Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1Cite this page: Alves de Castro JV, Jaffe ES. Mediastinal gray zone lymphoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lymphomamediastinalgrayzone.html. Accessed March 30th, 2025.
Definition / general
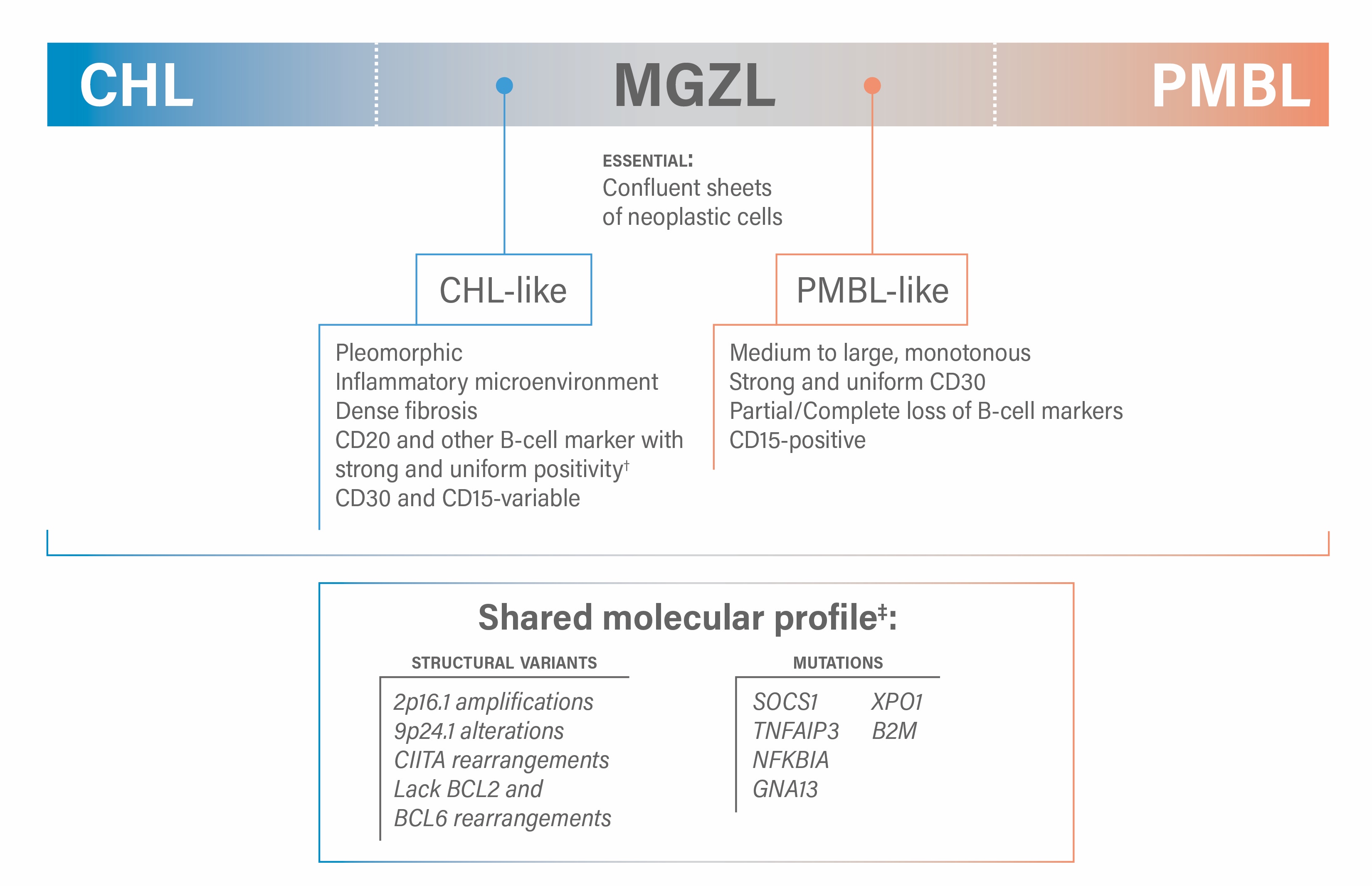
- Mediastinal gray zone lymphoma (MGZL) is an aggressive B cell lymphoma that arises in the mediastinum and shows asynchronous morphologic and immunophenotypic features between classic Hodgkin lymphoma (CHL) and primary mediastinal large B cell lymphoma (PMBL)
Essential features
- Aggressive B cell lymphoma presenting with mediastinal involvement
- Sheets of neoplastic cells (high tumor density) with broad morphological spectrum
- 2 morphologic and immunophenotypic scenarios: one resembling CHL morphology but with an immunophenotype closer to PMBL and another resembling PMBL morphology with immunophenotype closer to CHL; composite lymphomas with separate areas of PBML and of CHL are not considered MGZL
- MGZL cases are Epstein Barr virus (EBV) negative; there is an ongoing controversy in the literature if EBV positive MGZL can be accepted, without clear criteria to establish such a diagnosis
Terminology
- Mediastinal gray zone lymphoma
- B cell lymphoma, unclassifiable, with features between diffuse large B cell lymphoma and classical Hodgkin lymphoma (obsolete)
- Large B cell lymphoma with Hodgkin features (obsolete)
- Hodgkin-like anaplastic large cell lymphoma (obsolete)
ICD coding
Epidemiology
- M > F
- Median age range is 20 - 40 years
- Less frequent in African American and Asian populations
- References: Am J Surg Pathol 2005;29:1411, Mod Pathol 2011;24:1586, Blood 2014;124:1563, Blood 2021;137:1765
Sites
- Anterior mediastinum
- Involvement of supraclavicular and cervical lymph nodes may be seen
- Involvement of nonhematopoietic organs is rare
- Nonmediastinal cases are exceedingly rare and controversial
- Nonmediastinal gray zone lymphoma (GZL) is not recognized by the International Consensus Classification (ICC) since such cases are more closely related to diffuse large B cell lymphoma, NOS (DLBCL, NOS) (Blood 2021;137:1765)
- 5th edition of the WHO mentions gray zone lymphoma with primary extramediastinal presentation as a disseminated disease while acknowledging that there is no consensus on its precise definition and that this diagnosis should be used with great caution in routine practice
Pathophysiology
- Immune escape (Mod Pathol 2011;24:1586)
- Amplification of 9p24.1, including the PDL1 gene locus
- Downregulation of MHC class II proteins due to CIITA translocations
- NFκB and JAK / STAT pathway activation (Blood 2021;137:1765)
- Common mutations in TNFAIP3 and SOCS1 as well as NFKBIE
- Amplification of 9p24.1 includes JAK2
- Microenvironmental signature closer to CHL (Blood Cancer Discov 2020;1:155)
Etiology
- Unknown
Diagrams / tables
Clinical features
- Cough
- Dyspnea
- Superior vena cava syndrome
- B symptoms (fever and night sweats)
- Reference: Blood Adv 2017;1:2600
Diagnosis
- Requires a tissue biopsy to confirm the histopathologic features of the disease
Laboratory
- Elevated lactate dehydrogenase (LDH) in a substantial proportion of patients
- Anemia
- Hypoalbuminemia
- References: Blood 2021;137:1765, Blood 2014;124:1563
Radiology description
- Anterior mediastinal mass, which can be bulky (Blood 2014;124:1563)
Prognostic factors
- Adverse prognostic factors
- Low lymphocyte count
- Eastern Cooperative Oncology Group (ECOG) performance status over 1 correlates with poor event free survival (EFS) and overall survival
- Anemia (< 10.5 g/dL)
- Hypoalbuminemia (3 year progression free survival [PFS]; hypoalbuminemia [< 4.0 g/dL] versus normal albumin: 64% versus 12%; P [p value] = .01)
- CD15 expression, as observed in 54% of MGZL patients in the Wilson et al. cohort, correlated with worse EFS (Blood 2014;124:1563)
- References: Haematologica 2017;102:150, Br J Haematol 2017;179:503, Blood Adv 2017;1:2600, Blood 2014;124:1563
Case reports
- 47 year old woman presented with neck swelling and shortness of breath (Cureus 2023;15:e37096)
- 69 year old woman with a mass on the right side of the neck (World J Clin Cases 2022;10:5708)
Treatment
- Currently, no consensus regarding optimal treatment
- DA-EPOCH-R (dose adjusted etoposide, prednisone, vincristine, cyclophosphamide, doxorubicin and rituximab) (Blood 2014;124:1563, Br J Haematol 2016;174:345)
- R-CHOP (rituximab, cyclophosphamide, doxorubicin hydrochloride, vincristine and prednisone) (Blood Adv 2017;1:2600, Br J Haematol 2016;174:345)
- Hodgkin-like treatments (doxorubicin hydrochloride [Adriamycin], bleomycin sulfate, vinblastine sulfate and dacarbazine [ABVD]) seem less effective (Br J Haematol 2017;179:503)
- Consolidative radiotherapy for localized / bulky disease has also been advocated (Br J Haematol 2016;174:345)
Gross description
- Fish flesh appearance, often with areas of necrosis
- Fibrosis may be evident, leading to areas of nodularity
Frozen section description
- It is not advisable to make a diagnosis of MGZL exclusively based on the assessment of a frozen section slide; immunophenotypic studies are essential for the diagnosis
Microscopic (histologic) description
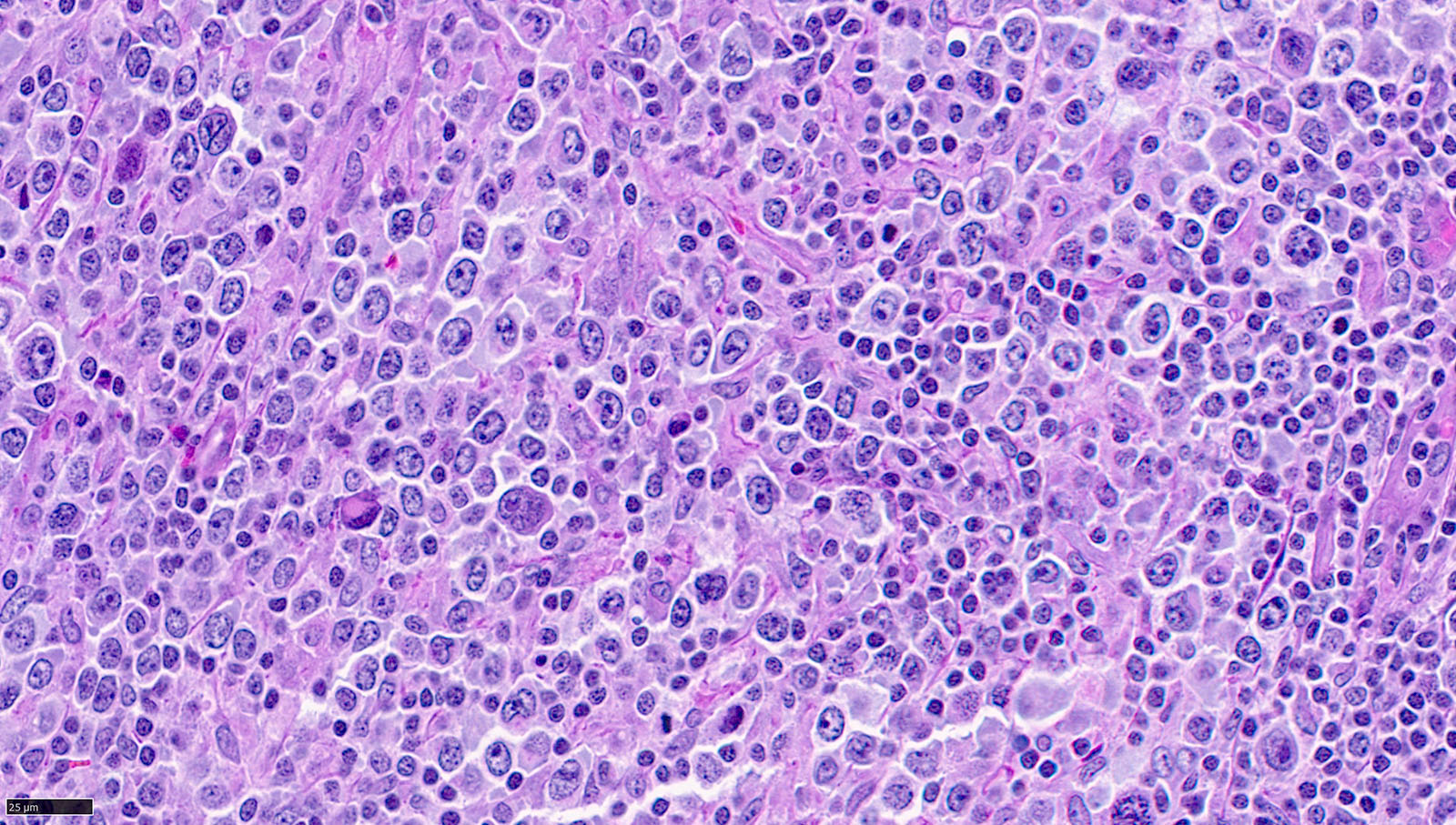
- Tumor cell richness is essential to the diagnosis (Virchows Arch 2023;482:207, Blood Adv 2017;1:2600)
- Broad morphologic spectrum, with more pleomorphism than expected for PMBL, is a key feature (Blood Adv 2017;1:2600)
- Cases with a CHL-like appearance have features resembling the syncytial variant (grade 2) of nodular sclerosis CHL but with more variation in the cytologic spectrum (i.e., showing centroblastic / large cell cytology) (Virchows Arch 2023;482:207)
- Cases with a PMBL-like appearance have features resembling PMBL (i.e., fine compartmentalizing sclerosis and clear cytoplasm) but usually with more pleomorphism (Virchows Arch 2023;482:207)
- Tumor microenvironment is usually less prominent than what is expected for CHL, being rich in macrophages and small T cells
Microscopic (histologic) images
Positive stains
- CD30: strongly positive in 90 - 100% of cases in both subtypes of MGZL but can be less uniform than in CHL (Virchows Arch 2023;482:207)
- B cell markers: in CHL-like, at least 2 should be strongly and diffusely positive; in PMBL-like, the intensity is more variable
- CD15: often strong in PMBL-like cases
- CD23
- PDL1 (Eur J Haematol 2018;100:511)
- References: Blood Adv 2017;1:2600, Virchows Arch 2023;483:733
Negative stains
- CD15: often negative or variable in CHL-like cases
- B cell markers: loss of the B cell program should be seen in PMBL-like cases
- LMP1
- References: Blood Adv 2017;1:2600, Virchows Arch 2023;483:733
Molecular / cytogenetics description
- EBV encoded small RNAs (EBER) in situ hybridization should be negative in the vast majority of cases
- Positivity strongly favors alternative diagnoses such as EBV positive diffuse large B cell lymphoma (DLBCL)
- Cytogenetics (Mod Pathol 2011;24:1586)
- Amplifications: 9p24.1; 2p16.1
- CIITA translocations
- Lack of BCL2 and BCL6 rearrangements (Blood 2021;137:1765)
- Gene expression profile: intermediate between CHL and PMBL but closer to CHL (Blood Cancer Discov 2020;1:155)
- Downregulated: germinal B cell and IFN regulatory factor 4 (IRF4) signatures
- Upregulated: T cell and macrophage signatures, NFκB signaling
- Genomics: mutations in SOCS1 (40%), TNFAIP3 (20%), NFKBIA (29%), GNA13 (24%), XPO1 (16%) and B2M (32%)
- Epigenetics: methylation array analysis of laser capture microdissected samples reveals an intermediate but distinct profile between CHL and PMBL (Haematologica 2011;96:558)
Sample pathology report
- Lymph node, supraclavicular, excisional biopsy:
- Mediastinal gray zone lymphoma (see comment)
- Comment: Sections of the lymph node reveal effacement of the normal nodal architecture by an atypical infiltrate in a vaguely nodular pattern and a background of dense fibrosis. The atypical infiltrate is composed of medium to large cells with round to irregular nuclear contours, vesicular chromatin and occasionally prominent nucleoli, especially in larger forms, admixed with small lymphocytes and histiocytes.
- The large, atypical cells are positive for CD30, CD15, PAX5 (weak), CD79a (weak), CD19, MUM1, CD45 and CD23 (subset). They are negative for CD10, BCL6 and CD20. EBER stain is negative. The proliferation index (Ki67) is high, estimated as 80% of the neoplastic cells. CD3 highlights numerous T cells in the background.
- These findings are consistent with mediastinal gray zone lymphoma. The features show morphology and phenotype overlapping with both classic Hodgkin lymphoma and primary mediastinal large B cell lymphoma (PMBL), fulfilling the criteria for mediastinal gray zone lymphoma.
Differential diagnosis
- Classic Hodgkin lymphoma:
- Downregulation of B cell markers is characteristic of CHL
- CD15 is seen more frequently in CHL than in MGZL
- Primary mediastinal large B cell lymphoma:
- Less pleomorphism than MGZL
- Usually CD15 negative
- Has a preserved expression of B cell markers
- EBV positive diffuse large B cell lymphoma, NOS:
- EBV is negative in the majority of MGZL cases
- EBV positive MGZL is acceptable in mediastinal cases with otherwise typical features of MGZL
- EBV positive polymorphic B cell lymphoproliferative disorder (LPD), NOS:
- In EBV positive polymorphic B cell LPD, NOS, the EBER positive cells show a wide range of cell sizes
- EBV positive MGZL is acceptable in mediastinal cases with otherwise typical features of MGZL; the neoplastic cells are larger and more pleomorphic than in EBV positive polymorphic B cell LPD, NOS
- Peripheral T cell lymphoma (PTCL) with Hodgkin / Reed-Sternberg (HRS)-like cells:
- PTCL with HRS-like cells demonstrates significant atypia in the background T cells
- HRS-like cells have a B cell phenotype and a significant proportion are EBV positive (Am J Surg Pathol 1999;23:1233, Am J Surg Pathol 2017;41:506)
- TCR clonality is positive in PTCL with HRS-like cells
Additional references
Board review style question #1
A 33 year old man presents with chronic cough and B symptoms for 3 months. During clinical workup, he is found to have an anterior mediastinal mass measuring up to 8 cm. The histopathological evaluation of a mediastinoscopy specimen reveals the findings shown in the figure above. Which of the following is correct about the possible differential diagnoses?
- Among the diagnostic possibilities, MGZL is less aggressive than classic Hodgkin lymphoma (CHL) and primary mediastinal large B cell lymphoma (PMBL)
- EBV positivity would be helpful in the current scenario, favoring MGZL over PMBL
- Given the pleomorphic appearance and sheets of neoplastic cells, mediastinal gray zone lymphoma (MGZL) is a possibility
- Lack of CD30 positivity is characteristic of MGZL due to its intermediate features between CHL and PMBL
Board review style answer #1
C. Given the pleomorphic appearance and sheets of neoplastic cells, mediastinal gray zone lymphoma (MGZL) is a possibility. Sheets of neoplastic cells are essential to the diagnosis of MGZL and greater pleomorphism than PMBL is usually seen. Answer A is incorrect because MGZL is more aggressive than both CHL and PMBL. Answer D is incorrect because MGZL is CD30 positive in the vast majority of cases. Answer B is incorrect because EBV positivity is very rare in MGZL and should prompt consideration of alternative diagnoses such as EBV positive diffuse large B cell lymphoma, NOS.
Comment Here
Reference: Mediastinal gray zone lymphoma
Comment Here
Reference: Mediastinal gray zone lymphoma