Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Flow cytometry description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2 | Board review style question #3 | Board review style answer #3Cite this page: Neely C, Bradley K. In situ mantle cell neoplasm. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lymphomaisMCN.html. Accessed April 1st, 2025.
Definition / general
- Cyclin D1 positive B cells with CCND1 rearrangements restricted to the mantle zones of reactive appearing lymphoid tissue (Blood 2016;127:2375)
Essential features
- Lymphoid architecture preserved with slight or no mantle zone expansion (Blood 2016;127:2375, Semin Diagn Pathol 2018;35:76)
- Cyclin D1 positive B cells with CCND1 rearrangement restricted to mantle zones (Blood 2016;127:2375, Mod Pathol 2012;25:1629)
- Rare; usually an incidental finding (Blood 2016;127:2375)
- Typically a stable disease with indolent behavior and long term survival, even without therapy (Blood 2016;127:2375)
- Infrequent (< 10%) progression to overt mantle cell lymphoma (Blood 2016;127:2375, Haematologica 2012;97:270)
Terminology
- In situ mantle cell neoplasia is accepted terminology
- Previous terms are not recommended: in situ mantle cell lymphoma, in situ involvement by mantle cell lymphoma-like cells or mantle cell lymphoma-like B cells of uncertain / undetermined significance (Semin Diagn Pathol 2018;35:76)
ICD coding
- ICD-10: C83.1 - mantle cell lymphoma (Western Australian Coding Rule: 1215/02 Mantle Cell Lymphoma In Situ [Accessed 1 May 2023])
Epidemiology
- Median age: 65 - 66 years (Haematologica 2012;97:270, Int J Clin Exp Pathol 2014;7:1042)
- Rare; usually an incidental finding (Blood 2016;127:2375)
- 2 cases of isolated and incidental in situ mantle cell neoplasia were identified in lymph nodes resected from 341 patients (0.6%) with colorectal or breast adenocarcinoma (Am J Surg Pathol 2016;40:943)
- 0 cases of in situ mantle cell neoplasia were identified in 1,292 reactive lymph nodes from 131 patients without evidence of lymphoma (Mod Pathol 2012;25:1629)
Sites
- Frequently nodal but may be seen in extranodal locations, including appendix, gallbladder, lacrimal gland, lung, nasopharynx, small intestine, oropharynx, spleen and urinary bladder (Haematologica 2012;97:270, Head Neck 2013;35:E333, J Hematop 2012;5:169)
- Involvement of more than 1 tissue site does not exclude the diagnosis (Blood 2016;127:2375)
- Peripheral blood involvement is permitted
- 5 of 17 patients showed peripheral blood or bone marrow involvement (Haematologica 2012;97:270)
Pathophysiology
- t(11;14) IGH::CCND1 translocation results in overexpression of cyclin D1 and dysregulation of the cell cycle (J Clin Invest 2012;122:3416)
- Low levels of B cells with t(11;14) translocation have been identified in peripheral blood of healthy individuals (Mod Pathol 2012;25:1629)
- Cyclin D1 positive B cells with CCND1 rearrangements may colonize the mantle zones of lymphoid follicles (Blood 2016;127:2375)
- Risk of progression is very low (Blood 2016;127:2375)
Etiology
- Unclear
Clinical features
- Indolent behavior (Blood 2011;117:3954, Haematologica 2012;97:270)
- Infrequent (< 10%) progression to overt mantle cell lymphoma (Blood 2016;127:2375, Semin Diagn Pathol 2018;35:76)
- May be identified in association with another lymphoma, including chronic lymphocytic leukemia / small lymphocytic lymphoma, marginal zone lymphoma and follicular lymphoma (Haematologica 2012;97:270)
Diagnosis
- Usually an incidental finding discovered when cyclin D1 immunohistochemistry is performed on a lymph node
Radiology description
- No specific radiologic findings
Case reports
- Man in his 40s with involved cervical lymph node and follicular lymphoma and man in his 70s with involved cervical lymph node (Histopathology 2008;52:256)
- 52 year old man and 65 year old woman with in situ mantle cell lymphoma in cervical lymph nodes (Int J Clin Exp Pathol 2014;7:1042)
- 58 year old man with involved inguinal node and marginal zone lymphoma (Am J Clin Pathol 2015;143:274)
- 65 year old man with involved mesenteric node and follicular lymphoma (Case Rep Hematol 2014;2014:145129)
- 70 year old woman with involved nasopharynx (Head Neck 2013;35:E333)
- 75 year old woman with composite follicular lymphoma and in situ mantle cell neoplasm (Pathol Res Pract 2020;216:153067)
Treatment
- Treatment guided by the presence or absence of coexistent overt lymphoma (Blood 2011;117:3954)
- In the absence of coexistent overt lymphoma, watchful waiting is appropriate (Semin Diagn Pathol 2018;35:76)
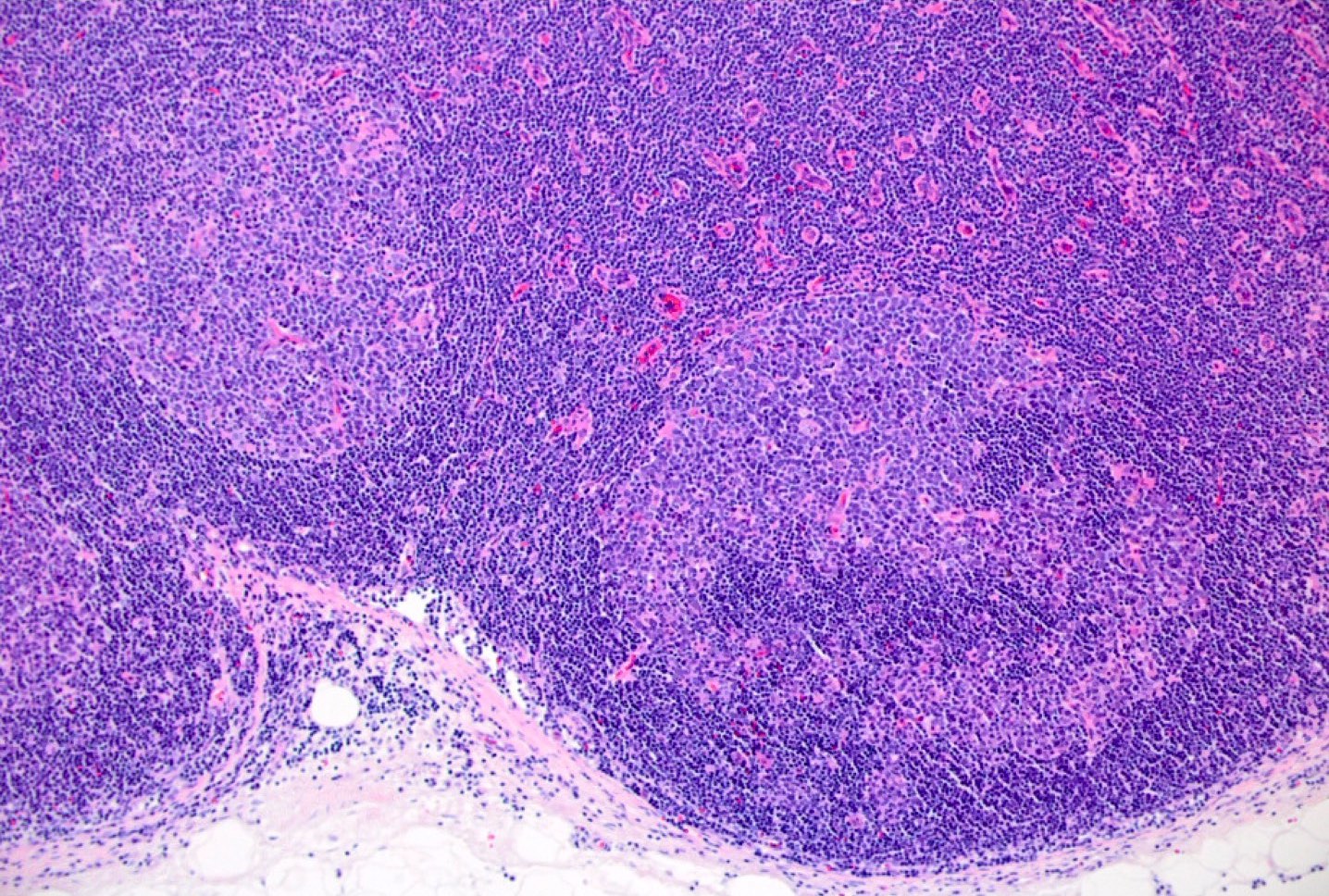
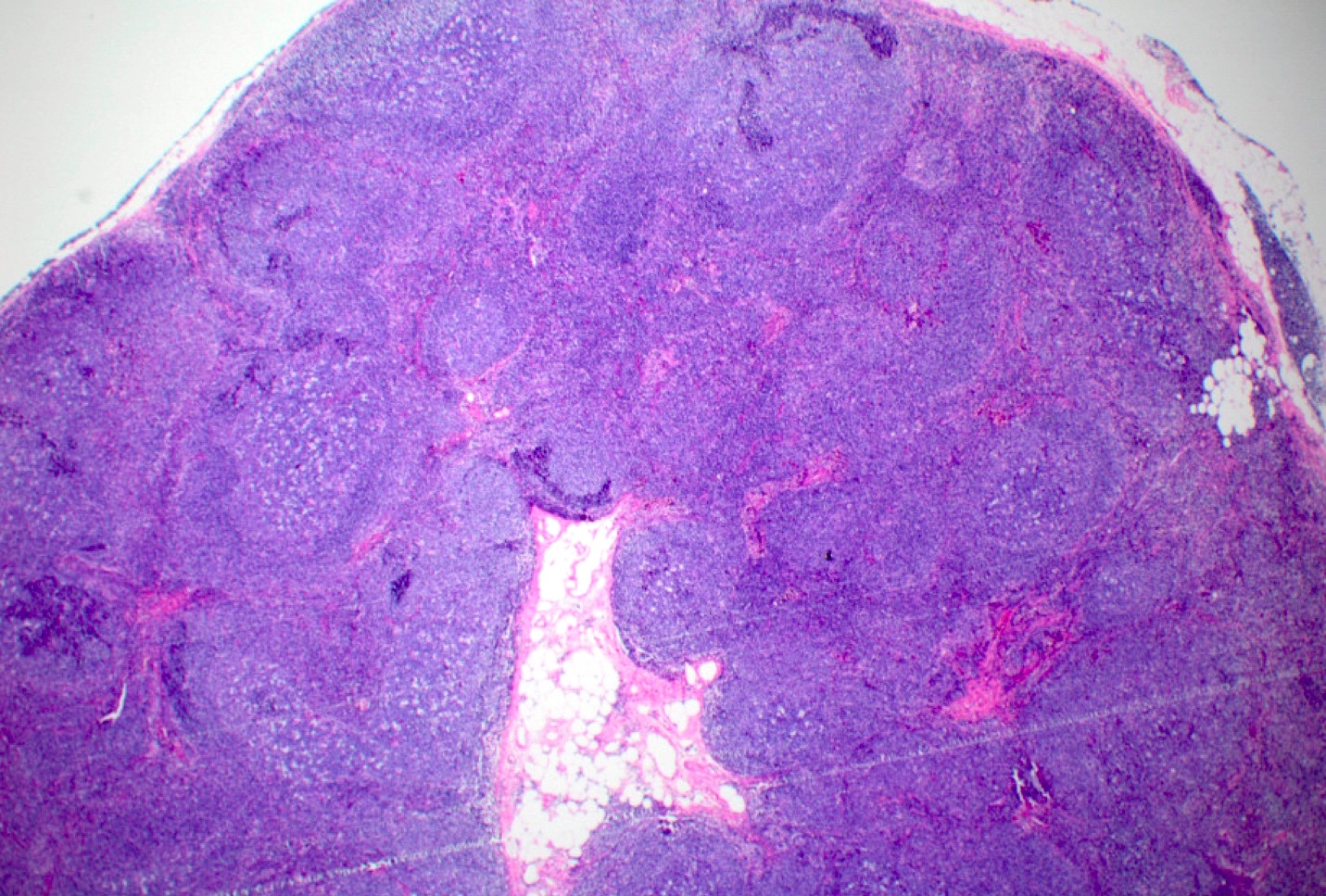
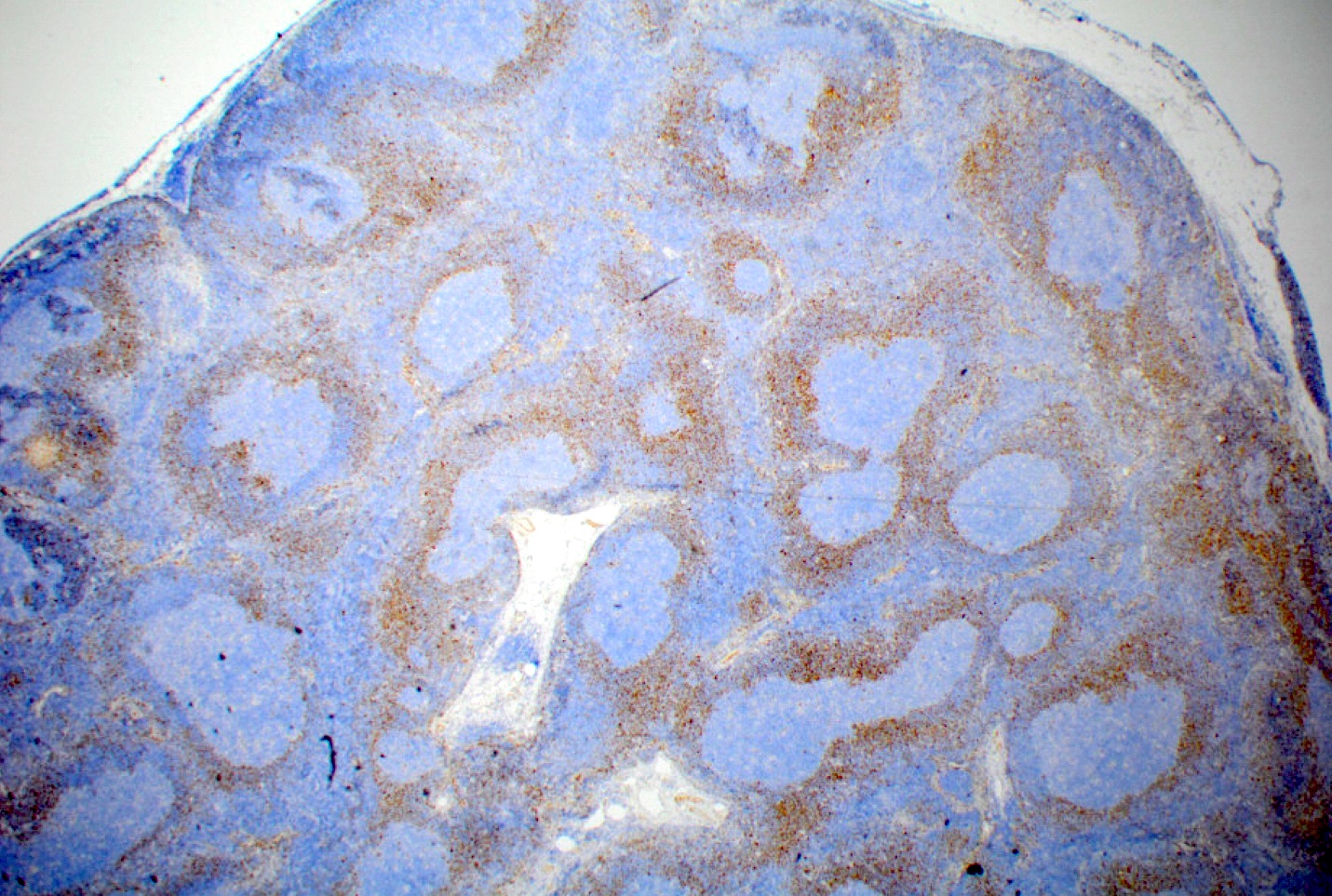
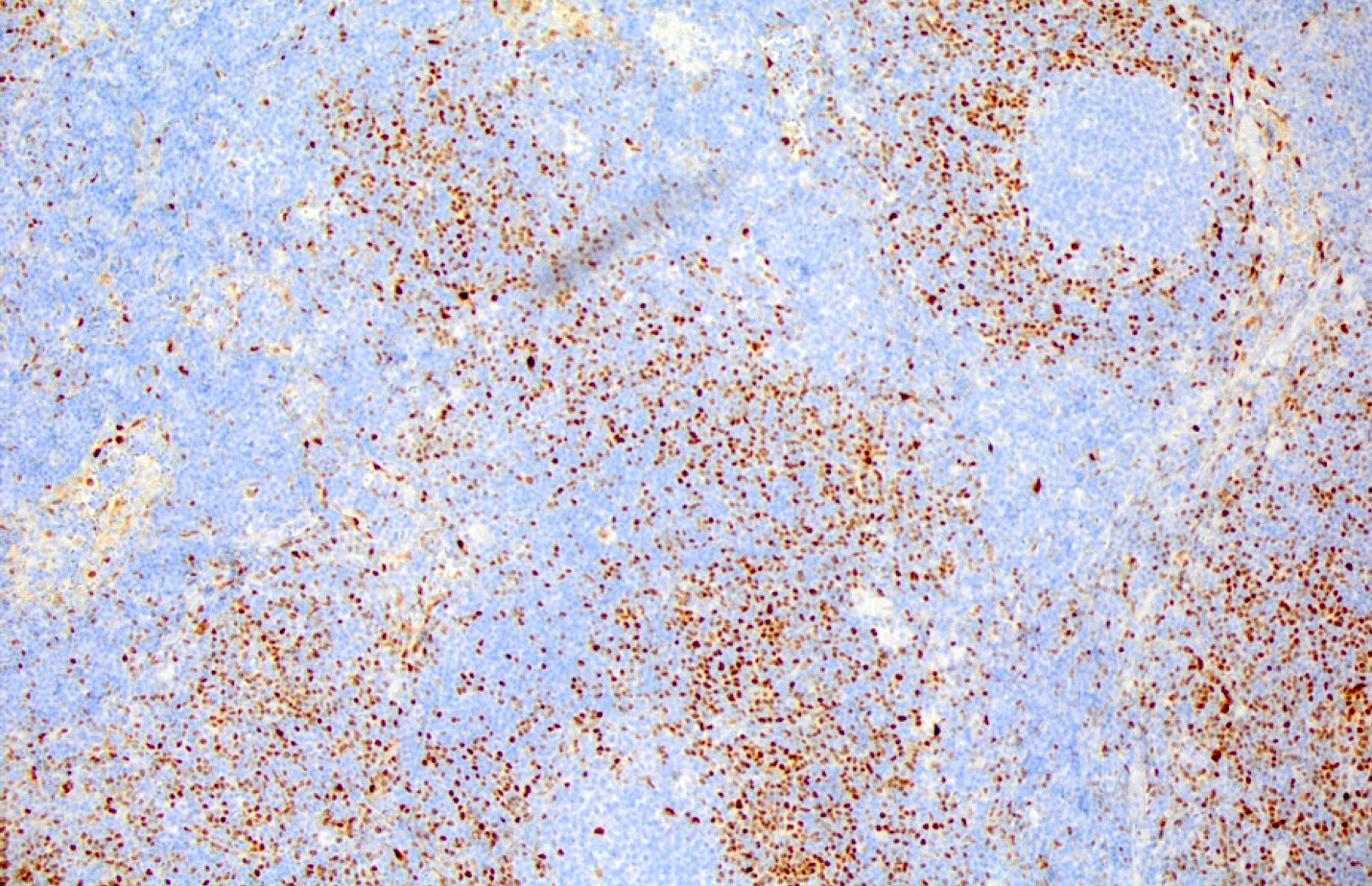
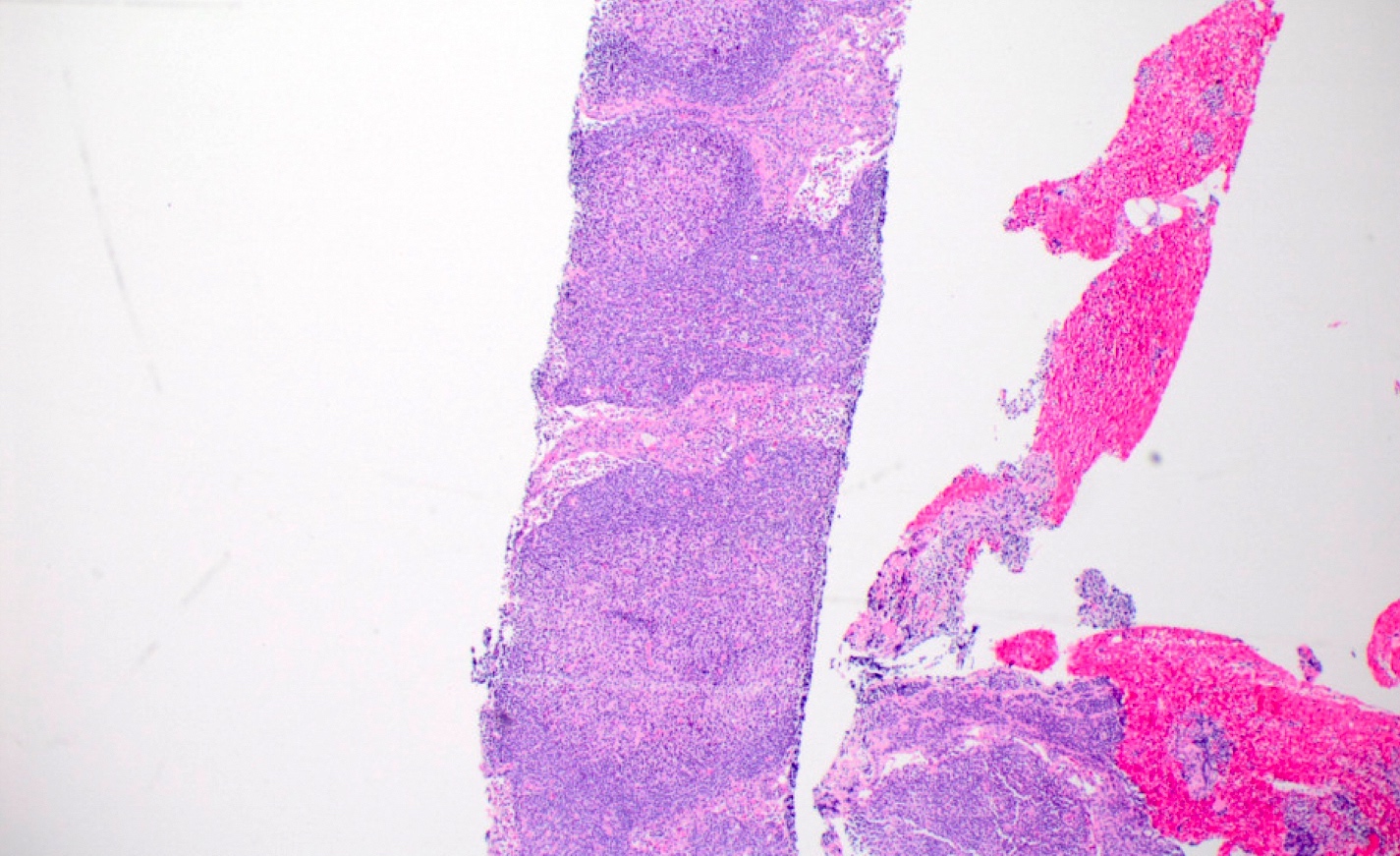
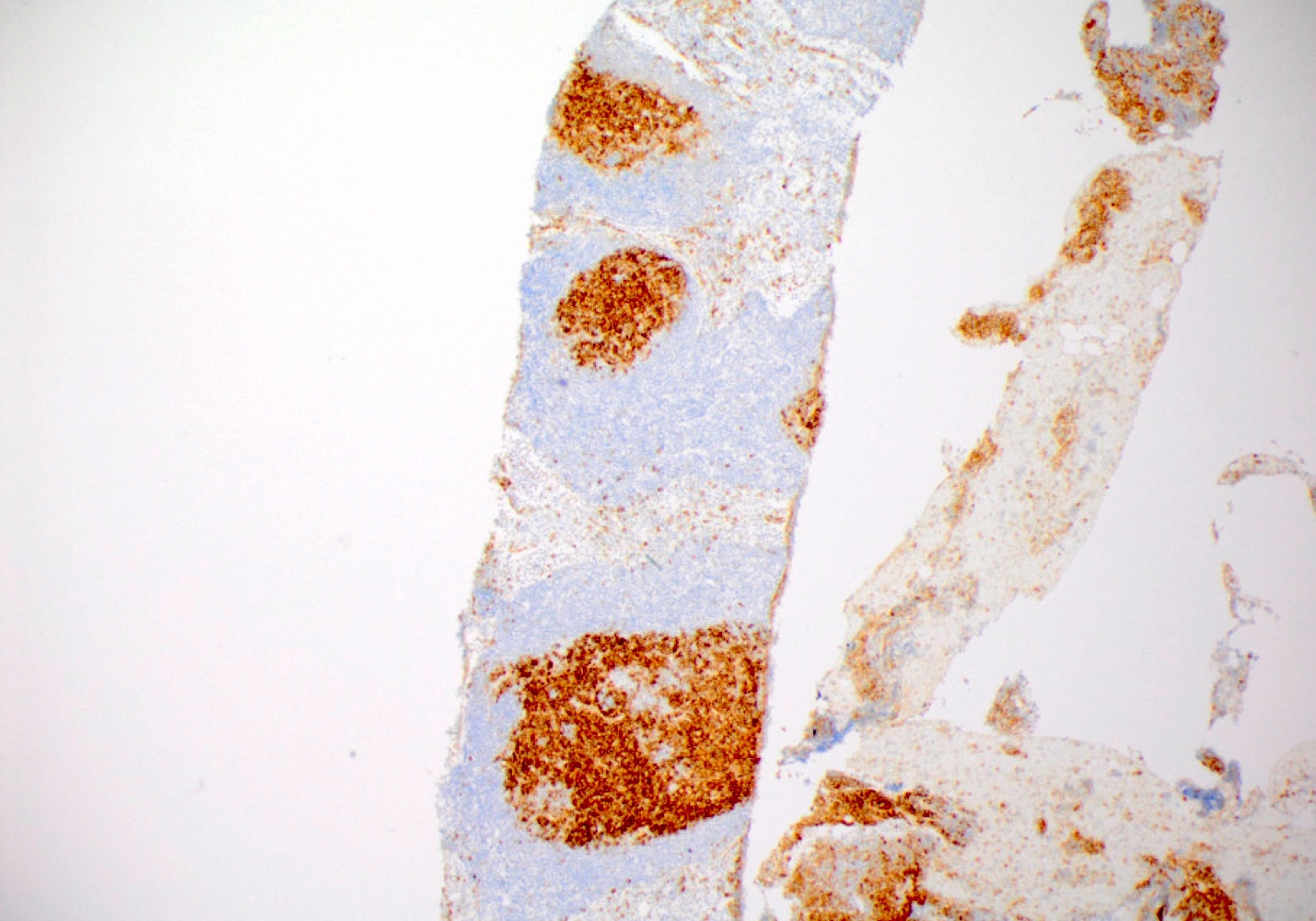
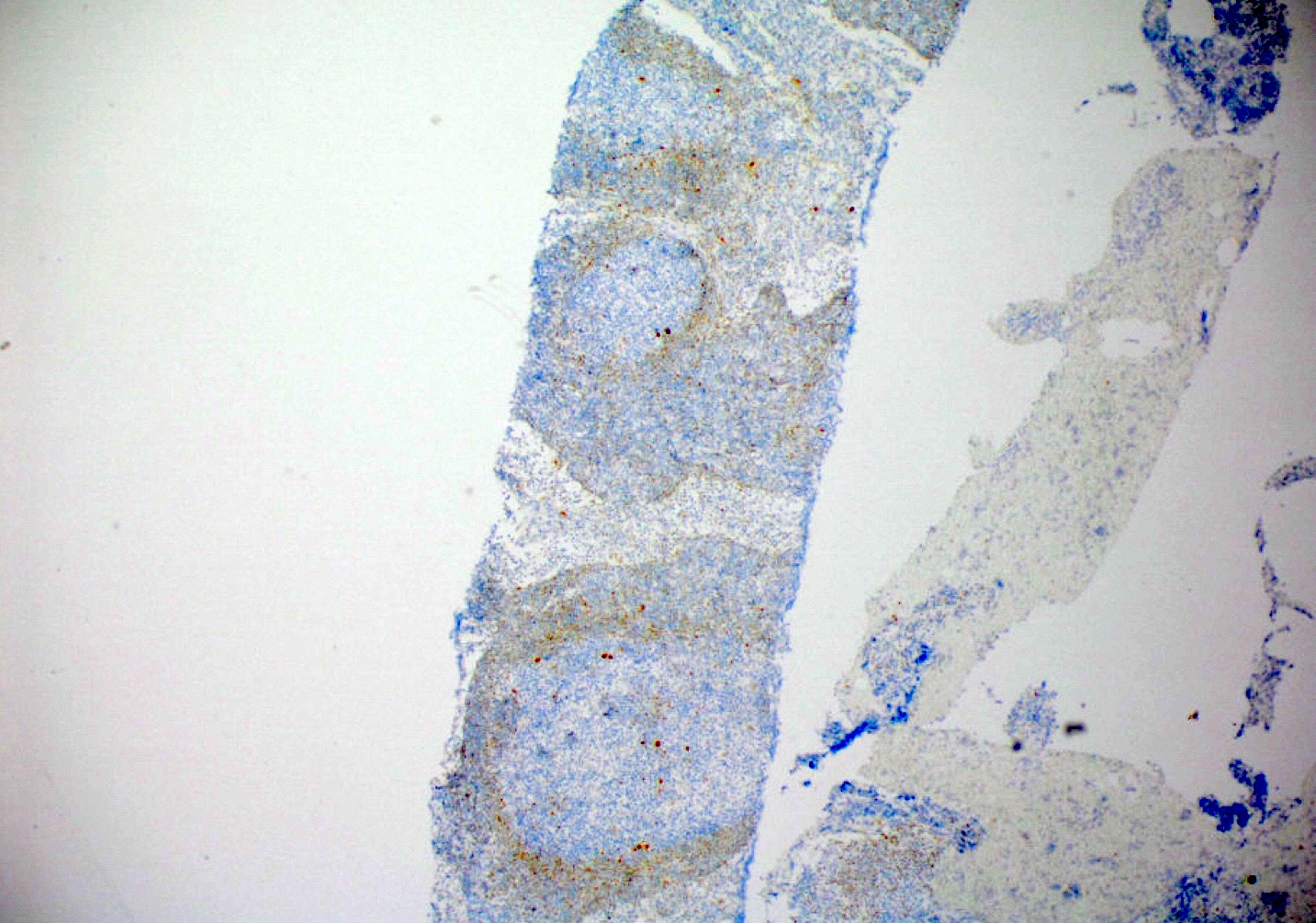
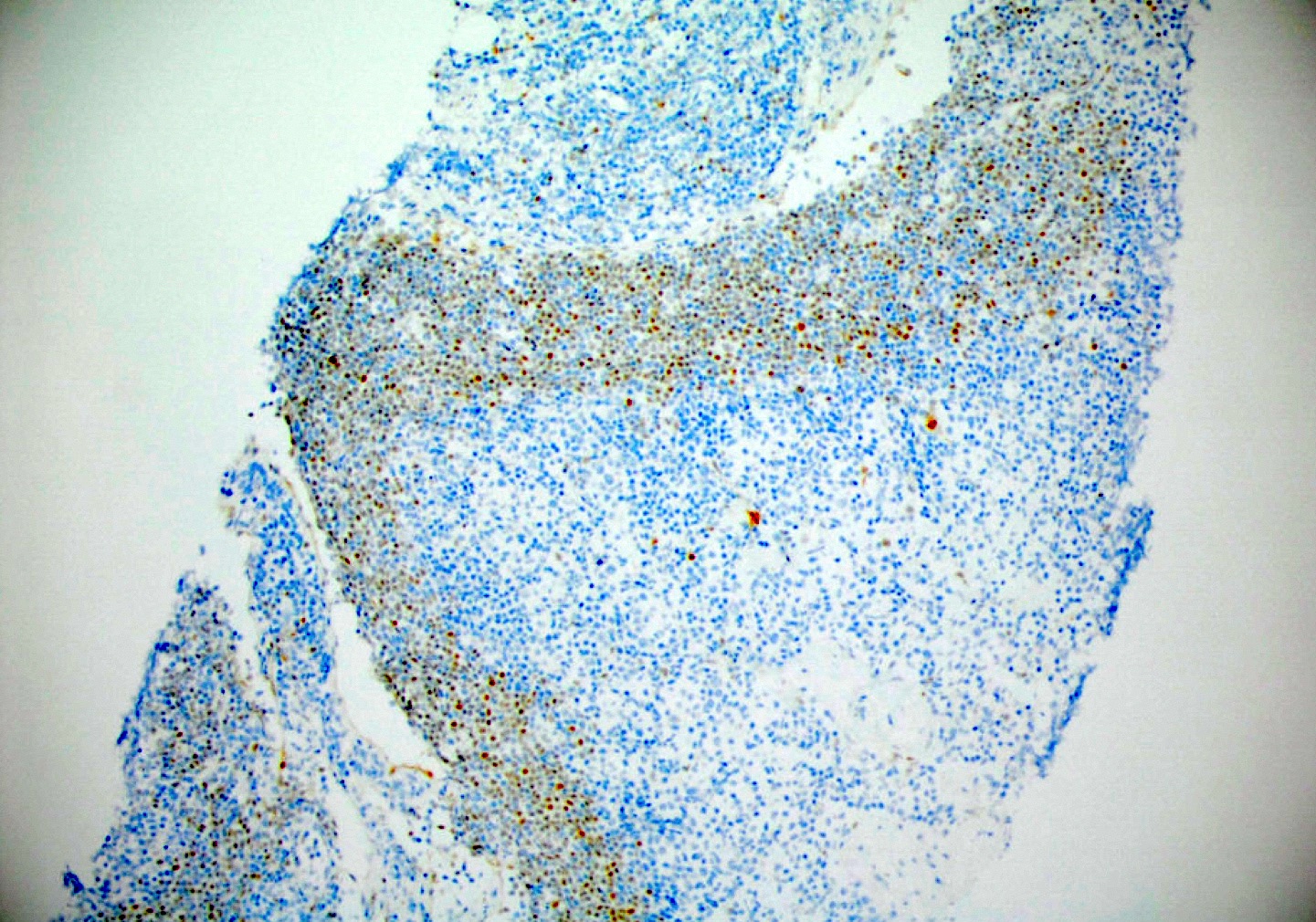
Microscopic (histologic) description
- Lymphoid architecture preserved with no or slight mantle zone expansion (Blood 2016;127:2375, Semin Diagn Pathol 2018;35:76)
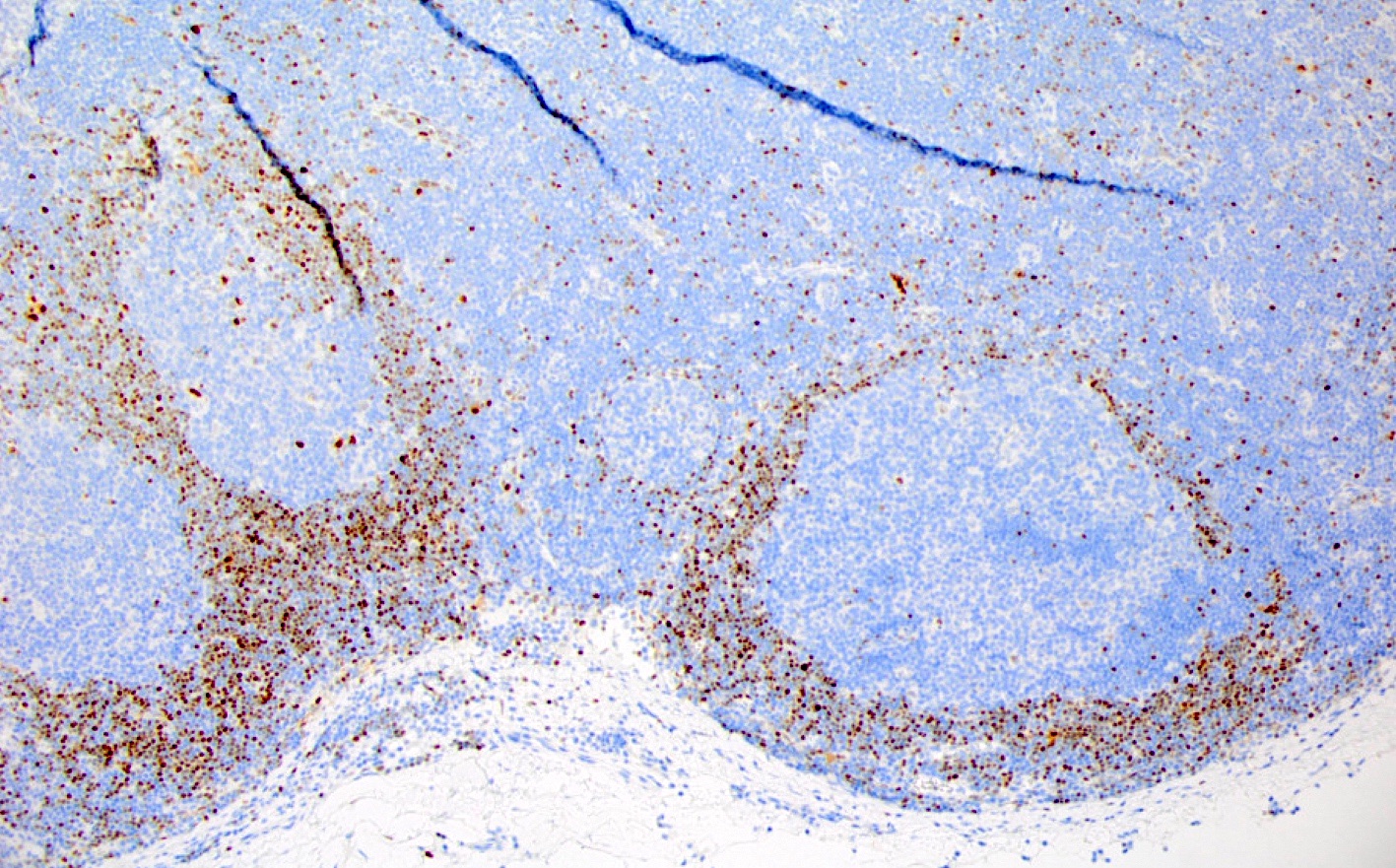
- Cyclin D1 positive B cells identified within the mantle zone (Blood 2016;127:2375, Virchows Arch 2016;468:245, Haematologica 2012;97:270)
- Usually restricted to the inner mantle zone
- Rarely scattered throughout the mantle zone or present in the outer mantle zone
- Very rarely intrafollicular or focally within germinal centers
- May involve multiple follicles in a lymph node (Am J Surg Pathol 2016;40:943)
- May be identified in association with another lymphoma (Blood 2016;127:2375)
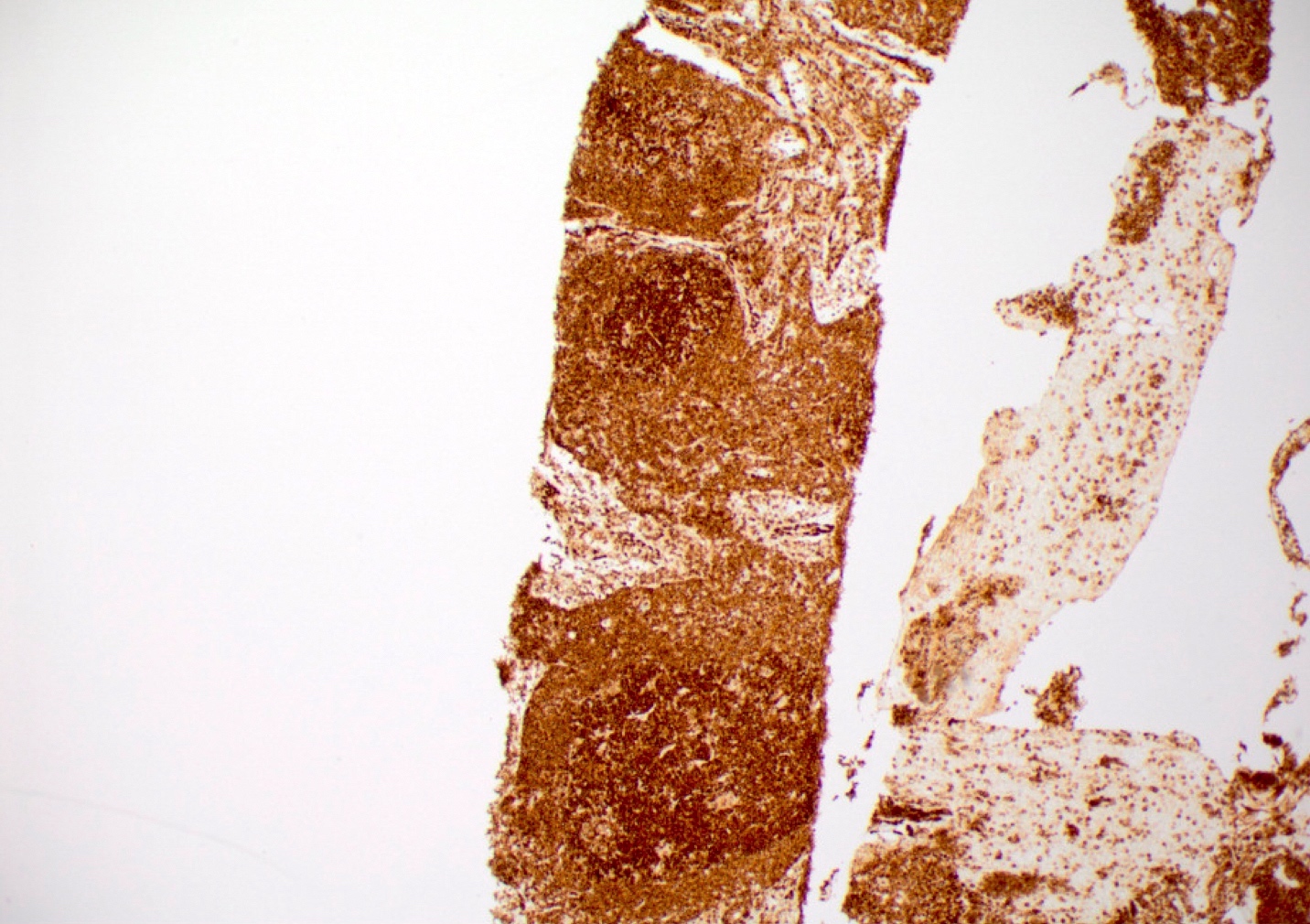
Microscopic (histologic) images
Positive stains
- B cell markers (e.g., CD20, PAX5, CD79a, BOB1, OCT2), cyclin D1, BCL2, IgD (J Hematop 2012;5:169)
- Usually CD5 and CD43
- More frequently CD5 negative and CD43 negative than overt mantle cell lymphoma (Semin Diagn Pathol 2018;35:76, J Hematop 2012;5:169)
- Variable SOX11
- 7/16 cases (44%) (Haematologica 2012;97:270)
- 100% (number of cases not clearly specified) (J Hematop 2012;5:169)
Flow cytometry description
- Clonal in situ mantle cell neoplasm cells may be detected by flow cytometry but this may require careful gating strategies due to the presence of nonclonal B cells present in involved lymph nodes
- Phenotype is indistinguishable from typical mantle cell lymphoma
- Reference: Am J Clin Pathol 2015;143:274
Molecular / cytogenetics description
- Characteristic translocation t(11;14) IGH::CCND1 results in overexpression of cyclin D1 (Virchows Arch 2016;468:245)
Sample pathology report
- Lymph node, right axilla, excision:
- In situ mantle cell neoplasm (see comment)
- Comment: The H&E stained sections show morphologic features consistent with a benign lymph node with follicular hyperplasia. A cyclin D1 immunohistochemical stain demonstrates cyclin D1 positive cells confined to the inner mantle zones of lymphoid follicles without mantle zone expansion. These findings are consistent with a diagnosis of in situ mantle cell neoplasm. In situ mantle cell neoplasm typically follows an indolent course; however, rare cases may progress to overt mantle cell lymphoma.
Differential diagnosis
- Mantle cell lymphoma with mantle zone growth pattern (Semin Diagn Pathol 2018;35:76):
- Expansion of the mantle zone, complete replacement of the mantle zone or significant extension into the interfollicular region or germinal centers by cyclin D1 positive B cells warrants a diagnosis of mantle cell lymphoma rather than in situ mantle cell neoplasm (Blood 2016;127:2375)
- Reactive follicular hyperplasia (Semin Diagn Pathol 2018;35:76):
- Reactive follicular hyperplasia lacks cyclin D1 positive cells within the mantle zones (Semin Diagn Pathol 2018;35:76)
Board review style question #1
In situ mantle cell neoplasm is characterized by which of the following translocations?
- t(8;14) MYC::IGH
- t(9;22) BCR::ABL1
- t(11;14) IGH::CCND1
- t(14;18) BCL2::IGH
Board review style answer #1
C. t(11;14) IGH::CCND1. The characteristic translocation of in situ mantle cell neoplasia is t(11;14) IGH::CCND1, resulting in overexpression of cyclin D1. Answer B is incorrect because t(9;22) BCR::ABL1 is the Philadelphia chromosome associated with AML, CML and B ALL. Answer D is incorrect because t(14;18) BCL2::IGH is associated with follicular lymphoma. Answer A is incorrect because t(8;14) MYC::IGH is associated with Burkitt lymphoma.
Comment Here
Reference: In situ mantle cell neoplasm
Comment Here
Reference: In situ mantle cell neoplasm
Board review style question #2
In a lymph node biopsy, which of the following features supports a diagnosis of in situ mantle cell neoplasm?
- Cyclin D1 positive B cells extending into the interfollicular region
- Mantle zones prominently expanded by cyclin D1 positive B cells
- Monoclonal proliferation of BCL2 positive B cells confined to germinal centers
- Preserved lymphoid architecture
Board review style answer #2
D. Preserved lymphoid architecture. In situ mantle cell neoplasm is characterized by cyclin D1 positive B cells restricted to the mantle zone of reactive appearing lymphoid tissue. Lymphoid architecture is preserved. Answers A and B are incorrect because prominent expansion of the mantle zone, complete replacement of the mantle zone or significant extension into the interfollicular region or germinal center by cyclin D1 positive B cells warrants a diagnosis of mantle cell lymphoma rather than in situ mantle cell neoplasm. Answer C is incorrect because a monoclonal proliferation of BCL2 positive B cells confined to germinal centers in a hyperplastic appearing lymphoid follicle is consistent with in situ follicular B cell neoplasm.
Comment Here
Reference: In situ mantle cell neoplasm
Comment Here
Reference: In situ mantle cell neoplasm
Board review style question #3
Which of the following is true of in situ mantle cell neoplasm?
- Characterized by aggressive behavior
- May be seen in extranodal locations
- Peripheral blood involvement is not permitted
- Usually progresses to overt mantle cell lymphoma
Board review style answer #3
B. May be seen in extranodal locations. In situ mantle cell neoplasm is a rare finding that is most commonly seen in lymph nodes but may be seen in extranodal locations. Answer C is incorrect because peripheral blood involvement is permitted. Answers A and D are incorrect because it is typically a stable disease with indolent behavior and infrequent (< 10%) progression to overt mantle cell lymphoma.
Comment Here
Reference: In situ mantle cell neoplasm
Comment Here
Reference: In situ mantle cell neoplasm