Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Laboratory | Prognostic factors | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Peripheral smear description | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Marques-Piubelli M, Segura-Rivera R, Miranda R, Torres-Cabala C. Mycosis fungoides subtypes. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lymphomamycosisfungoidesvariants.html. Accessed April 1st, 2025.
Definition / general
- Mycosis fungoides is the most common type of primary cutaneous T cell lymphoma and is characterized by the proliferation of atypical cerebriform or hyperconvoluted T cells, progressive clinical course and evolution of stages of patches, plaques and tumors (J Dtsch Dermatol Ges 2018;16:543, Mod Pathol 2000;13:502, Eur J Cancer 2021;156:S35)
- Subtypes of mycosis fungoides usually present with a distinct clinical course; 3 subtypes are currently recognized by WHO
classification (5th edition)
- Folliculotropic mycosis fungoides
- Pagetoid reticulosis
- Granulomatous slack skin disease
- Other variants / subtypes
- Granulomatous mycosis fungoides (Cells 2024;13:419)
- Pediatric mycosis fungoides (JAMA Dermatol 2021;157:431)
- Syringotropic mycosis fungoides (Am J Surg Pathol 2011;35:100)
- Hypopigmented mycosis fungoides (An Bras Dermatol 2013;88:954)
Essential features
- Diagnosis of mycosis fungoides and its variants must include clinical findings; subtypes may show underlying and characteristic features of mycosis fungoides but also show distinct clinical features
- Folliculotropic mycosis fungoides
- Usually presents as early (patch / thin plaque) or less commonly as advanced (thick plaque / tumor) disease
- Presents as follicular papules (often grouped), follicular keratosis with or without scarring or nonscarring alopecia, palmar / plantar lesions or acneiform lesions
- Histologically the lymphomatous lymphocytes infiltrate hair follicles as well as the surrounding dermis
- Pagetoid reticulosis
- Solitary or multiple, slow growing, psoriasiform, crusty or hyperkeratotic patch or plaque, often arising on distal limbs or trunk and histologically showing prominent epidermotropism with pagetoid pattern
- Neoplastic lymphocytes are usually CD8+
- Granulomatous slack skin disease
- Circumscribed areas of pendulous folds of lax skin in intertriginous areas (axillae, inguinal and gluteal regions), with an indolent clinical course
- May coexist with more typical mycosis fungoides lesions
- Folliculotropic mycosis fungoides
Terminology
- Pagetoid reticulosis: Woringer-Kolopp disease (localized disease), Ketron-Goodman disease (disseminated disease); mycosis fungoides palmaris and plantaris
Epidemiology
- Folliculotropic mycosis fungoides (Arch Dermatol 2008;144:738, JAMA Dermatol 2021;157:157, Clin Cosmet Investig Dermatol 2022;15:1899, J Am Acad Dermatol 2016;75:347, JAMA Dermatol 2016;152:992, Sci Rep 2021;11:10555, J Cutan Pathol 2020;47:241)
- Most common subtype of mycosis fungoides
- ~20% of all mycosis fungoides types
- ~5% of all primary cutaneous lymphomas
- More common in male adults
- Most common subtype of mycosis fungoides
- Pagetoid reticulosis (Mod Pathol 2000;13:502, J Cutan Pathol 2014;41:703)
- May occur in all ages but is more common in adults
- Granulomatous slack skin (Dermatol Pract Concept 2020;10:e2020044, Eur J Cancer 2021;156:S35, Arch Dermatol 2008;144:1609)
- Rare
- Most common in male adults
- Granulomatous mycosis fungoides (Arch Dermatol 2008;144:1609, Cells 2024;13:419)
- Most common in White male adults
- Pediatric mycosis fungoides (JAMA Dermatol 2021;157:431)
- More common in male patients
- Syringotropic mycosis fungoides (Am J Surg Pathol 2011;35:100)
- Most common in male adults
- Hypopigmented mycosis fungoides (An Bras Dermatol 2013;88:954)
- Younger patients, usually CD8 positive
Sites
- Folliculotropic mycosis fungoides: head and neck (eyebrows), extremities and abdomen (Arch Dermatol 2008;144:738, JAMA Dermatol 2021;157:157, Clin Cosmet Investig Dermatol 2022;15:1899, Mod Pathol 2020;33:83)
- Pagetoid reticulosis: distal extremities (hands and soles), trunk (Mod Pathol 2000;13:502, J Cutan Pathol 2014;41:703)
- Granulomatous slack skin: intertriginous areas (axilla, inguinal region and buttocks) (Dermatol Pract Concept 2020;10:e2020044, Eur J Cancer 2021;156:S35, Mod Pathol 2020;33:83)
Pathophysiology
- No specific pathogenesis has been identified in the subtypes of mycosis fungoides (Arch Dermatol 2008;144:738, Cells 2024;13:419)
- Alteration of tumor suppression pathways associated with T cell activation
- Folliculotropic mycosis fungoides
- Potential role of Th2 cytokines
- Granulomatous mycosis fungoides
- Potential role of Th1 / Th17
- Hypopigmented and pediatric mycosis fungoides
- Th1 mediated response (driven by CD8+ phenotype)
Etiology
- No clear etiology identified
Clinical features
- Folliculotropic mycosis fungoides (Acta Derm Venereol 2021;101:adv00537, Arch Dermatol 2008;144:738, JAMA Dermatol 2021;157:157, Clin Cosmet Investig Dermatol 2022;15:1899, J Am Acad Dermatol 2016;75:347, JAMA Dermatol 2016;152:992, Sci Rep 2021;11:10555, J Cutan Pathol 2020;47:241)
- Usually presents as early (patch / thin plaque) and less commonly as advanced (thick plaque / tumor) disease
- Pruritus is often present
- Follicular papules (often grouped), follicular keratosis, scarring or nonscarring alopecia, palmar / plantar lesions and acneiform lesions / comedo-like
- Trichoscopy may show nonscarring alopecia (diminished pilosebaceous units, dotted dilated vessels, broken dystrophic hair and vellus hair) or scarring alopecia (white dots and absence of follicular dots)
- Pseudotumors and tumor lesions may be observed
- Most commonly affected sites are head and neck / face region (eyebrows with follicular accentuation), upper extremities and thorax
- Secondary bacterial infection may be present
- Pagetoid reticulosis (Woringer-Kolopp disease) (Mod Pathol 2000;13:502, J Cutan Pathol 2014;41:703)
- Solitary or multiple, slow growing, psoriasiform, crusty or hyperkeratotic patch or plaque
- Often arises on distal limbs or trunk
- Granulomatous slack skin (Dermatol Pract Concept 2020;10:e2020038, Eur J Cancer 2021;156:S35, Arch Dermatol 2008;144:1609, J Eur Acad Dermatol Venereol 2012;26:1472)
- Circumscribed areas of pendulous folds of lax skin in intertriginous areas (axillae, inguinal and gluteal regions)
- Pruritus, patches and erythema may be present
- Indolent clinical course
- Paraneoplastic events may occur
- May coexist with more typical mycosis fungoides lesions
- Granulomatous mycosis fungoides (JAAD Case Rep 2015;1:298, Arch Dermatol 2008;144:1609, Cells 2024;13:419)
- Erythematous and indurated patches and plaques in head and neck areas, extremities and trunk
- Absence of bulky skin folds (cutis laxa-like features)
- Most cases are diagnosed in early stage
- Ulcers can be noted in advanced stages
- May be associated with alopecia
- Second malignancy may be associated
- Pediatric mycosis fungoides (JAMA Dermatol 2021;157:431)
- Usually diagnosed at early stage of disease
- Mostly characterized by hypopigmented lesions (patches followed by plaques), which delay the diagnosis
- Syringotropic mycosis fungoides (Am J Surg Pathol 2011;35:100, J Am Acad Dermatol 2014;71:926)
- Solitary or multiple, well circumscribed, red-brown plaque or patches, often associated with alopecia
- Skin directed therapy may be inadequate (similar to folliculotropic mycosis fungoides)
- Hypopigmented mycosis fungoides (An Bras Dermatol 2013;88:954)
- Hypopigmented to achromic patches that usually occur in patients with high phototype
- Usually occurs on trunk and proximal extremities
Laboratory
- Laboratory findings can be normal or show increase of lactate dehydrogenase (LDH) or β2 microglobulin (Dermatol Pract Concept 2020;10:e2020044, Cells 2024;13:419)
Prognostic factors
- Folliculotropic mycosis fungoides (Arch Dermatol 2008;144:738, JAMA Dermatol 2021;157:157, J Dtsch Dermatol Ges 2018;16:543, JAMA Dermatol 2016;152:992, Sci Rep 2021;11:10555, Br J Dermatol 2017;177:223, J Cutan Pathol 2020;47:241)
- Old age and intense infiltrate may be associated with adverse prognosis
- Worse prognosis when compared to classic mycosis fungoides
- Old age and intense infiltrate may be associated with adverse prognosis
- Pagetoid reticulosis (Mod Pathol 2000;13:502, J Cutan Pathol 2014;41:703)
- Indolent and benign clinical course (Woringer-Kolopp disease)
- Granulomatous slack skin (Dermatol Pract Concept 2020;10:e2020044, Eur J Cancer 2021;156:S35, Arch Dermatol 2008;144:1609)
- Indolent clinical course but most patients die due to the disease
- Granulomatous mycosis fungoides (Arch Dermatol 2008;144:1609)
- Variable prognosis
- Pediatric mycosis fungoides (JAMA Dermatol 2021;157:431)
- Benign outcome and most patients have a good response to treatment
- Syringotropic mycosis fungoides (J Am Acad Dermatol 2014;71:926)
- Usually a good prognosis (5 year survival rate: 100%)
- Hypopigmented mycosis fungoides (An Bras Dermatol 2013;88:954)
- Better prognosis when compared to classic mycosis fungoides
Case reports
- 2 year old girl with pagetoid reticulosis (Woringer-Kolopp disease) presented with a solitary verrucous plaque on the hand evolving over 1 year (JAAD Case Rep 2018;5:104)
- 28 year old man with long duration erythema on the ear and the diagnosis of granulomatous mycosis fungoides (JAAD Case Rep 2015;1:298)
- 64 year old woman with folliculotropic mycosis fungoides mimicking venous leg ulcers (Acta Derm Venereol 2021;101:adv00537)
- 64 year old man with a history of multiple shiny patches on extremities and the diagnosis of syringotropic mycosis fungoides mimicking necrobiosis lipoidica diabeticorum (JAAD Case Reports 2024 March 8 [Epub ahead of print])
- 74 year old man with erythematous plaque on the right axilla of 1 year duration and the diagnosis of granulomatous slack skin (Dermatol Pract Concept 2020;10:e2020044)
Treatment
- Folliculotropic mycosis fungoides (Acta Derm Venereol 2021;101:adv00537, Arch Dermatol 2008;144:738, Clin Cosmet Investig Dermatol 2022;15:1899, Br J Dermatol 2017;177:223)
- Variable response to treatment
- Psoralen plus ultraviolet A (PUVA)
- Bexarotene with or without topical steroids
- Systemic steroid or oral retinoids
- Peginterferon alpha-2a
- Mogamulizumab (anti-CCR4)
- Alemtuzumab (anti-CD52)
- Electron beam therapy / local radiotherapy
- Pagetoid reticulosis (JAAD Case Rep 2018;5:104, Mod Pathol 2000;13:502)
- High potency topical steroids
- PUVA
- Electron beam therapy / local radiotherapy
- Granulomatous slack skin (Dermatol Pract Concept 2020;10:e2020044, Eur J Cancer 2021;156:S35)
- PUVA
- Local corticosteroids
- Methotrexate
- Brentuximab vedotin
- Bexarotene
- Gemcitabine
- Doxorubicin
- Chemoimmunotherapy
- Radiotherapy
- Granulomatous mycosis fungoides (JAAD Case Rep 2015;1:298, Arch Dermatol 2008;144:1609)
- PUVA
- Low dose interferon alpha
- Chemotherapy
- Bexarotene
- Radiotherapy
- Pediatric mycosis fungoides (JAMA Dermatol 2021;157:431)
- Narrowband UVB
- Topical corticosteroids
- Syringotropic mycosis fungoides (Am J Surg Pathol 2011;35:100, J Am Acad Dermatol 2014;71:926)
- Topical steroids
- PUVA
- Bexarotene
- Hypopigmented mycosis fungoides (An Bras Dermatol 2013;88:954)
- Phototherapy
- Narrowband UVB
- Electron beam therapy / radiotherapy
Clinical images
Microscopic (histologic) description
- Folliculotropic mycosis fungoides (Arch Dermatol 2008;144:738, JAMA Dermatol 2021;157:157, J Am Acad Dermatol 2016;75:347, JAMA Dermatol 2016;152:992, Sci Rep 2021;11:10555, J Cutan Pathol 2020;47:241)
- Patterns observed include
- Folliculotropism with or without follicular mucinosis
- Eosinophilic folliculitis-like pattern
- Cystic pattern
- Basaloid lymphoid hyperplasia
- Granulomatous pattern
- Atypical lymphocytes infiltrate the epithelium of hair follicles (perifollicular and intrafollicular)
- Intensity should be determined for therapeutic and prognostic implications
- Mild (early stage)
- Intense (advanced stage)
- Intensity should be determined for therapeutic and prognostic implications
- Infiltrate often spares the epidermis or shows only minimal epidermotropism / Pautrier microabscesses
- Often (but not always) associated with mucinosis (follicular mucinosis), cystic dilatation and hyperplastic eccrine glands
- Papillary dermal fibrosis and syringotropism may be associated
- Often many eosinophils present
- Large cell transformation may occur
- Patterns observed include
- Pagetoid reticulosis (JAAD Case Rep 2018;5:104, Mod Pathol 2000;13:502, J Cutan Pathol 2014;41:703)
- Marked infiltrate of intraepidermal, medium to large, atypical hyperchromatic cerebriform lymphocytes and Pautrier microabscesses, as well as smaller and typical lymphocytes in the dermis and at the dermo-epidermal junction
- Hyperplasia and parakeratosis may be present
- Sponge-like disaggregation of epidermis and epidermal hyperplasia
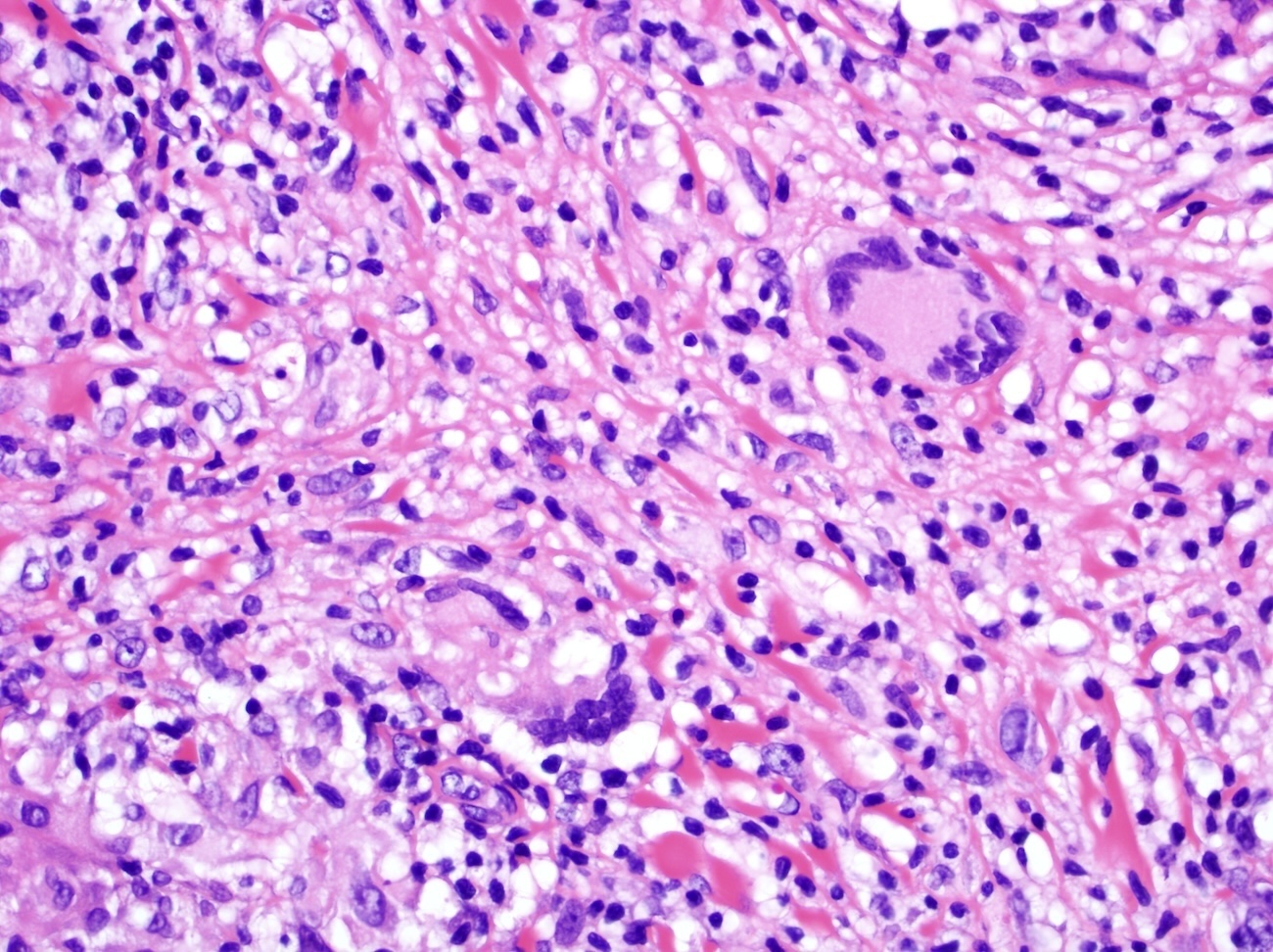
- Granulomatous slack skin and granulomatous mycosis fungoides (Dermatol Pract Concept 2020;10:e2020044, JAAD Case Rep 2015;1:298, Eur J Cancer 2021;156:S35, Arch Dermatol 2008;144:1609)
- Granulomatous slack skin and granulomatous mycosis fungoides have overlapping histology at presentation
- Infiltrate often shows destruction of elastic tissue by loose aggregates of histiocytes, including multinucleated forms (giant cells)
- Infiltrate is composed of small / intermediate atypical lymphocytes and macrophages
- Large multinucleated giant cells with a very increased number of nuclei are more frequent in granulomatous slack skin
- Elastophagocytosis and lymphophagocytosis may be present
- Epidermotropism is minimal or absent
- Eosinophils may be present
- Pediatric mycosis fungoides (JAMA Dermatol 2021;157:431)
- Similar histological presentation to classic mycosis fungoides but with CD8+ phenotype
- Syringotropic mycosis fungoides (Am J Surg Pathol 2011;35:100, J Am Acad Dermatol 2014;71:926)
- Hyperplastic eccrine ducts and glands infiltrated by atypical lymphocytes
- Often abundant eosinophils present
- Often seen in combination with folliculotropic mycosis fungoides
- Variable degree of syringometaplasia
- Similar to conventional mycosis fungoides but with postinflammatory pigment incontinence
- Hypopigmented mycosis fungoides (An Bras Dermatol 2013;88:954)
- Similar histologic presentation to classic mycosis fungoides but with CD8+ phenotype
Microscopic (histologic) images
Contributed by Roberto N. Miranda, M.D. and Carlos A. Torres-Cabala, M.D.
Peripheral smear description
- Variable and rare involvement of peripheral blood (Dermatol Pract Concept 2020;10:e2020044)
Positive stains
- CD4 (Acta Derm Venereol 2021;101:adv00537, Dermatol Pract Concept 2020;10:e2020044, Arch Dermatol 2008;144:738, Mod Pathol 2000;13:502, Sci Rep 2021;11:10555, J Cutan Pathol 2014;41:703, Arch Dermatol 2008;144:1609, JAMA Dermatol 2021;157:431)
- CD2, CD5, CD3, TCR βF1 (Arch Dermatol 2008;144:738, Cells 2024;13:419)
- CD45, CCR4 (Clin Cosmet Investig Dermatol 2022;15:1899)
- CD14+ / CD68+ monocytes in wreath-like pattern
- Associated with the loss of the elastic fibers are hallmarks of granulomatous slack skin
- Ki67 is variable (Mod Pathol 2000;13:502)
- > 30% in pagetoid reticulosis
Negative stains
- CD8 (Acta Derm Venereol 2021;101:adv00537, Dermatol Pract Concept 2020;10:e2020044, Arch Dermatol 2008;144:738, Mod Pathol 2000;13:502, J Cutan Pathol 2014;41:703, Arch Dermatol 2008;144:1609, JAMA Dermatol 2021;157:431, An Bras Dermatol 2013;88:954)
- Except for pagetoid reticulosis, pediatric and hypopigmented variants
- Pagetoid reticulosis
- Florid scattered in all epidermic levels
- TIA1 (Acta Derm Venereol 2021;101:adv00537, Dermatol Pract Concept 2020;10:e2020044, Arch Dermatol 2008;144:1609)
- Negative in mycosis fungoides, except for cases that are classically CD8 positive, such as pagetoid reticulosis
- CD7 is more often lost when compared to CD5 but CD5 loss is more specific for T cell lymphoma
- CD25 (Cells 2024;13:419)
- CD30 (Mod Pathol 2000;13:502, J Cutan Pathol 2014;41:703)
- When positive, it is usually expressed by large cells
- Usually positive in pagetoid reticulosis
- Not necessary for diagnosis of large cell transformation
- CD56 (JAMA Dermatol 2021;157:431)
- B cell antigens: CD19, CD20, PAX5, CD79a (Cells 2024;13:419)
- TCR γδ (Cells 2024;13:419)
Molecular / cytogenetics description
Sample pathology report
- Right eyebrow, skin punch:
- Primary cutaneous T cell lymphoma, most consistent with folliculotropic mycosis fungoides (see comment)
- Comment: According to clinical notes, the patient is a 37 year old man presenting with progressive and pruritic papules on his eyebrows of 8 months of evolution, with comedo-like features and associated with local alopecia. The lesions are also present in upper thorax and palmar / plantar regions. Sections show an adequate skin punch biopsy with intense infiltrate composed of atypical and small to intermediate in size lymphocytes in hair follicles. The infiltrate spares the epidermis and no epidermotropism is noted. Areas of follicular mucinosis and cystic dilatation are present. The atypical lymphoid infiltrate is diffusely positive for CD2, CD3, CD4 and T cell receptor beta (βF1). Atypical lymphocytes are negative for CD5, CD7, CD8 and T cell receptor gamma / delta (TCR γδ). Scattered cells are positive for CD30 and the proliferation index by Ki67 is ~40%. Molecular studies show monoclonal TCR gene rearrangement. These findings are, in the right clinical context, consistent with folliculotropic mycosis fungoides.
Differential diagnosis
- Lichen planopilaris (An Bras Dermatol 2022;97:348):
- Variant of frontal fibrosing alopecia
- Asymmetric, single or multifocal patches
- Perifollicular erythema and follicular scar
- Small lymphocytic lichenoid infiltrate with no atypia in the infundibuloisthmic portion of the hair follicle, with absent or rare involvement of interfollicular epidermis
- Lichenoid infiltrate is polyclonal
- Follicular psoriasis (Dermatol Online J 2020;26:13030):
- Uncommon variant of psoriasis characterized by folliculocentric hyperkeratotic eruptions on the trunk and extremities
- Follicular ostium is usually infiltrated by a mixed inflammatory infiltrate composed of neutrophils and small round to oval lymphocytes
- Polyclonal lymphoid infiltrate
- Papular mucinosis / scleromyxedema (J Scleroderma Relat Disord 2019;4:118):
- Usually presents as waxy and erythematous papules that start on upper extremities and spread to the forearms, trunk and face
- Histologically characterized by dermal mucin deposition and an increased number of fibroblasts
- Mild and superficial lymphoid infiltrate without atypia may be found in perivascular regions
- Polyclonal lymphoid infiltrate
- Lepromatous leprosy (J Trop Med 2022;2022:8652062):
- Usually affects patients with suboptimal cell mediated immunity in endemic areas
- Presents with macules, papules and plaques with lack of sensitivity
- Leonine facies may be observed in advanced stage disease
- Histologically presents with poorly circumscribed histiocytic infiltrate in the dermis and few scattered lymphocytes
- Macrophages may form globi and invade cutaneous adnexae
- Modified Ziehl-Neelsen stain is positive
- Cutaneous leishmaniasis (J Am Acad Dermatol 2015;73:911):
- Pityriasis rubra pilaris (JAMA Dermatol 2016;152:670):
- Diffuse and confluent plaques in elbows and knees and scaling papules on palms and soles
- Association with other cutaneous tumors
- Orthohyperkeratosis and parakeratosis associated with mild lymphoid infiltrate with no atypia and centered in perivascular and perifollicular regions
- Polyclonal lymphoid infiltrate
- Primary cutaneous CD8+ aggressive epidermotropic cytotoxic T cell lymphoma (Mod Pathol 2017;30:761):
- Rapidly progressive and aggressive disease
- Presents with eruptive papules, patches, plaques and nodules (or tumors) with central ulceration and necrosis
- May present with hyperkeratotic patches and plaques
- Prominent epidermotropism of medium to large atypical cells
- CD3+ / CD4- / CD8+ / TIA1+
- Usually treated with multiagent chemotherapy and allogeneic or autologous stem cell transplantation
- Lymphomatoid papulosis (LyP) type D (J Cutan Pathol 2014;41:88, Histopathology 2015;67:425):
Additional references
Board review style question #1
Which of the following statements is correct about subtypes of mycosis fungoides?
- Folliculotropic mycosis fungoides has an identical histologic presentation as classic mycosis fungoides and it is distinguished by its clinical presentation
- Folliculotropic mycosis fungoides is usually CD4+ / CD8-, while pagetoid reticulosis (Woringer-Kolopp disease) is usually CD4- / CD8+
- Granulomatous slack skin and granulomatous mycosis fungoides have the same clinical presentation and only histologic features may distinguish them
- Pagetoid reticulosis (Woringer-Kolopp disease) usually is a disseminated disease with a very aggressive clinical course
Board review style answer #1
B. Folliculotropic mycosis fungoides is usually CD4+ / CD8-, while pagetoid reticulosis (Woringer-Kolopp disease) is usually CD4- / CD8+. Answer A is incorrect because folliculotropic mycosis fungoides usually presents with hair follicle infiltration with minimal epidermotropism and dense interfollicular involvement, while classic mycosis fungoides is characterized by the prominent epidermotropism. Answer D is incorrect because pagetoid reticulosis (Woringer-Kolopp disease) is usually an indolent, localized disease and rare cases have a fatal outcome. Answer C is incorrect because granulomatous slack skin and granulomatous mycosis fungoides have similar histologic presentations but different clinical features. Granulomatous slack skin usually presents with pendulous skin in axillae, inguinal and gluteal regions, while granulomatous mycosis fungoides often shows the same clinical presentation as classic mycosis fungoides.
Comment Here
Reference: Mycosis fungoides subtypes
Comment Here
Reference: Mycosis fungoides subtypes
Board review style question #2
Which of the following statements about granulomatous slack skin is correct?
- It is a self limited disease with a benign clinical course and prognosis
- It is the most common subtype of mycosis fungoides and often presents in children
- Most cases involve blood, liver and spleen
- Most commonly affects the axillae, inguinal and gluteal regions
Board review style answer #2
D. Most commonly affects the axillae, inguinal and gluteal regions. Answer B is incorrect because granulomatous slack skin is a very rare variant of mycosis fungoides and often presents in young adults. Answer C is incorrect because very rare cases have systemic involvement (blood, liver and spleen). Answer A is incorrect because, although the disease is indolent and the survival rate is good, most patients have persistent disease.
Comment Here
Reference: Mycosis fungoides subtypes
Comment Here
Reference: Mycosis fungoides subtypes