Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2 | Board review style question #3 | Board review style answer #3Cite this page: Hall JM. Fibrin associated large B cell lymphoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lymphomafibrinassoc.html. Accessed April 2nd, 2025.
Definition / general
- Very rare, indolent, non mass forming, Epstein-Barr virus (EBV)+ large B cell lymphoproliferative disorder
- Noted incidentally on histological examination of tissues excised for some other reason (Am J Surg Pathol 2017;41:299)
- Neoplastic cells are typically found within fibrinous or amorphous material
Essential features
- Very rare, indolent, microscopic, EBV+ large B cell lymphoproliferative disorder
- Localized to a restricted anatomic site
- Non mass forming, noninvasive with no direct clinical signs or symptoms
- Noted incidentally on histological examination of tissues excised for other reasons
- Location of lymphoma cells limited to fibrinous or amorphous eosinophilic material
- No infiltration or effacement of adjacent normal tissues
- Excellent prognosis, usually with surgical excision alone
Terminology
- Fibrin associated (EBV+) large B cell lymphoma (FA DLBCL)
- Subtype of: diffuse large B cell lymphoma associated with chronic inflammation
ICD coding
Epidemiology
- EBV associated
- Median age 55.5 years
- M:F = 3:1
- No ethnic or racial predilection
Sites
- Localized disease in various restricted anatomic sites (Am J Surg Pathol 2017;41:299, Am J Surg Pathol 2005;29:832, Mod Pathol 2010;23:493, Am J Surg Pathol 2012;36:1074, Virchows Arch 2020;476:647)
- Pseudocysts (renal, adrenal, splenic, paratesticular and retroperitoneal)
- Hydrocele
- Cardiovascular lesions (cardiac myxomas, fibrin thrombi, prostheses and synthetic grafts, chronic subdural hematoma)
- Wear debris associated with metallic implants
Pathophysiology
- Unknown at this time
Etiology
- Unknown at this time
- May be associated with foreign body or chronic inflammation in some cases
- Localized immune suppression, dysfunction or evasion may play a role (Am J Surg Pathol 2017;41:299, Am J Surg Pathol 2012;36:1074, Virchows Arch 2020;476:647)
Clinical features
- Patients usually immunocompetent (Am J Surg Pathol 2017;41:299)
- Distinction from aggressive EBV+ lymphomas can prevent overtreatment
Diagnosis
- Requires a high index of suspicion
- Lymphoma cells incidentally noted only on microscopic examination of tissues
- Exclude systemic or invasive disease and primary or iatrogenic immunosuppression
- Localized to a restricted anatomic site
Radiology description
- No evidence of lymphoma on imaging (if performed)
Prognostic factors
- Excellent prognosis, usually with surgical excision alone
- Very rare cases may progress or recur, especially if complete excision is less attainable (Am J Surg Pathol 2017;41:299, Pathol Int 2015;65:138)
Case reports
- 50 year old man with FA DLBCL identified in cardiac myxoma (Blood 2019;133:882)
- 52 year old man with accumulations of discohesive large cells in cystic spaces of the regressively changed tumor bed of a GIST (Case of the month #529)
- 60 year old man with FA DLBCL identified in left atrial myxoma (Cardiovasc Pathol 2020;49:107264)
- 64 year old woman with FA DLBCL identified in cerebral artery aneurysm (BMC Cancer 2019;19:916)
- 71 year old woman with FA DLBCL identified in adrenal pseudocyst (Br J Haematol 2019;185:397)
- 81 year old man with FA DLBCL identified in cranial arachnoid cyst (Acta Neuropathol Commun 2017;5:60)
Treatment
- Surgical excision alone is usually adequate
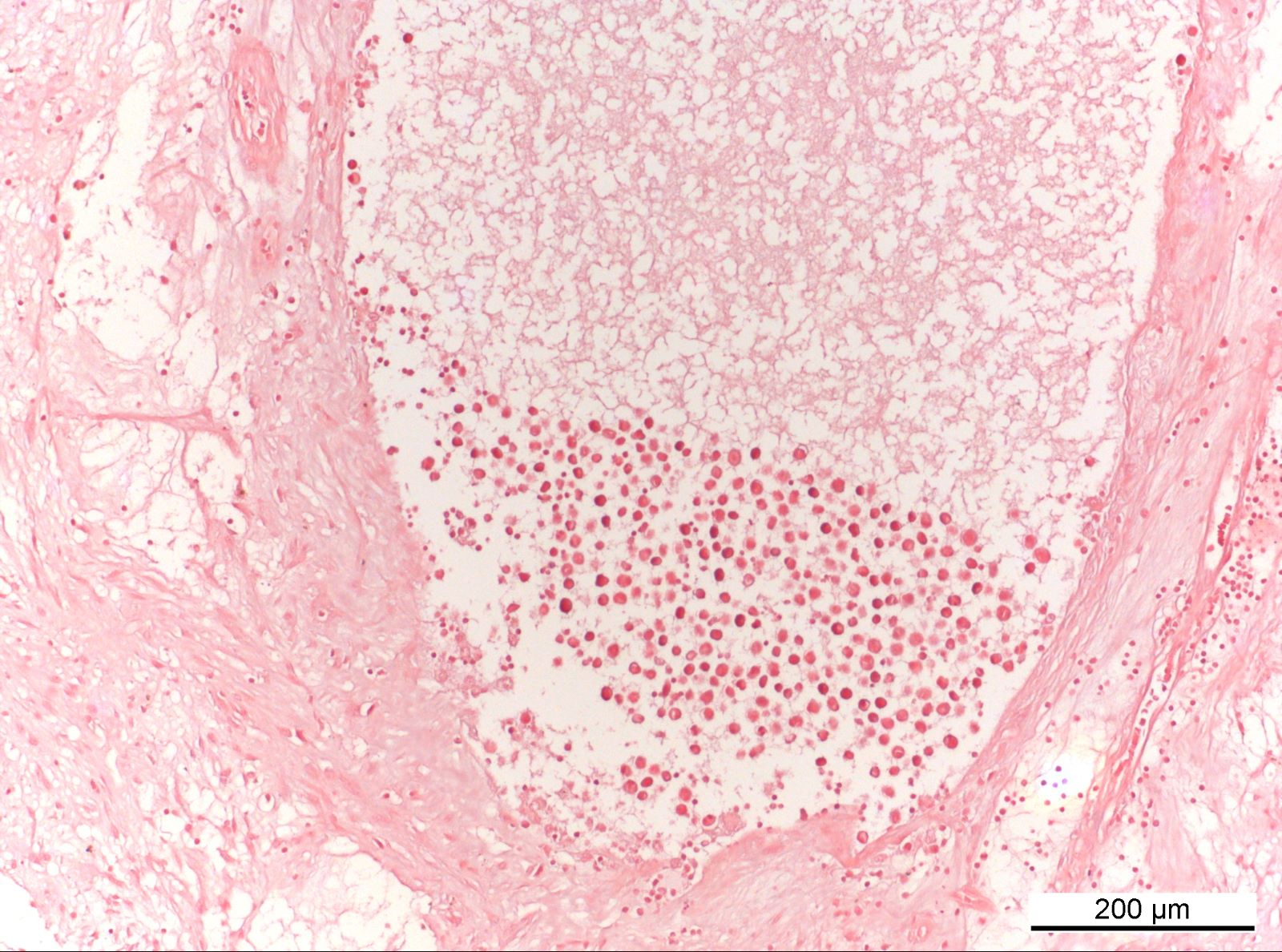
Gross description
- No gross tumor mass or evidence of lymphoma
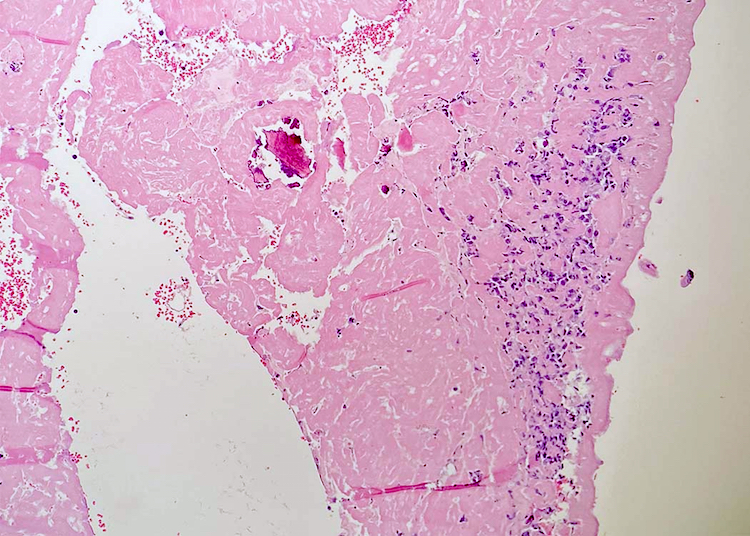
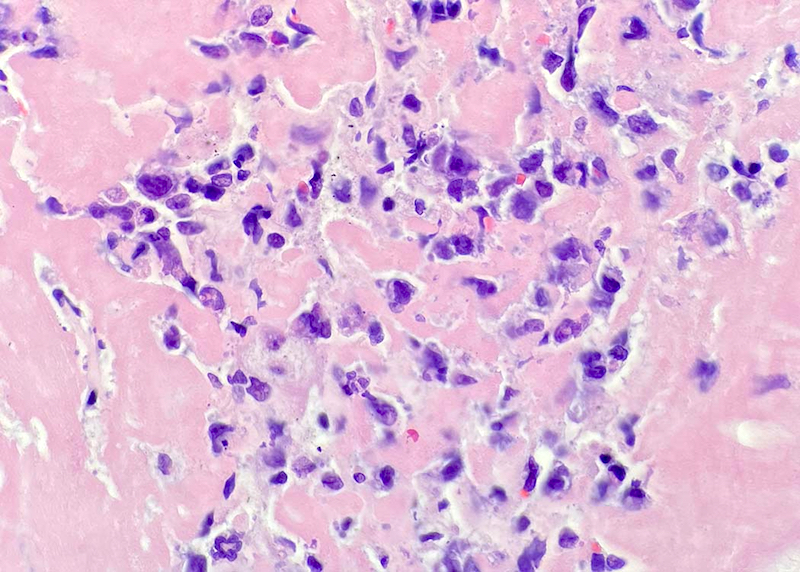
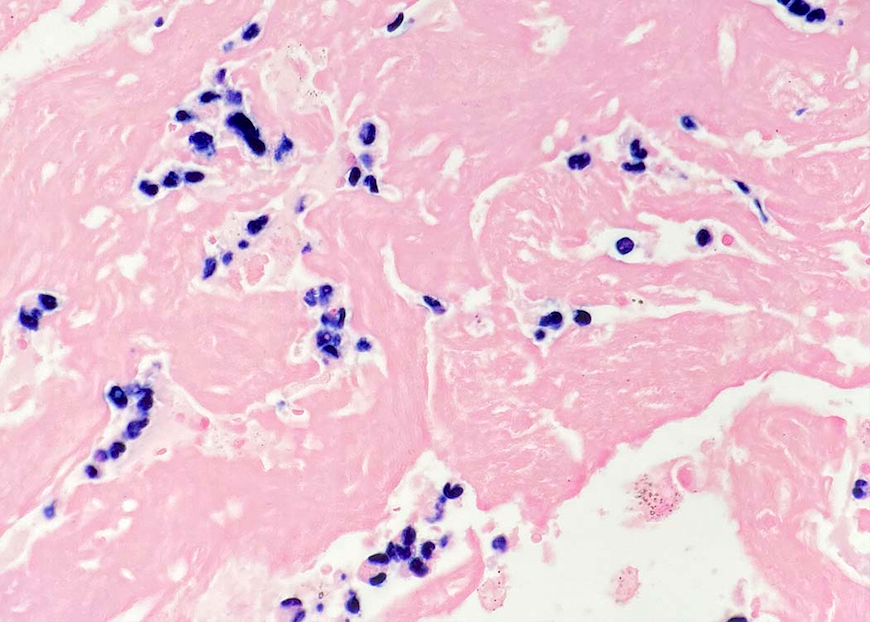
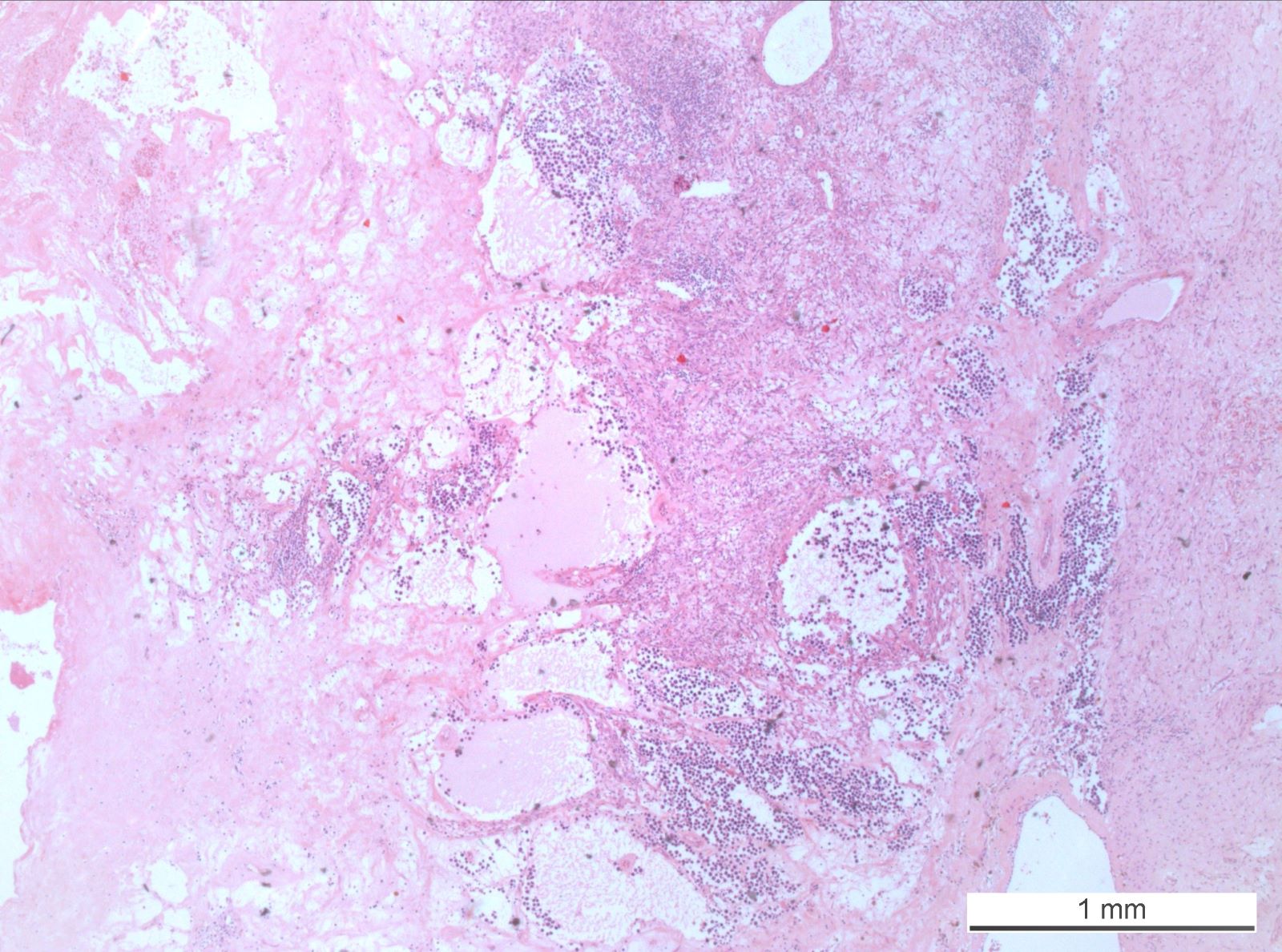
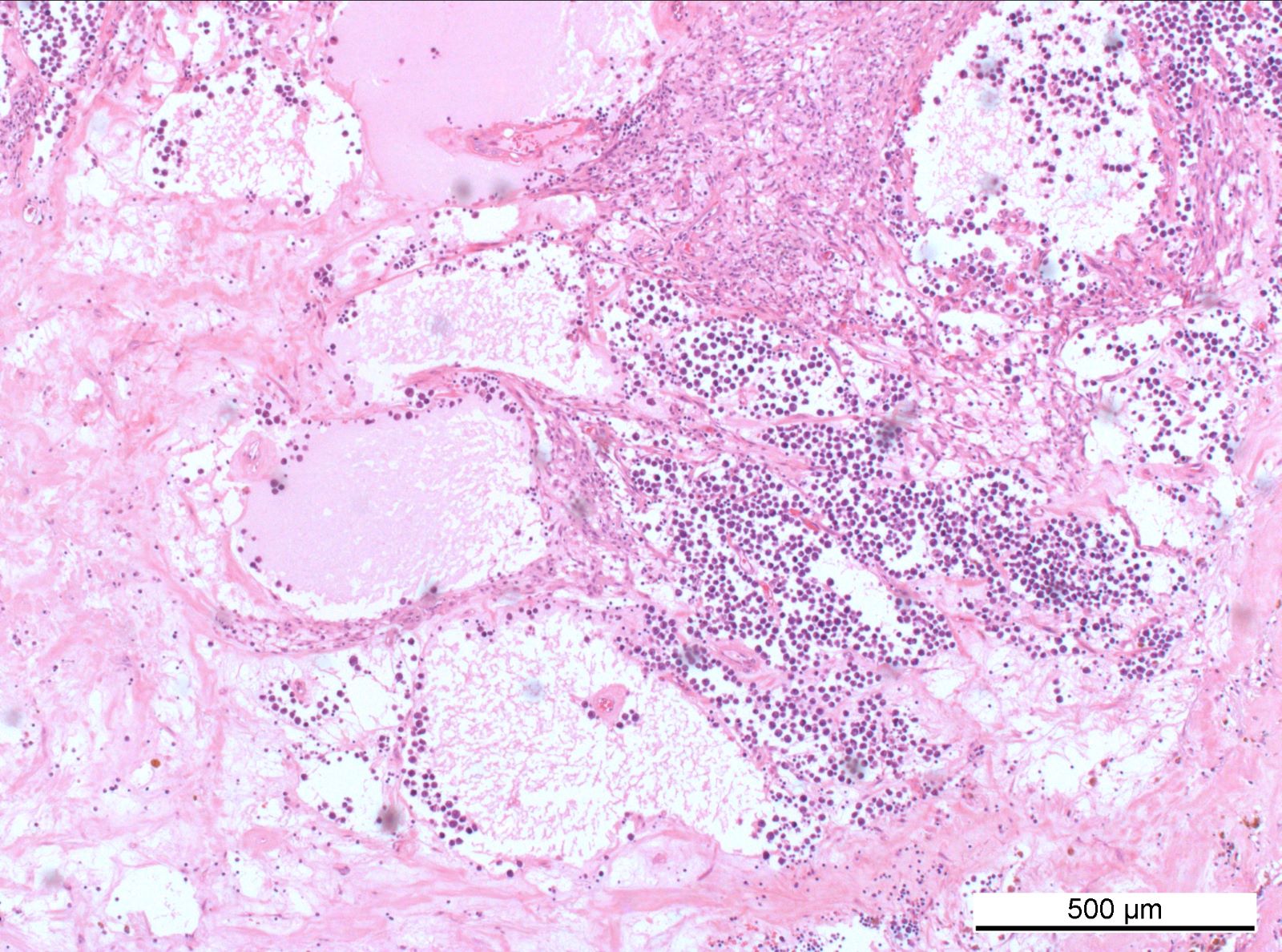
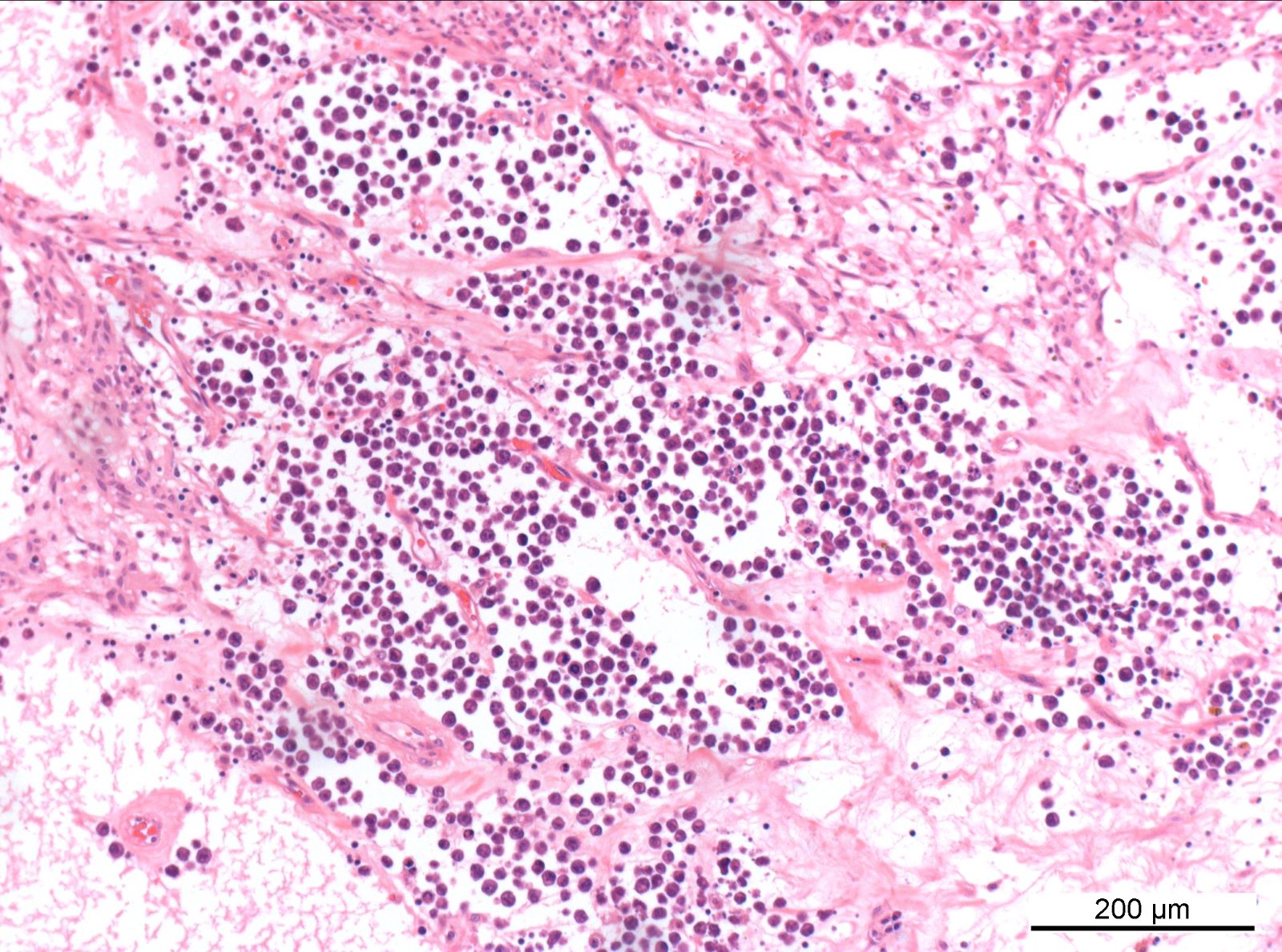
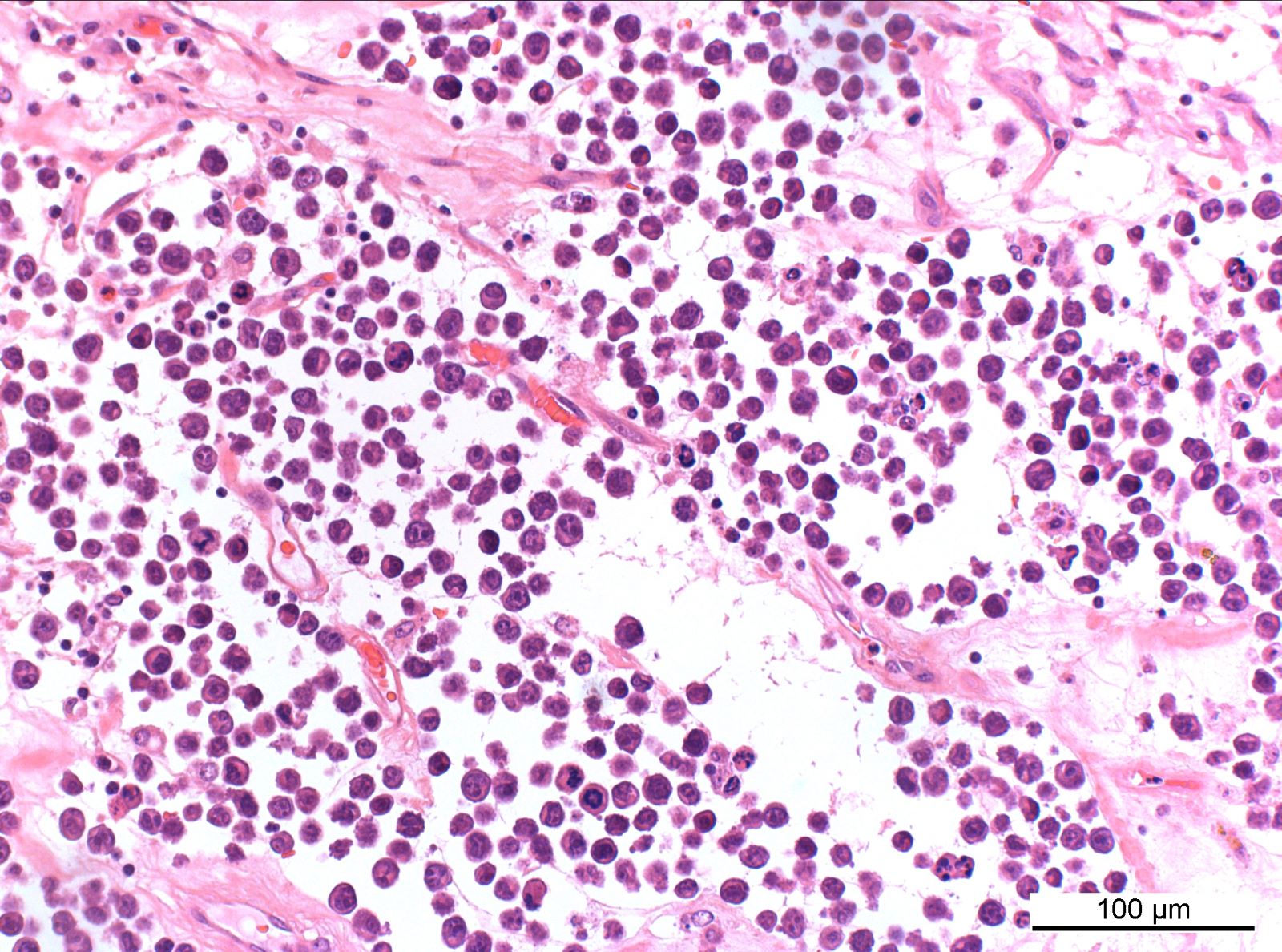
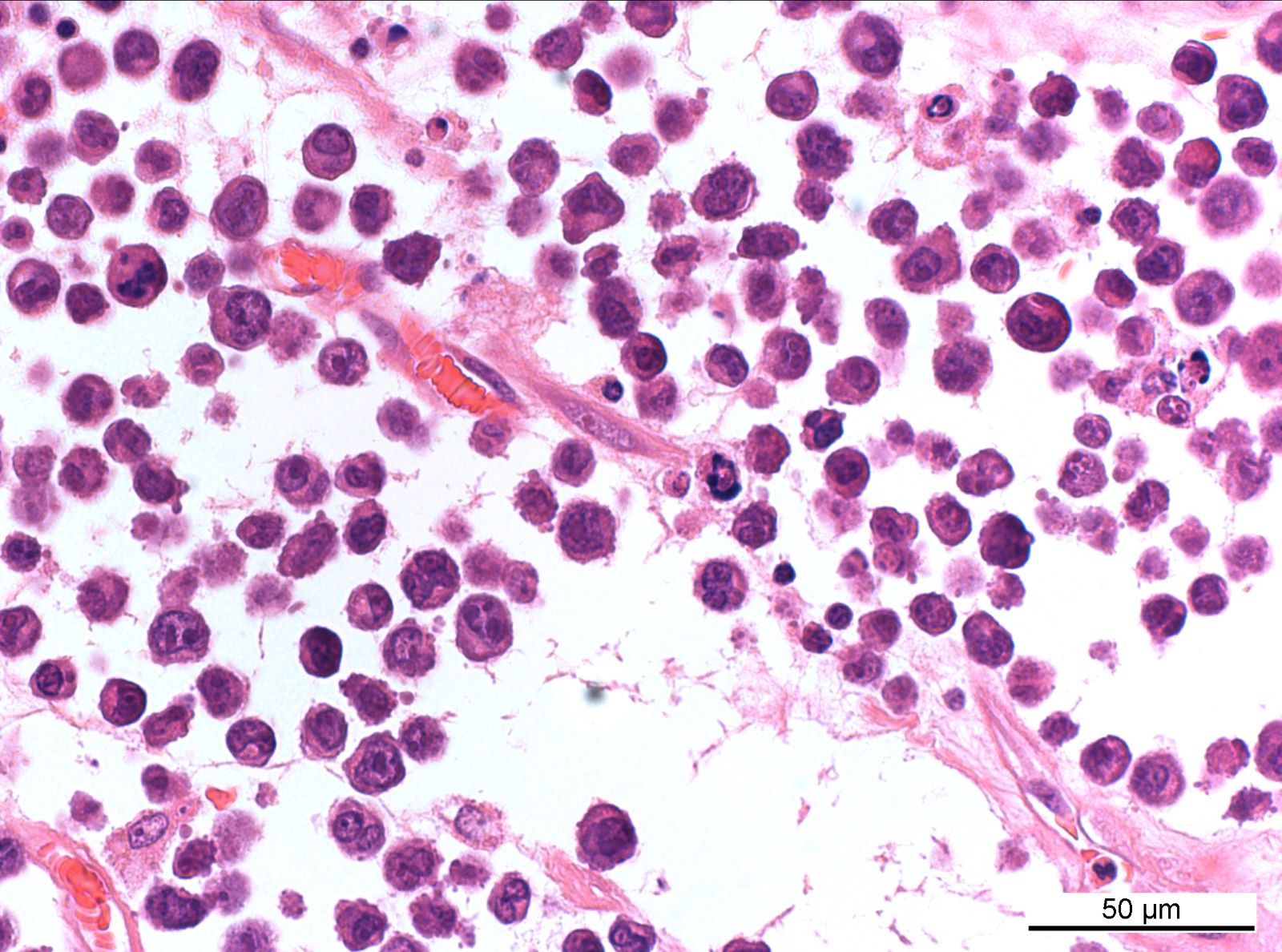
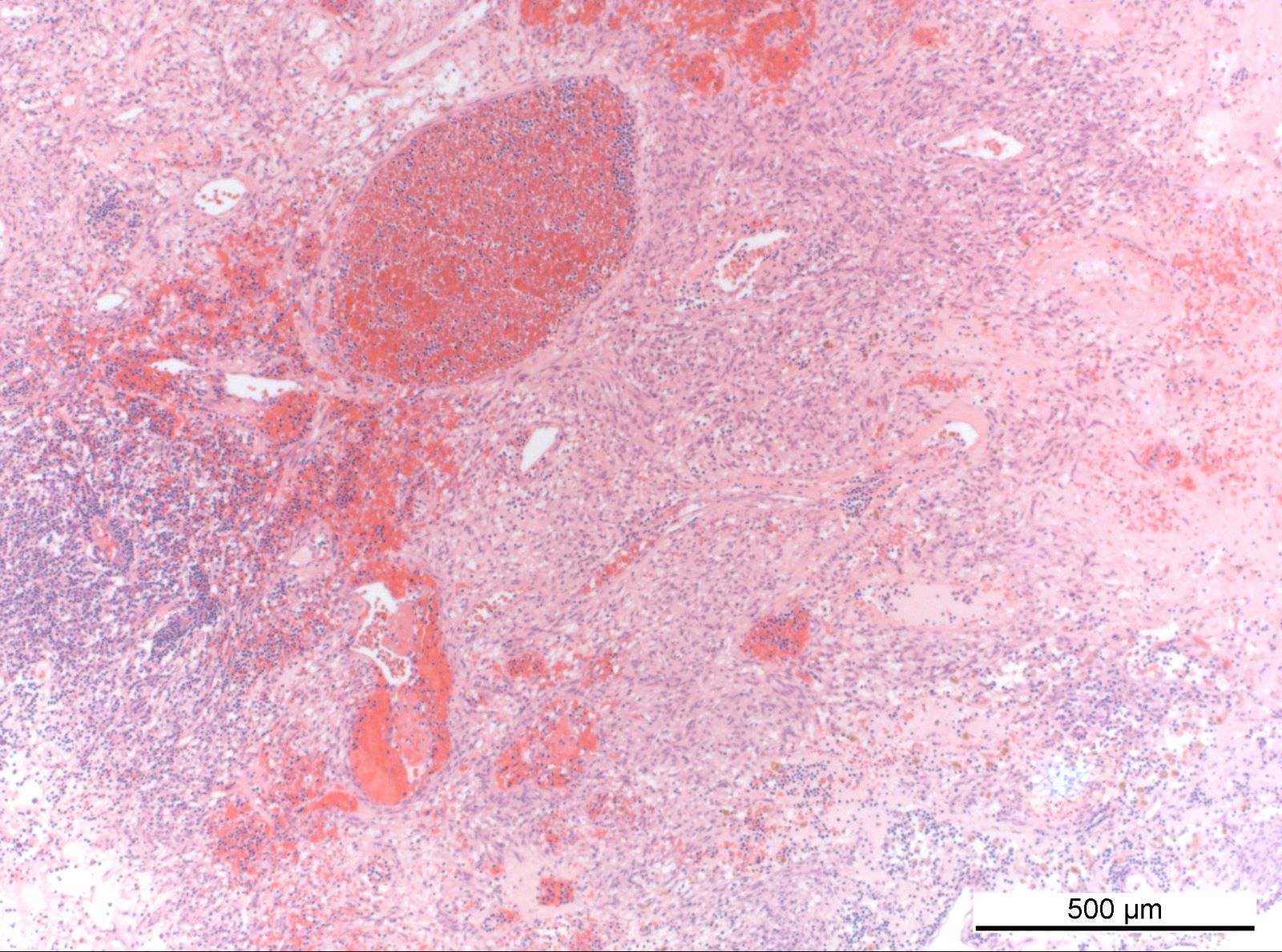
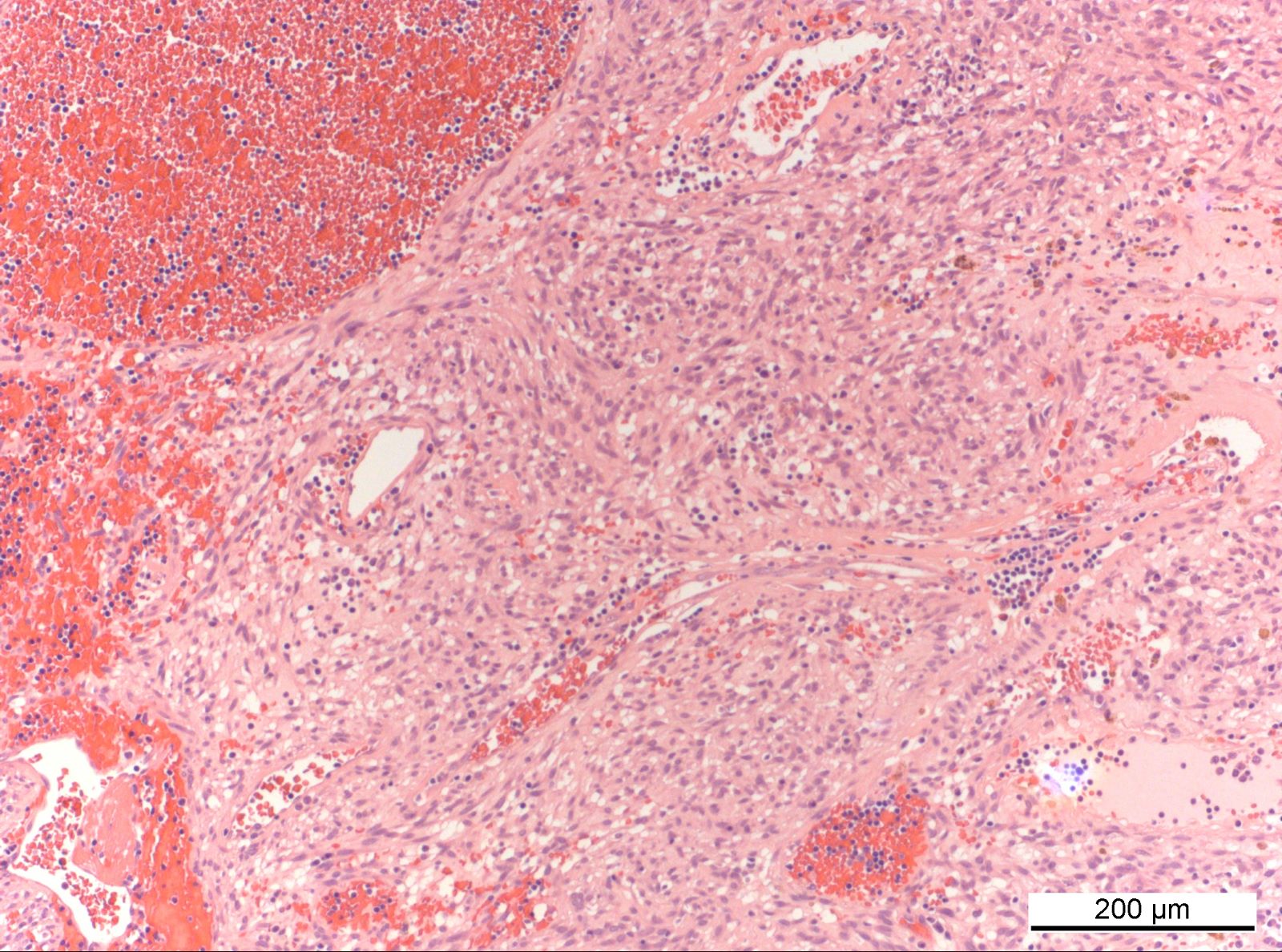
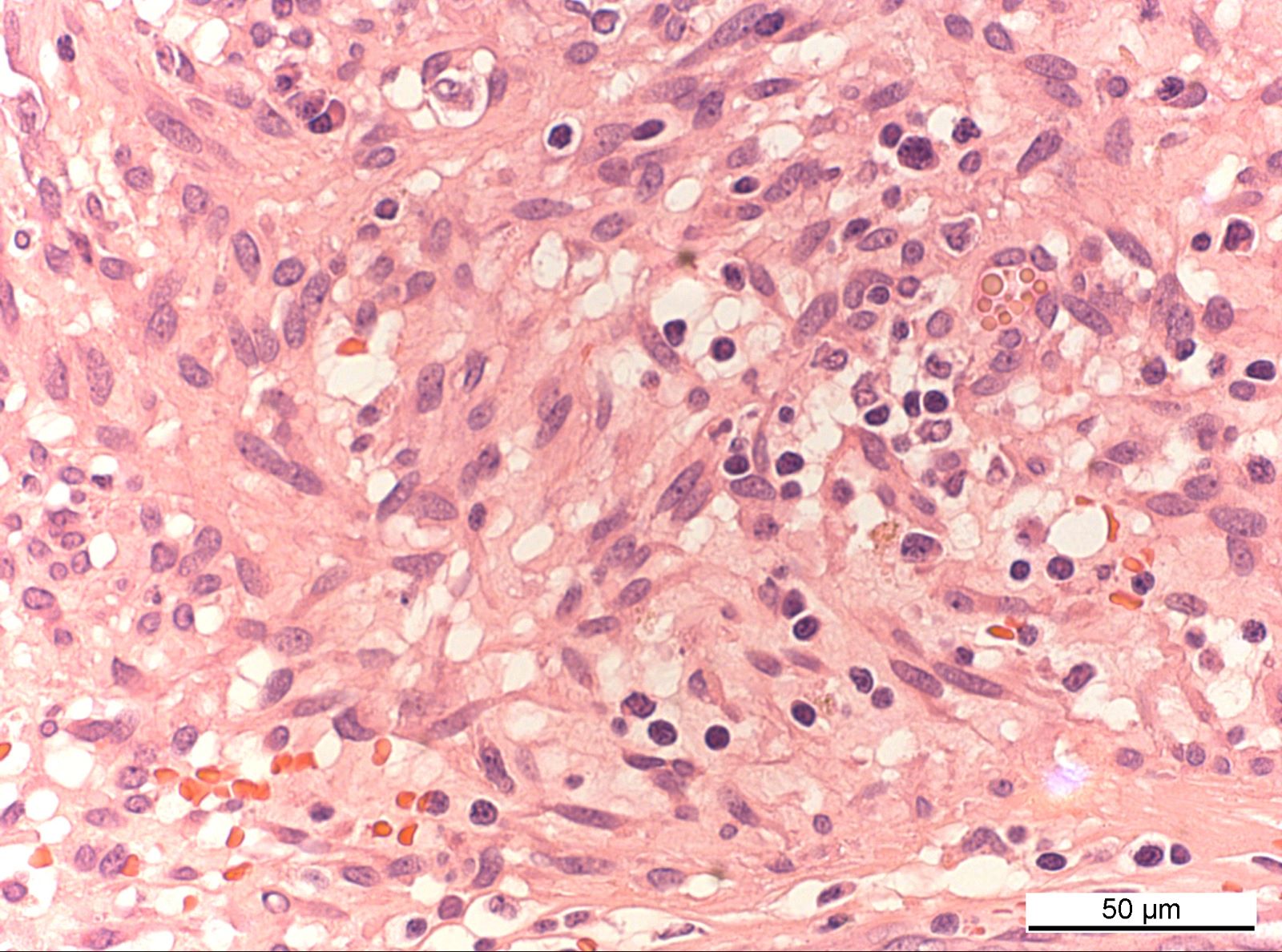
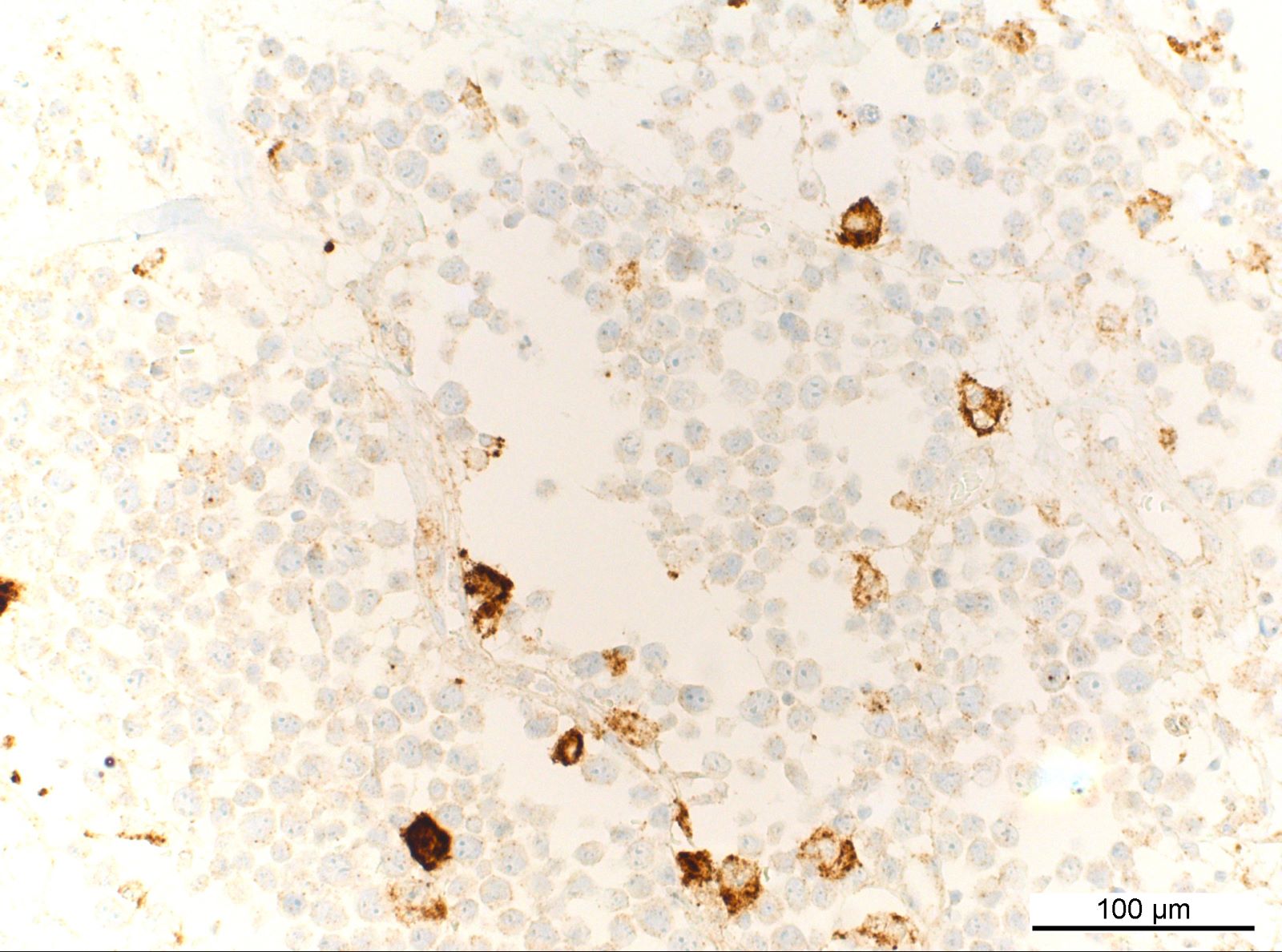
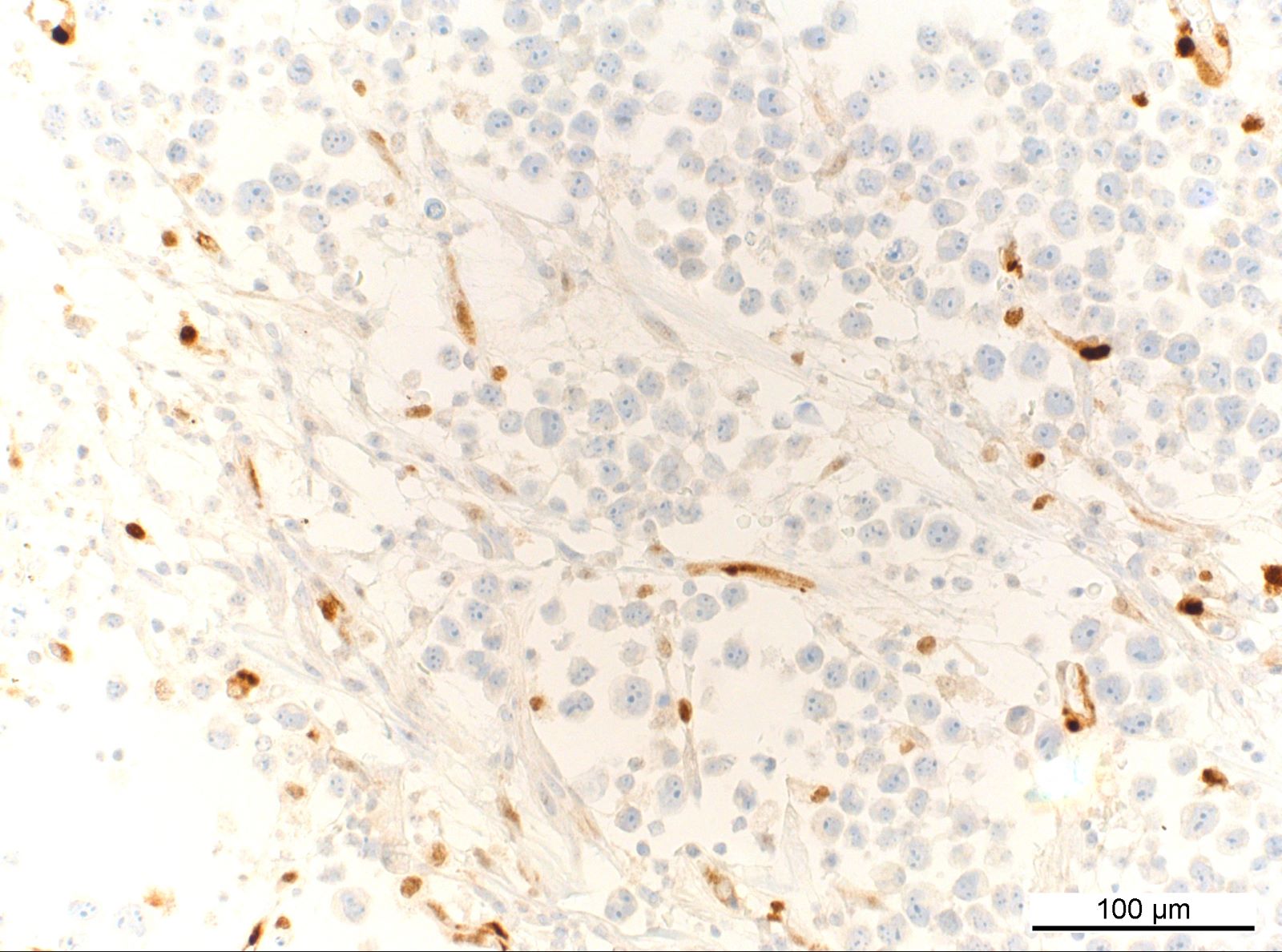
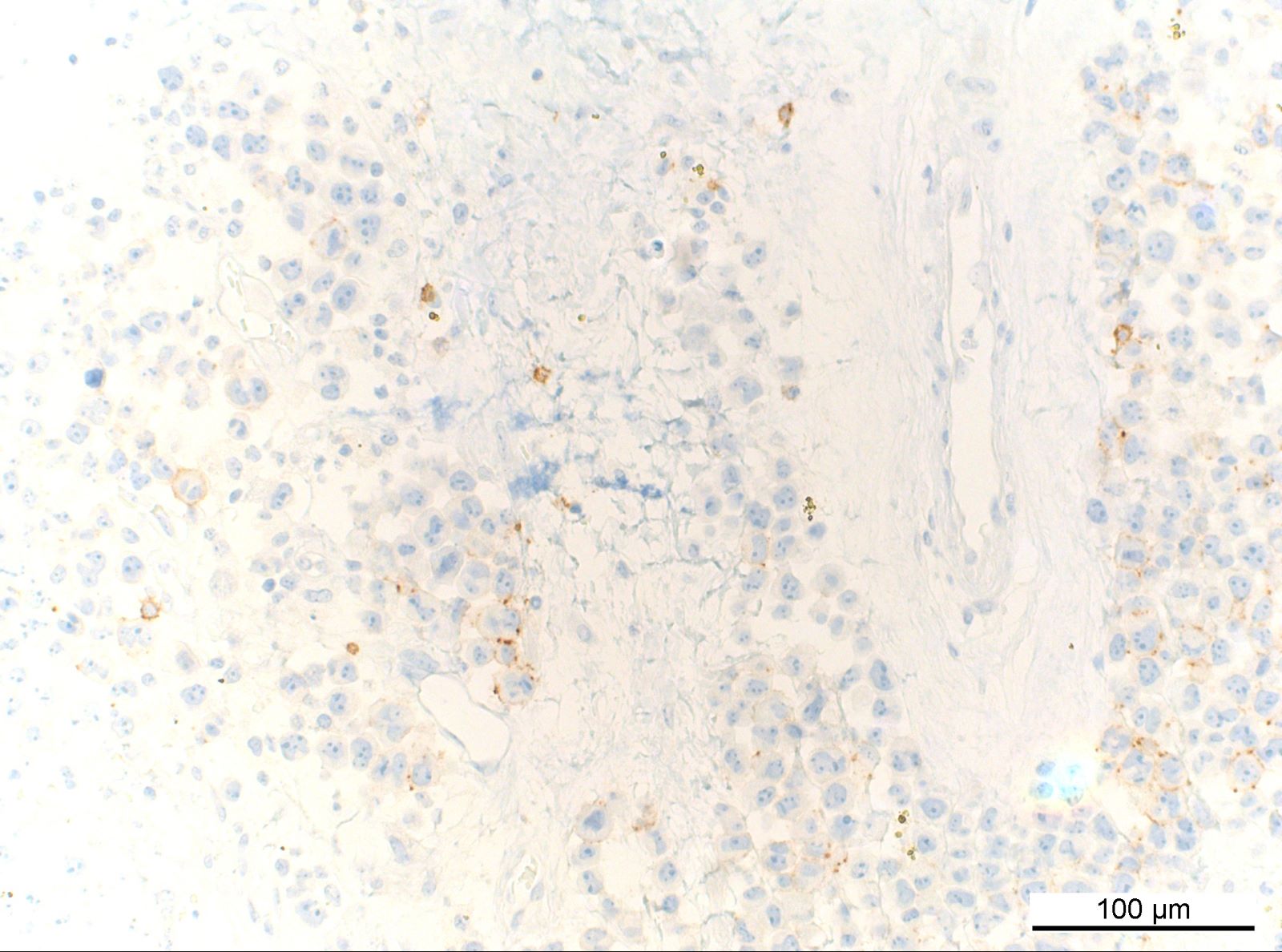
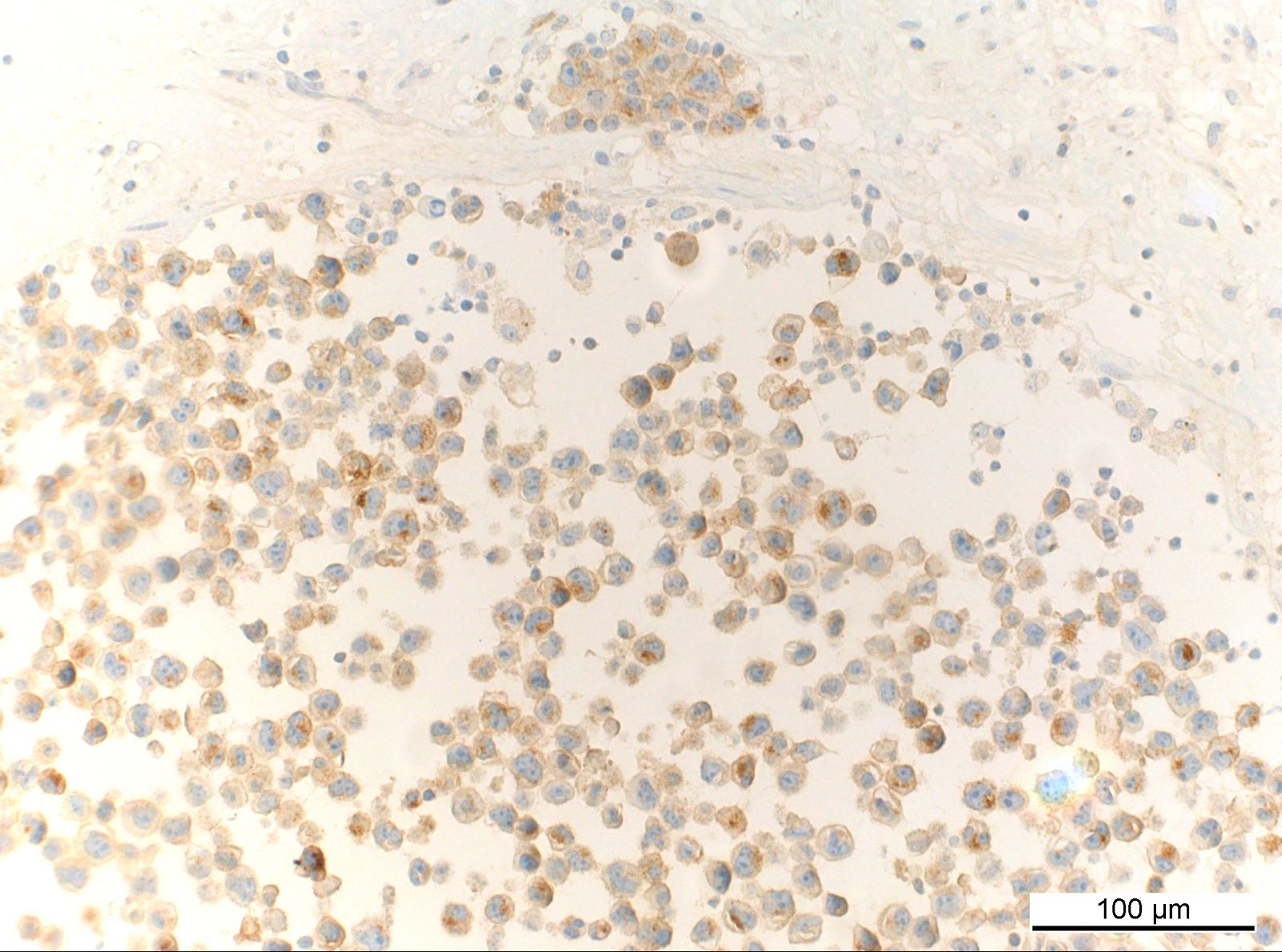
Microscopic (histologic) description
- Small foci of lymphoma cells in fibrinous or amorphous eosinophilic material
- Aggregates / clusters
- Ribbons
- Single cells
- Neoplastic cells are large and atypical
- Irregular nuclear contours
- Coarse chromatin
- Distinct nucleoli
- Amphophilic cytoplasm
- May be plasmacytoid or bizarre appearing
- Mitotic figures and apoptotic bodies present
- Lack of lymphomatous infiltration or effacement of adjacent normal tissues
- Usually lacks prominent inflammatory background in vicinity of lymphoma cells
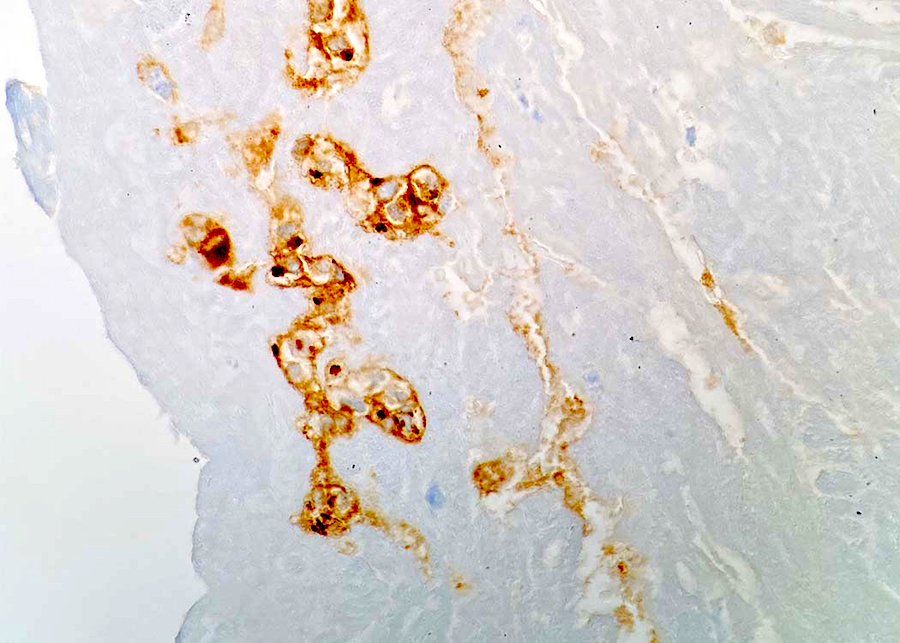
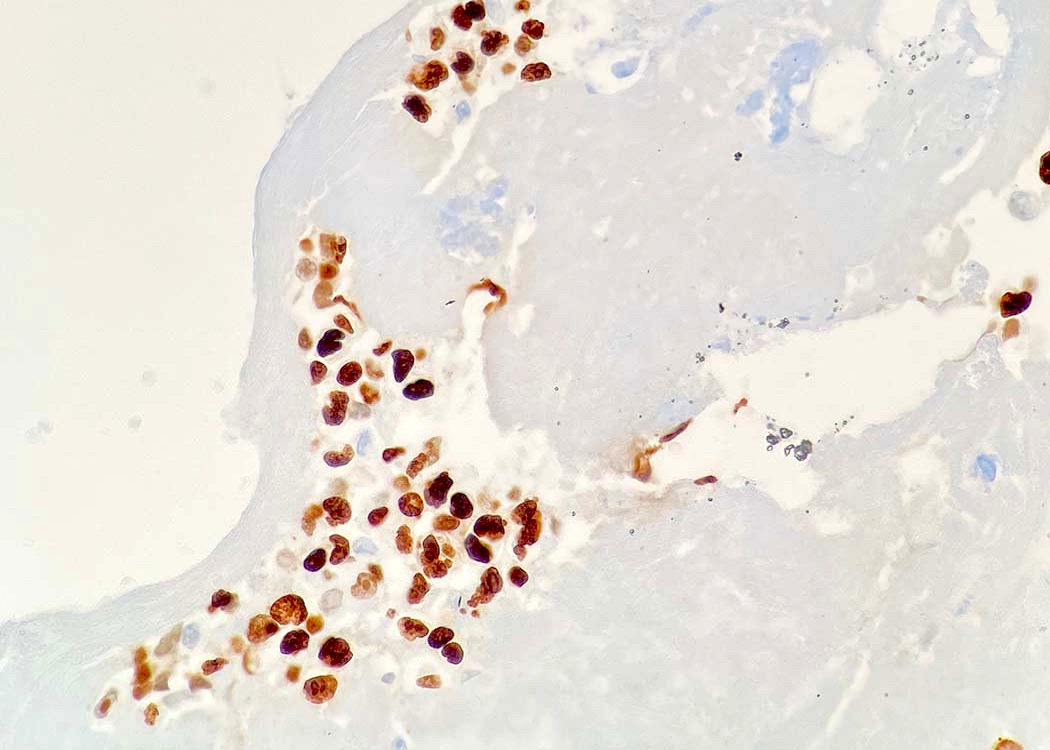
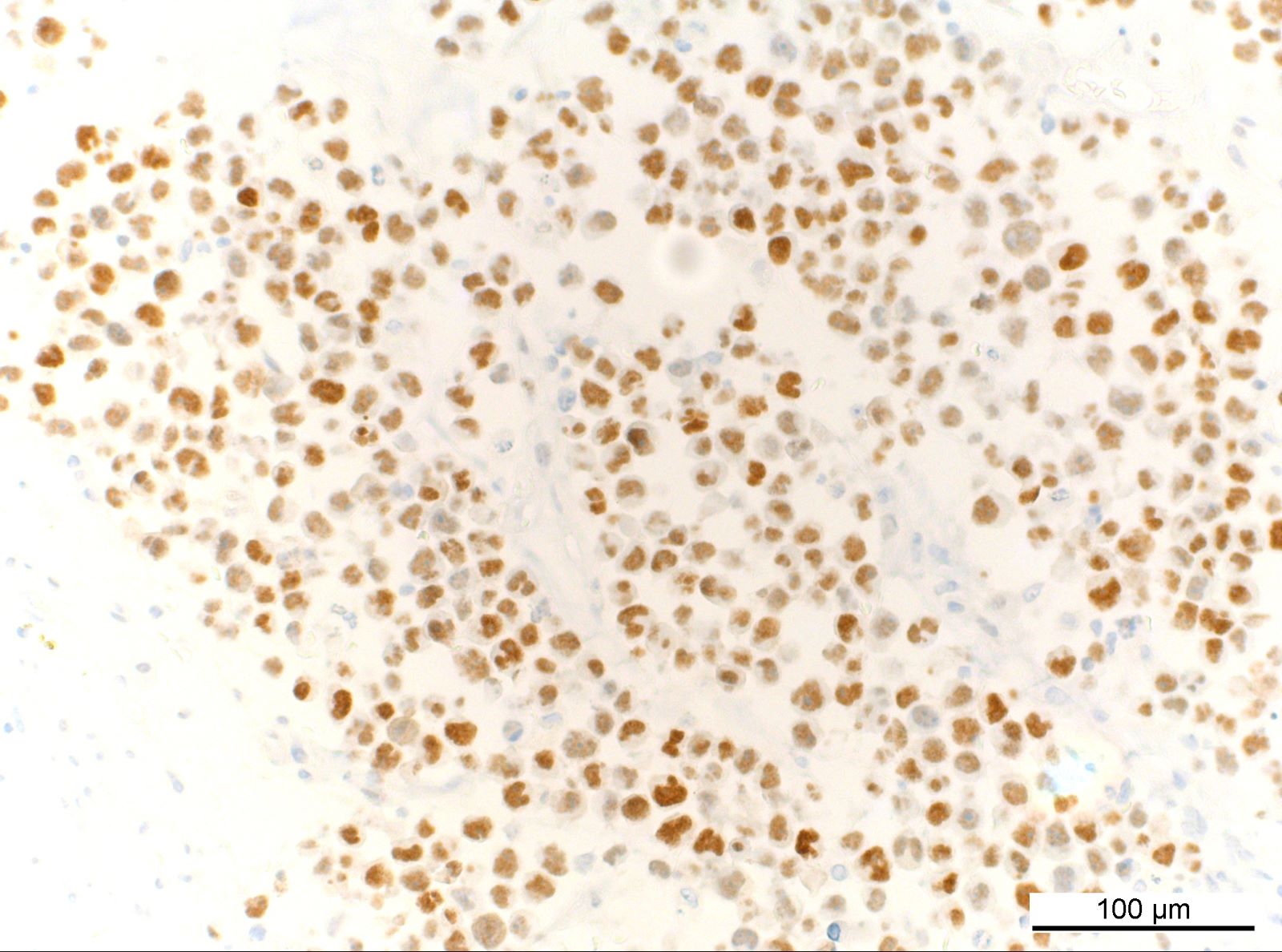
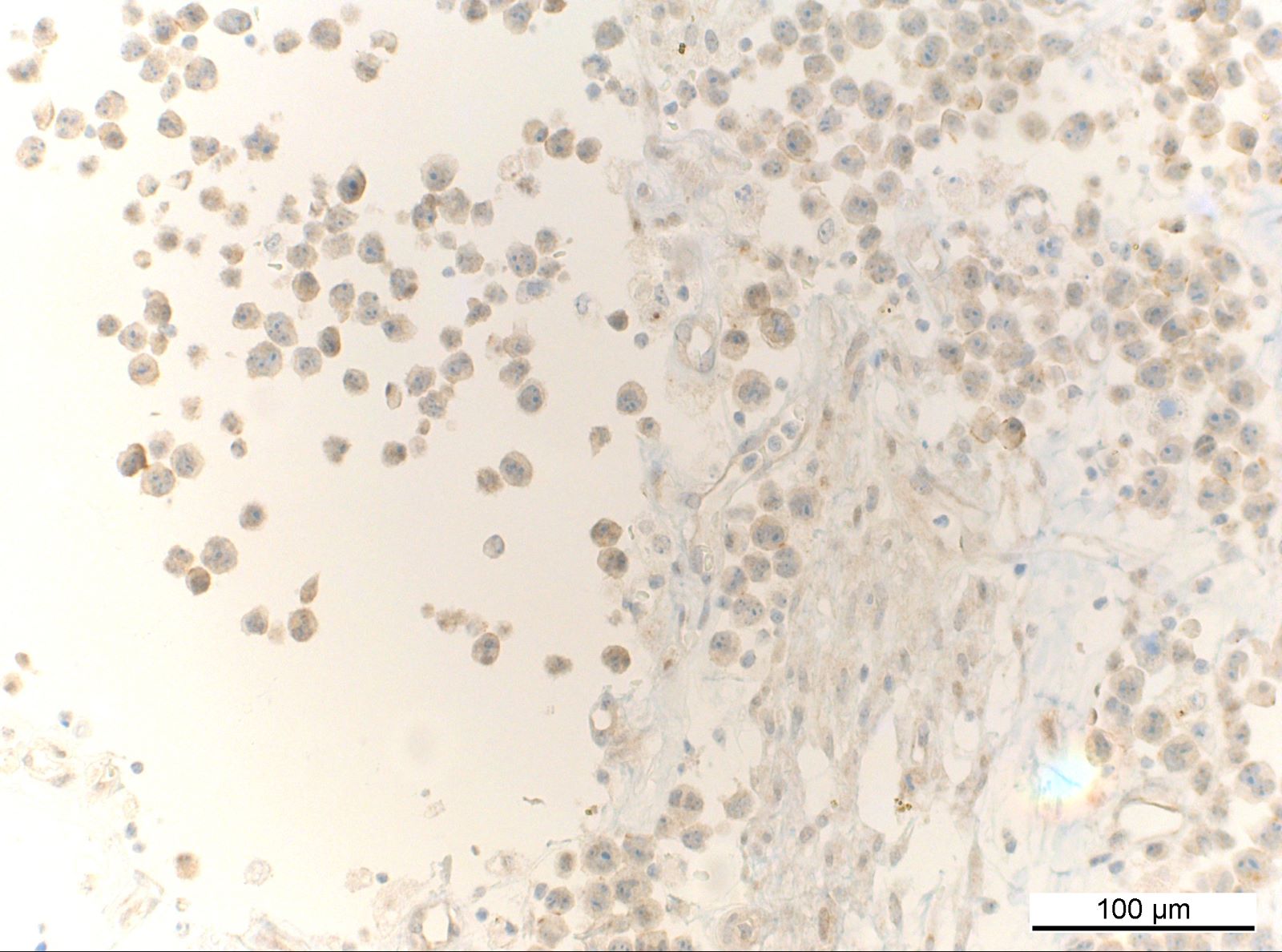
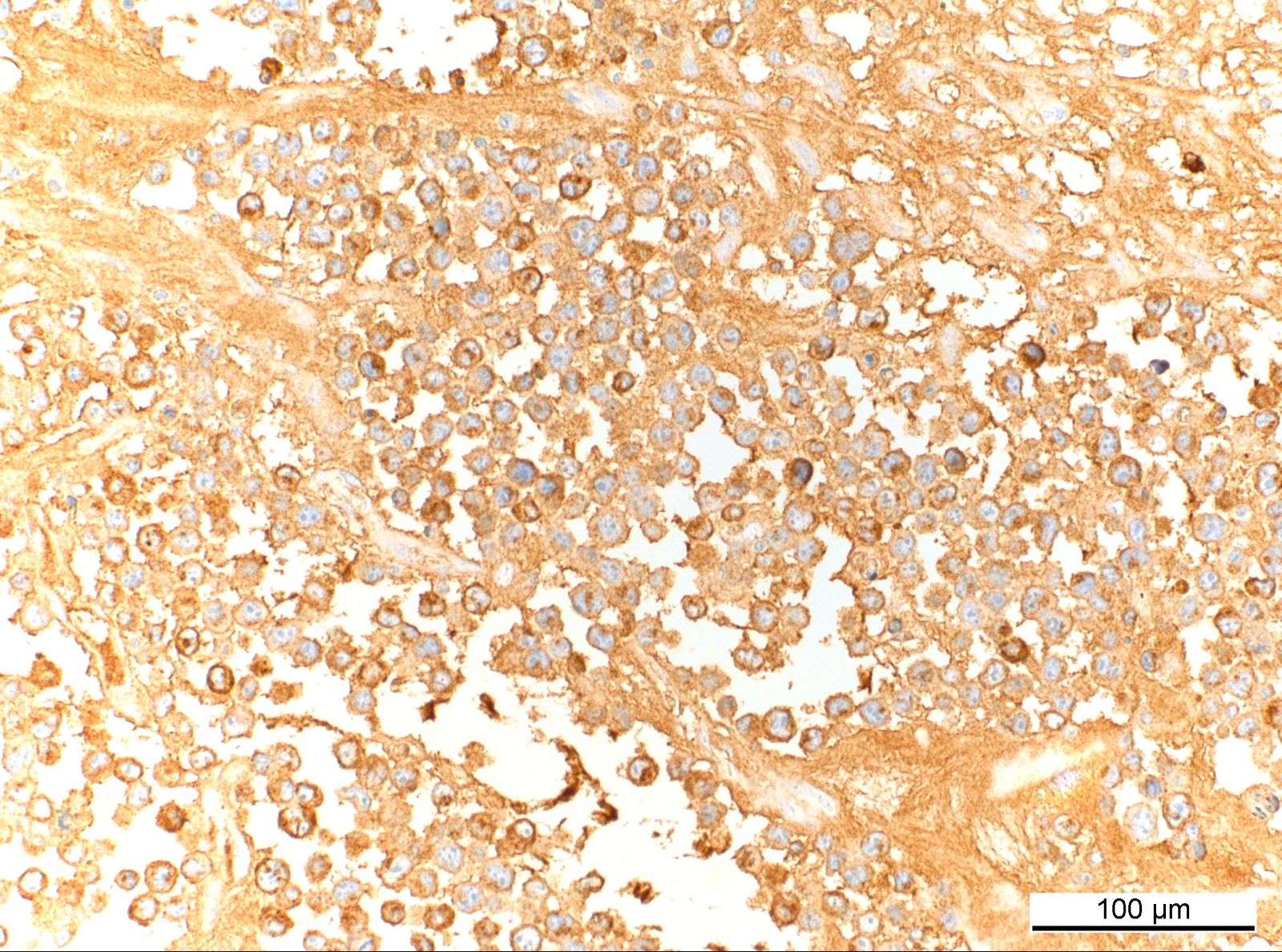
Microscopic (histologic) images
Contributed by Jordan M. Hall, M.D., Hyunkyu Shin, M.D., Dr. Christian Schürch, M.D., Ph.D., Falko Fend, M.D. and Claudia Wickenhauser, M.D., Ph.D. (Case #529)
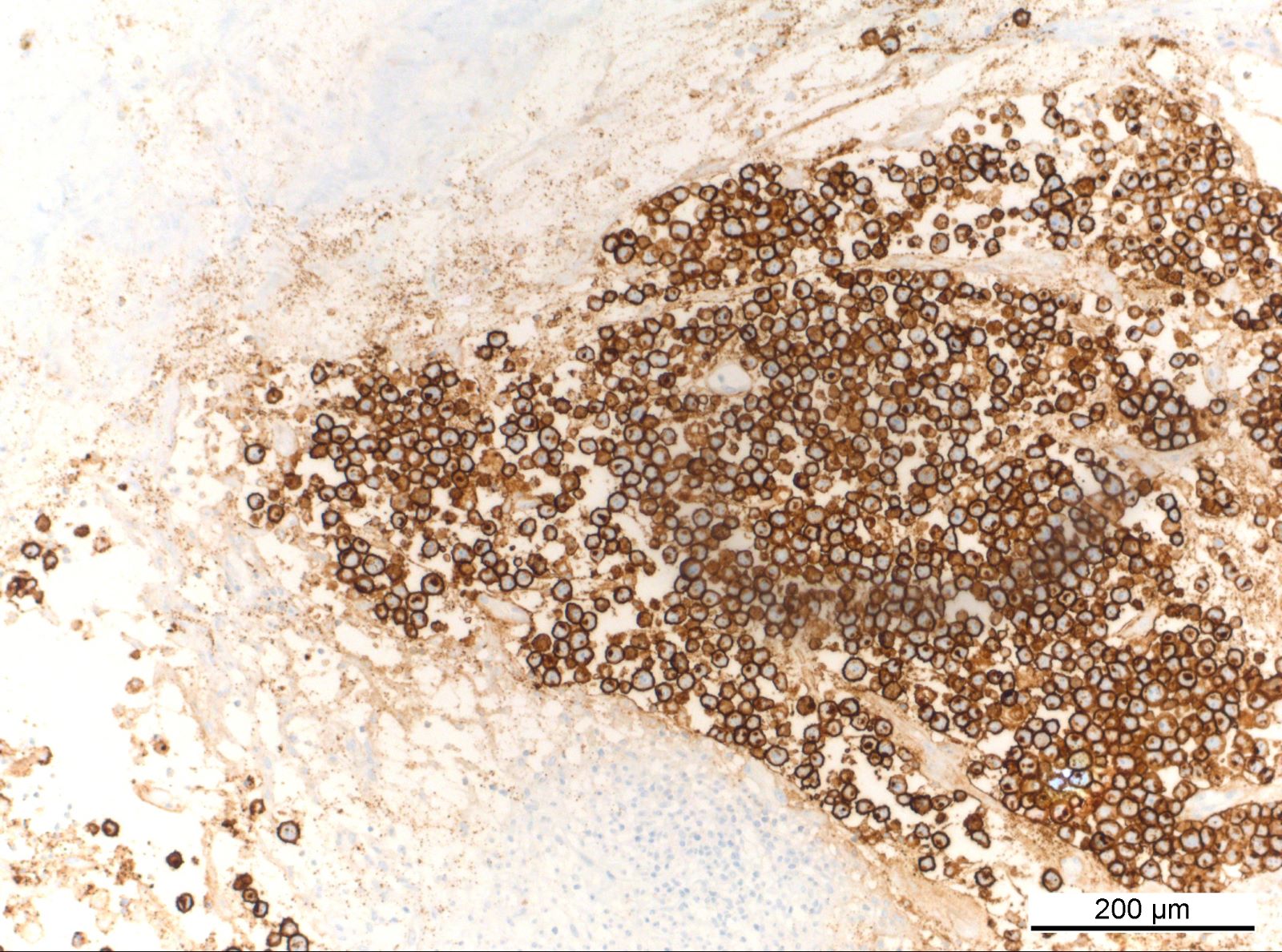
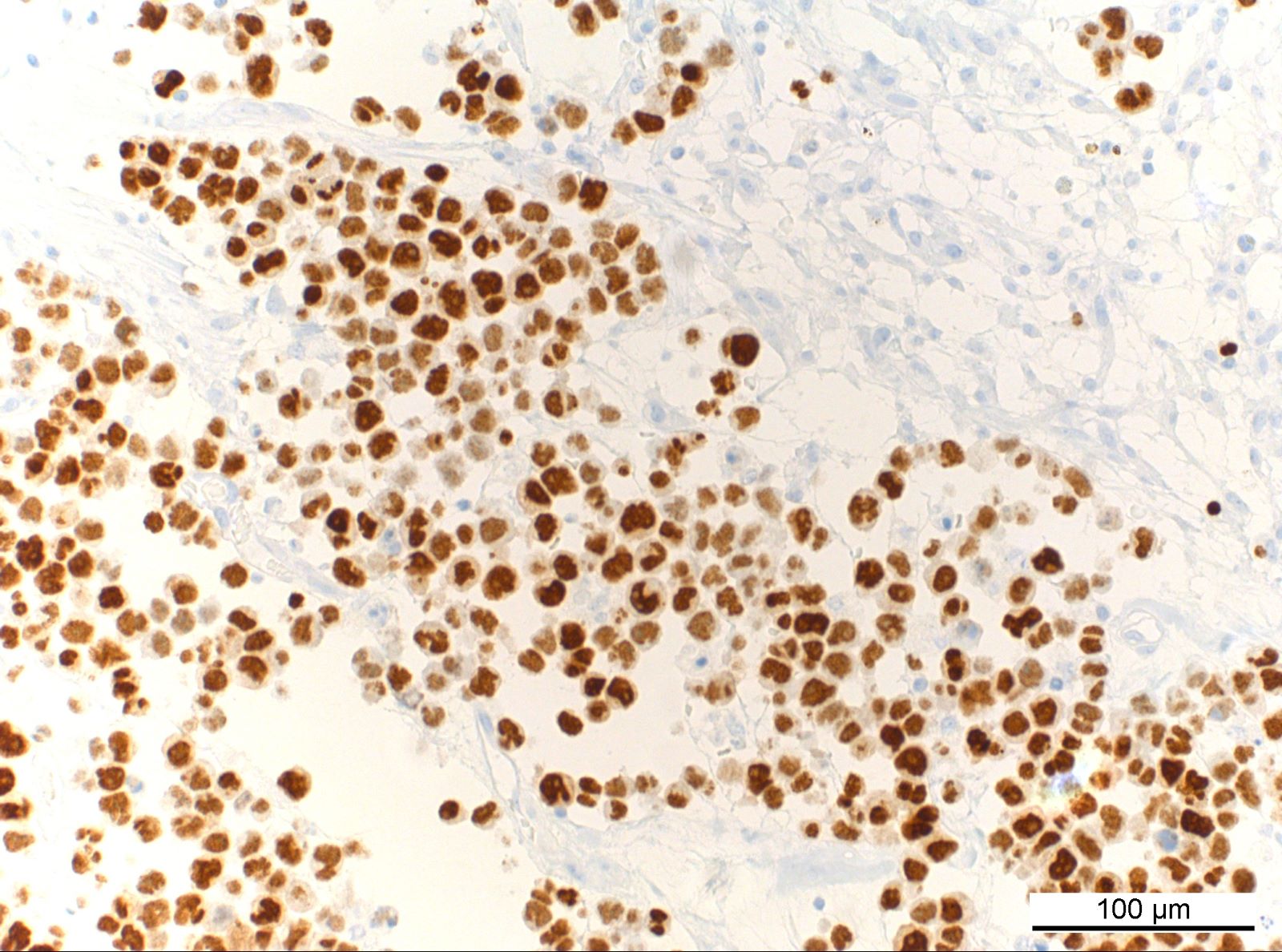
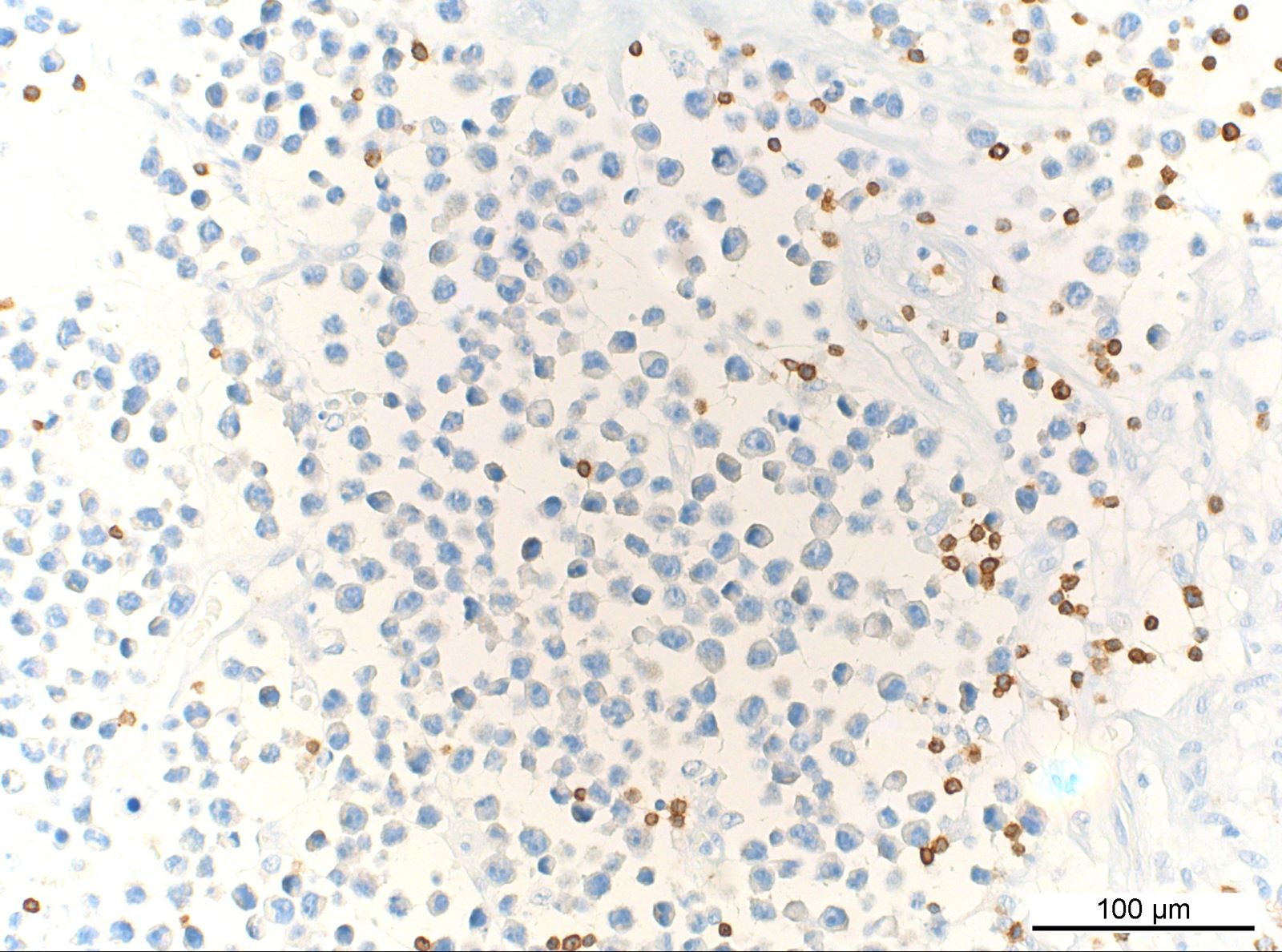
Positive stains
- EBV (EBER) positive in majority of cells
- CD20, PAX5, CD79a
- MUM1
- The majority of cases show a Ki67 proliferation rate of > 90% and are positive for CD30 and PDL1 (Am J Surg Pathol 2017;41:299)
- CD43 (75%) (Mod Pathol 2010;23:493)
- Parentheses with percentages indicate the percent of cases
Molecular / cytogenetics description
- Clonal immunoglobulin gene rearrangement (4 of 4 cases tested) (Am J Surg Pathol 2017;41:299)
Sample pathology report
- Soft tissue, right subpatellar space, excision:
- Fibrin associated diffuse large B cell lymphoma (see comment)
- Comment: Histopathologic evaluation reveals fragments of synovium with patchy chronic inflammation and abundant eosinophilic fibrinous material. Within and limited to the fibrin, there are scattered small collections of large atypical lymphoid cells noted. Immunohistochemistry shows these cells are positive for CD20, PAX5, CD30 and CD43, express an activated B cell immunophenotype (CD10 negative, BCL6 negative, MUM1 positive) and show a high proliferative rate (> 90% Ki67 positivity). These cells are also positive for Epstein-Barr virus encoded small RNA (EBER) by chromogenic in situ hybridization. Negative stains include CD3, CD15, CD68, CD163, CD138, ALK1 and SOX11. Impression: The histopathologic findings and available clinical history of arthroplasty without clinical suspicion for neoplasia support a diagnosis of FA DLBCL. This is a clinically indolent lymphoproliferative disorder that is confined to a restricted anatomic space, typically an incidental finding on histopathologic examination only and usually adequately treated with surgical excision alone. That being said, correlation with the complete clinical and radiologic workup is recommended to exclude the possibility of more aggressive systemic disease.
Differential diagnosis
- DLBCL associated with chronic inflammation:
- Older age, longer latency, symptomatic mass with infiltration / effacement, higher mortality (54%) (Am J Surg Pathol 2017;41:299)
- EBV+ DLBCL, NOS:
- Normal tissue infiltration / effacement
- Primary effusion lymphoma:
- Immunodeficiency associated lymphoproliferative disorders (e.g. PTLD, primary immunodeficiency or other iatrogenic immunodeficiency):
- More extensive lymphoid proliferation, normal tissue infiltration or effacement, pertinent clinical history
- Plasmablastic lymphoma:
- Normal tissue infiltration / effacement, often HIV associated
- Classic Hodgkin lymphoma:
- Normal tissue infiltration / effacement, Hodgkin / Reed-Sternberg cell morphology, prominent inflammatory background
- Breast implant associated anaplastic large cell lymphoma:
Additional references
Board review style question #1
Board review style answer #1
Board review style question #2
- Fibrin associated diffuse large B cell lymphoma is currently included in the 2017 revised WHO classification as a subtype of which entity?
- Anaplastic large cell lymphoma
- Diffuse large B cell lymphoma associated with chronic inflammation
- EBV positive diffuse large B cell lymphoma, NOS
- High grade B cell lymphoma
- Primary effusion lymphoma
Board review style answer #2
B. Diffuse large B cell lymphoma associated with chronic inflammation
Comment Here
Reference: Fibrin associated large B cell lymphoma
Comment Here
Reference: Fibrin associated large B cell lymphoma
Board review style question #3
- Which of the following is a true feature of fibrin associated large B cell lymphoma (FA-LBCL)?
- Distinguishing this tumor from chronic inflammation associated (CI-)LBCL has no clinical importance because both are inflammation associated indolent neoplasms
- The neoplastic cells are derived from germinal center B cells
- This neoplasm is strongly associated with EBV infection with type III latency
- This tumor is a highly aggressive lymphoid neoplasm due to its association with acute fibrous inflammation
- With discohesive neoplastic cells, this tumor readily infiltrates pre-existing anatomic structure
Board review style answer #3
C. This neoplasm is strongly associated with EBV infection with type III latency. Except for rare cases as presented here, FA-LBCL is consistently associated with EBV infection showing type III latency with LMP1 and EBNA2 positivity. Answer A is incorrect because CI-LBCL exhibits a more aggressive clinical course than FA-LBCL with similar morphology, so these two entities should be clearly distinguished. Answer B is incorrect because the neoplastic cells of FA-LBCL show an activated (nongerminal center) B cell phenotype (CD10-, BCL6+/-, MUM1+). Answer D is incorrect because FA-LBCL is an indolent lymphoid neoplasm, so it is often discovered incidentally during careful examination. Answer E is incorrect because this tumor is mostly confined to cystic or pseudocystic spaces without infiltration of pre-existing anatomic structures or mass formation.
Comment Here
Reference: Fibrin associated large B cell lymphoma
Comment Here
Reference: Fibrin associated large B cell lymphoma