Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Peripheral smear description | Positive stains | Negative stains | Flow cytometry description | Flow cytometry images | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: El Hussein S, Khoury J. Aggressive NK cell leukemia. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lymphomanonBNKcell.html. Accessed December 26th, 2024.
Definition / general
- Aggressive NK cell leukemia (ANKL) is a rare disease with a dismal prognosis and many diagnostic challenges
- ANKL shares several overlapping features with other NK cell neoplasms
- The clinical presentation and course can help distinguish from other NK cell neoplasms
- ANKL can be subtle to detect morphologically and immunophenotypically
Essential features
- ANKL overlaps morphologically and genetically with extranodal NK / T cell lymphoma; however, its clinical presentation is acute and outcome is poorer
- As rare EBV negative ANKL have been described, EBV negative status cannot be used as the sole criterion to exclude a diagnosis of ANKL
- Bone marrow involvement by ANKL can be prominent or subtle
- Cytologic atypia can be notable, however, in a subset of cases; neoplastic cells are deceptively bland
Terminology
- Aggressive NK cell leukemia
ICD coding
- ICD-O: 9948/3 - aggressive NK cell leukemia
Epidemiology
- Asian population (mainly in EBV positive ANKL, as EBV negative ANKL have been shown to affect other ethnicities)
- Median age 40 years
- No gender predilection
- Strong association with EBV infection (although Epstein-Barr virus encoded small RNA (EBER) negative ANKL is a well established entity)
- References: Hum Pathol 2020;105:20, Mod Pathol 2017;30:1100, Am J Surg Pathol 2017;41:67, Am J Surg Pathol 2020;44:1235
Sites
- Peripheral blood, bone marrow, liver, spleen
Pathophysiology
- In EBV positive ANKL, EBV encoded small RNAs induce release of high amounts of IL10:
- IL10 activates the JAK / STAT pathway
- Stimulation of STAT3 phosphorylation
- Downstream MYC activation leading to clonal expansion
- In EBV negative ANKL, other unidentified mechanisms lead to
- Stimulation of STAT3 phosphorylation
- Downstream MYC activation leading to clonal expansion
- Reference: Cell Res 2018;28:172
Etiology
- In EBV positive ANKL: chronic active EBV infection (Jpn J Cancer Res 1997;88:82, Am J Hematol 1997;54:276, J Dermatol 2014;41:29)
- In EBV negative ANKL: unknown
Clinical features
- Fever, B symptoms, hepatosplenomegaly, lymphadenopathy
Diagnosis
- Bone marrow biopsy
- Biopsy of organs suspected of involvement by CT scan
- Peripheral blood smear
- Flow cytometry analysis
Laboratory
- Neutropenia, anemia, thrombocytopenia
- Elevated serum lactate dehydrogenase (LDH) levels
- Elevated liver functions tests
- Disseminated intravascular coagulopathy
- Hemophagocytic syndrome
- Reference: Cancers (Basel) 2020;12:2900
Prognostic factors
- Prognosis is very poor with a median survival of less than 2 months, despite intensive chemotherapy
Case reports
- 16 year old boy with EBV negative ANKL (J Hematol 2018;7:163)
- 28 year old woman in remission, 1 year post allogeneic hematopoietic stem cell transplant (Intern Med 2010;49:1907)
- 36 year old man with CD56 negative ANKL (Case Rep Hematol 2017;2017:3724017)
- 56 year old man with ANKL diagnosed by cerebrospinal fluid examination (Diagn Cytopathol 2016;44:314)
- 78 year old man with ANKL associated hemophagocytic lymphohistiocytosis (Blood 2016;127:2502)
Treatment
- Allogeneic hematopoietic stem cell transplantation (SCT) improves outcome in ANKL patients for a limited time
- No consensus chemotherapeutic regimen has been established to manage patients with ANKL; chemotherapy regimens used to manage ANKL include:
- SMILE (dexamethasone, methotrexate, ifosfamide, etoposide and L-asparaginase)
- AspaMetDex (L-asparaginase, methotrexate and dexamethasone)
- VIDL (etoposide, ifosfamide, dexamethasone and L-asparaginase)
- Reference: Cancers (Basel) 2020;12:2900
Microscopic (histologic) description
- Bone marrow involvement by ANKL can be prominent or subtle
- Two main patterns of infiltration: interstitial and sinusoidal
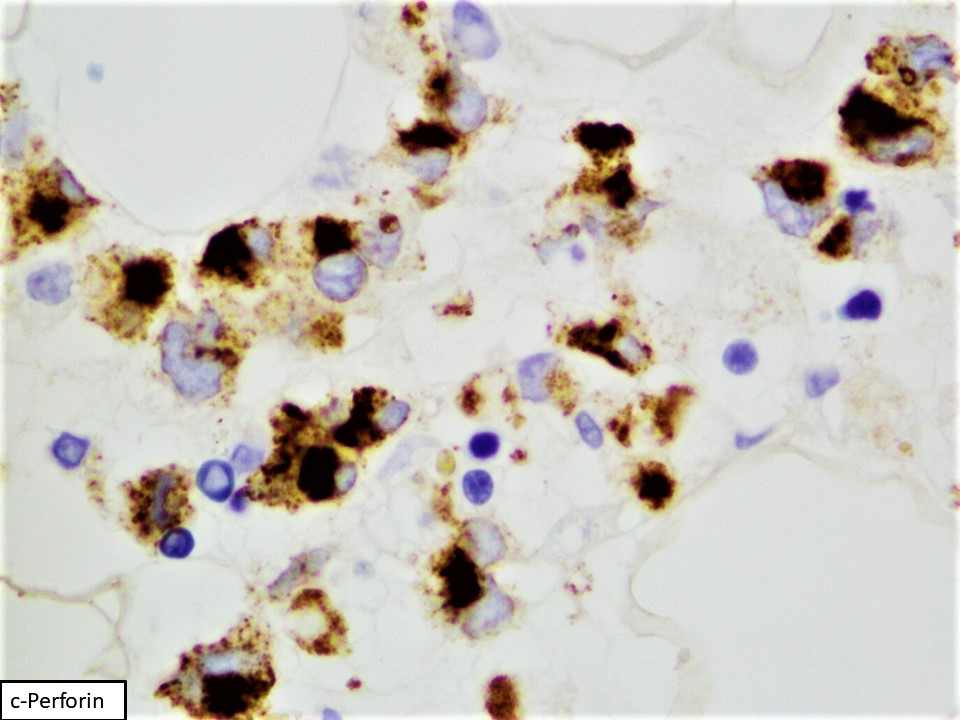
- Neoplastic cells are medium sized, with a moderate amount of cytoplasm, highly irregular nuclei with condensed chromatin and conspicuous nucleoli
- In some cases, atypia is subtle and neoplastic cells can look deceptively bland
- Apoptosis and focal necrosis are common findings
- Geographic necrosis is typically not observed in ANKL, unlike cases of extranodal NK / T cell lymphoma (ENKTL)
- Reference: Cancers (Basel) 2020;12:2900
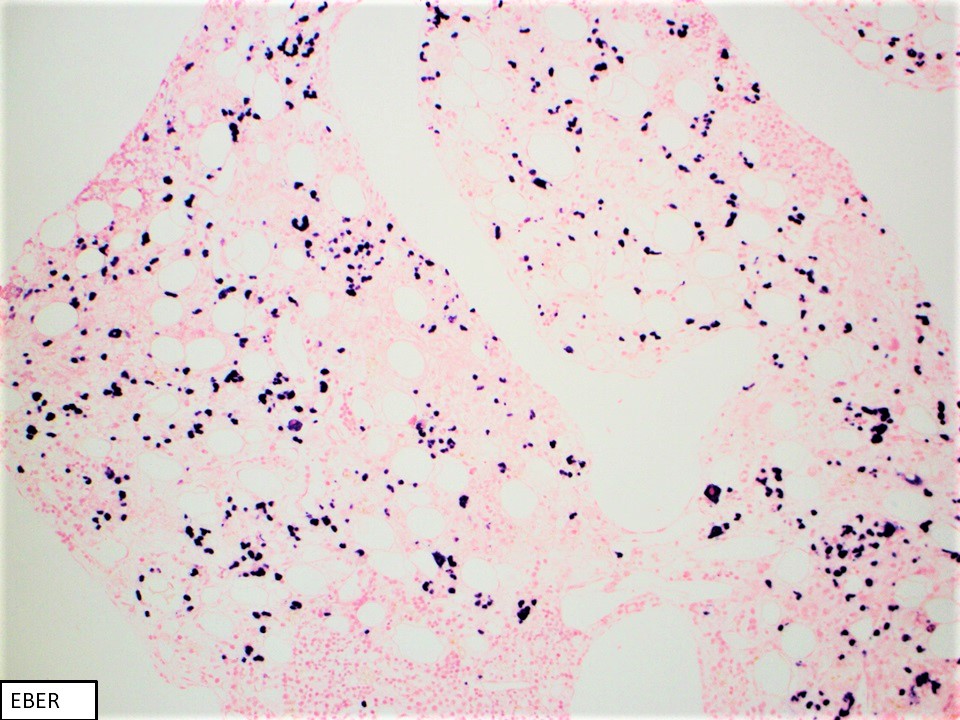
Microscopic (histologic) images
Cytology description
- Moderate amounts of basophilic agranular cytoplasm
- Punched out cytoplasmic vacuoles
- Highly irregular nuclear contours and an open chromatin pattern with prominent nucleoli
- Reference: Cancers (Basel) 2020;12:2900
Peripheral smear description
- Cells are intermediate to large in size
- Moderate amounts of basophilic agranular cytoplasm
- Punched out cytoplasmic vacuoles
- Highly irregular nuclear contours and an open chromatin pattern with prominent nucleoli
- Reference: Cancers (Basel) 2020;12:2900
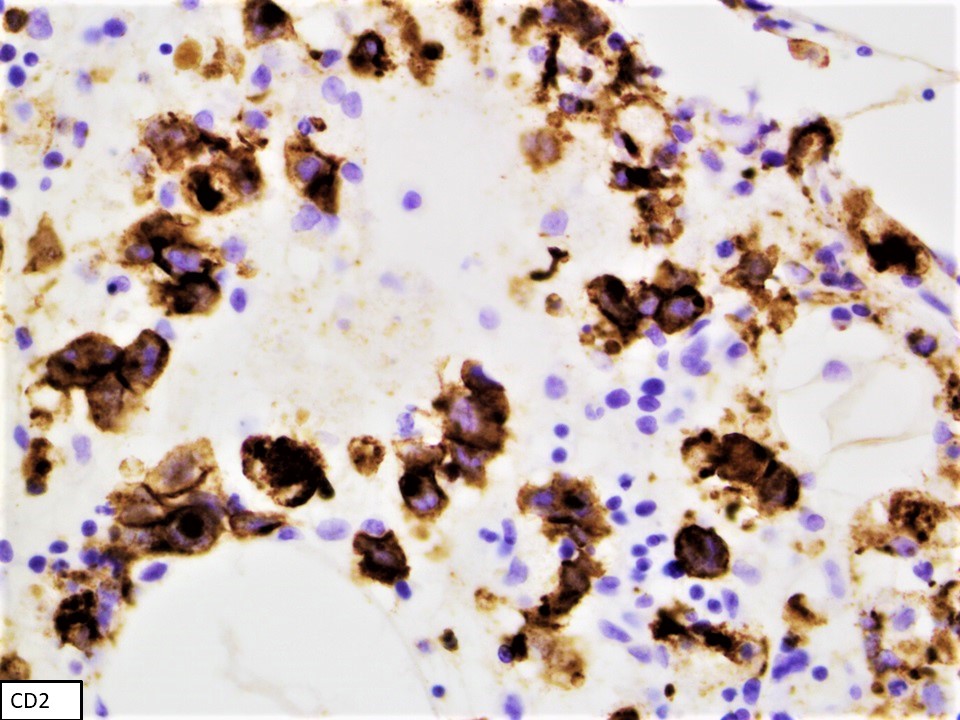
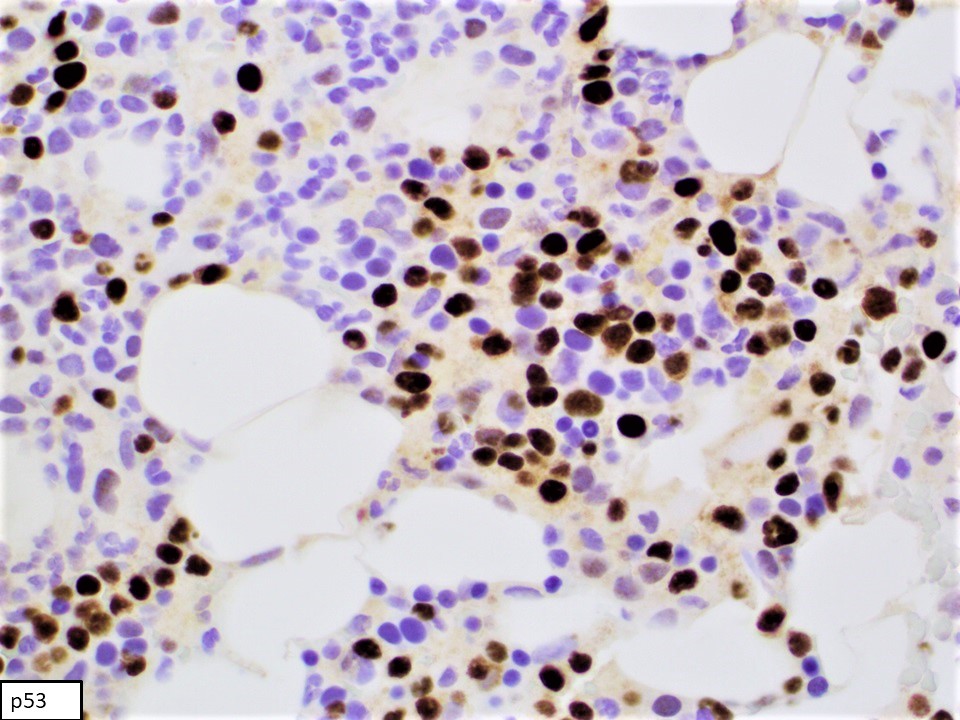
Positive stains
- CD2, cytoplasmic CD3 epsilon protein, CD56, perforin A, granzyme B, TIA, EBER (in most cases), PDL1 (in some cases), p53 (frequent), BCL2, MYC (Am J Surg Pathol 2020;44:1235, Mod Pathol 2017;30:1100)
Flow cytometry description
- Prominent forward scatter (FSC) (increased cell size when compared with nonneoplastic background lymphocytes)
- Consistently positive markers: CD2, cCD3 (cytoplasmic CD3), CD16, CD56, CD94
- Frequently positive markers: CD7, CD8
- Frequently negative markers: sCD3 (surface CD3), CD4, CD5, CD57, killer Ig-like receptors (KIR) (CD158a-e), TCRαβ and TCRγδ
- References: Leuk Lymphoma 2015;56:103, Cancers (Basel) 2020;12:2900, Am J Surg Pathol 2020;44:1235
Flow cytometry images
Molecular / cytogenetics description
- Array based comparative genomic hybridization (aCGH) analyses can demonstrate nonspecific cytogenetic findings (Genes Chromosomes Cancer 2005;44:247):
- Gains of 1q23.1-q23.2 and 1q31.3-q44
- Losses of 7p15.1-q22.3 and 17p13.1
- Whole genome and exome sequencing and next generation sequencing have shown mutations in the following pathways (Am J Surg Pathol 2020;44:1235, Nat Commun 2018;9:1567, Cell Res 2018;28:172):
- JAK / STAT (STAT3, STAT5B, STAT5A, JAK2, JAK3, STAT6, SOCS1, SOCS3 and PTPN11)
- RAS / MAPK
- Epigenetic modifiers (TET2, CREBBP, KMT2D, BCOR, SET2D, GFI1)
- RNA helicase (DDX3X)
- Cell cycle regulation and DNA damage repair (TP53, ASXL1, ASXL2, BRINP3)
- mRNA splicing (PRPF40B)
Sample pathology report
- Bone marrow, posterior iliac crest, core biopsy, clot section, aspirate smears and touch imprint:
- Aggressive NK cell leukemia (ANKL) (see comment)
- Comment: Hypocellular bone marrow for age 20 - 30%, with residual trilineage hematopoiesis
- Flow cytometry immunophenotypic studies are performed using bone marrow aspirate material of the specimen. A distinct population of aberrant NK cells is detected. The neoplastic cells account for 49% of all analyzed cells. The neoplastic cells are positive for CD2, cytoplasmic CD3, CD7 (bright), CD45 (bright), CD48 (partial), CD56 and CD158b. The neoplastic cells are negative for CD1a, surface CD3, CD4, CD5, CD10, CD8, CD13+CD33, CD19, CD25, CD30, CD34, CD117, CD123, CD158a, CD158e, TdT, TCRαβ, TCRγδ, myeloperoxidase and HLA-DR.
- Bone marrow biopsy: quality - suboptimal, subcortical; cellularity - 20 - 30% in the most cellular areas; megakaryocytes - significantly decreased, with unremarkable morphology; infiltrate - numerous medium sized cells with dense chromatin and scant cytoplasm in interstitial distribution
- Bone marrow clot section: quality - adequate, particles present; cellularity: 30 - 40%; megakaryocytes - present; infiltrate - numerous medium sized cells with dense chromatin and scant cytoplasm in interstitial distribution
- Stains on clot: Immunohistochemical stains were performed using fixed, paraffin embedded tissue of clot specimen. The neoplastic cells are positive for CD2, CD56 and p53. In situ hybridization studies for Epstein-Barr virus encoded small RNA (EBER) using fixed, paraffin embedded tissue of clot specimen were performed. The neoplastic cells are strongly positive for EBER.
- Bone marrow aspirate: quality / cellularity - adequate, particles present; granulocytes - complete maturation; erythrocytes - complete maturation; megakaryocytes - present; lymphocytes - markedly increased, predominantly medium size, with open nuclear chromatin, inconspicuous nucleoli and moderate amount of deep basophilic cytoplasm with vacuoles
Differential diagnosis
- Extranodal NK / T cell lymphoma (ENKTL):
- Strong association with EBV infection
- Cytokine secretion function
- Overlapping morphologic and genetic features with ANKL
- Less aggressive clinical presentation and outcome
- Predilection to involve upper aerodigestive tract (most commonly nasal cavity), gastrointestinal tract, skin, soft tissue and testes
- Chronic lymphoproliferative disorder of NK cells (CLPD-NK):
- Unknown stimulus, possibly viral
- No EBV association
- Cytotoxic function
- Uniform CD8 positivity
- Loss of CD2 expression
- Less aggressive clinical course
- Patients are mostly asymptomatic or have symptoms related to cytopenias (Eur J Haematol 2018;100:444)
Additional references
Board review style question #1
Which of the following statements is true?
- Aggressive NK cell leukemia (ANKL) and extranodal NK / T cell lymphoma (ENKTL) overlap morphologically and genetically
- ANKL harbors specific cytogenetic features
- ANKL is characteristically negative for sCD3 and cCD3 by flow cytometry analysis
- EBER negativity rules out the diagnosis of ANKL
Board review style answer #1
A. ANKL and ENKTL overlap morphologically and genetically, rendering these 2 diagnoses very challenging in certain cases to distinguish clinically. ANKL is characteristically negative for sCD3 but positive for cCD3 by flow cytometry analysis. No specific cytogenetic features characterize ANKL cases. EBER negative ANKL cases have been well established in literature, thus EBER negativity does not rule out ANKL.
Comment Here
Reference: Aggressive NK cell leukemia
Comment Here
Reference: Aggressive NK cell leukemia
Board review style question #2
Which of the following statements is true?
- Aggressive NK cell leukemia (ANKL) tumor burden in bone marrow sample is invariably high
- Cytologic atypia in ANKL is consistently prominent
- Prognosis of ANKL is remarkably ameliorated posttransplant and chemotherapy
- The most commonly involved genetic pathway in ANKL is the JAK / STAT pathway
Board review style answer #2
D. The most commonly involved genetic pathway in ANKL is the JAK / STAT pathway. ANKL tumor burden in bone marrow sample is variable and some cases have a very low bone marrow involvement, making such cases very challenging to diagnose morphologically and immunophenotypically. Cytomorphology of leukemic cells in ANKL can be deceptively bland in a prominent percentage of cases. Prognosis of ANKL remains dismal, even posttransplant and chemotherapy.
Comment Here
Reference: Aggressive NK cell leukemia
Comment Here
Reference: Aggressive NK cell leukemia