Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology images | Peripheral smear description | Peripheral smear images | Positive stains | Negative stains | Flow cytometry description | Flow cytometry images | Electron microscopy description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Al-Maashari B, Werner D. Hairy cell leukemia. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lymphomahcl.html. Accessed April 3rd, 2025.
Definition / general
- Hairy cell leukemia (HCL) is a rare, indolent lymphoproliferative neoplasm of mature B cells with a distinct clinical presentation that includes peripheral blood cytopenias, splenomegaly and a small number of circulating neoplastic cells with hair-like cytoplasmic projections
Essential features
- Pancytopenia and monocytopenia
- Splenomegaly
- Immunophenotype positive for CD11c, CD19, CD20 bright, CD22 bright, CD25, CD103, CD123 and CD305 (LAIR)
- BRAF V600E mutation is a hallmark genetic mutation in > 95% of cases
Terminology
- Hairy cell leukemia: no changes were made to this entity in the recent 5th edition of the WHO classification of hematolymphoid tumors
- Classic hairy cell leukemia (cHCL): used in some of the medical literature to best distinguish hairy cell leukemia from splenic B cell lymphoma / leukemia with prominent nucleoli (WHO 5th edition; formerly known as HCL variant [HCL-v])
- Leukemic reticuloendotheliosis: obsolete by the WHO classification of tumors of hematopoietic and lymphoid tissues
ICD coding
- ICD-O: 9940/3 - hairy cell leukemia
Epidemiology
- Incidence: < 2% of all leukemias, < 1 per 100,000 persons/year in U.S.
- M:F = 4:1
- Median age of diagnosis is 55 years
- More common in whites and less in African, Asian and Arab populations
- Increased risk: farming and exposure to pesticides (Scand J Work Environ Health 1996;22:285)
- Smoking has been reported as a significant negative association and appears to be protective (Br J Haematol 1995;91:154)
Sites
- Common sites of involvement: bone marrow, peripheral blood and spleen
- Uncommon sites of involvement: liver, lymph node and skin
Pathophysiology
- BRAF V600E mutation is the causal genetic event in the vast majority of HCL
- Mutation constitutively activates BRAF by autophosphorylation of the protein and downstream MEK-ERK signaling pathway, leading to increased expression of genes involved in survival and proliferation and promoting leukemic transformation (Blood 2016;128:1918)
Etiology
- Epidemiologic data shows a multifactorial etiology that is influenced by ethnicity and geographical factors
- Farming and exposure to pesticides, petroleum products, diesel and ionizing radiation are associated with an increased risk (Best Pract Res Clin Haematol 2015;28:175)
Clinical features
- Pancytopenia and monocytopenia are common findings
- Often reported symptoms are fatigue and infection
- Splenomegaly: massive splenomegaly that can cause left sided abdominal pain is less commonly seen today due to early detection
- Lymphadenopathy is not usually seen in HCL (Blood 2017;129:553)
Diagnosis
- Diagnosis is based on peripheral blood and bone marrow morphology, flow cytometry immunophenotyping, immunohistochemistry and molecular studies
Laboratory
- CBC and differential count: pancytopenia and monocytopenia (Blood 2017;129:553)
- Peripheral blood smear morphology: circulating neoplastic hairy cells are present but at a low frequency and they can be difficult to identify
Prognostic factors
- Chronic, relatively indolent leukemia that predominantly responds well to current chemotherapy; 5 year event free survival rate after treatment is ~90%
- Poor prognostic factors include:
- Massive splenomegaly, leukocytosis (> 10 x 109/L), high number of neoplastic hairy cells in the blood (> 5 x 109/L) and high beta2 microglobulin (Blood 2012;119:3330)
- Unmutated IGHV status (Am J Hematol 2017;92:1382)
- IGHV4-34 positive immunoglobulin variable heavy chain gene rearrangement (Blood 2009;114:4687)
- CD38 expression (Cancer Res 2015;75:3902)
Case reports
- 16 year old boy presented with hairy cell leukemia (Blood 2018;132:1216)
- 41 year old man presented with unilateral sudden hearing loss as an initial manifestation of hairy cell leukemia (Int J Surg Case Rep 2019;60:200)
- Man in mid-60s presented with severe Legionnaires disease pneumonia associated with undiagnosed hairy cell leukemia (BMJ Case Rep 2019;12:e230130)
- 70 year old African American man with hairy cell leukemia presented with pancytopenia but without splenomegaly (Case Rep Hematol 2014;2014:354810)
- 72 year old man presented with coexisting chronic lymphocytic leukemia and hairy cell leukemia (Blood 2019;133:1264)
- 74 year old woman presented with osteolytic lesions in a case of hairy cell leukemia mimicking multiple myeloma (Lancet Oncol 2019;20:e187)
- 79 year old man with relapsed hairy cell leukemia diagnosed by endoscopic ultrasound guided FNA (Cytojournal 2006;3:1)
Treatment
- Not curative; asymptomatic patients usually do not require treatment
- Standard therapy is purine analogues (i.e., cladribine, pentostatin), which are effective in the majority of HCL
- Late relapses are not uncommon; choices for relapsed and refractory HCL include moxetumomab (anti-CD22), pasudotox (anti-CD22), vemurafenib (BRAF inhibitor) and bendamustine plus rituximab
- Splenectomy as salvage therapy (Blood 2017;129:553)
Gross description
- Spleen: splenomegaly, > 150 g; spleen shows a diffuse and marked enlargement without nodules
Microscopic (histologic) description
- Spleen:
- Red pulp involvement by sheets of bland tumor cells that are larger than lymphocytes with modest, pale blue agranular cytoplasm, round or folded nuclei and no distinct nucleoli
- There is an increase in volume, surface and length of red pulp vessels that can classically form pools or lakes of blood lined by hairy cells
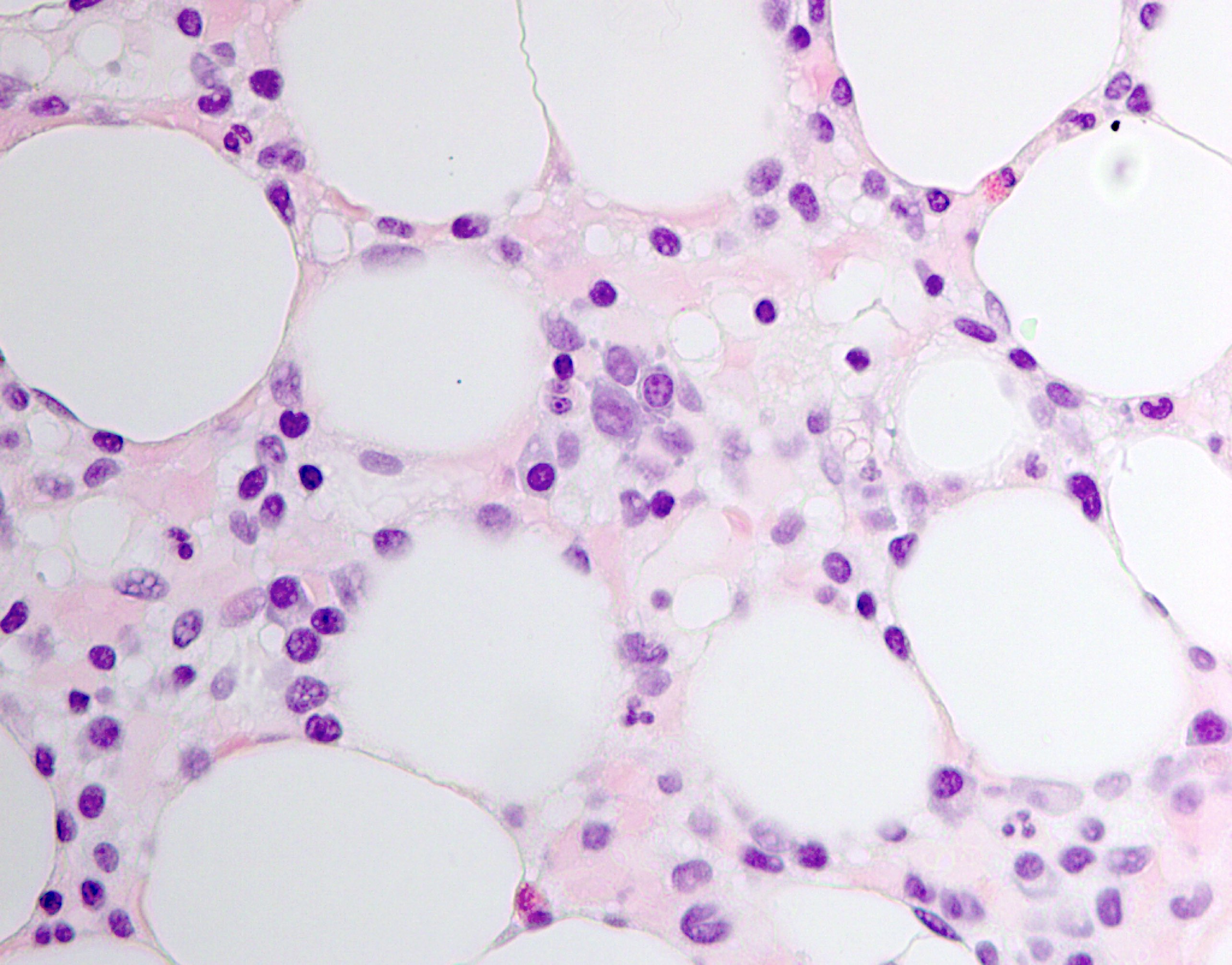
- Bone marrow:
- Bone marrow aspirate is often a dry tap due to extensive marrow fibrosis as demonstrable by reticulin stain; however, neoplastic hairy cells, as described in the peripheral blood description, can be seen (Blood 2003;102:1051)
- Bone marrow biopsy: always involved
- Neoplastic infiltrates can vary and have a patchy and subtle, interstitial or diffuse solid pattern
- Presence of fibrosis is common; ~10% of cases can be markedly hypocellular and mimic aplastic anemia
Microscopic (histologic) images
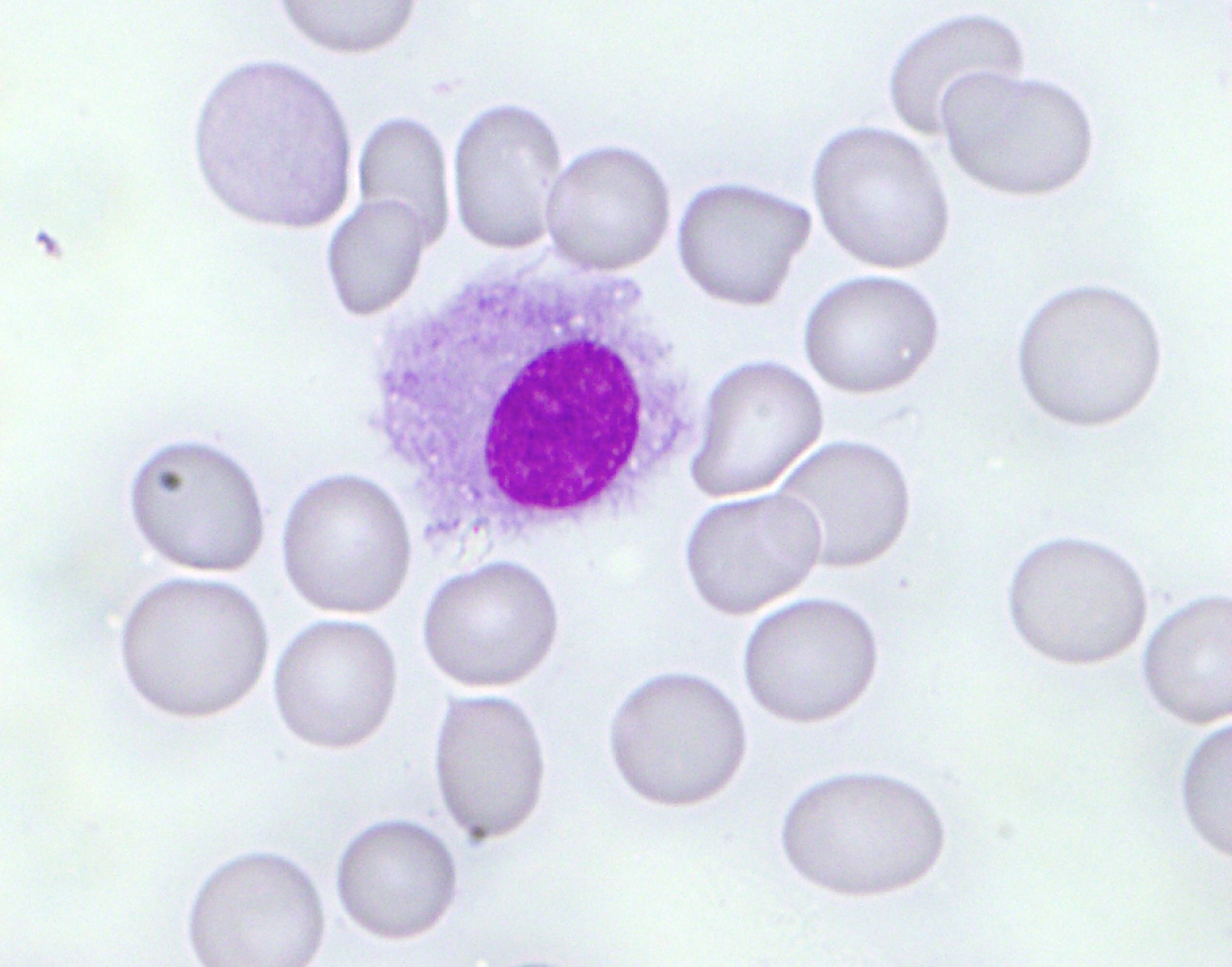
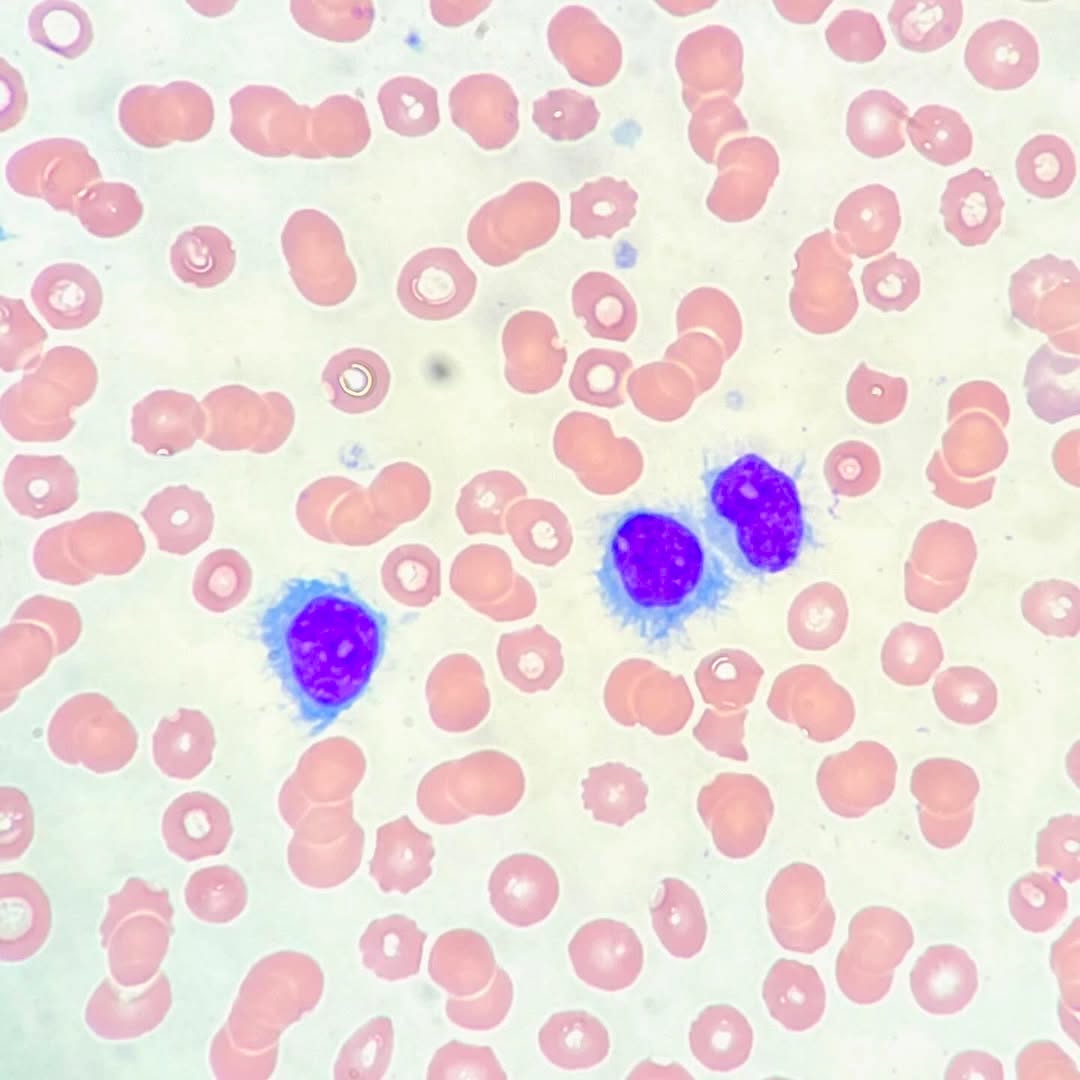
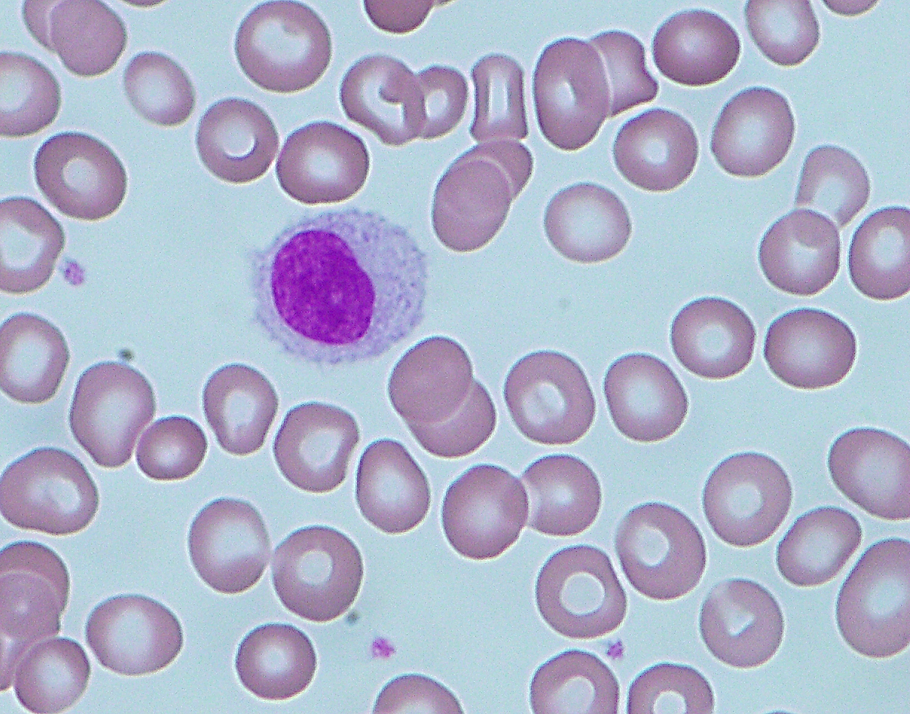
Peripheral smear description
- Smear shows pancytopenia with rare hairy cells that are medium in size with moderately abundant pale blue cytoplasm, reniform nuclei, open chromatin, absent nucleoli and a characteristic serrated cytoplasmic border (Blood 2017;129:553)
Peripheral smear images
Contributed by Buthaina Al-Maashari, M.D., Dietrich Werner, M.D. and @pleasingpathology on Instagram
Images hosted on other servers:
Positive stains
- Bone marrow IHC stain is important to appreciate tumor infiltration
- Typical pattern for B cell lymphocytes includes CD19, CD20, CD79a and PAX5
- Annexin A1 expression is specific to distinguishing HCL from other B cell lymphomas including HCL variant; however, correlation with B cell markers is needed, particularly in hypocellular and low tumor burden cases since annexin is also expressed by T cells and myeloid cells (Lancet 2004;363:1869)
- TRAP (tartrate resistant acid phophotase): done by immunohistochemistry; in the aspirate smears, TRAP test by enzyme stain is not commonly done anymore since it is a more difficult technical and interpretative procedure
- TRAP IHC in the core biopsy is currently more commonly used
- DBA-44: combined TRAP and DBA-44 is sensitive and fairly specific (Am J Surg Pathol 2005;29:474)
- Cyclin D1: positive staining; dim staining compared to what is seen in mantle cell lymphoma (Mod Pathol 2000;13:1308)
- BRAF V600E: positive overexpression by immunohistochemistry studies; point mutations are also detected by molecular studies
- Reticulin is increased due to the presence of fibrosis
- TIA1 is seen in 56% of cases (Mod Pathol 2004;17:840)
Negative stains
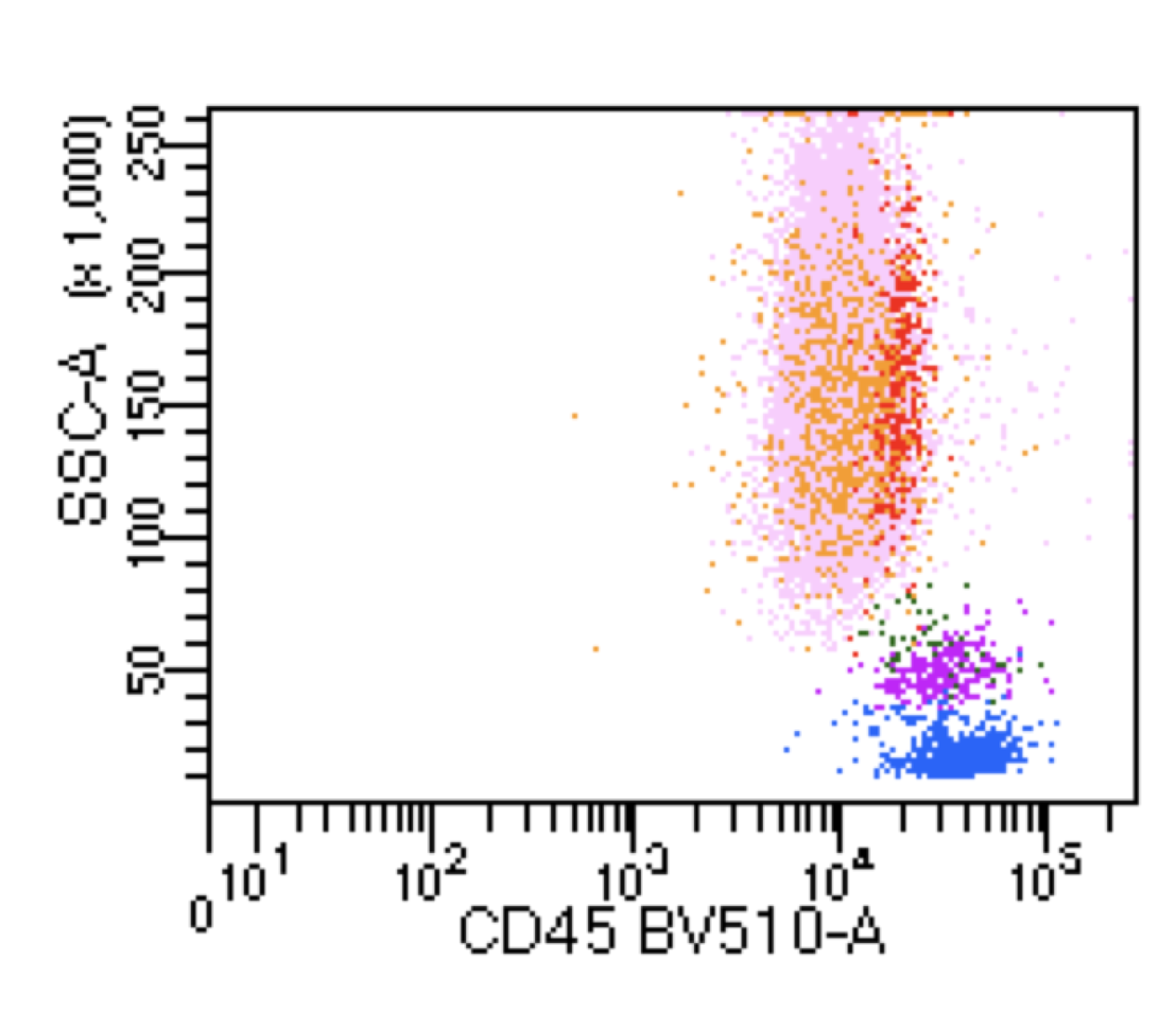
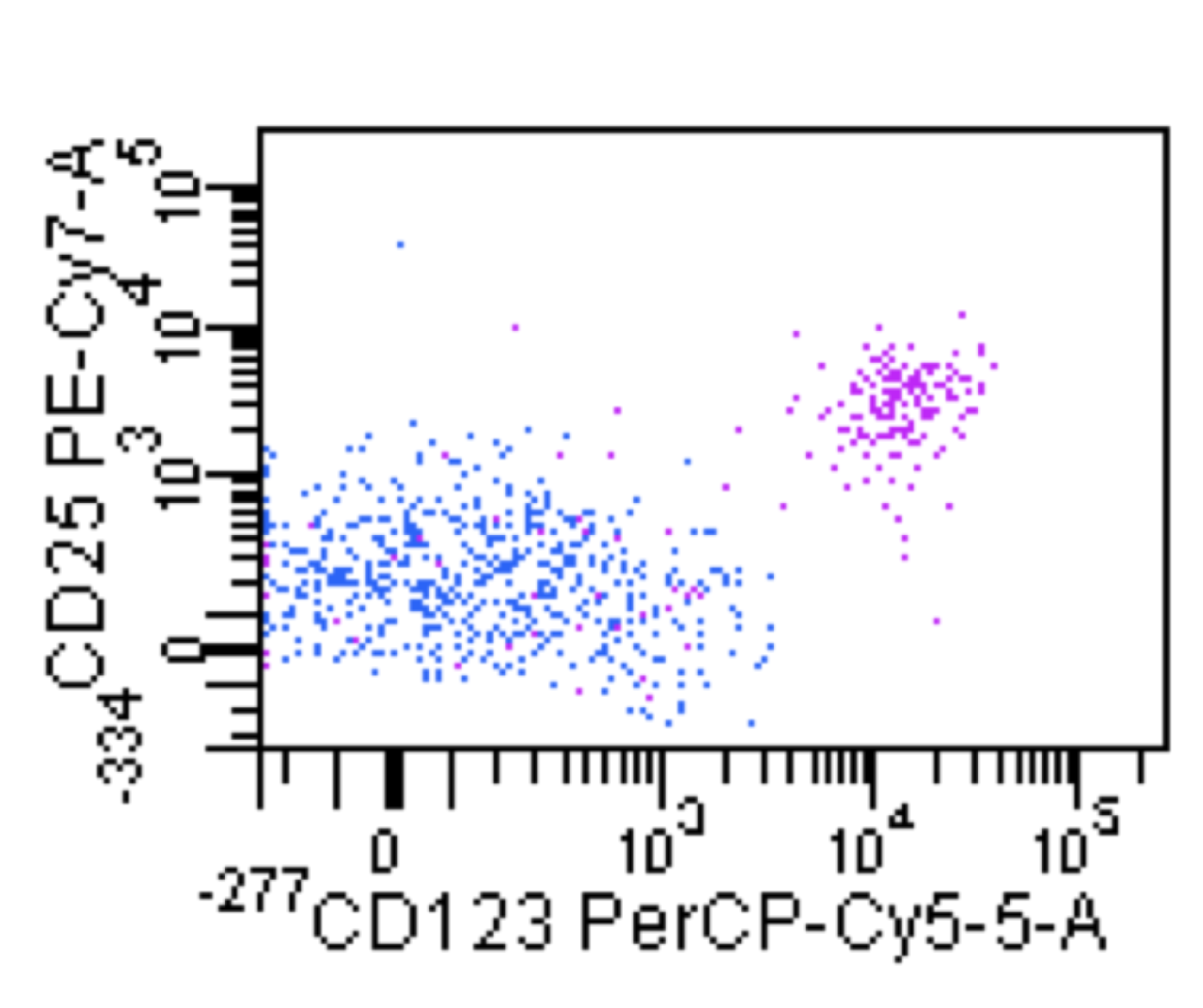
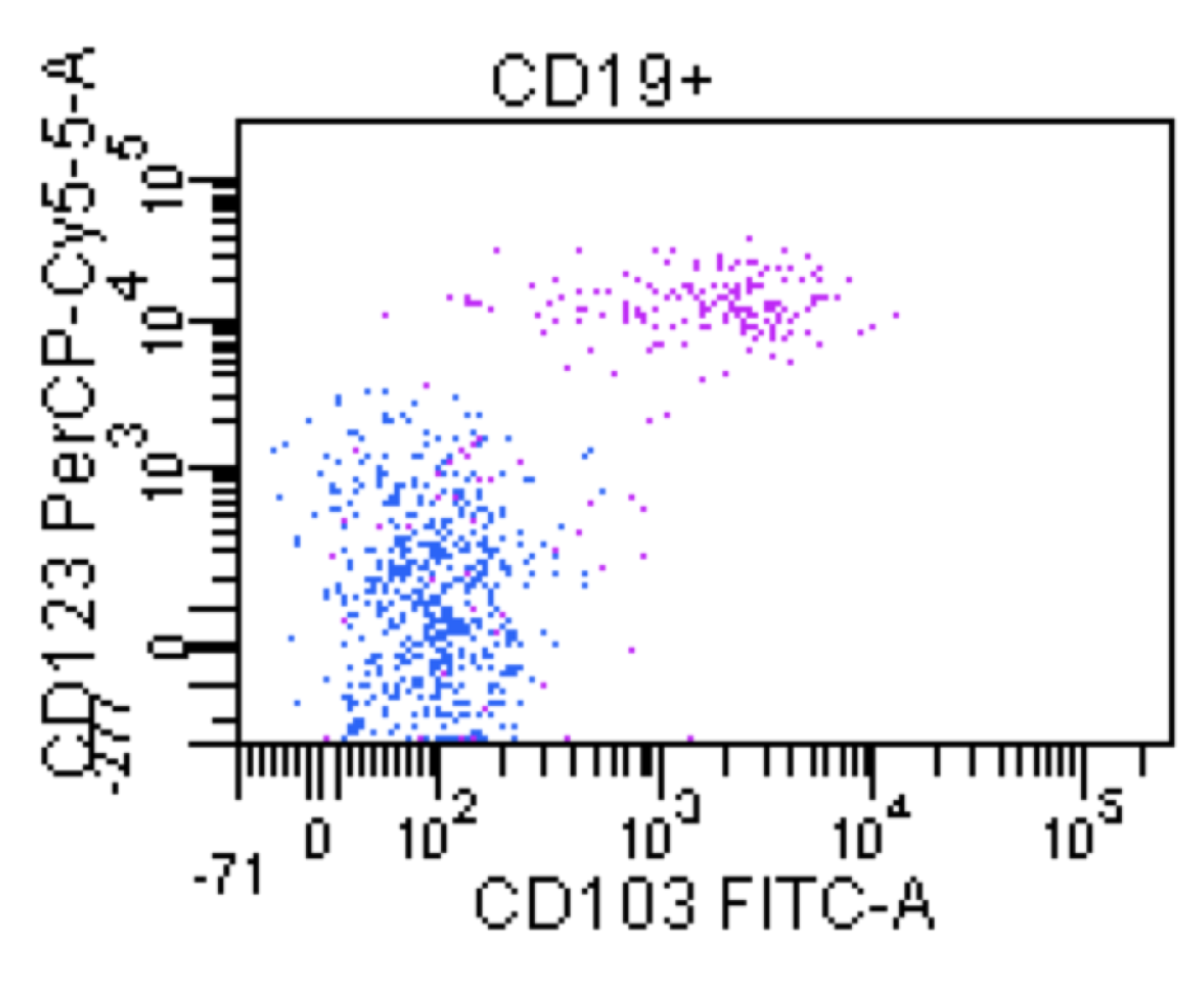
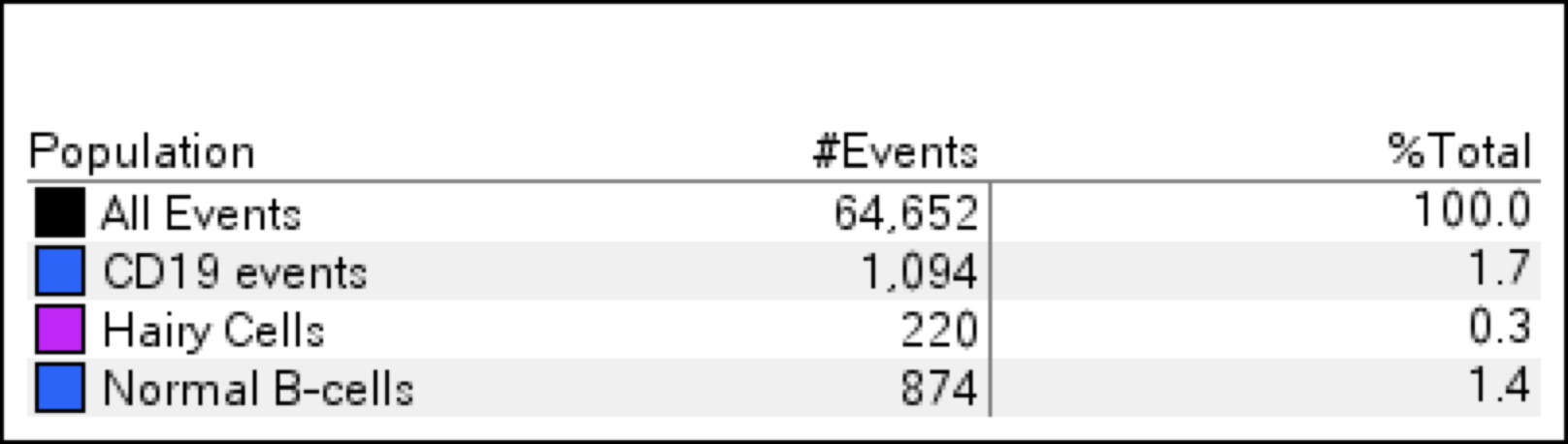
Flow cytometry description
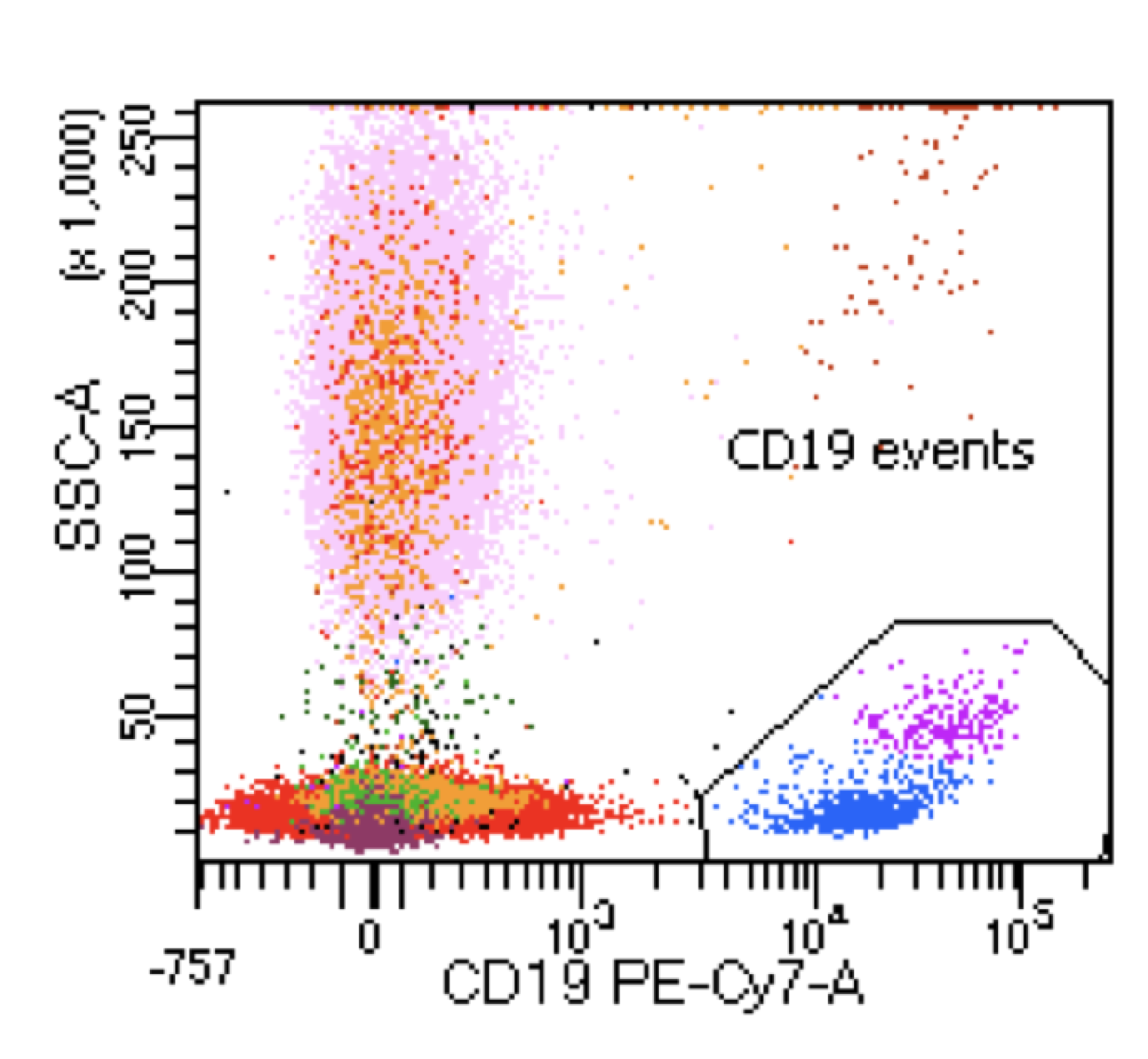
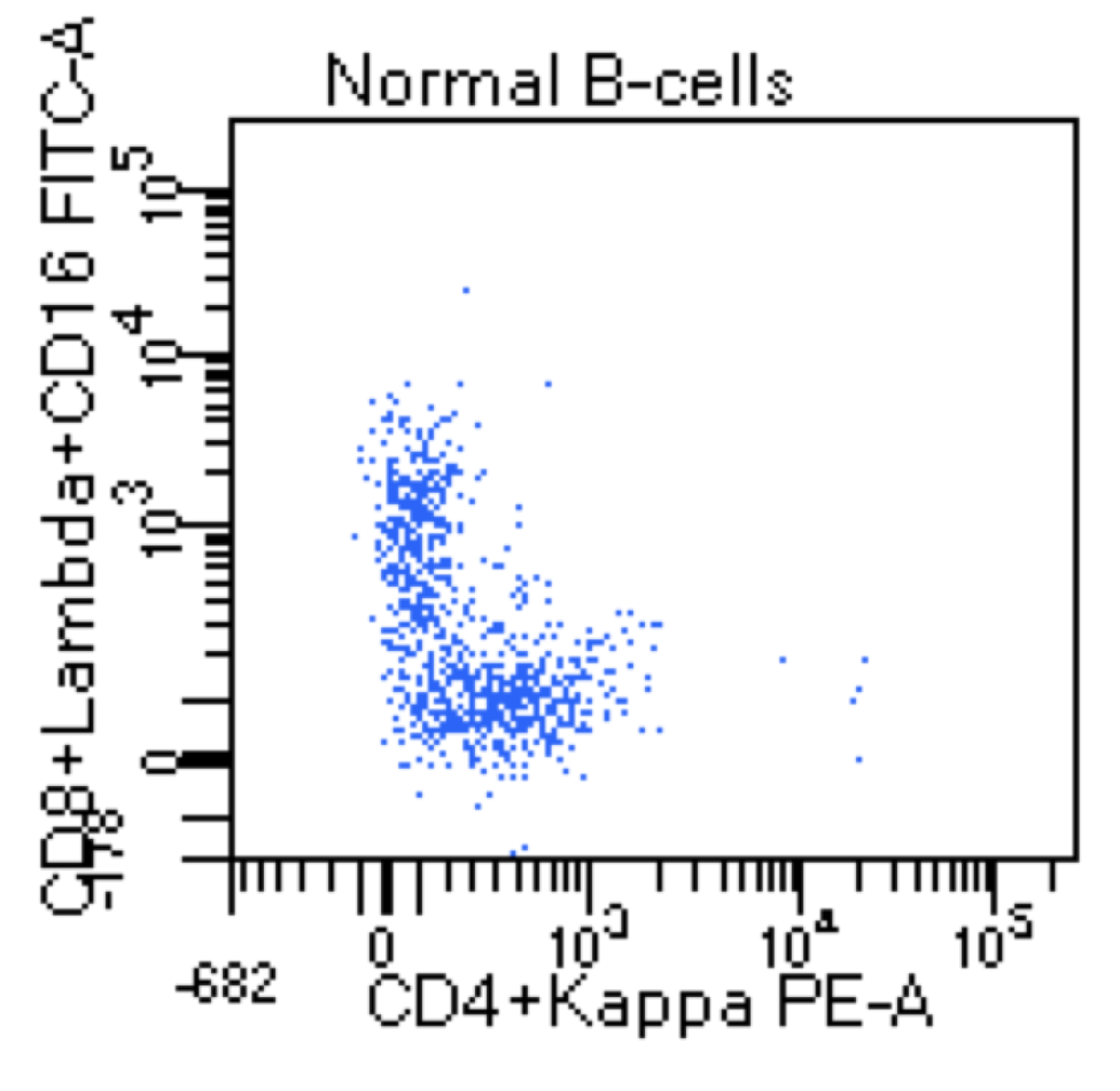
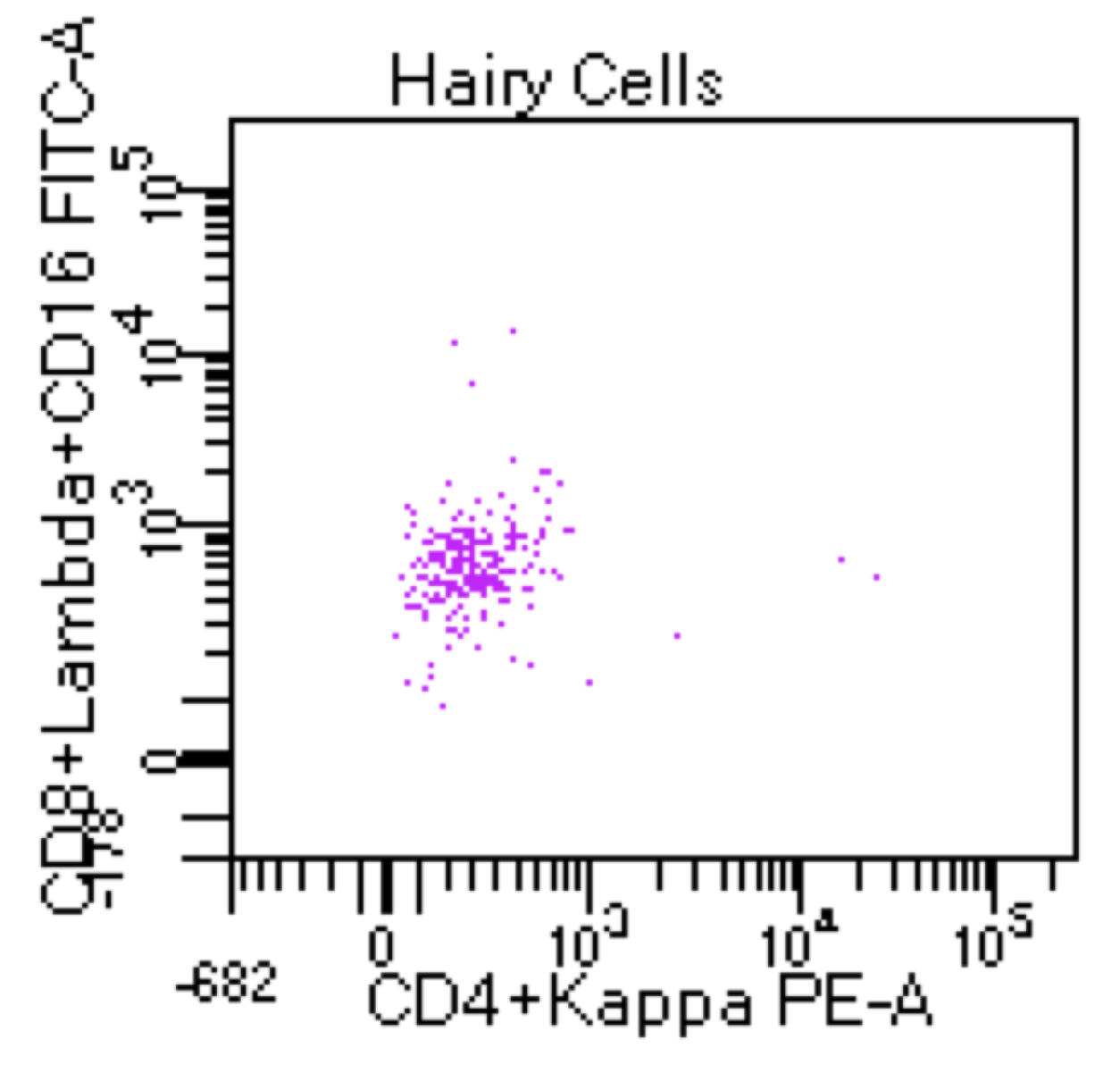
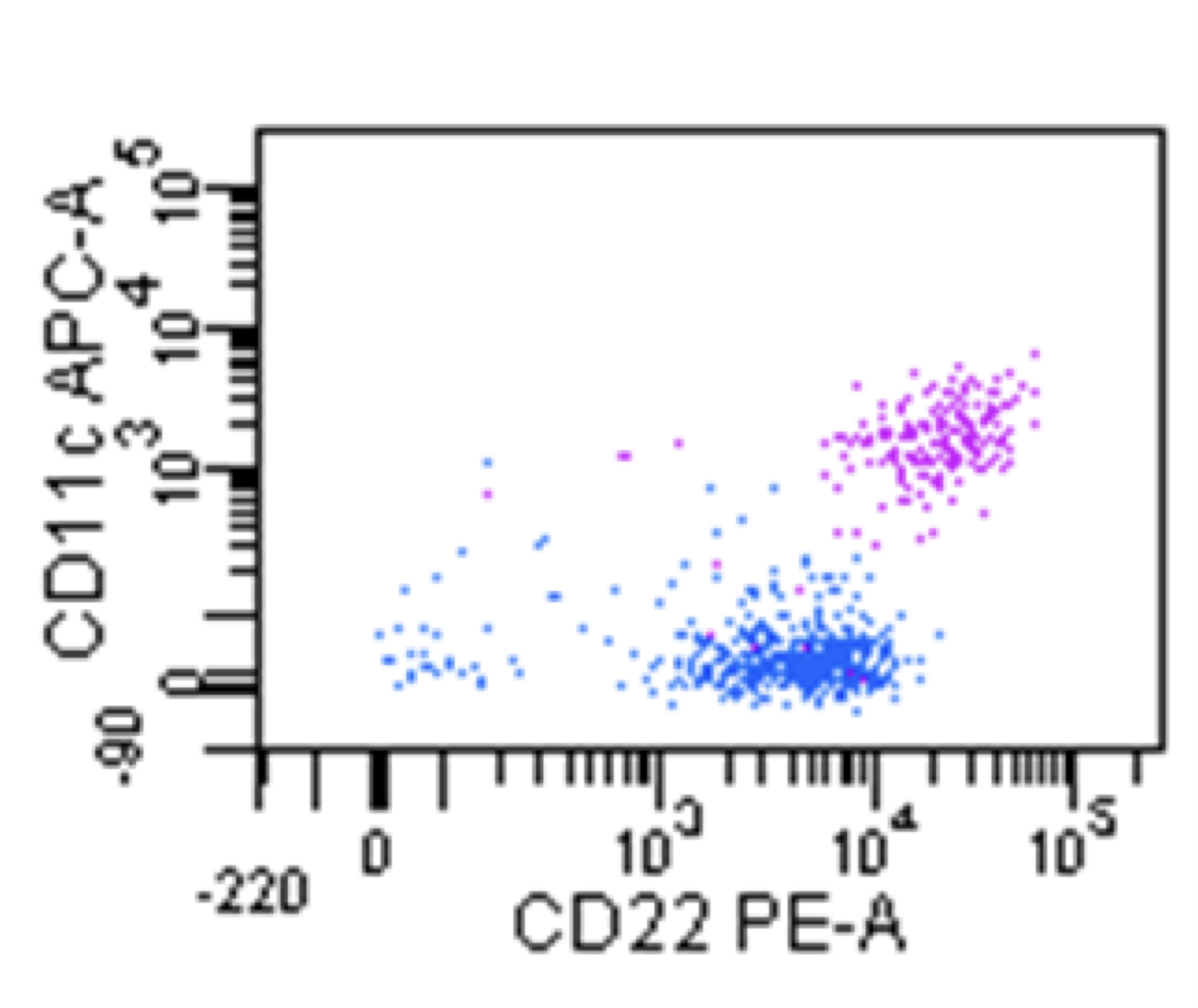
- Flow cytometry immunophenotyping is helpful for the diagnosis of HCL (Leuk Lymphoma 2011;52:11)
- HCL has high side scatter and it is placed in the monocytic region on a CD45 / SSC plot
- Bright expression of CD20, CD22 and monotypic surface light chain immunoglobulin
- Positive expression for CD11c
- Positive coexpression for specific hairy cell leukemia markers CD123, CD103, CD25 and CD305 (LAIR)
- Positive expression for CD200
- Usually negative or dim for CD5, CD23, CD10, CD79b and CD27
- ~10% of cases show CD10 coexpression (Am J Clin Pathol 2003;120:228)
Flow cytometry images
Electron microscopy description
- A cytoplasmic inclusion known as the ribosome - lamellae complex (RLC) has been described but may also occur in other hematolymphoid neoplasms (Lab Invest 1980;42:236, Arch Pathol Lab Med 1991;115:1259, Ultrastruct Pathol 2007;31:135)
Molecular / cytogenetics description
- BRAF V600E mutation is a hallmark for classical HCL; this mutation is not seen in HCL variant
- Rare cases that are BRAF V600E mutation negative will be positive for IGHV4-34
- Histone methyltransferase KMT2C (MLL3) and CDKN1B are commonly mutated genes in cHCL
- BRD4, CEBPA, CREBBP, RUNX1, EP300 and MED12, Notch signaling (NOTCH1 and NOTCH2) and DNA repair
- Deletions of chromosomes 7q and 13q and gains of chromosome 5 (Blood 2017;130:1644)
Sample pathology report
- Bone marrow, (R)PSIS, aspirate, biopsy and peripheral blood:
- Positive for classical hairy cell leukemia involving ~40% of the sample (see comment)
- Comment: Peripheral blood with pancytopenia and rare circulating neoplastic hairy cells, < 1%. Hypocellular bone marrow, 15 - 20% with decreased trilineage hematopoiesis. Positive for hairy cell leukemia involving ~40% of the sample. Tumor burden is based on the core biopsy with the help of immunohistochemistry that is felt to be more accurate for this case. Flow cytometry shows a small clonal population in ~2% of the sample that shows positive coexpression for the specific hairy cell leukemia markers CD123, CD103 and CD25. Next generation sequencing is positive for BRAF V600E mutation. Flow cytometry and molecular studies support the diagnosis.
Differential diagnosis
- Splenic B cell lymphoma / leukemia with prominent nucleoli, formerly known as HCL variant (HCL-v):
- Splenic marginal zone lymphoma:
- Can have circulating neoplastic cells with cytoplasmic projections; these cells are called villous lymphocytes
- Usually show involvement of the white pulp in the spleen and are negative for classical hairy cell markers CD123, CD103, CD25 and CD305 (LAIR) by flow cytometry
- Negative by IHC for annexin 1 and cyclin D1 and negative for BRAF V600E mutations
- Splenic diffuse red pulp lymphoma (SDRPL):
Additional references
Board review style question #1
Board review style answer #1
Board review style question #2
Molecular testing detected a BRAF V600E mutation on a bone marrow sample that contained a B cell clonal population that fell on the monocyte gate by flow cytometry and is estimated to constitute ~4% of the total sample. What is your diagnostic interpretation?
- Chronic lymphocytic leukemia
- Diffuse large B cell lymphoma
- Hairy cell leukemia
- Mantle cell lymphoma
- Monoclonal B cell lymphocytosis
Board review style answer #2