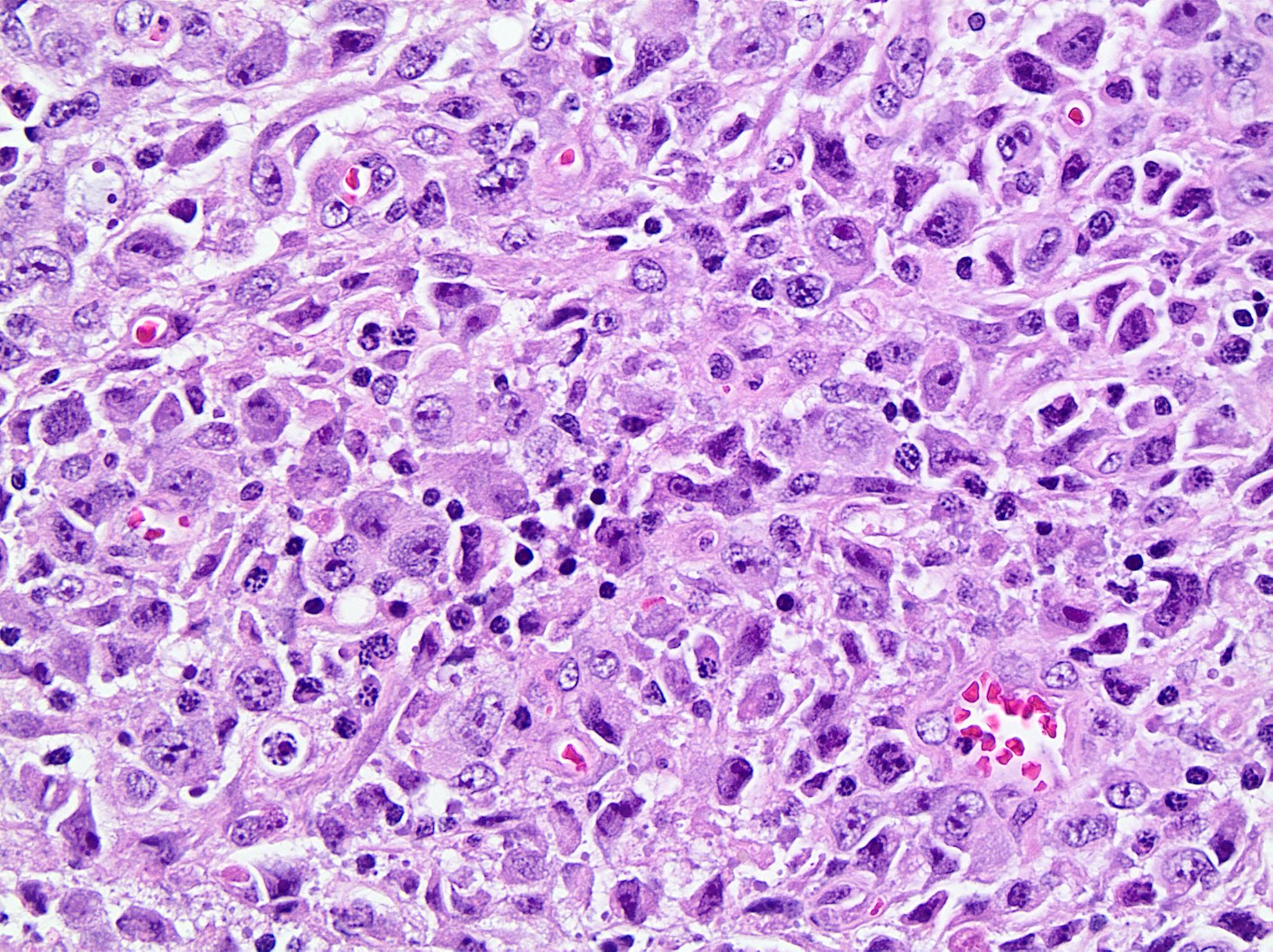
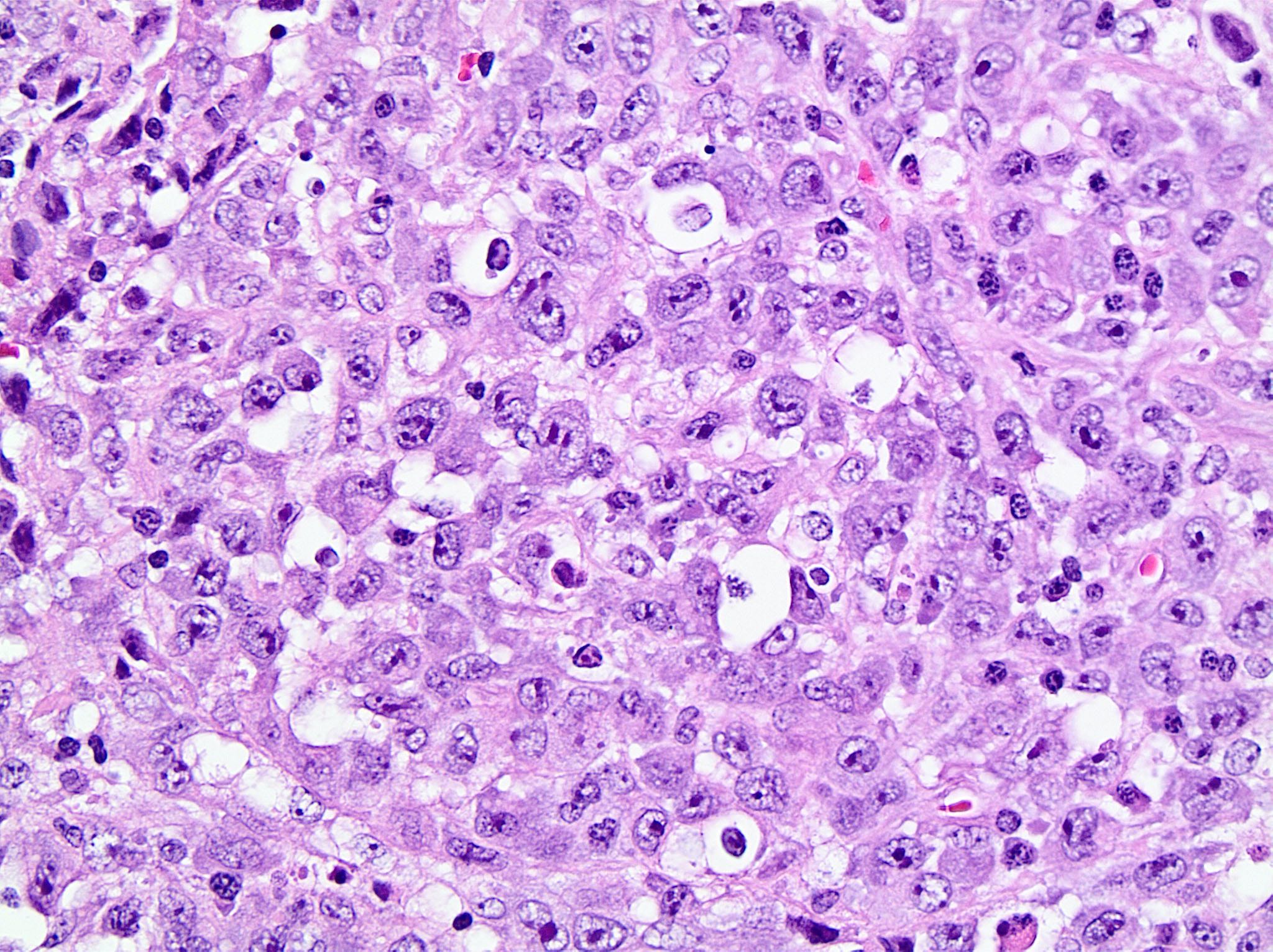
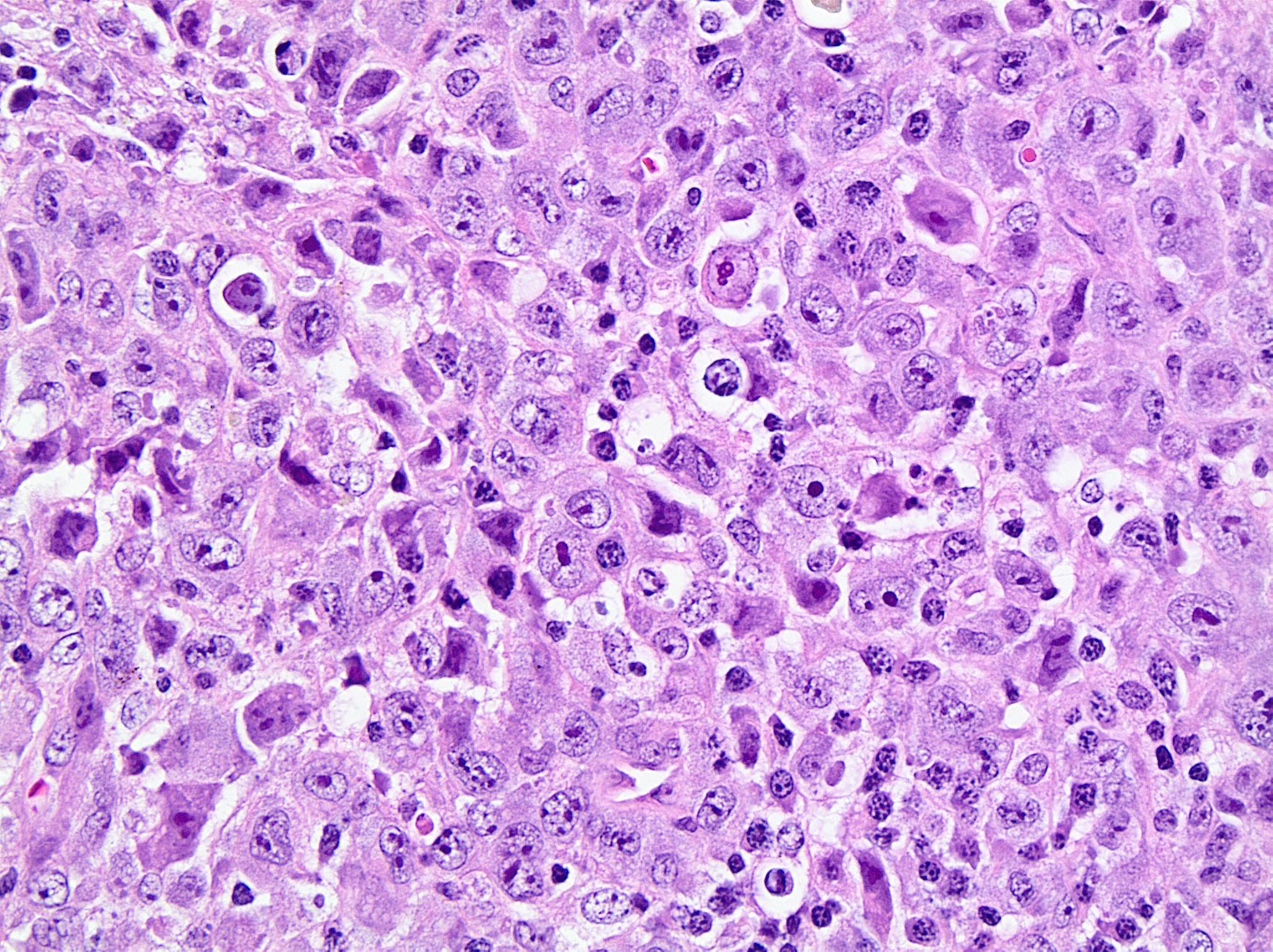
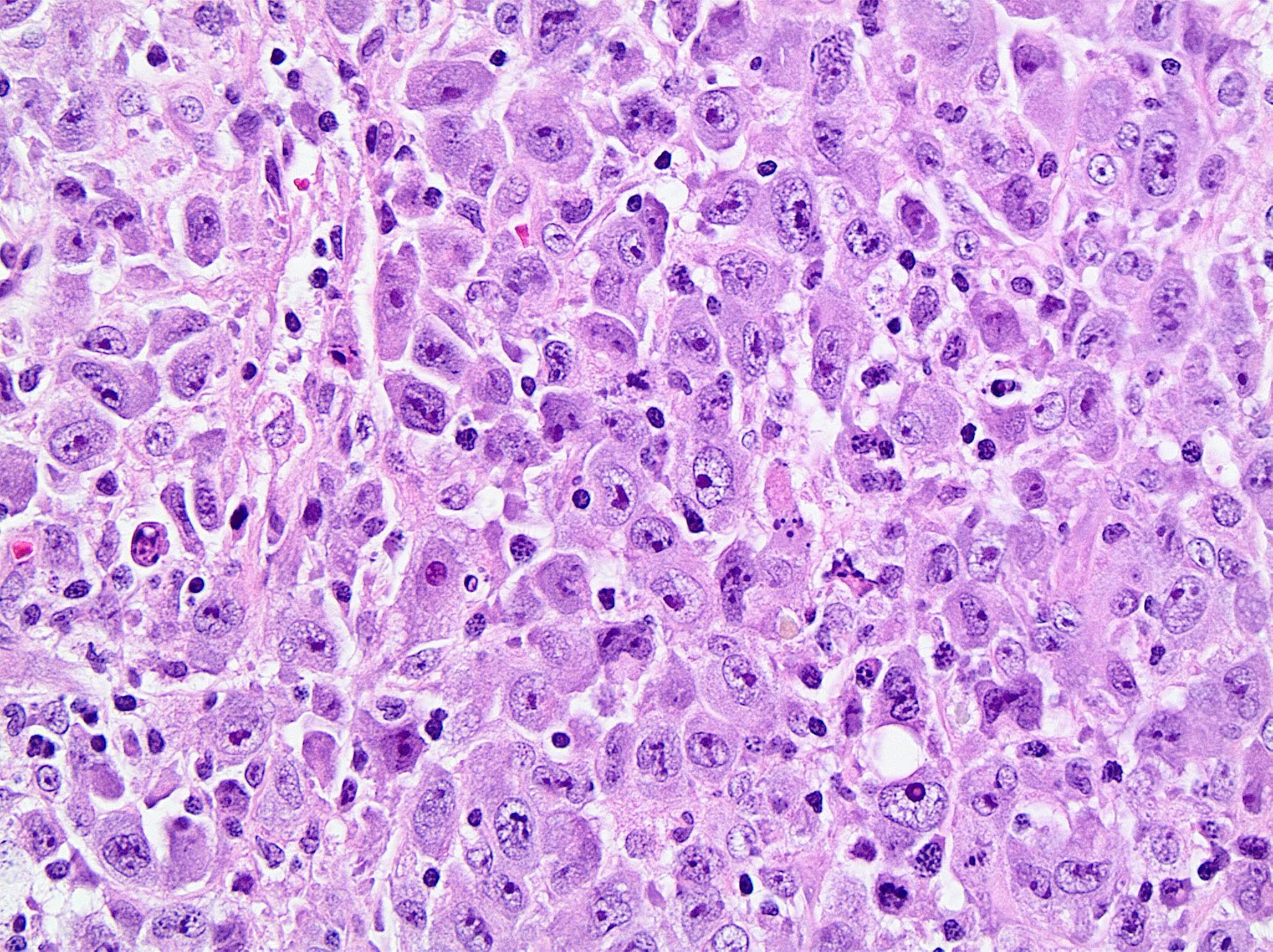
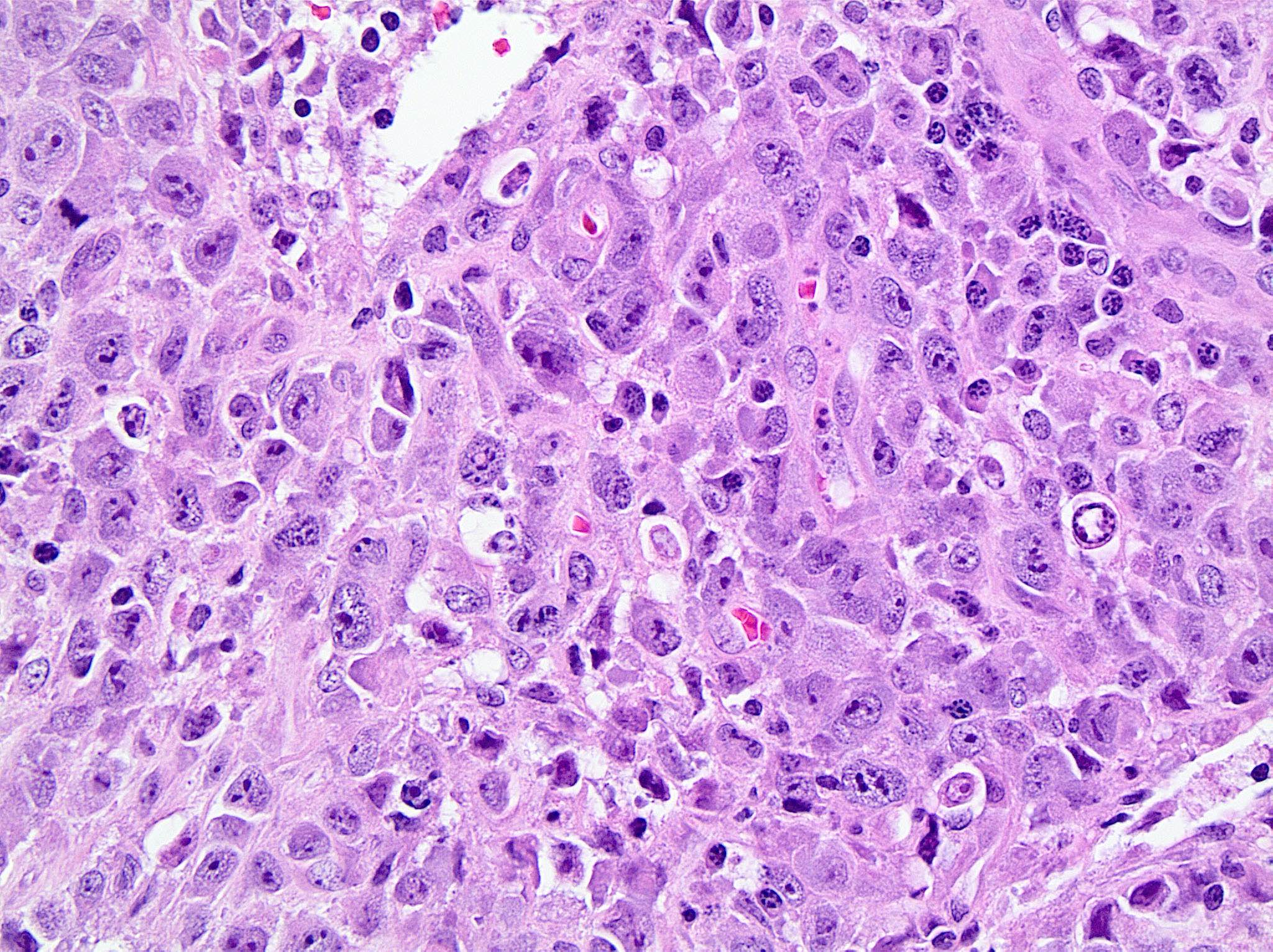
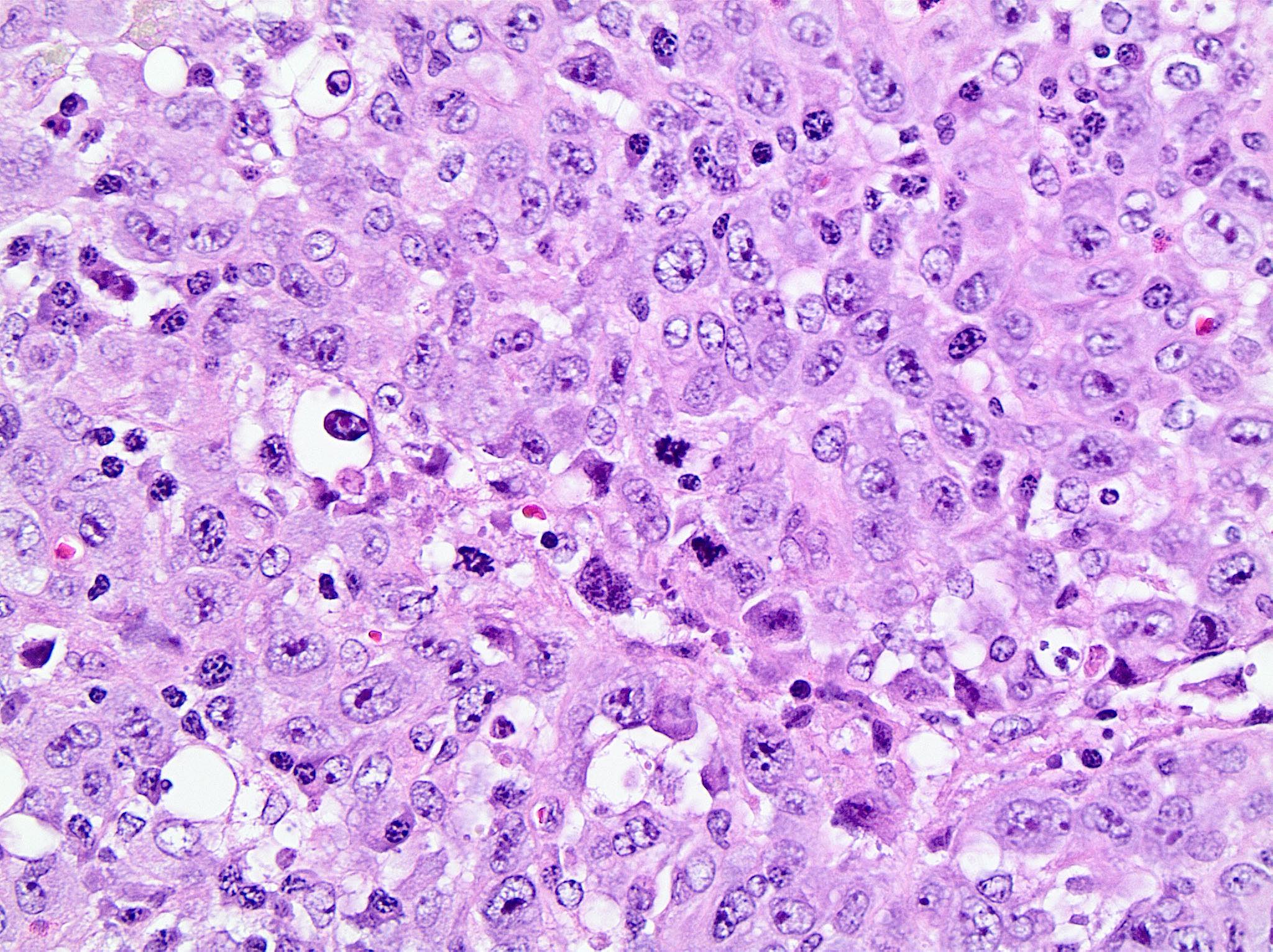
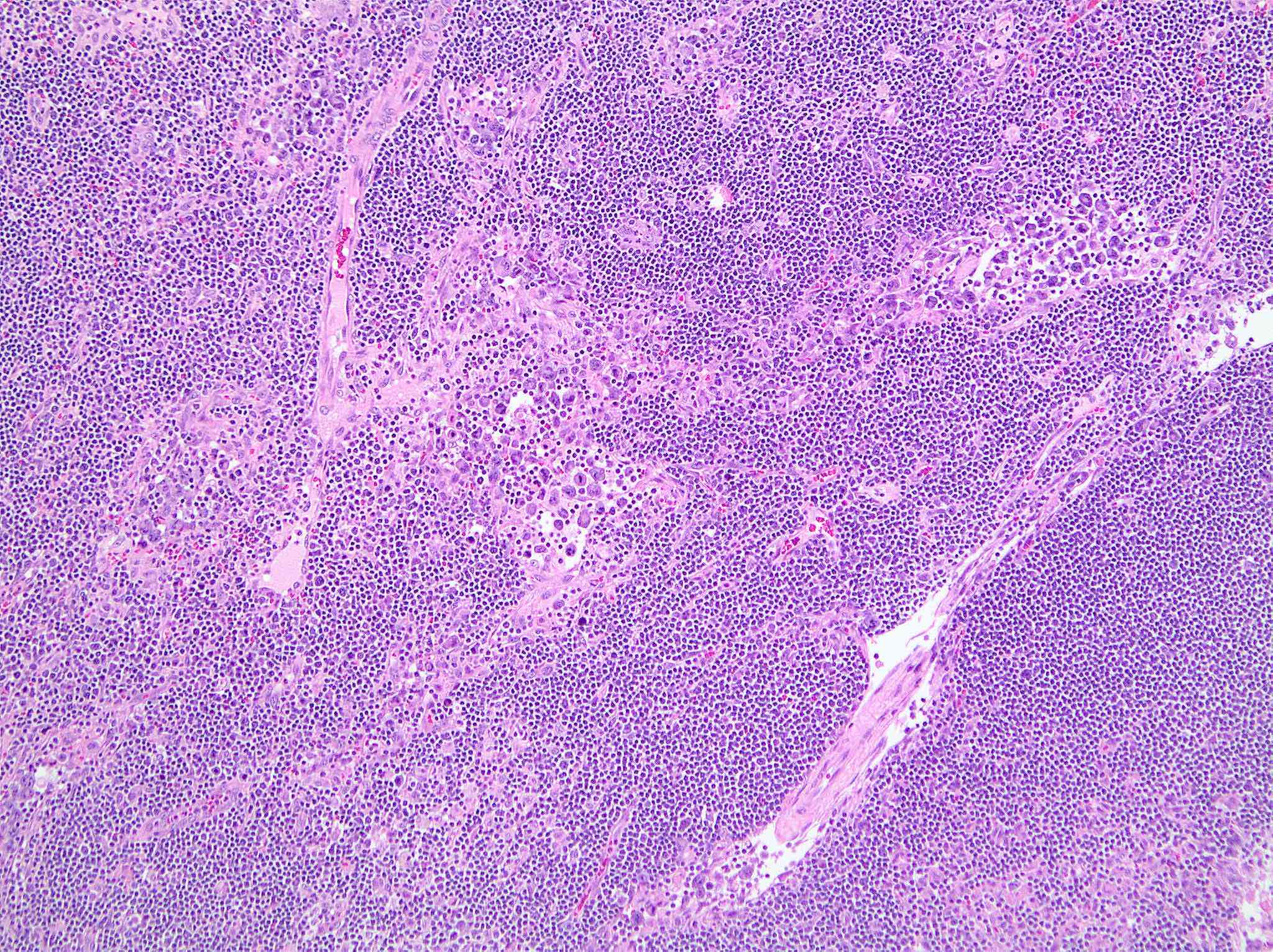
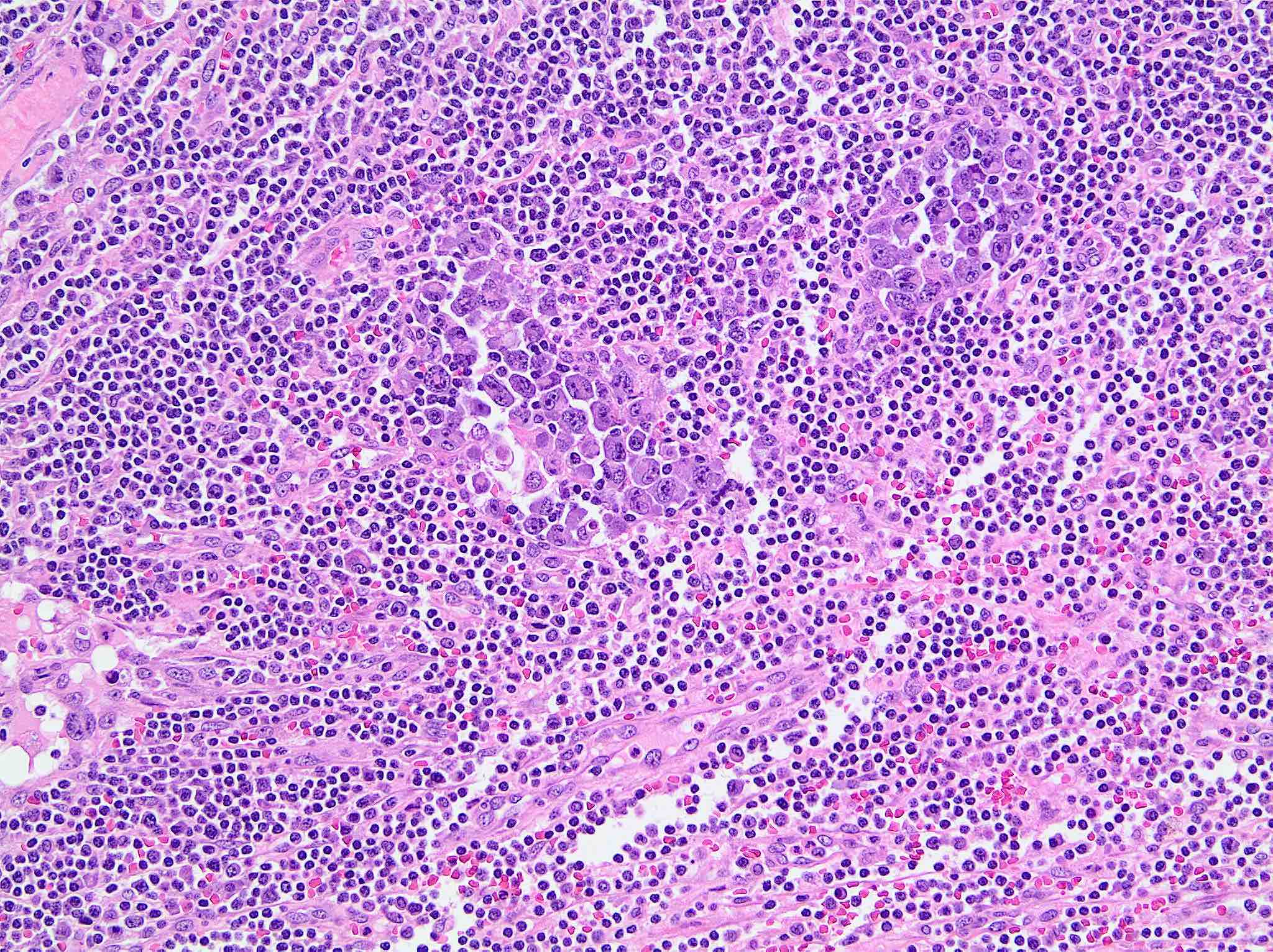
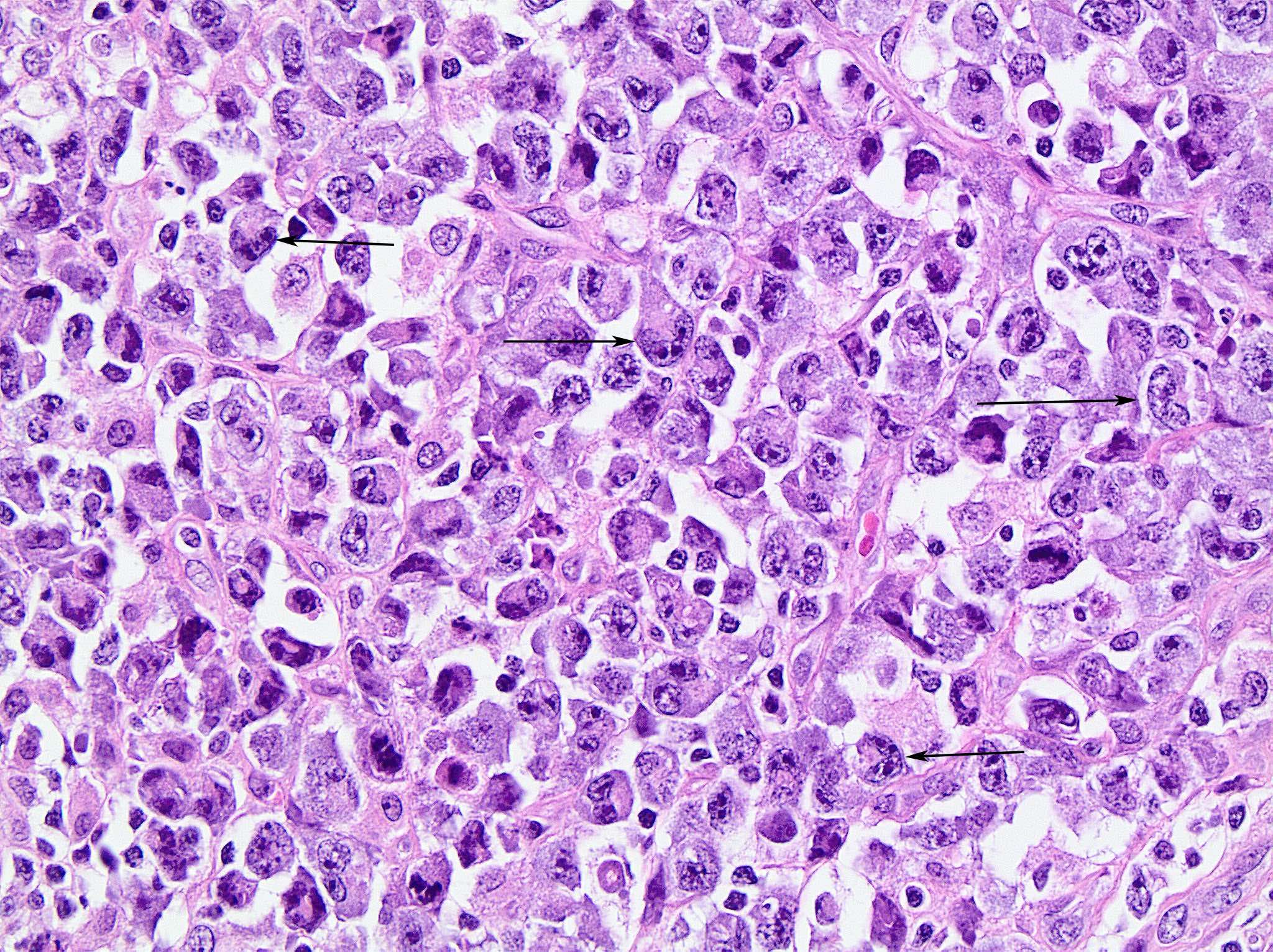
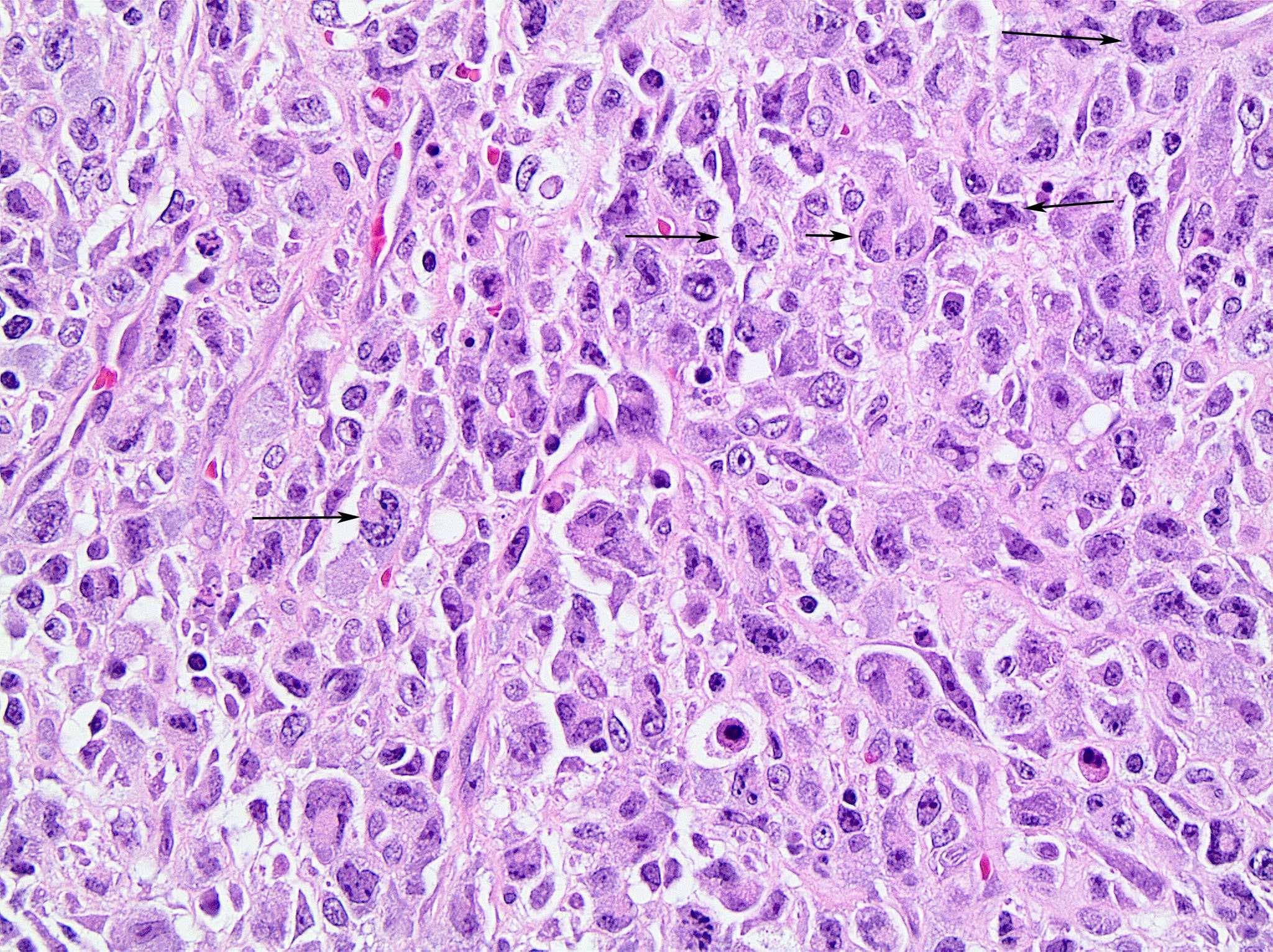
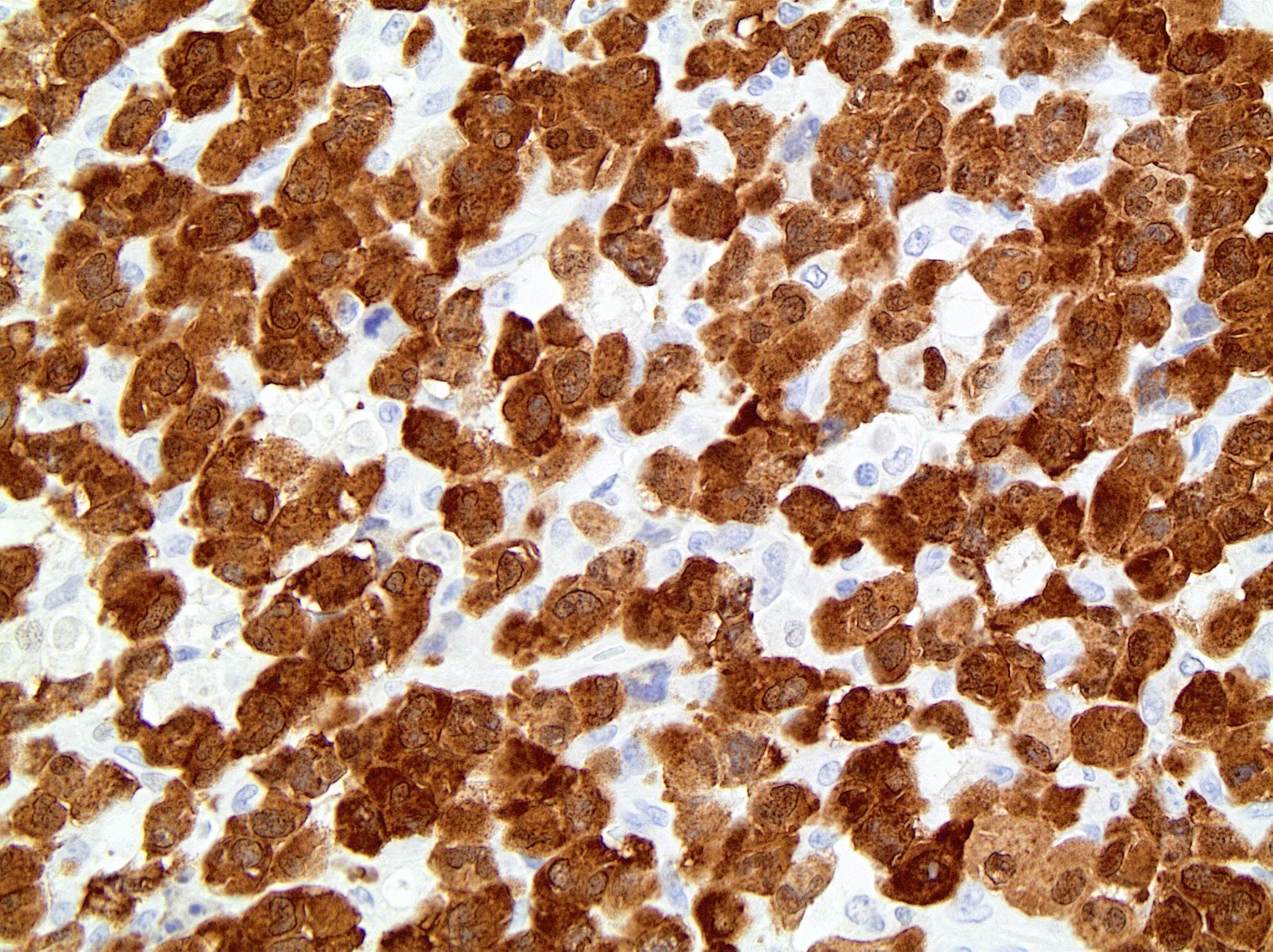
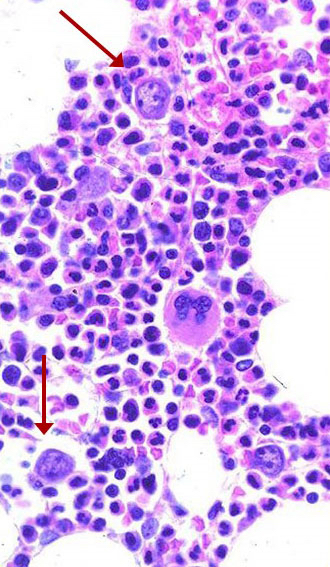
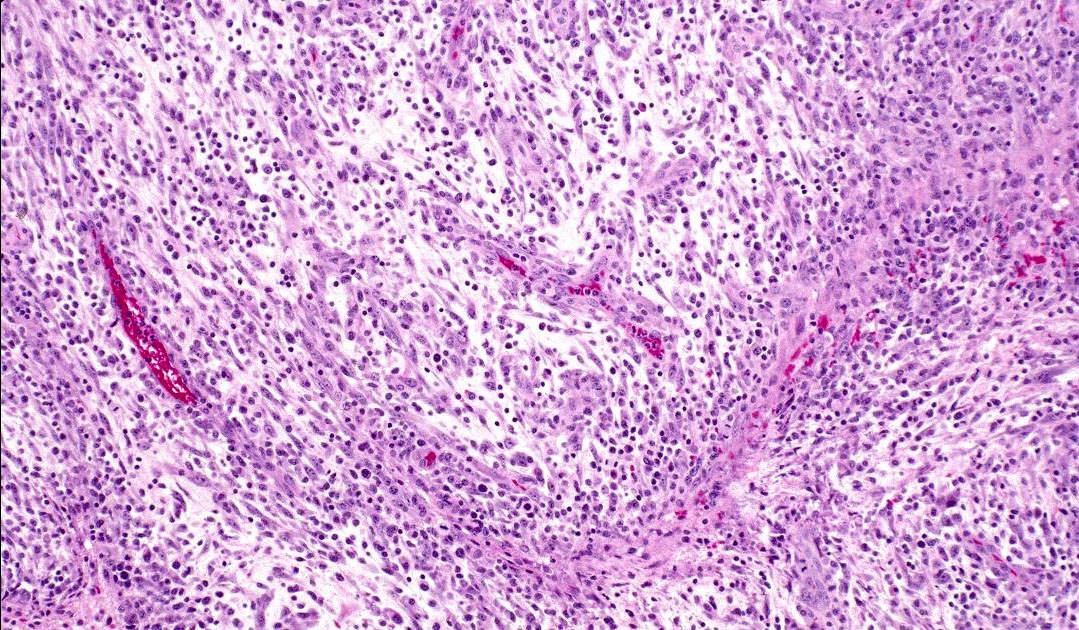
- Broad morphologic spectrum: small to medium sized to large anaplastic cells (Pathology 2020;52:100)
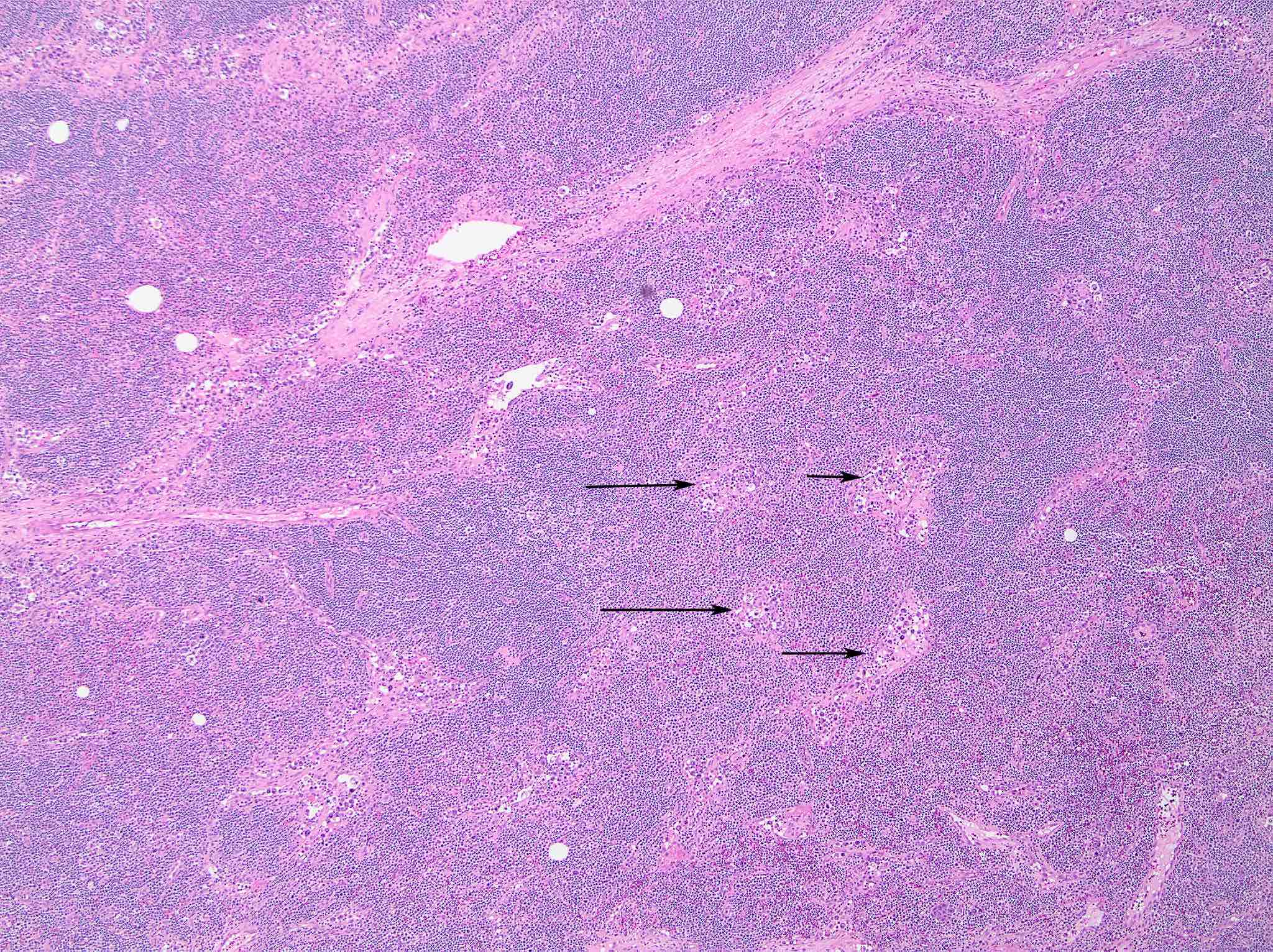
- Infiltration of interfollicular T zones and subcapsular sinuses by neoplastic cells
- Cells show cohesive growth pattern
- Intrasinusoidal infiltration pattern (Blood 2015;126:17)
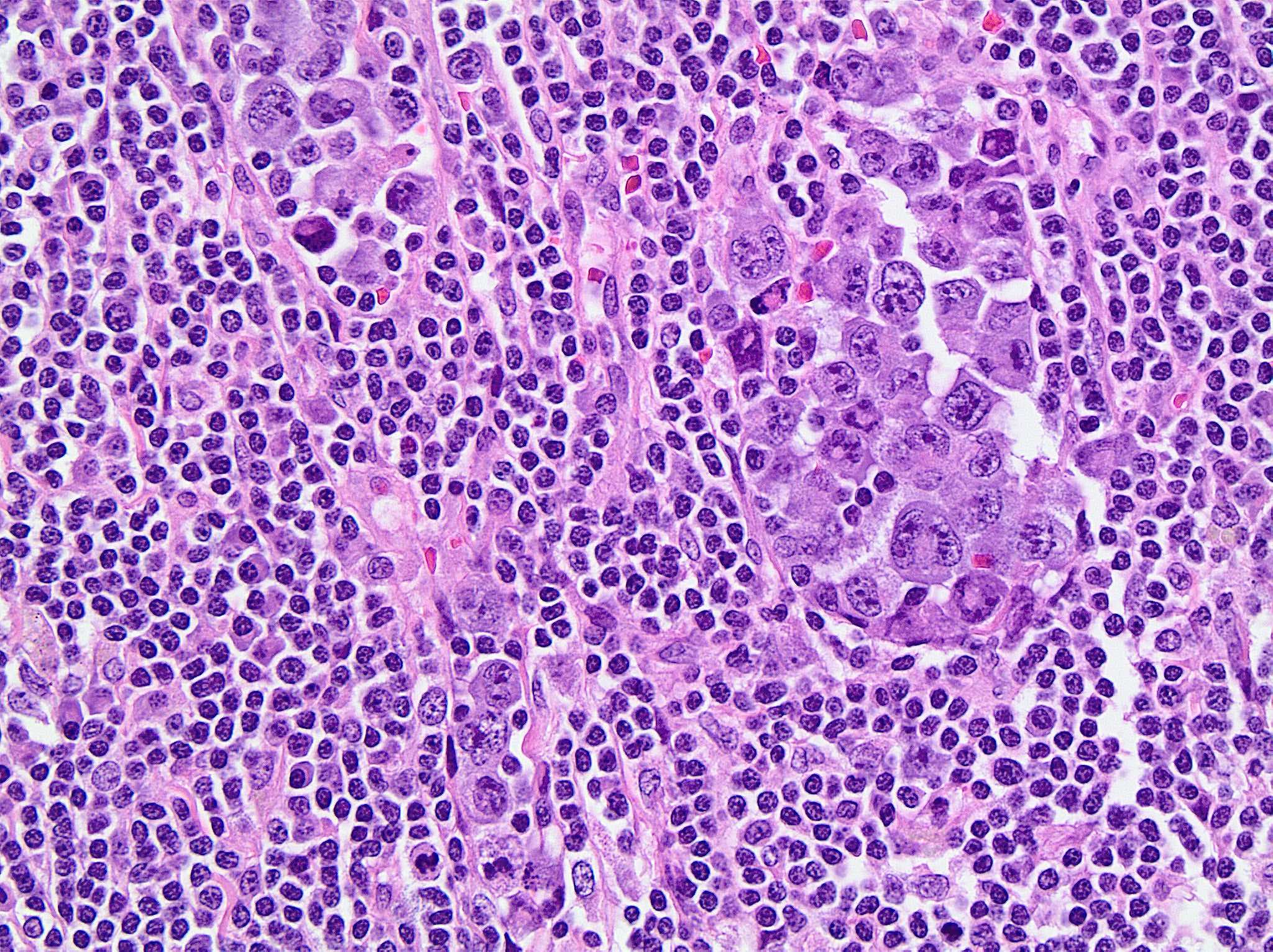
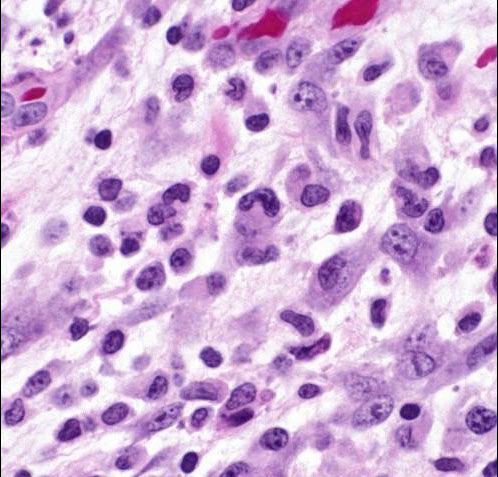
- Anaplastic large cells with abundant cytoplasm, wreath-like or multiple nuclei, open chromatin, multiple nucleoli, perinuclear eosinophilic region (prominent Golgi zone) (Crit Rev Oncol Hematol 2012;83:293)
- Cells with horseshoe / kidney / embryo shaped nuclei are referred to as hallmark cells (Cancers (Basel) 2018;10:E107)
- Occasional nuclear pseudoinclusions (doughnut cells) (Adv Anat Pathol 2015;22:29)
- Brisk mitotic activity
- Sinusoidal involvement may mimic histiocytic neoplasms
- In the lymphohistiocytic variant, neoplastic cells may be masked by abundant histiocytes
- Peripheral distribution of neoplastic cells is common in lymph nodes and other sites
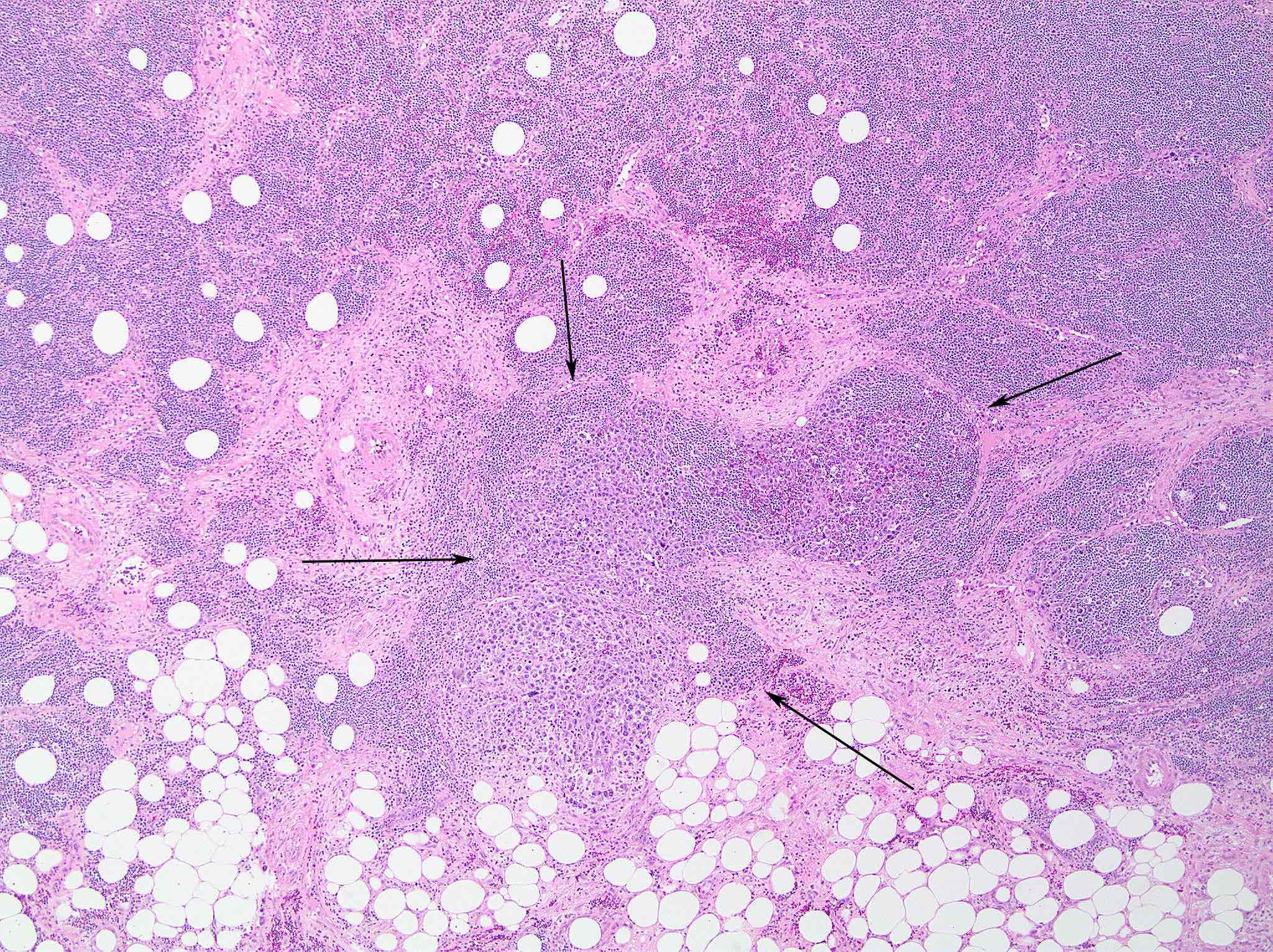
- Bone marrow varies from extensive involvement by tumor cells to only scattered cells that may be overlooked
Morphologic variants
- Lymphohistiocytic (10%) (Histopathology 1990;16:383, Virchows Arch 2008;452:599)
- Numerous histiocytes and small lymphocytes, occasional erythrophagocytosis
- Neoplastic cells tend to cluster around blood vessels
- Small cell (5 - 10%) (Arch Pathol Lab Med 2010;134:1706)
- 25% transform to classic anaplastic large cell lymphoma, usually associated with death within a year; necrosis may predict transformation (Am J Surg Pathol 1999;23:49)
- Often systemic symptoms, often misdiagnosed as peripheral T cell lymphoma, not otherwise specified
- Loss of CD3 is clue to diagnosis and distinction from peripheral T cell lymphoma
- High incidence of marrow involvement but difficult to identify without immunostains
- Leukemic presentation more common in this variant
- Predominantly small cells with irregular nuclei, hallmark cells present (tend to be perivascular), occasional fried egg cells, rare signet ring cells (Arch Pathol Lab Med 2011;135:19)
- Hodgkin-like (1 - 3%) (Am J Surg Pathol 2006;30:223)
- Mimics nodular sclerosis classic Hodgkin lymphoma; capsular fibrosis and fibrotic bands forming cellular nodules
- Mononuclear cells
- Binucleate Reed-Sternberg-like cells and mummified cells may be present
- Eosinophils and neutrophils less common than in classic Hodgkin lymphoma
- Hypocellular (Am J Surg Pathol 2000;24:1537)
- Small cell types may have hypocellular, granulation tissue-like appearance
- Young patients with lymphadenopathy
- Lymphoid cells separated by edematous or fibromyxoid stroma with myofibroblast-like neoplastic cells forming short, sweeping fascicles and histiocytes; occasional large cells with atypical nuclei noted; perivascular cuffing of large cells
- Other patterns described
- Sarcomatoid, giant cell rich and signet ring-like patterns
- Composite pattern (10 - 20%)
- More than one pattern may be seen in a single lymph node
- Relapses may differ morphologically from the original tumor
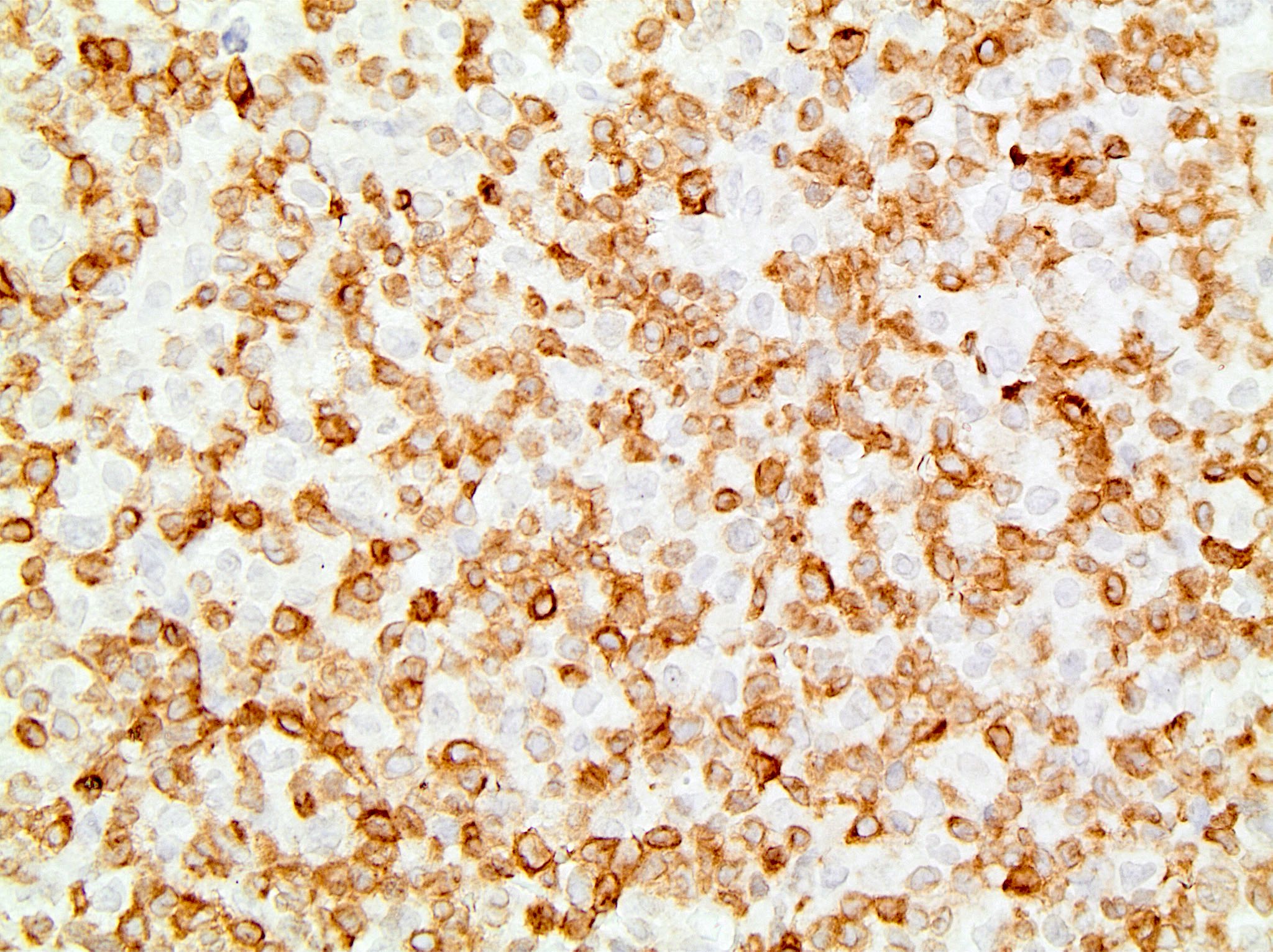
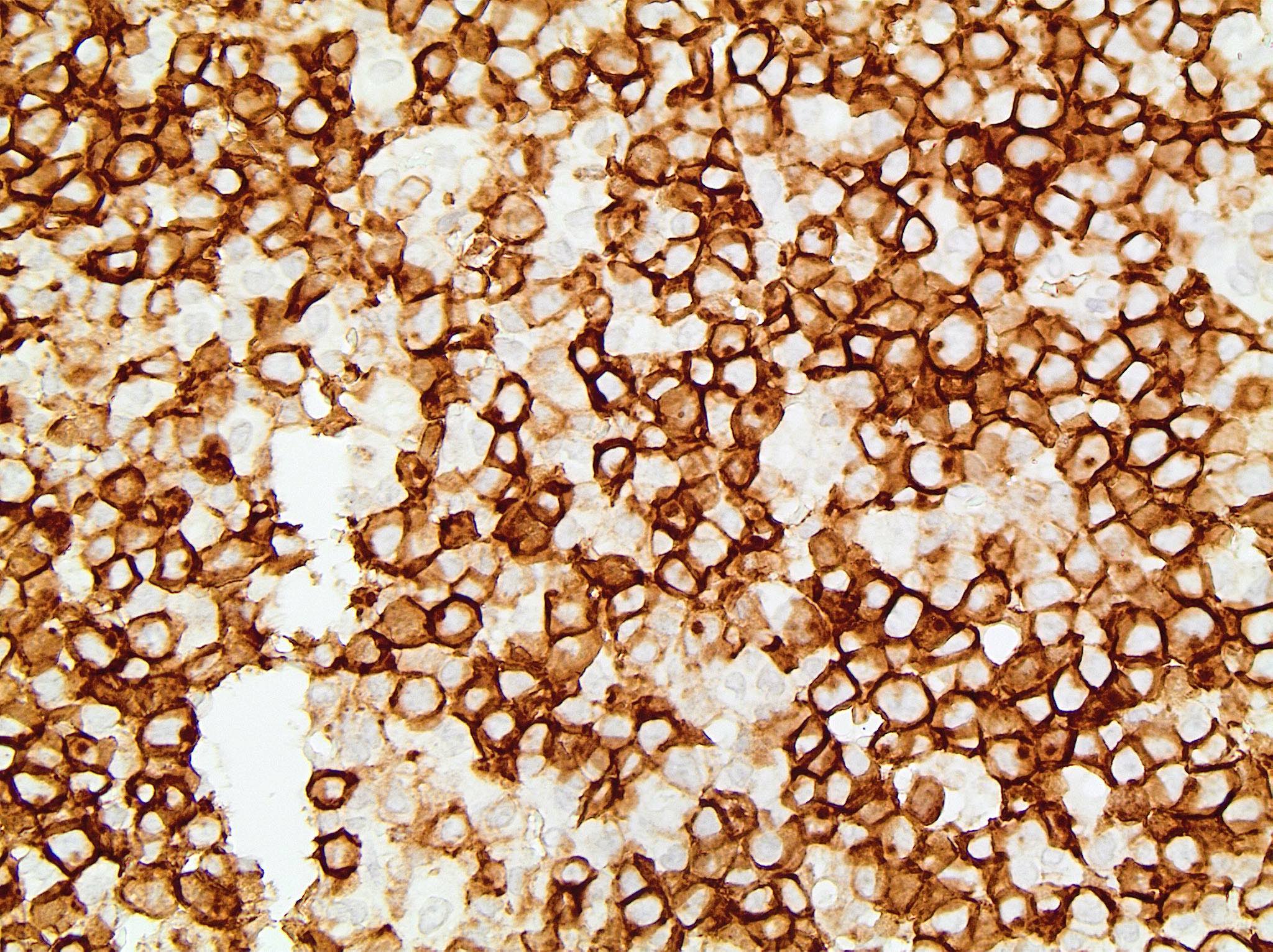
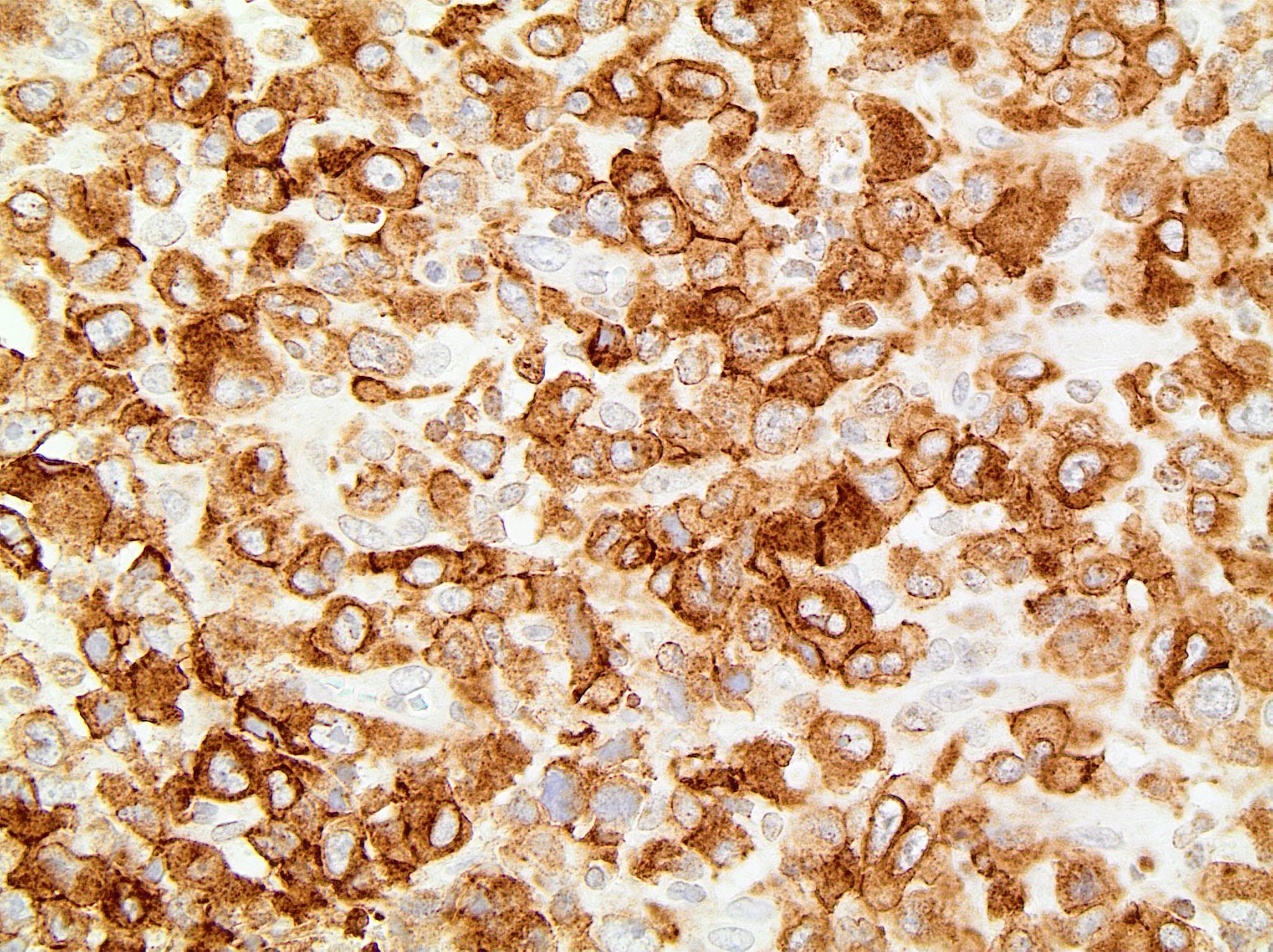
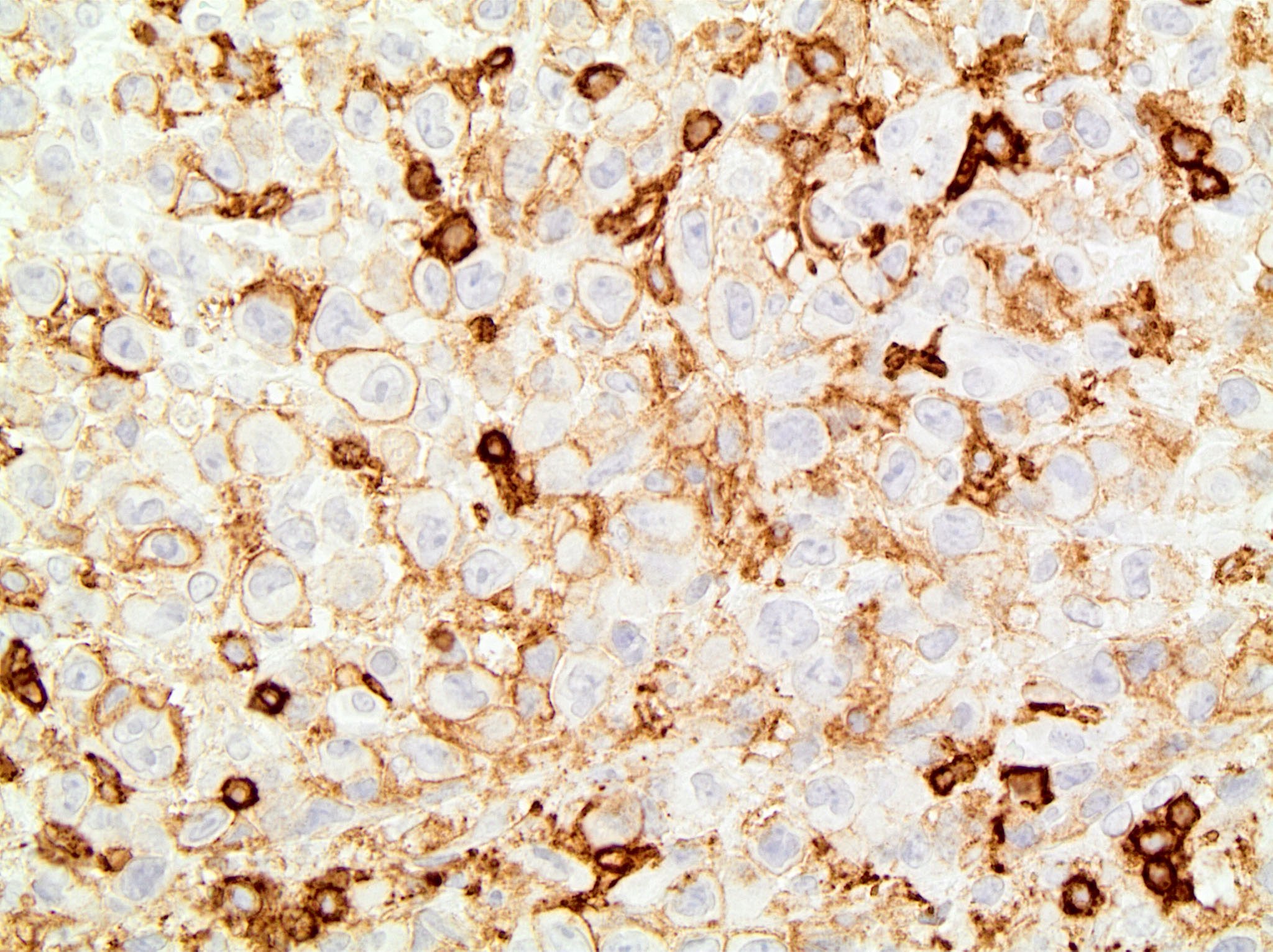
Microscopic (histologic) images
Contributed by Jayalakshmi Balakrishna, M.D., Elaine S. Jaffe, M.D.
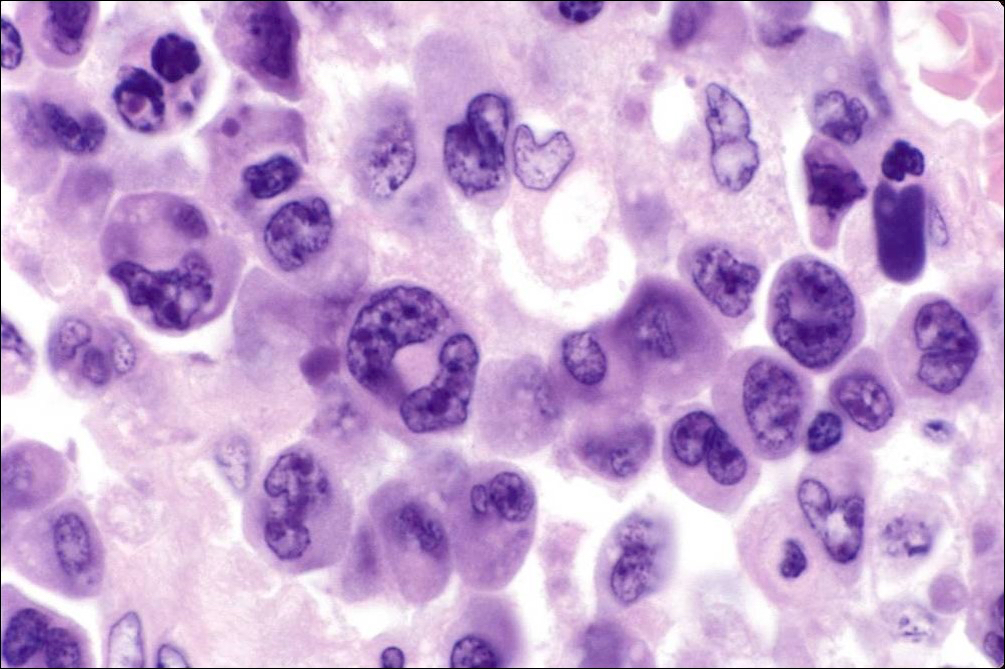
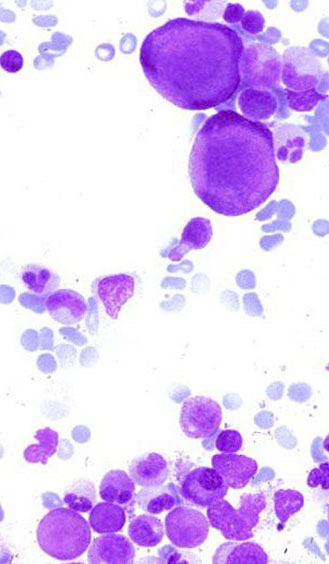
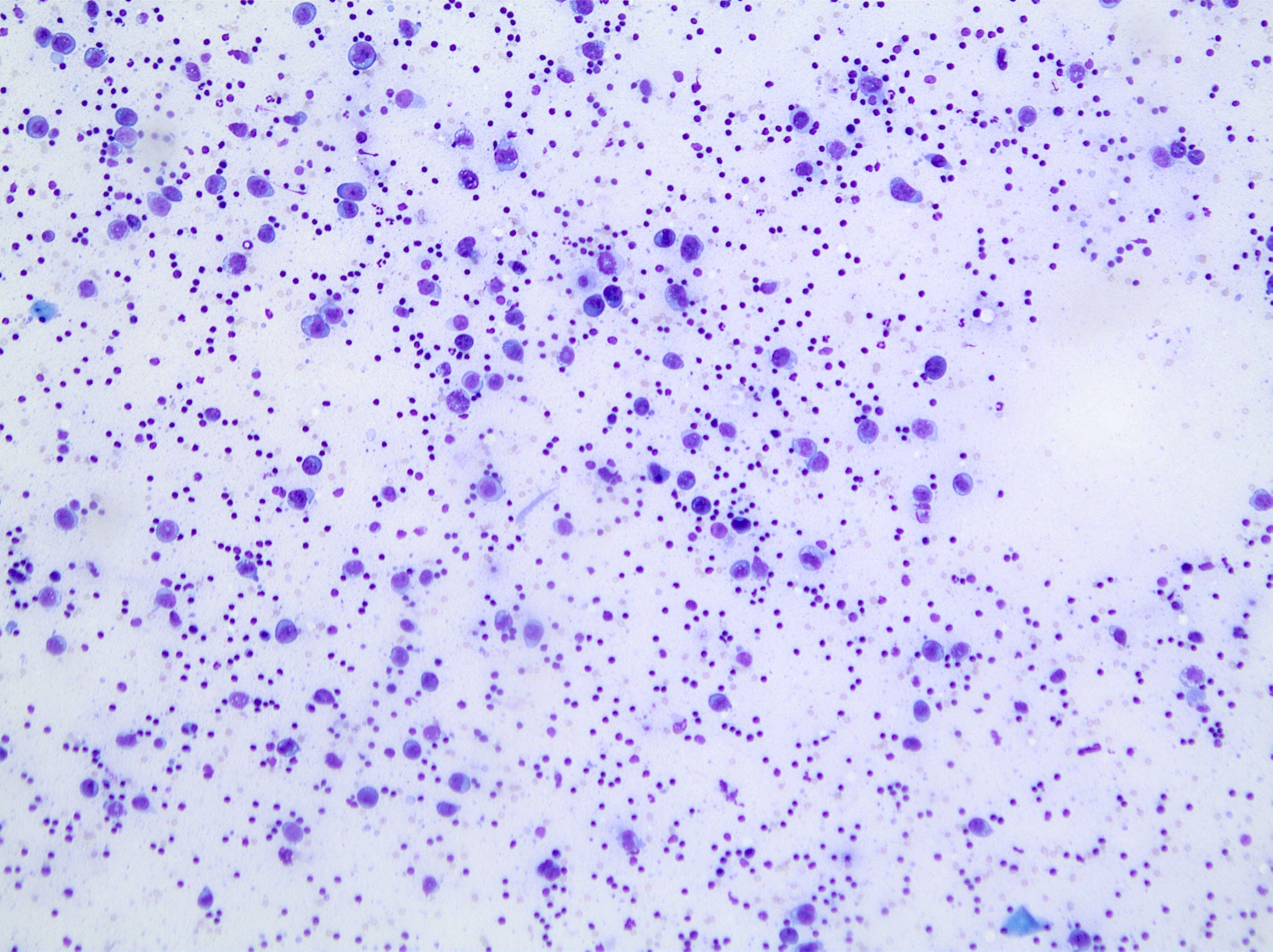
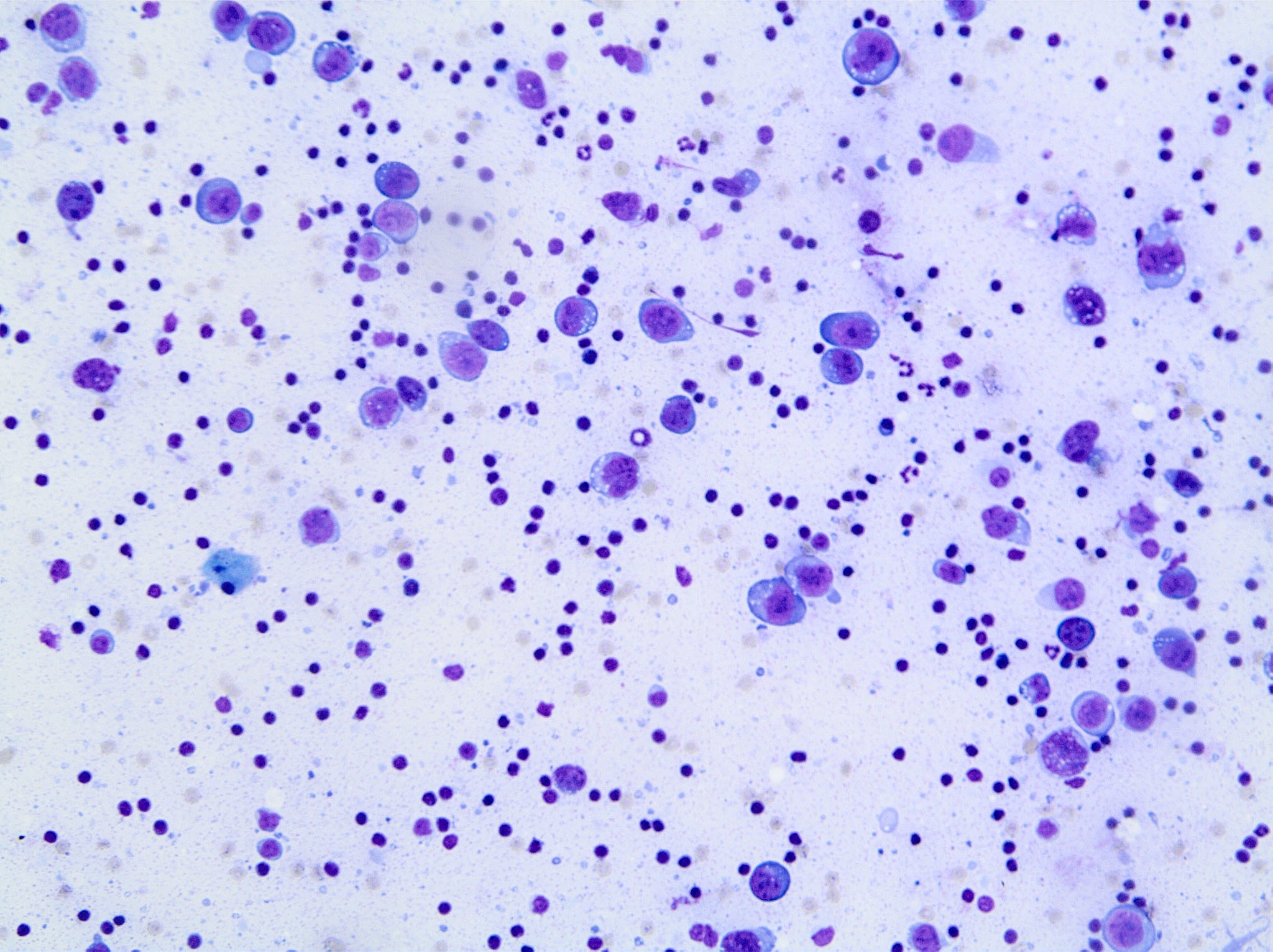
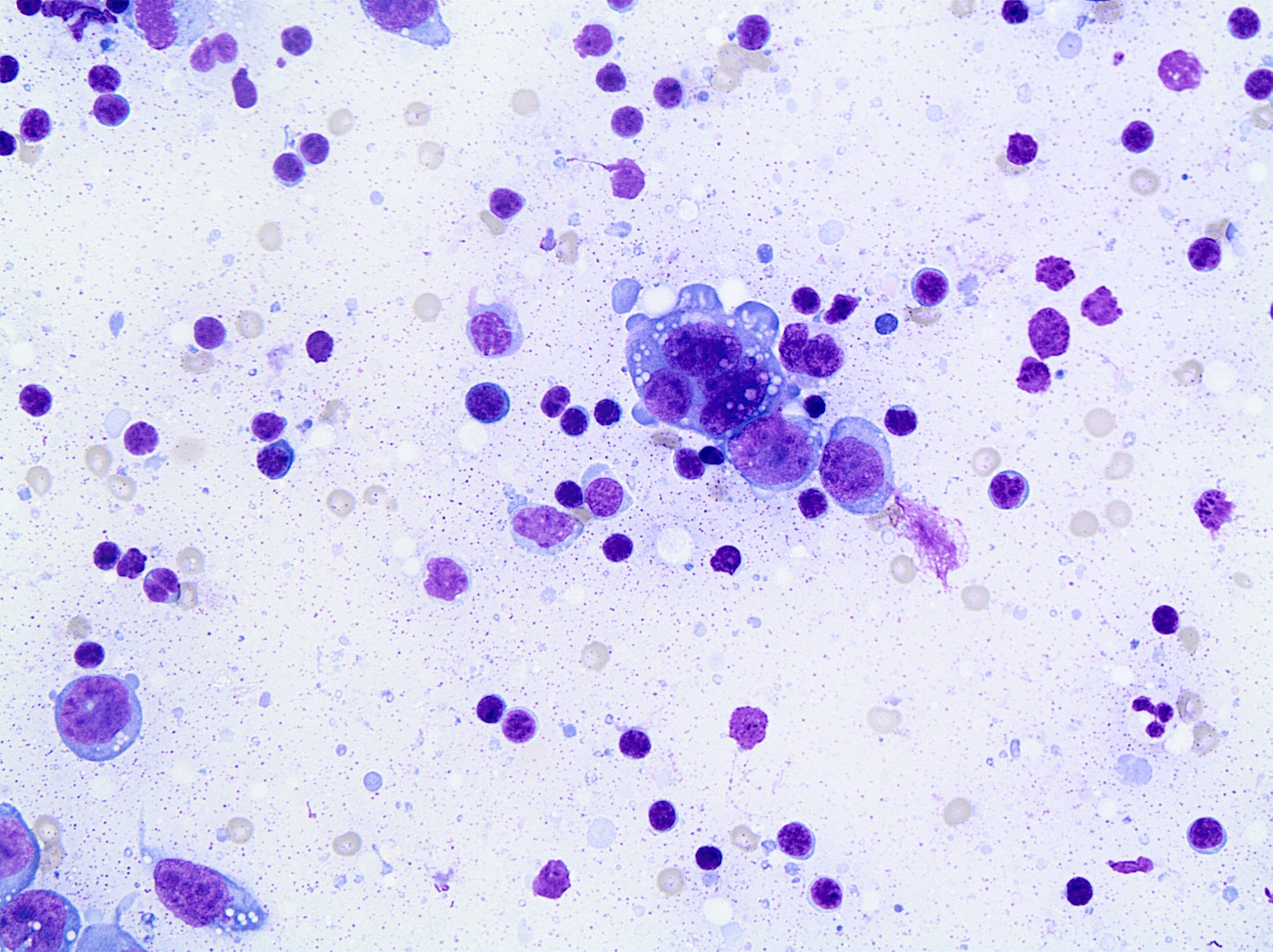
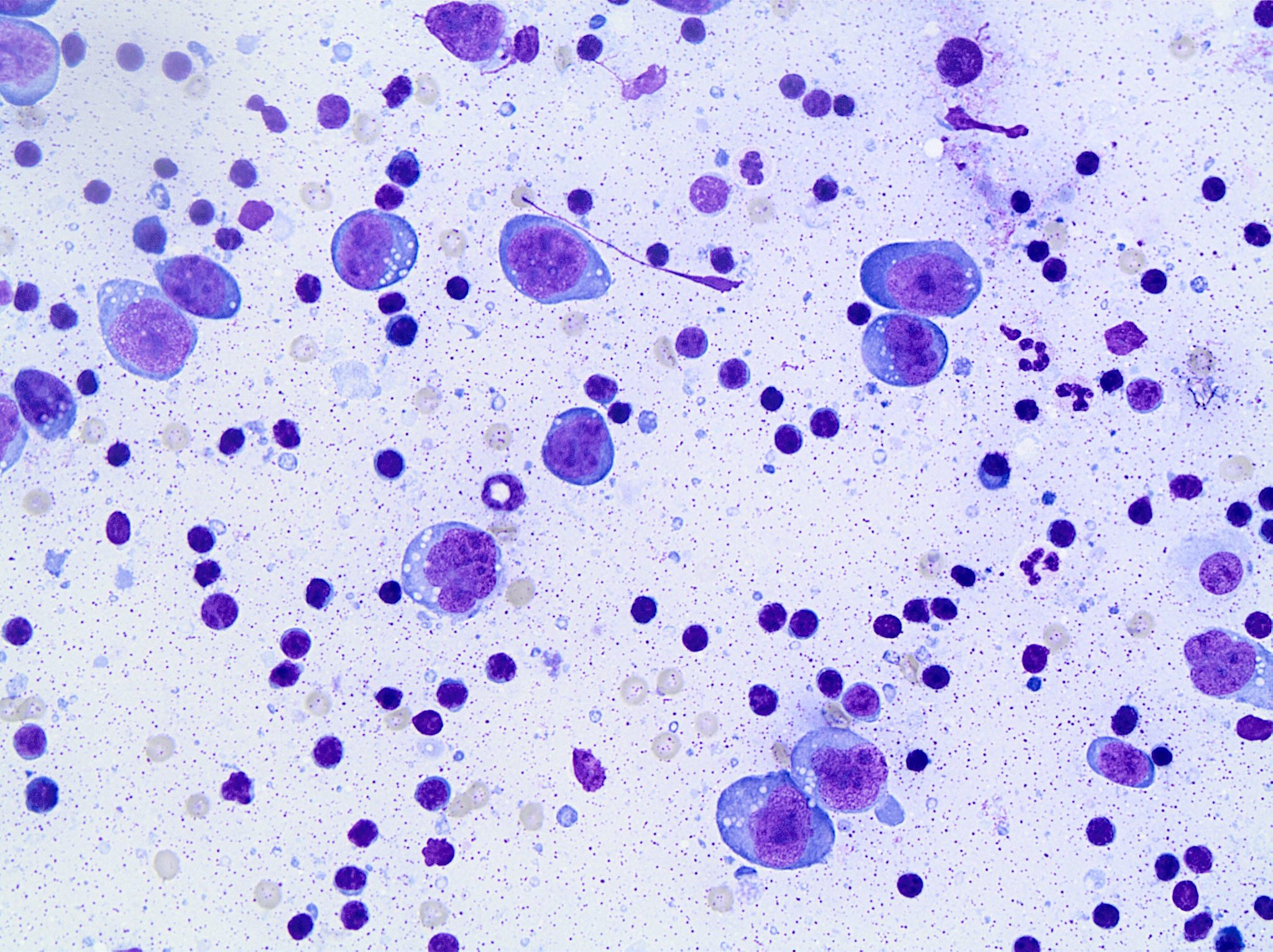
Cytology description
- Deeply basophilic cytoplasm, prominent vacuoles, round or lobate nuclei, prominent nucleoli, clumped chromatin, multinucleation
Cytology images
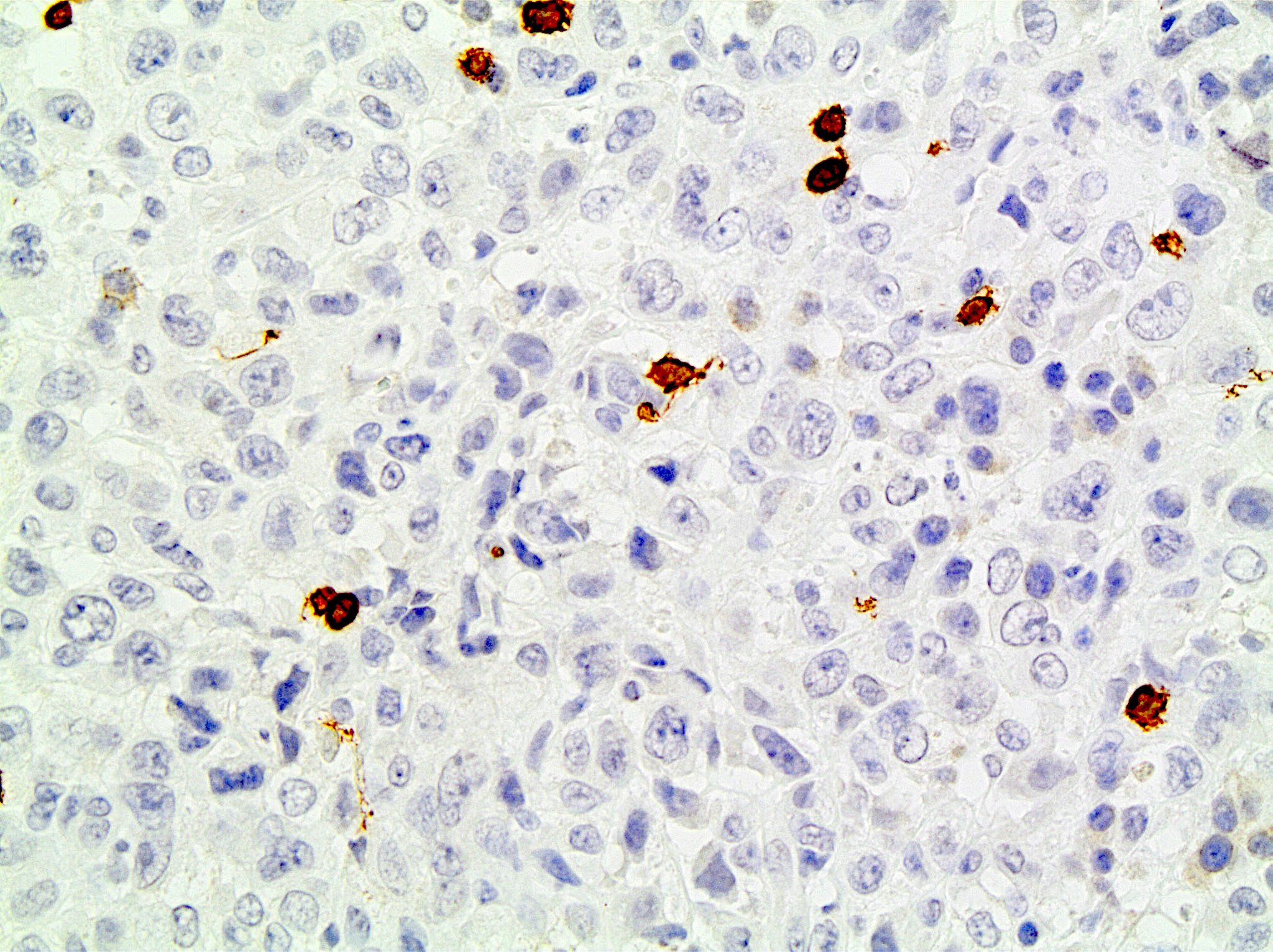
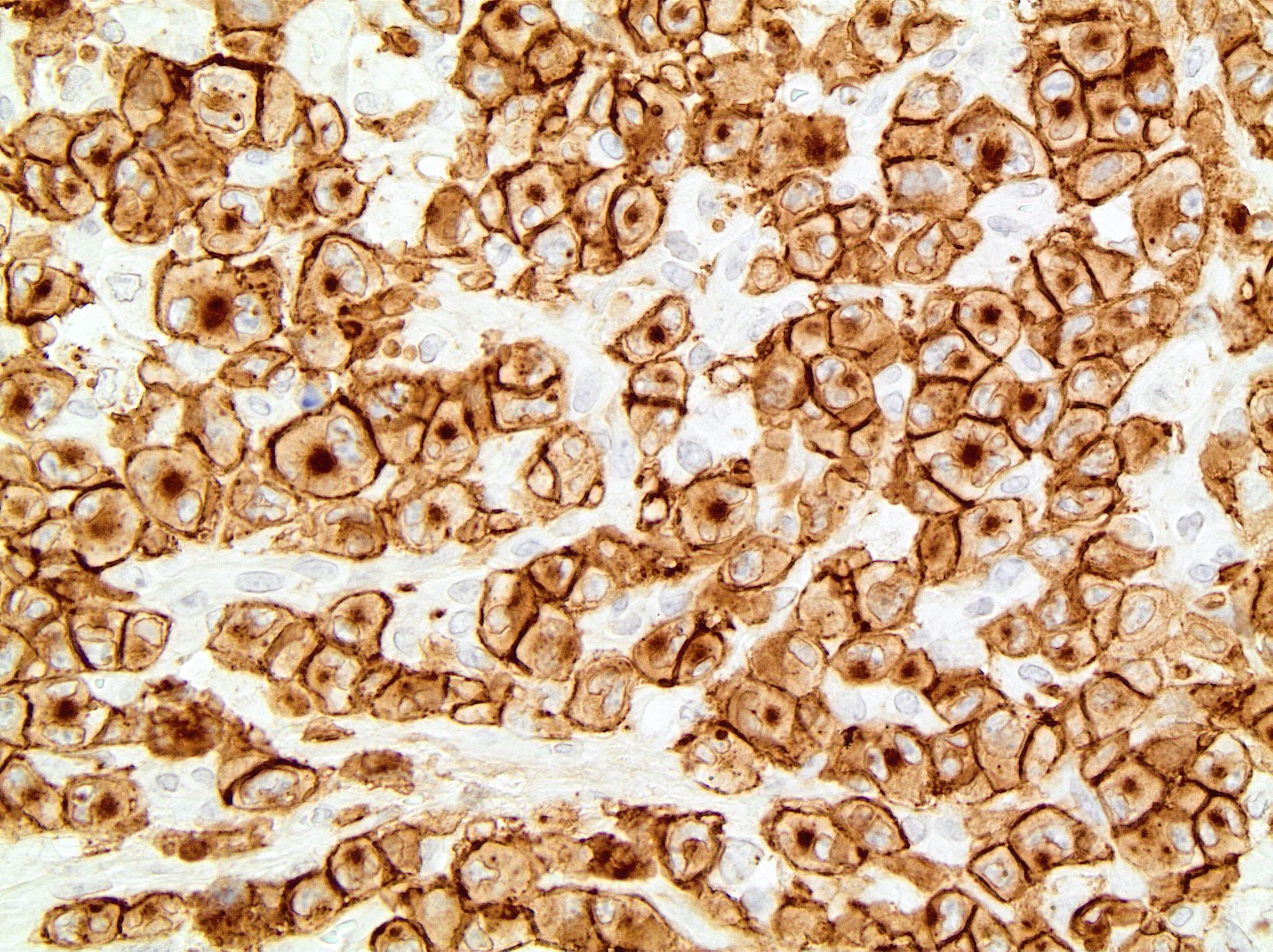
Positive stains
- ALK expression varies by translocation; use monoclonal antibodies (Adv Anat Pathol 2015;22:29)
- CD30 (cytoplasmic and Golgi staining, strongest in large cells), EMA (majority)
- CD2, CD4, CD5 (one is positive in 70% of cases), also TIA1, granzyme B, perforin, CD45, CD45RO, CD61, CD25 (strong)
- Often negative for CD3 (< 25%), CD43, B cell markers (10%)
- Rare CD8, CD15, clusterin, fascin, factor VIII, CD13 (Arch Pathol Lab Med 2000;124:1804)
- Small cell and lymphohistiocytic variants are ALK1+ but cells are not large or anaplastic
- ALK+ anaplastic large cell lymphoma (T or null) is considered a single entity since no other differences can be found and null cell phenotypes show genetic evidence for T cell lineage
Negative stains
Electron microscopy description
- Gold immunolabeling: CD30+ particles in the Golgi complex and cell membranes
- Long, slender, microvillus-like processes (anemone cell tumors, Ultrastruct Pathol 1984;7:143)
- However, most microvillous lymphomas are unusual variants of diffuse large B cell lymphoma (Am J Surg Pathol 1990;14:1047)
- Not used in routine diagnosis
Molecular / cytogenetics description
- Clonal T cell receptor (TCR) gene rearrangement seen in 90% (irrespective of T / null cell phenotype)
- All translocations result in upregulation of ALK protein (Science 1994;263:1281)
- ALK translocation results in activation of the downstream oncogenic transcription factor, STAT3 (Cancer Cell 2015;27:516)
- STAT3 activation regulates availability of hypoxia inducible factors involved in tumor growth and metastasis (Cancer Res 2014;74:6094)
- t(2;5)(p23;q35): ALK and NPM (75 - 85%); translocation of anaplastic lymphoma kinase on chromosome 2 and nucleophosmin gene on chromosome 5; gene product present in nucleus and cytoplasm, can also be detected by RT-PCR (Science 1994;263:1281)
- t(1;2)(q25;p23): tropomyosin 3 (TPM3) and ALK (13%), diffuse cytoplasmic staining with peripheral intensification (Blood 1999;93:3088)
- inv(2)(p23;q35): ALK and ATIC (1%), diffuse cytoplasmic staining (Blood 1998;92:2688)
- t(2;3)(p23;q21): ALK and TRK fused gene (TFG) (< 1%), diffuse cytoplasmic staining (Blood 1999;94:3265)
- t(2;17)(p23;q23): ALK and clathrin heavy chain-like (CLTCL) (< 1%), granular cytoplasmic staining
- t(2;X)(p23;q11-12): ALK and moesin gene (MSN) (< 1%), membrane staining (Hum Pathol 2004;35:1038)
- t(2;19)(p23;p13.1): ALK and nonmuscular tropomyosin gene (TPM4) (< 1%), diffuse cytoplasmic staining
- t(2;22)(p23;q11.2): ALK and myosin heavy chain 9 gene (MYH9) (< 1%), diffuse cytoplasmic staining (Genes Chromosomes Cancer 2003;37:427)
- t(2;17)(p23;q25): ALK and ALK lymphoma oligomerization partner (ALO17) (< 1%), diffuse cytoplasmic staining
- Secondary genetic alterations: -4, del11q, del13q, +7, +17p, +17q (different from anaplastic large cell lymphoma, ALK negative, Br J Haematol 2008;140:516)
- ALK immunohistochemistry, FISH and RT-PCR results are comparable (Am J Surg Pathol 1999;23:1386)
Sample pathology report
- Lymph node, right inguinal, excisional biopsy:
- Anaplastic large cell lymphoma, ALK positive
Differential diagnosis
- ALK negative anaplastic large cell lymphoma:
- ALK positive diffuse large B cell lymphoma with immunoblastic / plasmablastic features:
- Pleomorphic carcinoma:
- Hodgkin lymphoma:
- Lacks cohesive growth pattern, may have fewer neoplastic cells
- CD15+, PAX5+, ALK-, EMA- (Am J Clin Pathol 2007;127:707)
- Lymphomatoid granulomatosis:
- Angiocentric, has a background of reactive lymphocytes and histiocytes, EBV+
- Histiocytic sarcoma:
- Nonneoplastic disorders with atypical CD30+ cells
- Rhabdomyosarcoma and inflammatory myofibroblastic tumor:
Additional references
Board review style question #1
Board review style answer #1
D. CD30. Cytoplasmic stain with Golgi zone accentuation.
Comment Here
Reference: Anaplastic large cell lymphoma, ALK positive
Comment Here
Reference: Anaplastic large cell lymphoma, ALK positive
Board review style question #2
What is the downstream genetic pathway involved in the pathogenesis of anaplastic large cell lymphoma?
- MAPK
- NFκB
- STAT3
- Wnt
Board review style answer #2