Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Cytology description | Cytology images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Bladek P, Murga-Zamalloa C. Fluid overload associated LBCL. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lymphomafluidoverloadlbcl.html. Accessed April 1st, 2025.
Definition / general
- Body cavity large B cell lymphoma with no associated solid lymphoma involvement in immunocompetent individuals
- Negative for HHV8 infection and does not occur in the setting of chronic inflammatory / infectious related effusions
Essential features
- B cell lymphoma composed of large malignant cells present in body cavity effusions without any solid tissue lymphoma involvement
- Predominantly diagnosed in elderly and immunocompetent individuals with comorbidities that put them at risk for developing body cavity effusions (e.g., congestive heart failure, cirrhosis)
- Not associated with HHV8 infection
- EBV infection can be detected only in a minority of cases
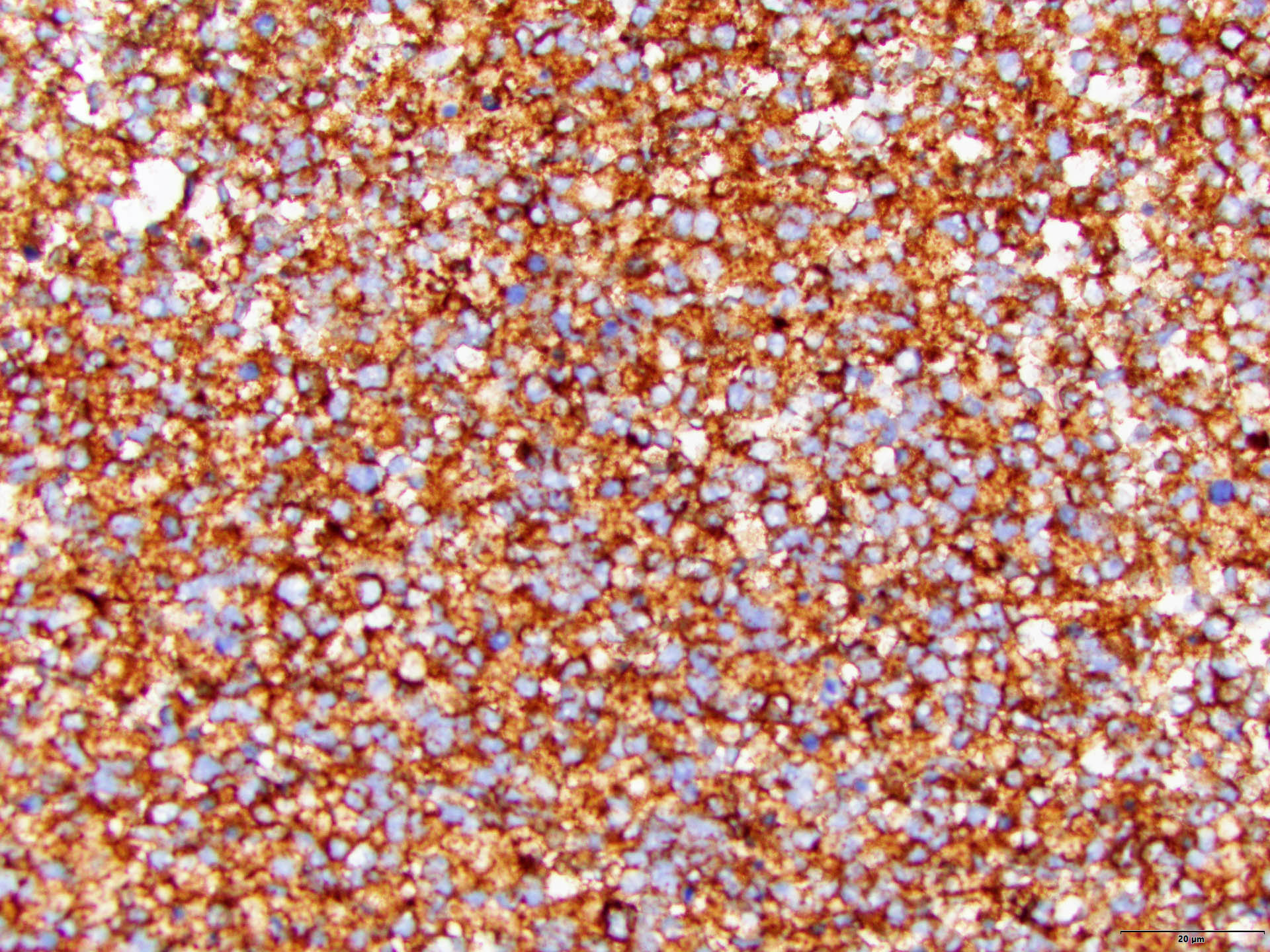
- Tumor cells are frequently positive for B cell markers (CD20, PAX5) and most are of nongerminal center type per the Hans algorithm
- References: Mod Pathol 2022;35:1411, J Blood Med 2021;12:833, J Am Soc Cytopathol 2015;4:37, Blood Adv 2020;4:4442, Histopathology 2018;72:930
Terminology
- Primary effusion lymphoma (PEL)-like lymphoma
- HHV8 negative effusion based large B cell lymphoma
- HHV8 negative malignant effusion lymphoma
- PEL-like lymphoma
- HHV8 unrelated PEL-like lymphoma
- Type II PEL
Epidemiology
- Represents < 1% of all diagnosed lymphomas
- Predominantly elderly patients (median age: 79)
- M:F = 1.26:1
- HIV positive (2% of individuals)
- Risk of fluid overload (e.g., congestive heart failure, cirrhosis) in 50 - 79% of cases
- References: Leuk Lymphoma 2017;58:80, Mod Pathol 2022;35:1411
Sites
- Body cavities, predominantly the pleural cavity
- May also be present in pericardial and peritoneal fluids
- Solid lymphoma involvement is absent
- Reference: Mod Pathol 2022;35:1411
Pathophysiology
- Most of the reported cases derive from postgerminal center B cell lymphocytes (Blood 2019;133:377)
Etiology
- Uncertain; ~50 - 79% feature fluid retention secondary to other comorbidities (Oncol Lett 2020;20:343)
Clinical features
- B symptoms are present in a minority of cases
- Association with hepatitis C virus infection in ~15% of cases
- Immunodeficiency is present in < 5% of cases
- References: Oncol Lett 2020;20:343, Mod Pathol 2022;35:1411, Am J Clin Pathol 2013;140:258
Diagnosis
- Nongynecological cytology analysis of effusion fluid
- Flow cytometry analysis of effusion fluid
Laboratory
- Findings depend on the site of fluid effusion and are otherwise nonspecific
- Lactate dehydrogenase (LDH) is typically elevated
Prognostic factors
- Overall survival was 11 months for non-Japanese residents and the median overall survival was 63.6 months for Japanese residents
- Presence of MYC rearrangements is associated with the worst survival
- Age of ≥ 79 is an independent unfavorable predictor
- References: Mod Pathol 2022;35:1411, Haematologica 2002;87:339
Case reports
- 65 year old woman noted to have monoclonal IgM spike in the pleural fluid (Am J Clin Pathol 2013;140:258)
- 70 year old man with abdominal pain and distention as well as accompanying dermatological symptoms (Front Oncol 2023;13:1145540)
- 72 year old immunocompetent woman with no medical history and new onset of idiopathic pericardial effusion (Lancet Haematol 2023;10:e306)
- 81 year old man with extensive heart disease and fluid overload, followed by cardiac complications of chemotherapy (J Blood Med 2021;12:833)
Treatment
- No standardized therapeutic approach is available due to the limited number of cases reported
- First line management usually includes rituximab combined with systemic chemotherapy
- Therapeutic drainage of effusions as the sole therapeutic intervention is performed in patients unsuitable for systemic chemotherapy
- Reference: Mod Pathol 2022;35:1411
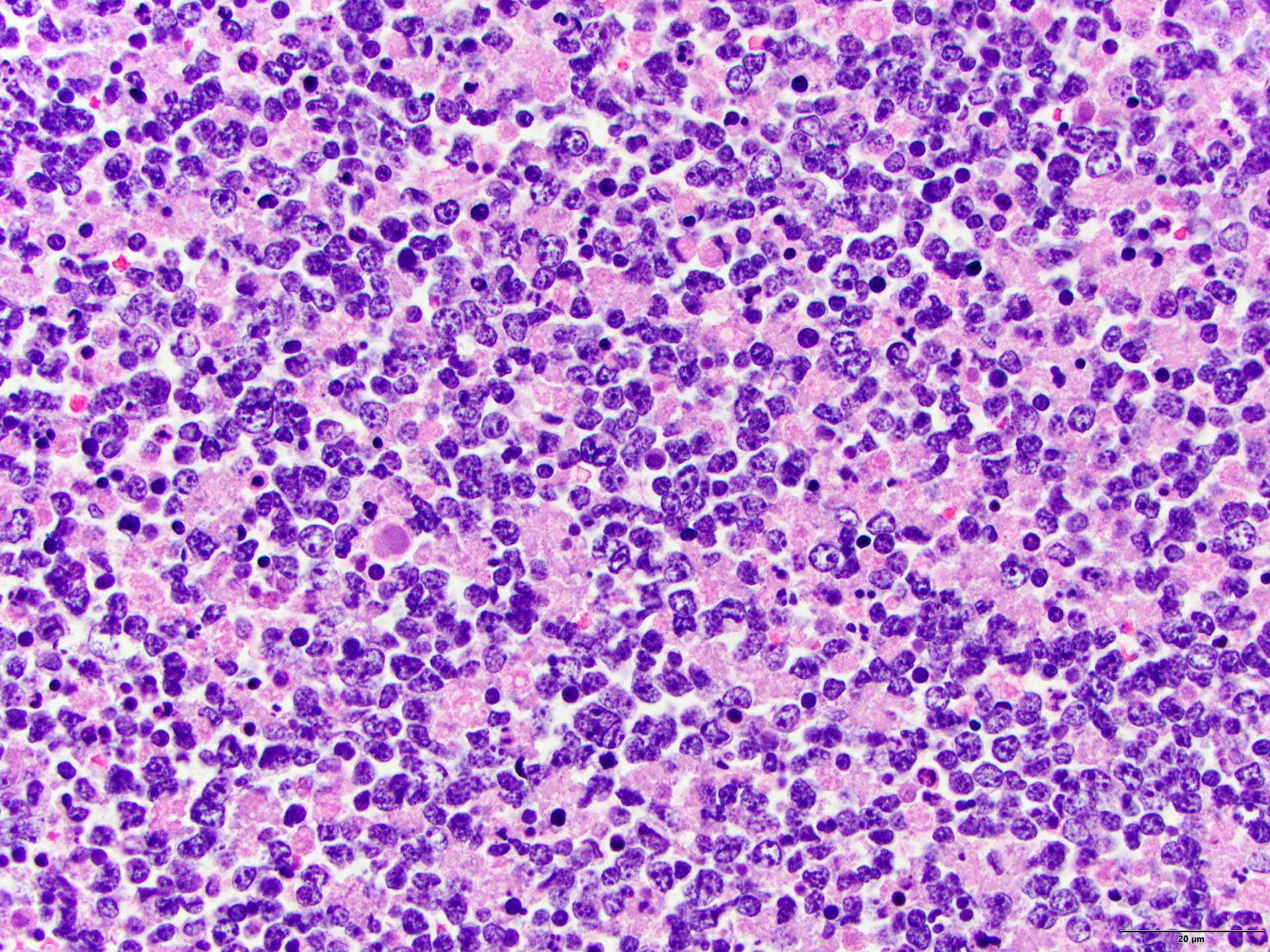
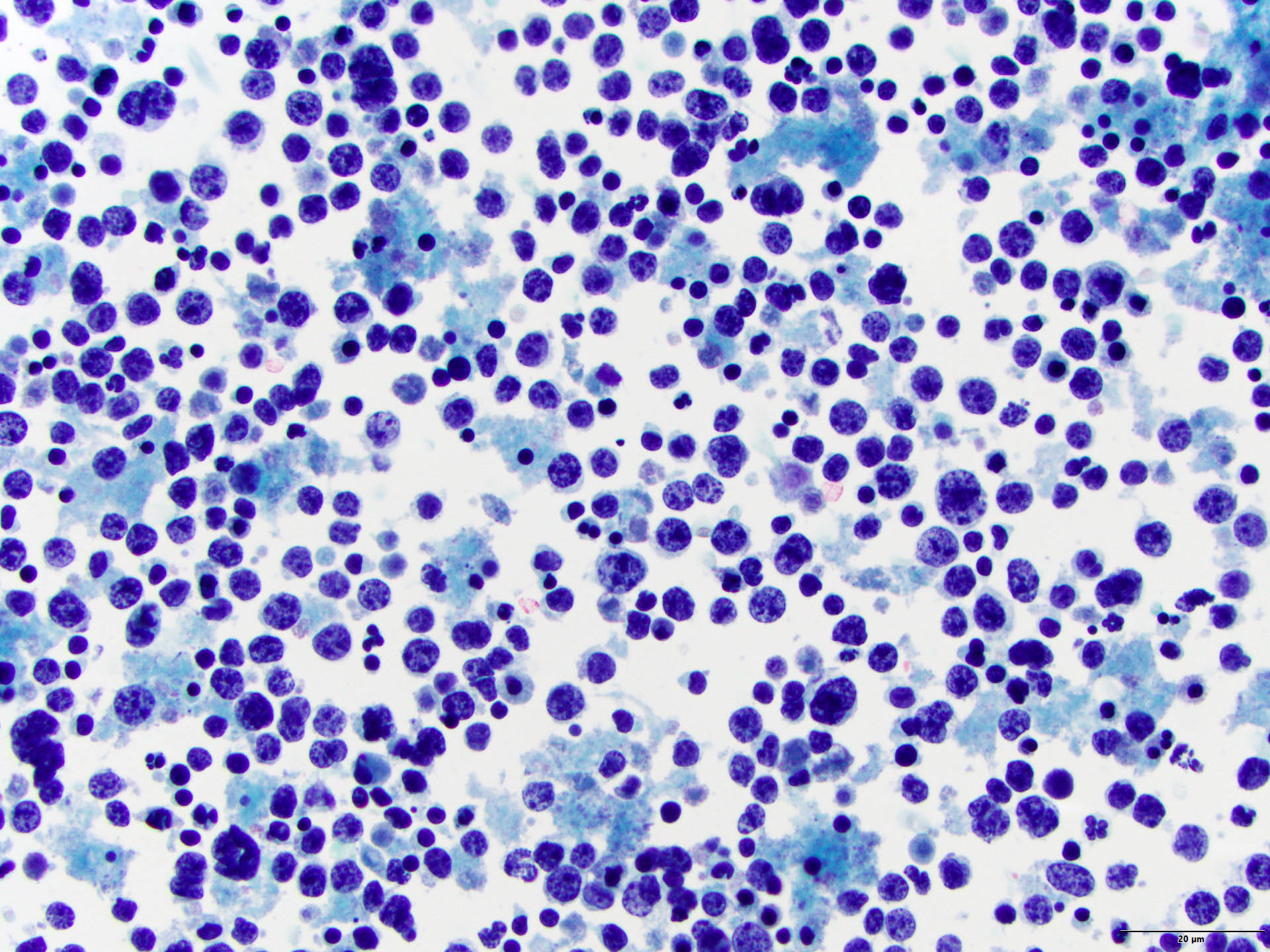
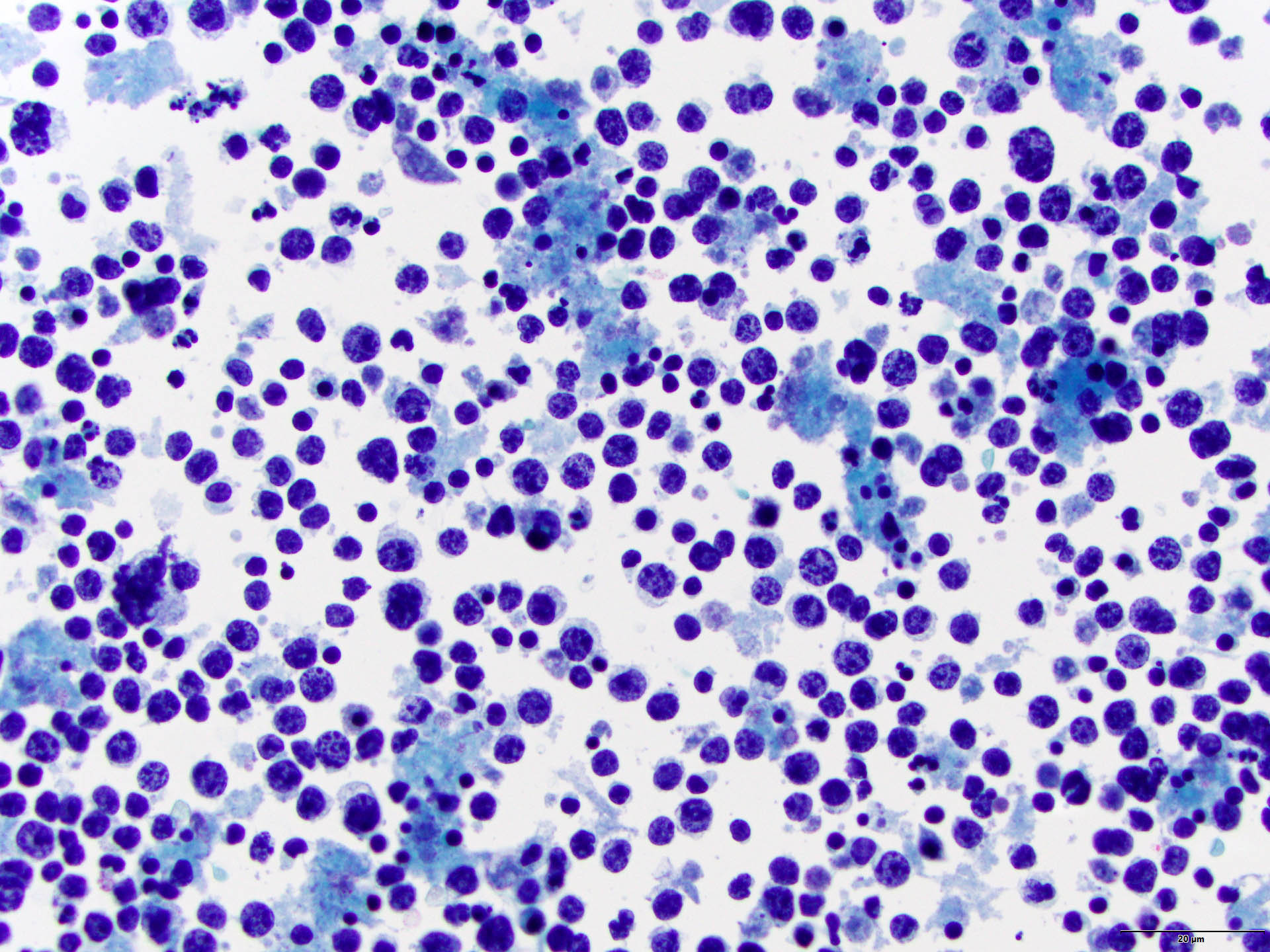
Cytology description
- Cellular effusion that is predominantly composed of lymphocytes
- Lymphocytes are large in size
- Lymphocytes show atypical features and are pleomorphic with centroblastic, immunoblastic or anaplastic morphologies
- References: Histopathology 2018;72:930, Am J Clin Pathol 2013;140:258, Mod Pathol 2022;35:1411
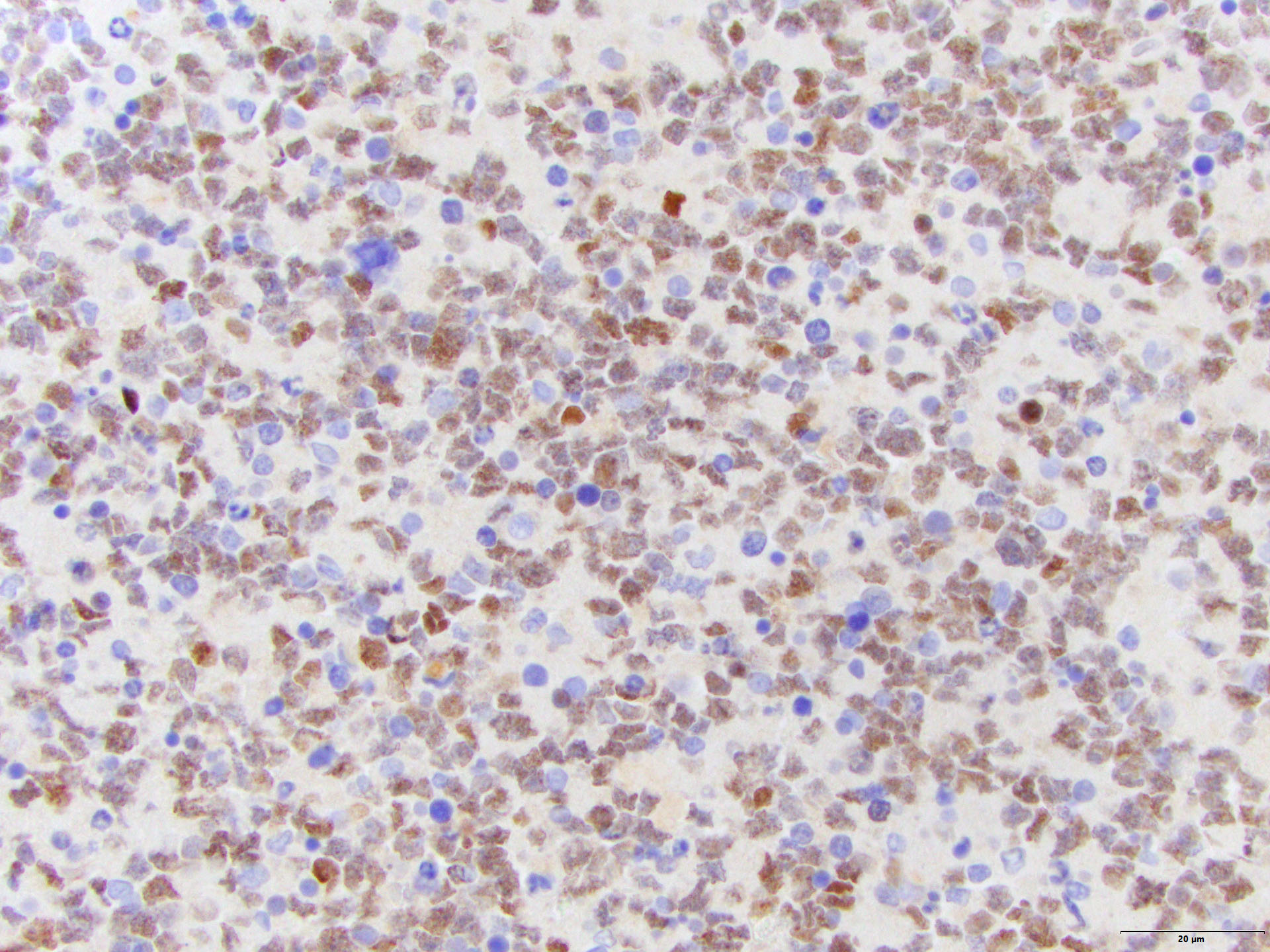
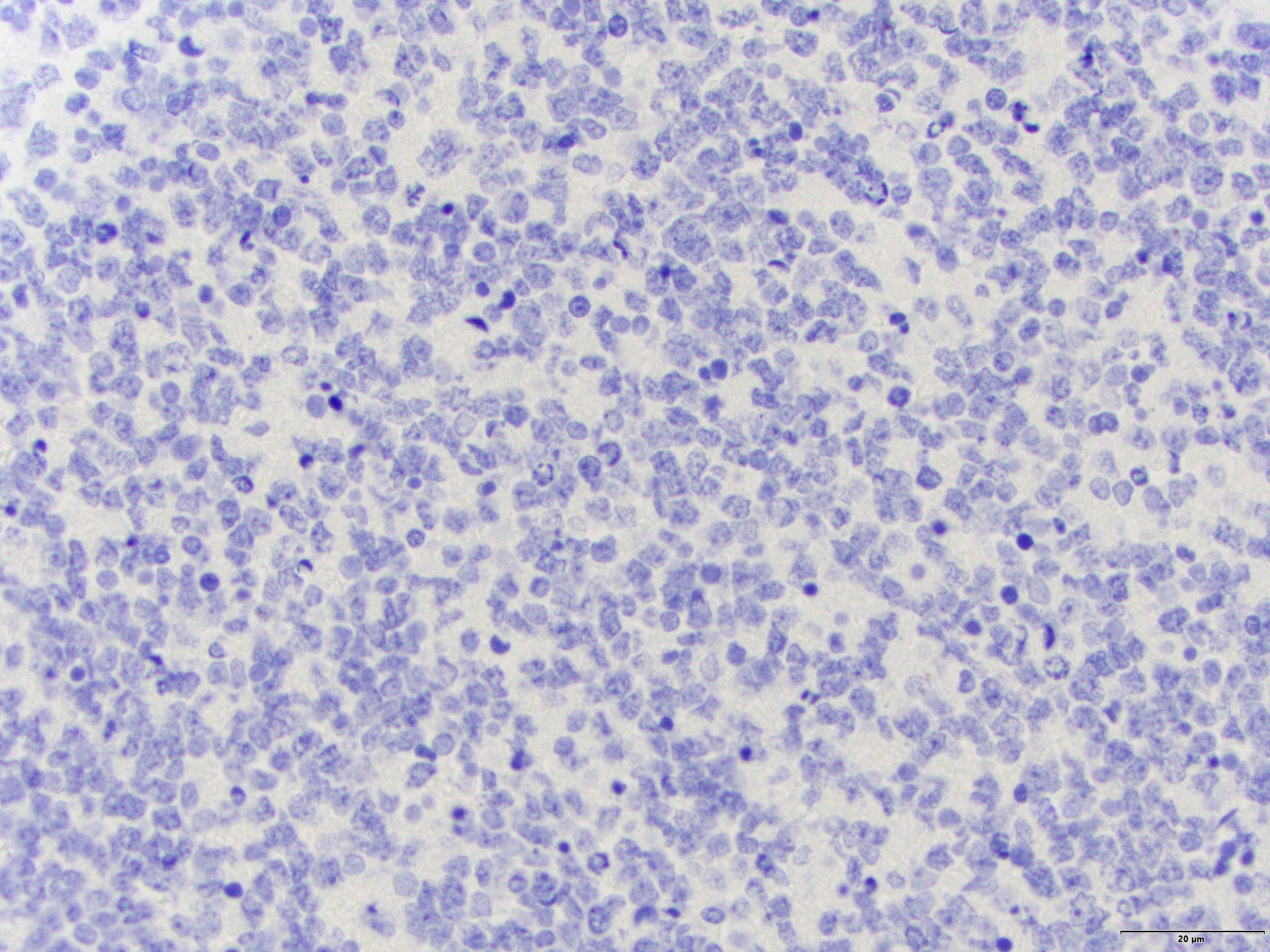
Cytology images
Positive stains
Negative stains
- HHV8
- CD138 (positive in 4 - 6% of cases)
- CD30 (variably positive in a subset of cells in 10 - 27% of cases)
- CD10 (positive in 13 - 16% of cases)
- Reference: Am J Clin Pathol 2013;140:258
Molecular / cytogenetics description
- BCL2 rearrangement (8 - 29% of cases)
- BCL6 rearrangement (11 - 21% of cases)
- MYC rearrangement (11 - 22% of cases)
- Recurrent mutations in MYD88 (including L265P) are identified in some cases (Blood 2019;133:377)
Sample pathology report
- Pleural fluid, thoracocentesis:
- Involved by HHV8 negative large B cell lymphoma (see comment)
- Comment: In the right clinical context and with the absence of involvement by lymphoma in solid tissues, the diagnosis is consistent with fluid overload associated LBCL.
Differential diagnosis
- Primary effusion lymphoma:
- Pyothorax associated lymphoma:
- Occurs in the setting of chronic inflammation and is EBV driven
- Patients are usually young with a longstanding history of pyothorax or pleuritis secondary to infectious etiologies (e.g., tuberculosis)
- Associated with solid lesions in the pleura or lung
- B cell lymphomas with associated pleural effusions:
- Other B cell lymphomas can secondarily involve the pleural, peritoneal or pericardial cavities, including Burkitt lymphoma, mantle cell lymphoma, plasmablastic lymphoma and diffuse large B cell lymphoma
- Nodal or solid tissue involvement is present at presentation or has been established before the effusion associated lymphoma
Board review style question #1
Which of the following is true regarding fluid overload associated LBCL?
- Association with tuberculosis related chronic pleural effusions is commonly observed
- Clinical course is usually indolent
- Diagnosis is usually established from lymph node biopsies
- Patients are usually young individuals
- Tumor cells are frequently positive for pan-B cell markers
Board review style answer #1
E. Tumor cells are frequently positive for pan-B cell markers, including CD20, PAX5 and CD79a. Answer A is incorrect because in contrast to pyothorax associated lymphoma, fluid overload associated LBCL is not associated with infectious / chronic pleural effusions, such as those associated with tuberculosis. Answer C is incorrect because per definition, no solid lymphoma involvement is detected. Answer B is incorrect because although initial reports suggested indolent clinical behaviors, larger series demonstrate poor clinical outcomes. Answer D is incorrect because this entity is predominantly diagnosed in elderly individuals and the median age of diagnosis is 79 years.
Comment Here
Reference: Fluid overload associated LBCL
Comment Here
Reference: Fluid overload associated LBCL
Board review style question #2
Which of the following is true regarding fluid overload associated LBCL?
- Cases are only delimited to the pleural cavity
- Cell of origin is predominantly germinal center type (by the Hans algorithm)
- Expression of CD30 is observed in virtually all the cases
- Patients are usually elderly immunocompetent individuals
- Presence of MYC rearrangements excludes the diagnosis
Board review style answer #2
D. Patients are usually elderly immunocompetent individuals. Most cases are detected in immunocompetent and elderly individuals. Answer A is incorrect because the tumor cells can involve other body cavities different from the pleural cavity, including the pericardial and peritoneal cavities. Answer C is incorrect because only 10 - 27% of the cases feature variable CD30 positive staining. Answer B is incorrect because the majority of the cases are nongerminal center types per the Hans algorithm. Answer E is incorrect because the presence of MYC rearrangements is associated with decreased survival and poor prognosis.
Comment Here
Reference: Fluid overload associated LBCL
Comment Here
Reference: Fluid overload associated LBCL