Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Dcunha NJ, Sigamani E. Lymphomatoid granulomatosis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lymphomalymphomatoidgran.html. Accessed March 31st, 2025.
Definition / general
- Lymphomatoid granulomatosis is an angiocentric and angiodestructive lymphoproliferative disease involving extranodal sites composed of Epstein–Barr virus (EBV) positive B cell admixed with reactive T cells, which usually predominate (Blood 2016;127:2375)
Essential features
- Angiocentric and angiodestructive lymphoproliferative disease involving extranodal sites composed of EBV positive B cell admixed with reactive T cells
Terminology
- Angiocentric immunoproliferative lesion
ICD coding
Epidemiology
- Very rare
- Usually occurs in adults; sometimes seen in children with immunodeficiency disorders (Cancer 1979;43:360)
- M:F ≥ 2:1
- More common in western countries than in Asia (Am J Surg Pathol 2015;39:141)
Sites
- Pulmunary involvement > 90% patients (Cancer 1979;43:360)
- Other common sites include: brain, kidney, liver and skin (Am J Surg Pathol 2010;34:e35, Arch Dermatol 1996;132:1464)
- Uncommon sites include: upper respiratory tract and gastrointestinal tract (Am J Surg Pathol 1999;23:1356)
- Rare sites: lymph nodes and spleen (Am J Surg Pathol 2015;39:141, Indian J Pathol Microbiol 2018;61:228)
Pathophysiology
- Lymphomatoid granulomatosis due to the predominance of T cells on pathologic examination, was initially thought to be a T cell disorder (Am J Med 1982;72:467)
- Subsequently, lymphomatoid granulomatosis was determined to be a B cell lymphoproliferative disorder secondary to EBV, with a prominent angiocentric T cell infiltrate (Mod Pathol 1990;3:435)
- Lymphomatoid granulomatosis has a complex relationship with the host’s underlying immune function and defective immune surveillance of EBV infected B cells, particularly a functional defect in CD8+ cytotoxic T cells, is hypothesized to lead to disease development (Blood 1996;87:4531)
- Particular study suggests that immunologic deficits are likely preexistent and that a quantitative or qualitative defect in mainly CD8+ cytotoxic T cells may be prerequisite for disease (Cancer 1982;49:2070)
Etiology
- Resembles an EBV driven lymphoproliferative disorder (Blood 1996;87:4531)
- Also common in many immunodeficiency states, such as AIDS, allogenic organ transplant, Wiskott-Aldrich syndrome and X linked lymphoproliferative syndrome (Cancer Surv 1997;30:233)
- Normal counterpart: mature B cell, transformed by EBV (Blood 2016;127:2375)
Clinical features
- Most commonly: cough, dyspnea and chest pain (Am J Surg Pathol 2010;34:e35, Am J Surg Pathol 2015;39:141)
- Other common symptoms: fever, malaise, weight loss, neurological symptoms, arthralgias, myalgia and gastrointestinal symptoms (Am J Surg Pathol 1999;23:1356)
- Patients with CNS disease; may show diplopia, hearing loss, dysarthria, ataxia, altered mental status or be asymptomatic (Radiology 2005;237:265)
- Skin manifestations can be painful and include subcutaneous nodules, dermal nodules, maculopapular eruptions, macular erythema and ulcerations (Dermatol Clin 2015;33:489)
- Few patients (2.8%) are asymptomatic (Cancer 1979;43:360)
Diagnosis
- Combination of light microscopy and immunohistochemical markers or in situ hybridization for EBV coded small RNA (EBER)
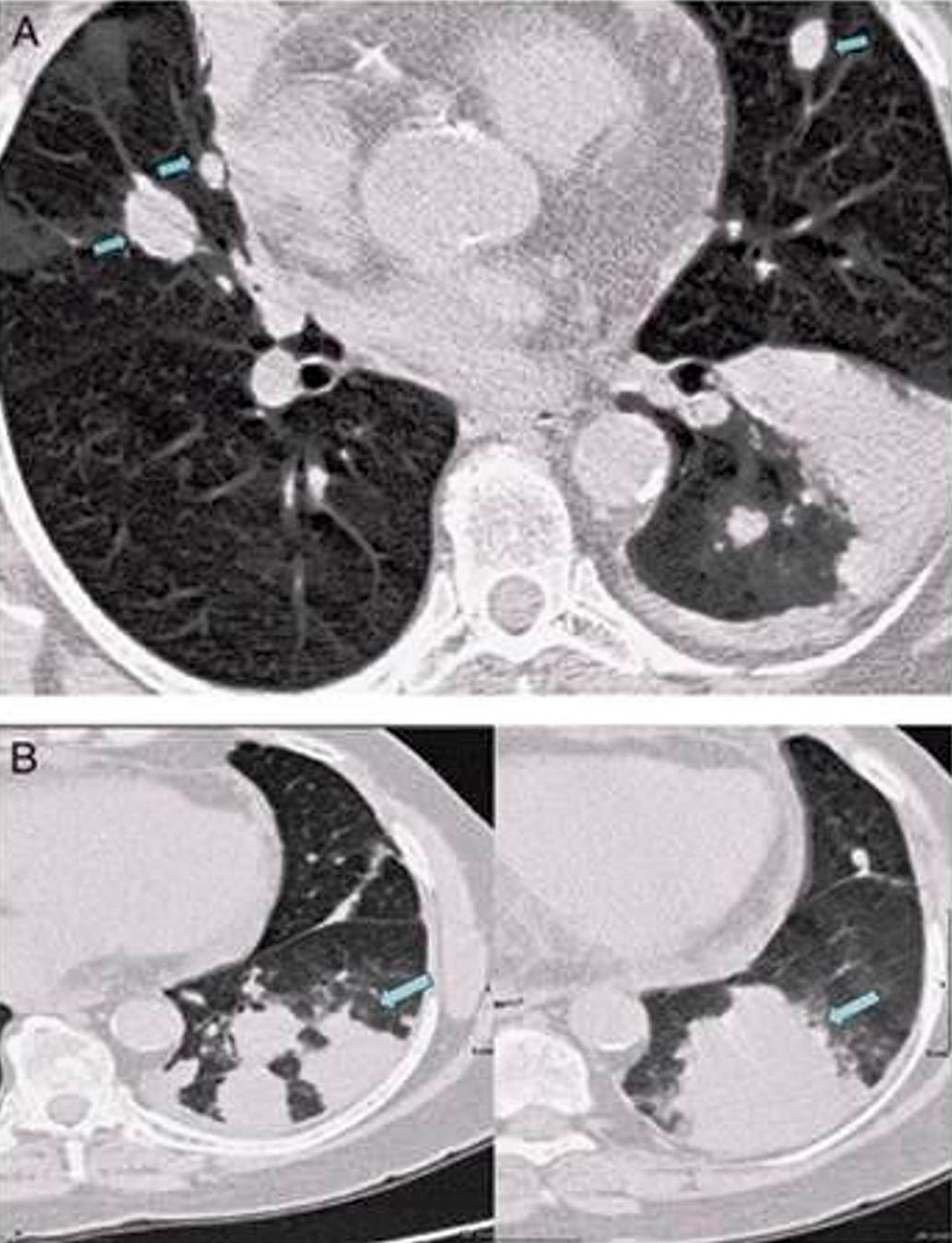
Radiology description
- Chest Xray may show single or multiple nodules with poorly defined margins
- CT scans show well defined and poorly defined nodules throughout both lungs (AJR Am J Roentgenol 2000;175:1335)
Radiology images
Prognostic factors
- Prognostic features are difficult to determine due the rarity of the disease
Case reports
- 14 year old boy with trisomy 21 and history of B lymphoblastic leukemia / lymphoma diagnosed 1.5 years previously on maintenance chemotherapy, with right lower lobe consolidation (Fetal Pediatr Pathol 2018;37:7)
- 22 year old man with lymphomatoid granulomatosis of the CNS (Neuropathology 2019;39:479)
- 56 year old renal allograft recipient; 11 years after transplantation (Transpl Infect Dis 2008;10:52)
- 72 year old woman with asymptomatic right lung mass (Arch Bronconeumol 2018;54:108)
- 79 year old man with bulky lung mass (Intern Med 2018;57:3163)
Treatment
- In a prospective NCI study, patients with low grade lymphomatoid granulomatosis received primary therapy with IFN-α while patients with high grade lymphomatoid granulomatosis received primary therapy with DA-EPOCH-R (dose adjusted etoposide, prednisone, vincristine, cyclophosphamide, doxorubicin and rituximab) every 3 weeks for up to 6 cycles of therapy (Blood 2018;132:785)
Gross description
- Lesions in the lung are mainly nodular and involve middle and lower lung fields; may exhibit central necrosis and cavitate (Am J Surg Pathol 2010;34:e35, Arch Dermatol 1996;132:1464)
- Kidney and brain lesions are also nodular and associated with central necrosis (Am J Surg Pathol 2015;39:141)
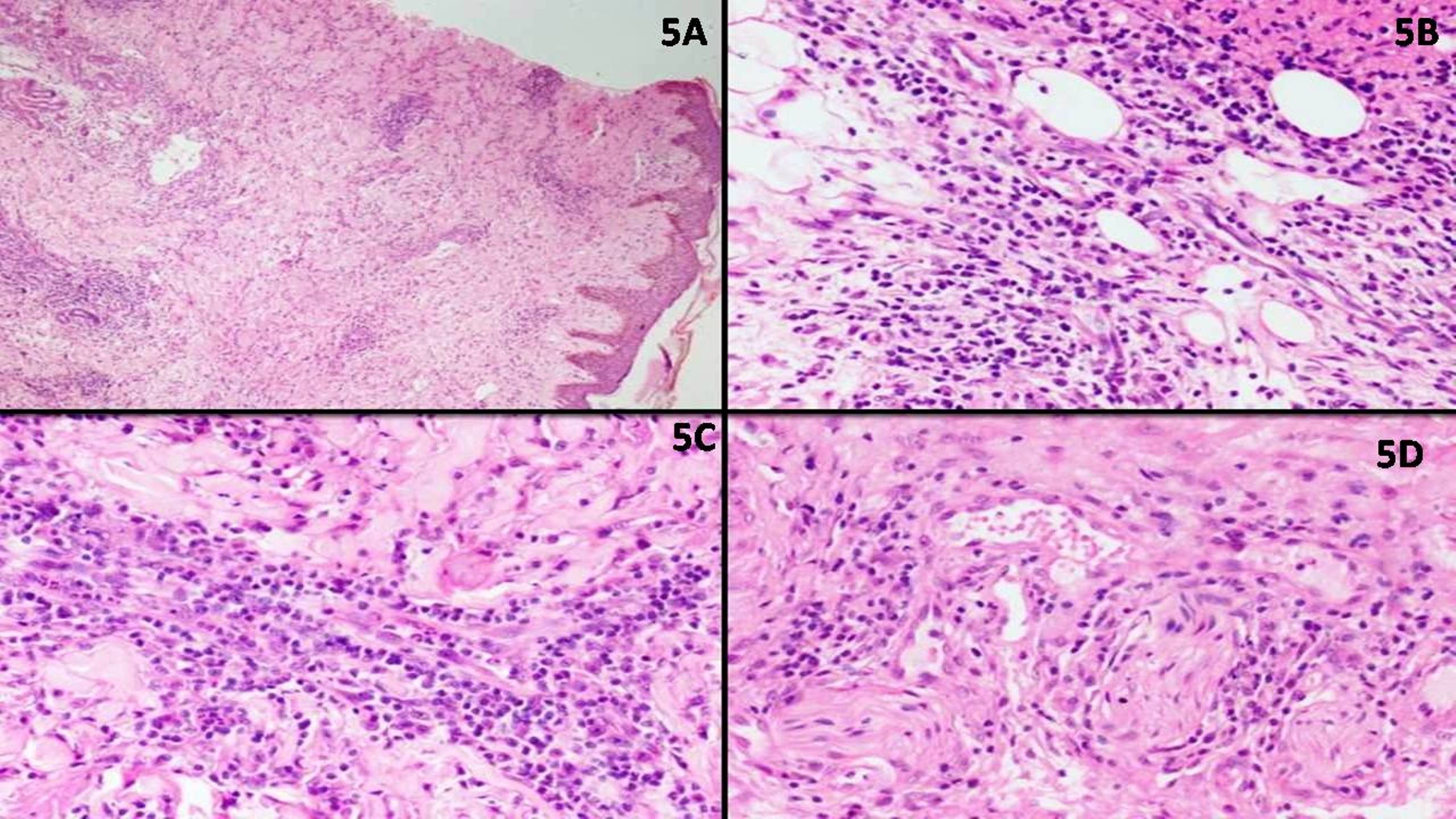
- Skin lesions range from nodules in subcutaneous tissue to dermal ulcers with necrosis; occasionally plaques or maculopapular rash-like presentation (Am J Surg Pathol 2001;25:1111)
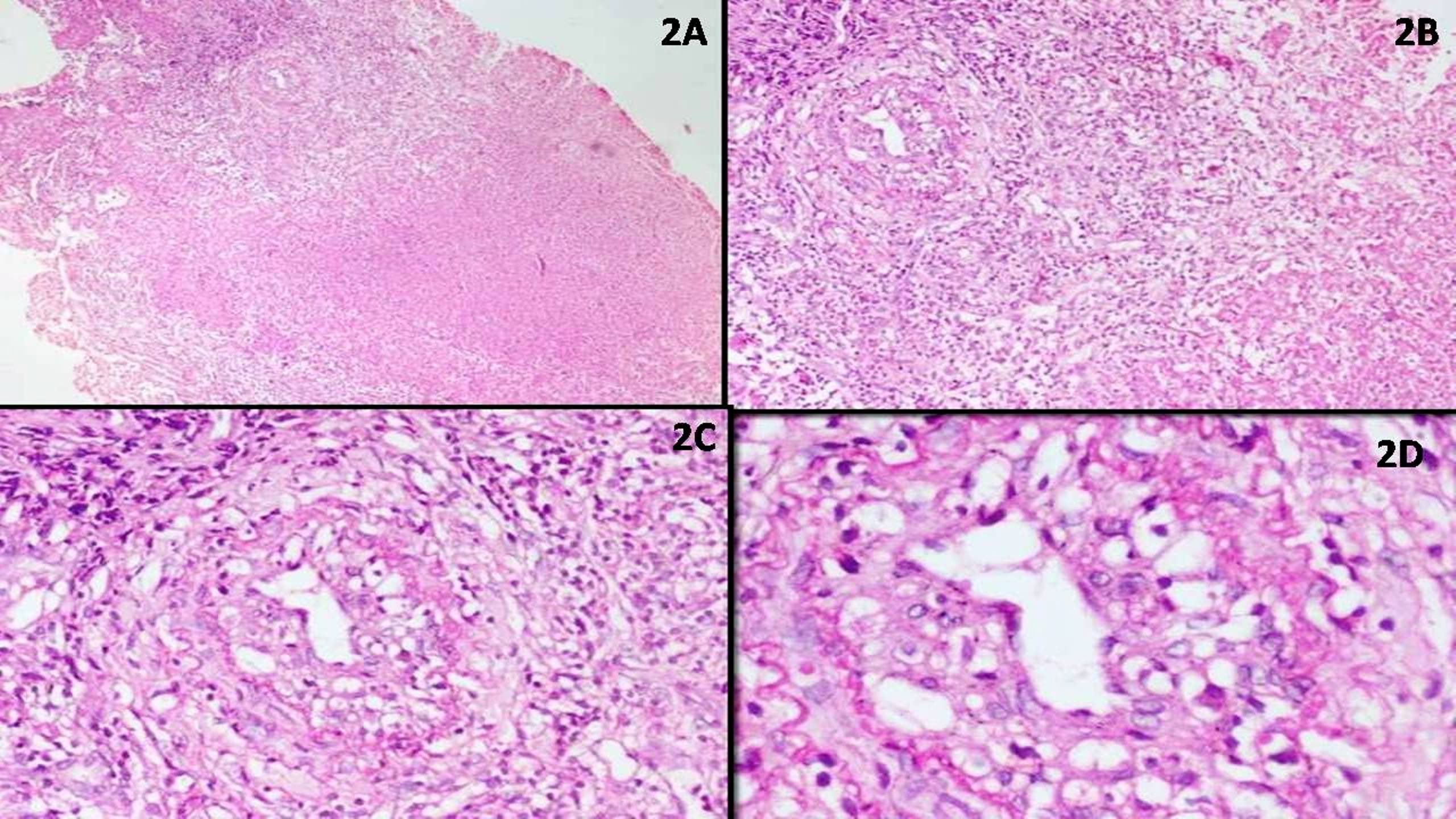
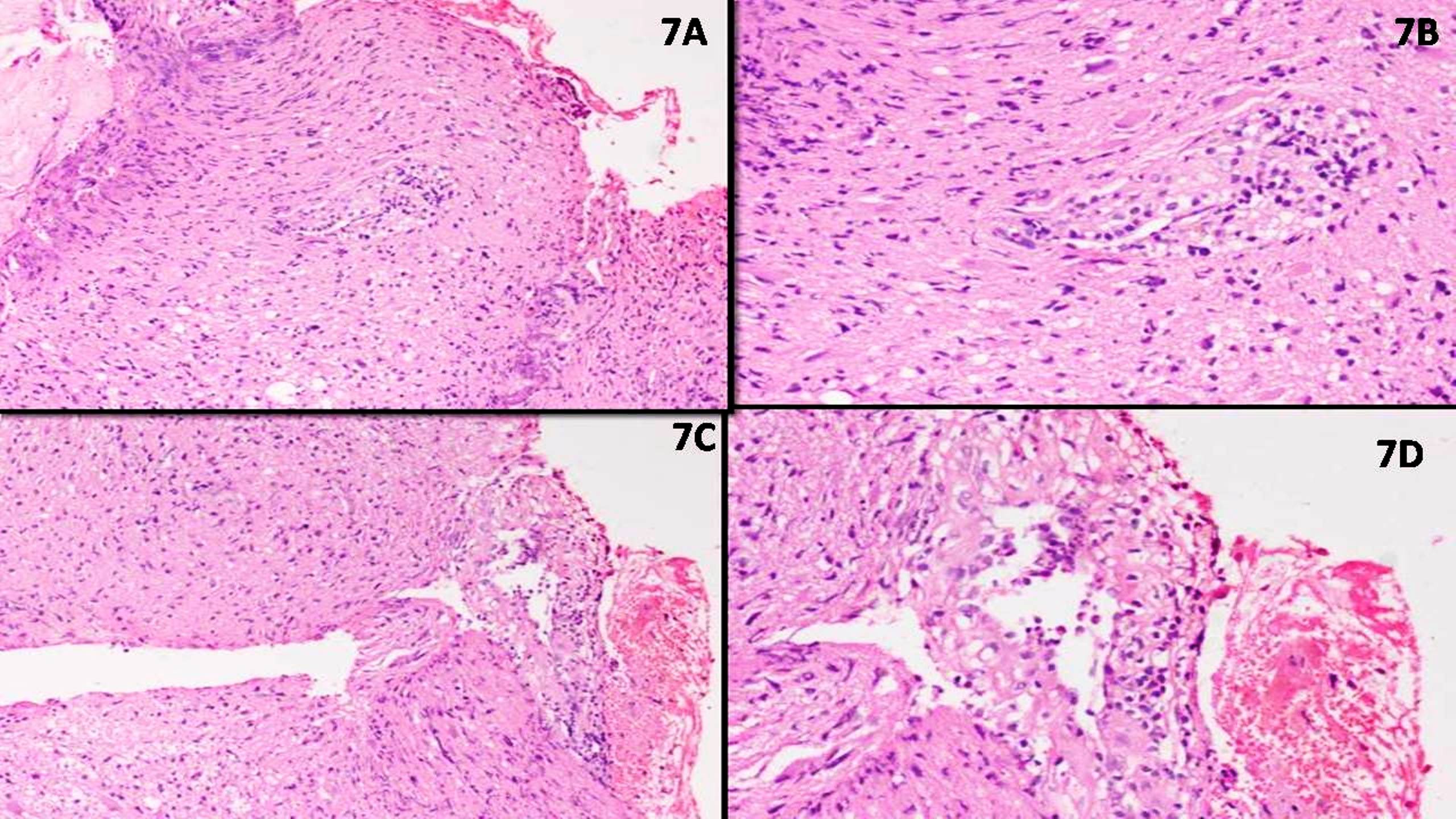
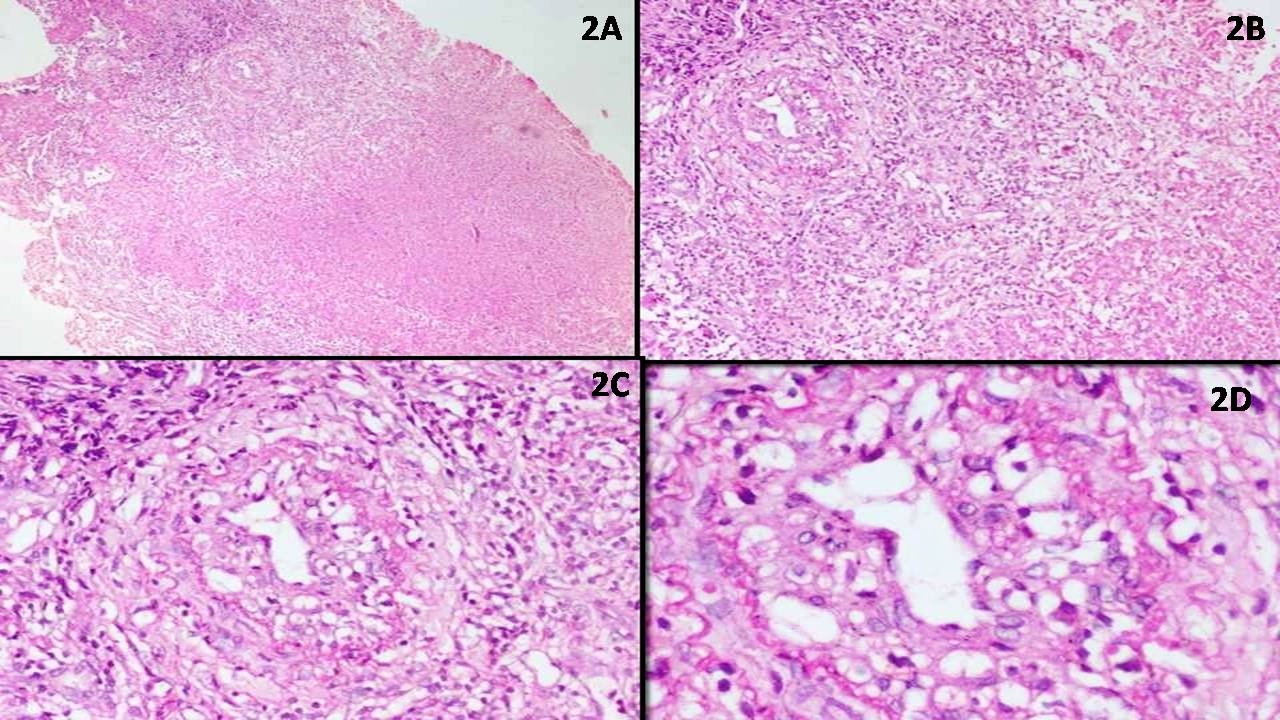
Microscopic (histologic) description
- Angiocentric and angiodestructive polymorphous lymphoid infiltrate (Cancer 1979;43:360)
- Lymphocytic vasculitis with infiltration of the vessel wall; may also show infarct like tissue necrosis or fibrinoid necrosis of vessel wall (Blood 1997;90:4099)
- Infiltrate is predominantly composed of lymphocytes with admixed plasma cells, immunoblasts and histiocytes; background lymphocytes; may show atypia but are not overtly neoplastic
- Lymphomatoid granulomatosis is composed of variable number of EBV positive B cells admixed with inflammatory background (Am J Surg Pathol 2010;34:e35)
- EBV positive cells resemble immunoblasts or are multinucleated; may show atypia
- Classic Reed-Sternberg cells are absent
- Well formed granulomas are typically not seen in lungs and most other extranodal sites except skin where granulomatous reaction might be seen in subcutaneous tissue (Am J Surg Pathol 2001;25:1111)
- Grading is based on the relative number of EBV positive B cells to the reactive lymphocyte background (Am J Surg Pathol 2015;39:141)
- Grade I: EBV positive cells are < 5 per high power field; absent or rare large transformed cells on light microscopy; necrosis if present is focal
- Grade II: EBV positive cells are 5 - 50 per high power field; few large transformed cells on light microscopy; necrosis is more commonly seen
- Grade III: EBV positive cells are > 50 per high power field; large transformed cells are easily seen on light microscopy; large areas of necrosis are common
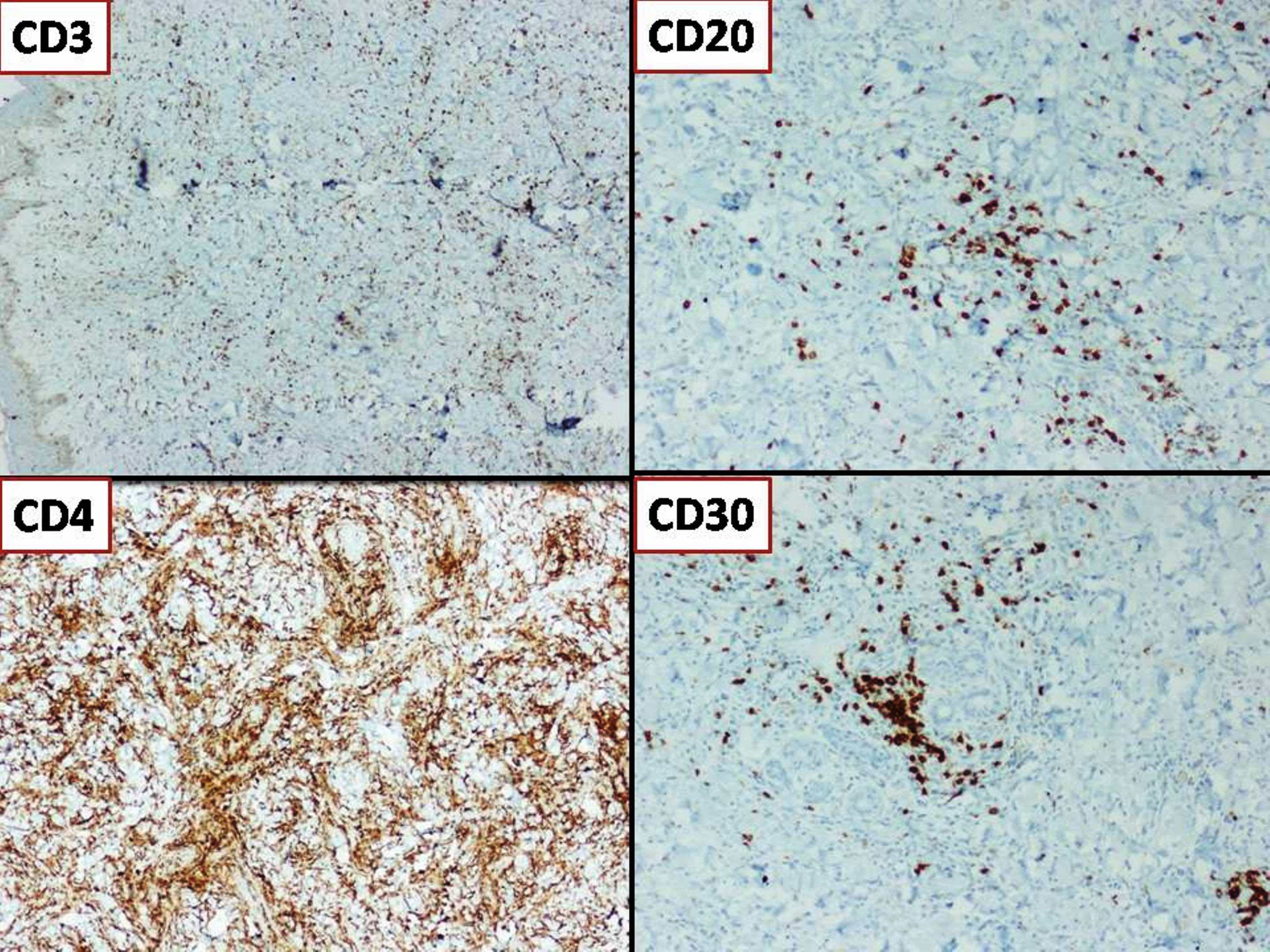
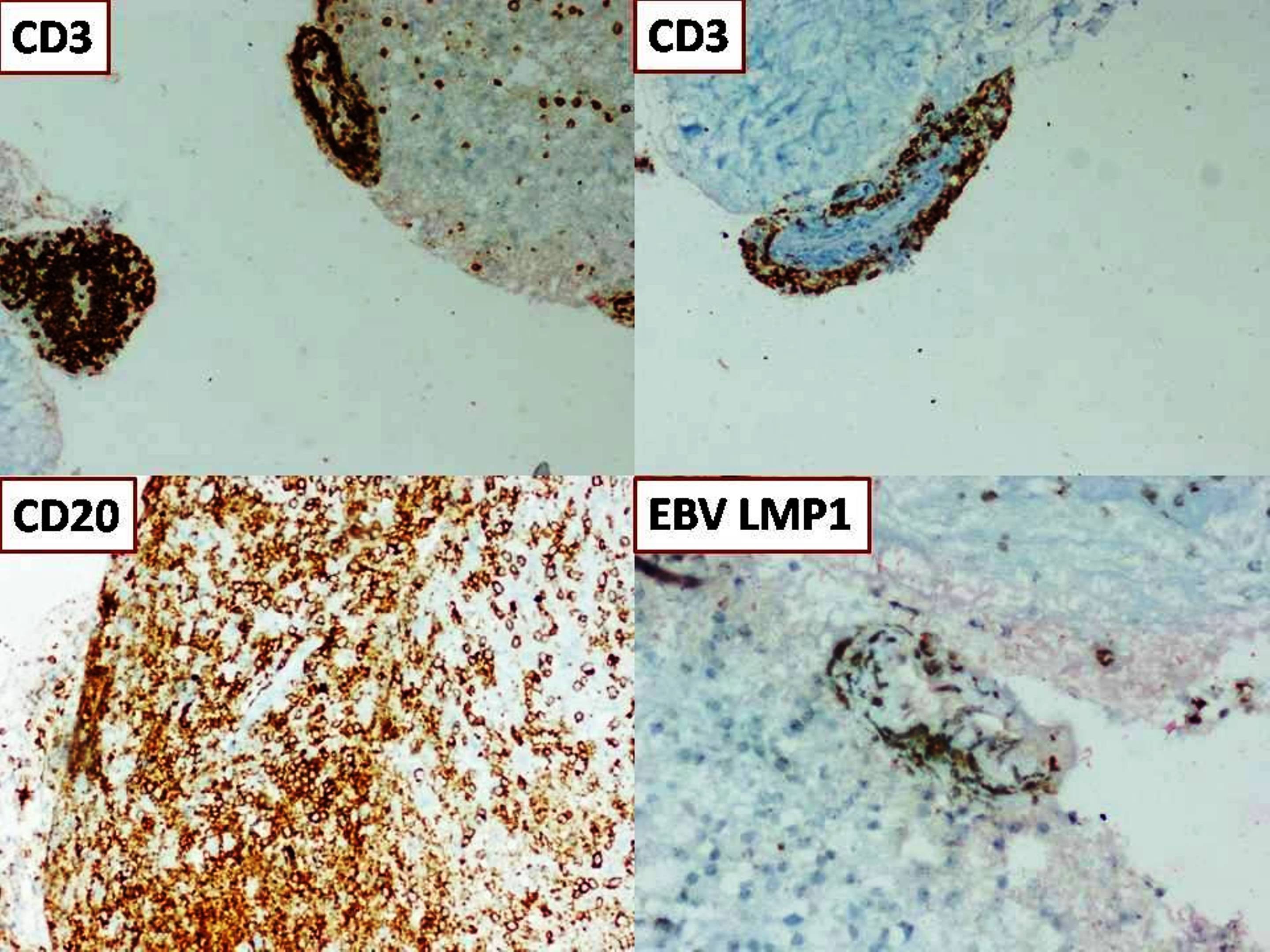
Microscopic (histologic) images
Contributed by Nicholas Joseph Dcunha, M.B.B.S., M.D. and Elanthenral Sigamani, M.B.B.S., M.D.
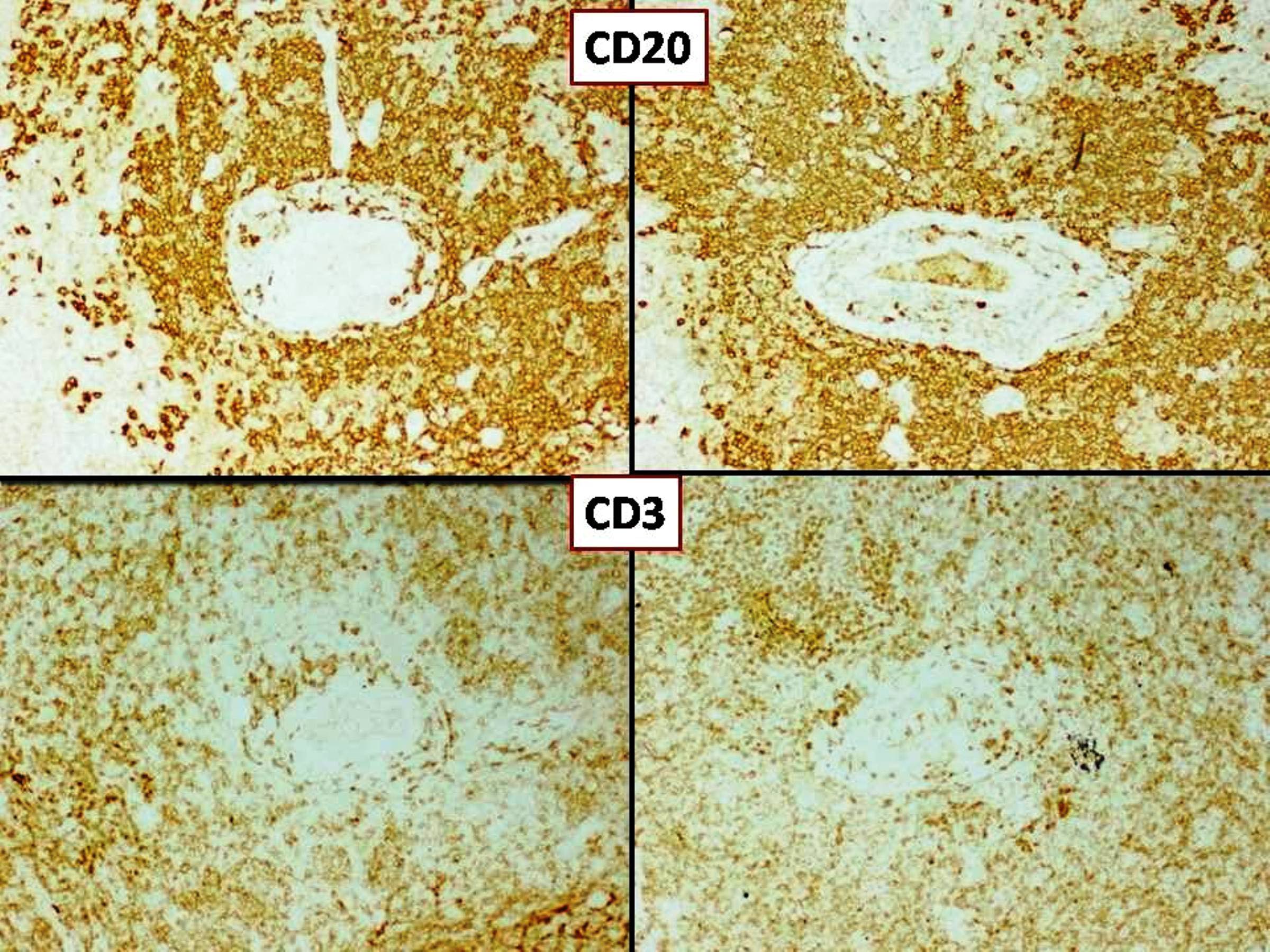
Positive stains
- B cell component: CD20, EBV LMP1, EBER, CD30 (variably) (Am J Surg Pathol 1998;22:1093)
- EBNA2 is frequently positive, consistent with latency type III (Am J Surg Pathol 2015;39:141)
- Background T cells: CD3 with CD4 more often than CD8 (Am J Surg Pathol 2015;39:141)
Negative stains
Molecular / cytogenetics description
- Most cases of grade II and III lymphomatoid granulomatosis show clonality for IG genes (Am J Surg Pathol 1994;18:753)
- Clonality of grade I lymphomatoid granulomatosis is less consistent; some cases of lymphomatoid granulomatosis might be polyclonal (Am J Surg Pathol 2015;39:141)
- T cell receptor (TR) genes do not show clonality (Hum Pathol 1991;22:1150)
Sample pathology report
- Lung tissue, bronchoscopic biopsy:
- Lymphomatoid granulomatosis, grade I, biopsies from left lung, upper and lower lobes (see comment)
- Comment: The small reactive lymphoid cells are CD3 positive. The scattered large cells are positive for CD20 and CD79a and show faint membrane positivity for EBV LMP1. The MIB1 proliferation index is low (approximately 10 - 20%). Special stains for microorganisms (AFB TB, PASD, GMS) are negative.
- Microscopic description: Dense interstitial and diffuse infiltrates of small lymphoid cells with round nuclei, clumped chromatin and scattered large lymphoid cells with round nuclei, visible nucleoli and moderate amounts of cytoplasm. Admixed with these are a few aggregates of histiocytes and occasional eosinophils. The lymphoid cells display angioinvasion with transmural infiltration by lymphocytes which adhere to the endothelium with focal luminal occlusion. There are extensive areas of necrosis with necrotic outlines of blood vessels. The adjacent lung tissue shows extensive type II pneumocyte hyperplasia.
Differential diagnosis
- EBV positive diffuse large B cell lymphoma (polymorphous variant):
- Does not show angiocentric and angiodestructive infiltrate
- Extranodal NK / T cell lymphoma:
- Shows angiocentric and angiodestructive infiltrate; atypical cells are T cells / NK cells and not B cells like in lymphomatoid granulomatosis
- Classic Hodgkin lymphoma (CHL):
- Shows polymorphous background; does not show angiocentric and angiodestructive infiltrate
- Tumor cells in classic Hodgkin lymphoma are CD30 and CD15 positive, CD20 and CD45 negative, while tumor cells in lymphomatoid granulomatosis are CD20 and CD45 positive and are negative for CD15
- Classic Reed-Sternberg-like cells are rarely seen in lymphomatoid granulomatosis
- Nodular lymphocyte predominant Hodgkin lymphoma (NLPHL):
- May show background of reactive T cells but nodular lymphocyte predominant Hodgkin lymphoma is a tumor predominantly of the lymph nodes, while lymphomatoid granulomatosis rarely involves lymph nodes
- EBV positivity is a must for lymphomatoid granulomatosis but rare in nodular lymphocyte predominant Hodgkin lymphoma
- Polymorphous lymphoid infiltration associated with immunodeficiency / transplant:
- May show polymorphous background with large atypical cells
- Does not show angiocentric or angioinvasive lymphoid infiltrate
Additional references
Board review style question #1
What cell is neoplastic in a case of lymphomatoid granulomatosis?
- B lymphocytes
- Histiocytes
- NK cells
- T lymphocytes
Board review style answer #1
Board review style question #2
Board review style answer #2