Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Flow cytometry description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Balakrishna J, Jaffe ES. Nodular lymphocyte predominant B cell lymphoma / nodular lymphocyte predominant Hodgkin lymphoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lymphomanonBNLPHL.html. Accessed April 2nd, 2025.
Definition / general
- Nodular lymphocyte predominant Hodgkin lymphoma (NLPHL) is a B cell neoplasm characterized by scattered clonal cells (termed lymphocyte predominant [LP] cells) in a background of reactive lymphocytes and histiocytes, with a mostly nodular and sometimes diffuse growth pattern (Am J Surg Pathol 1994;18:526, Oncologist 2009;14:739, Clin Lymphoma Myeloma Leuk 2014;14:261)
- LP cells (originally termed lymphocytic and histiocytic cells) have enlarged nuclei with lobular contours and variably prominent nucleoli
Essential features
- LP cells initially arise within altered follicles
- Background small B cells are numerous in early phases and decrease with time
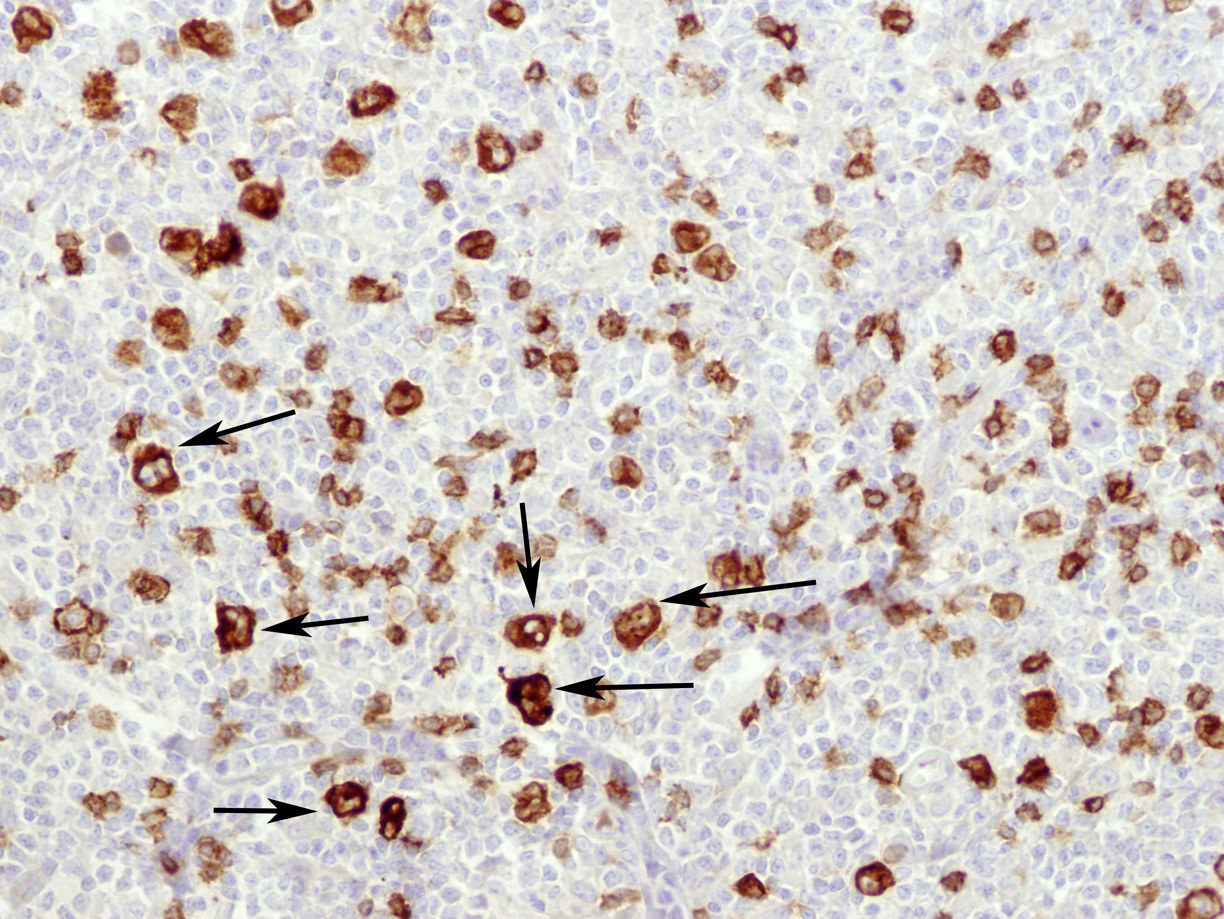
- LP cells rosetted by CD4+, PD-1+ T cells
- Number of background T cells increases over time, along with the loss of the nodular pattern
- Diffuse pattern resembles T cell / histiocyte rich large B cell lymphoma
- LP cells display a germinal center B cell phenotype: CD20, PAX5, OCT2 and BCL6 are positive, CD10 is negative
- CD30 is variably positive and if positive, is usually weak
- Most cases are negative for CD15
Terminology
- Fifth edition of the World Health Organization Classification of Haematolymphoid Tumours: nodular lymphocyte predominant Hodgkin lymphoma (Leukemia 2022;36:1720)
- International Consensus Classification 2022: nodular lymphocyte predominant B cell lymphoma (Blood 2022;140:1229)
- Hodgkin paragranuloma (obsolete)
ICD coding
- ICD-10
- C81.0 - nodular lymphocyte predominant Hodgkin lymphoma
- C81.00 - nodular lymphocyte predominant Hodgkin lymphoma, unspecified site
- C81.01 - nodular lymphocyte predominant Hodgkin lymphoma, lymph nodes of head, face and neck
- C81.02 - nodular lymphocyte predominant Hodgkin lymphoma, intrathoracic lymph nodes
- C81.03 - nodular lymphocyte predominant Hodgkin lymphoma, intra-abdominal lymph nodes
- C81.04 - nodular lymphocyte predominant Hodgkin lymphoma, lymph nodes of axilla and upper limb
- C81.05 - nodular lymphocyte predominant Hodgkin lymphoma, lymph nodes of inguinal region and lower limb
- C81.06 - nodular lymphocyte predominant Hodgkin lymphoma, intrapelvic lymph nodes
- C81.07 - nodular lymphocyte predominant Hodgkin lymphoma, spleen
- C81.08 - nodular lymphocyte predominant Hodgkin lymphoma, lymph nodes of multiple sites
- C81.09 - nodular lymphocyte predominant Hodgkin lymphoma, extranodal and solid organ sites
- C81 - Hodgkin lymphoma
Epidemiology
- ~5 - 10% of all Hodgkin lymphoma cases
- Annual incidence of ~1/830,000
- M:F = 3:1; median age at presentation is 30 - 40 years (Orphanet: Nodular Lymphocyte Predominant Hodgkin Lymphoma [Accessed 28 May 2024])
Sites
- Peripheral lymph nodes, generally cervical, axillary, inguinal
- Mesenteric lymph nodes can be affected (Clin Lymphoma Myeloma 2009;9:206)
- Mediastinal involvement is rare (Haematologica 2015;100:1579)
Pathophysiology
- LP cells are of germinal center B cell origin, with evidence of somatic hypermutation of IG genes (J Exp Med 2008;205:2251, Annu Rev Pathol 2009;4:151)
Etiology
- B cell neoplasm that is distinct from classic Hodgkin lymphoma (Clin Lymphoma Myeloma 2009;9:206, Orphanet: Nodular Lymphocyte Predominant Hodgkin Lymphoma [Accessed 28 May 2024])
- Some cases show overlap with T cell / histiocyte rich large B cell lymphoma
- Recurrent mutations in SGK1, DUSP2 and JUNB (Leukemia 2016;30:844)
- Familial form is rare (Am J Hematol 2013;88:719, J Clin Oncol 2013;31:938)
Clinical features
- Usually presents as localized disease; usually stage I / II (70 - 80%); 20% may present with advanced stage disease (Oncologist 2009;14:739)
- Advanced stage disease treated as an aggressive B cell lymphoma (Blood 2017;130:472)
- Presents with peripheral lymphadenopathy
- Rarely, mediastinal or bone marrow involvement; often a long history of localized disease (Am J Surg Pathol 2004;28:489)
- M > F
- Wide age range; may present in children
- B symptoms are uncommon (5 - 10%)
- Late recurrences are more common than in classic Hodgkin lymphoma (Cancer 2010;116:631)
Diagnosis
- Biopsy of the involved lymph node with immunohistochemistry
- LP cells in a background of small lymphocytes admixed with histiocytes
- LP cells: CD45+, CD20+, PAX5+ OCT+, BCL6+, CD15-, CD30 variable; a subset is positive for IgD, mainly in young men
- Background: small B cells and T cells are positive for CD4, PD-1 and partial CD57
- Variant histological patterns have prognostic relevance (Am J Surg Pathol 2003;27:1346)
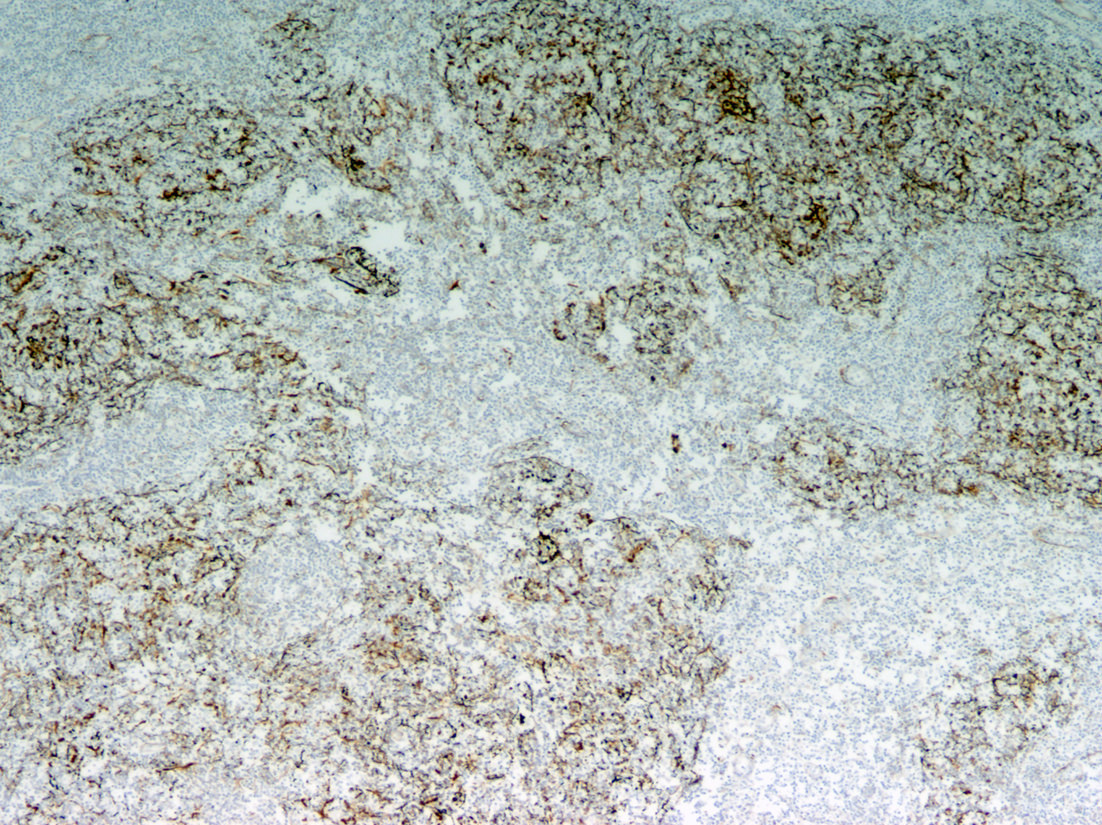
- Expanded follicular dendritic cell meshwork within nodular areas; follicular dendritic cell meshwork is lost with diffuse growth
- With progression to diffuse growth pattern, histology resembles T cell / histiocyte rich large B cell lymphoma
Prognostic factors
- Excellent prognosis; remission rate of 90 - 100% after primary therapy and overall 10 year survival rates > 90% in limited stage disease (Orphanet: Nodular Lymphocyte Predominant Hodgkin Lymphoma [Accessed 28 May 2024])
- 3 - 5% transform to diffuse large B cell lymphoma and tumor cells in each may be clonally related (Am J Clin Pathol 2001;116:506, Cancer 2010;116:631, Histopathology 2011;59:1194)
- Splenic involvement is associated with inferior 10 year survival rates (Blood 2014;123:3567)
- Stage III / IV disease including extranodal and bone marrow involvement is associated with aggressive disease (Am J Surg Pathol 2004;28:489)
- Diffuse T cell rich pattern may be associated with recurrence (Am J Surg Pathol 2003;27:1346)
Case reports
- 14 year old boy with a nonproductive cough, weight loss, fatigue and malaise (J Pediatr Hematol Oncol 2018;40:e454)
- 15 year old boy with Li-Fraumeni syndrome (J Pediatr Hematol Oncol 2018;40:e195)
- 27 year old Mediterranean man and 38 year old Caucasian man treated by radioimmunotherapy for first relapse of their nodular lymphocyte predominant Hodgkin lymphoma (Eur J Haematol 2018;101:415)
- 33 year old woman diagnosed with stage IIIA nodular lymphocyte predominant Hodgkin lymphoma (Leuk Lymphoma 2016;57:1974)
- 35 year old man with T cell histiocyte rich large B cell lymphoma-like transformation of nodular lymphocyte predominant Hodgkin lymphoma (Case Rep Oncol Med 2018;2018:6137454)
- 40 year old White woman with swelling of the left upper eyelid (Ophthalmic Plast Reconstr Surg 2017;33:e29)
- 43 year old woman with abnormal vaginal bleeding for 1 year (Clin Case Rep 2015;3:349)
- 48 year old woman with gamma heavy chain disease (Arch Pathol Lab Med 2001;125:803)
- 51 year old man with lower limb rash, fatigue and bulky abdominopelvic lymphadenopathy (Case Rep Hematol 2018;2018:4312594)
- 54 year old asymptomatic man with a 2 cm polypoid, nonobstructing, ulcerated lesion inside the ileocecal valve detected on routine screening colonoscopy (Case Rep Pathol 2017;2017:5981013)
- 65 year old woman with a right axillary swelling (Diagn Cytopathol 2017;45:262)
- 65 year old man with diffuse large B cell lymphoma stage IIa with splenomegaly, transformed from a nodular lymphocyte predominant Hodgkin lymphoma (Anticancer Res 2018;38:5363)
- 73 year old man with a 2 month history of a painless left laterocervical mass (Int J Surg Pathol 2015;23:419)
Treatment
- Recent approaches to treatment in early stage disease have included more conservative therapy such as localized radiation therapy, excision or observation (Semin Hematol 2016;53:190, Blood Adv 2019;3:1356)
- Rituximab may be useful for relapses / refractory cases; combination chemotherapy and combined therapeutic modalities are used in advanced stage disease, with treatment regimens similar to diffuse large B cell lymphoma (Blood 2008;111:109, Blood 2019;133:2121, Br J Haematol 2019;184:17, Clin Lymphoma Myeloma Leuk 2017;17:e75, Am J Hematol 2018;93:704, Haematologica 2015;100:1579, Blood 2017;130:472, Cancers (Basel) 2023;15:3310)
Gross description
- Involved lymph node is enlarged
- Firm, fleshy mass
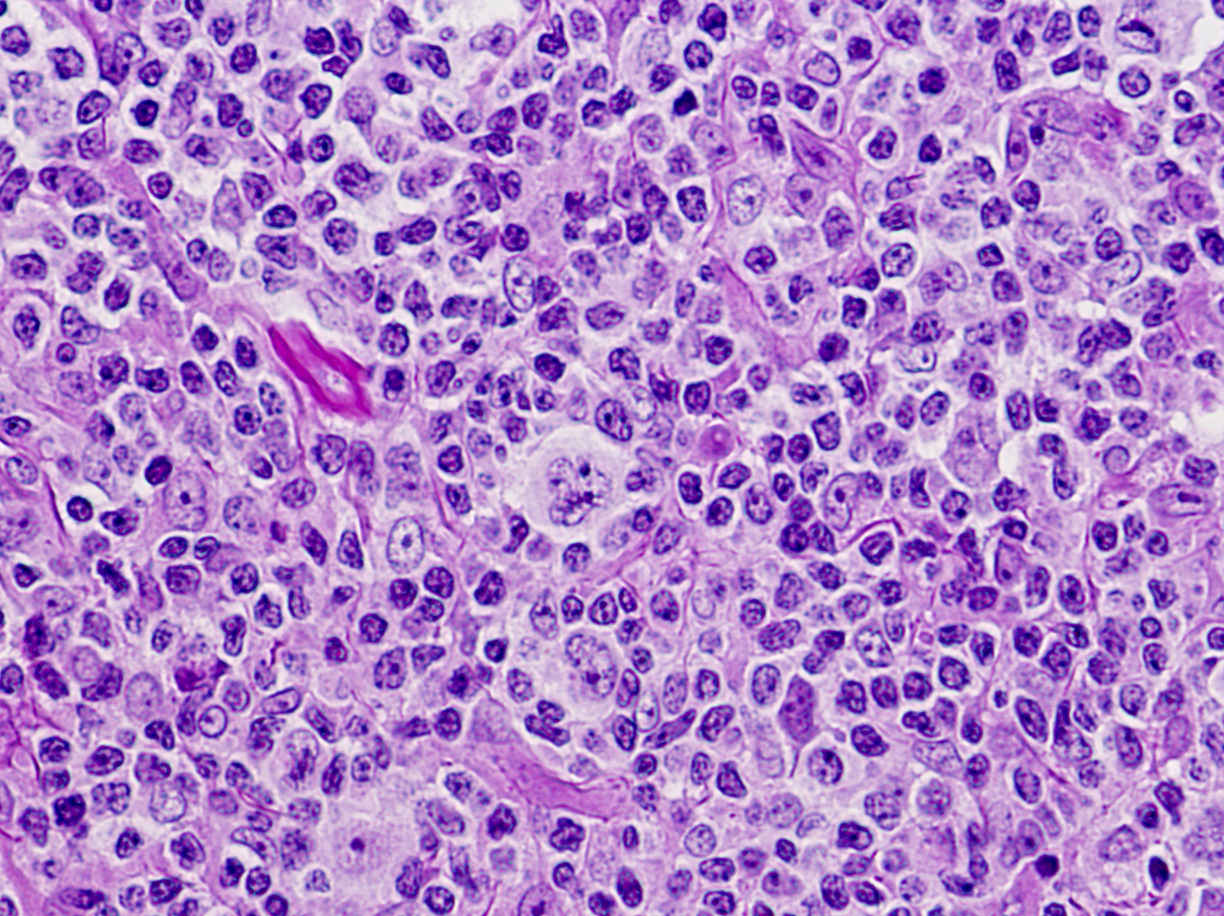
Microscopic (histologic) description
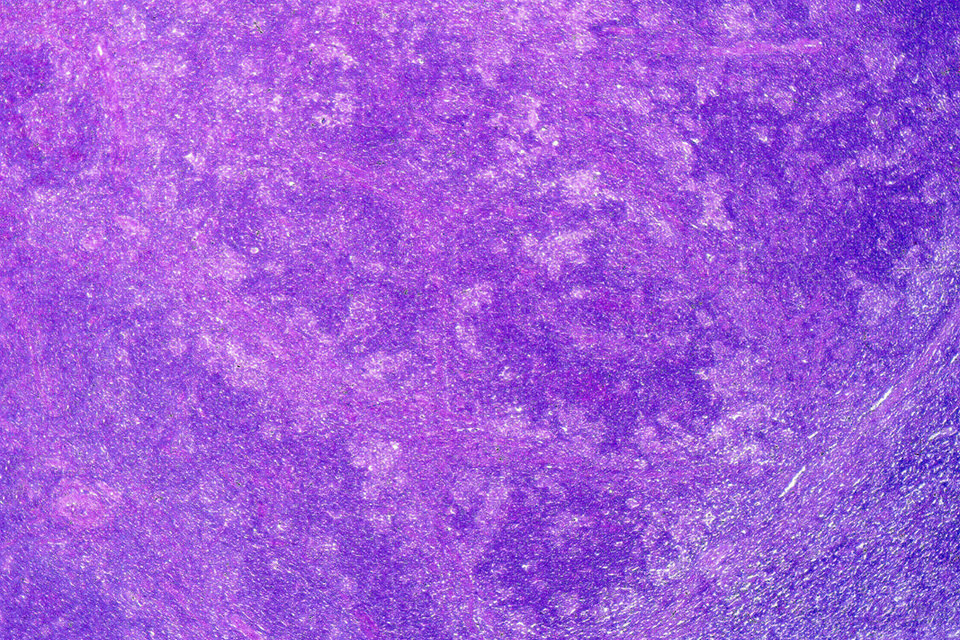
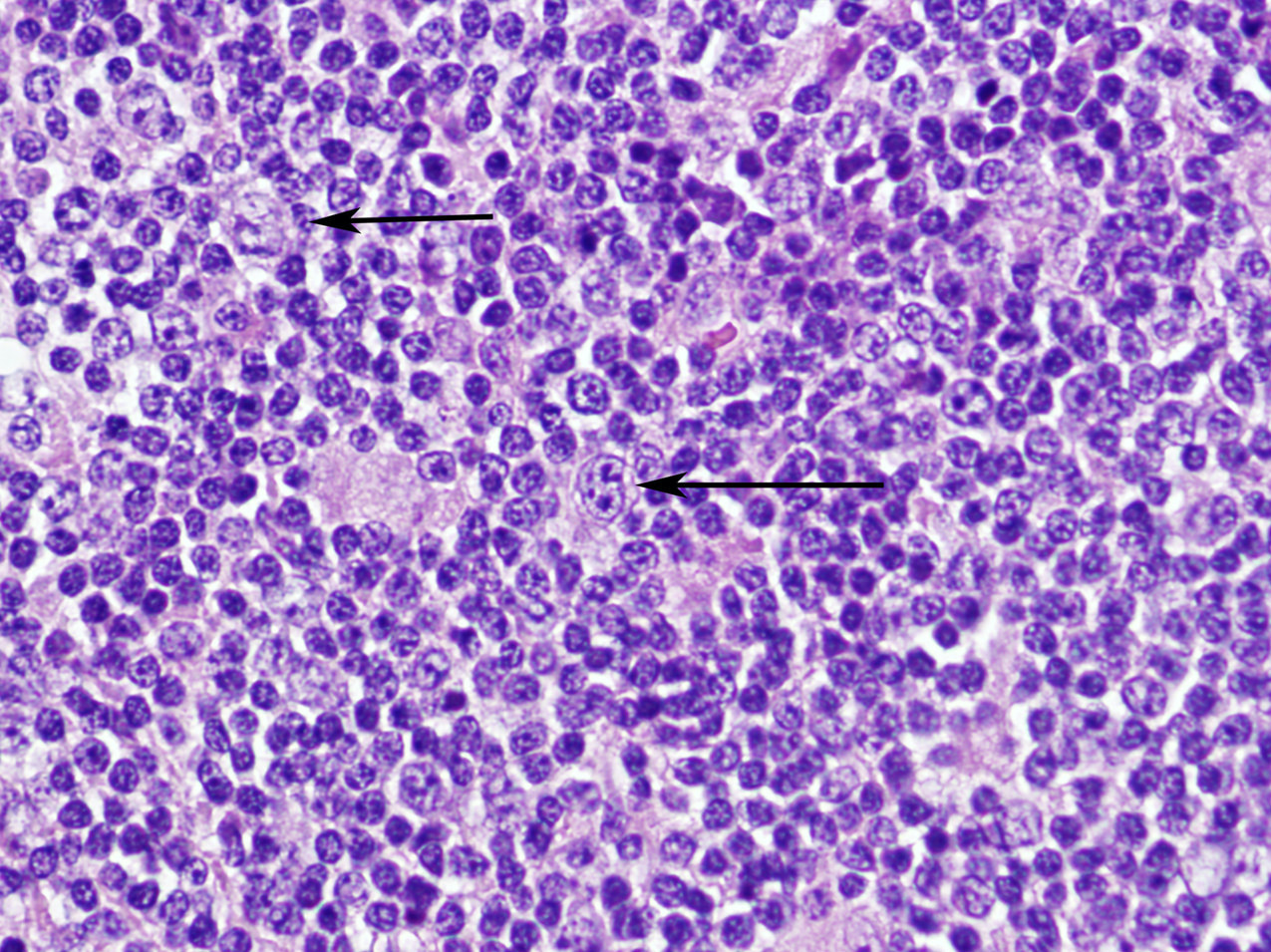
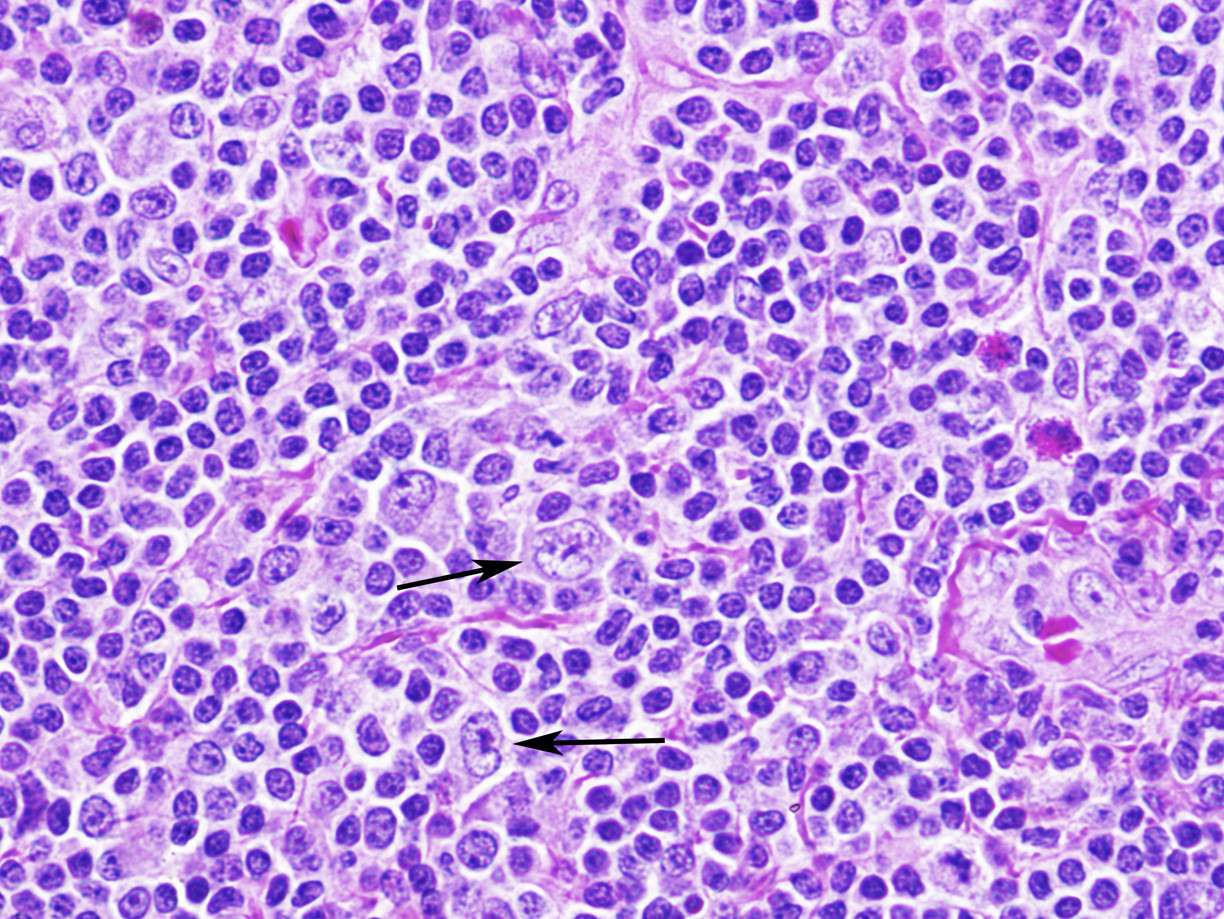
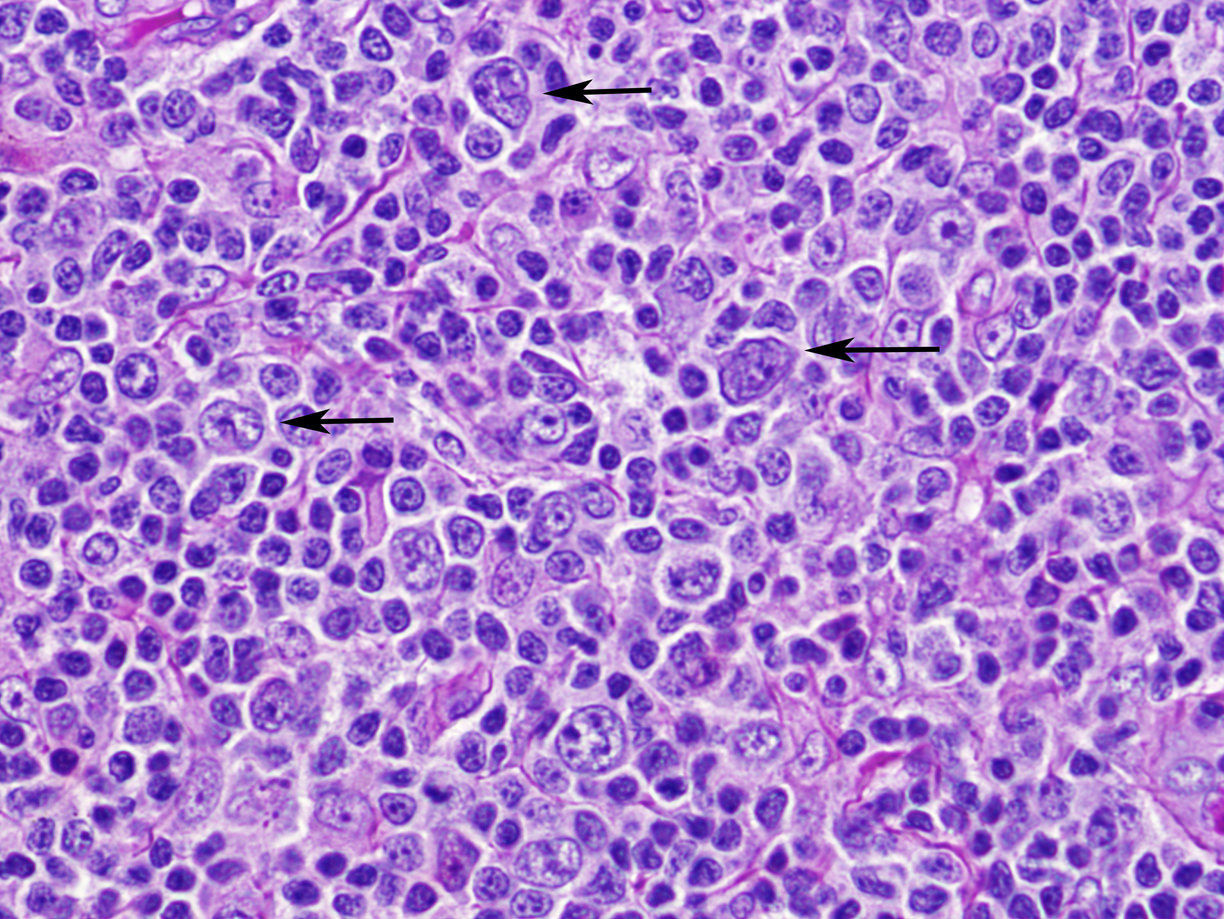
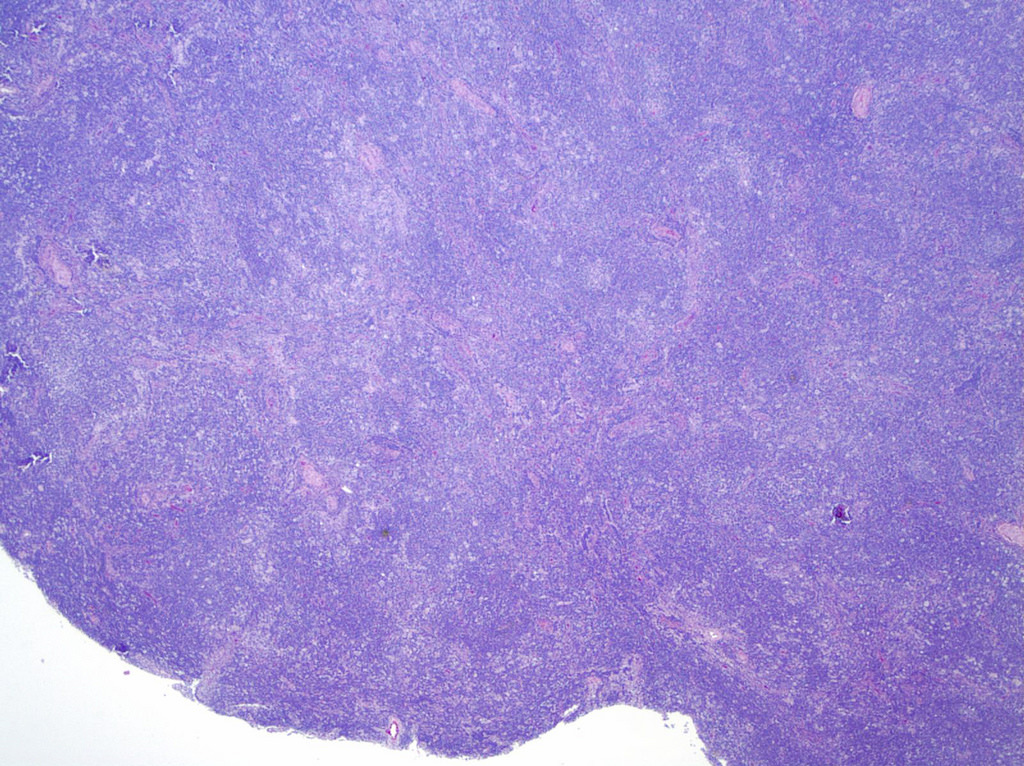
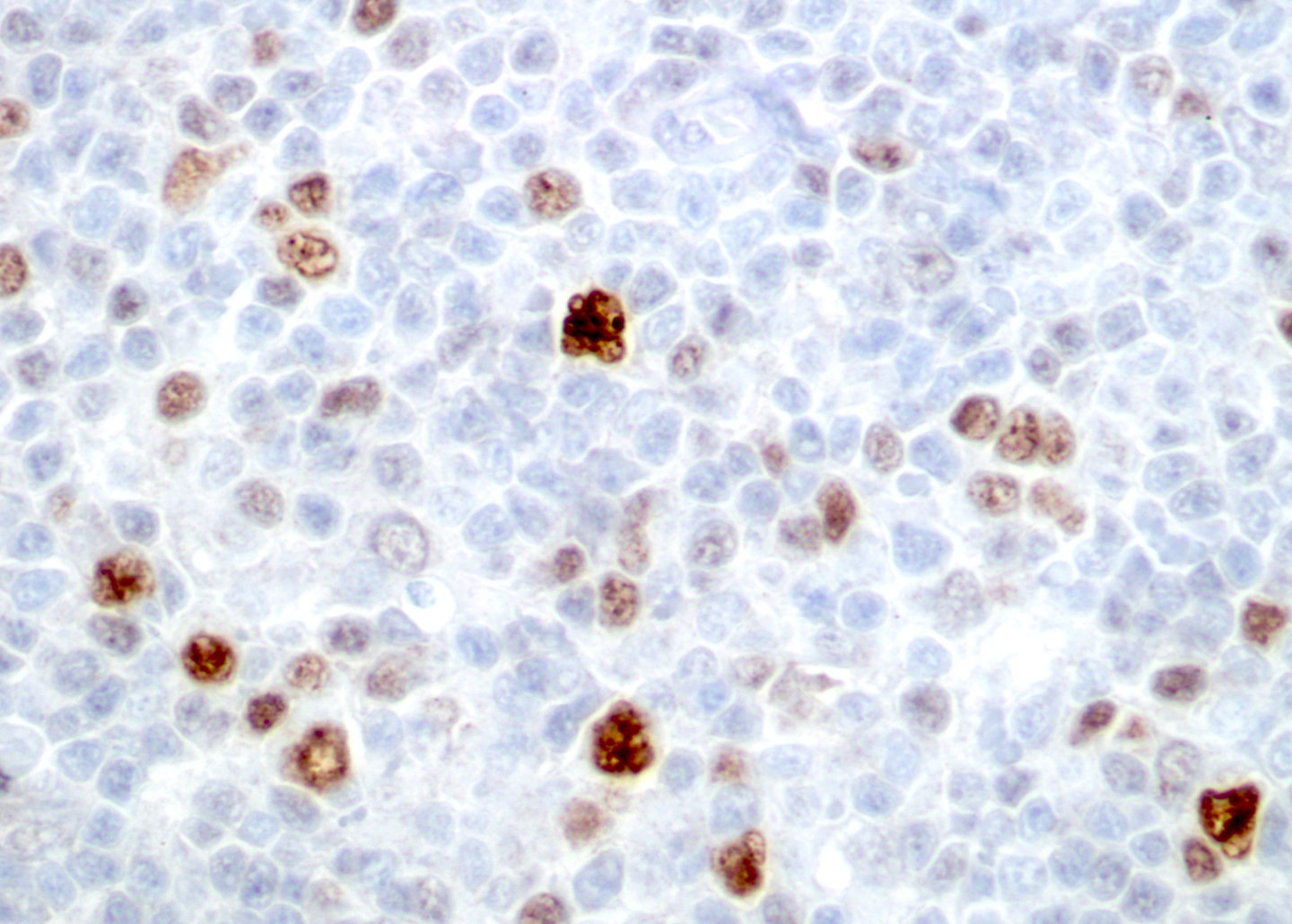
- Usually total replacement of nodal architecture by expansive vague nodules of small lymphocytes with sparse, relatively large tumor cells exhibiting multilobulated or round nuclei, thin nuclear membrane, finely granular chromatin and variable small nucleoli (popcorn cells) (Semin Hematol 2016;53:190, Clin Lymphoma Myeloma 2009;9:206)
- May have a rim of normal lymph node
- Large cells are called LP cells; previously known as lymphocytic and histiocytic cells
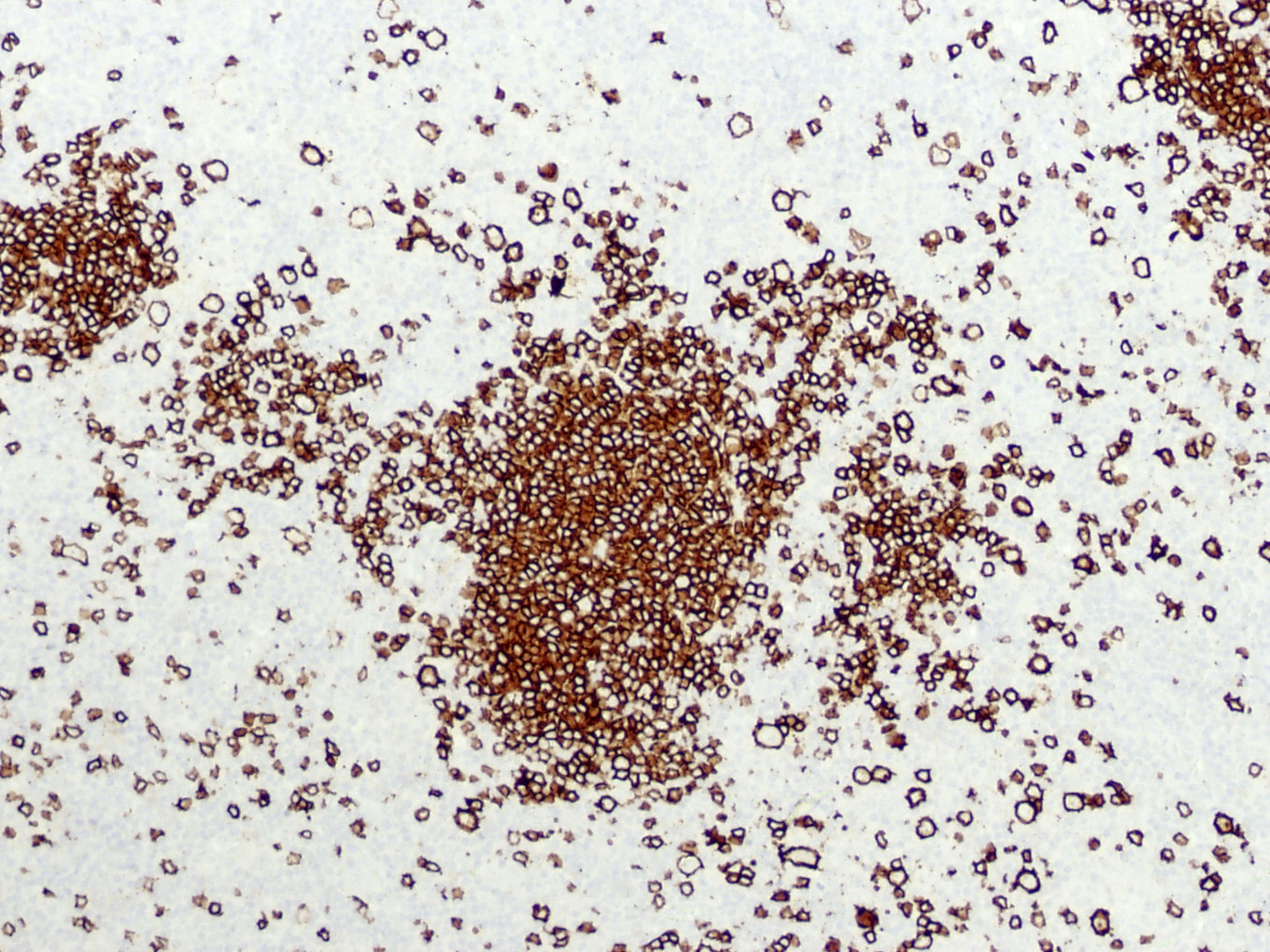
- LP cells are admixed with numerous small B lymphocytes, epithelioid histiocytes and CD21+ follicular dendritic cells
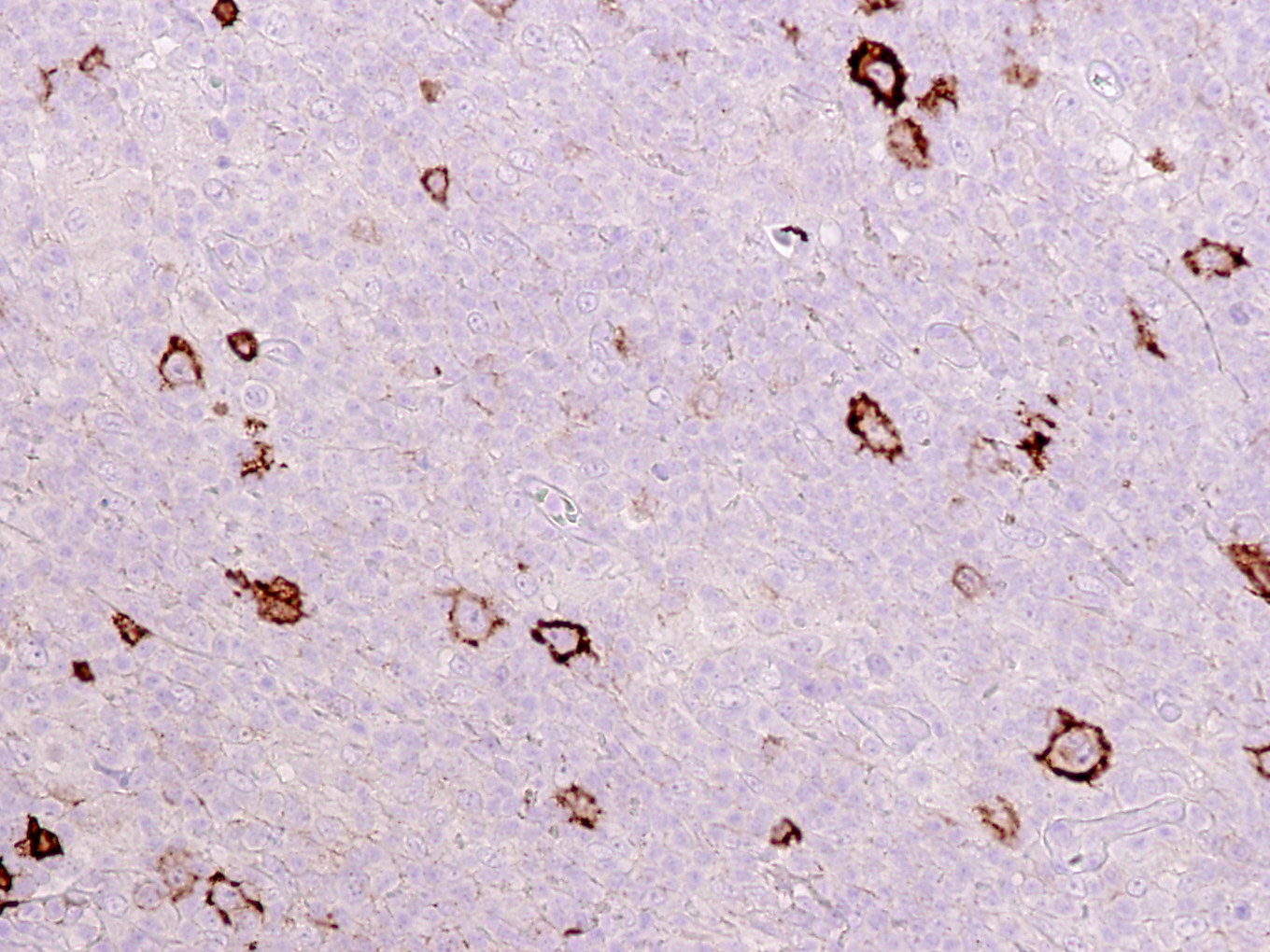
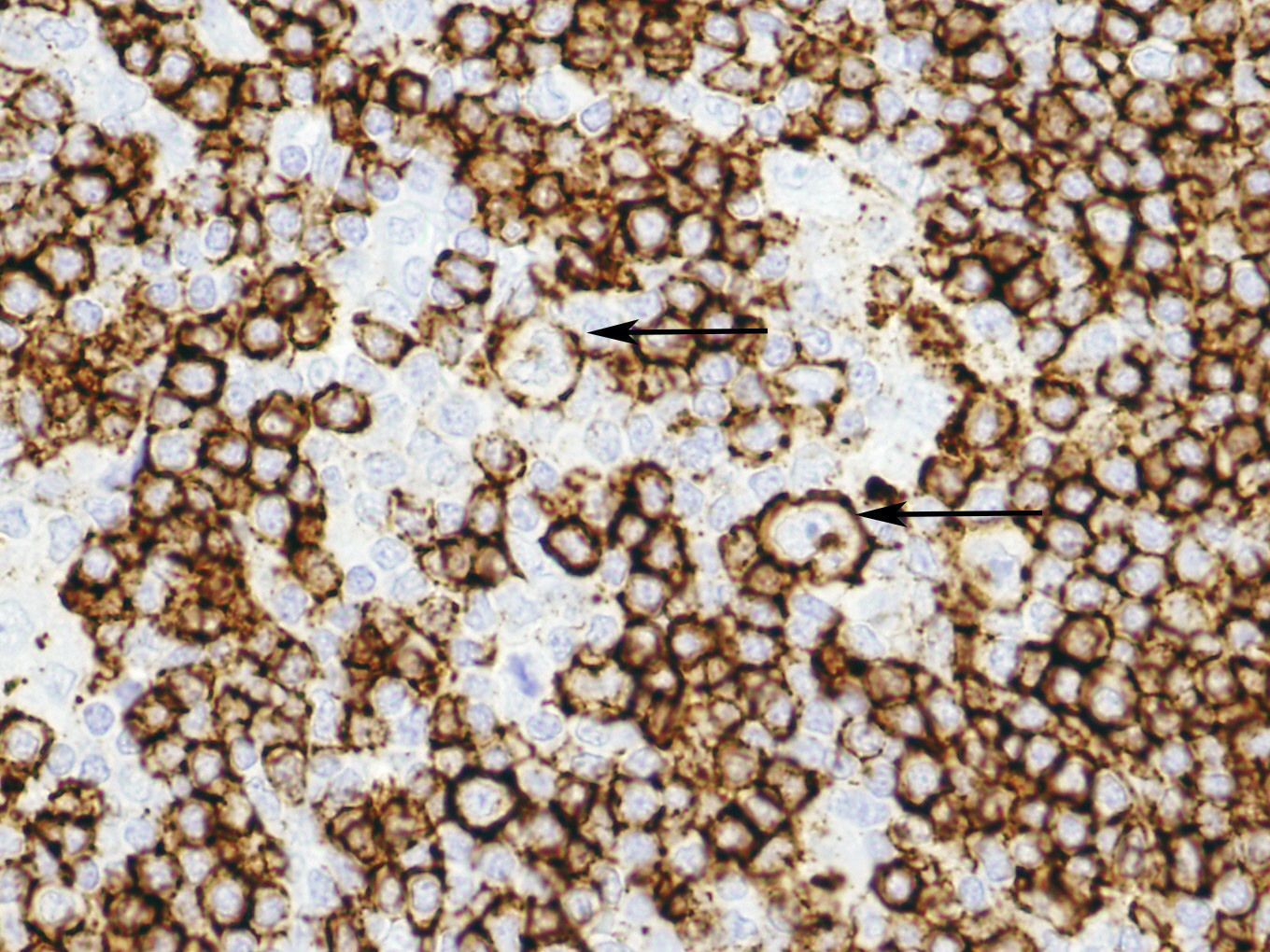
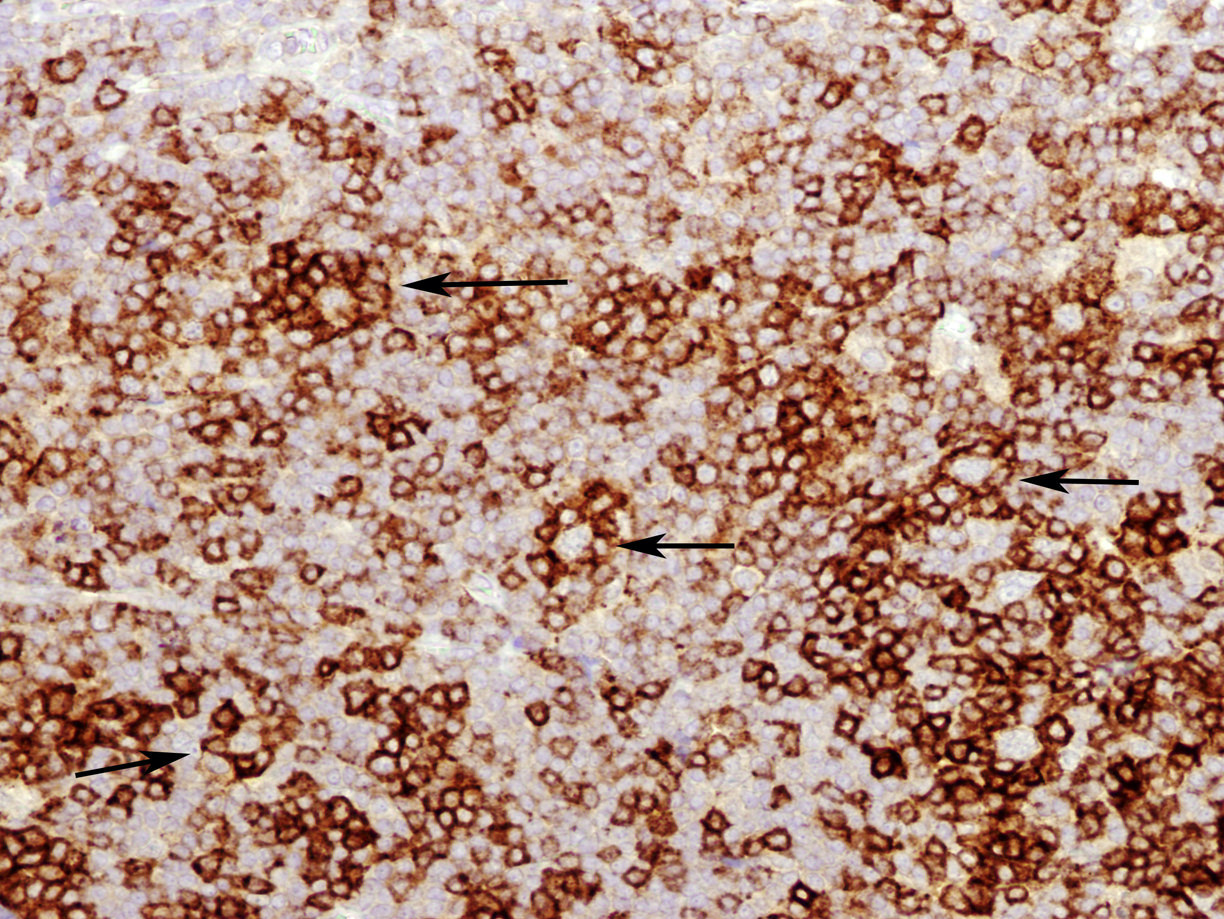
- Often PD-1+, T cell rosettes surrounding LP cells (Am J Surg Pathol 2008;32:1252, Blood 2017;129:802)
- Scant eosinophils, plasma cells or fibrosis
- Prominent sclerosis is unusual but may occur in older lesions
- Small germinal centers are rare between the nodules and usually present only at the compressed edge of normal lymph node tissue
- No / rare classic Reed-Sternberg cells, although LP cells may occasionally resemble Reed-Sternberg cells / variants
- No well formed granulomas, although epithelioid histiocytes may be prominent
- Diffuse patterns with background of reactive T cells
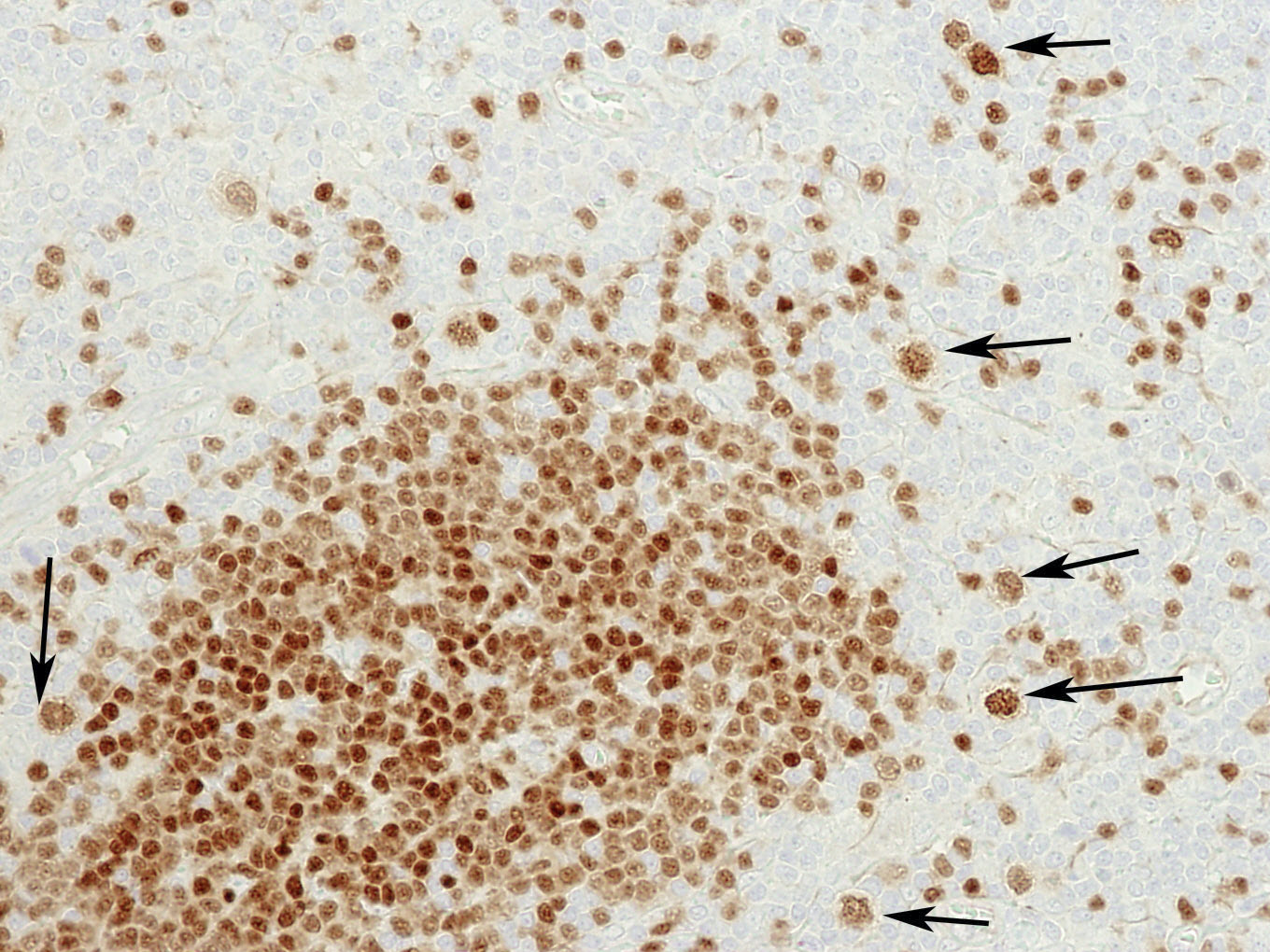
- 6 immunoarchitectural patterns have been described (Am J Surg Pathol 2003;27:1346)
- B cell rich nodular (typical / classic)
- Serpiginous / interconnected B cell rich
- Extranodular LP cells (variant)
- T cell rich nodular
- Diffuse T cell rich
- Diffuse B cell rich
- Variant patterns are associated with disease recurrence and transformation (Br J Haematol 2018;181:403, Br J Haematol 2014;167:238)
- Nodular lymphocyte predominant Hodgkin lymphoma and T cell histiocyte rich large B cell lymphoma are considered to be parts of the same disease spectrum (PLoS One 2013;8:e78812, Br J Haematol 2015;169:415)
- Syncytial variant is rarely reported (Am J Surg Pathol 2009;33:1725)
- Rare cases with features overlapping between T cell rich NLPHL and classic Hodgkin lymphoma (CHL) (i.e., neoplastic cells expressing both B cell program and CHL markers) have been reported (Arch Pathol Lab Med 2023 Dec 7 [Epub ahead of print])
- Bone marrow involvement: 3% of cases; involvement by large B cells (< 10% of all cases) in background of T cells and histiocytes
Microscopic (histologic) images
Contributed by Elaine S. Jaffe, M.D., Jayalakshmi Balakrishna, M.D. and Lauren B. Smith, M.D.
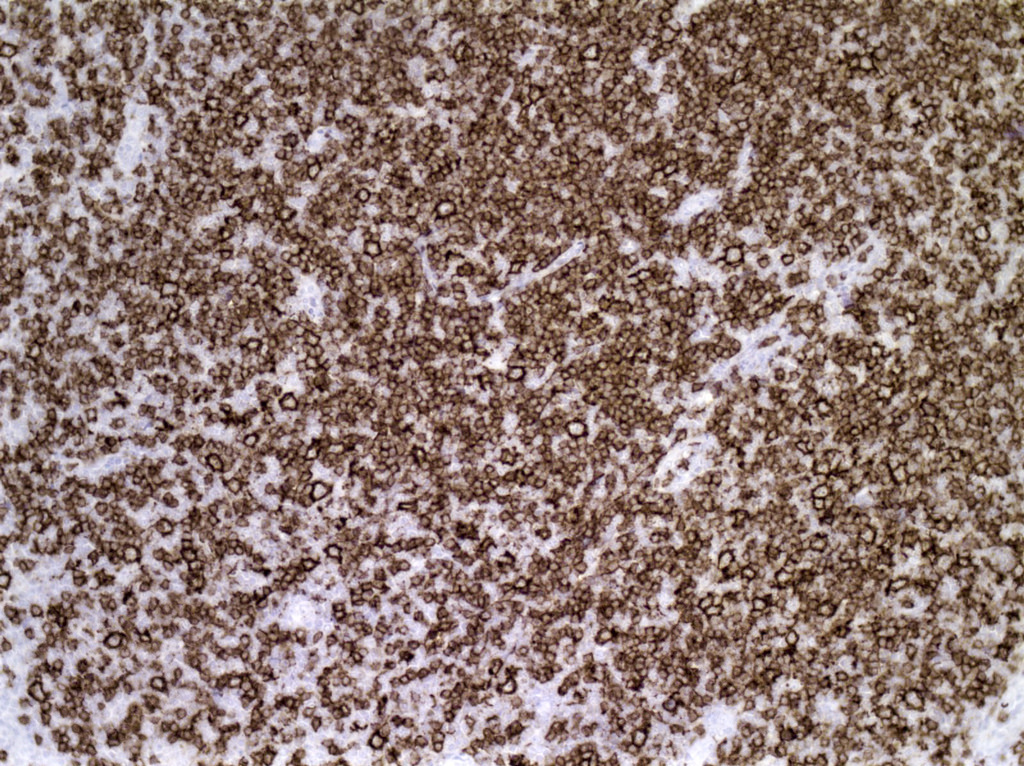
Positive stains
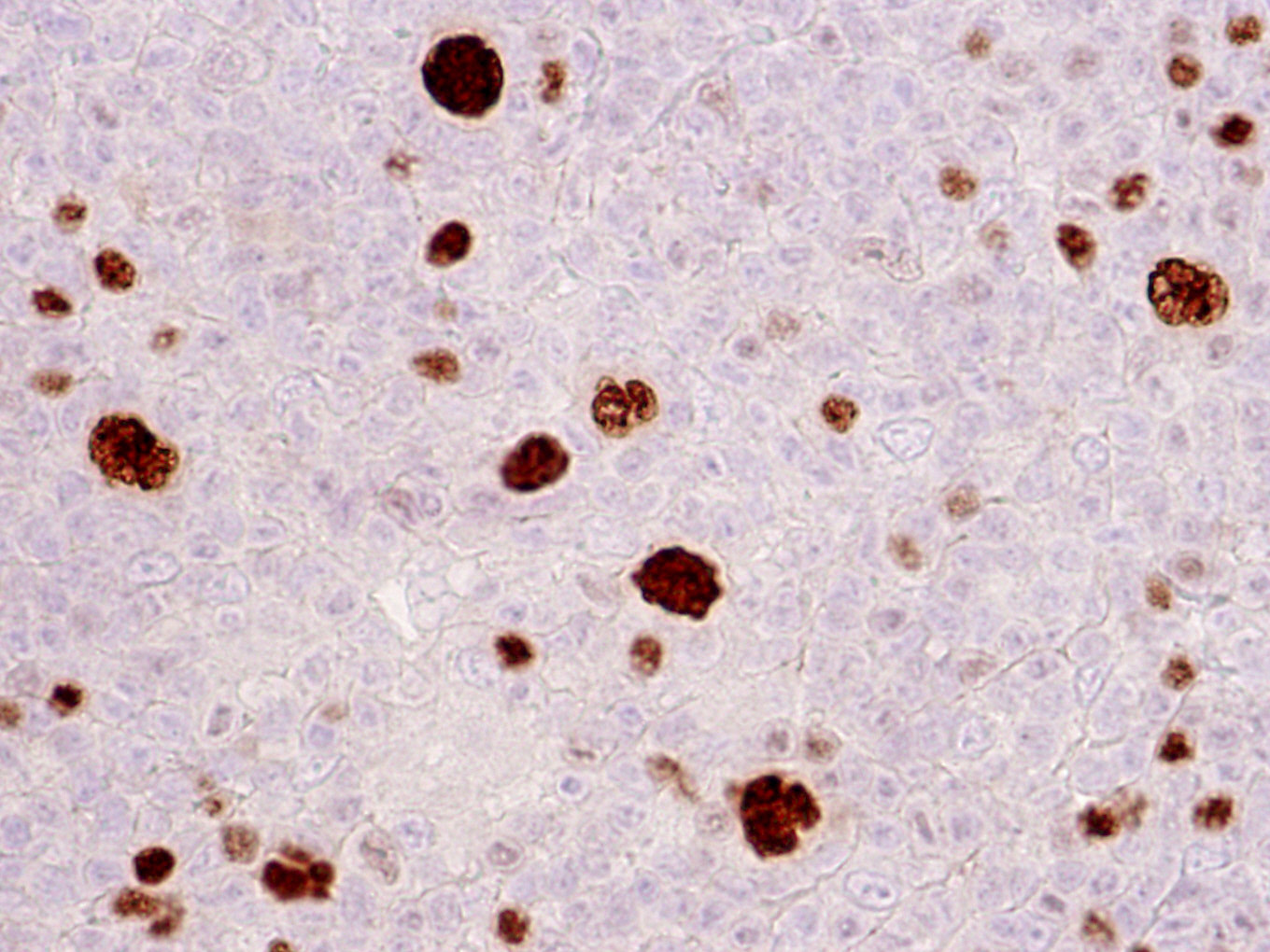
- LP cells
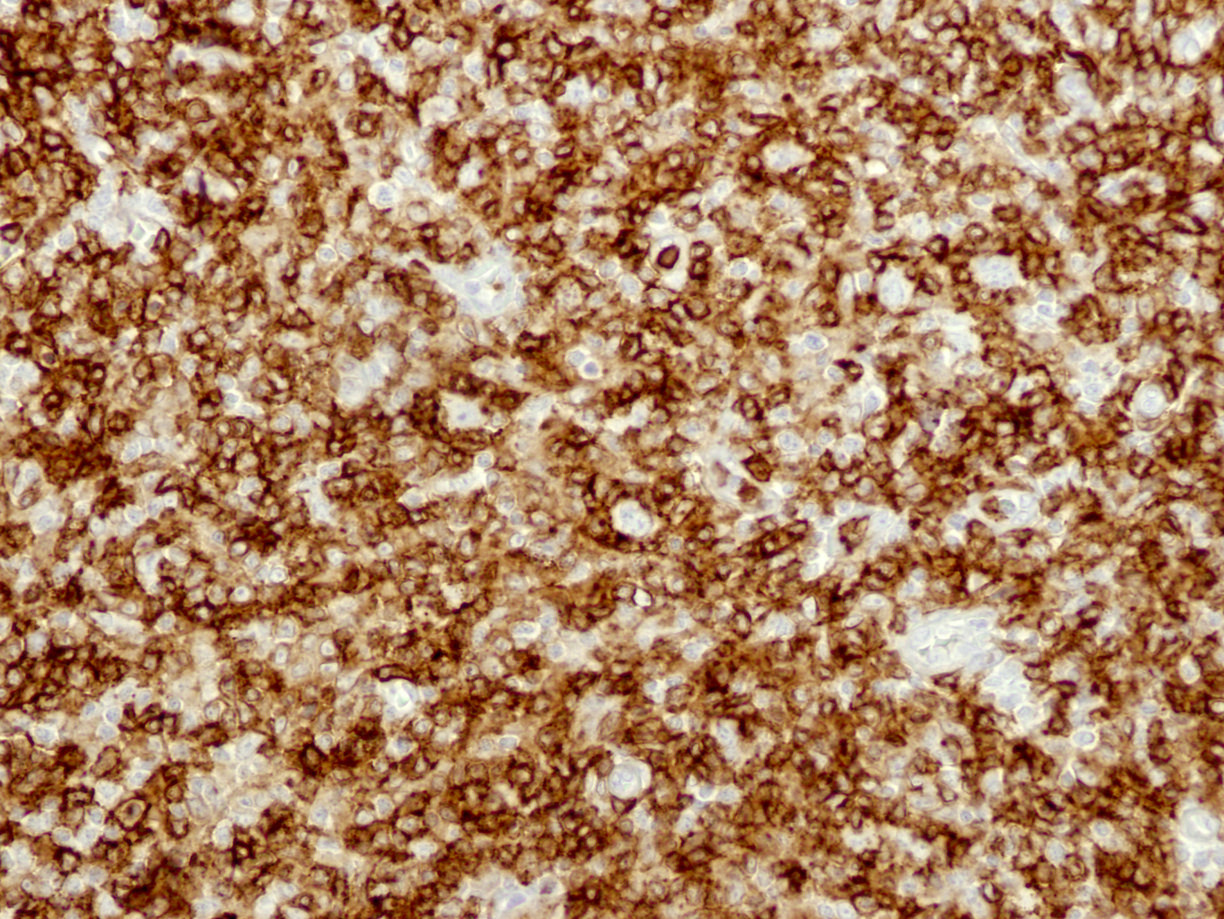
- CD45 (LCA), CD20, CD19 (Am J Clin Pathol 2003;119:192, Oncologist 2009;14:739)
- BCL6, OCT2, BOB1 and PU.1 (Br J Haematol 2019;184:45)
- CD79a, variable EMA (Semin Hematol 2016;53:190)
- IgD+ cases (27% frequency) compared with IgD- cases are associated with a younger median age (21 versus 44 years), male predominance (M:F = 23:1 versus 1.5:1) and frequent cervical lymph node involvement (Am J Surg Pathol 2006;30:585)
- In these cases, LP cells may be positive for Moraxella catarrhalis derived proteins (Nat Commun 2020;11:2465)
- EBER ISH: rare cases are positive for EBV; in these cases, LP cells show an atypical immunophenotype including CD30 expression (variable) (Hum Pathol 2022;129:32)
- Background cells
- CD20+ small B cells within nodules
- CD21+ expanded follicular dendritic cell meshwork
- T cell forming rosettes around LP cells are positive for PD-1, BCL6 and CD57 (variable)+ (T follicular helper phenotype) (Am J Surg Pathol 2000;24:1068, Am J Surg Pathol 2008;32:1252)
- T cell infiltrate expands over time and with progression
Negative stains
- LP cells
- CD3, CD15, CD30 (very rare cells may be positive) and EBV; usually fascin and JunB (Appl Immunohistochem Mol Morphol 2010;18:16)
- Rare cases may express CD15 (Histopathology 2011;58:803)
- CD30 expressing cases have also been reported and when expressed, CD30 is weak or variable (Pediatr Blood Cancer 2018;65:10.1002/pbc.26753)
Flow cytometry description
- Reactive T cells expressing both CD4 and CD8 (usually > 8%) have been described (Cytometry B Clin Cytom 2022;102:14)
Molecular / cytogenetics description
- LP cells show rearranged immunoglobulin genes and variably express Ig mRNA (Oncologist 2009;14:739)
- BCL6 rearrangements in a subset of cases: t(3;22)(q27;q11), t(3;7)(q27;p12), t(3;9)(q27;p13), t(3;14)(q27;q32) (J Mol Diagn 2005;7:352, Blood 2003;101:706)
- Aberrant activation of the JAK::STAT signaling pathway with nuclear accumulation of pSTAT6 in LP cells (Semin Hematol 2016;53:190)
- Mutations in JUNB, DUSP2, SGK1, SOCS1 and CREBBP (Haematologica 2019;104:330)
Sample pathology report
- Lymph node, right cervical, excision:
- Nodular lymphocyte predominant Hodgkin lymphoma (see comment and synoptic report)
Differential diagnosis
- Classic Hodgkin lymphoma, lymphocyte rich:
- Often extranodal, has Reed-Sternberg but not LP cells, no background of small reactive B cells
- CD30+, CD15+, CD20-, fascin+ and JunB+ (Ann Diagn Pathol 2019;39:105, Br J Haematol 2019;184:45)
- T cell / histiocyte rich large B cell lymphoma:
- Often with marrow involvement
- Diffuse and not nodular
- No LP cells and no T cell rosettes around neoplastic cells
- Differences in the composition of the microenvironment
- Higher numbers of follicular T helper cells in nodular lymphocyte predominant Hodgkin lymphoma
- More CD163+ macrophages in T cell histiocyte rich large B cell lymphoma-like nodular lymphocyte predominant Hodgkin lymphoma and in T cell histiocyte rich large B cell lymphoma
- Small T cells are predominantly of cytotoxic phenotype in T cell histiocyte rich large B cell lymphoma (Haematologica 2010;95:440, Int J Clin Exp Pathol 2009;3:39)
- Follicular lymphoma (especially the floral variant):
- Usually age 30+ years, complete effacement of nodal architecture, no LP cells
- Background of atypical cells and nonreactive small B cells as seen in nodular lymphocyte predominant Hodgkin lymphoma
- Progressive transformation of germinal centers:
- Benign / reactive condition
- Enlarged follicular structures with expanded mantle zones that invade into the germinal centers, a lack of typical LP cells and T cell rosettes and no lymph node effacement (Am J Surg Pathol 1999;23:27)
- May be seen in the same lymph node with NLPHL (Am J Surg Pathol 1984;8:253)
Additional references
Board review style question #1
A 20 year old man presents with an enlarged painless cervical lymph node that he has had for the past 6 months. An excisional biopsy is shown in the image. The neoplastic cells are positive for CD45 and CD20 and negative for CD15 and CD30. Which of the following is true about this entity?
- Background is rich in cytotoxic T cells
- Background lacks small B cells
- Neoplastic cells are OCT2 positive
- Neoplastic cells are PAX5 negative
Board review style answer #1
C. Neoplastic cells are OCT2 positive. Lymphocyte predominant (LP) cells preserve the B cell program and express B cell markers, including OCT2. Answer A is incorrect because the microenvironment in nodular lymphocyte predominant Hodgkin lymphoma (NLPHL) varies depending on the immunoarchitectural patterns and can be rich in B cells or T follicular helper cells. Answer B is incorrect because most immunoarchitectural patterns are rich in background small B cells except the diffuse T cell rich pattern, which resembles T cell / histiocyte rich large B cell lymphoma. Answer D is incorrect because the LP cells are B cells and express pan-B cell markers, including PAX5, CD20, CD19 and CD79a.
Comment here
Reference: Nodular lymphocyte predominant B cell lymphoma / nodular lymphocyte predominant Hodgkin lymphoma
Comment here
Reference: Nodular lymphocyte predominant B cell lymphoma / nodular lymphocyte predominant Hodgkin lymphoma
Board review style question #2
What is the immunophenotype of T cells in the microenvironment of nodular lymphocyte predominant Hodgkin lymphoma (NLPHL)?
- CD3+ / CD4+ / PD-1+
- CD3+ / CD8+ / CD57+
- CD3+ / CD8+ / CD57-
- CD3+ / CD8+ / PD-1+
Board review style answer #2
A. CD3+ / CD4+ / PD-1+. The background T cells in NLPHL are mostly T follicular helper (TFH) cells expressing CD4 and PD-1, along with other TFH markers like BCL6, ICOS and CXCL13. Answers B, C and D are incorrect because those are not the immunophenotype of TFH cells.
Comment here
Reference: Nodular lymphocyte predominant B cell lymphoma / nodular lymphocyte predominant Hodgkin lymphoma
Comment here
Reference: Nodular lymphocyte predominant B cell lymphoma / nodular lymphocyte predominant Hodgkin lymphoma