Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Flow cytometry description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Evans MG, Aster JC, Miranda RN, Medeiros LJ. High grade B cell lymphoma, NOS . PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lymphomahighgradebcell.html. Accessed April 2nd, 2025.
Definition / general
- Aggressive mature B cell lymphoma previously included in the 2008 WHO classification as "B cell lymphoma, unclassifiable, with features intermediate between diffuse large B cell lymphoma and Burkitt lymphoma"
- Newly defined high grade B cell lymphoma in the revised 2016 WHO (Blood 2016;127:2375)
- These lymphomas do not harbor combined MYC rearrangement (chromosome 8q24.2) and BCL2 (chromosome 18q21.3) and / or BCL6 (chromosome 3q27.3) rearrangement
- These neoplasms may carry a MYC rearrangement, or BCL2 and / or BCL6 rearrangement without MYC rearrangement, or extra copies of MYC, BCL2 and / or BCL6
Essential features
- Heterogenous category of aggressive mature B cell lymphomas that may be transformed or arise de novo
- Should be distinguished from diffuse large B cell lymphoma (DLBCL), NOS and Burkitt lymphoma (BL)
- Tumors with MYC (chromosome 8q24.2) and BCL2 (chromosome 18q21.3) and / or BCL6 (chromosome 3q27.3) rearrangements belong to a different category and must be excluded before rendering this diagnosis
Terminology
- High grade B cell lymphoma, NOS
- May be applicable to de novo or transformed cases
- Note:
- This diagnosis is rare and should be rendered only when diffuse large B cell lymphoma (DLBCL) and Burkitt lymphoma (BL) have been ruled out
- Cases with large cell morphology that have MYC rearrangement with or without amplification / gain of BCL2 should be considered DLBCL
- Pediatric cases with simple karyotypes and features of both DLBCL and BL have better prognosis than high grade B cell lymphoma, NOS and should instead be classified as either DLBCL or BL
- Half of these cases harbor MYC rearrangements and can demonstrate a gene expression profile resembling that observed in BL (Blood 2008;112:1374)
- Care should be taken before diagnosing a transformed follicular lymphoma as high grade B cell lymphoma, especially if any retained follicular architecture exists
ICD coding
- ICD-O: 9680/3 - B cell lymphoma, unclassifiable, with features intermediate between diffuse large B cell lymphoma and Burkitt lymphoma
Epidemiology
- Rare; true frequency is unknown but increases with age
- Typically reported in elderly patients in the sixth decade of life
- Occurs equally in men and women
Sites
- Generally presents within lymph nodes or extranodal sites without predilection for a specific body site (Hsi: Hematopathology - Foundations in Diagnostic Pathology, 3rd Edition, 2017)
Etiology
- Few studies have been conducted but this lymphoma may arise from germinal center B cells in 20 - 35% of cases with MYC rearrangement and amplification / gain of BCL2 (Mod Pathol 2015;28:208)
- Cell of origin is unknown in cases without MYC or BCL2 rearrangements (Mod Pathol 2009;22:1507)
Clinical features
- Advanced stage (stage III - IV) is most common, including involvement of bone marrow and central nervous system
- Typically presents with lymphadenopathy or with an extranodal mass
- B symptoms are common
- Rare cases demonstrate circulating tumor cells within the peripheral blood (Medeiros: Diagnostic Pathology - Lymph Nodes and Extranodal Lymphomas, 2nd Edition, 2017)
Diagnosis
- Morphological evaluation reveals cells that more likely resemble BL than DLBCL
- Nuclear size variations or a blastoid appearance uncharacteristic of BL are possible
- Simultaneous rearrangement of MYC and BCL2 or BCL6 should be excluded by classic cytogenetics, FISH or other molecular / genetic tests
- Note: amplification can be seen in conjunction with translocation (Blood Cancer J 2020;10:5, Jaffe: Hematopathology, 2nd Edition, 2016)
Laboratory
- Elevated serum lactate dehydrogenase or β-2-microglobulin
- Leukocytosis in cases with peripheral blood involvement (Medeiros: Diagnostic Pathology - Lymph Nodes and Extranodal Lymphomas, 2nd Edition, 2017)
Prognostic factors
- Despite some variability, generally associated with poor prognosis
- Survival is typically measured in months
- This category may have a slightly better outcome than high grade B cell lymphoma with MYC and BCL2 and / or BCL6 rearrangements (Am J Surg Pathol 2014;38:49, Br J Haematol 2013;162:40)
- The worst prognosis has been reported in instances of amplification / gain of MYC with or without rearrangement of BCL2 or in instances of amplification / gain of BCL2 with or without rearrangement of MYC (Mod Pathol 2015;28:208, Cancer 2012;118:1566)
- Poor outcome has been associated with age > 60 years, stage IV disease or a high International Prognostic Index (IPI) score (Br J Haematol 2013;162:40)
Case reports
- 21 year old man with right palatal mass (J Oral Maxillofac Pathol 2016;20:333)
- 59 year old man with para-aortic lymphadenopathy (Case Rep Hematol 2017;2017:2676254)
- 63 year old man with rectal mass (Case Rep Pathol 2013;2013:302304)
Treatment
- No standardized treatment exists
- This category is thought to be resistant to typical DLBCL, NOS and BL regimens, including rituximab, cyclophosphamide, doxorubicin, vincristine and prednisone (R-CHOP)
- Use of dose adjusted etoposide, prednisone, vincristine, cyclophosphamide, doxorubicin with rituximab (DA-EPOCH-R) has been favored in some settings (Hsi: Hematopathology - Foundations in Diagnostic Pathology, 3rd Edition, 2017)
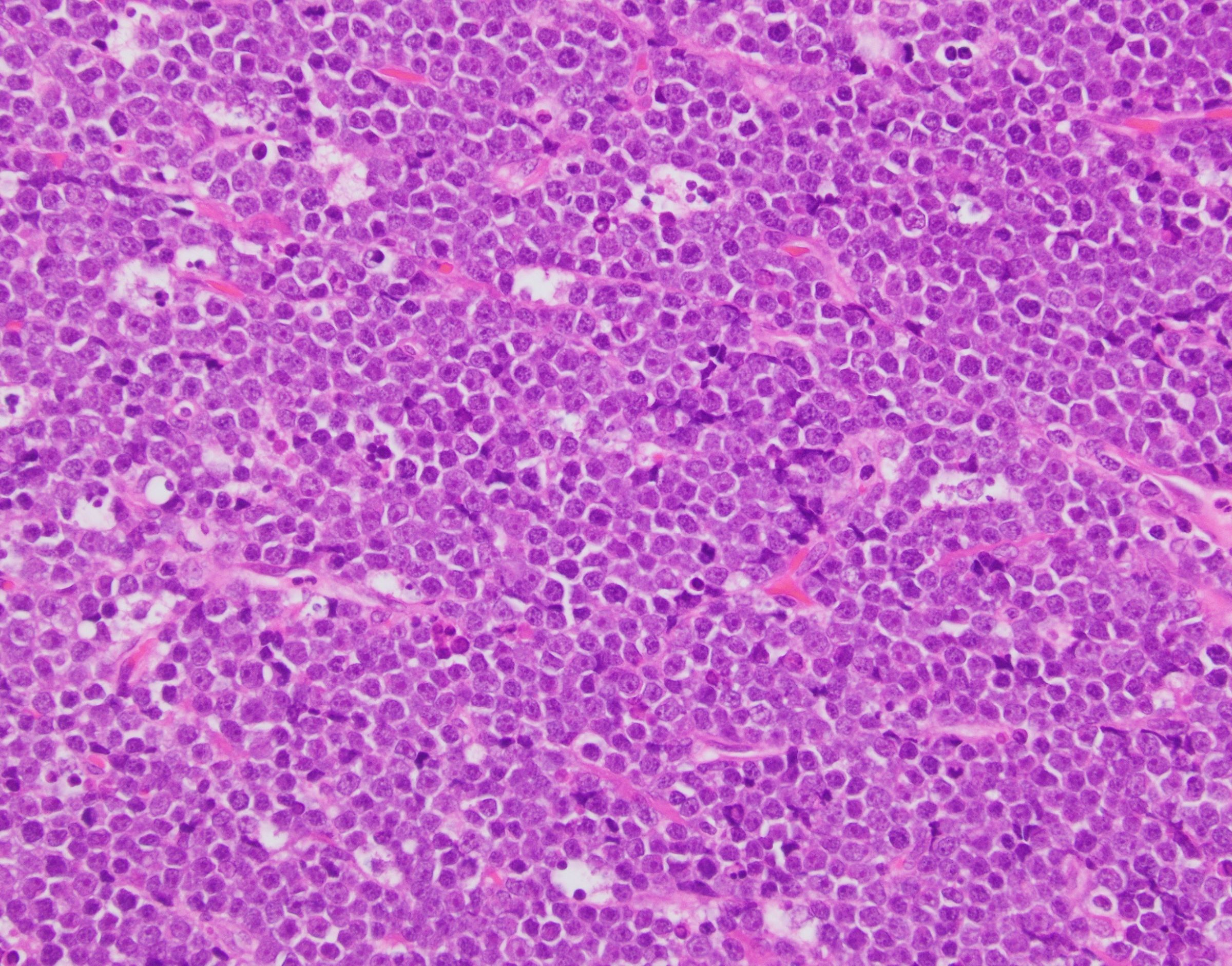
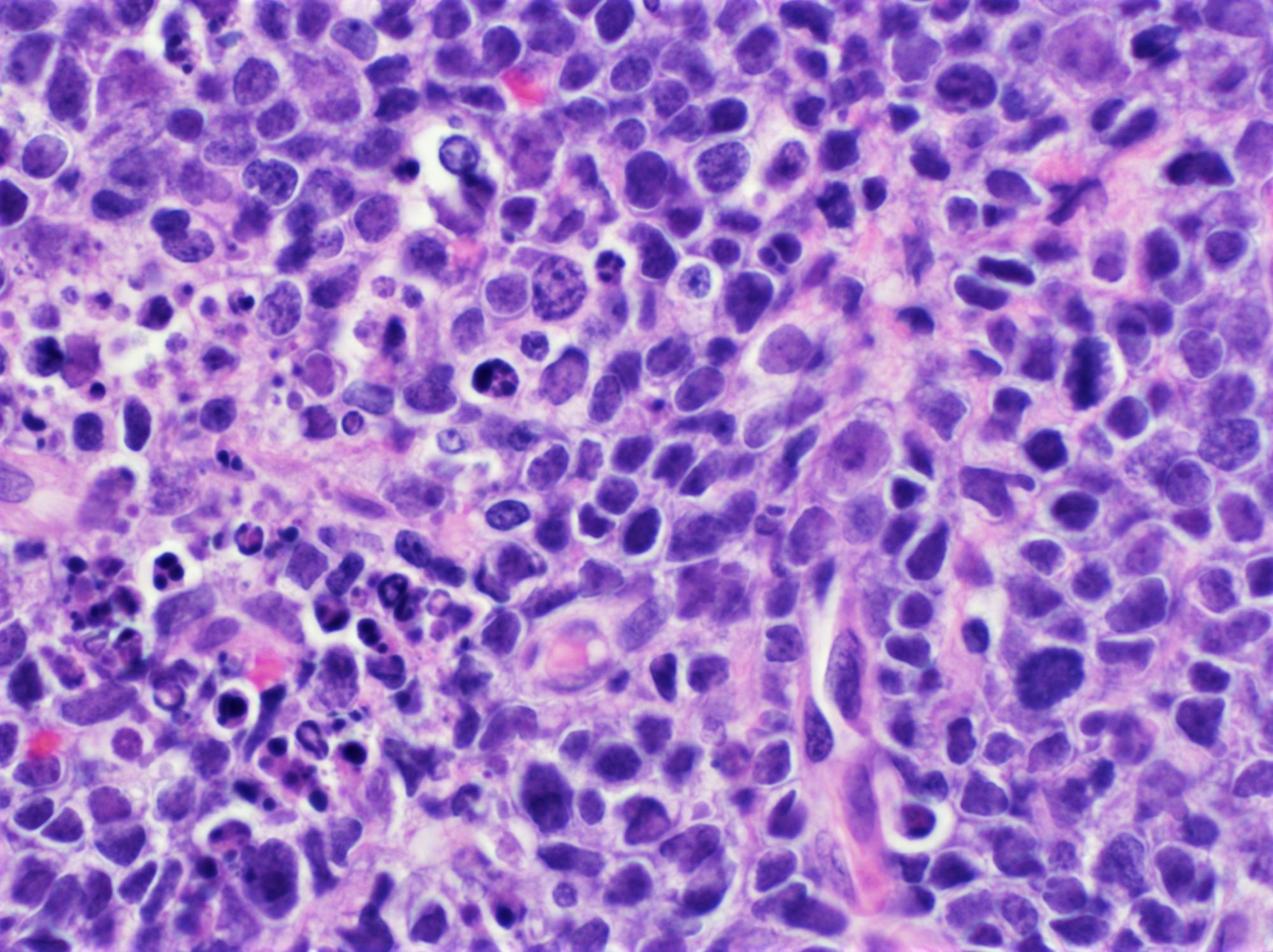
Microscopic (histologic) description
- 2 morphological variants have been defined (Pathology 2020;52:68)
- Variant previously described as B cell lymphoma, unclassifiable, with features intermediate between DLBCL and BL (BCL-U):
- Diffuse proliferation of intermediate sized, sometimes squared off cells similar to BL
- Other cases demonstrate a spectrum of intermediate and large sized cells
- Starry sky pattern is common
- Increased mitotic figures and apoptotic bodies are appreciated
- Sclerosis and admixed small lymphocytes are usually absent
- Blastoid variant:
- Intermediate sized cells with fine nuclear chromatin resembling lymphoblasts
- Starry sky pattern and frequent mitotic figures are common
Microscopic (histologic) images
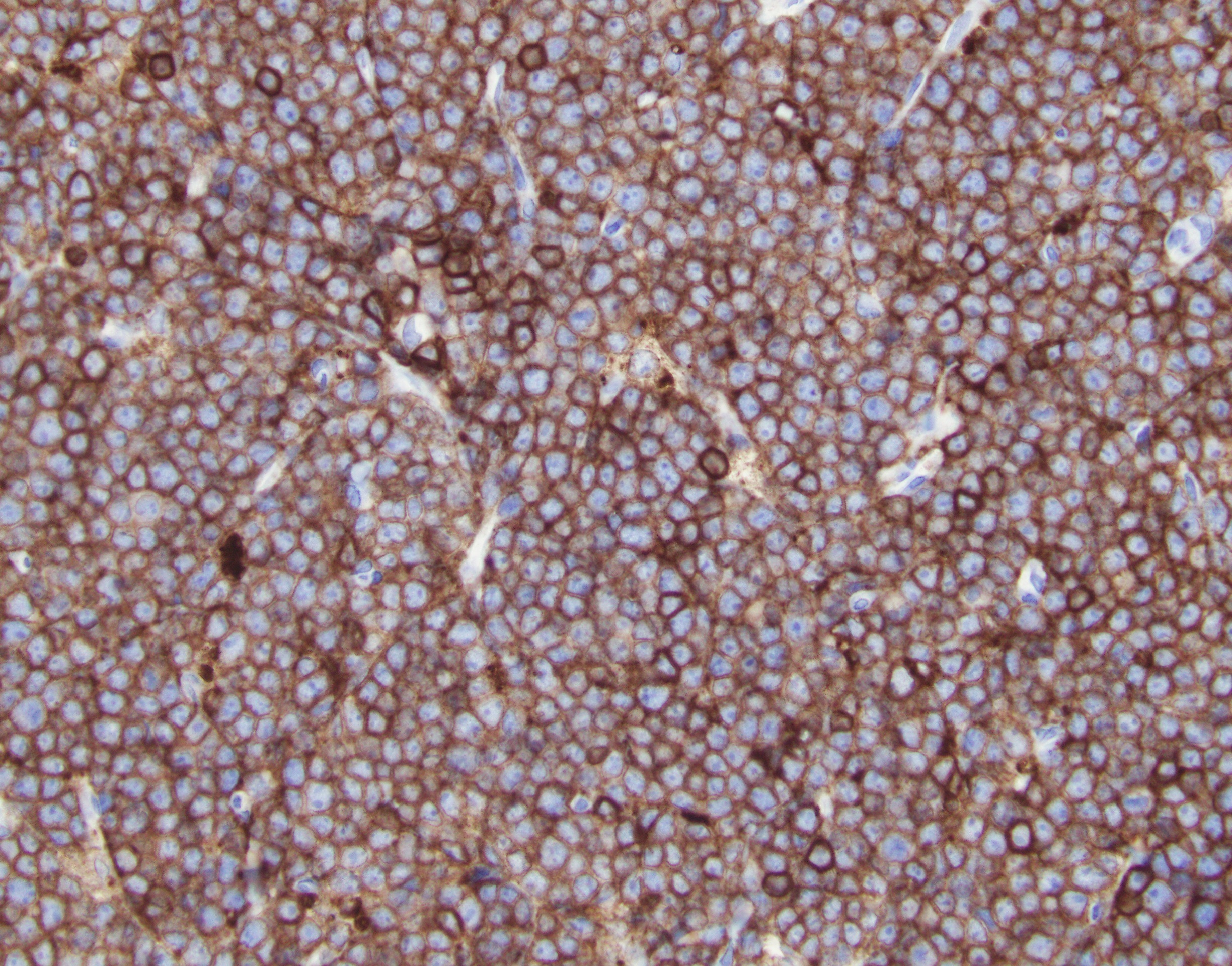
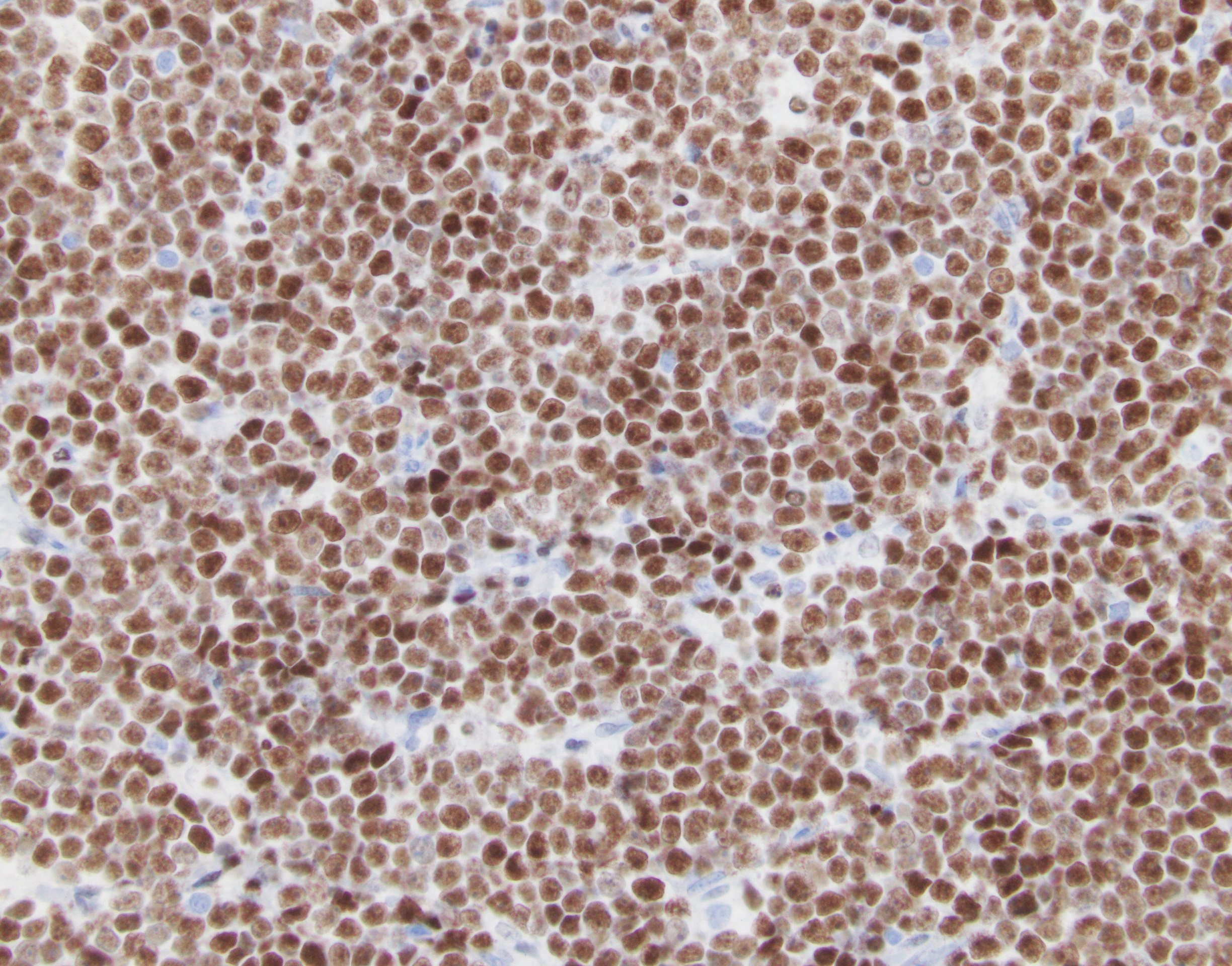
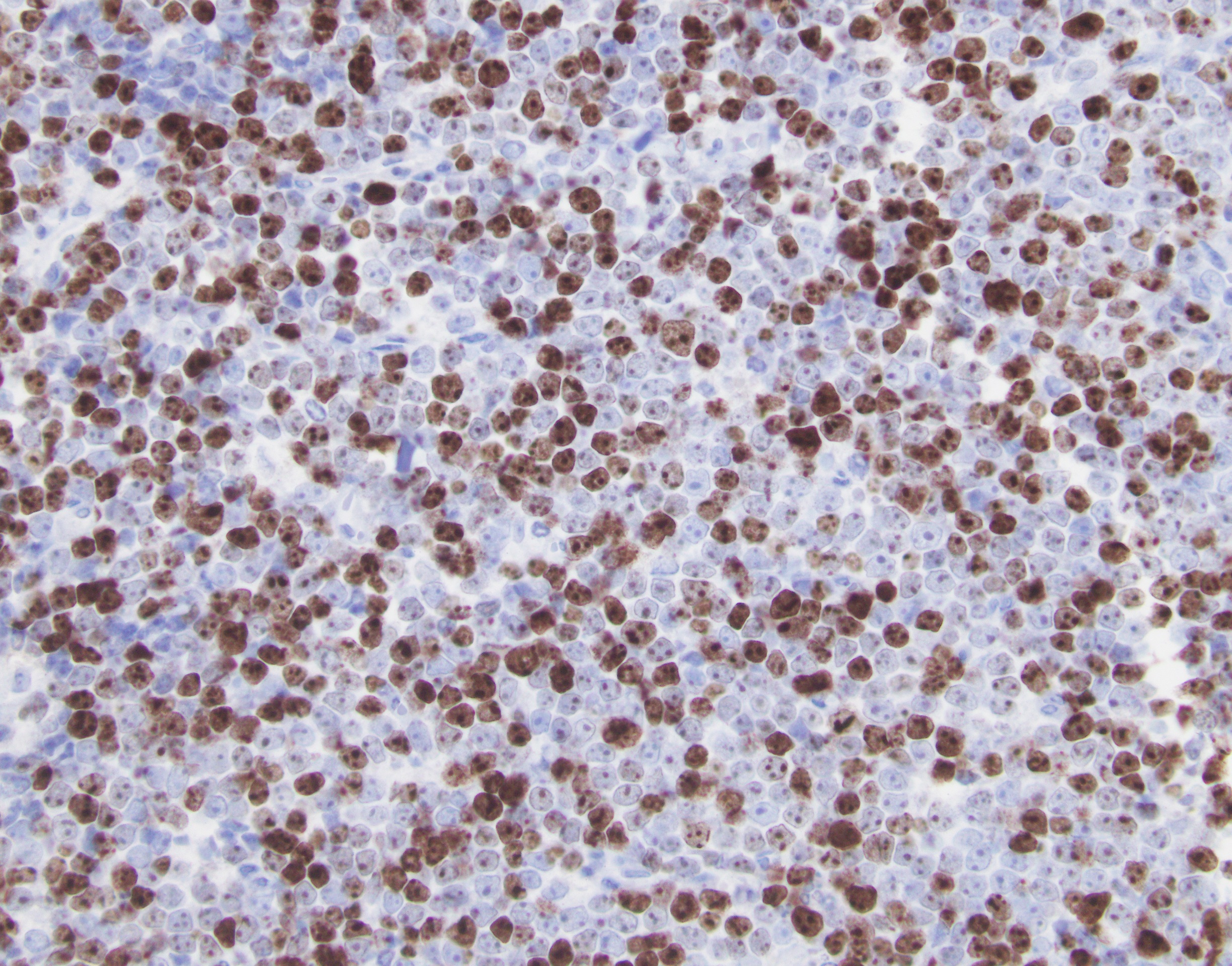
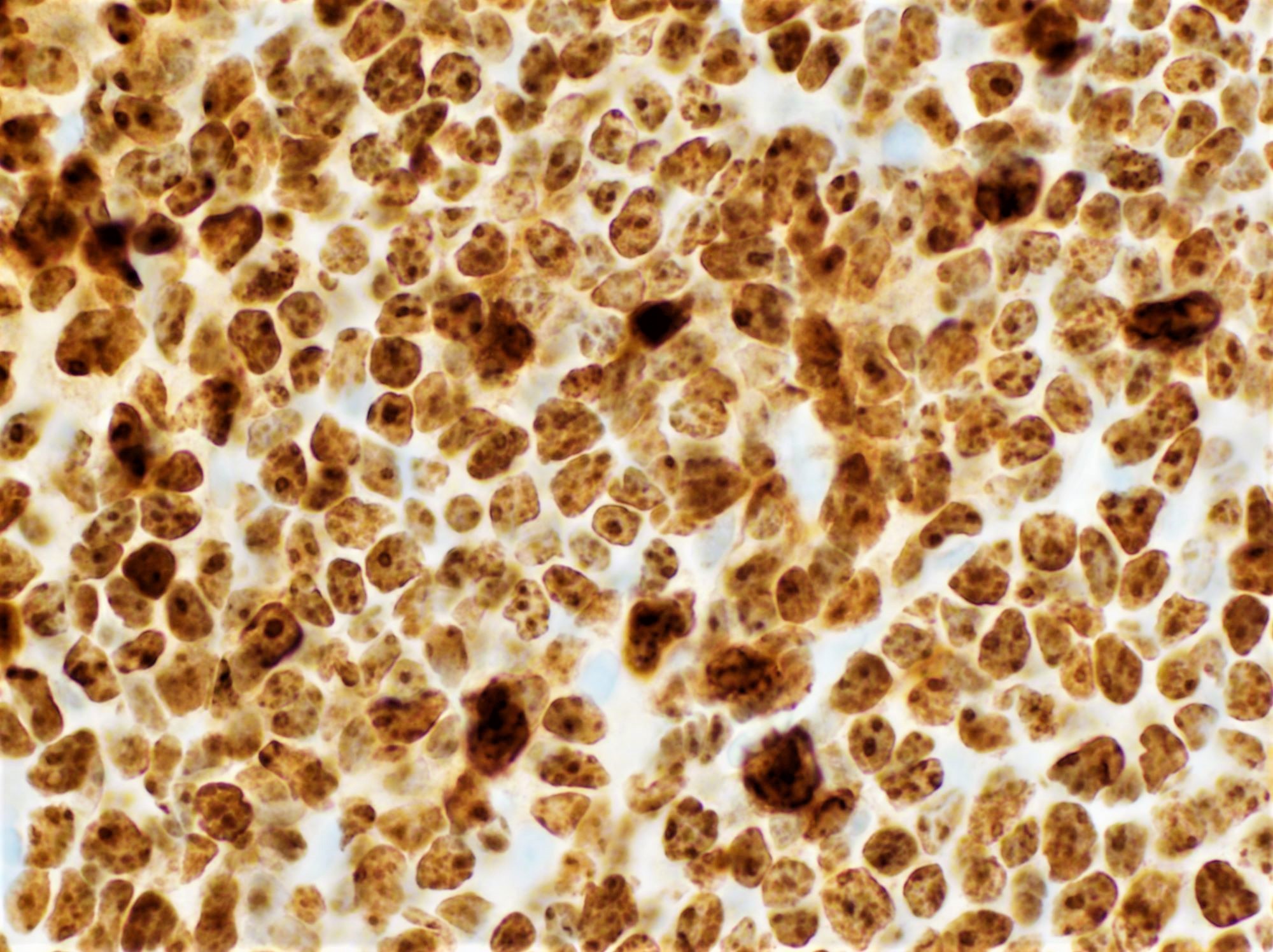
Positive stains
Flow cytometry description
- Surface immunoglobulin and pan B cell antigens are positive
- CD38, CD71 and HLA-DR may be positive in some cases (Medeiros: Diagnostic Pathology - Lymph Nodes and Extranodal Lymphomas, 2nd Edition, 2017)
Molecular / cytogenetics description
- Clonal IGH rearrangements are present
- 20 - 35% of cases demonstrate MYC rearrangements and amplification / gain of BCL2 (Mod Pathol 2015;28:208)
- Significant proportion of cases with blastoid morphology lack MYC or BCL2 rearrangements (Histopathology 2012;61:945)
- Complex karyotypes with ≥ 3 abnormalities are common
- Genomic gains and losses include but are not limited to:
- Gains of 1cen-q25, 1q31-35, 7/7q, 8q24-qter, 13q11-q13, 13q31-q33
- Losses of 13q14 and 17p12-pter (Haematologica 2008;93:1327)
- 11q gain / loss was recently described in cases of high grade B cell lymphoma, NOS with MYC rearrangement (Am J Clin Pathol 2017;149:17)
- Genetic profile intermediate between DLBCL and BL has been observed including mutations in:
- ID3, CCND3, MYC, BCL2, EZH2, CREBBP1, SGK1 (Leukemia 2015;29:1789)
Sample pathology report
- Stomach, ulcer, biopsy:
- B cell lymphoma with aggressive features; pending FISH for further classification (see comment)
- Microscopic description: The sections show gastric mucosa with a diffuse infiltrate comprised of intermediate to large sized lymphoid cells with round to irregular nuclei, vesicular chromatin, distinct nucleoli and moderate amounts of cytoplasm. Interspersed are small lymphocytes. Mitotic figures and apoptotic bodies are easily appreciated. Areas of necrosis are seen. Immunoperoxidase studies show that the larger cells are positive for CD20, CD10, BCL6 and BCL2 (weak, small subset) and are negative for CD5 and cyclin D1. CD3 study highlights interspersed T cells. MYC expression is noted in about 50% of the tumor cells. Ki67 shows a proliferative index of more than 95%. In situ hybridization study for EBV encoded RNA (EBER) is negative.
- Comment: The morphologic and immunophenotypic findings support the diagnosis of involvement by diffuse large B cell lymphoma with high grade features based on the proliferation rate. CD10 and BCL6 coexpression suggests a follicular center cell derivation. The differential diagnosis includes diffuse large B cell lymphoma, NOS and so called double hit lymphoma. Additional materials have been sent for FISH analysis, the results of which will be reported separately and in an addendum.
- Addendum: FISH analysis showed no c-MYC rearrangement in 50/50 interphase nuclei. A normal MYC FISH finding can result from absence of MYC rearrangement, from an atypical MYC rearrangement or from an insufficient number of neoplastic cells in the specimen. Features of a double hit lymphoma are not seen. The findings are most consistent with involvement by a high grade B cell lymphoma, NOS.
Differential diagnosis
- High grade B cell lymphoma with MYC and BCL2 and / or BCL6 rearrangements:
- Morphologically, may demonstrate blastoid cells or features intermediate between DLBCL and BL
- Is excluded by detecting rearrangements of MYC and BCL2 and / or BCL6
- DLBCL, NOS:
- Larger, more pleomorphic nuclei, vesicular chromatin, prominent nucleoli
- Potentially lower proliferation rate
- MYC rearrangement present or absent
- Burkitt lymphoma (BL):
- Medium sized nuclei with a morphology that may be indistinguishable from that of high grade B cell lymphoma, NOS
- High proliferation rate (Ki67 ~ 100%)
- Weak or absent BCL2 expression
- MYC rearrangement
- Negative for BCL2 translocation
- Cytoplasmic vacuoles can be seen on touch imprints (often absent in high grade B cell lymphoma, NOS)
- Burkitt-like lymphoma with 11q aberration:
- Similar histology to BL
- Lacks MYC translocation
- 11q aberration
- Weak or negative BCL2 expression
- Negative for BCL2 translocation
- B lymphoblastic leukemia / lymphoma with MYC and BCL2 rearrangement:
- Small blasts
- TdT+, CD10+, BCL6-, CCND1-
- May arise from follicular lymphoma (Hum Pathol 2015;46:260)
- Mantle cell lymphoma, blastoid variant:
- Medium sized nuclei
- Cyclin D1+
- Presence of t(11;14) translocation
- Follicular lymphoma, grade 3B:
- Will retain follicular architecture
- Would not necessarily demonstrate MYC rearrangement / amplification in addition to the IGH-BCL2 translocation (Blood 2016;127:2375)
Additional references
Board review style question #1
A 57 year old woman presents with generalized lymphadenopathy and bilateral pulmonary nodules. A representative photograph of her lung biopsy is provided. FISH detected an MYC rearrangement without associated abnormalities in BCL2 or BCL6. Immunohistochemistry was positive for CD79a and CD20 but negative for TdT and cyclin D1. The most appropriate diagnosis is
- Burkitt lymphoma
- Diffuse large B cell lymphoma, NOS with MYC rearrangement
- High grade B cell lymphoma, NOS
- High grade B cell lymphoma with MYC and BCL2 or BCL6 rearrangements
Board review style answer #1
B. Diffuse large B cell lymphoma, NOS with MYC rearrangement
Comment Here
Reference: High grade B cell lymphoma, NOS
Comment Here
Reference: High grade B cell lymphoma, NOS
Board review style question #2
Cases of high grade B cell lymphoma, NOS usually demonstrate which of the following?
- BCL6 expression
- Concurrent MYC and BCL2 rearrangements
- Low to moderate Ki67 proliferation index
- Prominent inflammatory background of small lymphocytes
Board review style answer #2